HOW MANY DOES IT TAKE ACHIEVEMENT OF EUPLOID
- Slides: 1
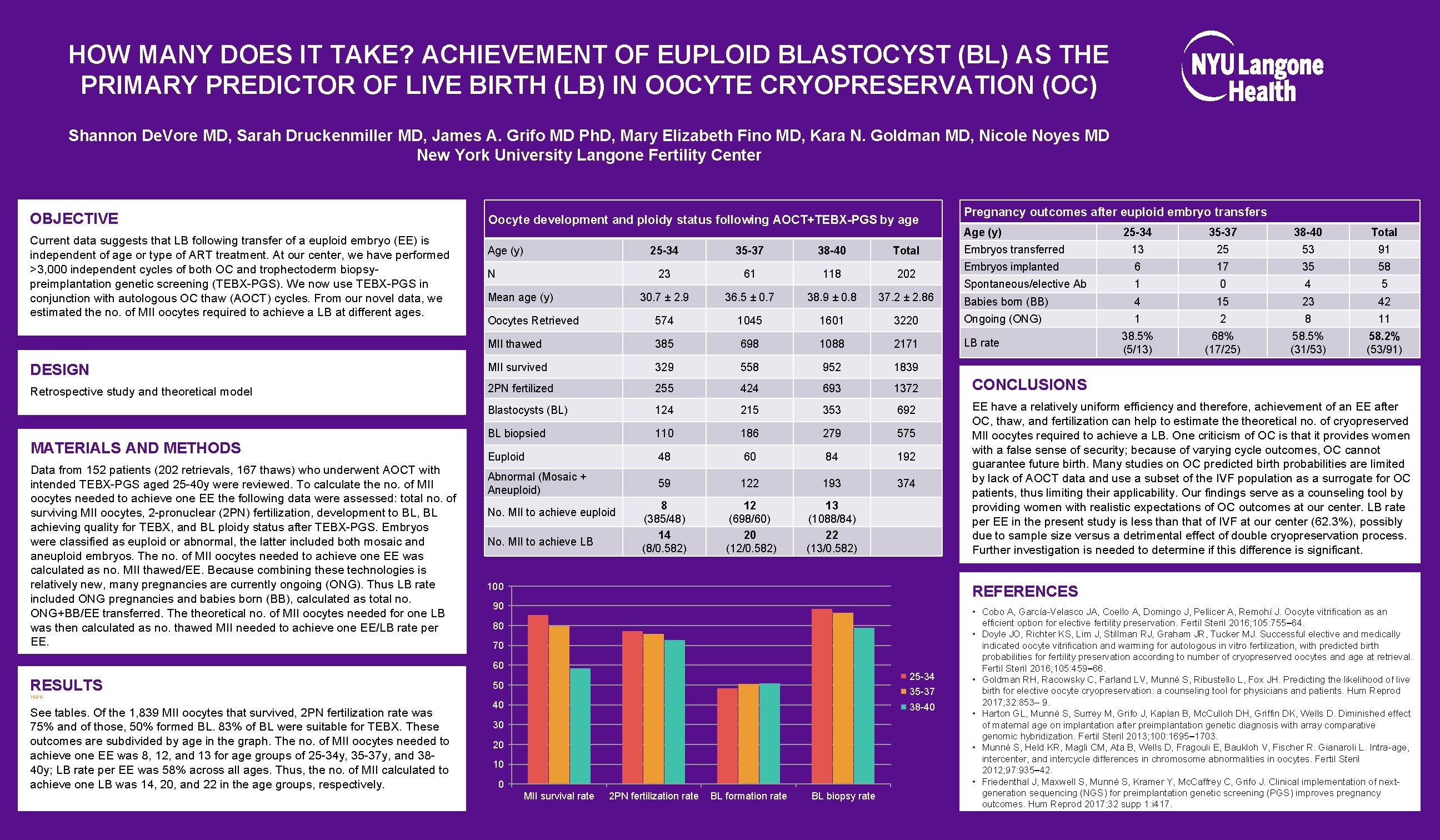
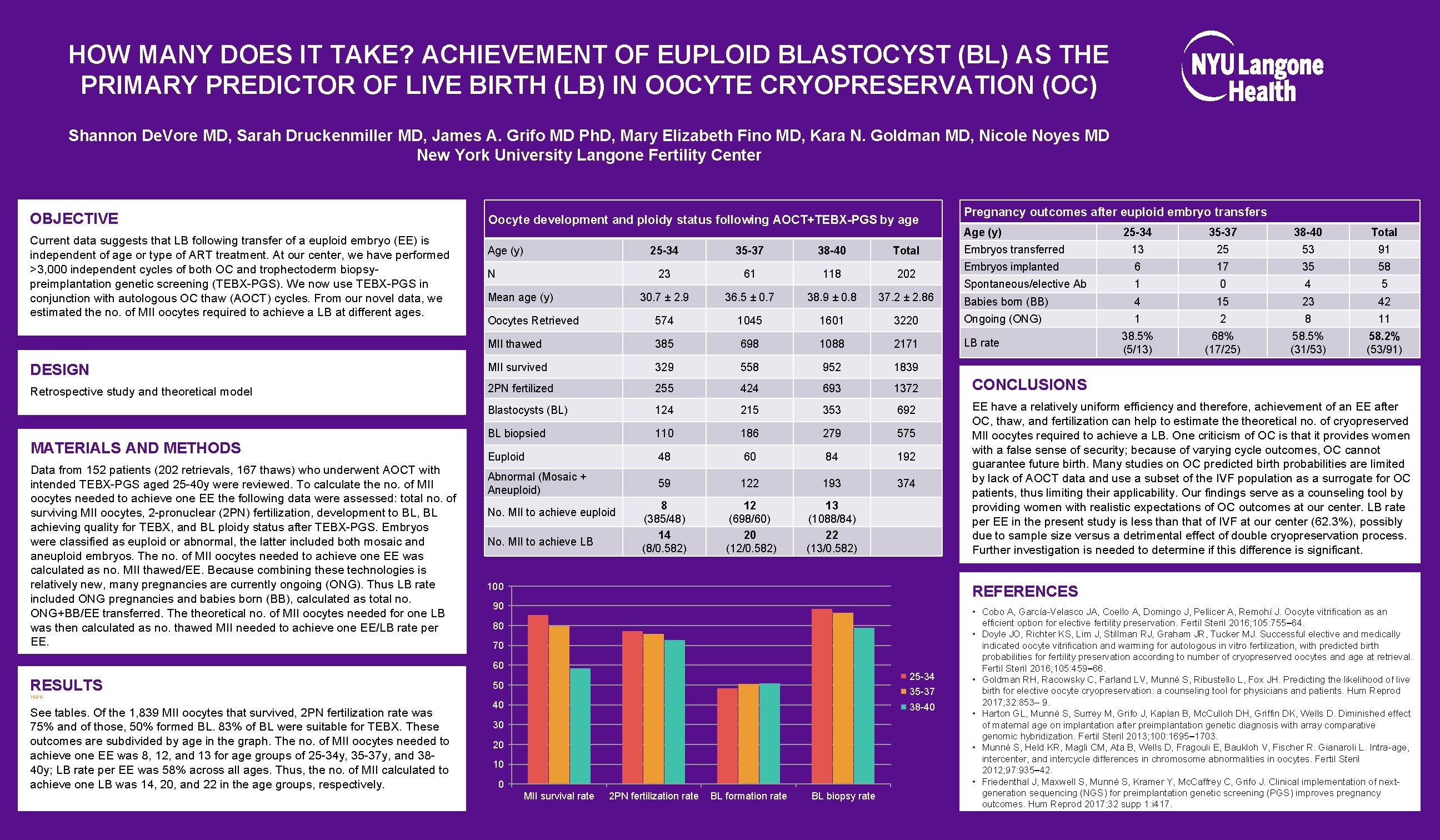
HOW MANY DOES IT TAKE? ACHIEVEMENT OF EUPLOID BLASTOCYST (BL) AS THE PRIMARY PREDICTOR OF LIVE BIRTH (LB) IN OOCYTE CRYOPRESERVATION (OC) Shannon De. Vore MD, Sarah Druckenmiller MD, James A. Grifo MD Ph. D, Mary Elizabeth Fino MD, Kara N. Goldman MD, Nicole Noyes MD New York University Langone Fertility Center OBJECTIVE Current data suggests that LB following transfer of a euploid embryo (EE) is independent of age or type of ART treatment. At our center, we have performed >3, 000 independent cycles of both OC and trophectoderm biopsypreimplantation genetic screening (TEBX-PGS). We now use TEBX-PGS in conjunction with autologous OC thaw (AOCT) cycles. From our novel data, we estimated the no. of MII oocytes required to achieve a LB at different ages. Oocyte development and ploidy status following AOCT+TEBX-PGS by age Age (y) 25 -34 35 -37 38 -40 Total Embryos transferred 13 25 53 91 Embryos implanted 6 17 35 58 Spontaneous/elective Ab 1 0 4 5 Babies born (BB) 4 15 23 42 1 2 8 11 38. 5% (5/13) 68% (17/25) 58. 5% (31/53) 58. 2% (53/91) 25 -34 35 -37 38 -40 Total 23 61 118 202 30. 7 ± 2. 9 36. 5 ± 0. 7 38. 9 ± 0. 8 37. 2 ± 2. 86 Oocytes Retrieved 574 1045 1601 3220 Ongoing (ONG) MII thawed 385 698 1088 2171 LB rate DESIGN MII survived 329 558 952 1839 Retrospective study and theoretical model 2 PN fertilized 255 424 693 1372 Blastocysts (BL) 124 215 353 692 BL biopsied 110 186 279 575 Euploid 48 60 84 192 Abnormal (Mosaic + Aneuploid) 59 122 193 374 8 (385/48) 14 (8/0. 582) 12 (698/60) 20 (12/0. 582) 13 (1088/84) 22 (13/0. 582) MATERIALS AND METHODS Data from 152 patients (202 retrievals, 167 thaws) who underwent AOCT with intended TEBX-PGS aged 25 -40 y were reviewed. To calculate the no. of MII oocytes needed to achieve one EE the following data were assessed: total no. of surviving MII oocytes, 2 -pronuclear (2 PN) fertilization, development to BL, BL achieving quality for TEBX, and BL ploidy status after TEBX-PGS. Embryos were classified as euploid or abnormal, the latter included both mosaic and aneuploid embryos. The no. of MII oocytes needed to achieve one EE was calculated as no. MII thawed/EE. Because combining these technologies is relatively new, many pregnancies are currently ongoing (ONG). Thus LB rate included ONG pregnancies and babies born (BB), calculated as total no. ONG+BB/EE transferred. The theoretical no. of MII oocytes needed for one LB was then calculated as no. thawed MII needed to achieve one EE/LB rate per EE. Age (y) Pregnancy outcomes after euploid embryo transfers N Mean age (y) No. MII to achieve euploid No. MII to achieve LB 100 90 80 70 25 -34 50 35 -37 18. 9% See tables. Of the 1, 839 MII oocytes that survived, 2 PN fertilization rate was 75% and of those, 50% formed BL. 83% of BL were suitable for TEBX. These outcomes are subdivided by age in the graph. The no. of MII oocytes needed to achieve one EE was 8, 12, and 13 for age groups of 25 -34 y, 35 -37 y, and 3840 y; LB rate per EE was 58% across all ages. Thus, the no. of MII calculated to achieve one LB was 14, 20, and 22 in the age groups, respectively. EE have a relatively uniform efficiency and therefore, achievement of an EE after OC, thaw, and fertilization can help to estimate theoretical no. of cryopreserved MII oocytes required to achieve a LB. One criticism of OC is that it provides women with a false sense of security; because of varying cycle outcomes, OC cannot guarantee future birth. Many studies on OC predicted birth probabilities are limited by lack of AOCT data and use a subset of the IVF population as a surrogate for OC patients, thus limiting their applicability. Our findings serve as a counseling tool by providing women with realistic expectations of OC outcomes at our center. LB rate per EE in the present study is less than that of IVF at our center (62. 3%), possibly due to sample size versus a detrimental effect of double cryopreservation process. Further investigation is needed to determine if this difference is significant. REFERENCES 60 RESULTS CONCLUSIONS 40 38 -40 30 20 10 0 MII survival rate 2 PN fertilization rate BL formation rate BL biopsy rate • Cobo A, García-Velasco JA, Coello A, Domingo J, Pellicer A, Remohí J. Oocyte vitrification as an efficient option for elective fertility preservation. Fertil Steril 2016; 105: 755– 64. • Doyle JO, Richter KS, Lim J, Stillman RJ, Graham JR, Tucker MJ. Successful elective and medically indicated oocyte vitrification and warming for autologous in vitro fertilization, with predicted birth probabilities for fertility preservation according to number of cryopreserved oocytes and age at retrieval. Fertil Steril 2016; 105: 459– 66. • Goldman RH, Racowsky C, Farland LV, Munné S, Ribustello L, Fox JH. Predicting the likelihood of live birth for elective oocyte cryopreservation: a counseling tool for physicians and patients. Hum Reprod 2017; 32: 853– 9. • Harton GL, Munné S, Surrey M, Grifo J, Kaplan B, Mc. Culloh DH, Griffin DK, Wells D. Diminished effect of maternal age on implantation after preimplantation genetic diagnosis with array comparative genomic hybridization. Fertil Steril 2013; 100: 1695– 1703. • Munné S, Held KR, Magli CM, Ata B, Wells D, Fragouli E, Baukloh V, Fischer R. Gianaroli L. Intra-age, intercenter, and intercycle differences in chromosome abnormalities in oocytes. Fertil Steril 2012; 97: 935– 42. • Friedenthal J, Maxwell S, Munné S, Kramer Y, Mc. Caffrey C, Grifo J. Clinical implementation of nextgeneration sequencing (NGS) for preimplantation genetic screening (PGS) improves pregnancy outcomes. Hum Reprod 2017; 32 supp 1: i 417.