How To Take Gynecological History Authors Dr Manisha




- Slides: 21
How To Take Gynecological History Author(s): Dr Manisha Mathur, MBBS, MRCOG (UK) Level: Basic Academic Affiliation : KK Women's and Children's Hospital Department of O&G, Consultant Version No: 1. 0 Submitted: August 2016 Editors’ Review:
2 Role of a Doctor • Listening to the patient tell her story • Generating a hypothesis • Testing the hypothesis – By interrogation 50% – By examination 10% – By selective testing 40% • If at first you don’t succeed… • Go back and listen to the patient
3 Considerations • History taking sequence remains same • Should follow a logical and chronological sequence • Some unique areas of focus specific to specialty • Requires sensitivity and preservation of dignity for the patient • Ensure confidentiality • Always consider the possibility of pregnancy when presented with abnormal bleeding or pain
4 Presenting Complaint The Gynecological History follows the usual method of taking a history but there are specific key areas that need to be expanded on. These are: • Menstrual history • Common gynae issues: vaginal discharge, abdominal/pelvic mass • Contraception and sexual health • Obstetric history • Uro-gynecological history • Pap smear and related vaccination history • Past gynae/surgical history
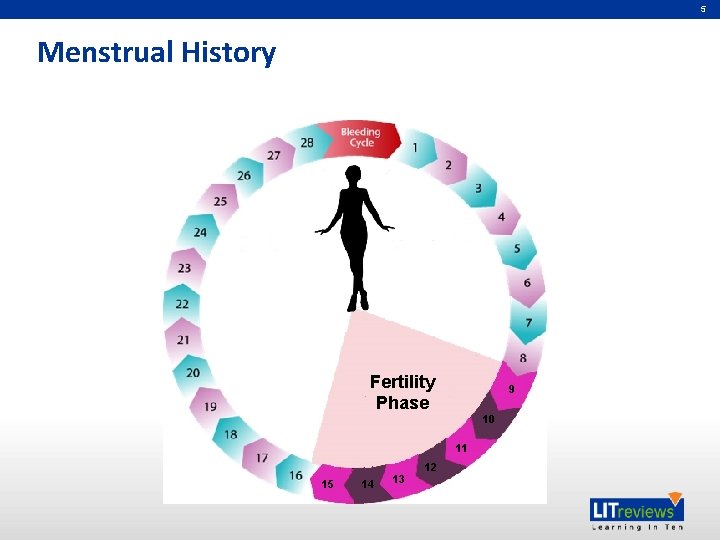
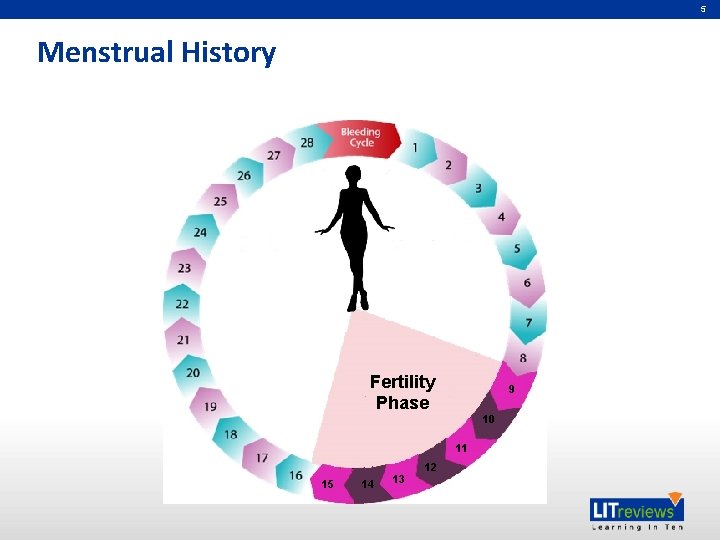
5 Menstrual History Fertility Phase 9 10 11 15 14 13 12
6 Patterns of Abnormal Menstrual Loss • Menorrhagia – Excessive menstrual loss at regular intervals • Metrorrhagia – Frequent and irregular menstrual loss • Polymenorrhoea – Regular cycles at <21 days • Oligomenorrhoea – Infrequent menstruation (>35 days) • Intermenstrual Bleeding – Bleeding between menstrual periods – Requires careful questioning
7 Menstrual History: Tips • Tell me about your Menses? – – – Age at menarche LMP? Arrive at expected time? Pattern of bleeding Was last period normal? • How often do they occur? Regularly? Irregularly? – Do they “come early” or do they “come late” – Regular menses – range 21 to 35 days – Usually 28 to 30 days • How long do they last for? – From the beginning of one period to the beginning of the next

8 Menstrual History: Tips • Estimating menstrual loss – How frequent do you change pad? – Pad completely soaked? – Clots/flooding • Are periods painful? Normally painful? – When does pain start? (Before menses or with menses? ) – Severity…. does it keep you off work? • Changes in period pattern? • Any post-coital bleeding (PCB)? • Any inter-menstrual bleeding (IMB)? – Ask specifically about brown or bloody discharge between periods
9 Menorrhagia Used loosely means excessive menstrual loss….
10 What is Excessive Menstrual Loss? • Escapes from normal menstrual protection • Large clots – frequently • Changing at night more than once • Lasts longer than 7 days “full flow” • Interferes with normal life or duties • Causes iron deficiency (anaemia) – Other causes excluded
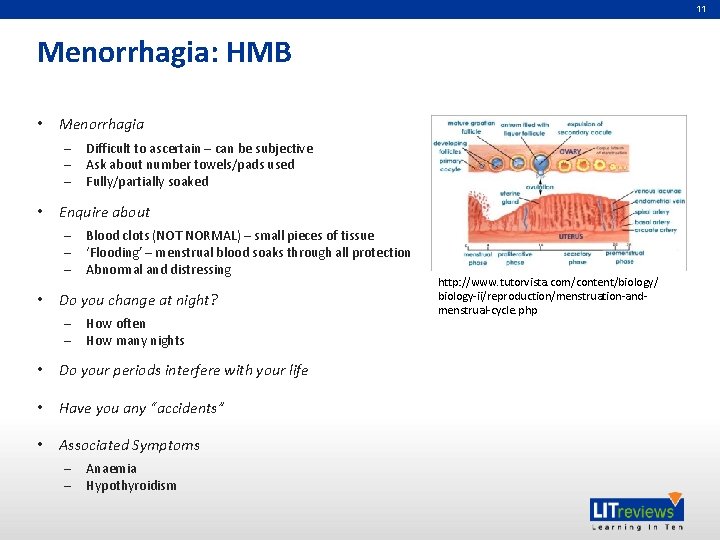
11 Menorrhagia: HMB • Menorrhagia – – – • Enquire about – – – • Difficult to ascertain – can be subjective Ask about number towels/pads used Fully/partially soaked Blood clots (NOT NORMAL) – small pieces of tissue ‘Flooding’ – menstrual blood soaks through all protection Abnormal and distressing Do you change at night? – – How often How many nights • Do your periods interfere with your life • Have you any “accidents” • Associated Symptoms – – Anaemia Hypothyroidism http: //www. tutorvista. com/content/biology/ biology-ii/reproduction/menstruation-andmenstrual-cycle. php
12 Oligomenorrhoea • Irregular periods, Oligomenorrhoea or amenorrhea suggest anovulation or irregular ovulation • Amenorrhea = Absence of periods • Primary amenorrhea: Menstruation not established – – • 16 years with secondary sexual characters 14 years with no secondary characters Secondary amenorrhea: Absent of menses > 6 months – Think pregnancy • Oliogomenorrhoea: infrequent periods with a cycle of 35 days or more • Specific questions (causes of anovulation) – – – Weight change: Loss/Gain Acne/Greasy skin Hirsutism Galactorrhoea/Recurrent headaches Hyperthyroidism symptoms Flushes may help identify ovarian dysfunction: menopause
13 Dysmenorrhea • Primary – Starts with menses – Usually 2 to 3 days – Improves with age and after childbirth • Secondary – Secondary pathology – Usually starts a few days prior to menses • Severity: time off school/work? • Any aggravating/relieving factors • Any effect of painkillers • Family History: Endometriosis
14 Vaginal Discharge • Duration http: //www. pathology. stgeorges. nhs. uk/pathologyinvestigations/medical-microbiology/high-vaginal-swab-mcs • Cyclical? • Itchy • Amount • Colour: white/yellow/greenish/brown • Odour: odourless/fishy • Any previous history of same • Any treatment used • Other symptoms? Pain, fever, etc.

15 Mass in Abdomen • Duration • Change in size • Pain • Nausea, vomiting, change in bowel habits? • Weight loss • Associated symptoms: Menorrhagia, amenorrhea
16 Uro-gynaecological History • Any problems passing urine? • Urinary symptoms – frequency, nocturia, dysuria, incontinence, haematuria • Incontinence – Do you ever leak urine when don’t intend to? – Stress Incontinence: If so, find out what provokes it. e. g. coughing, sex, exercise – Urge Incontinence: Do you ever not make it to the toilet in time? Can you hold your urine without leaking? Do you pass small volumes frequently – Often a mixed picture • Prolapse: Associated with vaginal discomfort, feeling of something coming down
17 Obstetric History • Number of previous pregnancies • No. of children? – Birth weight • Any antenatal problems? • Mode of delivery labour prolonged? – Relevant to prolapse • Any terminations/Miscarriages – Surgical/Medical? – Gestation

18 Sexual History
19 Sexual History • Sensitive approach: Choose your words carefully • Begin with “I need to ask you some personal questions…. Hope that is OK? ” • Are you or have you ever been sexually active? • How old were you when you first had sex? • Are you in a stable relationship? • How many partners have you had in the last six months? • When was the last time you had sexual intercourse? • Have you ever suffered from any sexually transmitted infection? • Have you ever experienced sexual assault or incest? • Is there violence in any of your relationships?
20 Also Think About… • Previous gynaecological problems – STIs, endometriosis, infertility, surgery, polycystic ovarian disease • Contraception – Current/past – Hormonal/non-hormonal – Any problems? • Pap smear history – Date and results of last cervical smear – Any treatment in the past – Vaccine against cervival cancer • Bowel symptoms http: //www. cervexbrush. com/combi. html – Bleeding PR, fecal incontinence, bowel habits, mucus in stool, difficulty emptying bowel

Partners in Academic Medicine
 Manisha dasgupta
Manisha dasgupta Manisha has secured 79 marks in the college exam
Manisha has secured 79 marks in the college exam Dr manisha mathur
Dr manisha mathur Fdi notation for deciduous teeth
Fdi notation for deciduous teeth Dr gunasekera gordon
Dr gunasekera gordon Take a bus or take a train
Take a bus or take a train History also history physical
History also history physical Howard county young authors contest
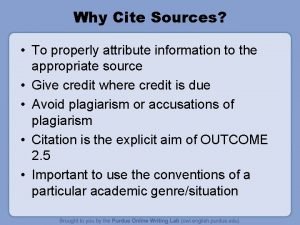
Howard county young authors contest In text citation
In text citation Authors purpose notes
Authors purpose notes What is author's purpose
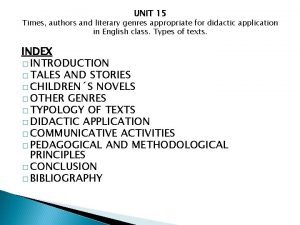
What is author's purpose Topic 15 periods authors and genres
Topic 15 periods authors and genres What is the author attitude towards the subject
What is the author attitude towards the subject Authors affiliation example
Authors affiliation example Ray bradbury the veldt
Ray bradbury the veldt In text citation chicago multiple authors
In text citation chicago multiple authors Why do writers use symbols
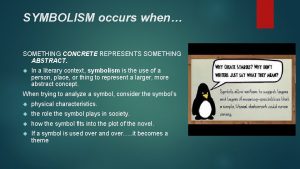
Why do writers use symbols What does concrete symbolize
What does concrete symbolize Technical terms in research example
Technical terms in research example How to cite many authors
How to cite many authors Hypophora
Hypophora Authors attitude
Authors attitude