HOW TO DEVELOP AND IMPLEMENT AN EFFECTIVE PRODUCTIVITY



- Slides: 59
HOW TO DEVELOP AND IMPLEMENT AN EFFECTIVE PRODUCTIVITY AND STAFFING MANAGEMENT SYSTEM January 5, 2018 BUILDING LEADERS – TRANSFORMING HOSPITALS – IMPROVING © HTS 3 2018

I HOPE YOU’REW ARM AND SAFE © HTS 3 2018 1
45 YEARS OF DELIVERING RESULTS Health. Tech. S 3 is a 45 year old, award-winning healthcare consulting and strategic hospital services firm based in Brentwood, Tennessee with clients across the United States. We are dedicated to the goal of improving performance, achieving compliance, reducing costs, and ultimately improving patient care. Leveraging consultants with deep healthcare industry experience, Health. Tech. S 3 provides actionable insights and guidance that supports informed decision making and drives efficiency in operational performance. Our consultants are former hospital leaders and executives. Health. Tech. S 3 has the right mix of experienced professionals that service hospital clients across the nation. Health. Tech. S 3 offers flexible and affordable services, consulting, and technology as we focus on delivering solutions that can be implemented and provide a positive, measurable impact. © HTS 3 2018 2 2
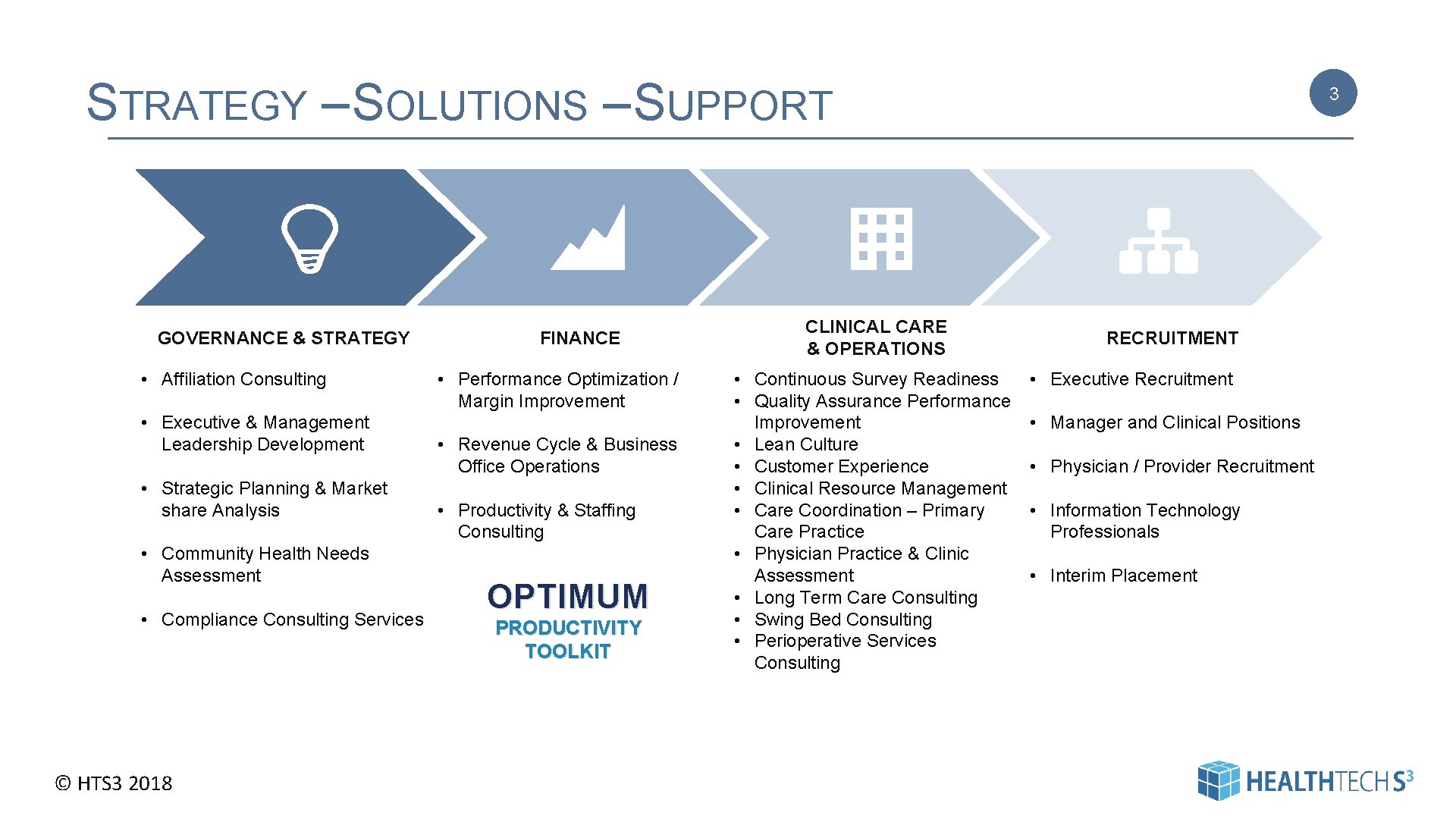
STRATEGY – SOLUTIONS – SUPPORT GOVERNANCE & STRATEGY • Affiliation Consulting • Executive & Management Leadership Development • Strategic Planning & Market share Analysis • Community Health Needs Assessment • Compliance Consulting Services © HTS 3 2018 FINANCE • Performance Optimization / Margin Improvement • Revenue Cycle & Business Office Operations • Productivity & Staffing Consulting OPTIMUM PRODUCTIVITY TOOLKIT CLINICAL CARE & OPERATIONS • Continuous Survey Readiness • Quality Assurance Performance Improvement • Lean Culture • Customer Experience • Clinical Resource Management • Care Coordination – Primary Care Practice • Physician Practice & Clinic Assessment • Long Term Care Consulting • Swing Bed Consulting • Perioperative Services Consulting 3 RECRUITMENT • Executive Recruitment • Manager and Clinical Positions • Physician / Provider Recruitment • Information Technology Professionals • Interim Placement
1 QUARTER 2018 WEBINARS ST How to Develop and Implement an Effective Productivity and Staffing Management System Host: Carolyn St. Charles, RN, BSN, MBA, Regional Chief Clinical Officer Date: January 5 th, 2018 Time: 12: 00 pm CT Register Here: http: //bit. ly/2 z. Vvh 0 z What’s New in the 2018 Regulations for CCM? : Understanding the Alphabet Soup of Care Management Host: Faith M Jones, MSN, RN, NEABC, Director of Care Coordination and Lean Consulting Date: January 18 th, 2018 Time: 12: 00 pm CT Register Here: http: //bit. ly/2 z. Wr 6 Sj Challenges/Opportunities in Population Health Management IT Host: Diane Bradley, Ph. D, RN, NEABC, CPHQ, FACHE, FACHCA, Regional Chief Clinical Officer Date: January 22 nd, 2018 Time: 12: 00 pm CT Register Here: http: //bit. ly/2 z. VOtvy © HTS 3 2018 4 Continuous Survey Readiness: Yes it’s Possible Host: Carolyn St. Charles, RN, BSN, MBA, Regional Chief Clinical Officer Date: February 2 nd, 2018 Time: 12: 00 pm CT Register Here: http: //bit. ly/2 j. FLUau Office of Inspector General Work Plan: Change towards Transparency Host: Cheri Benander MSN, RN, NHA, CHC, NHCE-C Health Services Consultant, Health. Tech. S 3 Date: February 8 th, 2018 Time: 12: 00 pm CT Register Here: http: //bit. ly/2 m. Lb. R 9 I Strategies to Maximize Service Lines and Improve Accountability Host: Diane Bradley, Ph. D, RN, NEABC, CPHQ, FACHE, FACHCA, Regional Chief Clinical Officer Date: February 16 th, 2018 Time: 12: 00 pm CT Register Here: http: //bit. ly/2 h. GBBP 9
1 QUARTER 2018 WEBINARS (CONT’D) ST 5 Funding Diversification Takes Planning: Do you have a Grant Plan? Hosts: Faith M Jones, MSN, RN, NEABC, Health. Tech. S 3 Director of Care Coordination and Lean Consulting; and Bianca Policastro, Vice-President, The Policastro Group Date: February 22 nd, 2018 Time: 12: 00 pm CT Register Here: http: //bit. ly/2 h. R 1 Zt. H Strategic Alignment of Practice Measures in Care Coordination: Making it Meaningful Hosts: Faith M Jones, MSN, RN, NEA-BC Health. Tech. S 3 Director of Care Coordination and Lean Consulting; and Deb Anderson, Business Relationship Manager, Health Technology Services Date: March 22 nd, 2018 Time: 12: 00 pm CT Register Here: http: //bit. ly/2 B 7 AVLc Community Health Needs Assessment – Your Partner in Population Health Host: Carolyn St. Charles, RN, BSN, MBA, Regional Chief Clinical Officer Date: March 2 nd, 2018 Time: 12: 00 pm CT Register Here: http: //bit. ly/2 B 84 k. Fn Cost Effective Care Models That Improve Outcomes Host: Diane Bradley, Ph. D, RN, NEABC, CPHQ, FACHE, FACHCA, Regional Chief Clinical Officer Date: March 23 rd, 2018 Time: 12: 00 pm CT Register Here: http: //bit. ly/2 je 44 w 2 Recruitment Tips: Get It Right The First Time Host: Peter Goodspeed, Vice President Executive Placement Date: March 26 th, 2018 Time: 12: 00 pm CT Register Here: http: //bit. ly/2 iz. Spsg © HTS 3 2018
SPEAKER 6 Carolyn began her healthcareer as a staff nurse in Intensive Care. She has worked in a variety of staff, administrative and consulting roles and has been in her current position as Regional Chief Clinical Officer with Health. Tech. S 3 for the last fifteen years. Carolyn St. Charles Regional Chief Clinical Officer In her role as Regional Chief Clinical Officer, Carolyn St. Charles conducts mock surveys for Critical Access Hospitals, Acute Care Hospitals, Long Term Care, Rural Health Clinics. Carolyn also works with rural hospitals to develop staffing strategies that are realistic and cost-effective. carolyn. stcharles@healthtechs 3. com 360 -584 -9868 © HTS 3 2018
OUR AGENDA I. Why Do We Care? II. A Few Basics III. Developing a Productivity System IV. Monitoring and Controlling V. Common Problems © HTS 3 2018 7
I. WHY WE CARE 8 • Labor cost is the single largest expense item in every hospital and in almost every hospital department • Left unmonitored FTE’s have a tendency to increase – beware the creep……. © HTS 3 2018 | Pag e 8
VALUE OF A PRODUCTIVITY SYSTEM • Sets aggressive but attainable targets • Ties productivity targets to daily operational staffing tools • Links productivity targets to departmental budgets • Provides managers with staffing guidelines based on targets that are specific and appropriate for their individual department • Fosters accountability © HTS 3 2018 9 | Pag e 9
II. A FEW BASICS © HTS 3 2018
DEFINITIONS 11 Worked Hours: Worked hours are direct care hours plus management hours and any other support staff assigned to the unit. Include hours of all staff that work in a department including the unit secretary, staff “floated” from other departments, agency/contract staff and management hours. Do not include hours on-call. Direct Care Hours: Hours spent actually providing care, treatment, tests, etc. Does not include management or support staff such as unit secretaries. Accurate Allocation: Accurate allocation of worked hours to the appropriate cost center is critical for creating accurate productivity data as well as for creating accurate reporting of costs. In smaller facilities where staff may be responsible for covering multiple areas and it is not practical to allocate actual hours, it may be necessary to allocate based on a pre-determined formula agreed to with finance. A roll-up can also be used for departments such as medical imaging that has multiple modalities, or when one group of staff cover multiple departments Hours per Workload Unit: The number of hours in a given time period divided by the workload unit or unit of service for that same time period. Education and Orientation Hours: Hours staff spend in education or orientation. Include as part of worked (productive) hours. Modality: 15 -minute billed increments. Non-Productive Hours: Paid time off such as vacation, sick time, family leave. Paid Hours: Total of all productive (worked) and non-productive hours. Productive Hours or Worked Hours: Includes direct care hours, support staff, Capture of Workload: Capture of all workload is critical for having accurate productivity data and staff buy-in. This is especially important for workload that management hours, education and orientation. may not be consistently captured such as observation or outpatient procedures. Target: Amount of hours to produce a given volume of work. May be stated as a FTE or as worked hours per workload unit or unit of service. Minimum Staffing: Some facilities may experience periods of “minimum staffing. ” Minimum staffing levels will vary between organizations but include at least two licensed nursing staff at all times. Some states, such as California and Unit of Service (UOS) or Workload Unit (WLU): Measure of volume for a specific department. New York, have mandated staffing ratios. Adjusted patient day: Inpatient days multiplied by a factor resulting from dividing total hospital-wide revenue by inpatient hospital-wide revenue. © HTS 3 2018 11
KEY TERMS • • • © HTS 3 2018 12 Full Time Equivalent (FTE) Paid Hours Worked Hours (Productive Hours) Unit of Service Worked Hours per Unit of Service | Page
FTE DEFINITION 13 1 FTE (Full Time Equivalent) is based upon 2, 080 hours per year. This is the universal standard for an FTE in healthcare for comparative benchmarking purposes. It doesn’t matter if your hospital’s standard for full time is less than 2, 080 (for example nurses who work 72 hours / pay period are sometimes considered full-time). 2080 hours per year should always be the denominator to determine FTEs. 23, 500 hours = 11. 3 FTEs (23500/2080) © HTS 3 2018 | Page
PAID HOURS 14 Total paid hours include: – – Worked Hours Registry / Contract Labor Call Back Hours Paid Time Off • • • Vacation Sick Leave Holiday Personal Leave Jury Duty Bereavement Leave Paid hours do not include: – On-Call Pay – Shift Differential © HTS 3 2018 | Page
WORKED HOURS 15 • Worked hours are a subset of total hours • Worked hours may be referred to as “productive hours” – Actual worked hours – Registry / contract labor – Hours “called back” to work – Education and orientation – Overtime counts! • Worked hours DO NOT include – Vacation, Sick, Holiday, Jury Duty, On-Call, Shift Differential © HTS 3 2018 | Page
UNIT OF SERVICE - MEASURE OF VOLUME Net Revenue Trips Cases Billable Procedures Patient Days Square Feet Meals © HTS 3 2018 16 16
WORKED HOURS PER UNIT OF SERVICE 17 Worked hours (divided by) volume = worked hours per unit of service 23, 500 hours / 2, 000 patient days = 11. 75 worked hours per patient day 6, 000 hours / 3, 000 procedures = 2. 0 worked hours per procedure © HTS 3 2018 | Page
III. DEVELOPING A FUNCTIONAL & EFFECTIVE PRODUCTIVITY SYSTEM © HTS 3 2018 18 18

ESTABLISH TARGETS 19 Step 1: Identify a unit of service (i. e. patient days, procedures, treatments, etc. ) for each department Step 2: Estimate volume or workload (usually based on budget or historical data) Step 3: Determine what will be included in worked hours Step 4: Calculate worked hours per unit of service and salary (cost) per unit of service © HTS 3 2018 | Pag e 19
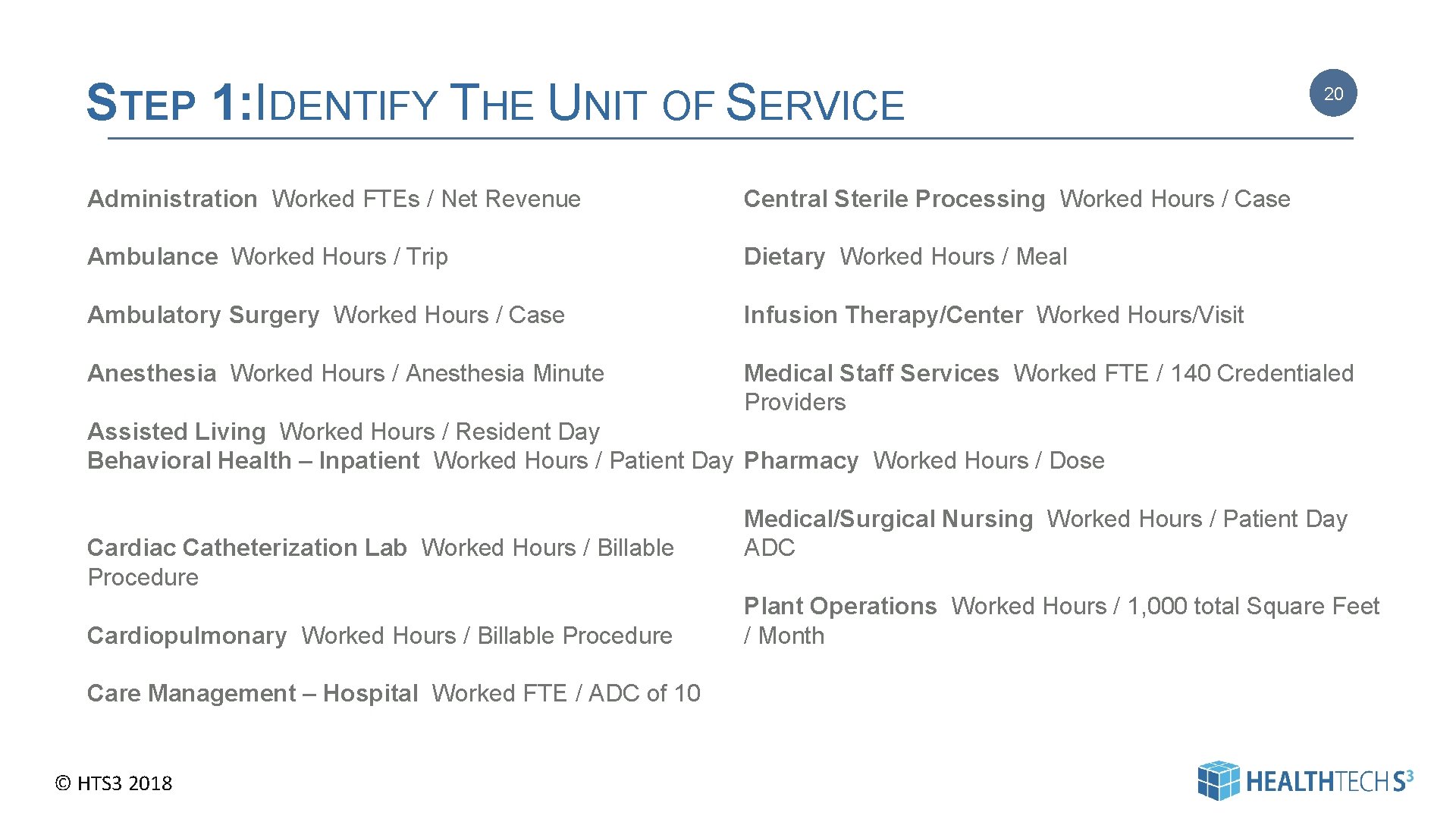
STEP 1: IDENTIFY THE UNIT OF SERVICE 20 Administration Worked FTEs / Net Revenue Central Sterile Processing Worked Hours / Case Ambulance Worked Hours / Trip Dietary Worked Hours / Meal Ambulatory Surgery Worked Hours / Case Infusion Therapy/Center Worked Hours/Visit Medical Staff Services Worked FTE / 140 Credentialed Providers Anesthesia Worked Hours / Anesthesia Minute Assisted Living Worked Hours / Resident Day Behavioral Health – Inpatient Worked Hours / Patient Day Pharmacy Worked Hours / Dose Cardiac Catheterization Lab Worked Hours / Billable Procedure Cardiopulmonary Worked Hours / Billable Procedure Medical/Surgical Nursing Worked Hours / Patient Day ADC Plant Operations Worked Hours / 1, 000 total Square Feet / Month Care Management – Hospital Worked FTE / ADC of 10 © HTS 3 2018 20
AND A DEFINITION FOR EACH 21 ADMITTING AND OUTPATIENT REGISTRATION ____(target) worked hours per total registration Definition: The Admitting and Outpatient Registration Department admits patients for hospital services. This department admits both inpatients and outpatients providing services by: assisting with filling out admission forms, scheduling admission times, accompanying patients to rooms or service areas after admission, arrangement of admission details; verifying insurance and obtaining pre-authorization of services. Standard Unit of Measure: The number of registrations is the unit of measure. Count each registration conducted for outpatient, inpatient, and emergency room. When hospital registration staff conducts the registration function for clinics, count each registration as well. When clinic staff conducts clinic registrations, the count resides in the clinic productivity target. © HTS 3 2018 21
DEFINITION - EXAMPLE 22 PHYSICAL THERAPY ____ (target) worked hours per modality excluding home health ____(target) worked hours per visit home health Definition: The Physical Therapy Department provides therapy for the preservation, enhancement, or restoration of movement and physical function impaired or threatened by disability, injury, or disease that utilizes therapeutic exercise, physical modalities (as massage and electrotherapy), assistive devices, and patient education and training. Standard Unit of Measure: The number of modalities is the unit of measure for inpatients and outpatients excluding home health. Modalities are defined as 15 -minute billed increments. Utilize the home health target of 2. 25 worked hours per visit for home health patients. Transfer hours to the home health cost center. All staff working within the Physical Therapy Department are included within the target (physical therapists, physical therapy assistants, administrative assistants, etc. ). © HTS 3 2018 22
DEFINITION - EXAMPLE 23 Med-Surg Nursing ____(target) worked hours per patient day Definition: Medical/Surgical units provide nursing care to patients whose conditions or disorders are treated medically, pharmacologically, or surgically and are appropriate for inpatient or observation care. Patients requiring intensive care level care not included. In many rural facilities the medical-surgical unit also provides nursing care for pediatric patients and/or outpatients requiring procedures such as blood transfusions or IV infusions. Standard Unit of Measure: The unit of measure is patient days. Include swing bed patients, unless they are cared for in a distinct unit with separate staff. Include observation patients cared for on the Medical /Surgical Unit as equivalent patient days. Considerations relative to the additional services provided by Med-Surg staff: Pediatric integrated within Medical/Surgical: Calculate pediatric patient days at the appropriate target above Swing Bed integrated within Medical/Surgical: Calculate Swing Bed patient days at the same target as Medical / Surgical. Outpatient procedures integrated into Medical/Surgical: When outpatient procedures are conducted by staff on the Medical/Surgical Unit (e. g. , blood transfusions, IV antibiotics, chemotherapy, etc. ) use the outpatient center target of ____ hours per procedure. It is very important to allocate any hours to the Outpatient cost center (and not to Med-Surg) to ensure an accurate reporting of costs. EKGs conducted by Medical/Surgical staff: When Medical/Surgical staff conduct EKGs, transfer the hours to the EKG cost center, to ensure an accurate reporting of costs. Ambulatory Surgery: When patients are admitted to the ambulatory surgery area prior to their procedure or surgery - but secondary recovery and discharge is provided by Medical/Surgical staff - transfer hours to the ambulatory surgery cost center up to a maximum of ____ hours per patient. When patients are admitted to Medical/Surgical prior to surgery and secondary recovery is the responsibility of the Medical/Surgical staff – transfer a maximum of ____ hours to the ambulatory surgery cost center. It is very important to allocate any applicable hours to the Outpatient cost center to ensure an accurate reporting of costs. © HTS 3 2018 23
STEP 2: ESTIMATE VOLUME OR WORKLOAD 1. Historical Volume – Identify seasonal variations – Identify daily / weekly variations – Minimum Staffing 2. Projected Volume – Identify planned changes in service lines (new surgeon / new oncologist / IV infusion / Observation Unit) – Determine if volume changes will impact non-direct care departments (Admitting, Dietary, etc. ) – Minimum Staffing 3. Discuss and gain concurrence from managers (no vacuums) © HTS 3 2018 24 24
A NOTE ABOUT VOLUME AND EFFICIENCY 25 If you have more than one inpatient unit ----- it’s better (more efficient) to have one unit staffed at a defined census level --- than to have 2 or 3 units that are staffed inefficiently due to fluctuations in census. © HTS 3 2018 25
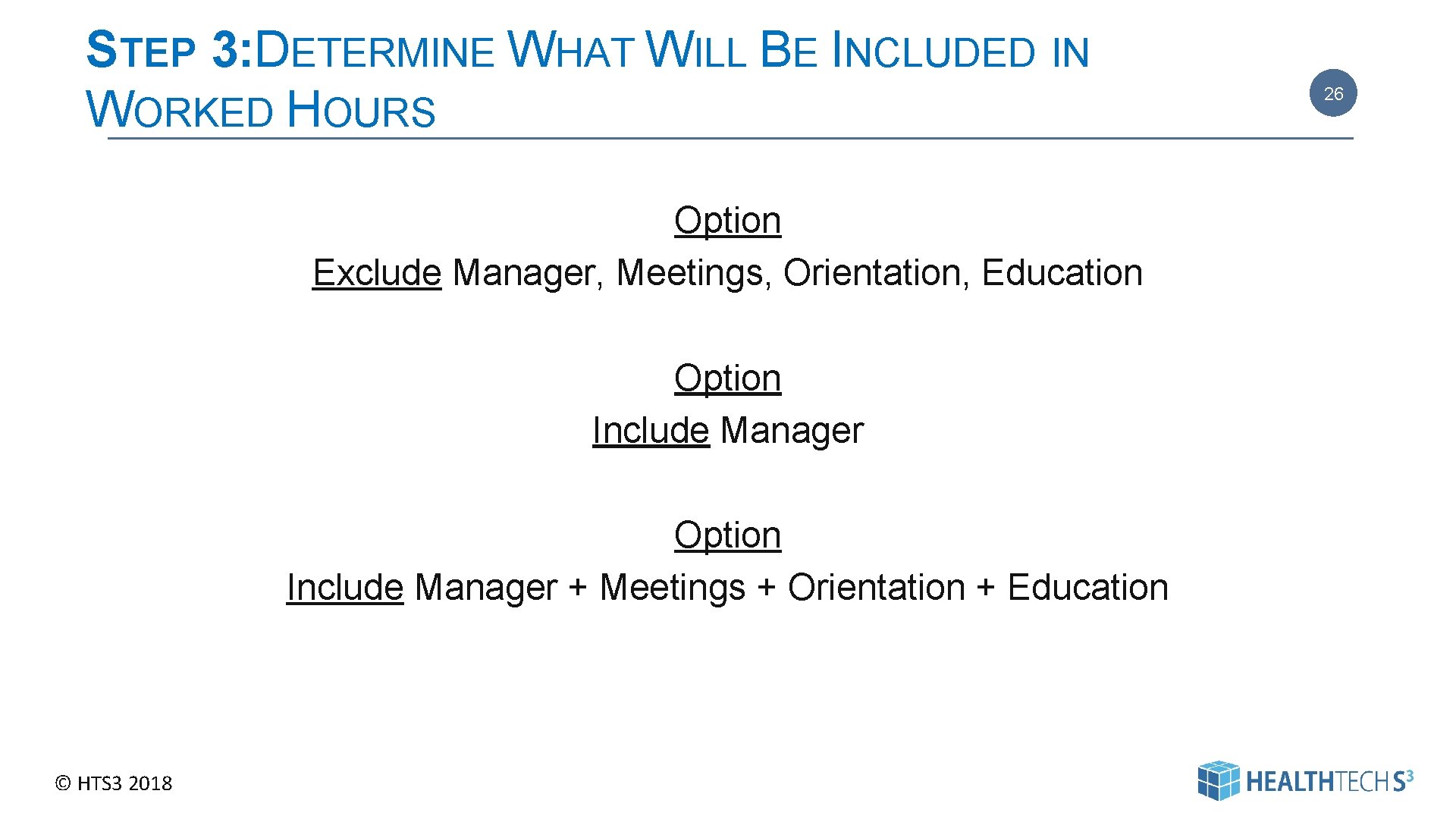
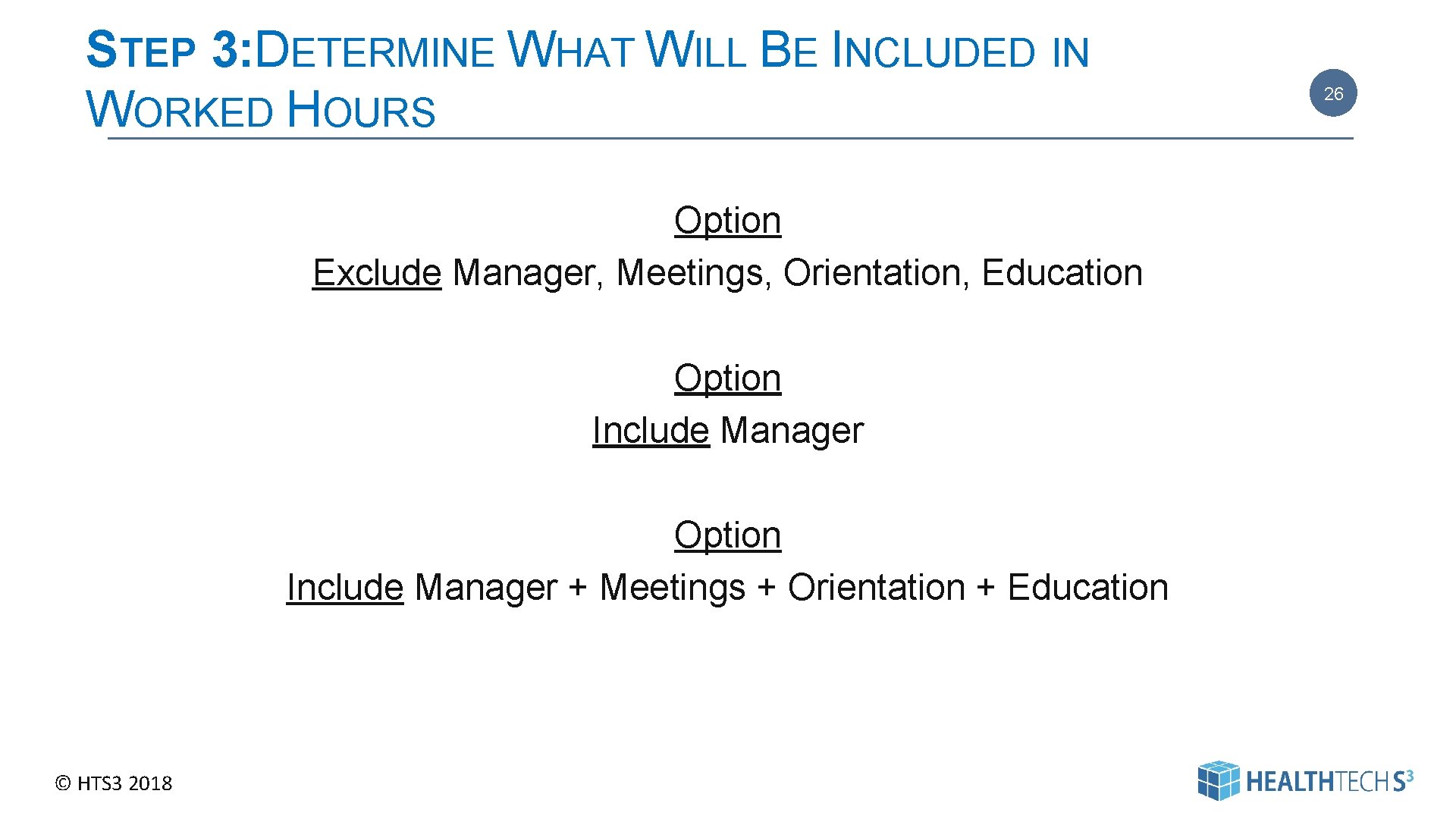
STEP 3: DETERMINE WHAT WILL BE INCLUDED IN WORKED HOURS Option Exclude Manager, Meetings, Orientation, Education Option Include Manager + Meetings + Orientation + Education © HTS 3 2018 26 26
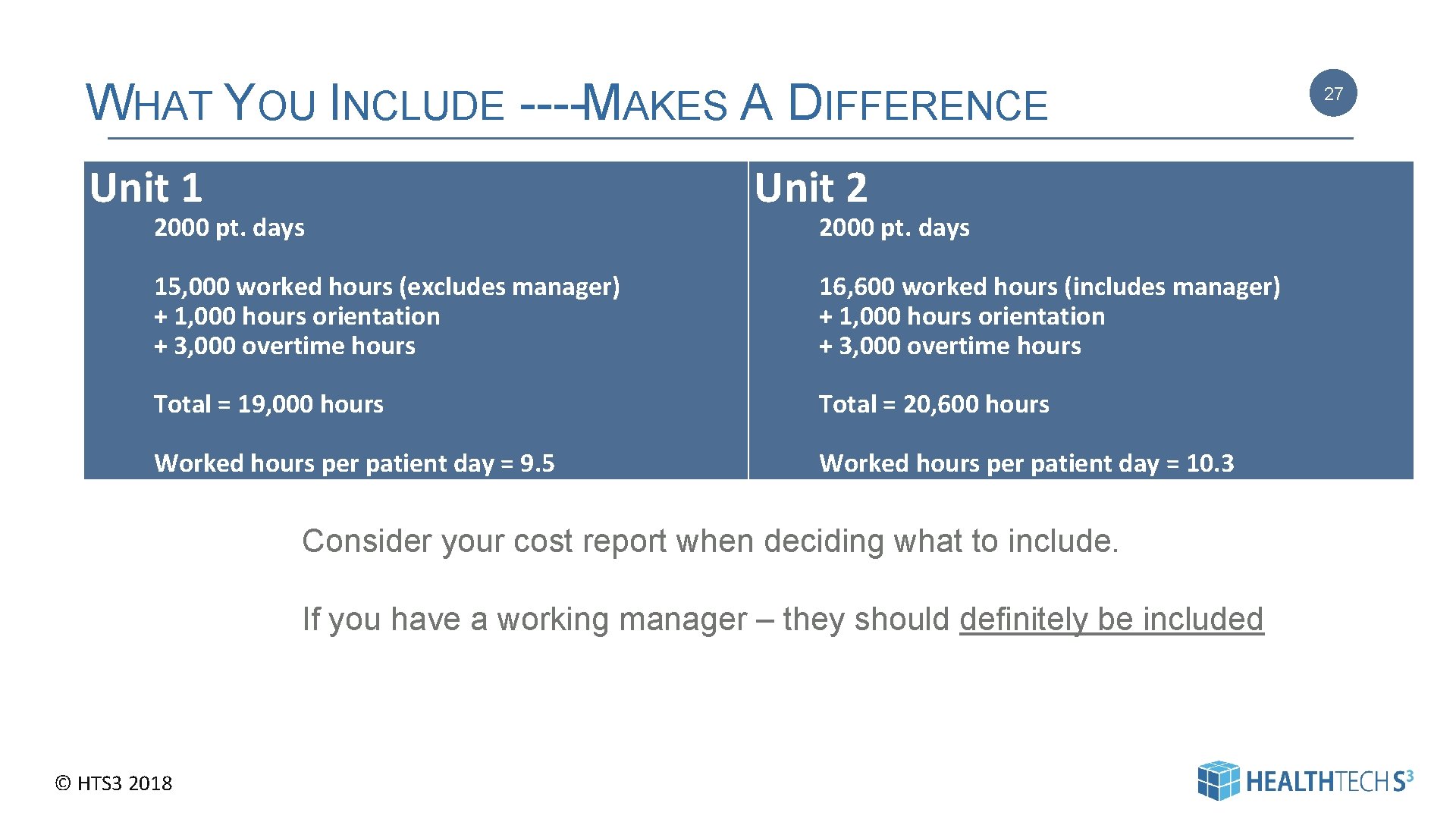
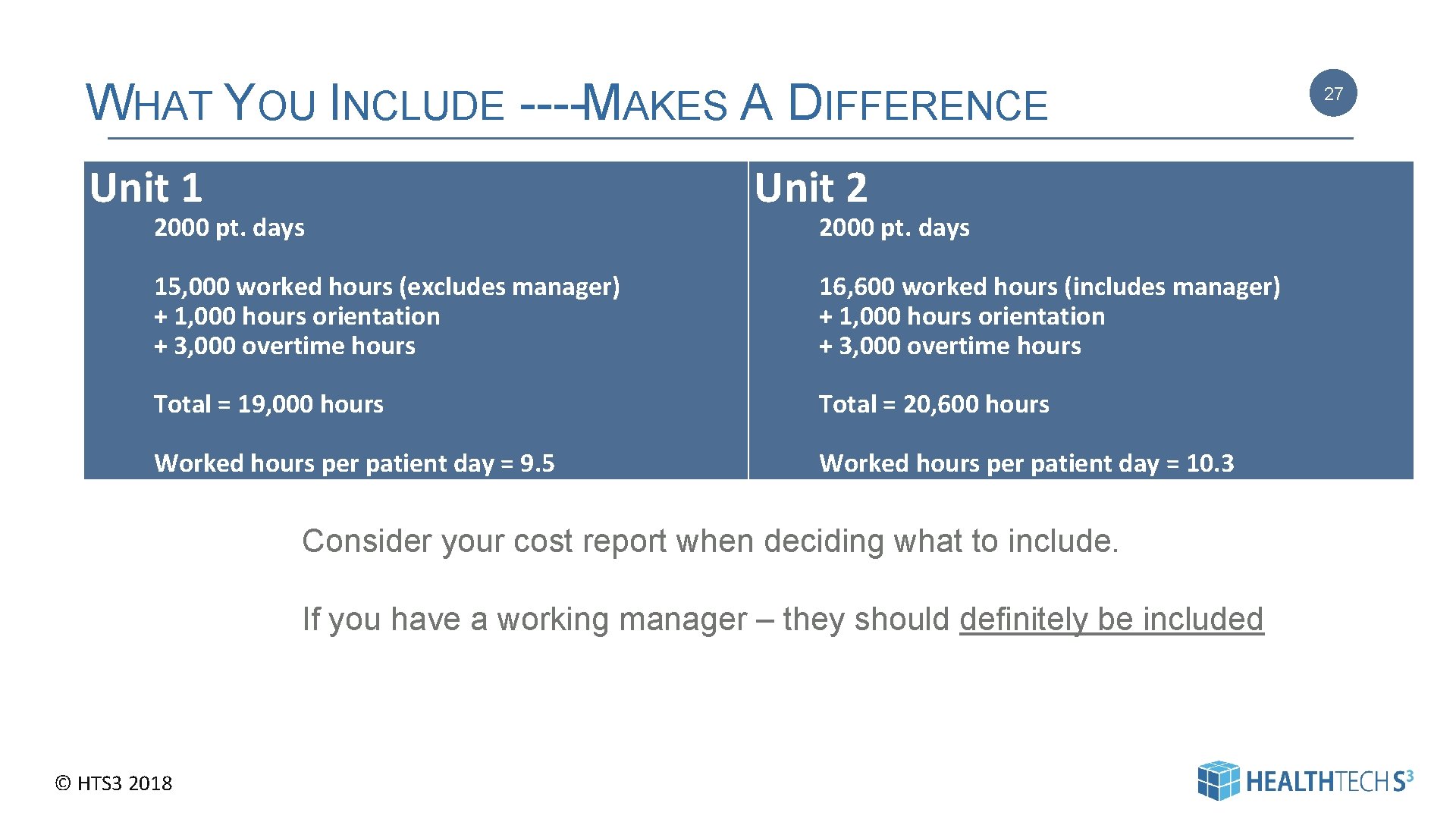
WHAT YOU INCLUDE ---- MAKES A DIFFERENCE Unit 1 2000 pt. days Unit 2 2000 pt. days 15, 000 worked hours (excludes manager) + 1, 000 hours orientation + 3, 000 overtime hours 16, 600 worked hours (includes manager) + 1, 000 hours orientation + 3, 000 overtime hours Total = 19, 000 hours Total = 20, 600 hours Worked hours per patient day = 9. 5 Worked hours per patient day = 10. 3 Consider your cost report when deciding what to include. If you have a working manager – they should definitely be included © HTS 3 2018 27
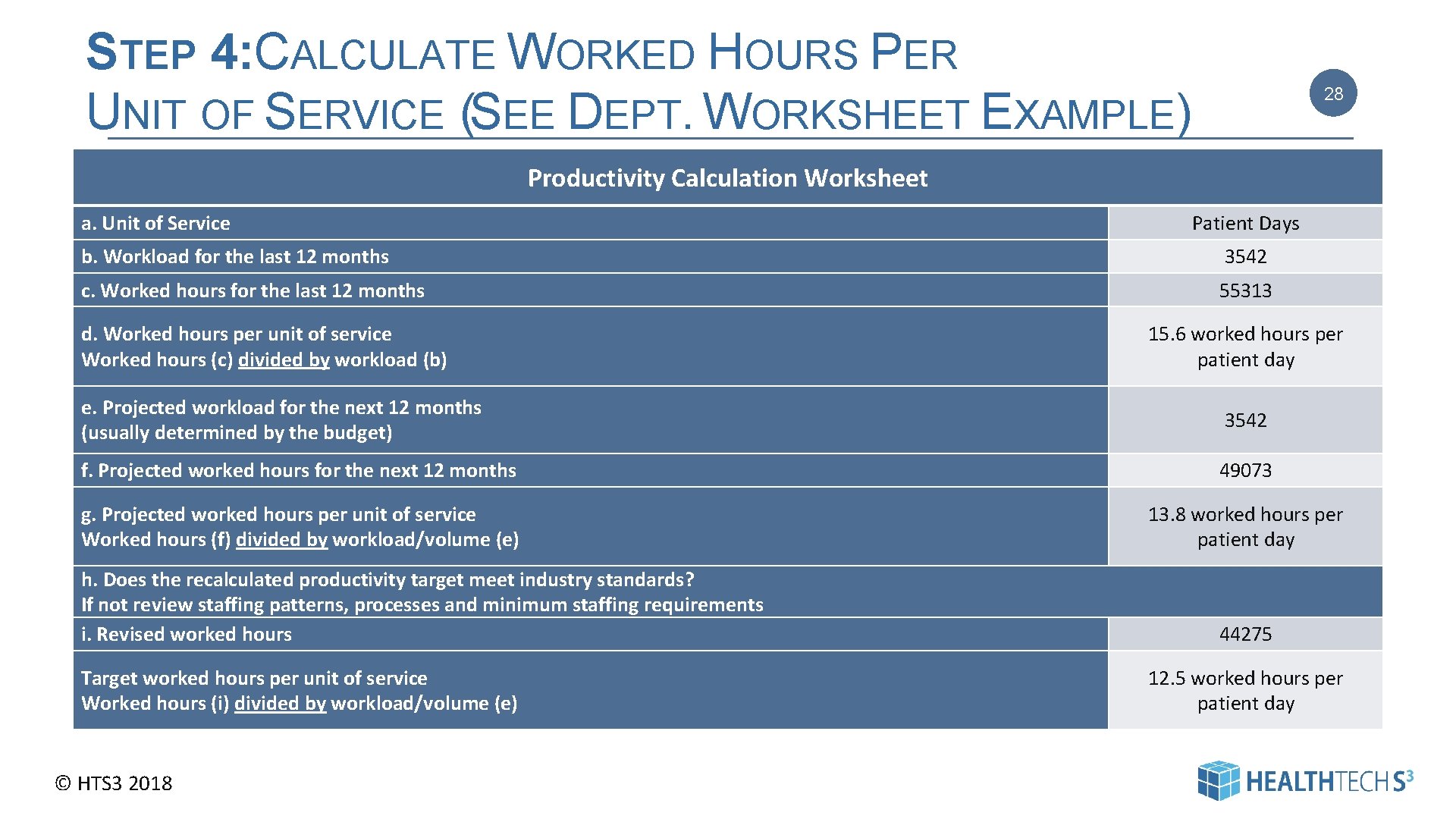
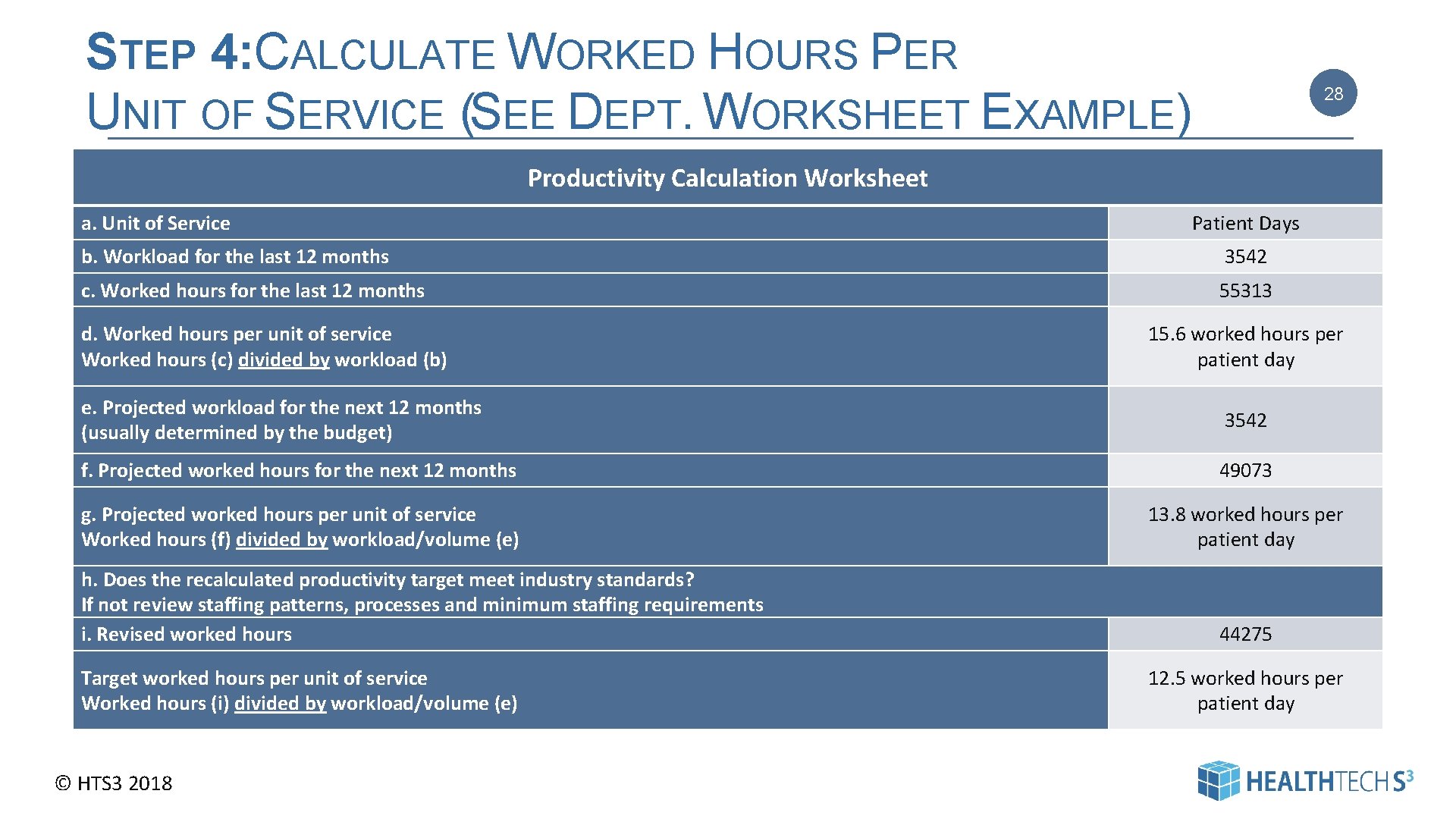
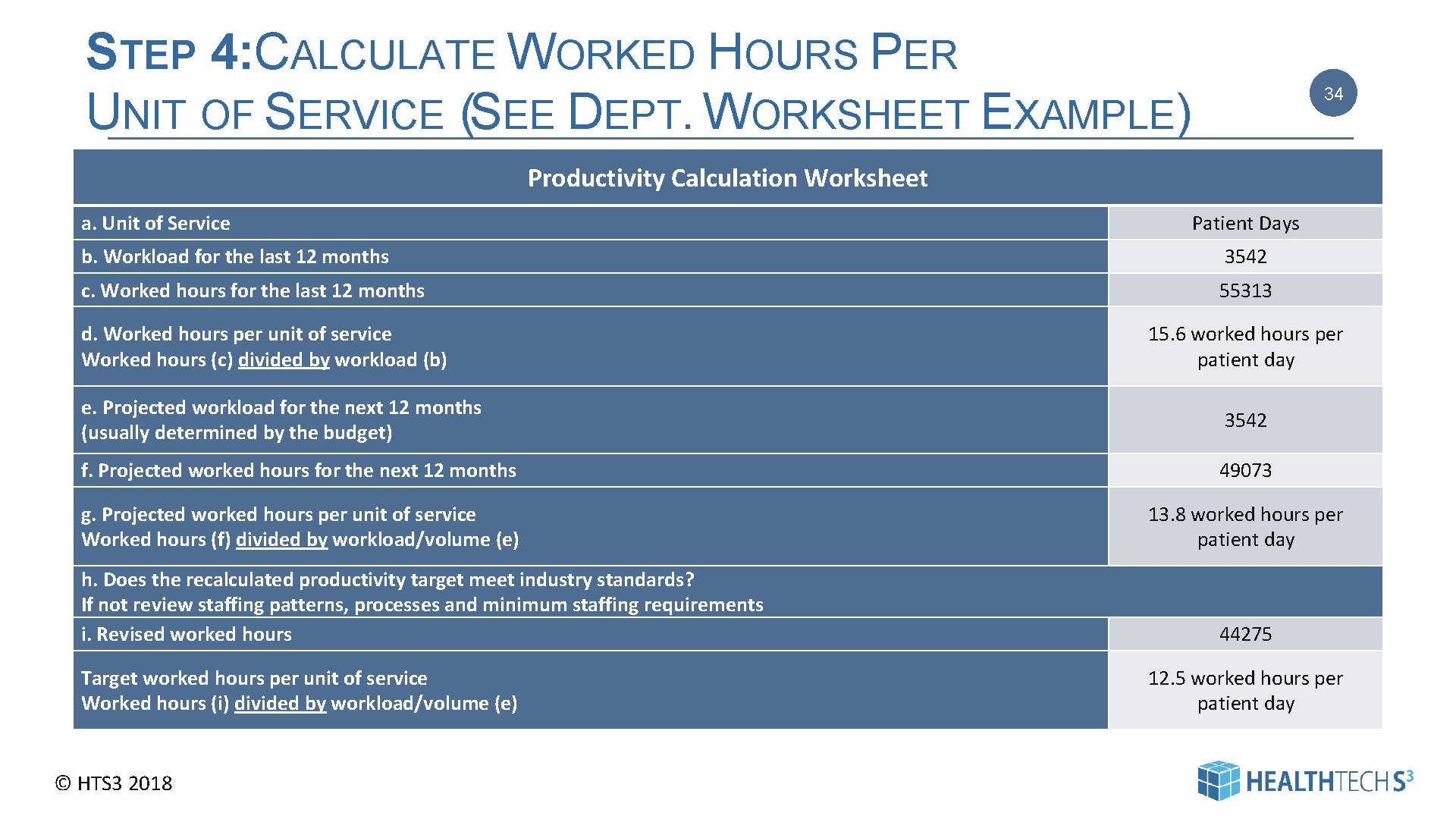
STEP 4: CALCULATE WORKED HOURS PER UNIT OF SERVICE (SEE DEPT. WORKSHEET EXAMPLE) 28 Productivity Calculation Worksheet a. Unit of Service Patient Days b. Workload for the last 12 months 3542 c. Worked hours for the last 12 months 55313 d. Worked hours per unit of service Worked hours (c) divided by workload (b) 15. 6 worked hours per patient day e. Projected workload for the next 12 months (usually determined by the budget) 3542 f. Projected worked hours for the next 12 months 49073 g. Projected worked hours per unit of service Worked hours (f) divided by workload/volume (e) 13. 8 worked hours per patient day h. Does the recalculated productivity target meet industry standards? If not review staffing patterns, processes and minimum staffing requirements i. Revised worked hours Target worked hours per unit of service Worked hours (i) divided by workload/volume (e) © HTS 3 2018 44275 12. 5 worked hours per patient day 28
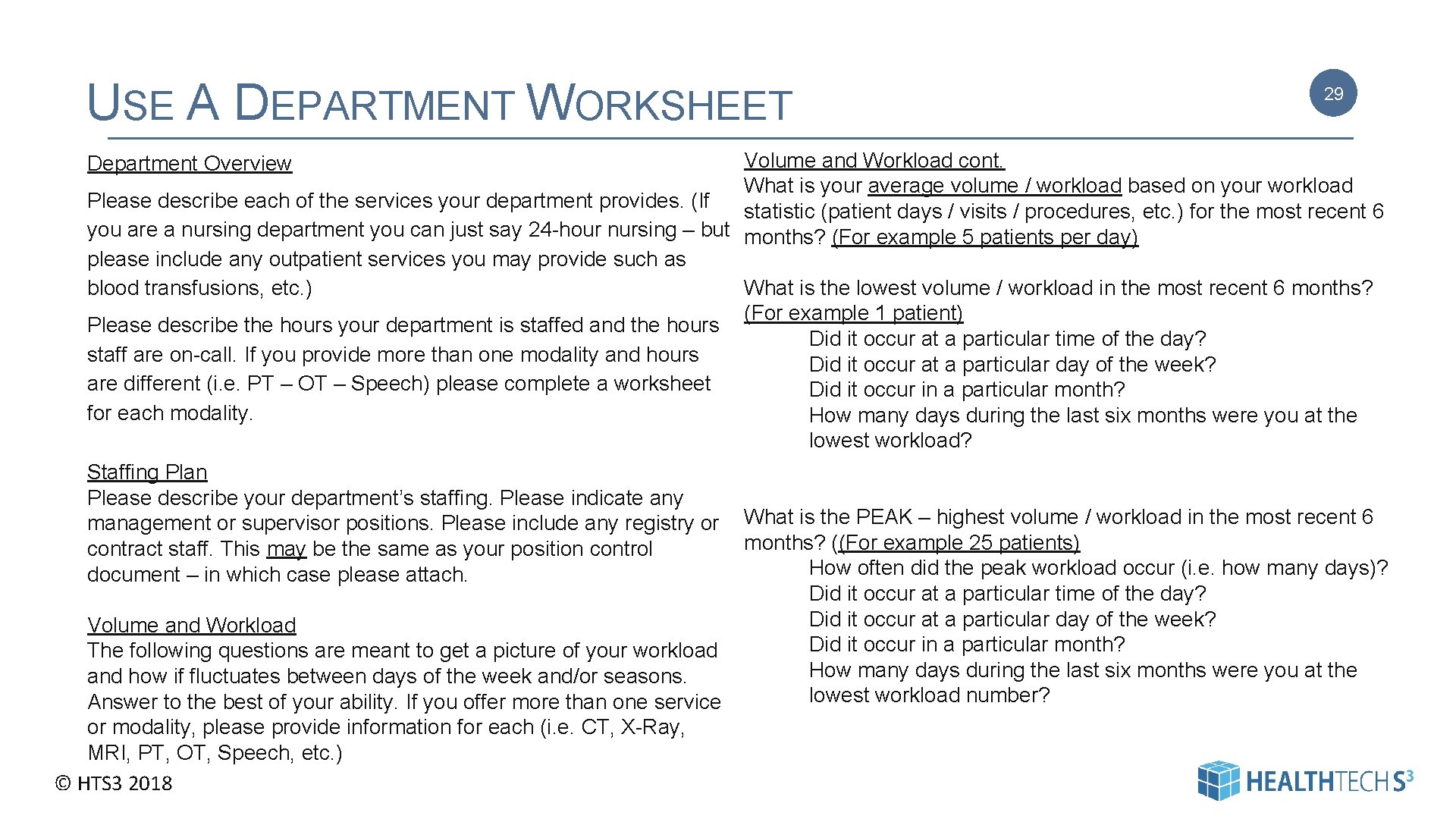
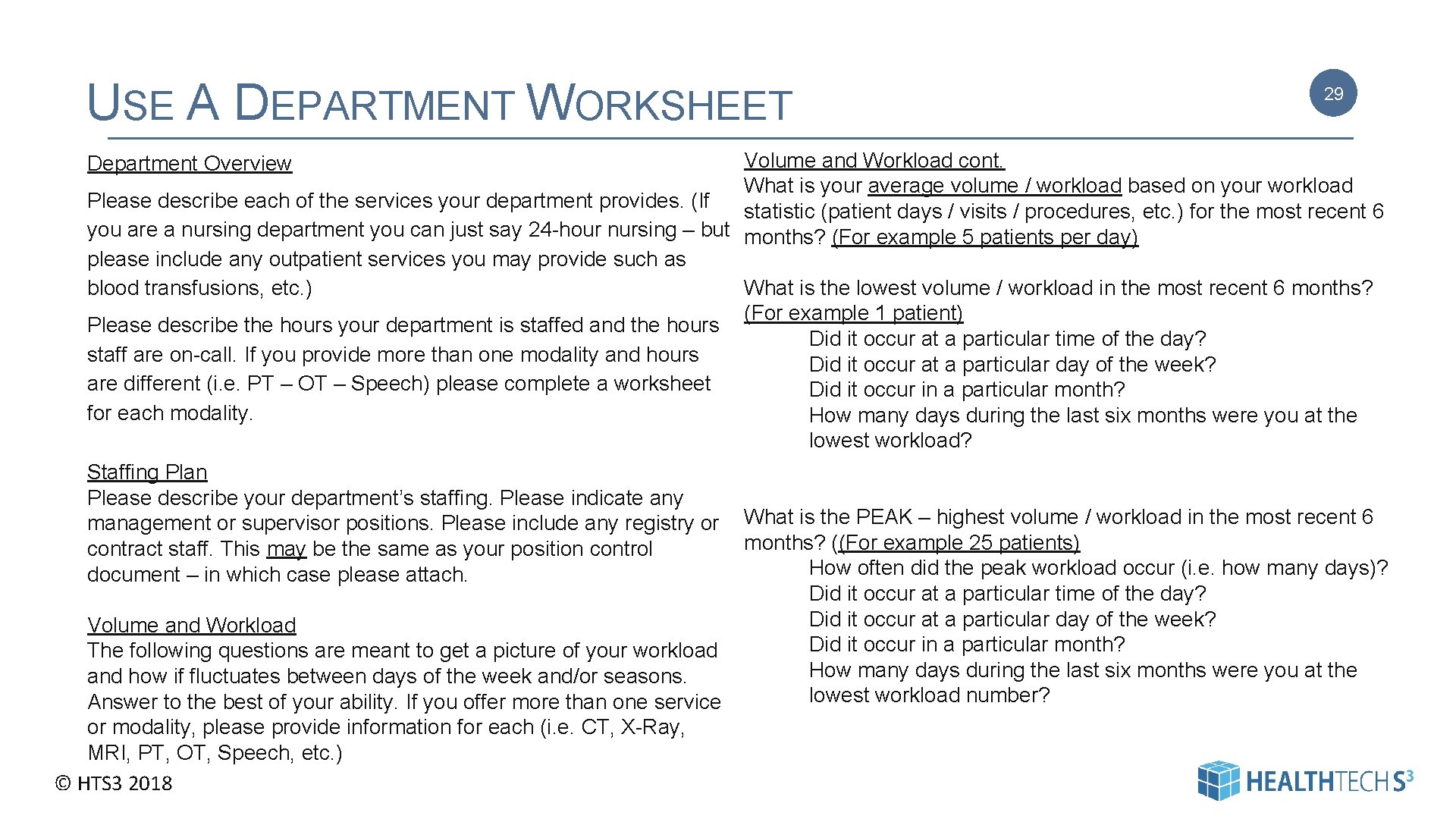
USE A DEPARTMENT WORKSHEET 29 Volume and Workload cont. What is your average volume / workload based on your workload Please describe each of the services your department provides. (If statistic (patient days / visits / procedures, etc. ) for the most recent 6 you are a nursing department you can just say 24 -hour nursing – but months? (For example 5 patients per day) please include any outpatient services you may provide such as What is the lowest volume / workload in the most recent 6 months? blood transfusions, etc. ) (For example 1 patient) Please describe the hours your department is staffed and the hours Did it occur at a particular time of the day? staff are on-call. If you provide more than one modality and hours Did it occur at a particular day of the week? are different (i. e. PT – OT – Speech) please complete a worksheet Did it occur in a particular month? for each modality. How many days during the last six months were you at the lowest workload? Staffing Plan Please describe your department’s staffing. Please indicate any management or supervisor positions. Please include any registry or What is the PEAK – highest volume / workload in the most recent 6 months? ((For example 25 patients) contract staff. This may be the same as your position control How often did the peak workload occur (i. e. how many days)? document – in which case please attach. Did it occur at a particular time of the day? Did it occur at a particular day of the week? Volume and Workload Did it occur in a particular month? The following questions are meant to get a picture of your workload How many days during the last six months were you at the and how if fluctuates between days of the week and/or seasons. lowest workload number? Answer to the best of your ability. If you offer more than one service or modality, please provide information for each (i. e. CT, X-Ray, MRI, PT, OT, Speech, etc. ) © HTS 3 2018 Department Overview 29
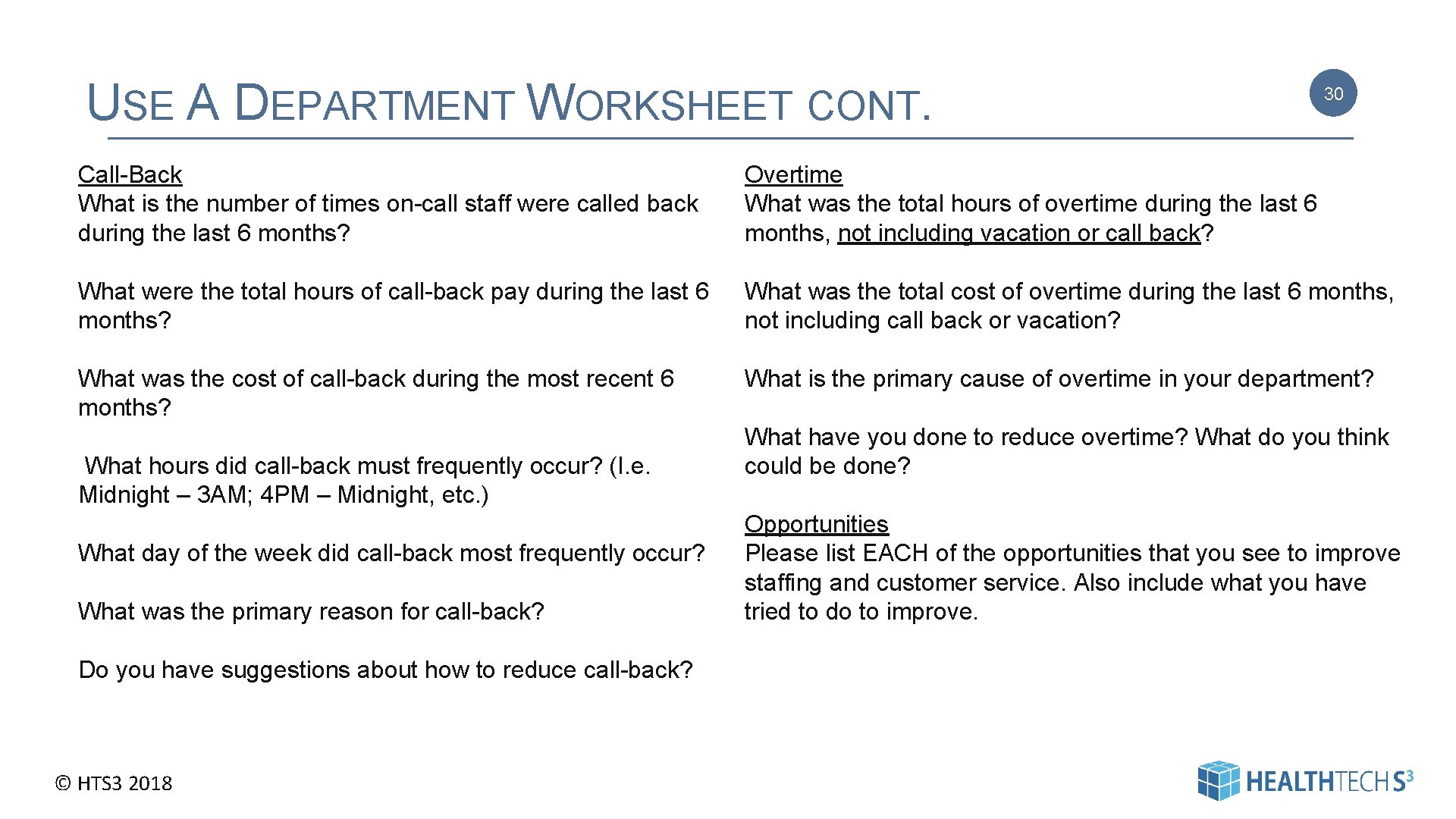
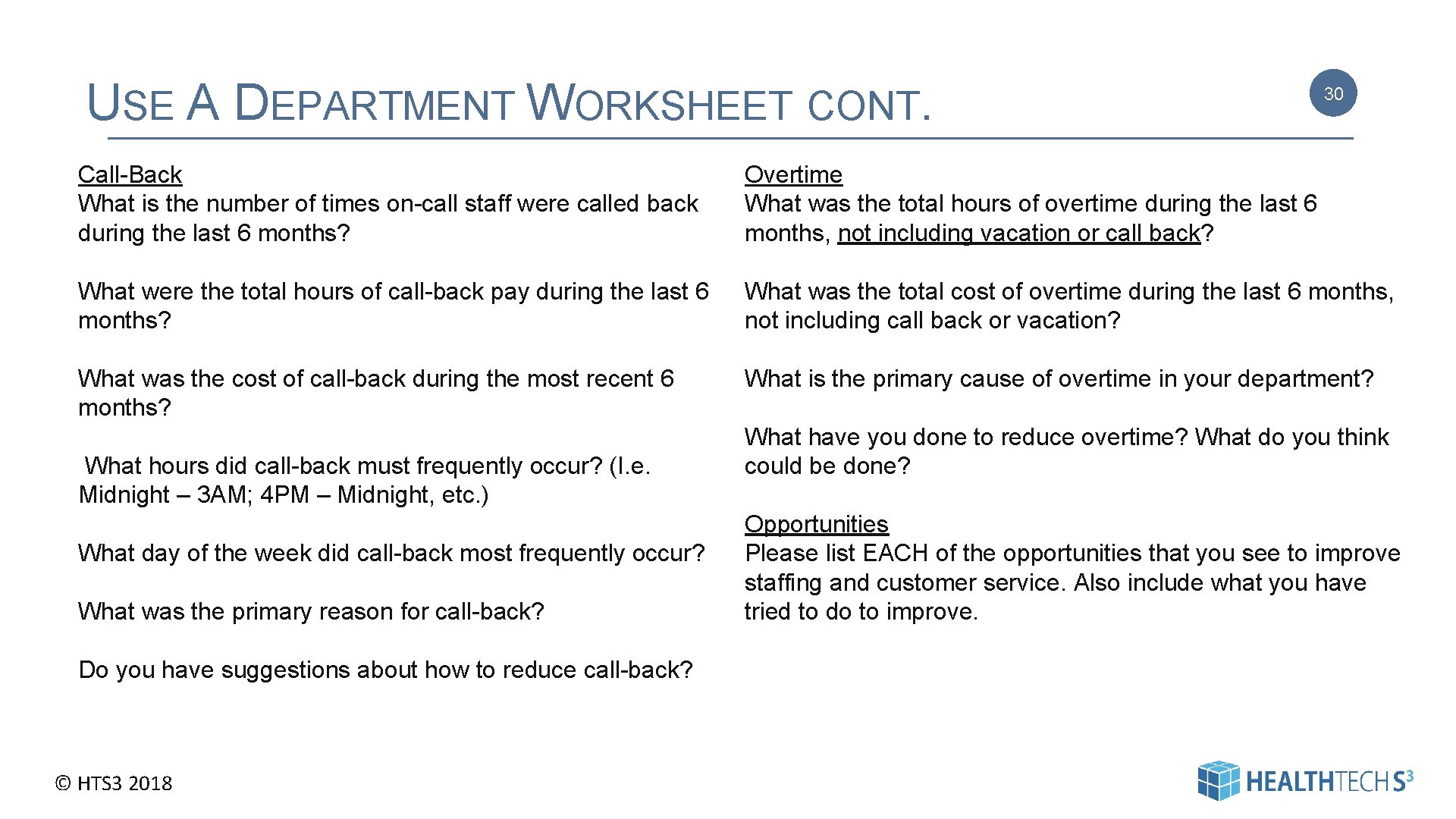
USE A DEPARTMENT WORKSHEET CONT. 30 Call-Back What is the number of times on-call staff were called back during the last 6 months? Overtime What was the total hours of overtime during the last 6 months, not including vacation or call back? What were the total hours of call-back pay during the last 6 months? What was the total cost of overtime during the last 6 months, not including call back or vacation? What was the cost of call-back during the most recent 6 months? What is the primary cause of overtime in your department? What hours did call-back must frequently occur? (I. e. Midnight – 3 AM; 4 PM – Midnight, etc. ) What day of the week did call-back most frequently occur? What was the primary reason for call-back? Do you have suggestions about how to reduce call-back? © HTS 3 2018 What have you done to reduce overtime? What do you think could be done? Opportunities Please list EACH of the opportunities that you see to improve staffing and customer service. Also include what you have tried to do to improve. | Pag e 30

THE PROBLEM WITH THE MIDNIGHT CENSUS Time 7 AM 8 AM 9 AM 10 AM 11 AM Noon 1 PM 2 PM 3 PM 4 PM 5 PM 6 PM © HTS 3 2018 Census 14 15 15 16 16 15 14 13 12 12 Time Census 7 PM 12 8 PM 12 9 PM 12 10 PM 12 11 PM 12 Midnight 12 1 AM 12 2 AM 12 3 AM 12 4 AM 12 5 AM 12 6 AM 12 31 Beware The Churn Admissions Discharges Maximum # of Patients Midnight Census = 4 = 16 = 12 16 patients X 10 worked hours per patient day = 160 hours 12 patients X 10 worked hours per patient day = 120 hours Difference = 40 hours Or if you just want to look at one shift (highest census) 16 patients X 5 worked Hours per patient day = 80 hours 12 patients X 5 worked hours per patient day = 60 hours Difference = 20 hours 31
A FEW MORE NOTES 32 Sometimes (? ) it’s more efficient to have staff 24 hours – than to pay call-back hours. It’s Important to review Hours of Operation. It’s important to review roles and responsibilities. © HTS 3 2018 32
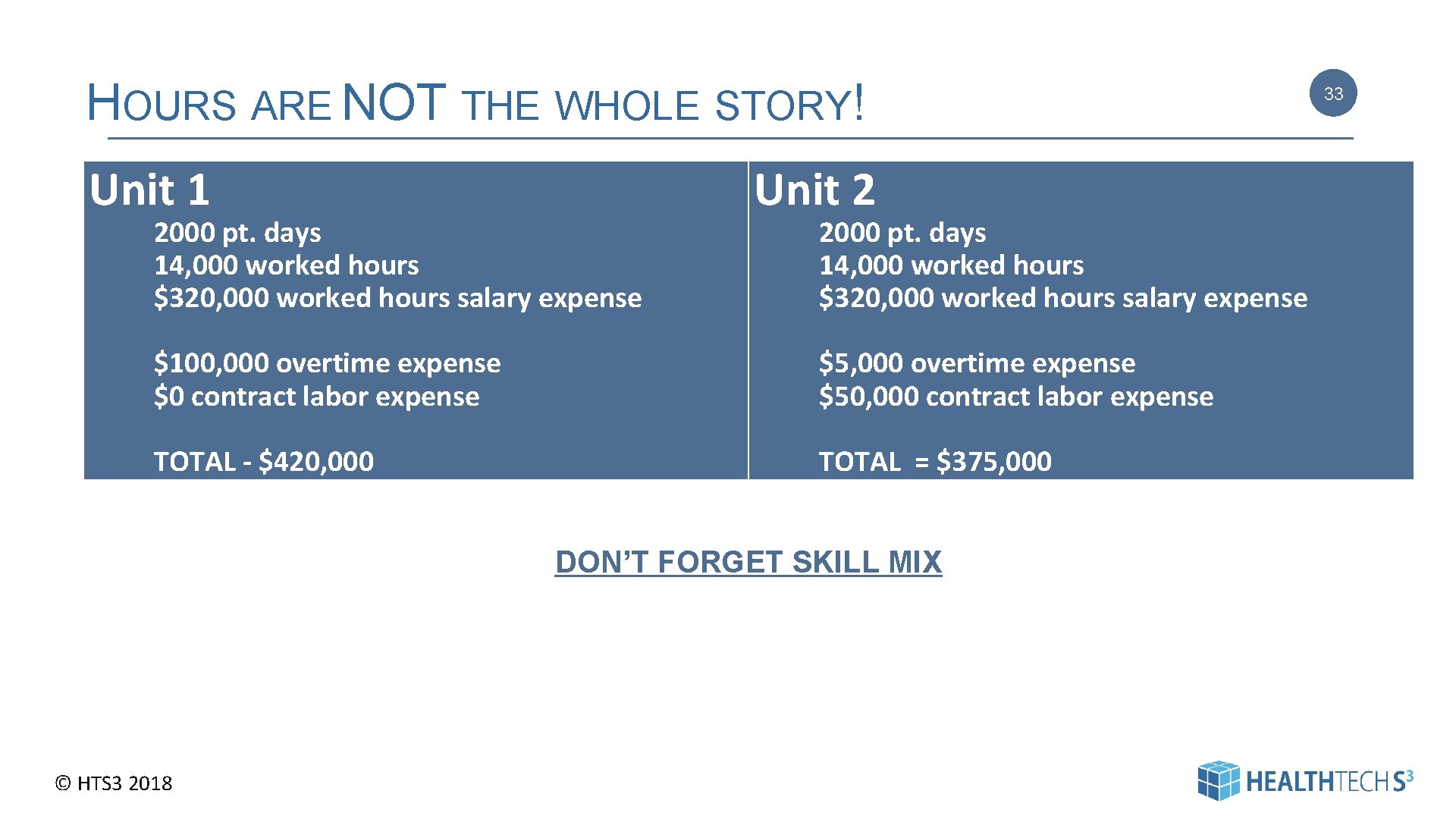
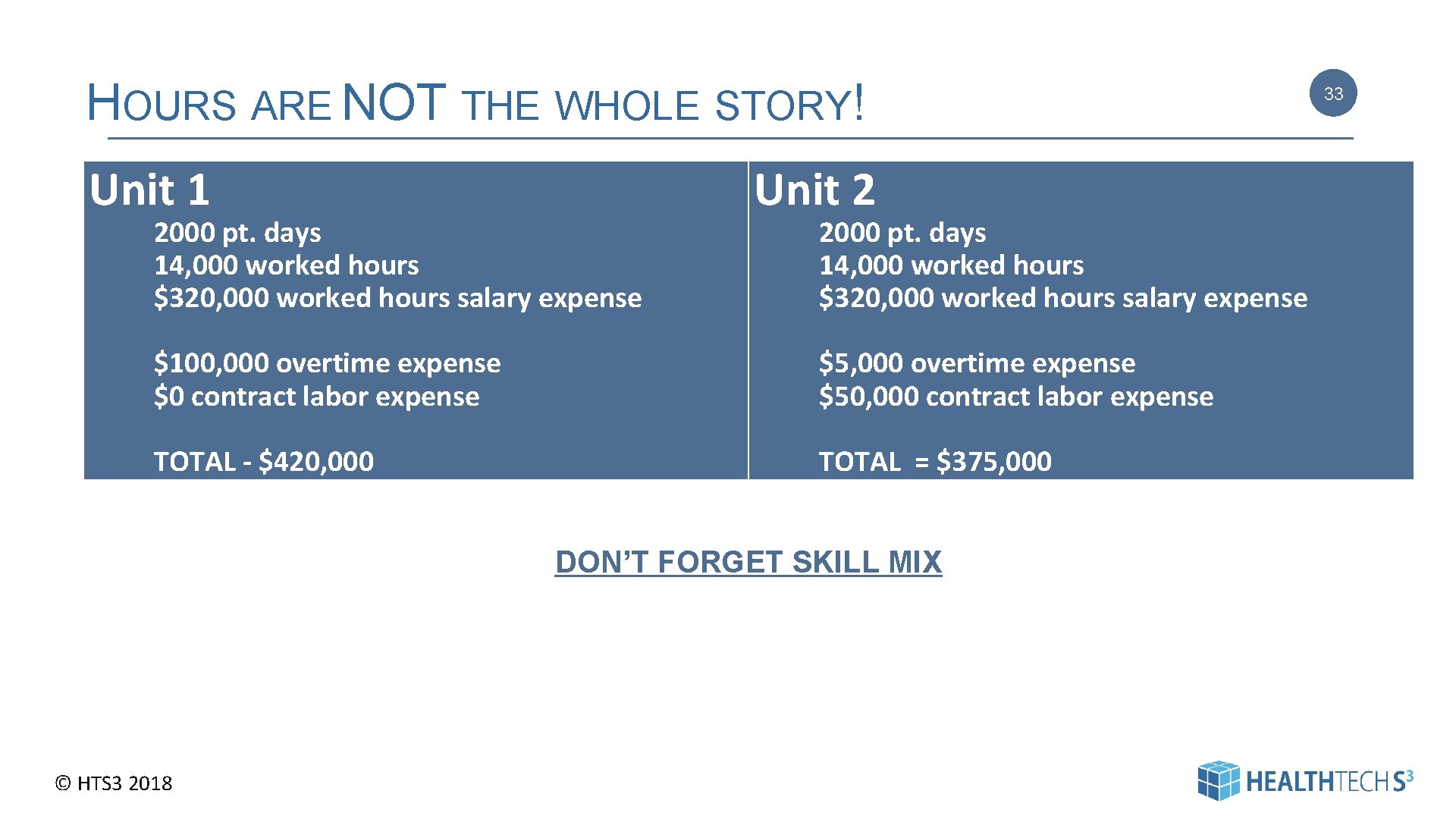
HOURS ARE NOT THE WHOLE STORY! Unit 1 2000 pt. days 14, 000 worked hours $320, 000 worked hours salary expense Unit 2 2000 pt. days 14, 000 worked hours $320, 000 worked hours salary expense $100, 000 overtime expense $0 contract labor expense $5, 000 overtime expense $50, 000 contract labor expense TOTAL - $420, 000 TOTAL = $375, 000 DON’T FORGET SKILL MIX © HTS 3 2018 33
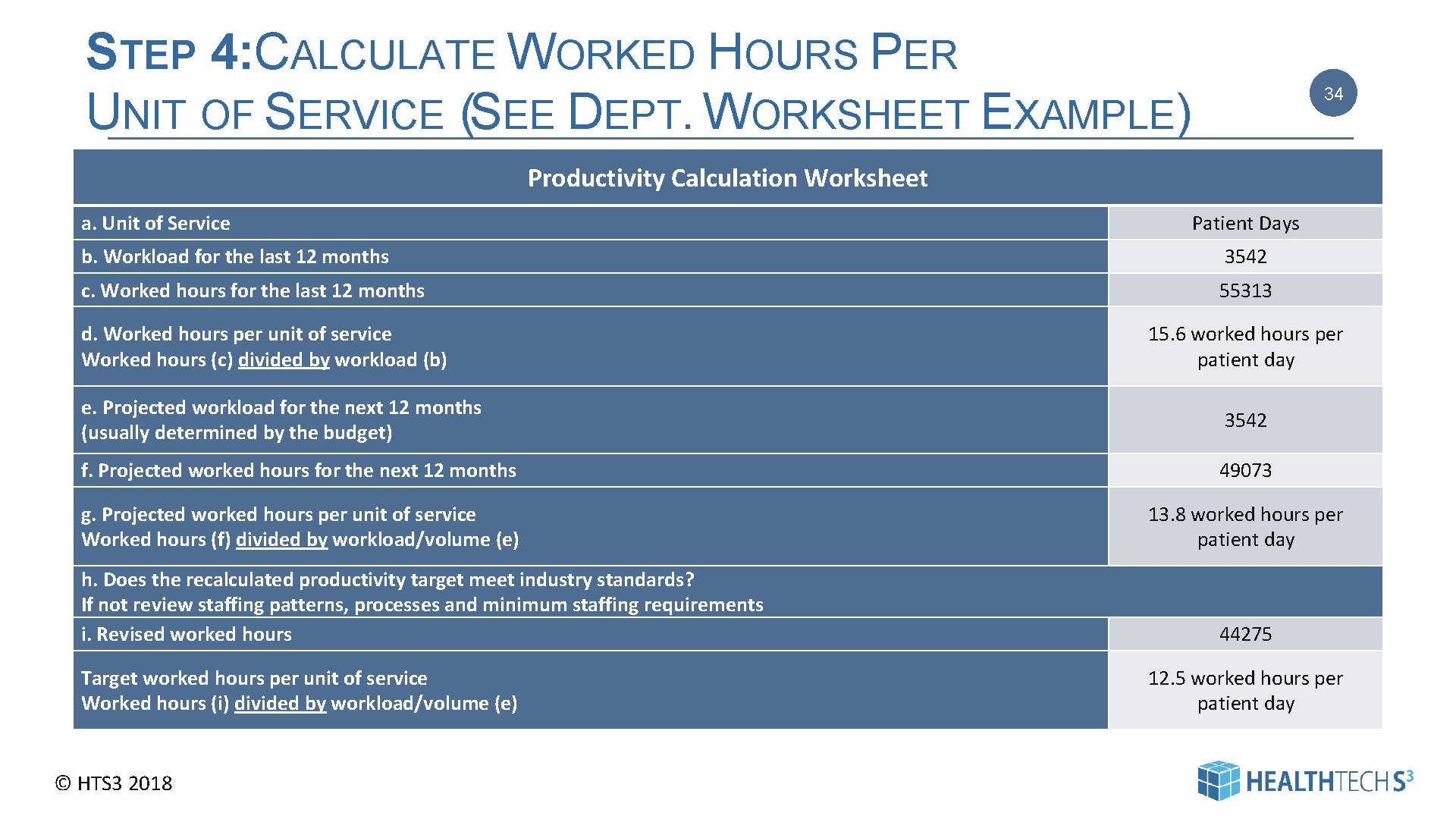
STEP 4: CALCULATE WORKED HOURS PER UNIT OF SERVICE (SEE DEPT. WORKSHEET EXAMPLE) 34 Productivity Calculation Worksheet a. Unit of Service Patient Days b. Workload for the last 12 months 3542 c. Worked hours for the last 12 months 55313 d. Worked hours per unit of service Worked hours (c) divided by workload (b) 15. 6 worked hours per patient day e. Projected workload for the next 12 months (usually determined by the budget) 3542 f. Projected worked hours for the next 12 months 49073 g. Projected worked hours per unit of service Worked hours (f) divided by workload/volume (e) 13. 8 worked hours per patient day h. Does the recalculated productivity target meet industry standards? If not review staffing patterns, processes and minimum staffing requirements i. Revised worked hours Target worked hours per unit of service Worked hours (i) divided by workload/volume (e) © HTS 3 2018 44275 12. 5 worked hours per patient day 34
IV. MONITORING – CONTROLLING – GETTING BETTER You can’t improve what you don’t measure © HTS 3 2018 35 | Pag e 35
MONITORING PRODUCTIVITY 36 1. Productivity reports daily (or at least bi-weekly) by department with roll-ups by VP and/or Administrator 2. Manager required variance reports 3. Senior Leader required variance reports 4. Individual meetings with manager and senior leader if continued variances © HTS 3 2018 36
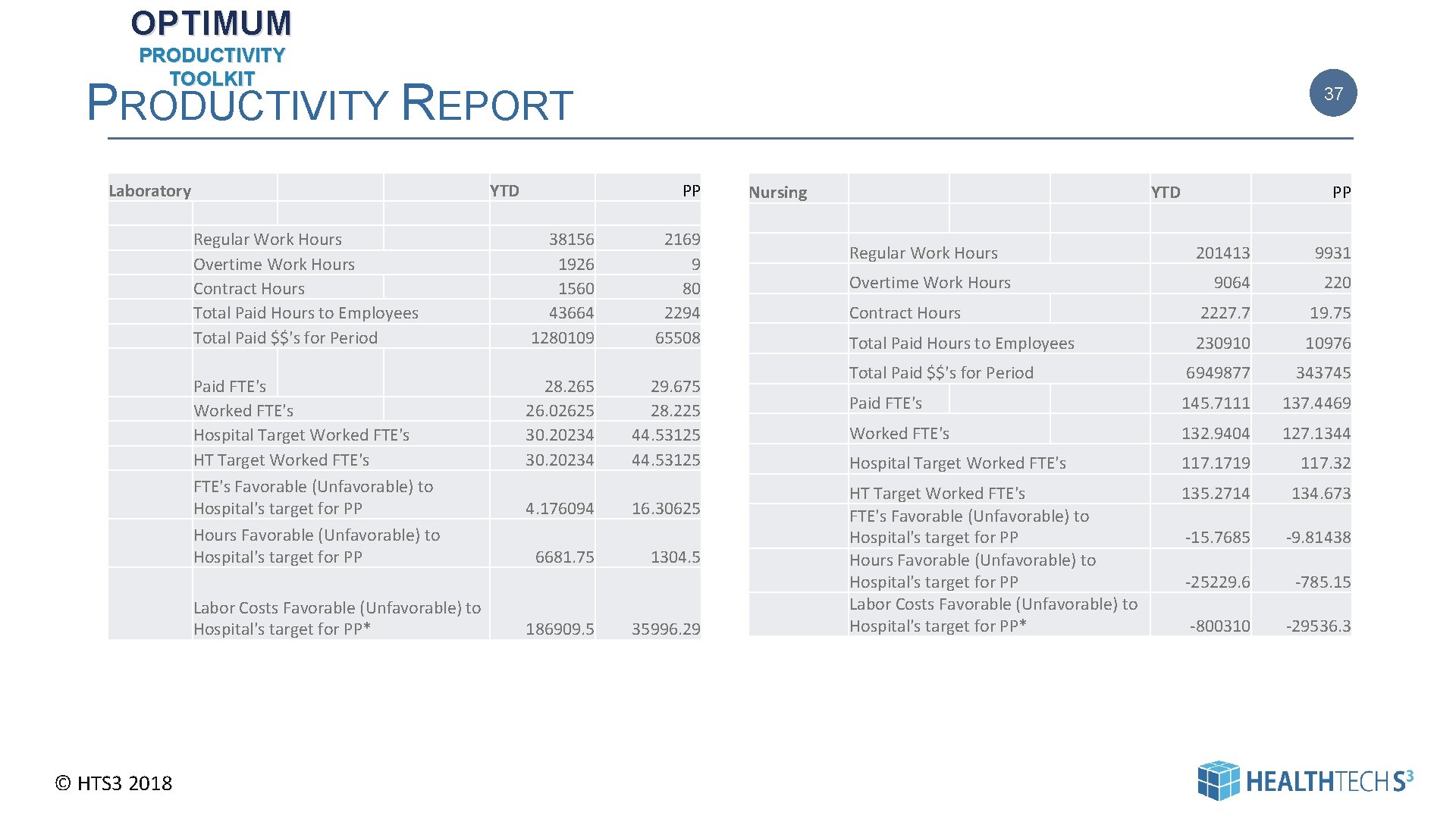
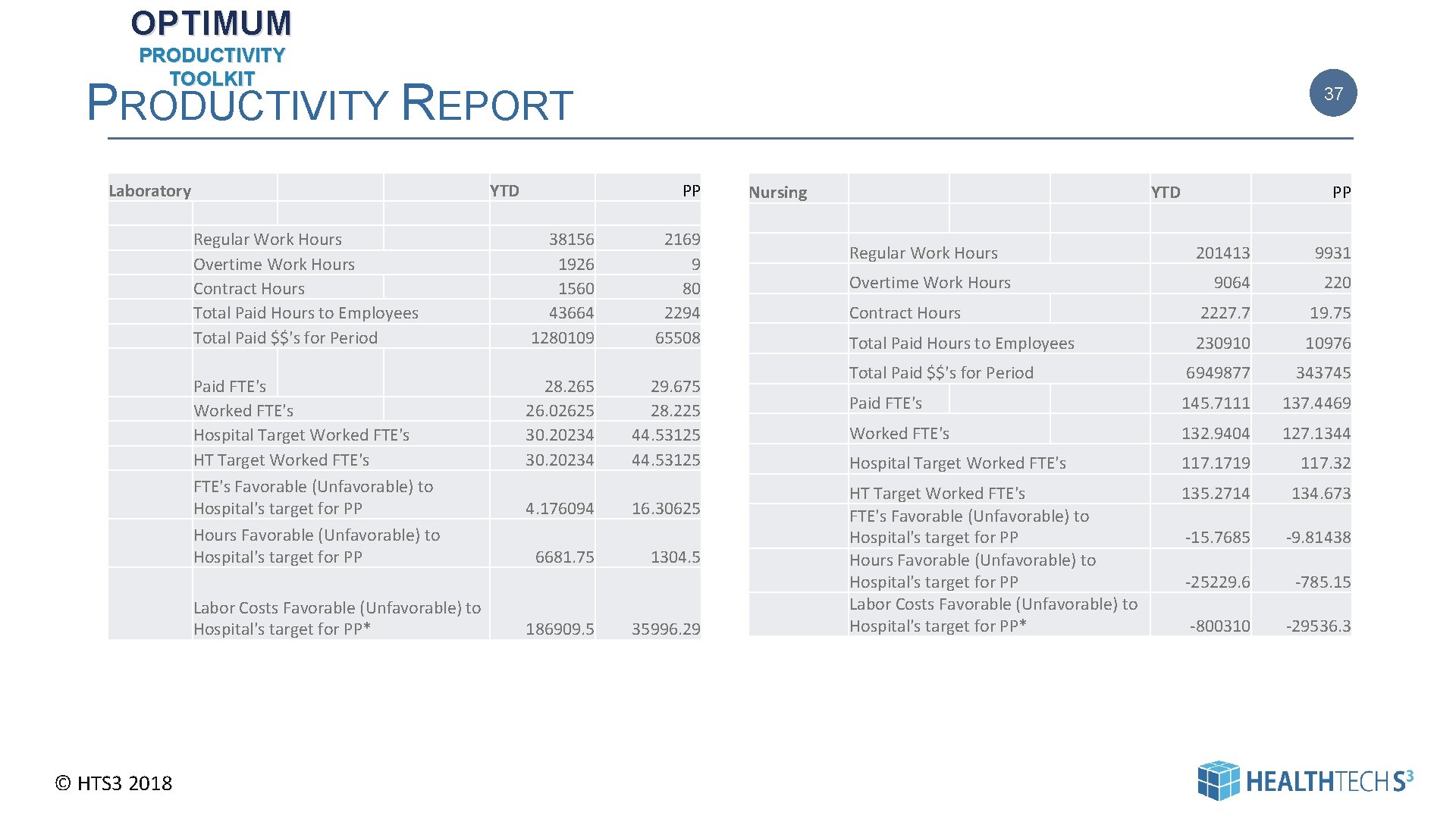
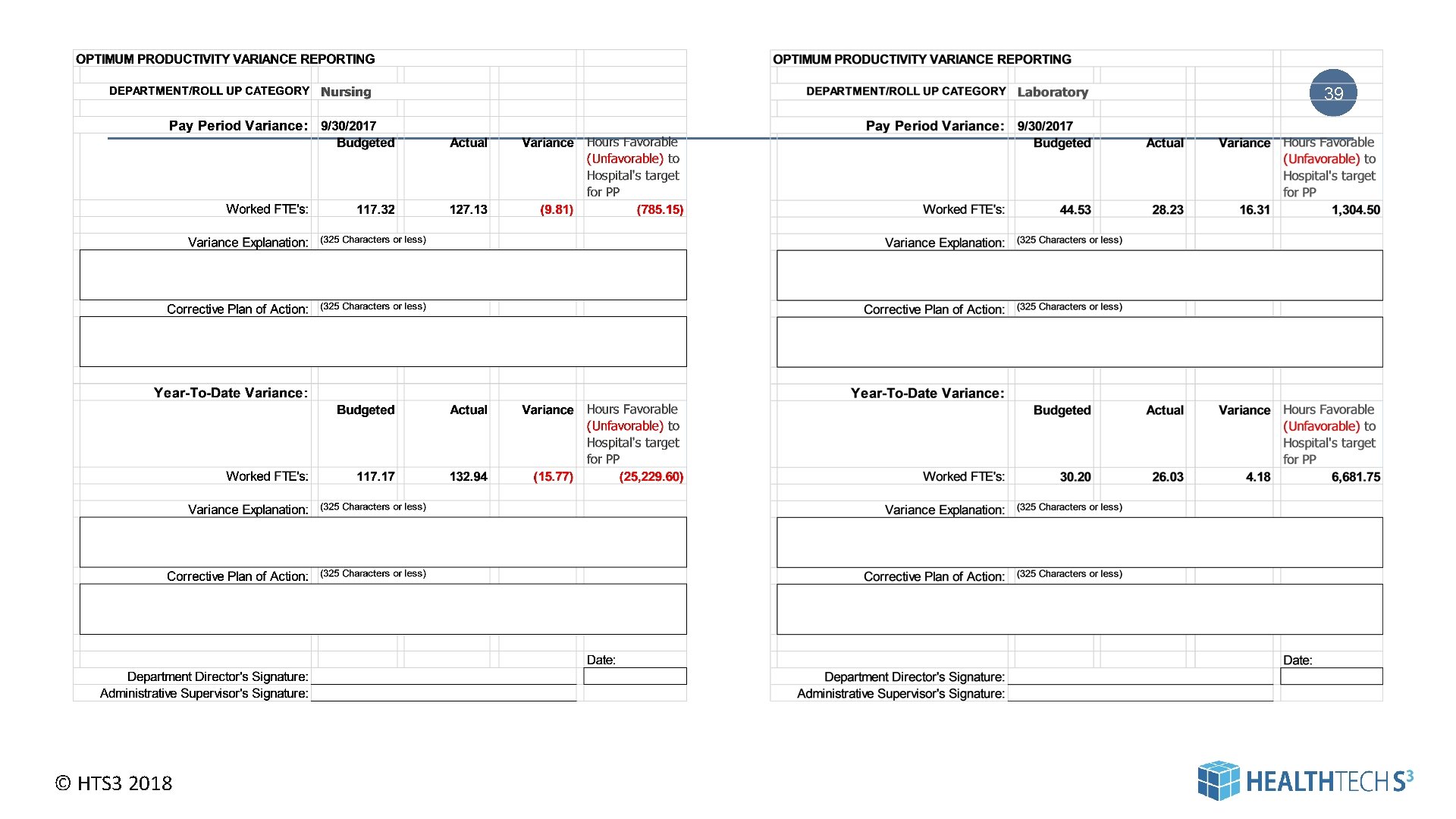
OPTIMUM PRODUCTIVITY TOOLKIT PRODUCTIVITY REPORT Laboratory YTD Regular Work Hours Overtime Work Hours Contract Hours Total Paid Hours to Employees Total Paid $$'s for Period Paid FTE's Worked FTE's Hospital Target Worked FTE's HT Target Worked FTE's Favorable (Unfavorable) to Hospital's target for PP Hours Favorable (Unfavorable) to Hospital's target for PP Labor Costs Favorable (Unfavorable) to Hospital's target for PP* © HTS 3 2018 37 PP 38156 1926 1560 43664 1280109 28. 265 26. 02625 30. 20234 4. 176094 6681. 75 186909. 5 2169 9 80 2294 65508 29. 675 28. 225 44. 53125 16. 30625 1304. 5 35996. 29 Nursing YTD Regular Work Hours PP 201413 9931 9064 220 Contract Hours 2227. 7 19. 75 Total Paid Hours to Employees 230910 10976 Total Paid $$'s for Period 6949877 343745 Paid FTE's 145. 7111 137. 4469 Worked FTE's 132. 9404 127. 1344 Hospital Target Worked FTE's 117. 1719 117. 32 HT Target Worked FTE's Favorable (Unfavorable) to Hospital's target for PP Hours Favorable (Unfavorable) to Hospital's target for PP Labor Costs Favorable (Unfavorable) to Hospital's target for PP* 135. 2714 134. 673 -15. 7685 -9. 81438 -25229. 6 -785. 15 -800310 -29536. 3 Overtime Work Hours 37
VARIANCE REPORTS Variance: Reason – Why? Is this one-time or is it expected to continue? What have you done to manage (reduce or eliminate) variance? © HTS 3 2018 38 38
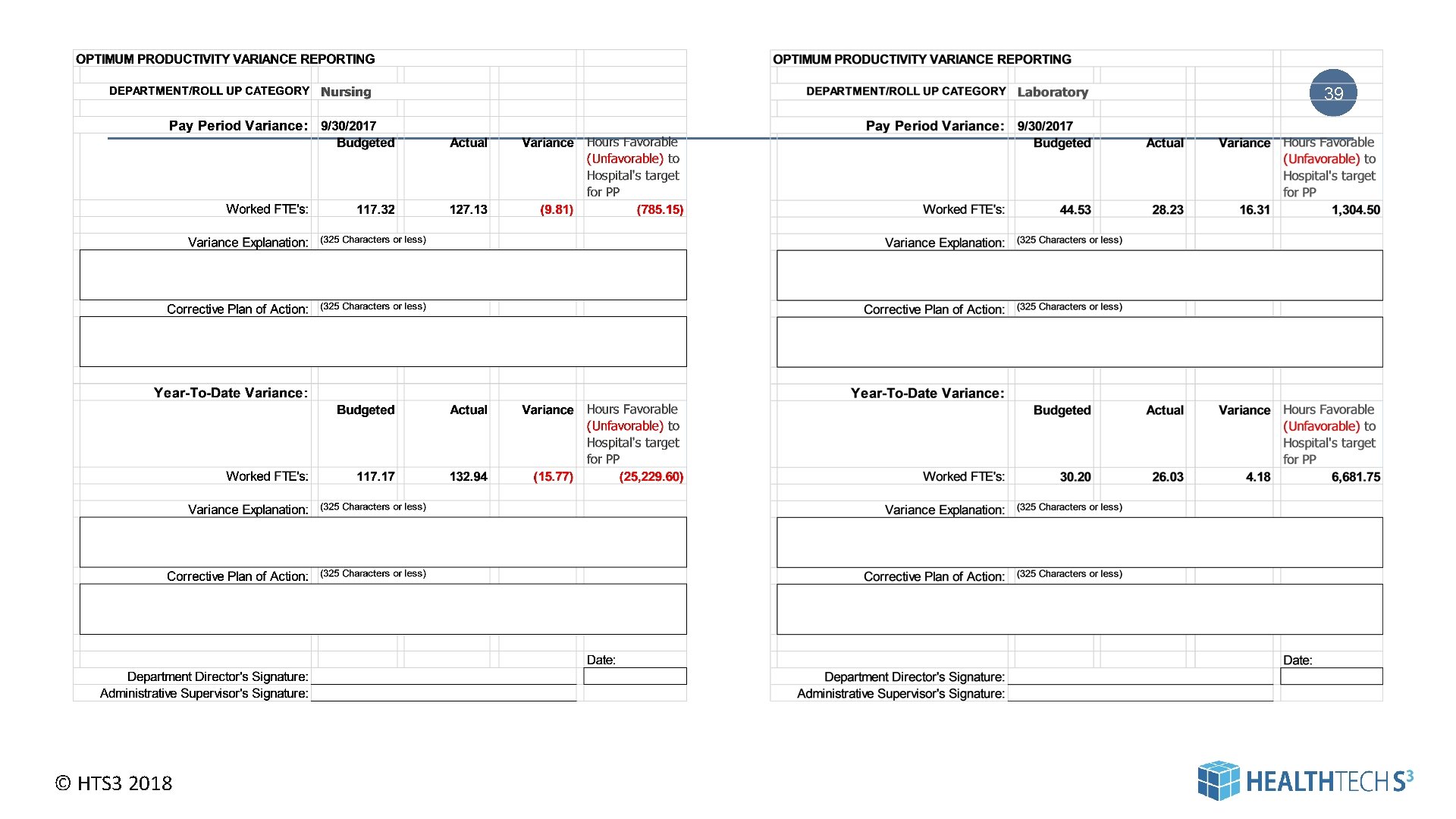
39 © HTS 3 2018
INDIVIDUAL MEETINGS --- FIRST SEEK TO UNDERSTAND © HTS 3 2018 40 40
IMPROVING PRODUCTIVITY - ONE CHOCOLATE AT A TIME 41 SPEED IT UP!!! Asking Staff To Do More with the Same Resources and the Same Systems – Seldom Works © HTS 3 2018 | Pag e 41
WASTE • Waste of time • Waste of ideas • Waste of methods / supplies • Waste of machinery / equipment • Waste of manpower • Waste of space © HTS 3 2018 42 “If it doesn’t add value, it’s waste. ” – Henry Ford “Waste is often disguised as useful work. ” – Hiroyuki Hirano “Activity that adds cost but not value. ” – Taiichi Ohno | Pag e 42
FUNDAMENTAL PRINCIPALS 43 Work redesign and process improvement are not “theoretical” but an essential component of effective staffing management 1. 2. Invest in work redesign 3. Invest in people – Evaluate how work is done – look – Team training at processes – Individual training – Remove rework / redundancy – Reward efforts from the system – Utilize technology 4. Measure Invest in clinical improvement – Utilize measurement – Use clinical protocols methodologies – Focus on prevention of complications – Focus on error prevention and patient safety © HTS 3 2018 | Pag e 43
V. A FEW PROBLEMS - A FEW SOLUTIONS © HTS 3 2018 44 44
PROBLEM: MANAGERS LACK THE NECESSARY KNOWLEDGE AND EXPERTISE 1. Invest - provide education and support for managers / charge nurses / shift supervisors / non- nursing department supervisors 2. Ensure that managers and supervisors are knowledgeable and understand concepts of effective staffing management 3. Provide regular information and feedback to staff and key stakeholders regarding staffing goals and objectives © HTS 3 2018 45 | Pag e 45
PROBLEM: IT’S NOT MY DEPARTMENT – IT’S NOT MY JOB – IT’S NOT MY RESPONSIBILITY 46 1. Facilitate departments working together to achieve organization wide improvements 2. Don’t make changes that improve one department’s productivity but decreases the productivity in another department’s without mutual agreement from all involved © HTS 3 2018 | Pag e 46
PROBLEM: OVERTIME IS EXPENSIVE © HTS 3 2018 47 | Pag e 47
TYPES OF OVERTIME • Planned • Incidental • Emergent Regardless, they are all Expensive! © HTS 3 2018 48 | Pag e 48
OVERTIME REDUCTION 1. Develop staffing rules to ensure there is staff coverage when it is needed – – – 2. Vacation Requested days off Number of staff who can be off at any one time Look at overtime every day, every pay period 3. Look at hours – dollars – percent – They each tell a different story 1. Drill down to understand WHY Your Improvement Strategy must depend on the “reason” for incurring overtime. If not it will likely fail. © HTS 3 2018 49 | Pag e 49
ASK WHY 5 TIMES Incidental Overtime - End of Shift WHY - Joe can’t finish work on time WHY – He’s the Supervisor and also has a full patient load WHY – Not enough staff – lots of vacancies WHY – No applicants WHY – No recruitment plan WHY - Call-Off (sick) replacement WHY – Average of 3 call-offs each week WHY – Not sure but it’s usually 2 specific staff WHY – No systems to counsel WHY - © HTS 3 2018 50 Vacation / Holiday replacement WHY – Staff can take vacation anytime WHY – No facility rules for how many staff can be off at one time WHY – We have never needed it – staff selfscheduled to ensure coverage but not working now WHY – Lots of new / younger staff WHY – 50
PROBLEM: WE SPEND A LOT OF MONEY ON ORIENTATION AND 51 EDUCATION Initial and Ongoing Education and Training as well as competency is absolutely critical in today’s healthcare environment 1. Separate types of education - to help understand where dollars are being spent and WHY – – – At-hire – Organization orientation Annual Unit / Department Orientation Nurse Residency Cross-Training If you have HIGH turnover you are going to have HIGH education / orientation costs! 2. Develop a plan for the Hospital and every department 3. Review the plan at least annually 4. Incorporate education hours /dollars in the staffing budget 5. Make use of on-line resources ----- but you can’t rely on them exclusively! © HTS 3 2018 51
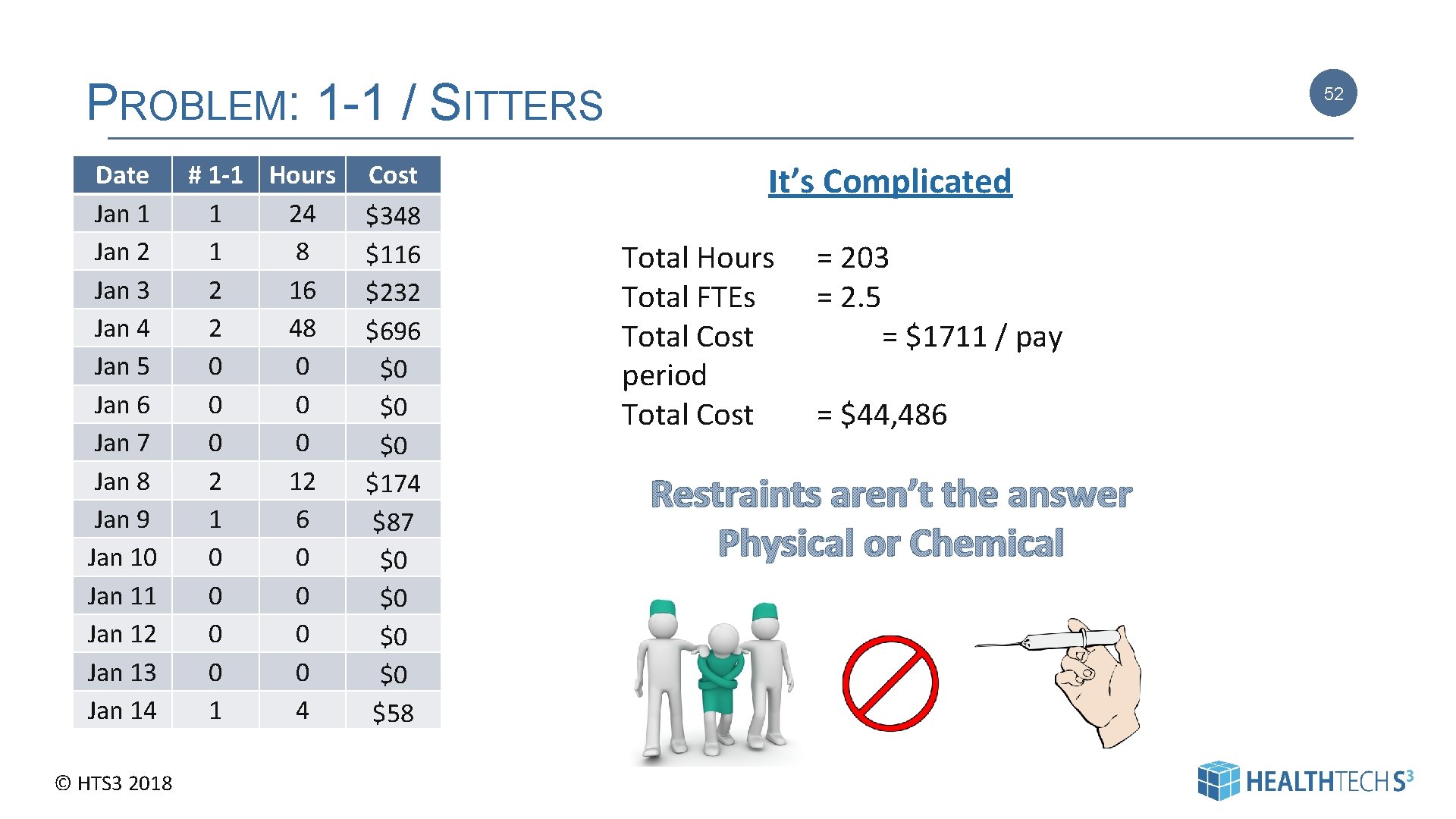
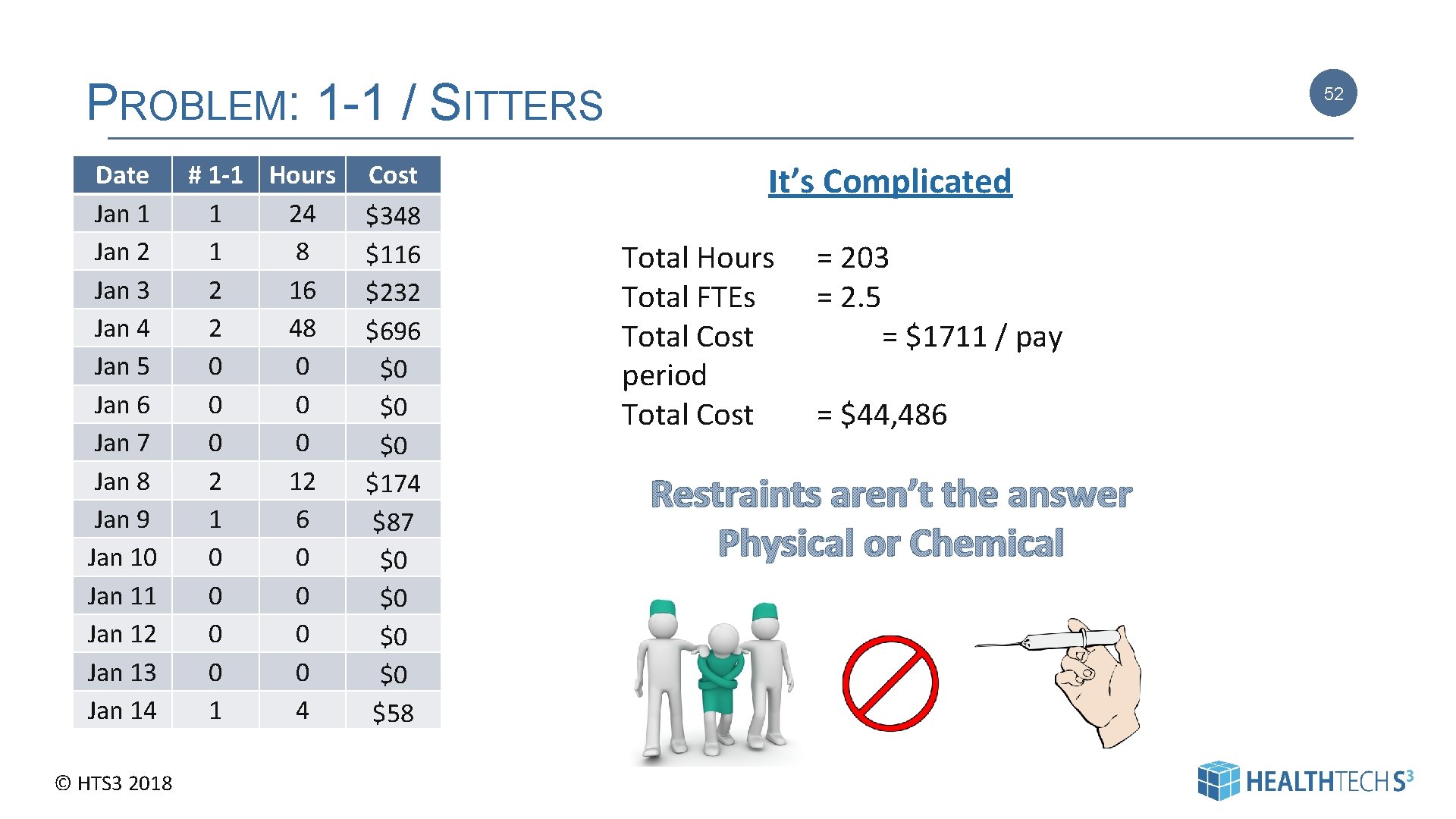
PROBLEM: 1 -1 / SITTERS Date Jan 1 Jan 2 Jan 3 Jan 4 Jan 5 Jan 6 Jan 7 Jan 8 Jan 9 Jan 10 Jan 11 Jan 12 Jan 13 Jan 14 © HTS 3 2018 # 1 -1 Hours 1 24 1 8 2 16 2 48 0 0 0 2 12 1 6 0 0 0 0 1 4 Cost $348 $116 $232 $696 $0 $0 $0 $174 $87 $0 $0 $58 52 It’s Complicated Total Hours Total FTEs Total Cost period Total Cost = 203 = 2. 5 = $1711 / pay = $44, 486 Restraints aren’t the answer Physical or Chemical 52
PROBLEM: TOO MANY STAFF - NOT ENOUGH STAFF – NEVER THE RIGHT NUMBER OF STAFF 53 1. Schedule with an understanding of historical volume for days of the week as well as seasons (Fall / Summer, etc. ) 5. Analyze the hours ancillary departments are open for business 6. Review on-call cost compared to having staff on-site 24/7. Repeat periodically for changes. 7. Flexible labor pool (yes it’s possible) 2. Explore/Develop /Utilize alternative shifts 3. Understand “minimum” staffing requirements 4. Do not schedule for “what if’s” – but make 8. sure you have adequate staffing for expected changes ---- 80%? Utilize shift supervisors / charge nurses to monitor and reassign workload throughout the day Research has demonstrated that lower quality of care occurs as a result of both being over and under staffed © HTS 3 2018 | Pag e 53
PROBLEM: WE DON’T HAVE THE RIGHT STAFF WITH THE RIGHT SKILLS WHEN WE NEED THEM 54 1. Review and adjust delivery model and skill mix to most effectively and efficiently meet the needs of both the patients and the facility for clinical and non-clinical departments 2. Develop position control so you can get to the right skill mix if you don’t have it now 3. Invest in cross-training ---- make it a requirement of employment © HTS 3 2018 | Pag e 54
PROBLEM: USE OF CONTRACT LABOR TO COVER BASIC STAFFING NEEDS 1. Invest in local colleges/ schools - “grow your own” 2. Encourage clinical program clinical affiliations 3. Develop an aggressive recruitment plan – HR is your friend 4. Set a timeline – and a target 5. Review your culture – is it a good place to work? Why are staff leaving? © HTS 3 2018 55 | Pag e 55
FINAL THOUGHTS WHERE ARE YOU SALARY DOLLARS GOING? DO YOU KNOW? WHERE ARE THE OPPORTUNITIES IN YOUR ORGANIZATION? By position – By department • Basic salary • Premium pay • Call-Back • Contract labor • Vacation / Holiday • Sick calls • Overtime • Orientation • Education © HTS 3 2018 56 56
A ZEN MOMENT 57 Yes – You’re looking at the numbers But You are in an ideal position to be the champion of change and improvement by looking at and understanding systems and processes related to staffing management © HTS 3 2018 57
58 Thank you! If you would like more information - or - have questions - or - would like to discuss our staffing management system at your facility please feel free to contact us. OPTIMUM PRODUCTIVITY TOOLKIT © HTS 3 2018 Dallas Office Brentwood Office Our Phone 2745 North Dallas Parkway, Suite 100, Plano, TX 75093 5110 Maryland Way, Suite 200 Brentwood, TN 37027 Main Office: 615. 309. 6053 Executive Placement: 972. 265. 4549 Consultants Kevin Stringer Kevin. stringer@healthtech. S 3. com 615 -636 -9779 John Freeman John. freeman@healthtech. S 3. com 615 -309 -7433 Diane Bradley Diane. Bradley@healthtechs 3. com 585 -671 -2212 Carolyn St. Charles Carolyn. stcharles@healthtechs 3. com 360 -584 -9868 58 58