HORMONE RESISTANCE SYNDROME AND MULTIPLE ENDOCRINE NEOPLASIA HORMONE


- Slides: 23

HORMONE RESISTANCE SYNDROME AND MULTIPLE ENDOCRINE NEOPLASIA
HORMONE RESISTANCE SYNDROME Condition caused by a reduced or absent responsiveness to a biologically active hormone, due to a hormone receptor defect or a post-receptor defect.
Thyroid hormone resistance syndrome Disorders in which the body’s tissues are resistance to the effects of thyroid hormone. Generalised resistance to thyroid hormone (GRTH) Resistance in pituitary gland most or all peripheral tissue. Selective primary pituitary resistance to thyroid hormone (PRTH) Resistance in pitutary gland but not in peripheral tissues. Selective peripheral resistance (Per. RTH) Resistance in peripheral tissues but not in the pitutary.
Causes: Mutations of the beta form THRB gene of the thyroid hormone receptor. Mutations in MCT 8 and SECISBP 2 also associated. Incidence: Rare syndrome-1 in 50000 or 1 in 40000 live births.
Symptoms: Eumetabolic-goiter, elevated plasma levels of thyroxine and triiodouridine, delayed bone maturation, mental retardation, learning disabilities and hearing defects. Treatment: Clinically euthyroid requires no treatment but for PRTH –not satisfactory.
Insulin resistance syndrome Combination of medical conditions links to an increased risk of premature heart disease. Risk for type 2 diabetes and atherosclerosis, obesity, high blood pressure, abnormal cholesterol levels. Insulin Resistance: The increase in glucose in blood stream signals the pancreas to increase the secretion of insulin hormone and it is used for energy.
In resistance, the body cells have diminished ability to respond to the action of insulin. To compensate this, pancreas secretes more insulin. This can develops high diabetes as high insulin levels. Components: Impaired fasting glucose High blood pressure Abnormal cholesterol levels Heart disease Obesity Kidney damage.
Diagnosis: No simple test. More than one parent or sibling have the risk factors that will leads the children to get this syndrome.
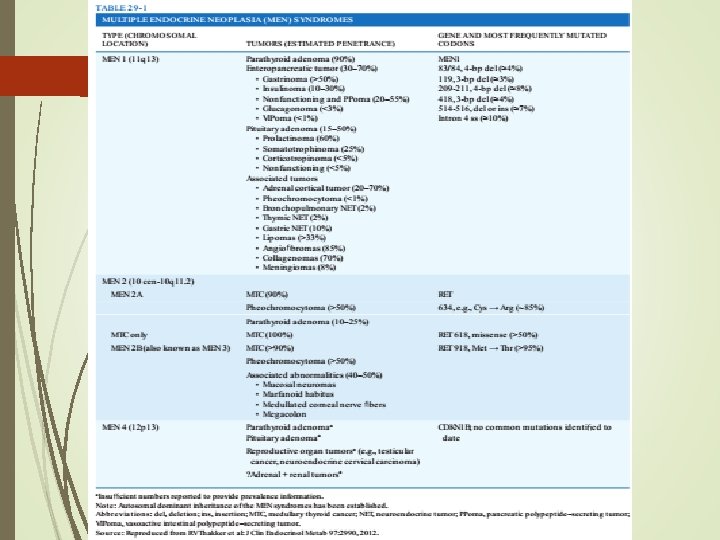
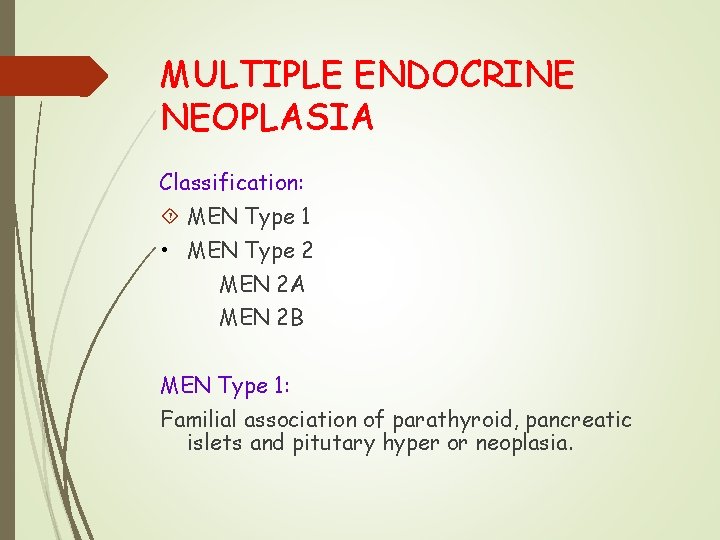
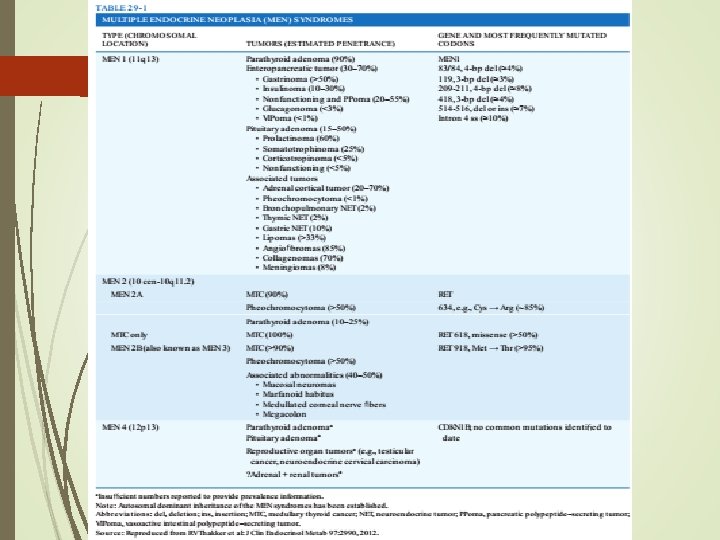
MULTIPLE ENDOCRINE NEOPLASIA Classification: MEN Type 1 • MEN Type 2 MEN 2 A MEN 2 B MEN Type 1: Familial association of parathyroid, pancreatic islets and pitutary hyper or neoplasia.
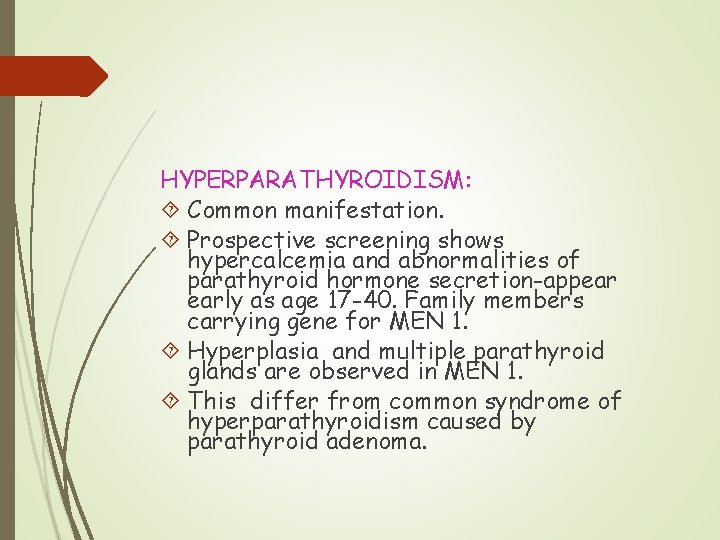
HYPERPARATHYROIDISM: Common manifestation. Prospective screening shows hypercalcemia and abnormalities of parathyroid hormone secretion-appear early as age 17 -40. Family members carrying gene for MEN 1. Hyperplasia and multiple parathyroid glands are observed in MEN 1. This differ from common syndrome of hyperparathyroidism caused by parathyroid adenoma.
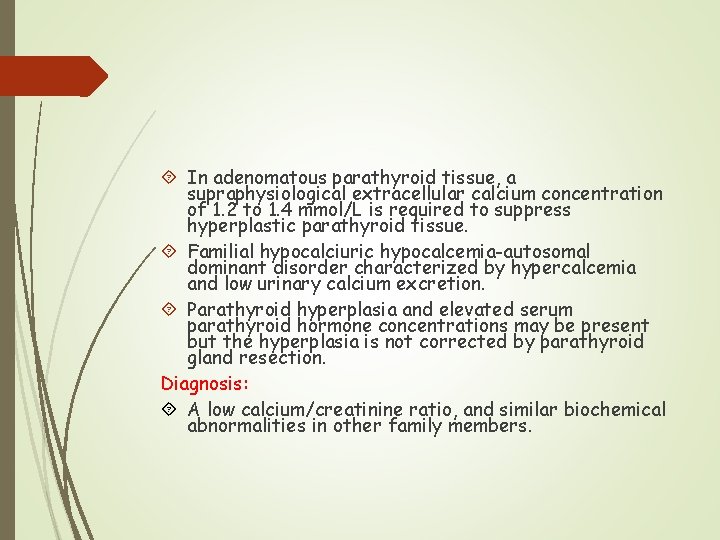
In adenomatous parathyroid tissue, a supraphysiological extracellular calcium concentration of 1. 2 to 1. 4 mmol/L is required to suppress hyperplastic parathyroid tissue. Familial hypocalciuric hypocalcemia-autosomal dominant disorder characterized by hypercalcemia and low urinary calcium excretion. Parathyroid hyperplasia and elevated serum parathyroid hormone concentrations may be present but the hyperplasia is not corrected by parathyroid gland resection. Diagnosis: A low calcium/creatinine ratio, and similar biochemical abnormalities in other family members.

Treatment: Parathyroid surgery with an albumin adjusted serum calcium level higher than 3. 0 mmol/L. Remove three or one half parathyroid glands. PANCREATIC ISLET CELL TUMORS: Neoplasia of the pancreatic islet cells is second manifestations of MEN 1 and occurs in 80% of patients. This cells produce hormonal manifestations and can undergo malignant transformation and metastasis. Treatment: No surgical cure. Improved drugs are used.
Gastrinoma Zollinger-Ellison syndrome is the major cause of morbidity in MEN 1 patients. Increased gastrin production with functional pancreatic tumors. The syndrome includes gastric acid hypersecretion, solitary or multiple peptic ulcers, diarrhoea and elevated gastrin secretion.
Insulinoma Second common pancreatic islet cell tumour. Diagnosis: Demonstrating fasting hypoglycaemia-elevated serum insulin concentration. Treatment: Surgical removal of insulin producing tissue.
Glucogonama: This consists hyperglycemia, anorexia, glossitis, anemia, diarrhoea and venous thrombosis. The watery diarrhoea syndrome: Hypokalema, hypochlorhydria and acidosis in MEN 1 occurs with both pancreatic islet cell and carcinoid tumors. Prolactinoma: This is a pitutary tumor. Third common manifestation of MEN 1. Family screening: Identification of gene carrier. Done by albumin adjusted or ionized serum calcium measurement.
TYPE 2 A MEN The clinical syndrome is described by Sippe and others. Consists of bilateral and multicentric madullary thyroid carcinoma, unilateral or bilateral pheochromocytoma, parathyroid hyperplasia or adenomatosis. Pheochromocytomas are subsequently identified in half of the patients. Parathyroid abnormalities occur in 10 to 20%.
Medullary thyroid carcinoma Multicentric neoplasam of c cell of the thyroid gland. Treatment Surgical removal of all the central lymph nodes. Pheochromocytoma Increased urinary excretion of ephinephrine and norephinephrine in 24 hours urine sample. Diagnosis Computed tomography or magnetic resonance imaging of the abdomen.
Hyperparathyroidism Occurs in 20 -30%. Presence of either parathyroid hyperplasia or multiple parathyroid adenoma. Family screening For medullary thyroid carcinoma-measurement of serum calcitonin levels before and after the intravenous injection of pentagastrin.
TYPE 2 B MEN Definition: The association of medullary thyroid carcinoma and pheochromocytoma with multiple mucosal neuromas. The hallmarks mucosal neuromas on the distal portion of the tongue, on the lips and gastrointestinal tract.
Diagnosis Slit lamp examination Enlarged nerves are noted during neck or abdominal surgery. MIXED TYPE OF MEN The syndromes do not fit in type 1 and 2. Overlap syndromes encompass one or more elements in a single parent.
Overlap syndromes Pitutary and adenomedullary tumors with or without hyperparathyroidism, gastrinoma in MEN 2 A patient. Adenomataous polyposis and MEN 2 B. Posterior pitutary tumor and MEN 1. Prolactinoma in MEN 2 A.
REFERENCES Harrison’s Endocrinology 4 th Edition. 2017, Mc Graw Hill Education, Pages – 390 – 404. Editor – J. Larry Jameson.