How I do CMR in valvular heart disease

- Slides: 23
‘How I do’ CMR in valvular heart disease Dr. Saul Myerson Clinical Lecturer in Cardiovascular Medicine For www. scmr. org 02/2007 This presentation posted for members of scmr as an educational guide – it represents the views and practices of the author, and not necessarily those of SCMR. University of Oxford Centre for Clinical Magnetic Resonance Research (OCMR)
Advantages of CMR • All areas of the body accessible - free choice of imaging planes with no ‘hidden’ sections • Range of imaging techniques – anatomical, cine, angiography, flow • Quantification of flow and thus valve lesion severity • 3 D imaging with angiography • No ionising radiation • Other techniques (Echo) do have strengths, esp. in the acute setting © Saul Myerson 2007
Standard imaging for all studies • Long axis planes – HLA, VLA, LVOT coronal, (RVOT +/- RV inflow if right -sided lesions) • Need two perpendicular views of the valve(s) in question • LV & RV function © Saul Myerson 2007
LV and RV function This is important for assessing the impact of the valve lesion on the LV / RV and should be performed in all cases See How I do a CMR volume study by James Moon, here âGold standard accuracy for volumes, mass & function © Saul Myerson 2007
Specific valve lesions - overview • Aortic valve disease • Mitral valve disease • Pulmonary stenosis & regurgitation • Tricuspid regurgitation • Complex lesions – Mixed stenosis/regurgitation – Multiple valves © Saul Myerson 2007
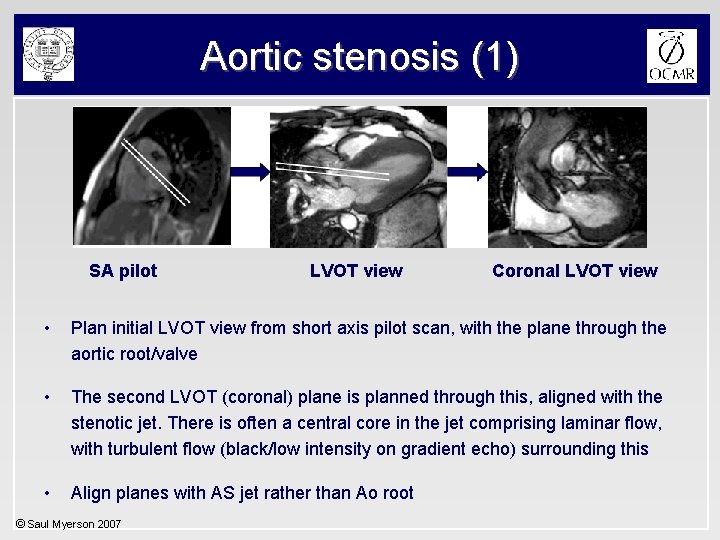
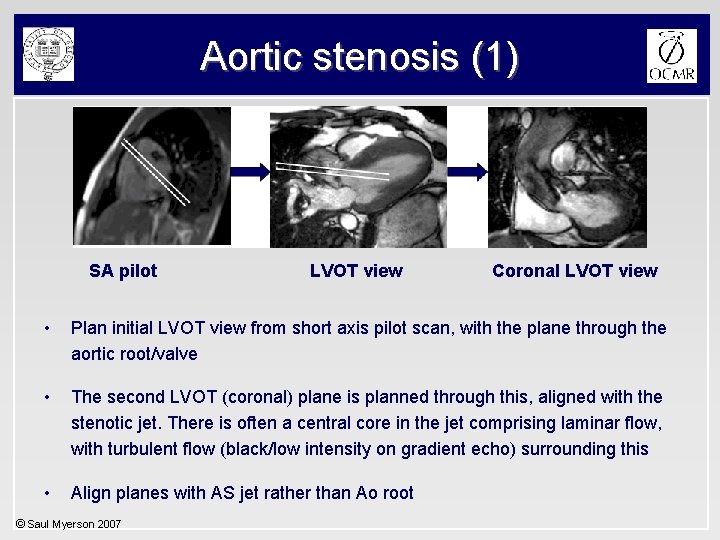
Aortic stenosis (1) SA pilot LVOT view Coronal LVOT view • Plan initial LVOT view from short axis pilot scan, with the plane through the aortic root/valve • The second LVOT (coronal) plane is planned through this, aligned with the stenotic jet. There is often a central core in the jet comprising laminar flow, with turbulent flow (black/low intensity on gradient echo) surrounding this • Align planes with AS jet rather than Ao root © Saul Myerson 2007
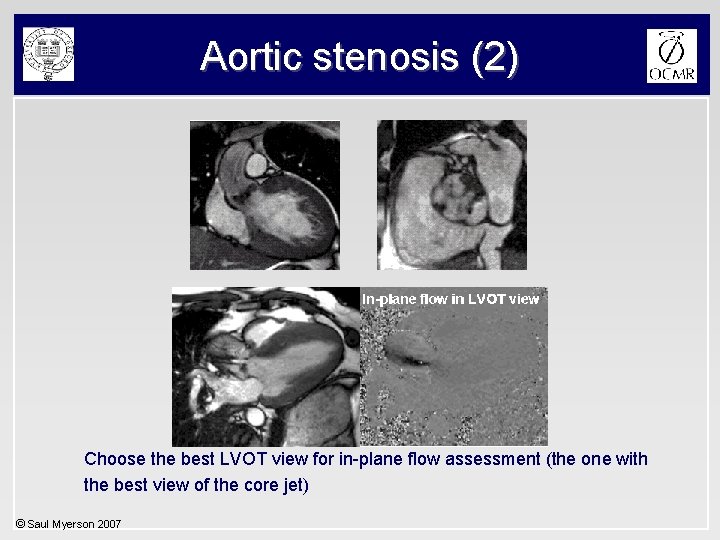
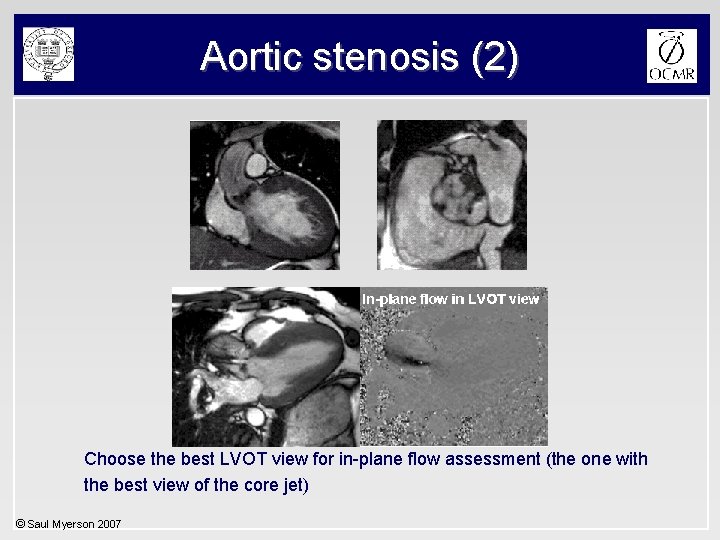
Aortic stenosis (2) Choose the best LVOT view for in-plane flow assessment (the one with the best view of the core jet) © Saul Myerson 2007
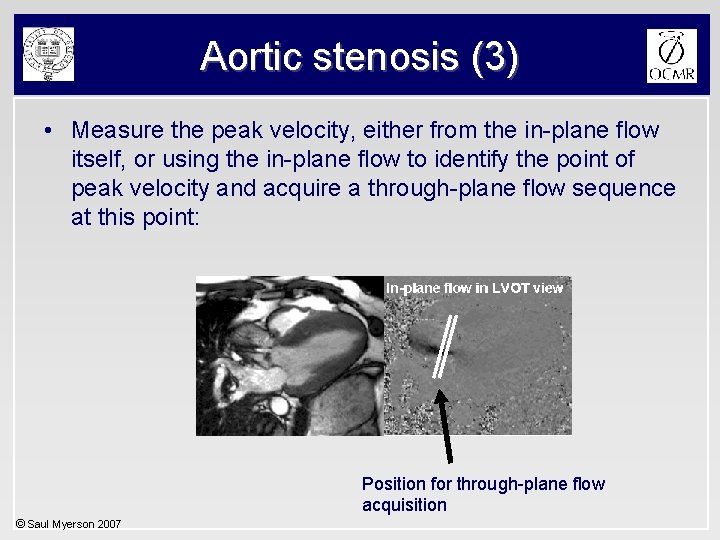
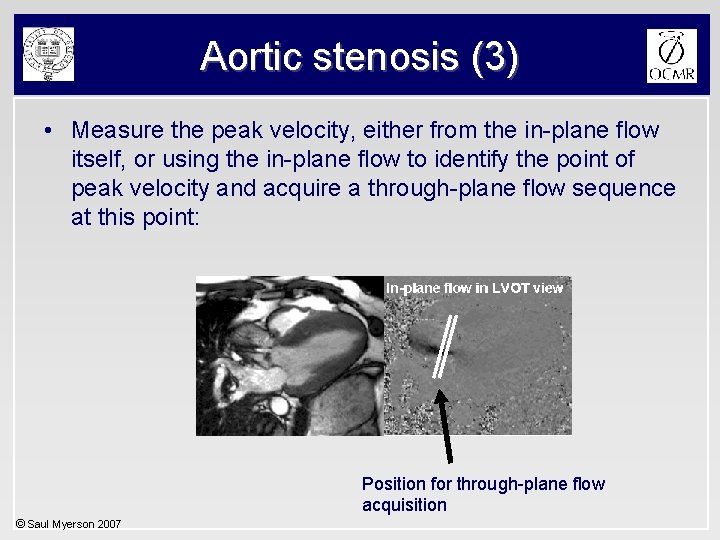
Aortic stenosis (3) • Measure the peak velocity, either from the in-plane flow itself, or using the in-plane flow to identify the point of peak velocity and acquire a through-plane flow sequence at this point: Position for through-plane flow acquisition © Saul Myerson 2007
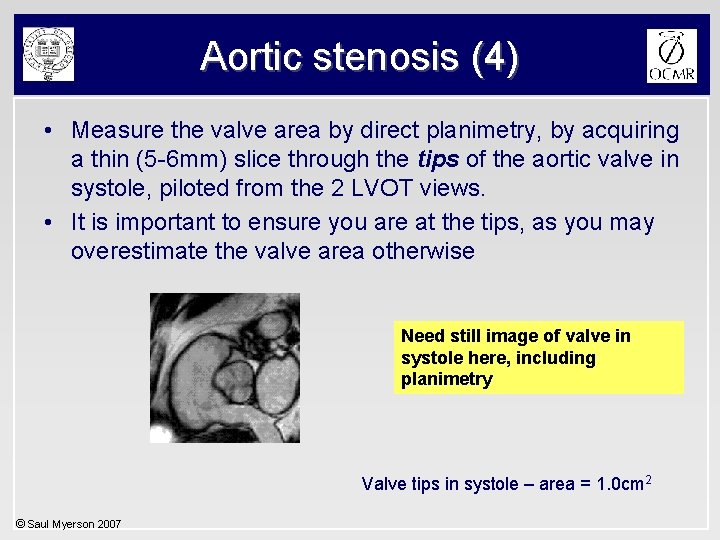
Aortic stenosis (4) • Measure the valve area by direct planimetry, by acquiring a thin (5 -6 mm) slice through the tips of the aortic valve in systole, piloted from the 2 LVOT views. • It is important to ensure you are at the tips, as you may overestimate the valve area otherwise Need still image of valve in systole here, including planimetry Valve tips in systole – area = 1. 0 cm 2 © Saul Myerson 2007
Aortic stenosis (5) Advantages of CMR: • Correct alignment with AS jet – Accurate trans-valvular velocity (in-plane / through plane) – avoids underestimation with angulated roots • Valve orifice area (direct planimetry) • LV mass & volumes to assess impact on LV © Saul Myerson 2007
Aortic regurgitation • Through-plane flow measurement • Allows quantification of regurgitation © Saul Myerson 2007
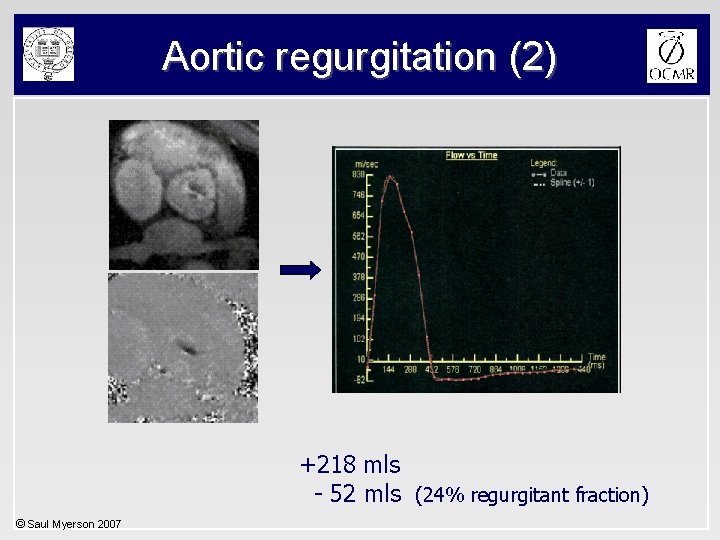
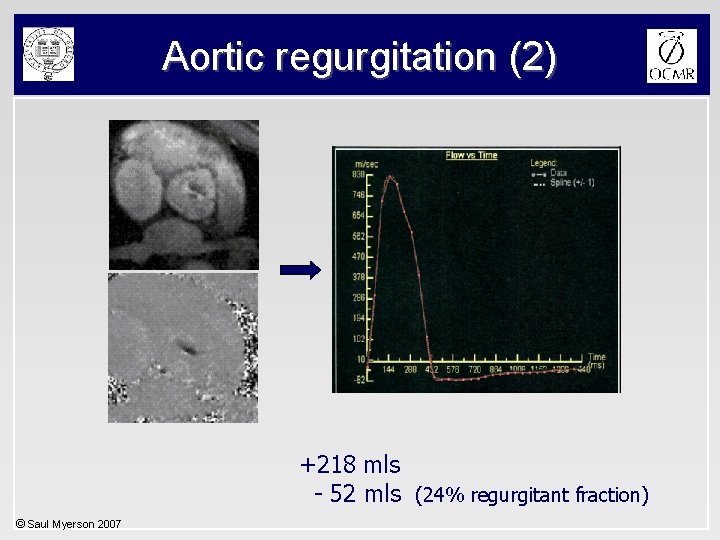
Aortic regurgitation (2) +218 mls - 52 mls (24% regurgitant fraction) © Saul Myerson 2007
Aortic regurgitation (3) • Quantification allows more accurate assessment of severity (echo parameters less precise) • More detail required on how quantification fits into clinical practice © Saul Myerson 2007
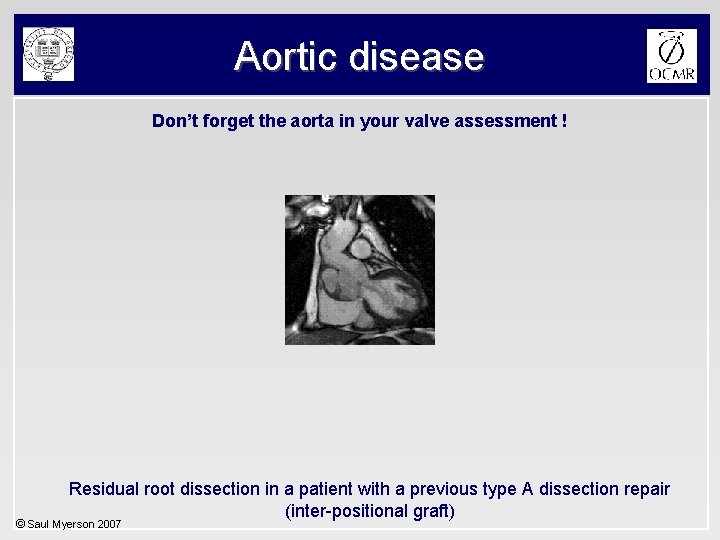
Aortic disease Don’t forget the aorta in your valve assessment ! Residual root dissection in a patient with a previous type A dissection repair (inter-positional graft) © Saul Myerson 2007

Mitral regurgitation Standard methods of quantification are indirect: 1) Regurgitant flow = LVSV - Ao systolic flow (independent of other valve lesions) 2) Regurgitant flow = LVSV - RVSV © Saul Myerson 2007
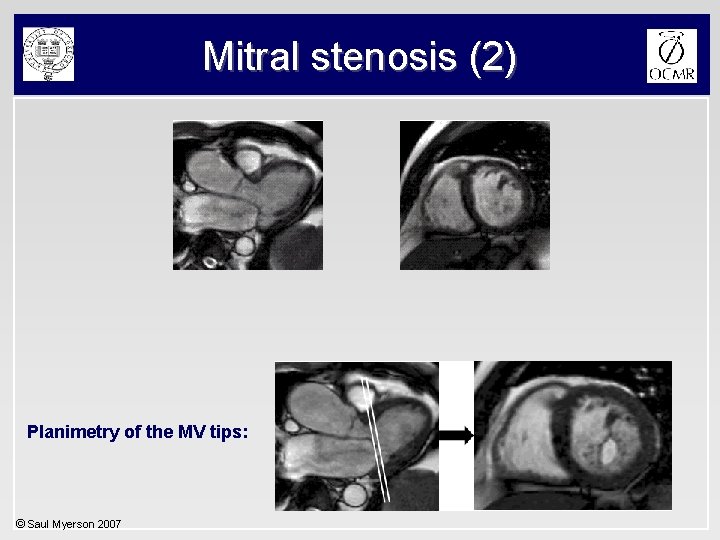
Mitral stenosis • Can assess mitral valve area by direct planimetry • Important to ensure correct slice positioning at MV tips (as for echo) • Diastolic flow (volume and velocity) is feasible though temporal resolution is lower than echo © Saul Myerson 2007
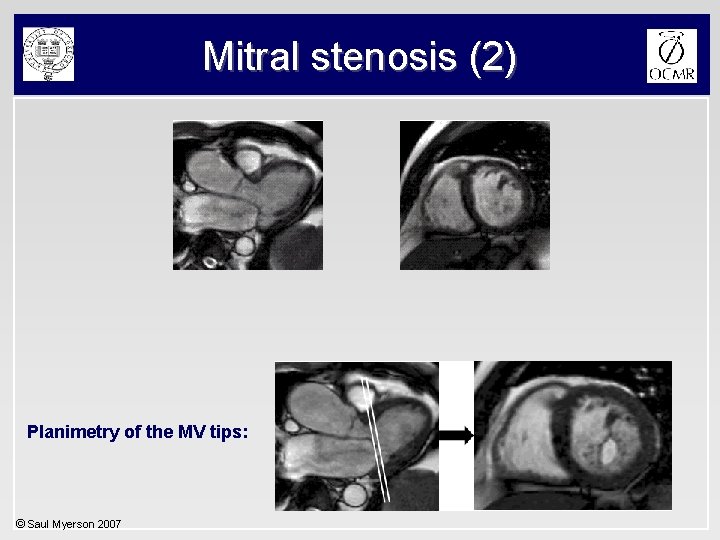
Mitral stenosis (2) Planimetry of the MV tips: © Saul Myerson 2007
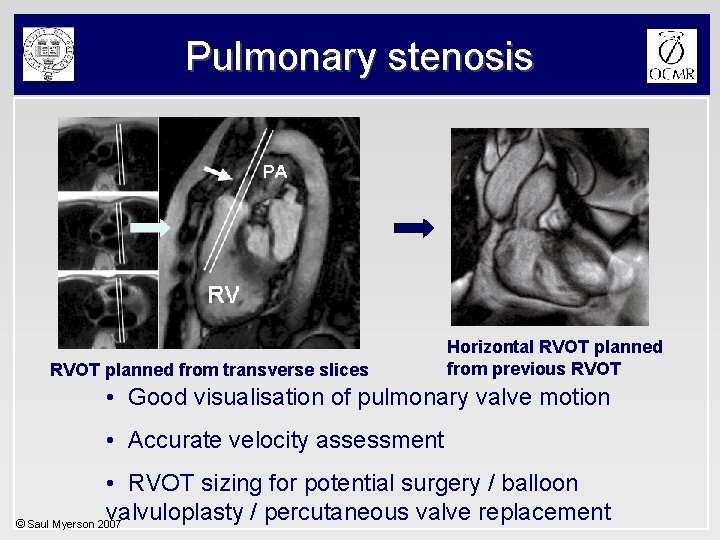
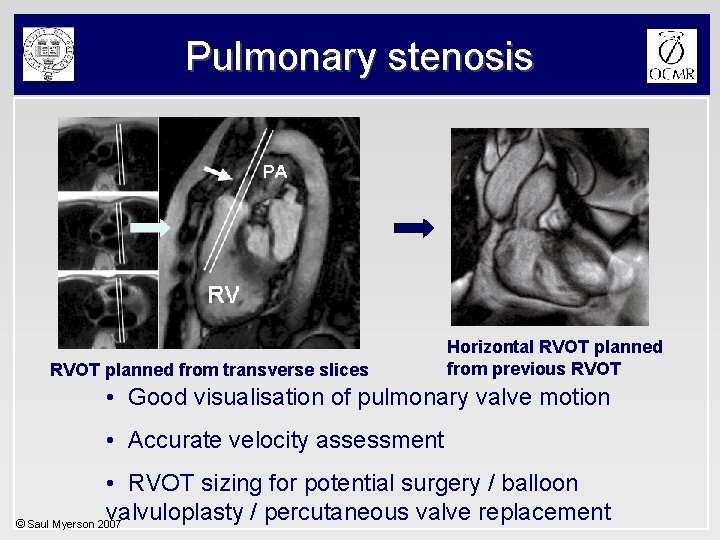
Pulmonary stenosis RVOT planned from transverse slices Horizontal RVOT planned from previous RVOT • Good visualisation of pulmonary valve motion • Accurate velocity assessment • RVOT sizing for potential surgery / balloon valvuloplasty / percutaneous valve replacement © Saul Myerson 2007
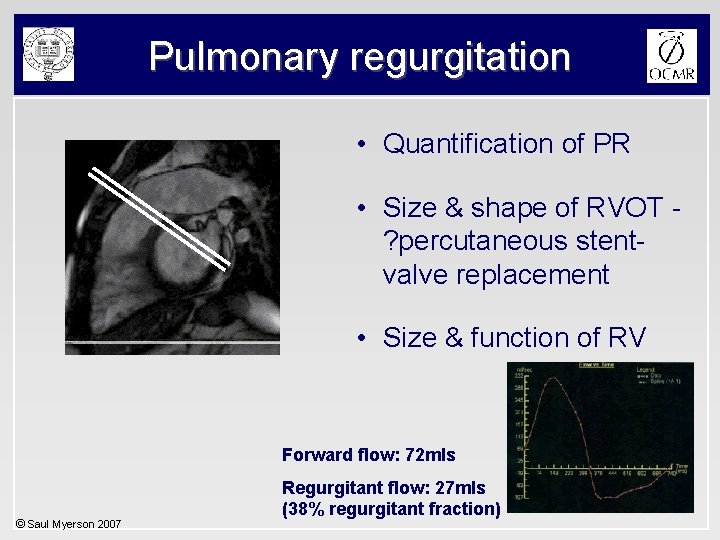
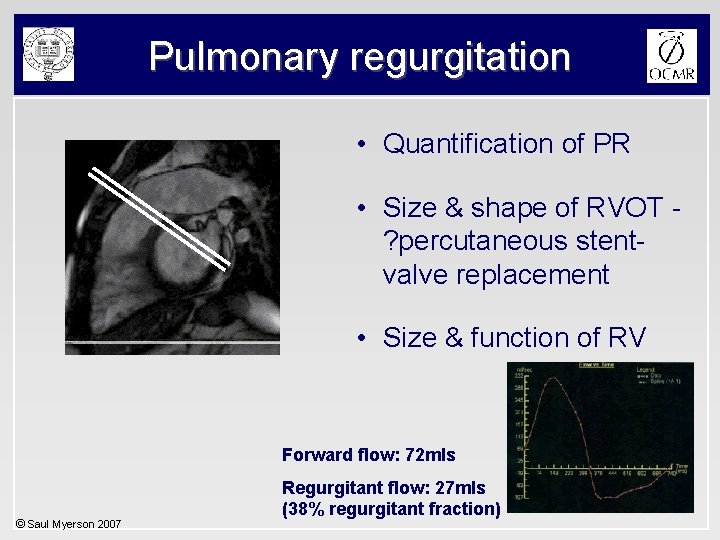
Pulmonary regurgitation • Quantification of PR • Size & shape of RVOT ? percutaneous stentvalve replacement • Size & function of RV Forward flow: 72 mls © Saul Myerson 2007 Regurgitant flow: 27 mls (38% regurgitant fraction)
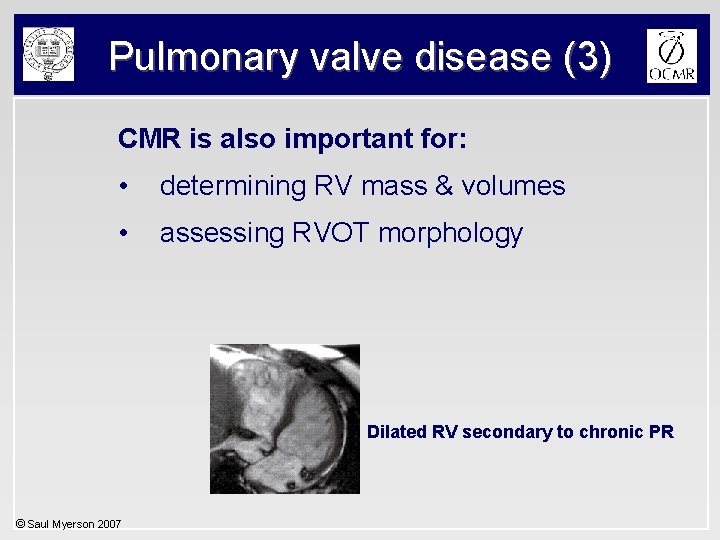
Pulmonary valve disease (3) CMR is also important for: • determining RV mass & volumes • assessing RVOT morphology Dilated RV secondary to chronic PR © Saul Myerson 2007
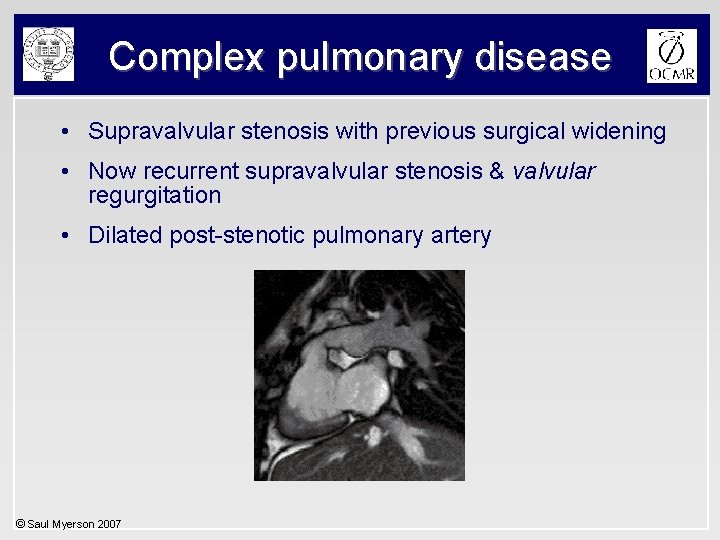
Complex pulmonary disease • Supravalvular stenosis with previous surgical widening • Now recurrent supravalvular stenosis & valvular regurgitation • Dilated post-stenotic pulmonary artery © Saul Myerson 2007
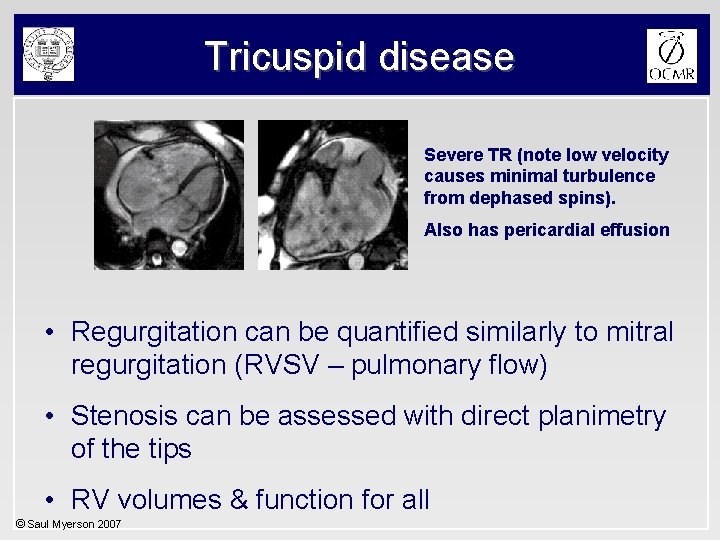
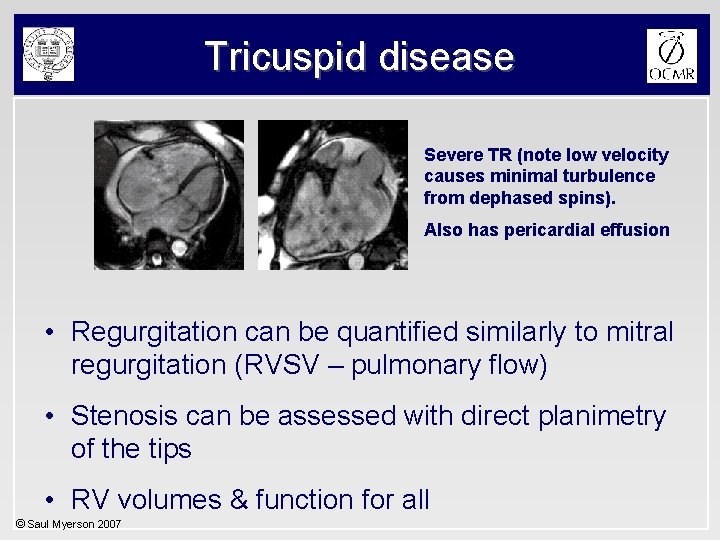
Tricuspid disease Severe TR (note low velocity causes minimal turbulence from dephased spins). Also has pericardial effusion • Regurgitation can be quantified similarly to mitral regurgitation (RVSV – pulmonary flow) • Stenosis can be assessed with direct planimetry of the tips • RV volumes & function for all © Saul Myerson 2007
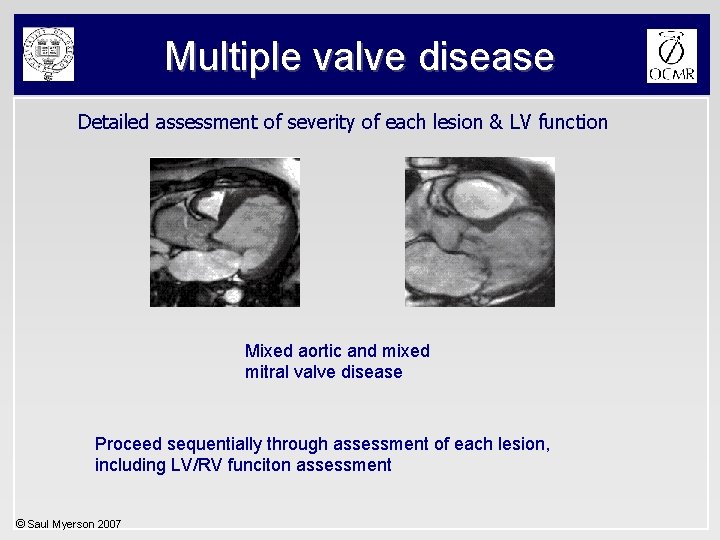
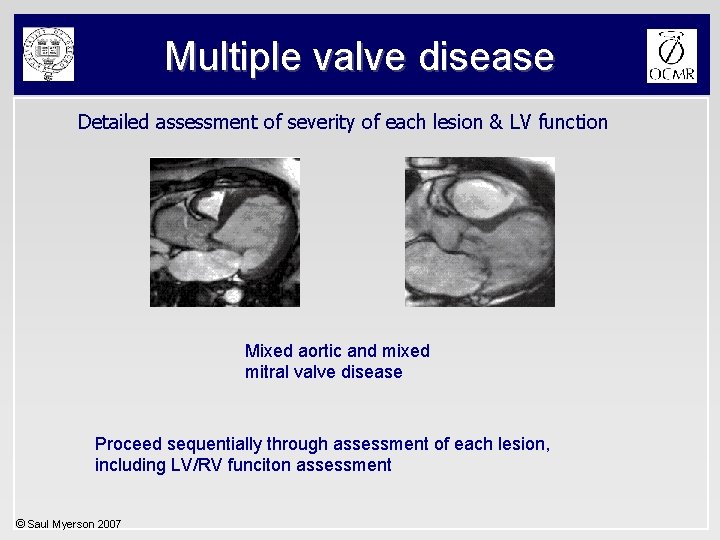
Multiple valve disease Detailed assessment of severity of each lesion & LV function Mixed aortic and mixed mitral valve disease Proceed sequentially through assessment of each lesion, including LV/RV funciton assessment © Saul Myerson 2007