How to Deal with Medical Uncertainty in the

- Slides: 55
How to Deal with Medical Uncertainty in the Biopsychosocial Model: The Educators Challenge. Joane Baumer, MD and Anita Webb, Ph. D JPS Health Network and Residency Programs 34 th Forum for Behavioral Science in Family Medicine Chicago 2013
Agenda • Introduction • Uncertainty in medical decision making • Impact of Uncertainty for the physician and patient relationship • Teaching uncertainty in residency – Israel- Palestine elective • Discussion
Objectives • Describe uncertainty in the medical setting • Describe the research in the area of uncertainty • Delineate an approach to teaching uncertainty to medical learners

MAIN THEMES 1. Uncertainty is an inescapable aspect of medicine. 2. There are different types of uncertainty. 3. Uncertainty can be detrimental or beneficial. 4. Personality affects how you deal with uncertainty. 5. Training can increase uncertainty awareness
BASELINE • “Medicine’s ground state is uncertainty” – Atul Gawande, MD – 1. Complications: a surgeon’s notes on an imperfect science. Metro Books/Henry Holt & Co. NY 2002.
HOWEVER: “Culture of Western Medicine” • • “Educated for dogmatic certainty” “Rigid, unrealistic” “In love with technology” “Culture of conformity” -[ibid. ]
Realities of Medicine • • Instability Uniqueness Uncertainty Incomplete information – About patient – About science/medicine • These realities create stress
PLUS: Confounding Factors • • • -Value conflicts with patients -Contrasting medical opinions -Legal issues -Institutional rules -Conflicts within patient’s family – e. g. End-of-life issues
The Problem with Uncertainty • “Analysis Paralysis” • Decisions must be made – In spite of limited information. • Creates stress – For physician and for patient
Possible Benefits of Uncertainty? • • Motivator: Adds impetus Thoroughness: Consider all aspects Promotes caution May result in restructuring of problem With new solution • “Uncertainty sometimes is essential for success. ”
What is Certain? The modern clinical team for the patient centered model of care MUST BE COMFORTABLE WITH UNCERTAINTY
WISDOM • “Wisdom – – “For both patients and physicians - • “Is defined by: – “How one copes with [uncertainty]. ” – 1. Gawande (2002)
TOLERANCE • “Physicians differ in their ability to tolerate uncertainty. ” • “This varying tolerance has been linked with – “Choice of specialty” – 2. Ghosh (2004).
Research on Low Tolerance • Increased – Test ordering – Anxiety – Costs (etc. ) • Decreased comfort with – Geriatrics – Psychological problems • 2. Ghosh (2004)
Intolerance of Uncertainty • • Authoritarian personality (e. g. dictator) Rigid mindset: Inflexible Sees the world in black-and-white Threatened by uncertainty – Feels out of control, which is frightening – Difficulty adjusting to change – “My way or the highway”
Medical Dictionary • “Authoritarian Personality” • Desire for security, order, power, and status – Structured lines of authority – Conventional set of values or outlook – Demands unquestioning obedience – Tendency to be hostile toward minority or nontraditional groups
Training for Uncertainty Management • Physician Personality • Stages of Development • Research – Boston Study – London Study – Recent Study • The Palestine/Israel Elective – At JPS
Selection of Physicians Up Front Do we need to assess temperment ? Which are the most likely to be successful?
Physician’s Temperament • “Much of medical uncertainty has to do with the practitioner. ” – “Some are at home with uncertainty, – “Whereas others require definitive answers. ” • “These differences in temperament dictate – “Choice of specialty. ” – 3. Wellbery. Associate Professor of Family Medicine, Georgetown Univ. Med. Center; Associate Deputy Editor, Am. Family Physician.
Temperament (cont. ) • “Most of what doctors do is help patients navigate – “Ambivalence, complexity and – “The unknowns of their illness…” • “These practitioners do not lose competence or confidence in the setting of uncertainty. – “Rather, they ride the uncertainty as part of care… – “And at times, experience their richest moments in pondering its mysteries. ” – ibid.
Temperament (cont. ) • “Medical uncertainty is also an opportunity. ” – “Ambiguity and uncertainty are not obstacle to be overcome – “But rather avenues to be explored. ” • Physicians who are comfortable with uncertainty – “Can turn medical uncertainty to their advantage “ – “By redirecting patients’ priorities. ” – ibid.
Family Physician Advantages • • Communication skills Relationships with patients Trust, respect, continuity Knowledge of the patient – Fears, hopes – Tolerance of uncertainty – Social circumstances – Personalized patient feedback
“It is a fact of life” • Human beings find it difficult to maintain – Consistent, self-conscious appreciation of the extent – To which uncertainty accompanies them on daily rounds • Physicians will acknowledge medicine’s uncertainty – Once its presence is forced into conscious awareness, – Yet at the same time will continue to conduct their practices as if uncertainty did not exist. • 4. Katz J. Why doctors don’t disclose uncertainty. Hastings Center Report, Feb. 1984; 14(1): 35 -44.
RESEARCH • “Research on physician disclosure of uncertainty to patients is sparse. ” • A study at university-based medical clinic in Boston – 43 physicians – 216 continuity patients – Audiotaped clinic visits • Results: physician verbal expressions of uncertainty – In 71% of clinic visits. ” • (continued)
Results (cont. ) • More positive talk and partnership building • Gave more information to patients – More education – Patients had greater desire for information • Associated with greater patient satisfaction – 5. Gordon 2000
London Study • Questionnaires: 66 GP’s, 550 patients • Patients and GPs rated physician verbal expressions of uncertainty as potentially damaging to confidence. – Especially younger, lower socioeconomic patients – BUT: OK to consult book or computer in exam room • Verbal expressions of uncertainty have – A “consistently detrimental effect” on patients – Negative effect was underestimated by physicians – 6. Ogden 2002
Great Britain: Study • How clinicians deal with uncertainty: 10 clinics • 1. Focus on certainty – “Slippage into general reassurance” • 2. Coherent account of medical evidence – Giving the impression of certainty • 3. Acknowledge inherent uncertainty in medicine – Negotiate a provisional decision – 7. Griffiths 2005
Recent Study • “Research has not yet identified – “Best practices for communicating uncertainty to patients about harms and benefits of treatment. ” • Need research on: – “How people process, interpret, and respond to – “Various types of uncertainty – “Inherent in clinical decisions. ” • 8. Politi 2012
JPS Israel Palestine Elective Immersion Learning? • 1 month elective underway for 3 years – 2 weeks in Israel and 2 weeks in Palestine • Focus is on comparative systems • Primary goal is to get participants to compare systems of care for systems based practice requirement • Surprising outcome was a marked increase in participant awareness of ambiguity, uncertainty and increase in tolerance
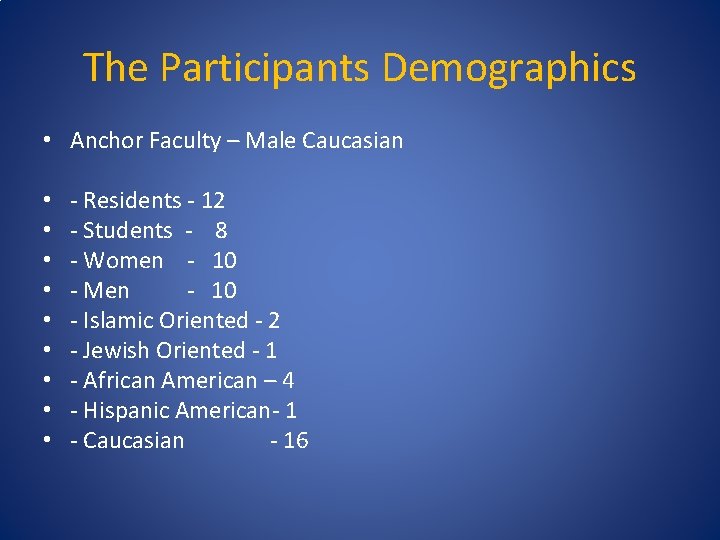
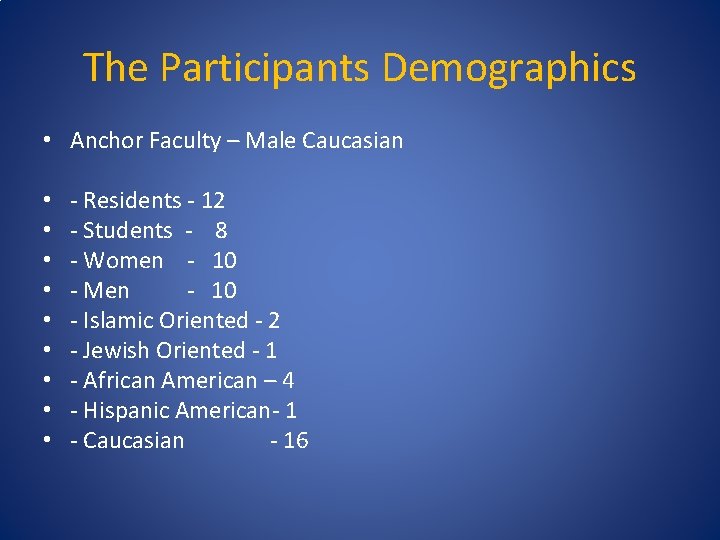
The Participants Demographics • Anchor Faculty – Male Caucasian • • • - Residents - 12 - Students - 8 - Women - 10 - Men - 10 - Islamic Oriented - 2 - Jewish Oriented - 1 - African American – 4 - Hispanic American- 1 - Caucasian - 16
The Setting- A Juxtaposition • A high functioning public health system in Israel • VS • A fractured 4 branched system in Palestine with abject poverty , social isolation and lack of access for most and some US style hospital services for the wealthy • An occupation limiting access
Students’ Comment “I became aware of my own biases and learned how to see the world through the eyes of others. ” “Out of all of my experiences, this has truly shaped my world view and changed my perspective”
Resident’s comment • “ I know there are no simple answers • I know there will be violence” • This trip has made profoundly aware of the gap in my knowledge regarding the interpretation of these data”
Residents’ Comment’s • “My comments may come across as harsh and biased, but they reveal some of the tension and emotions I experienced” • “Often, I am so overwhelmed by the prescriptions, protocols and pathology of medicine that I overlook the reason I was called to practice medicine”
Impact of Uncertainty • “I understand now the overpowering psychosomatic stress of utter uncertainty”
Impact of Positivity in difficult situations • “I am often frustrated by the limits of the power of Western Medicine – wishing I could do something more for my patients…. . • my experiences in Palestine have shown me the true power of positivity and I return with the goal of being a positive influence in the lives of my patients, friends and family members every day”
Another Example from a student • “ I have seen a lot of right and wrong in the last month, but I have also seen a lot of smiles and laughter and hope. It will never cease to amaze me how the greatest joy seems to swell from some of the most terrible circumstances”
final note - resident • “ It showed me , that whatever frustrations I have with practicing medicine, … never to be deterred. If I allow my frustrations with patients to spoil my initial motivations to practice medicine , I make myself my own enemy. I am now striving to be a more empathetic and resourceful physician as the Palestinian physicians are on a daily basis. ”
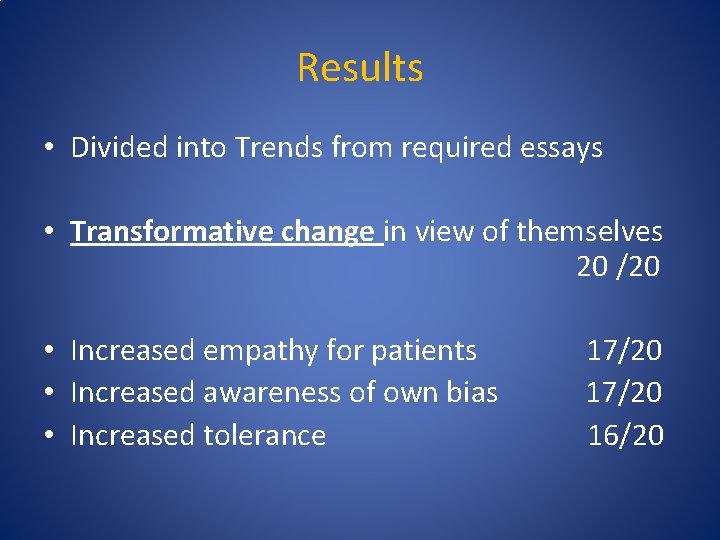
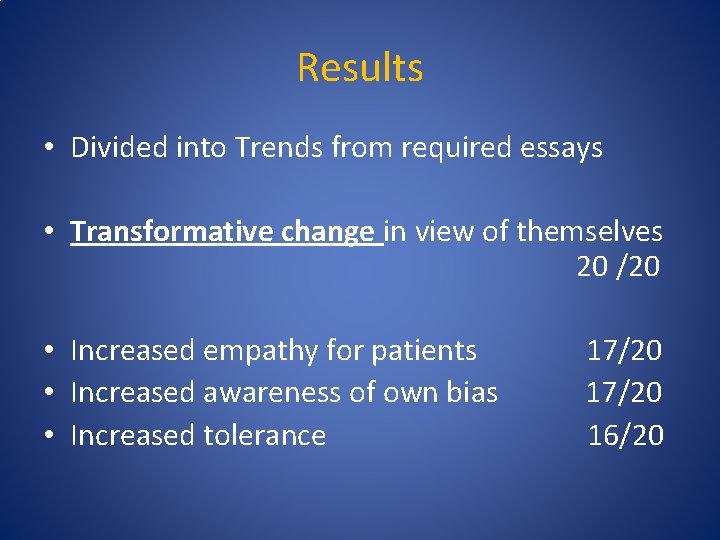
Results • Divided into Trends from required essays • Transformative change in view of themselves 20 /20 • Increased empathy for patients • Increased awareness of own bias • Increased tolerance 17/20 16/20
CONCLUSION ◦ Participants returned with renewed purpose in their careers ◦ They recognized the transformation in themselves ◦ They recognized the uncertainty and increased tolerance of the environments
Other encouraging trends • A comparison of tolerance in 264 medical students and practicing physicians demonstrates better tolerance in practicing physicians in Israel • A corroborative study of 1184 physicians in Switzerland demonstrated the greatest anxiety from uncertainty in physicians in training compared to practicing physicians
Complex Adaptive Systems • Comprised of agents who learn and adapt – “Embracing uncertainty and surprise” – (Complexity Science) • “No one is better prepared to understand the implications of complexity science – “Than those of us in family medicine. – “Intuitively, we do. ” – [Referring to medical education, also applies to practice. ] • 9. Parchman 2009
How to Teach • Still anecdotal • Early evidence is promising • Will require a great deal more research to see if : – Nature ( inherent personality of clinician) can be modified by Nurture – (impact of our training programs)
Domains of Dynamic Progression • -COGNITIVE: Increasing information, plus ability to process/integrate facts, opinions • -PERSONALITY: Greater tolerance for differing opinions • -MORAL: Increasing tolerance of ambiguity • -PROFESSIONAL: Increasing experience, confidence and “power”
Managing “Uncertainty Anxiety” • • • Meticulous history-taking Meticulous evaluation Exclusion of worrisome diagnoses Critical appraisal of current literature Establishing trust with patient Shared decision-making
Shared Decision Making • Must have precise communication • Requires accurate knowledge of patient capabilities, culture and literacy. • Requires resident self-awareness of their own cultural bias • Requires the resident to assess how much risk they and the patient can tolerate
Then What?
The Art of the Educated Guess • With each patient the resident can master uncertainty when the dyad can discuss: – What is the worst case scenario? – What is the best case scenario? – What is the most likely case scenario? – What is the risk of waiting to make a definitive diagnosis and plan • Then both can move forward with a plan
Discussion • Is there a specific strategy for dealing with uncertainty and/or ambiguity in your curriculum? • What has worked? • Do you agree with the trends in the research?
SUGGESTIONS for LEARNERS • • Acknowledge, accept your personality type. Learn stress management techniques. Look for the “opportunity” in uncertainty. Help your patients accept uncertainty by focusing on their life priorities.
References • • • 1. Gawande, Atul. Complications: a surgeon’s notes on an imperfect science. Metro Books/Henry Holt & Co. NY 2002. 2. Ghosh, AK. Understanding medical uncertainty: a primer for physicians. JAPI, 2004 -japi. org. 3. Wellbery, C. A case of medical uncertainty. Am. Fam Physician. 2012 Mar 1; 85(5): 501, 508. 4. Katz, J. Why doctors don’t disclose uncertainty. Hastings Center Report, Feb. 1984; 14(1): 35 -44. 5. GH Gordon, SK Joos, J Byrne. Physician expressions of uncertainty during patient encounters. Patient Ed and Counseling, 2000 Elsevier. 6. Ogden, J, Fuks K, Gardner M, Johnson S. Doctors expressions of uncertainty and patient confidence. Patient education, 2002 – Elsevier.
References (cont. ) 7. Griffith F, Green E, Tsouroufli M. The nature of medical evidence & its inherent uncertainty for the clinical consultation: qualitative study, BMJ. 2005 Mar 5; 330(7490): 511. 8. Politi MC, Studts JL, Hayslip JW. Shared Decision Making in Oncology Practice: What Do Oncologists Need to Know? The Oncologist, Jan 2012; 17: 1 91 -100. 9. Parchman ML. Complexity Science and pre-doctoral education: Embracing uncertainty and surprise. Undated Power. Point presentation. Available at: http: //www. fmdrl. org/index. cfm? event=c. begin. Browse. D&clear. S elections=1&criteria=Michael L. Parchman#2119