How I do CMR in HCM Dr Sanjay
- Slides: 23
‘How I do’ CMR in HCM Dr Sanjay Prasad, Royal Brompton Hospital London, UK. For SCMR August 2006 This presentation is posted for members of scmr as an educational guide – it represents the views and practices of the author, and not necessarily those of SCMR. s. prasad@rbht. nhs. uk
Hypertrophic Cardiomyopathy ‘How I do’ : CMR in HCM
Hypertrophic Cardiomyopathy: Clinical Aspects n n n Characterized by myocyte disarray, hypertrophy, and interstitial fibrosis 90% of pts have familial disease 10% de novo mutations Increased risk of SCD Adult prevalence 1: 500 (Autosomal Dominant) 1 st degree-relatives -1: 2 risk gene carrier ‘How I do’ : CMR in HCM
HCM: Diagnosis n n n Unexplained hypertrophy Measured wall thickness exceeds 2 SD for gender-, age-, and BSA-matched populations ≥ 1. 5 cm in absence of a recognized cause There may be associated systolic anterior motion of the mitral valve leaflets and outflow tract obstruction Multiple causative mutations in at least 10 different sarcomeric proteins Variable phenotype and clinical outcome Seidman et al 2002; Chien 2003 ‘How I do’ : CMR in HCM
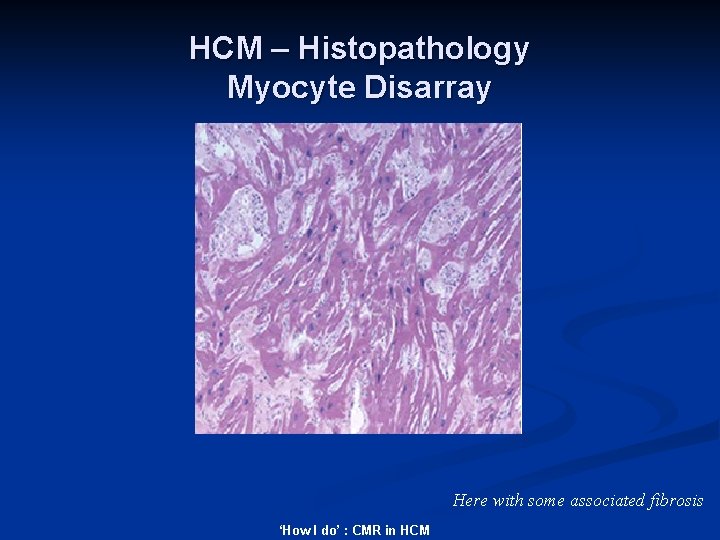
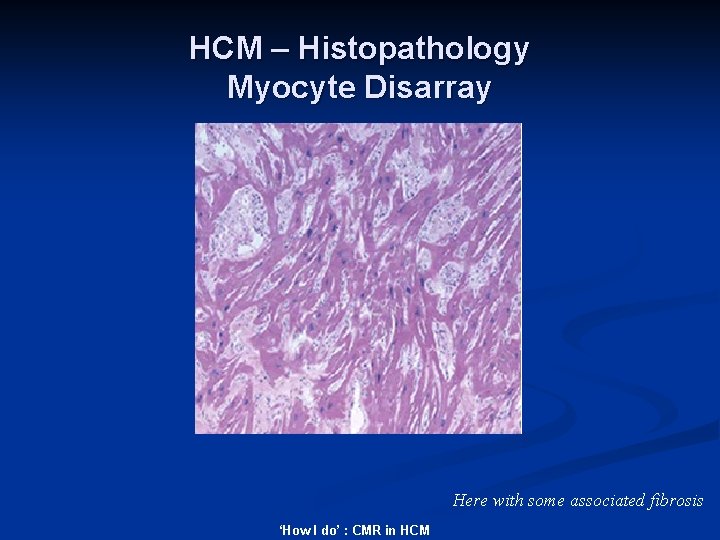
HCM – Histopathology Myocyte Disarray Here with some associated fibrosis ‘How I do’ : CMR in HCM
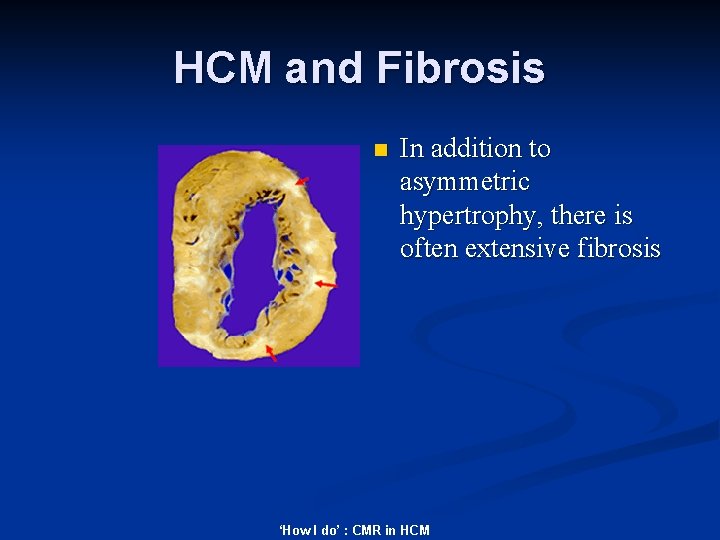
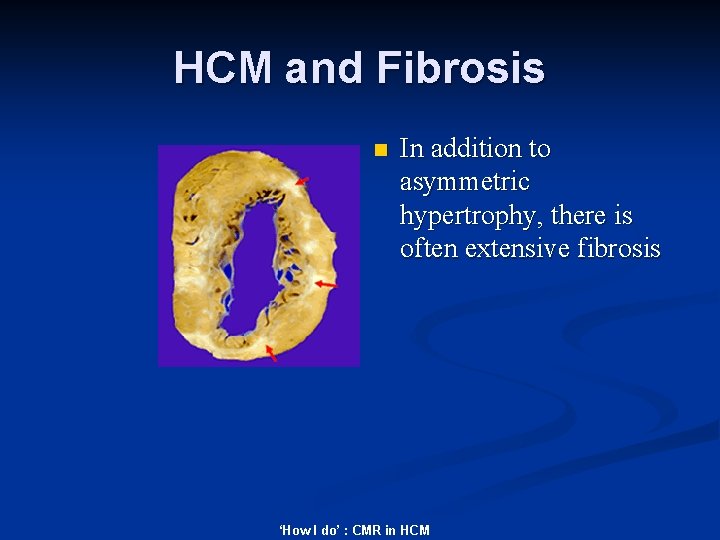
HCM and Fibrosis n In addition to asymmetric hypertrophy, there is often extensive fibrosis ‘How I do’ : CMR in HCM
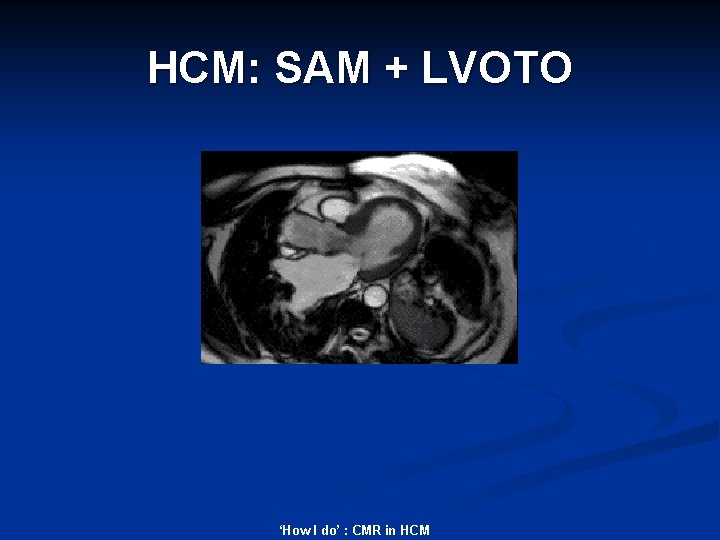
HCM: SAM + LVOTO ‘How I do’ : CMR in HCM
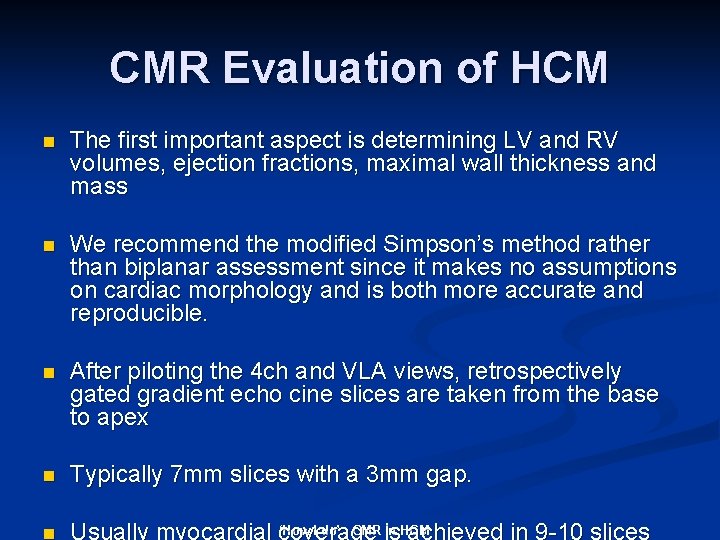
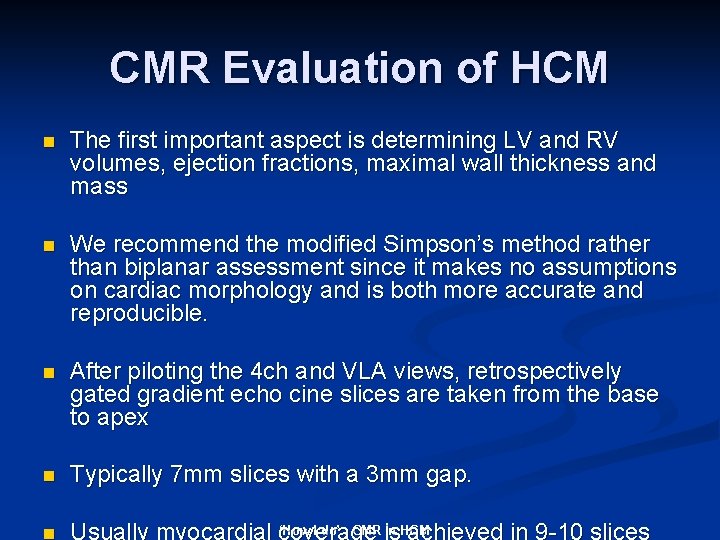
CMR Evaluation of HCM n The first important aspect is determining LV and RV volumes, ejection fractions, maximal wall thickness and mass n We recommend the modified Simpson’s method rather than biplanar assessment since it makes no assumptions on cardiac morphology and is both more accurate and reproducible. n After piloting the 4 ch and VLA views, retrospectively gated gradient echo cine slices are taken from the base to apex n Typically 7 mm slices with a 3 mm gap. n ‘How I do’ : CMR is in HCM Usually myocardial coverage achieved in 9 -10 slices
CMR Quantification See the presentation ‘how I do’ LV volumes Downloadable from www. scmr. org ‘How I do’ : CMR in HCM
HCM: Cine Imaging n The key questions to address are: - 1. Presence, distribution, and severity of LVH and RVH. LV/RV mass and wall thickness 2. Extent of septal involvement 3. Distribution of hypertrophy in the variant forms of hypertrophic cardiomyopathy ‘How I do’ : CMR in HCM
Functional Assessment n n Cine images are then acquired to determine if there is SAM and LVOTO. SSFP images with retrospective gating recommended ‘How I do’ : CMR in HCM
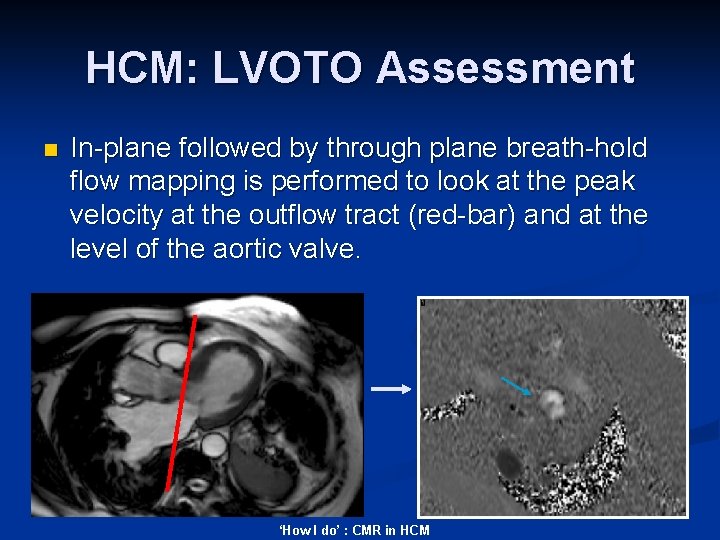
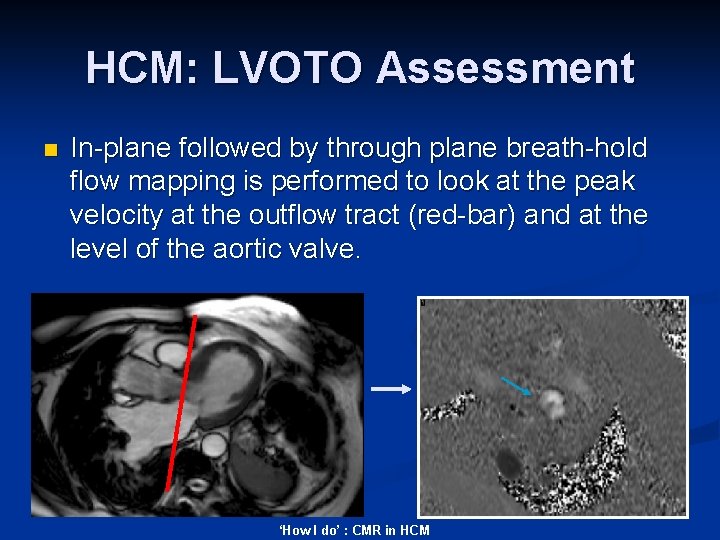
HCM: LVOTO Assessment n In-plane followed by through plane breath-hold flow mapping is performed to look at the peak velocity at the outflow tract (red-bar) and at the level of the aortic valve. ‘How I do’ : CMR in HCM
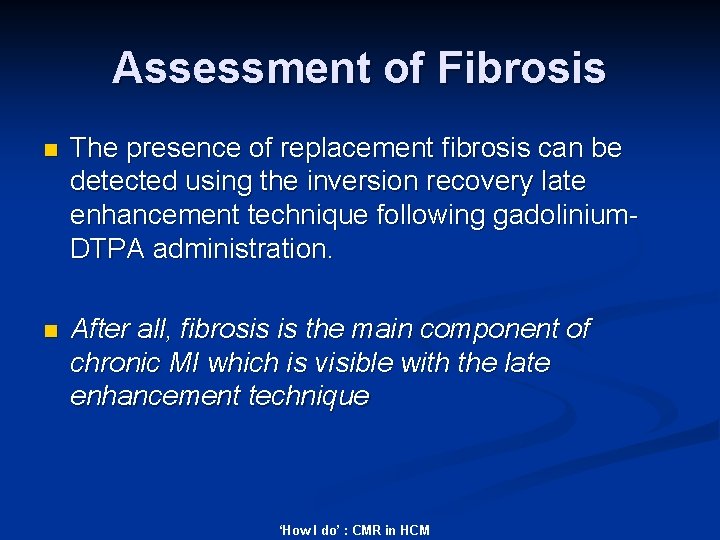
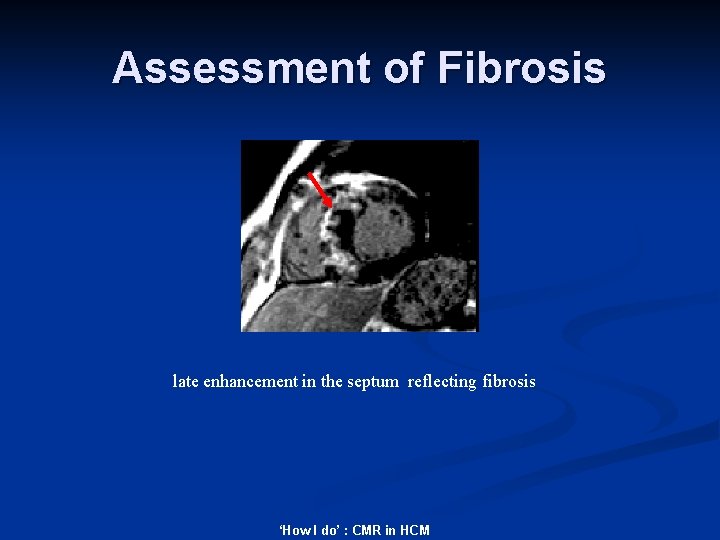
Assessment of Fibrosis n The presence of replacement fibrosis can be detected using the inversion recovery late enhancement technique following gadolinium. DTPA administration. n After all, fibrosis is the main component of chronic MI which is visible with the late enhancement technique ‘How I do’ : CMR in HCM
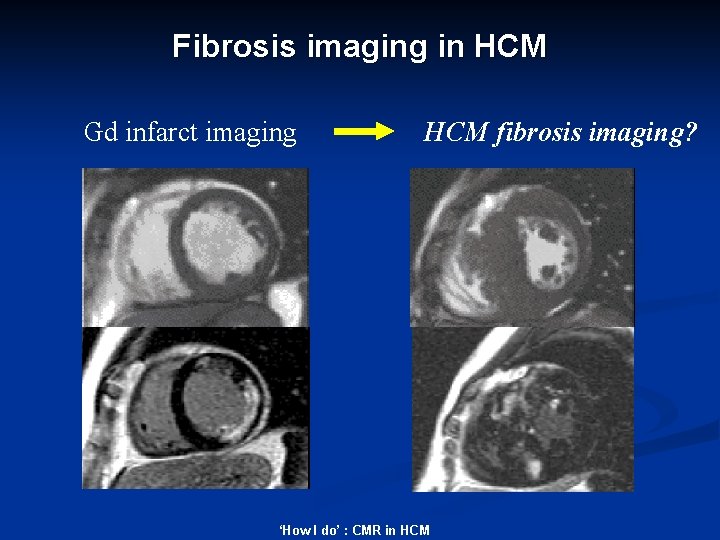
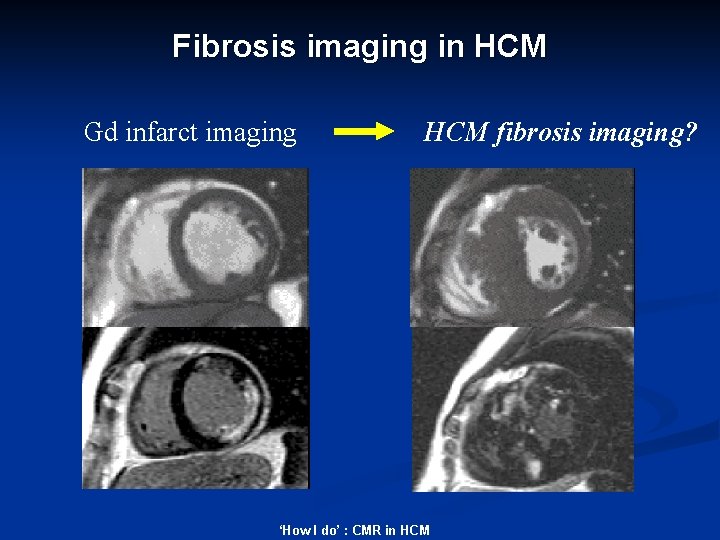
Fibrosis imaging in HCM Gd infarct imaging HCM fibrosis imaging? ‘How I do’ : CMR in HCM
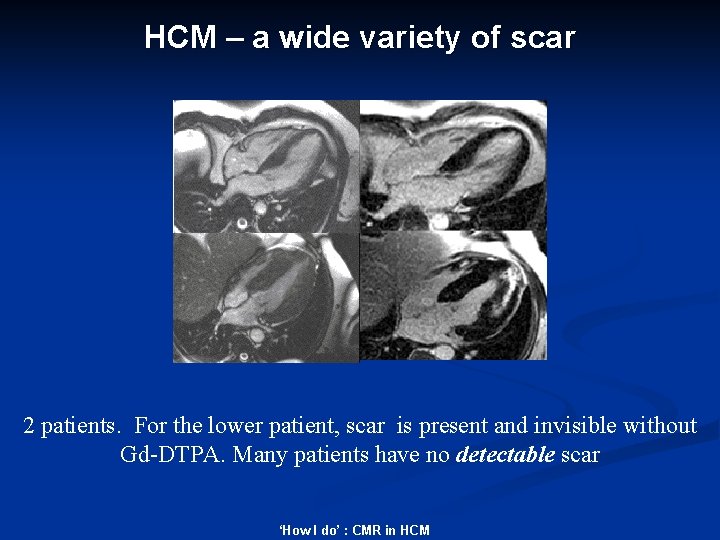
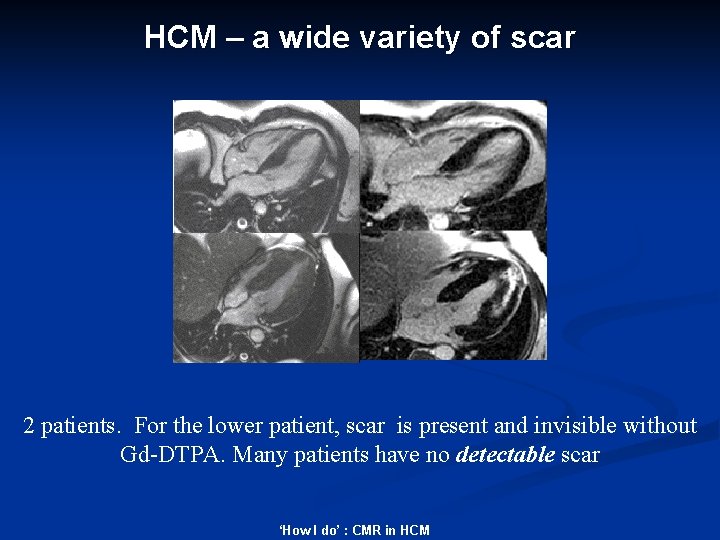
HCM – a wide variety of scar 2 patients. For the lower patient, scar is present and invisible without Gd-DTPA. Many patients have no detectable scar ‘How I do’ : CMR in HCM
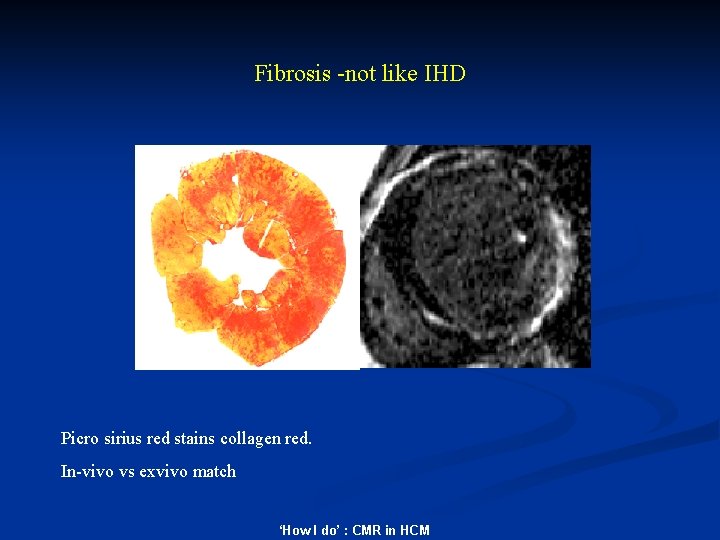
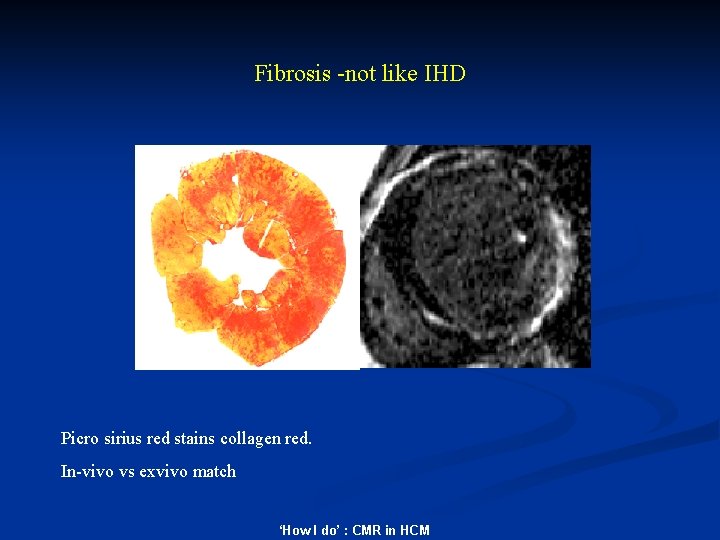
Fibrosis -not like IHD Picro sirius red stains collagen red. In-vivo vs exvivo match ‘How I do’ : CMR in HCM
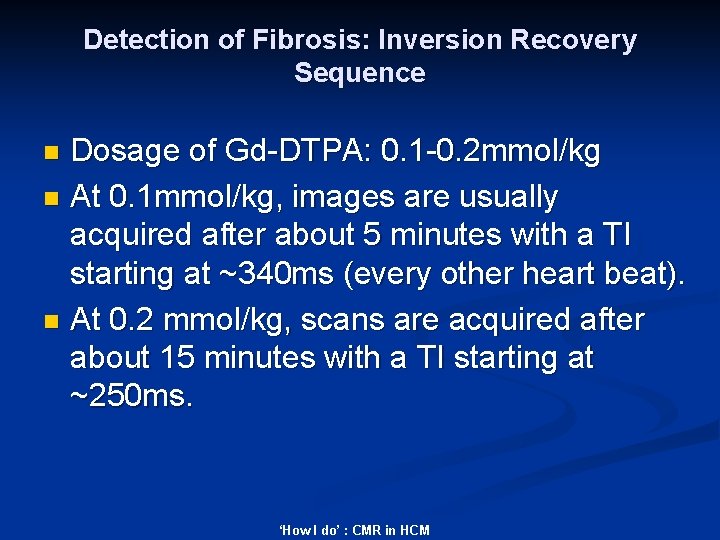
Detection of Fibrosis: Inversion Recovery Sequence Dosage of Gd-DTPA: 0. 1 -0. 2 mmol/kg n At 0. 1 mmol/kg, images are usually acquired after about 5 minutes with a TI starting at ~340 ms (every other heart beat). n At 0. 2 mmol/kg, scans are acquired after about 15 minutes with a TI starting at ~250 ms. n ‘How I do’ : CMR in HCM
HCM: Detection of Fibrosis n LGE is predominantly seen in a patchy distribution and correlates with wall thickness. n Unlike in IHD, the subendocardium is not necessarily affected. Unlike DCM, the distribution is typically more diffuse and not specific to mid-wall circumferential fibres. n ‘How I do’ : CMR in HCM
Detection of Fibrosis: Inversion Recovery Sequence n Tips to confirm fibrosis and not artefact: 1. Phase swap each slice 2. If mid-wall enhancement is seen, ensure TI is optimal and if need be, repeat the slice with a different TI 3. Cross-cut through any areas of suspected mid-wall enhancement 4. If subendocardial enhancement is seen, reconsider the diagnosis or assess if this reflects ‘bystander’ coronary disease 5. It is common to see some fibrosis around the LVOT ‘How I do’insertion : CMR in HCM points and at the RV/LV septal
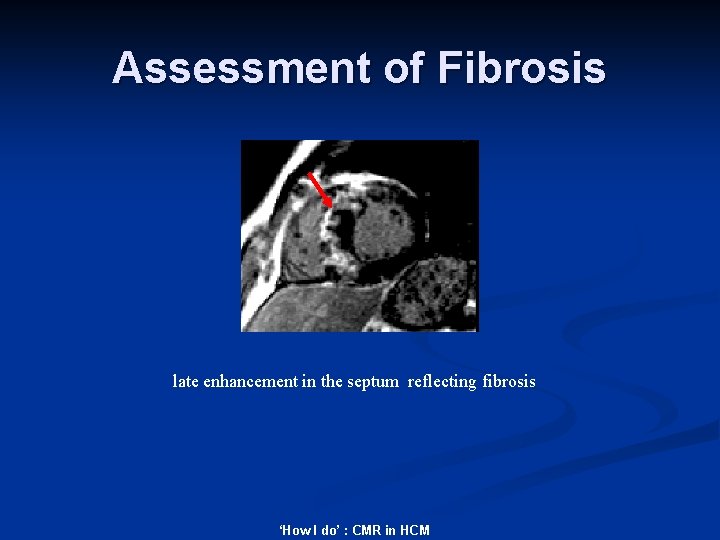
Assessment of Fibrosis late enhancement in the septum reflecting fibrosis ‘How I do’ : CMR in HCM
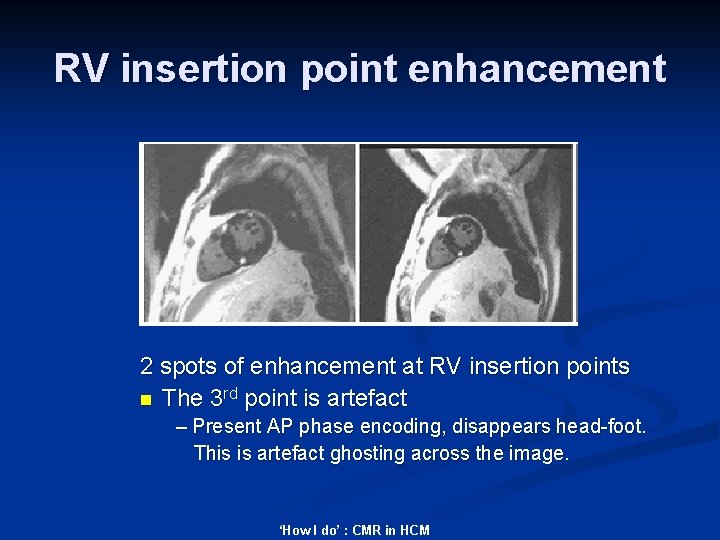
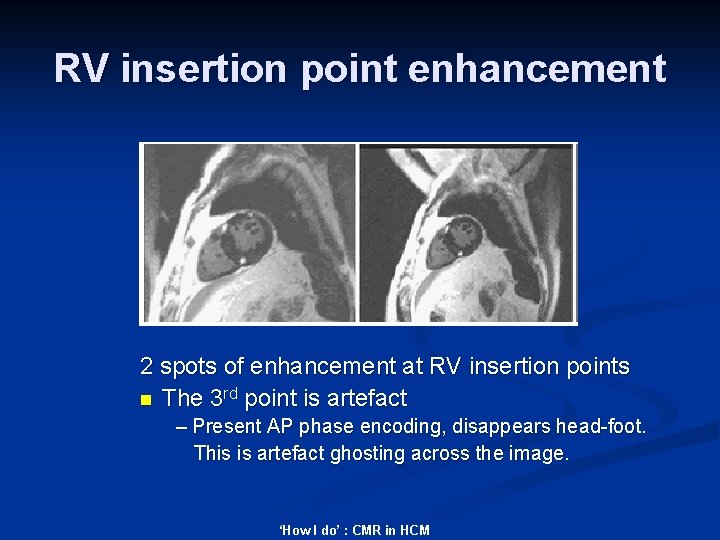
RV insertion point enhancement 2 spots of enhancement at RV insertion points n The 3 rd point is artefact – Present AP phase encoding, disappears head-foot. This is artefact ghosting across the image. ‘How I do’ : CMR in HCM
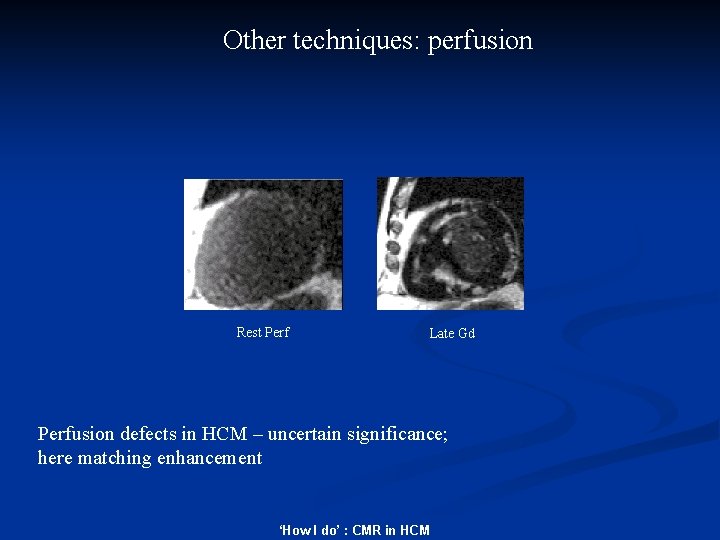
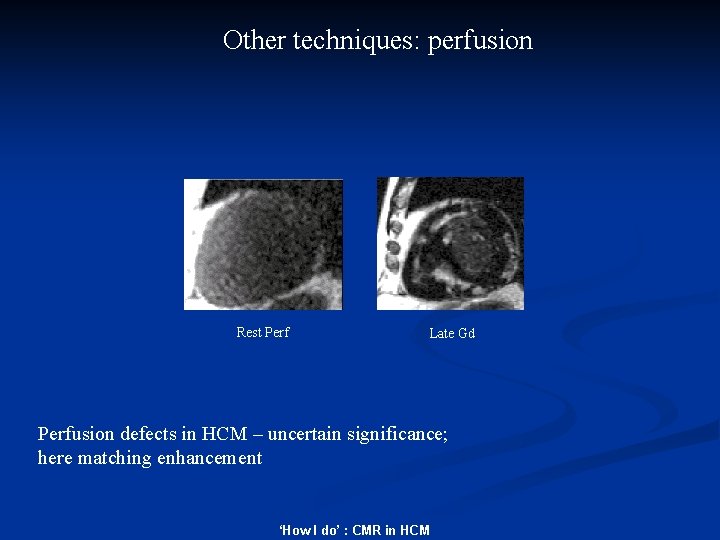
Other techniques: perfusion Rest Perf Late Gd Perfusion defects in HCM – uncertain significance; here matching enhancement ‘How I do’ : CMR in HCM
Summary n n n Evaluate function, volumes, maximal wall thickness, distribution of hypertrophy and overall mass index. Flow mapping to assess LVOTO Presence of fibrosis important using inversionrecovery Gd-DTPA s. prasad@rbht. nhs. uk ‘How I do’ : CMR in HCM