Hospital Acquired Delirium Computer Tutorial and Presentation Amy
- Slides: 46
Hospital Acquired Delirium Computer Tutorial and Presentation Amy Gajkowski RN
Instructions Use the purple navigation buttons at the bottom of the screen to move through the tutorial. This button will go to the previous slide This button will take you to the table of contents This button will move you to the next slide Click on any link on the table of contents to be directed to that section of the tutorial 10/7/2020 2
Expected Outcomes § Understand the causes of hospital acquired delirium. § Recognize appropriate nursing interventions to prevent hospital acquired delirium § Understand that prevention is the best treatment for this medical condition. 10/7/2020 3
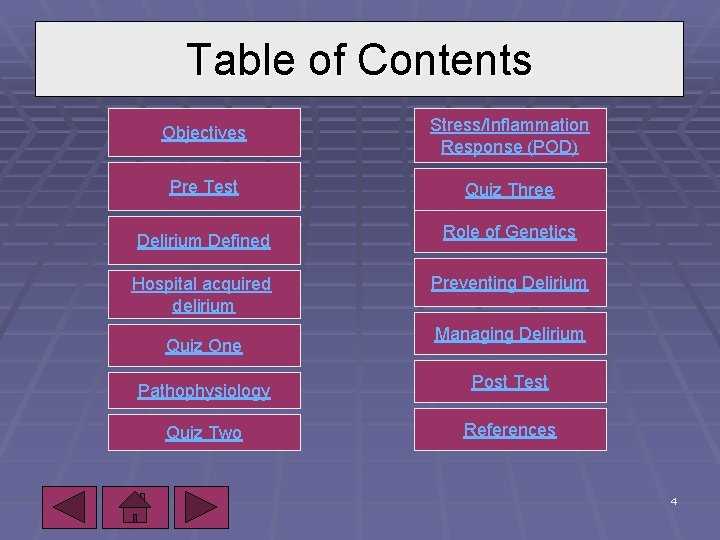
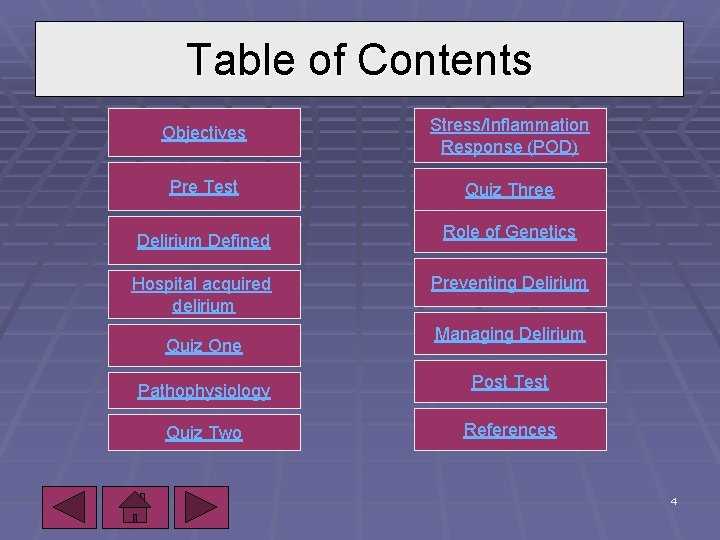
Table of Contents Objectives Stress/Inflammation Response (POD) Pre Test Quiz Three Delirium Defined Role of Genetics Hospital acquired delirium Preventing Delirium Quiz One 10/7/2020 Managing Delirium Pathophysiology Post Test Quiz Two References 4
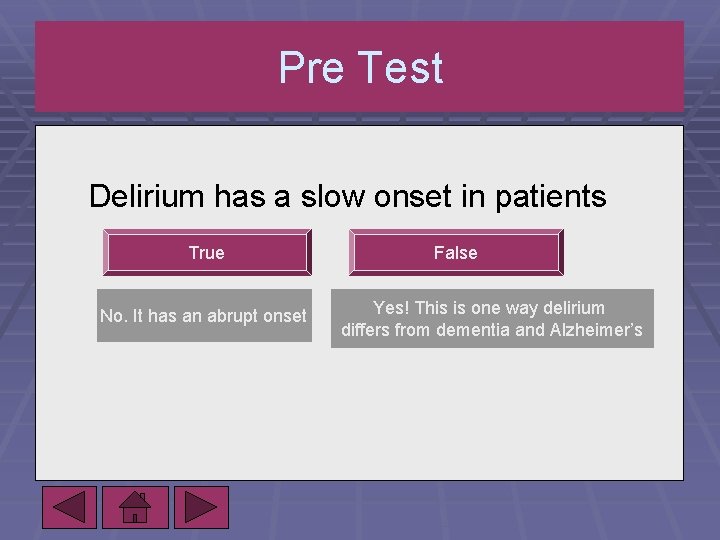
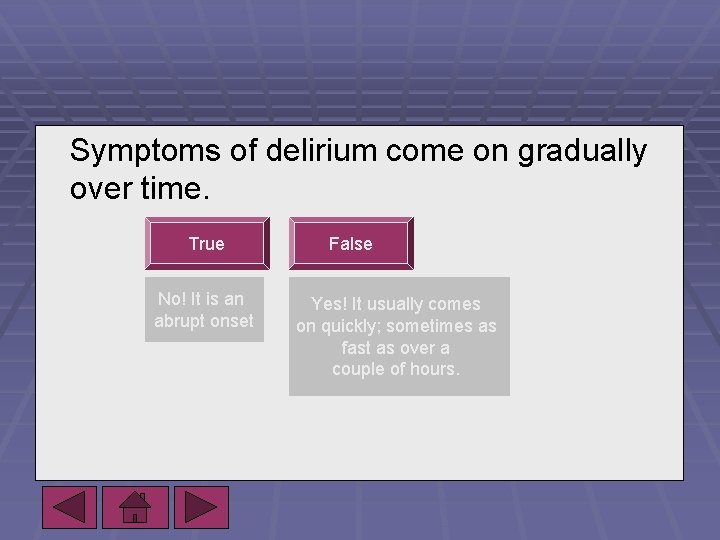
Pre Test Delirium has a slow onset in patients True No. It has an abrupt onset False Yes! This is one way delirium differs from dementia and Alzheimer’s
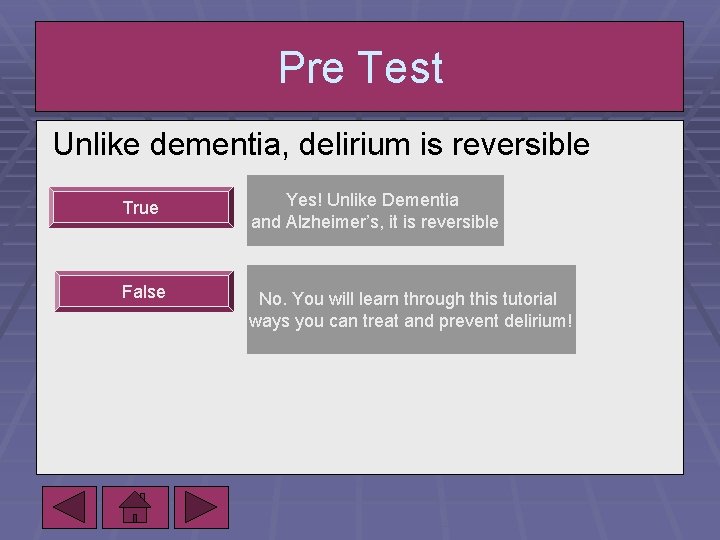
Pre Test Unlike dementia, delirium is reversible True Yes! Unlike Dementia and Alzheimer’s, it is reversible False No. You will learn through this tutorial ways you can treat and prevent delirium!
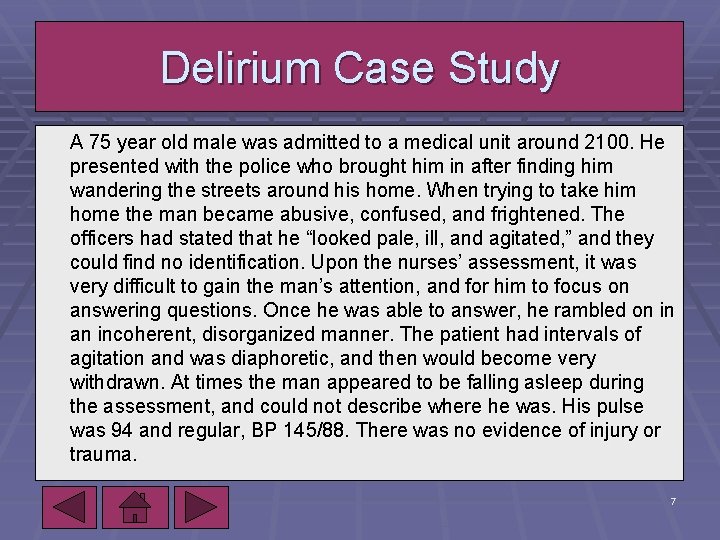
Delirium Case Study A 75 year old male was admitted to a medical unit around 2100. He presented with the police who brought him in after finding him wandering the streets around his home. When trying to take him home the man became abusive, confused, and frightened. The officers had stated that he “looked pale, ill, and agitated, ” and they could find no identification. Upon the nurses’ assessment, it was very difficult to gain the man’s attention, and for him to focus on answering questions. Once he was able to answer, he rambled on in an incoherent, disorganized manner. The patient had intervals of agitation and was diaphoretic, and then would become very withdrawn. At times the man appeared to be falling asleep during the assessment, and could not describe where he was. His pulse was 94 and regular, BP 145/88. There was no evidence of injury or trauma. 10/7/2020 7
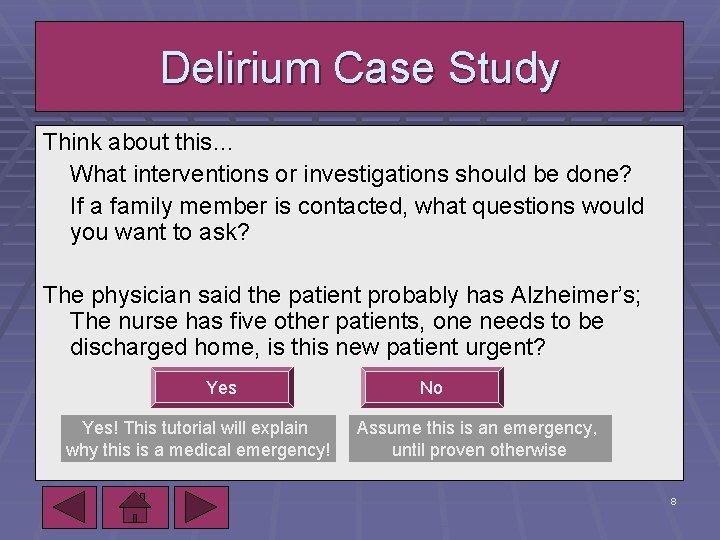
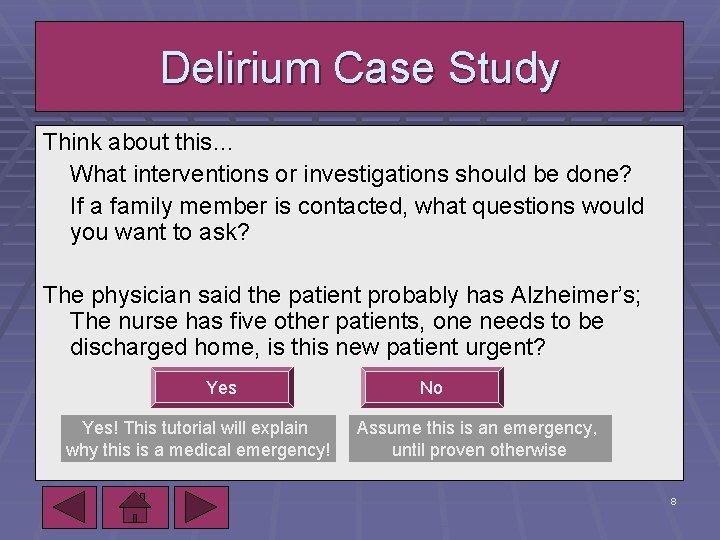
Delirium Case Study Think about this… What interventions or investigations should be done? If a family member is contacted, what questions would you want to ask? The physician said the patient probably has Alzheimer’s; The nurse has five other patients, one needs to be discharged home, is this new patient urgent? Yes! This tutorial will explain why this is a medical emergency! 10/7/2020 No Assume this is an emergency, until proven otherwise 8
Delirium Case Study § Delirium is often due to an acute illness or physiological change in the body. § It can be a presentation of many underlying diseases § It is often neglected as a medical emergency. § It is best to assume the onset of confusion is acute if there is no medical history available. 10/7/2020 9
Delirium Case Study § What should be done? § § CBC, electrolytes, renal/hepatic function, blood alcohol, chest x-ray, CT head. Results: UTI and dehydration. The patient improved, but was still confused. His son stated that he was fully functional at home with no memory impairments/confusion. The absence of history made it crucial to regard this patient as an emergency, and to observe him closely. 10/7/2020 10
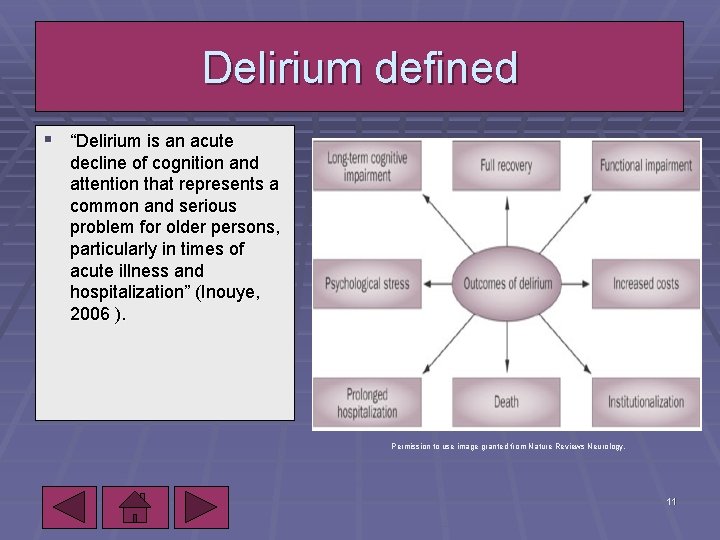
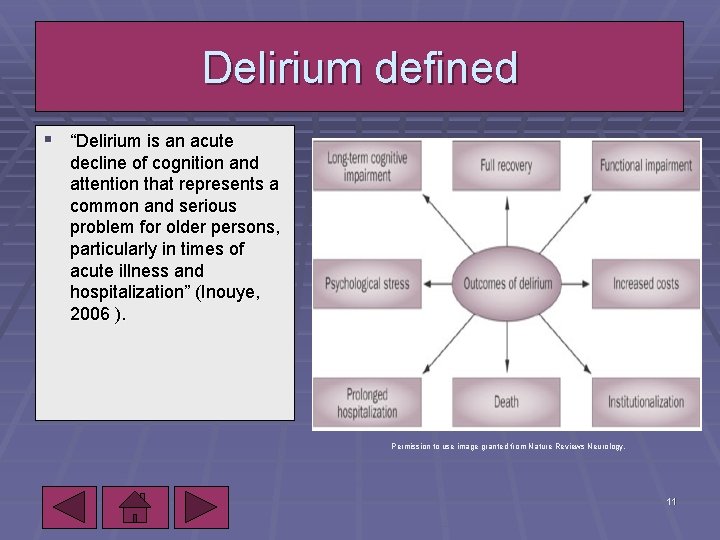
Delirium defined § “Delirium is an acute decline of cognition and attention that represents a common and serious problem for older persons, particularly in times of acute illness and hospitalization” (Inouye, 2006 ). Permission to use image granted from Nature Reviews Neurology. 10/7/2020 11
Delirium defined Clinical features of delirium… § Acute onset- occurs abruptly, over a period of hours or § § days. Fluctuating course- increase/decrease in severity, symptoms may come or go. Lucid intervals are common in post op patients. Inattention- shifting attention, difficulty focusing Disorganized thinking- illogical flow of ideas, rambling Altered level of consciousness- reduced clarity of environment, lethargy (Inouye, 2006). 10/7/2020 12
Symptoms of delirium come on gradually over time. True No! It is an abrupt onset False Yes! It usually comes on quickly; sometimes as fast as over a couple of hours.
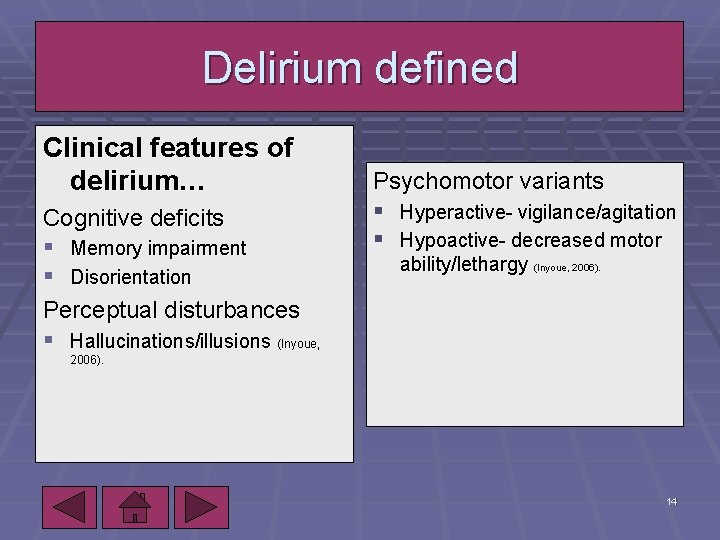
Delirium defined Clinical features of delirium… Cognitive deficits § Memory impairment § Disorientation Perceptual disturbances § Hallucinations/illusions (Inyoue, Psychomotor variants § Hyperactive- vigilance/agitation § Hypoactive- decreased motor ability/lethargy (Inyoue, 2006). 10/7/2020 14
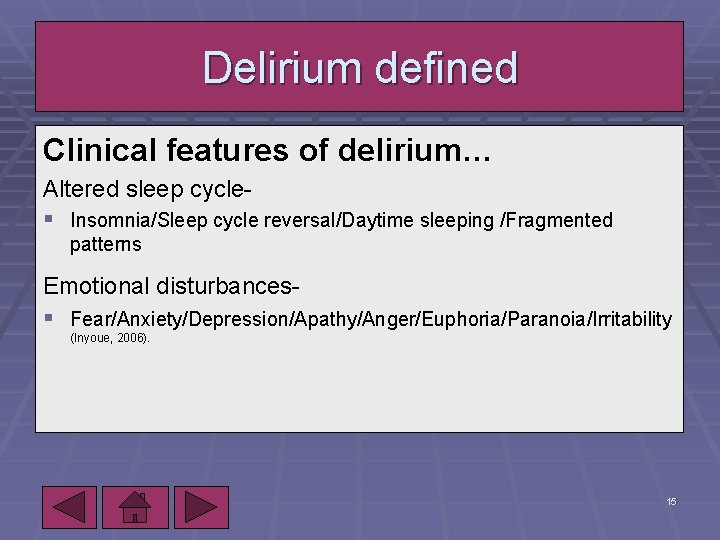
Delirium defined Clinical features of delirium… Altered sleep cycle§ Insomnia/Sleep cycle reversal/Daytime sleeping /Fragmented patterns Emotional disturbances§ Fear/Anxiety/Depression/Apathy/Anger/Euphoria/Paranoia/Irritability (Inyoue, 2006). 10/7/2020 15
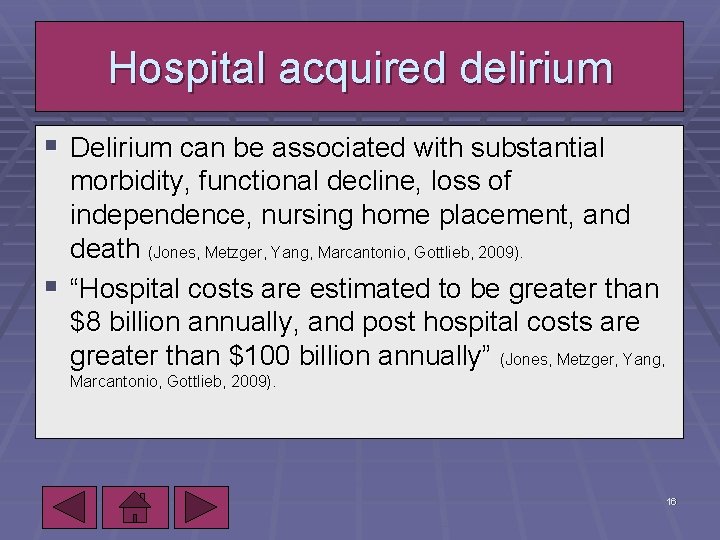
Hospital acquired delirium § Delirium can be associated with substantial morbidity, functional decline, loss of independence, nursing home placement, and death (Jones, Metzger, Yang, Marcantonio, Gottlieb, 2009). § “Hospital costs are estimated to be greater than $8 billion annually, and post hospital costs are greater than $100 billion annually” (Jones, Metzger, Yang, Marcantonio, Gottlieb, 2009). 10/7/2020 16
Hospital acquired delirium § Prevalence increases with age. § “The mortality rate among hospitalized patients with delirium range from 22 -76%” (Bryant, 2009 ). § The one year mortality rate associated with cases of delirium is 35 -40% (Jones, Metzger, Yang, Marcantonio, Gottlieb, 2009). 10/7/2020 17
Hospital acquired delirium § Delirium is often unrecognized due to § fluctuating nature § overlap with dementia § lack cognitive assessment § lack of knowledge of the consequences 10/7/2020 The best treatment for delirium is prevention! Risk Factors include: Age >65 Neurodegenerative disease 18
Quiz one What is the best treatment for delirium? Medications No, it is suggested to avoid medications Prevention Yes, prevention! 10/7/2020 19
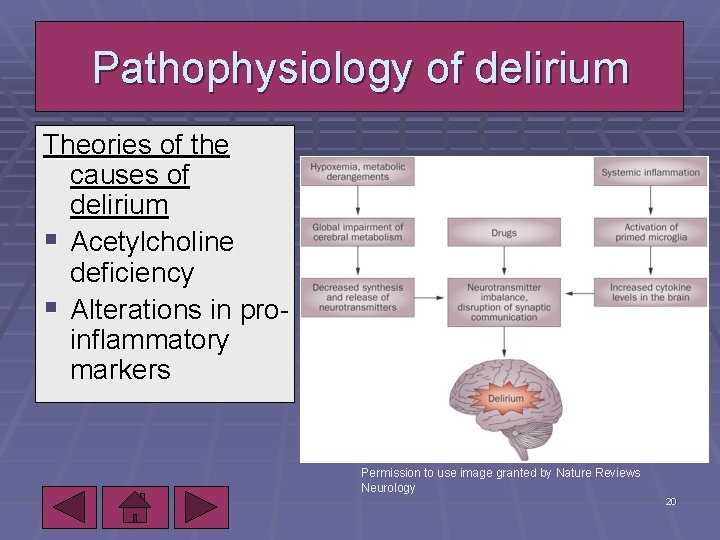
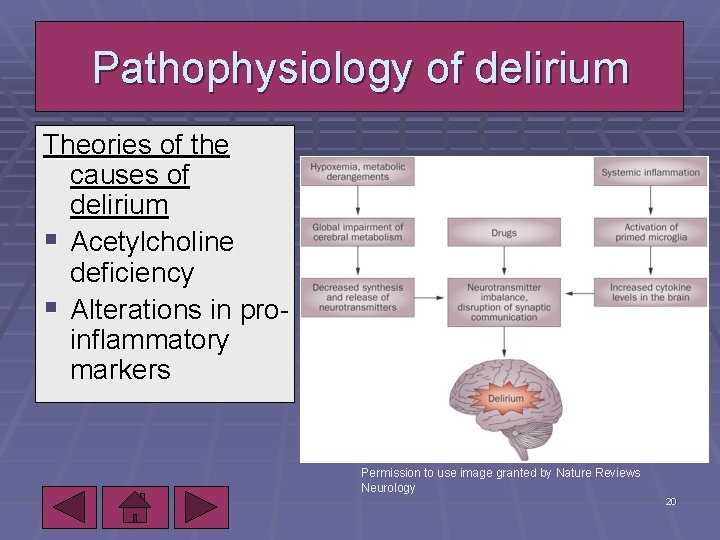
Pathophysiology of delirium Theories of the causes of delirium § Acetylcholine deficiency § Alterations in proinflammatory markers Permission to use image granted by Nature Reviews Neurology 10/7/2020 20
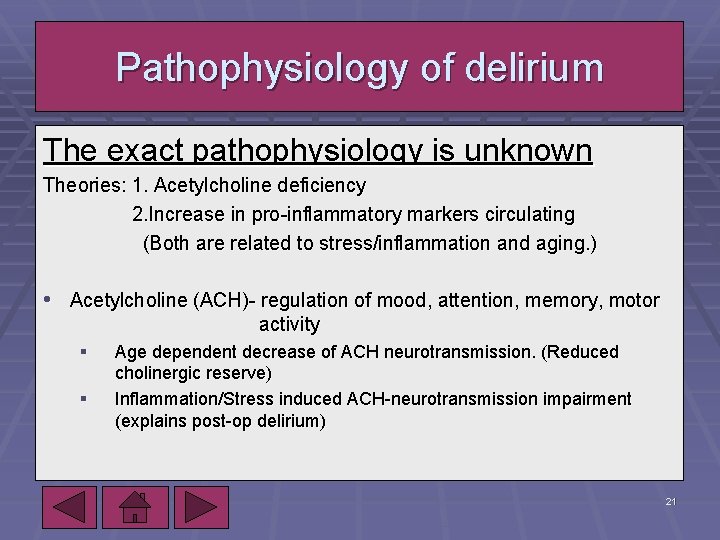
Pathophysiology of delirium The exact pathophysiology is unknown Theories: 1. Acetylcholine deficiency 2. Increase in pro-inflammatory markers circulating (Both are related to stress/inflammation and aging. ) • Acetylcholine (ACH)- regulation of mood, attention, memory, motor activity § § 10/7/2020 Age dependent decrease of ACH neurotransmission. (Reduced cholinergic reserve) Inflammation/Stress induced ACH-neurotransmission impairment (explains post-op delirium) 21
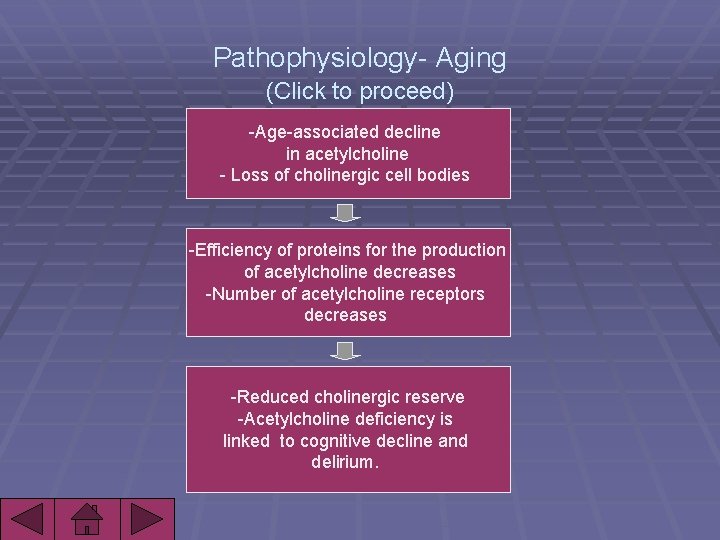
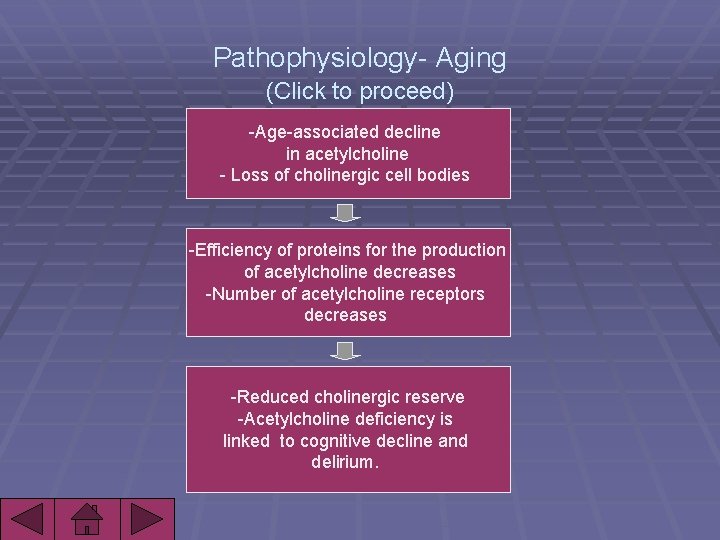
Pathophysiology- Aging (Click to proceed) -Age-associated decline in acetylcholine - Loss of cholinergic cell bodies -Efficiency of proteins for the production of acetylcholine decreases -Number of acetylcholine receptors decreases -Reduced cholinergic reserve -Acetylcholine deficiency is linked to cognitive decline and delirium.
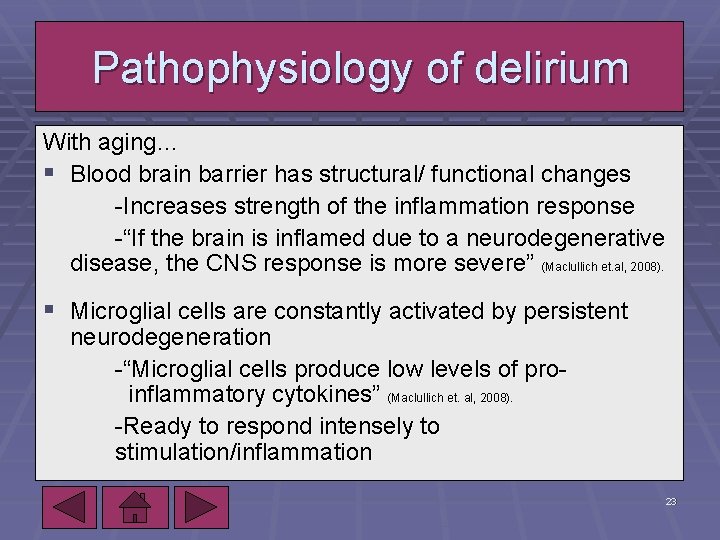
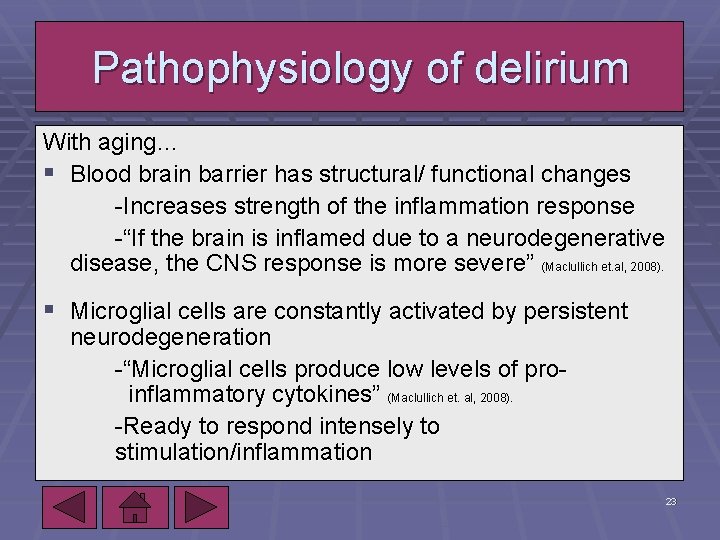
Pathophysiology of delirium With aging… § Blood brain barrier has structural/ functional changes -Increases strength of the inflammation response -“If the brain is inflamed due to a neurodegenerative disease, the CNS response is more severe” (Maclullich et. al, 2008). § Microglial cells are constantly activated by persistent neurodegeneration -“Microglial cells produce low levels of proinflammatory cytokines” (Maclullich et. al, 2008). -Ready to respond intensely to stimulation/inflammation 10/7/2020 23
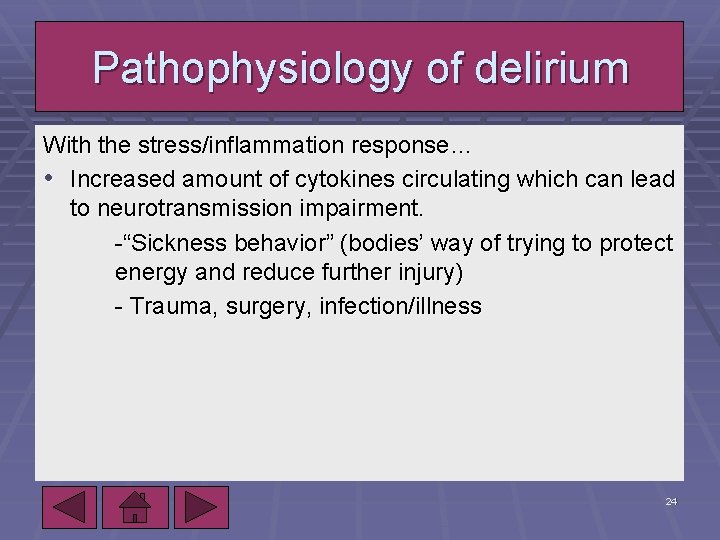
Pathophysiology of delirium With the stress/inflammation response… • Increased amount of cytokines circulating which can lead to neurotransmission impairment. -“Sickness behavior” (bodies’ way of trying to protect energy and reduce further injury) - Trauma, surgery, infection/illness 10/7/2020 24
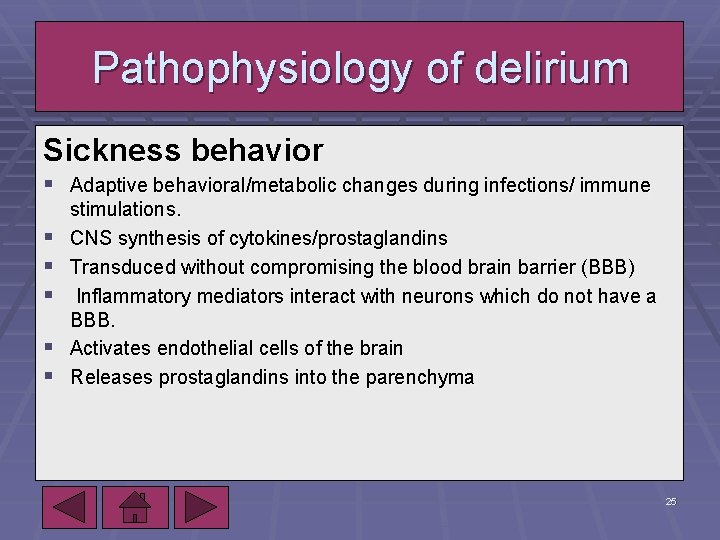
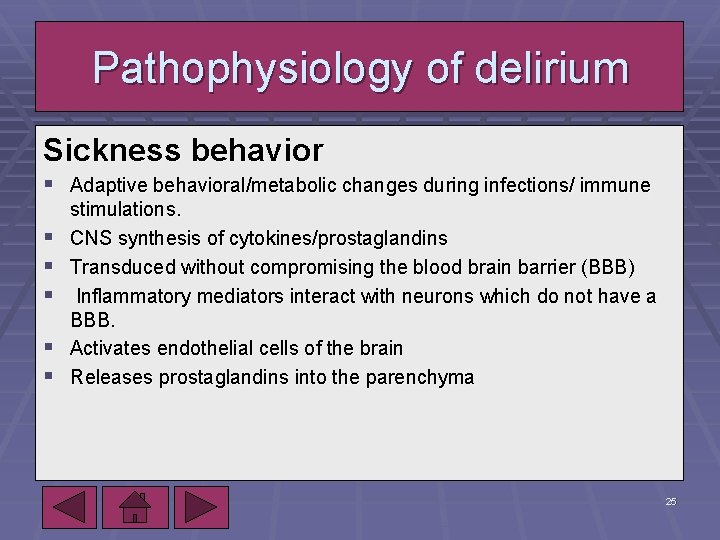
Pathophysiology of delirium Sickness behavior § Adaptive behavioral/metabolic changes during infections/ immune § § § stimulations. CNS synthesis of cytokines/prostaglandins Transduced without compromising the blood brain barrier (BBB) Inflammatory mediators interact with neurons which do not have a BBB. Activates endothelial cells of the brain Releases prostaglandins into the parenchyma 10/7/2020 25
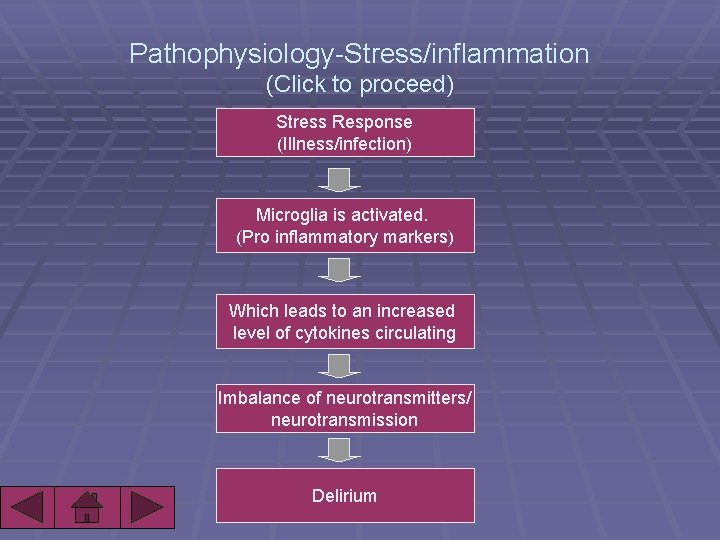
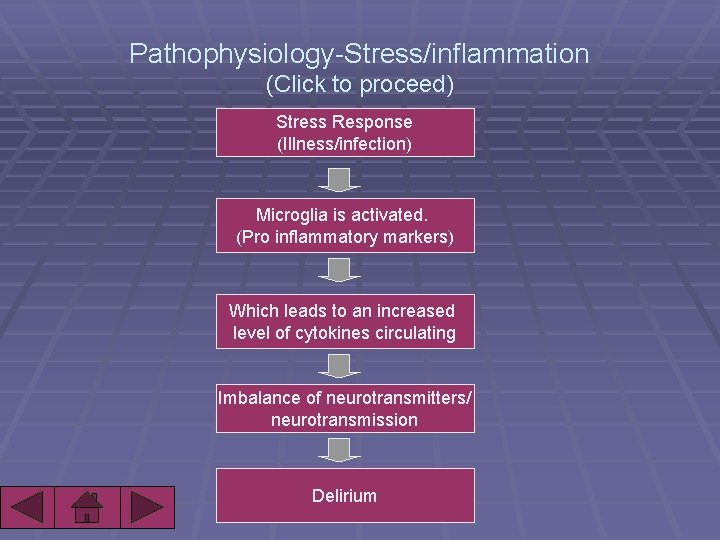
Pathophysiology-Stress/inflammation (Click to proceed) Stress Response (Illness/infection) Microglia is activated. (Pro inflammatory markers) Which leads to an increased level of cytokines circulating Imbalance of neurotransmitters/ neurotransmission Delirium
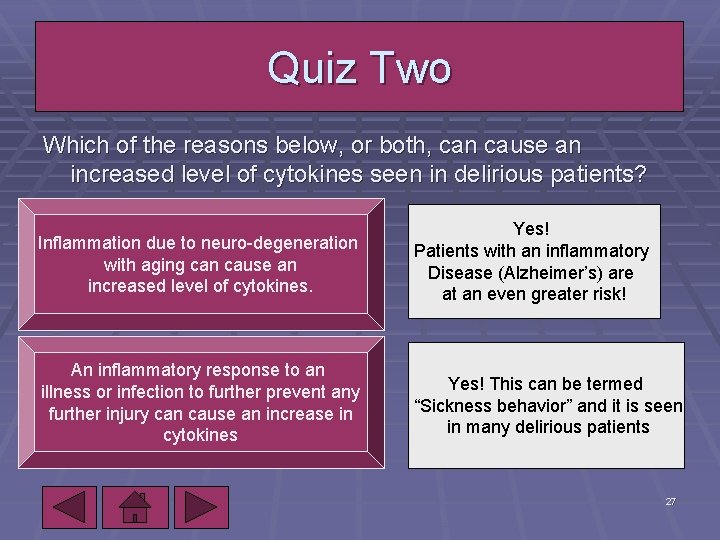
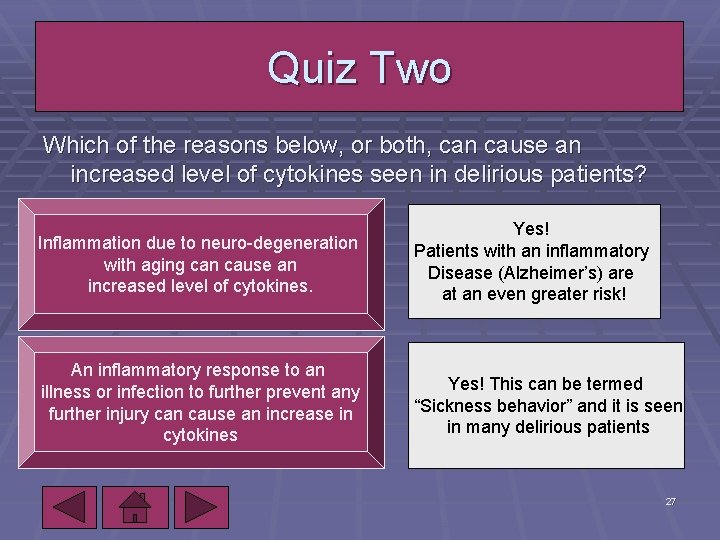
Quiz Two Which of the reasons below, or both, can cause an increased level of cytokines seen in delirious patients? Inflammation due to neuro-degeneration with aging can cause an increased level of cytokines. Yes! Patients with an inflammatory Disease (Alzheimer’s) are at an even greater risk! An inflammatory response to an illness or infection to further prevent any further injury can cause an increase in cytokines Yes! This can be termed “Sickness behavior” and it is seen in many delirious patients 10/7/2020 27
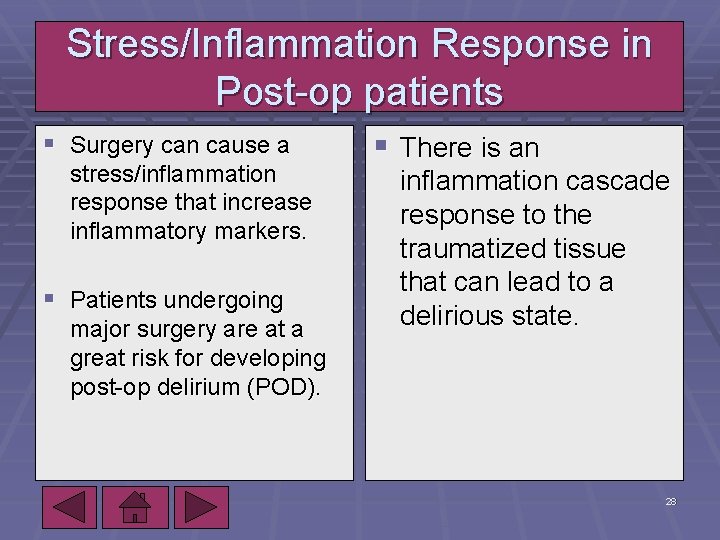
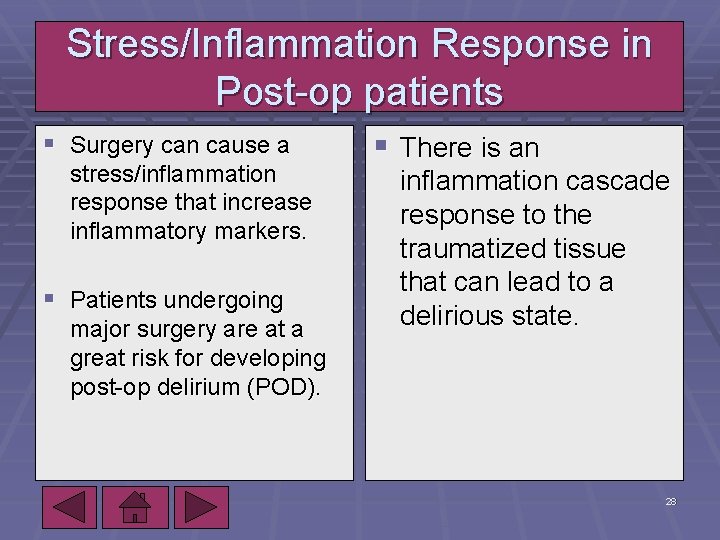
Stress/Inflammation Response in Post-op patients § Surgery can cause a stress/inflammation response that increase inflammatory markers. § Patients undergoing major surgery are at a great risk for developing post-op delirium (POD). 10/7/2020 § There is an inflammation cascade response to the traumatized tissue that can lead to a delirious state. 28
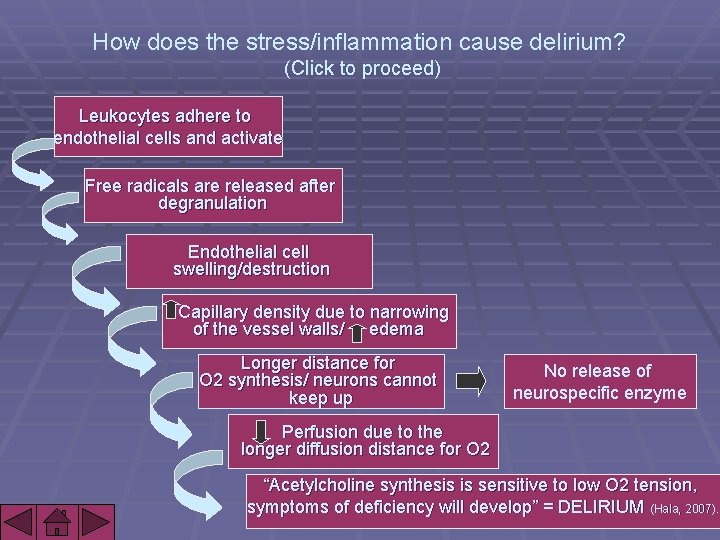
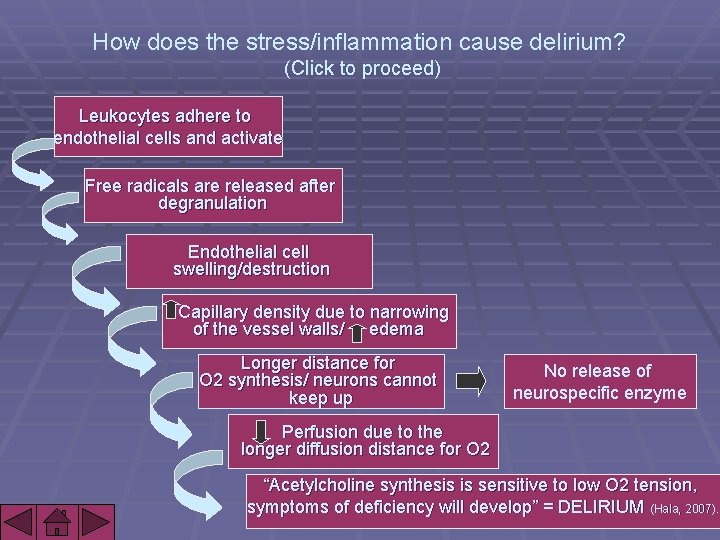
How does the stress/inflammation cause delirium? (Click to proceed) Leukocytes adhere to endothelial cells and activate Free radicals are released after degranulation Endothelial cell swelling/destruction Capillary density due to narrowing of the vessel walls/ edema Longer distance for O 2 synthesis/ neurons cannot keep up No release of neurospecific enzyme Perfusion due to the longer diffusion distance for O 2 “Acetylcholine synthesis is sensitive to low O 2 tension, symptoms of deficiency will develop” = DELIRIUM (Hala, 2007).
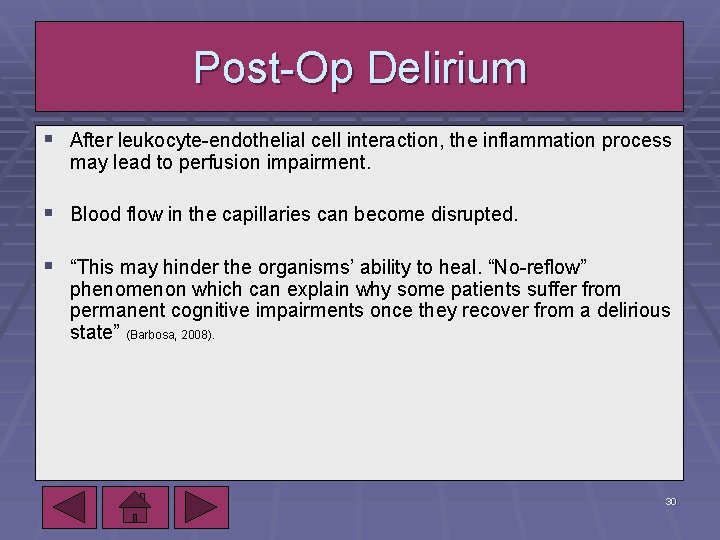
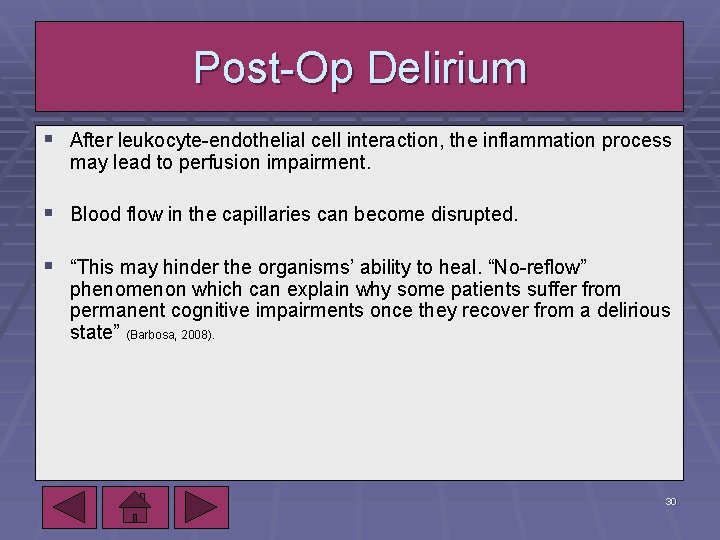
Post-Op Delirium § After leukocyte-endothelial cell interaction, the inflammation process may lead to perfusion impairment. § Blood flow in the capillaries can become disrupted. § “This may hinder the organisms’ ability to heal. “No-reflow” phenomenon which can explain why some patients suffer from permanent cognitive impairments once they recover from a delirious state” (Barbosa, 2008). 10/7/2020 30
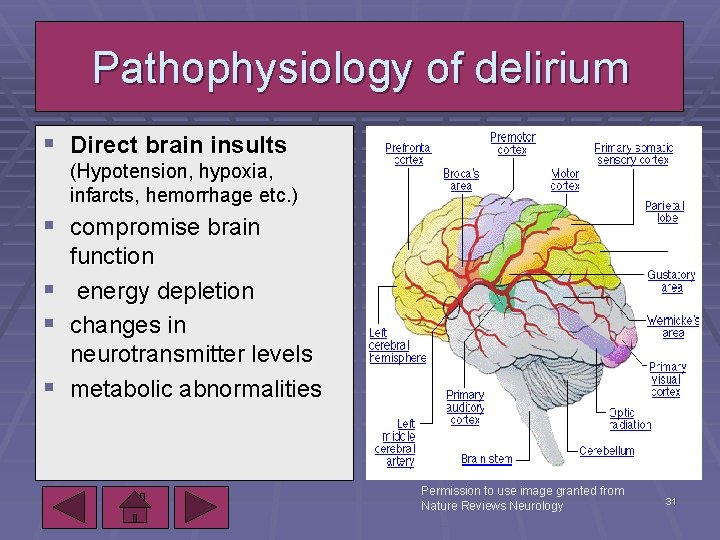
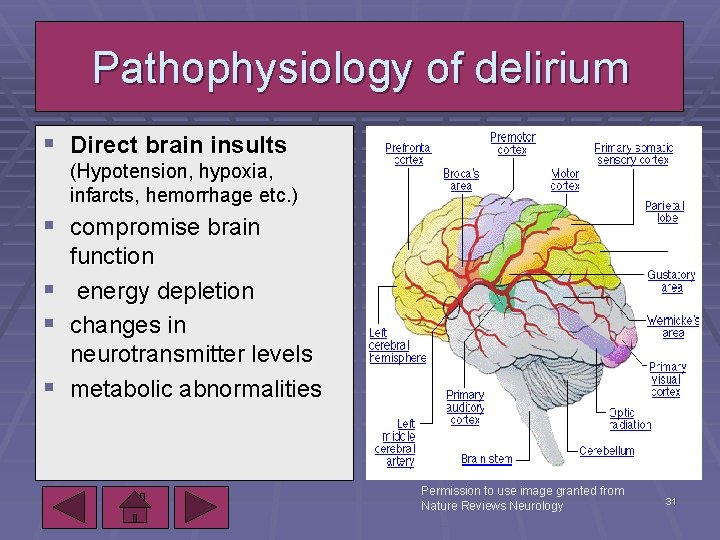
Pathophysiology of delirium § Direct brain insults (Hypotension, hypoxia, infarcts, hemorrhage etc. ) § compromise brain function § energy depletion § changes in neurotransmitter levels § metabolic abnormalities 10/7/2020 Permission to use image granted from Nature Reviews Neurology 31
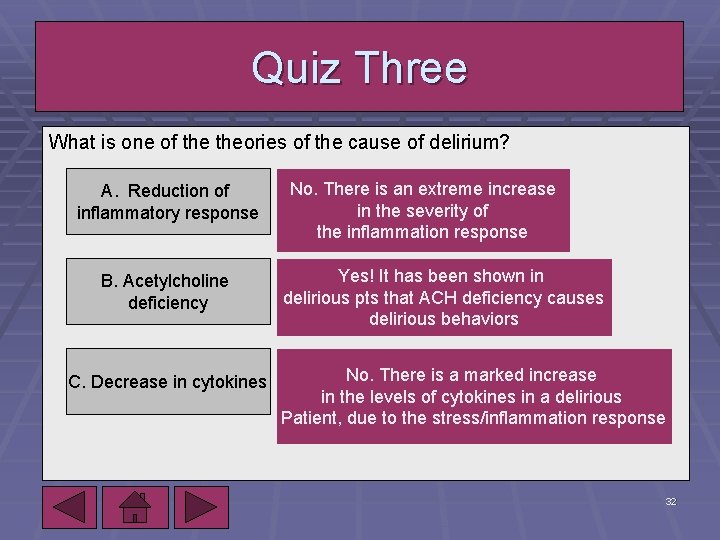
Quiz Three What is one of theories of the cause of delirium? A. Reduction of inflammatory response B. Acetylcholine deficiency C. Decrease in cytokines 10/7/2020 No. There is an extreme increase in the severity of the inflammation response Yes! It has been shown in delirious pts that ACH deficiency causes delirious behaviors No. There is a marked increase in the levels of cytokines in a delirious Patient, due to the stress/inflammation response 32
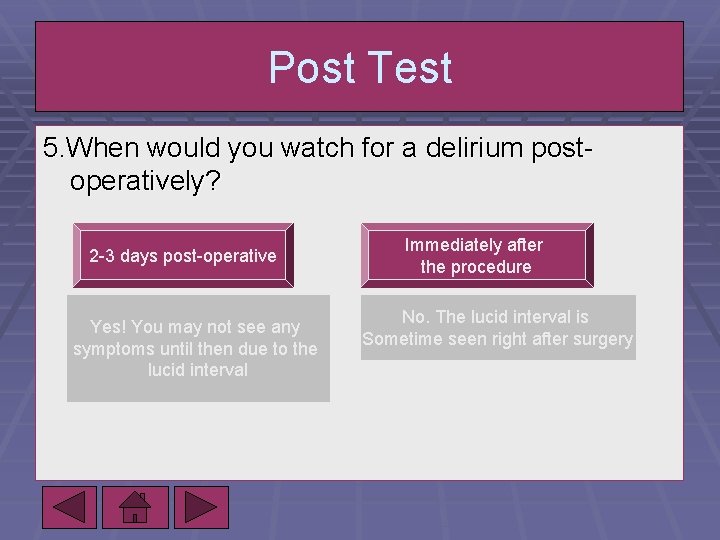
Post-Op Delirium § Sometimes there can be a lucid interval for a postop patient. § During the lucid interval, there may be no psychiatric symptoms. 10/7/2020 § Watch for symptoms on the second or third day! 33
Role of genetics in delirium § Studies link apolipoprotein E 4 allele (APOE) and delirium in elderly. § “linked to cognitive impairment in people with dementia. role in neural plasticity, repairs damaged neurons, and aids in neural transmission” (Van Munster, 2009) § “APOE E 4 genotype- increased inflammation, reduced cholinergic activity in the brain, increased cytokines and reduced acetylcholinergic pathways” (Van Munster, 2009). § According to the articles, more research is to come our way! 10/7/2020 34
Recognizing/Preventing Delirium § When a patient presents with confusion: § “Determining the acuity of the change in mental status is the essential first step” (Inouye, 2006). § Every older hospitalized patient should undergo formal cognitive testing. (Ex. CAM). § “Older adults should be aroused during rounds and evaluated if the hypoactive form of delirium is suspected” (Inouye, 2006). 10/7/2020 35
Recognizing/Preventing Delirium § § § § Address risk factors Provide orienting communication Encourage mobilization Use visual/ hearing aids Prevent dehydration Provide un-interrupted sleep time Avoid psychoactive drugs 10/7/2020 36
Recognizing/preventing delirium If there is a mental change that is acute… § “Perform a cognitive assessment and evaluation for delirium. Rule out depression, mania, and acute psychosis” (Inouye, 2006). In the case study, the nurse would have done a screening for delirium, such as a CAM score. The RN would have re-oriented the patient, and monitored his mental status closely. If delirium is confirmed… § “Provide supportive care/ prevent complications” (Inouye, 2006). 10/7/2020 37
Managing delirium nonpharmacologically § § § § Non-pharmacologic treatment strategies Continue delirium prevention Reorient patient, encourage family involvement Use sitters/avoid physical restraints/foley catheters Use music/massage/relaxation techniques for agitation Use of hearing/ visual aids /interpreters Maintain patient’s mobility Normalize sleep/wake cycle 10/7/2020 38
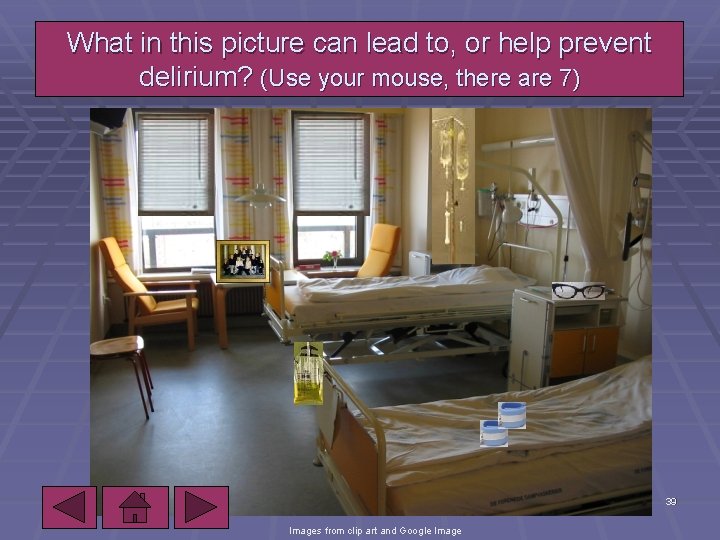
What in this picture can lead to, or help prevent delirium? (Use your mouse, there are 7) 10/7/2020 39 Images from clip art and Google Image
Managing delirium nonpharmacologically Supportive care includes… § Protecting airway/preventing aspiration § Provide nutritional support § Provide skin care/prevent pressure sores § Mobilization/ prevent DVT, and PE With the man from the case study, the RN would have checked a chest X-ray, EKG, other lab work, etc. to see if the patient had an infection or any other deficits that may be causing his delirium. 10/7/2020 40
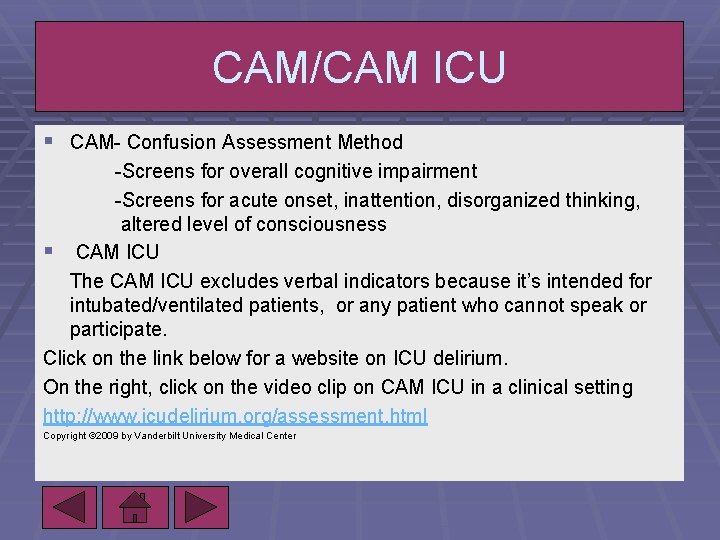
CAM/CAM ICU § CAM- Confusion Assessment Method -Screens for overall cognitive impairment -Screens for acute onset, inattention, disorganized thinking, altered level of consciousness § CAM ICU The CAM ICU excludes verbal indicators because it’s intended for intubated/ventilated patients, or any patient who cannot speak or participate. Click on the link below for a website on ICU delirium. On the right, click on the video clip on CAM ICU in a clinical setting http: //www. icudelirium. org/assessment. html Copyright © 2009 by Vanderbilt University Medical Center
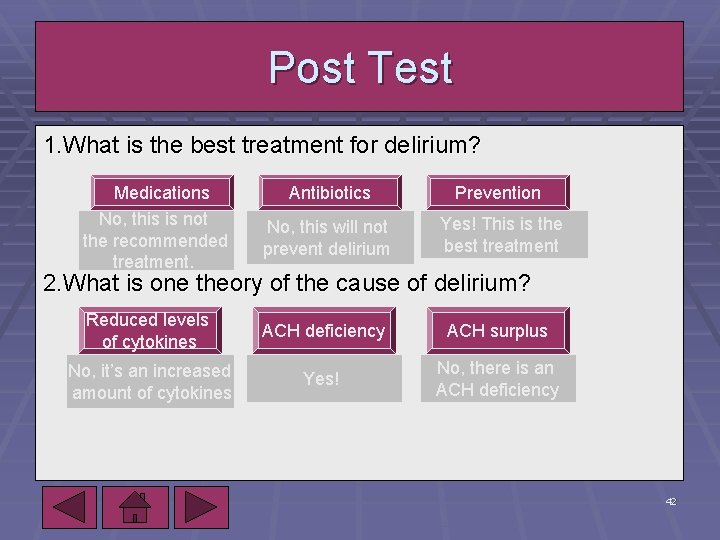
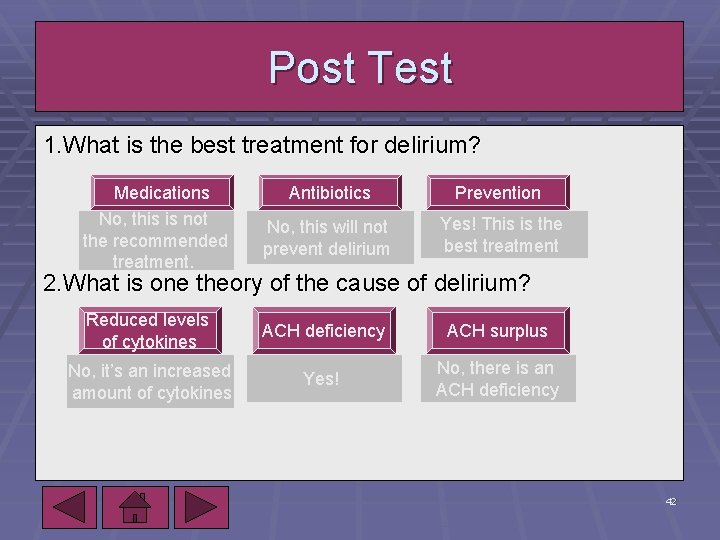
Post Test 1. What is the best treatment for delirium? Medications No, this is not the recommended treatment. Antibiotics Prevention No, this will not prevent delirium Yes! This is the best treatment 2. What is one theory of the cause of delirium? Reduced levels of cytokines ACH deficiency ACH surplus No, it’s an increased amount of cytokines Yes! No, there is an ACH deficiency 10/7/2020 42
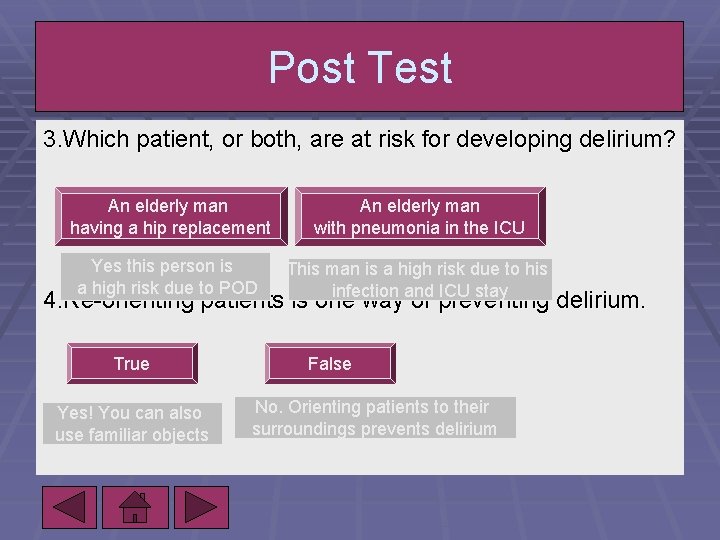
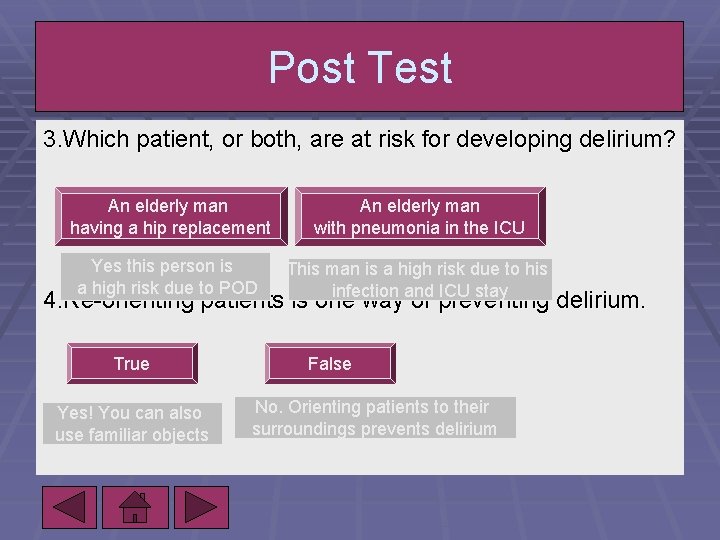
Post Test 3. Which patient, or both, are at risk for developing delirium? An elderly man having a hip replacement An elderly man with pneumonia in the ICU Yes this person is a high risk due to POD This man is a high risk due to his infection and ICU stay 4. Re-orienting patients is one way of preventing delirium. True Yes! You can also use familiar objects False No. Orienting patients to their surroundings prevents delirium
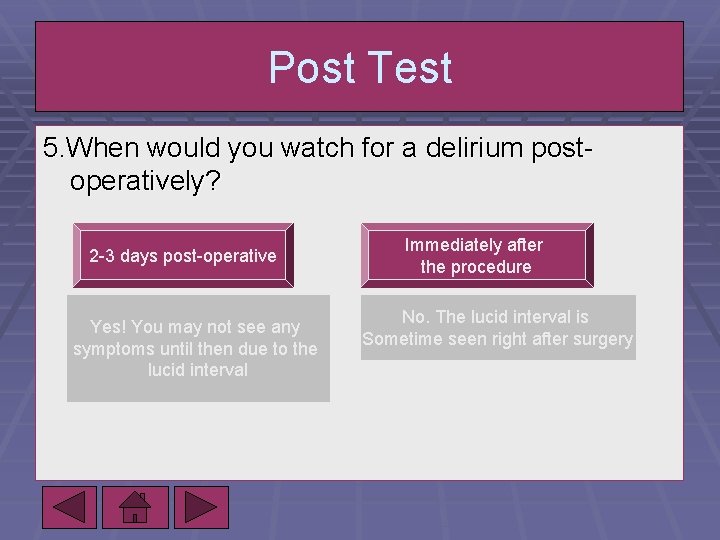
Post Test 5. When would you watch for a delirium postoperatively? 2 -3 days post-operative Yes! You may not see any symptoms until then due to the lucid interval Immediately after the procedure No. The lucid interval is Sometime seen right after surgery
Congratulations! You have completed this tutorial. Further Questions? Amy Gajkowski RN, BSN gajkowam@alverno. edu
References Barbosa, F, Martins da Cunha, R, & Pinto, A. (2008). Postoperative delirium in the elderly [vol 58 no. 6]. Retrieved from http: //www. scielo. br/scielo. php. doi: 10. 1590/S 0034 Bryant, C. (2010). Dementia, Delirium, Agitation, and Behavioural Problems. Journal of Psychosomatic Research, 200809. Wiley Inter. Science. Retrieved from: Http: //www. interscience. wiley. com/cgibin/summary/122300212/doi. org/10. 1002/9780470017975. Byrne, M, & Devine, E. (Ed. ). (2009). Knowledge Based nursing initiative- risk for delirium in adults in intensive care. Milwaukee: Aurora Health Care. Fong, T, Tulebaev, S, & Inouye, S. (2009). Delirium in elderly adults: diagnosis, prevention, and treatment. Nature Review, 5. Retrieved from http: //www. nature. com/nrneurol doi: 10. 1038/nrneurol. 2009. 24 Hala, M. (2007). Pathophysiology of postoperative delirium: Systemic inflammation as a response to surgical trauma causes diffuse microcirculatory impairment Medical Hypotheses, Volume 68, Issue 1, Pages 194 -196 Ham, R, & Sloan, P. (2008). Primary care geriatrics. St. Louis, MI: Mosby. Inouye, S. (2006). Delirium in older persons. The New England Journal of Medicine, 65. Retrieved from www. NEJM. org Jaafar, A, Heycock, R, & George, J. (2008). Frailty- a clinical overview. Review in Clinical Gerontology, 17. doi: 10. 1017/S 0959259808002642 Jones, R, Fong, T, Metzger, E, Tulebaev, S, & Yang, F. (2010). Aging, Brain disease, and Reserve: Implications for Delirium. American association for geriatric psychiatry. Retrieved (2010, March 23) Leentjens, A, & Van der Mast, R. (2005). Delirium in elderly people: an update. Current Opinion in Psychiatry, 18. Retrieved from http: //www. medscape. com/viewarticle/503089 Lemstra, A, kalisvaaart, K, Vreeswijk, R, Van Gool, W, & Eikelenboom, P. (2008). Pre-operative inflammatory markers and the risk of postoperative delirium in elderly patients. International Journal of Geriatric Psychiatry, 23. Retrieved from www. interscience. wiley. com doi: 10. 1002/gps. 2015 Luetz, A, Heymann, A, Radtke, F, Chenitir, C, & Heinz, A. (2010). Different assessment tools for intensive care unit delirium: which score to use? . Critical Care Medicine, 38(2), 409 -417. Maclullich, A, Ferguson, K, Miller, T, Roolj, E, & Cunningham, C. (2008). Unravelling the pathophysiology of delirium: a focus on the role of aberrant stress response. Journal of Psychosomatic Research, 65(3), Retrieved from http: //www. sciencedirect. com/science doi: 10. 1016/j. jpsychores. 2008. 05. 019 Rooji, S, Van Munster, B, Korevaar, J, & Levi, M. (2007). Cytokines and acute phase response in delirium. Journal of Psychosomatic Research, 62(5), Retrieved from www. sciencedirect. com/science doi: 10. 1016/j. jpschores. 2006. 11. 013 Van Munster, B, Rooij, S, & Korevaar, J. (2009). The Role of genetics in delirium in the elderly patient. Dementia and Geriatric Cognitive Disorders, 28. Retrieved from www. karger. com/dem doi: 10. 1159/000235796 10/7/2020 46