Hospital Acquired Infections and Infection control Infection control






- Slides: 55

Hospital Acquired Infections and Infection control
Infection control model • Source • Infection • Mode of transfer and entry • Susceptible host

Importance of HAI • Prevalence 15% • Majority are highly Virulent and cause death & disability • Needs expensive antibiotics to treat • Longer hospital stay • Cost to the hospital and patient Guidelines for control is essential
Causes • • Poor infection control activities Extensive use of antibiotics Mutations Changes in the host
Infection Control programme 1. Planning 2. Implementation 3. Feed back and evaluation
1. Planning • Situational Analysis – Collection of Data • Monthly infection Rates - Disease surveillance reports • Inquiry Reports – Out break , PM • Antibiotic usage pattern • ICN visit Reports – Identify Units with higher infection rates

Planning …. . – Process analysis • • • Infrastructure & standards Procedures Staff Equipments Suppliers Patients & Visitors

Planning – Develop Policies • Protocols for best infection control practices • Align them to Staff Performance indicators – Awareness programme • Policies • Protocols • Training Programmes – Infection control committee
Implementation • Infection control committee – Director, Microbiologist, ICN, Pharmacists , Consultants specialist • Monthly meetings • Outbreak Investigations
Implementation • Continues control 1. 2. 3. 4. 5. Infrastructure Water Kitchen HDU’s Cleaning 6. Waste Management 7. Staff 8. Suppliers 9. Laundry 10. Training
1. Infrastructure & Layouts • Air – Filters – Humidity – Temperature – Fresh air – Ventilation • Bottle necks in the Layout promoting infections
2. Water • • Chlorinated water Boiled cooled water Policy on home cooked meals / water Facilities for Hand washing
3. Kitchen • • Supplies Cleaning Cooking and its layout Storing Staff hygiene Utensils Drainage
4. Cleaning of the units • Simple detergent is enough not an antiseptic – 90 % of infections are washable – Antiseptics use only in an Out break • General units – Daily mopping – Weekly washing – Special washing - emergency – spills • Special units – Mopping after each procedure – Daily washing – Weekly cleaning • Equipments – Daily cleaning with a detergent – Special cleaning
Staff • Selected swabs – special units – Out breaks • Personnel Hygiene • Hand washing , hand washing ……. .
Universal precautions – Low risk – Injection - Gloves – Moderate Risk – IV Canula – Gloves, Apron – High risk –Vaginal delivery Mask, Cap, eye protectors Gloves, Apron
Standard Precautions 1. Hand washing 2. Use of Gloves 3. Personal Protective Equipment (PPE)
1. Hand Washing • Hand washing is the single most effective method of preventing cross infection. • All clinical staff should wash hands and forearms before : – Before and after examination of patients – Before any invasive procedure, before wearing sterile gloves – When contaminated with blood, body fluids, secretions, contaminated items – Wash hands immediately after removing gloves – Wash hands between contact with “dirty’ and ‘clean’ sites on the same patient
1. Hand Washing • Hands should be washed using soap and water. • Alcohol based hand rubs could be used if hands are not visibly soiled. • All clinical, paramedical, house keeping, kitchen and janitorial staff should keep their nails cut short and clean at all times. • Clinical staff should remove rings, bangles, bracelets, watches and should roll up sleeves before any invasive procedure.
2. Use of Gloves • Gloves should be worn when indicated to prevent the contamination of hands with microorganisms. • Gloves are not a substitute for hand washing. Precautions when using gloves include: – Clean gloves should be worn when handling blood, body fluids, secretions or excretions and contaminated items – When touching mucous membranes and non intact skin – Change gloves between contact with “dirty” and “clean” sites on the same patient – Used gloves should be promptly removed and discarded as clinical waste. – Hands should be washed immediately after removing gloves.
3. Personal Protective Equipment (PPE) • PPE provides a protective physical barrier to reduce the contamination of clothes, skin and mucous membranes like eyes, nose and mouth. • PPE includes gloves, mask, gowns, aprons, goggles, face shields, boots, caps etc. • The appropriate PPE should be chosen by the staff according to the risk of exposure
4. Patient care Equipment • Infections could be transmitted indirectly through contaminated equipments. • All reusable patient care equipment should be adequately cleaned or sterilized before using on another patient. • All disposable items should be discarded properly and never re used.
5. Environmental control • Environment should be visibly clean and should be free from dust and dirt. • The house keeping staff should ensure routine care, cleaning and disinfection of environment, surfaces, bed rails, bedside equipment and other frequently touched surfaces. • Wet cleaning and damp dusting is preferred to prevent airborne infections from the surfaces.
Environment…. • Regular cleaning using a general purpose detergent for cleaning of surfaces would be sufficient. • Use different cleaning equipment for cleaning of clinical areas, toilets and kitchen • Dishes, glasses, cups and cooking utensils could be washed with soap and water • Adequate ventilation in order to maintain positive air pressure for high risk areas and negative air pressure into contaminated areas. Ultra clean air should be available with uni directional laminar flow in theatres and other high dependency units.
Environment…. • Safe drinking water should be available to staff as well as for patients and visitors. The overhead storage tank should be cleaned regularly and the quality of the water should be checked by inspecting samples for faecal contamination. • In appropriate food handling in the kitchen as well as while serving food can contaminate the food items served to patients and staff. This could be minimized by purchasing supplies from reliable sources, proper storage of items, kitchen hygiene and by using appropriate cooking methods. • All food handlers should wash their hands before preparing and serving food. They should be visibly clean with clean uniforms, covered hair and trimmed finger nails. • Visitors would be discouraged from bringing food from out side into the hospital for hygienic reasons.
Management of spills Blood and body fluids 1. Heavy duty gloves should be worn. 2. Soak up the fluid using absorbent material like gauze, paper towel or wadding 3. Pour 1% hypochlorite solution till it is well soaked and leave for 10 minutes. 4. Remove with an absorbent material and discard as clinical waste. 5. Clean the area with detergent and water and allow to dry. 6. Discard used gloves as clinical waste 7. Wash hands. 8. Low risk body fluids and excreta like faeces, vomitus and urine
Linen • Linen should changed on discharge of a patient or if it becomes soiled. • Every patient should be given clean bed linen. • Soiled linen should be handled, transported and processed in a manner that prevents contamination of skin and mucous membranes of handlers. • The blood and body fluid stained linen and linen from isolated patients should be washed with hot water (71 degrees) using detergent. • Alternatively, they could be soaked in 0. 5% hypochlorite solution for 30 minutes before sending to the laundry.
Safety of Healthcare workers a. Pre recruitment evaluation b. Immunization of staff c. Personal Restrictions
a. Pre recruitment evaluation • it is advisable to carry out a personal health evaluation of staff members prior to their placement on duty. In this evaluation the following aspects should be included. – Past medical history of the individual – History of any condition that makes the person vulnerable to infectious diseases (e. g corticosteroid therapy) – Immunization history – Complete physical examination and laboratory investigations (FBC and ESR, UFR, RBS, +/- chest x ray)
b. Immunization of staff – • All clinical, paramedical, house keeping and janitorial staff should be immunized against Hepatitis B. Immunization programmes should be periodically carried out to include the newly recruited staff as well. In addition to Hepatitis B, the following vaccines are recommended if the individual has not been immunized against them before. • Measles, Mumps, Rubella, Varicella (MMR and Chicken Pox vaccines), Tuberculosis(BCG), Tetanus, Diphtheria • Post exposure prophylaxis is recommended in certain conditions like Diphtheria, whooping cough and meningococcal infections
c. Personal Restrictions • All hospital staff members are encouraged to inform ASAP when ever they have a potentially transmissible infections through the HOD’s. The respective HOD should take immediate measures to relieve duty of an affected staff member and to restrict work involving patients as well as to minimize the contact with the other staff members. The staff member affected should be provided with guidance to seek treatment and to obtain clearance for work from a relevant specialist consultant of Hemas Hospital after such an illness that needed work restriction. It is the duty of all HOD’s to educate and encourage their staff to report their condition considering the impact on infection control within the hospital.
d. Handling of sharps • Clean gloves should be used during phlebotomy to reduce contamination of hands with blood. • Discard used sharps directly into a “sharps bin” located as close as practical to the area it is being used. The sharps bin should be emptied when it is ¾ full by incinerating and later burying the residual. • Do not attempt to bend, remove, recap, break or otherwise manipulate needles by hand • Sharps such as scalpels, lancets, IV needles and syringes should be disposable and single use only. • Avoid recapping of needles. Always carry sharps in a suitable tray when moving from a place or when ever passing to another staff member. • The reusable glass syringes and special needles should be transported in puncture proof containers to be decontaminated at CSSD.
e. Prevention of mucous membrane exposures • Use appropriate PPE when ever patient care activities are likely to generate splashes or sprays of blood, body fluids, secretions and excretions. • Use mouth pieces, ventilation devices during resuscitation methods when ever possible.
f. Management of accidental Exposures to blood and body fluids – • Accidental sharp injuries and exposure to blood and body fluids may expose an individual to blood borne viruses like Hepatitis B, Hepatitis C and HIV. The risks can be minimized by safe practices, adhering to infection control measures and standard precautions. • If accidentally exposed:
f. Management of accidental Exposures to blood and body fluids – • If accidentally exposed: – the wound should be washed well with soap and water – Identify the source and the medical history of the individual – Collect 5 ml of blood from the source for Hep B, HCV and HIV serology with their consent. – Take 5 ml of blood for Hep B, HCV and HIV from the exposed staff member for investigations – May be immunized against Hep B considering the other medical conditions and medication, pregnancy etc. – Report all accidental exposures to the HOD
Management of accidental Exposures to blood and body fluids – – If the source is known to have Hep B, HIV or HCV; check the recipient’s blood for Hep. B Surface antigen, HIV or HCV RNA respectively. If negative, the same investigations should be carried out at 12 weeks, 24 weeks and after 1 year before arriving at the conclusion that the individual is not infected. – Accidental exposure to known cases of Rabies, Chicken pox and Tuberculosis too would need post exposure prophylaxis.
Management of accidental Exposures to blood and body fluids – • Rabies – one dose of ARV given IM on day 0, 7 and 28. Booster dose after 1 year. Those who are at continuous risk of exposure would benefit from one dose of ARV once in every 5 years. • Chicken pox –If exposed, isolate the individual, antivirals or Varicella immunoglobulins, vaccines could be given depending on the condition. • Tuberculosis – Known patients with TB should be isolated. If infected, they should be directed to medical treatment with anti TB drugs. All patients with Tuberculosis should be notified.
g. Isolation of patients • A patient who could transmit infections should be isolated as quickly as possible. • The isolation room should be designed in such a way to generate negative air pressure towards the patient’s room. • The isolation room should have designated patient care equipment and all who enter the room as well as leaving the room should essentially wash hands. • Clean gowns, masks and gloves should be worn when entering the room and should be removed and hung before leaving the room. Isolated patients should not be transported to other areas of the hospital for investigations or for procedures unless when it is absolutely necessary.
Prevention of Hospital acquired infections (HAI) • It is of paramount importance to develop a programme within the institution to control hospital acquired infections and to implement it with the support of all staff members. Good infection control practices would ensure the well being of the patients as well as of the staff.
Objectives of the programme • • • Training of staff in prevention and control of HAI Monitoring the incidence and out breaks of HAI Investigation of out breaks Controlling of out breaks by rectification of procedures, techniques and other lapses Monitoring of staff practices in order to prevent cross infections To set guidelines on isolation procedures and infection control measures Inspection of other services including waste disposal, laundry and the kitchen hygiene Monitoring and advising on the antibiotic policy of the hospital

Waste Management

Waste Management 1. Proper Collection 2. Segregation 3. Transport 4. Disposal 5. Awareness & training
1. Waste minimization and segregation • Minimization • The quantity can be minimized by recycling procedures of appropriate items. All non contaminated plastic items, unbroken glassware could be collected separately and handed over for recycling. • All broken glassware should follow the stream of sharp waste
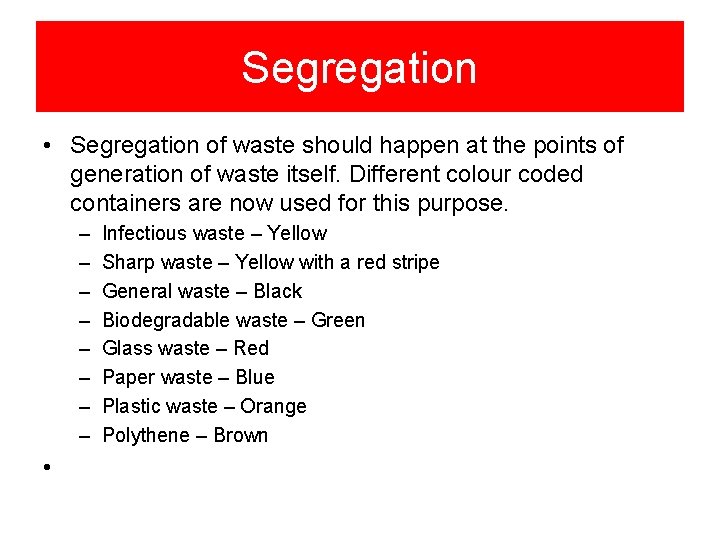
Segregation • Segregation of waste should happen at the points of generation of waste itself. Different colour coded containers are now used for this purpose. – – – – • Infectious waste – Yellow Sharp waste – Yellow with a red stripe General waste – Black Biodegradable waste – Green Glass waste – Red Paper waste – Blue Plastic waste – Orange Polythene – Brown
2. Waste Collection and Transport • Hazardous waste should be collected in yellow colour polythene bags placed in yellow bins • Sharps should be collected in puncture proof and leak proof plastic or cardboard boxes which should have a small opening to drop items into it. No attempts should be made to remove items once dropped into the sharp bin. The box should be of yellow colour with red stripes. • General waste to be collected in black polythene bags
Transport of waste • Waste should be collected from each ward on a regular schedule • Sanitary staff handling waste should wear protective clothing including face masks, aprons, boots and heavy duty gloves • All yellow bags should be sealed with adhesive tapes prior to transporting them. • The sharps bin should be closed and disposed when ¾ full. • The waste cart or the trolley used for transporting waste should not be used for any other purpose.
3. Waste Storage • A separate central storage facility should be provided for storage of waste. The non hazardous waste could be handed over to the local government authorities.
Waste Treatment & disposal • • • The hazardous waste should be treated prior to disposal. Blood – Blood bags should be incinerated. Samples of blood can be autoclaved before being discarded or concentrated hypochlorite can be used over night. Infectious solid waste – this could be incinerated, buried at a sufficient depth (>1 m) or autoclaved. Placenta and anatomical waste – All anatomical waste packed in yellow bags should be incinerated. It could be buried in a designated pit of > 1 m depth if the site is away (> 100 m) from any source of under ground water. Anatomical waste should be stored at a temperature between 1 – 5 degrees in the mortuary until transported. Chemical waste and pharmaceutical waste – Large quantities should be returned to the supplier to destroy
Waste treatment & disposal • Effluents – All liquid infectious waste should be discharged to the sewerage system after treatment with concentrated hypochlorite (10%) • Sharps – Sharps are destroyed along with the other infectious waste by incineration. They can be destroyed by autoclaving and shredding. The residues of incineration should be buried. • Radioactive waste – The guidelines given by the Atomic energy Authority regarding the storage and disposal should be followed. A written protocol should be displayed in the unit. All radioactive material should be placed in large containers or drums and should be labeled with the radiation symbol and the required standing period to allow decay to background level. They should be stored in a lead shielded storage room. Once decayed to background level, they can be disposed as infectious waste Liquid radioactive waste can be discarded into the sewerage system once it is certified as free of radioactivity.
Supplies • • • Detergents Soaps Efficient Low cost Disposable items
Laundry • Soiled clothes • CSSD
Continues training
Methods • Streamline Procedures – Invasive techniques – Other procedure • Hand washing techniques
Antibiotic policy
Management of MRSA