Hormonal Regulation of Calcium Balance Part 2 Calcitonin
Hormonal Regulation of Calcium Balance Part 2
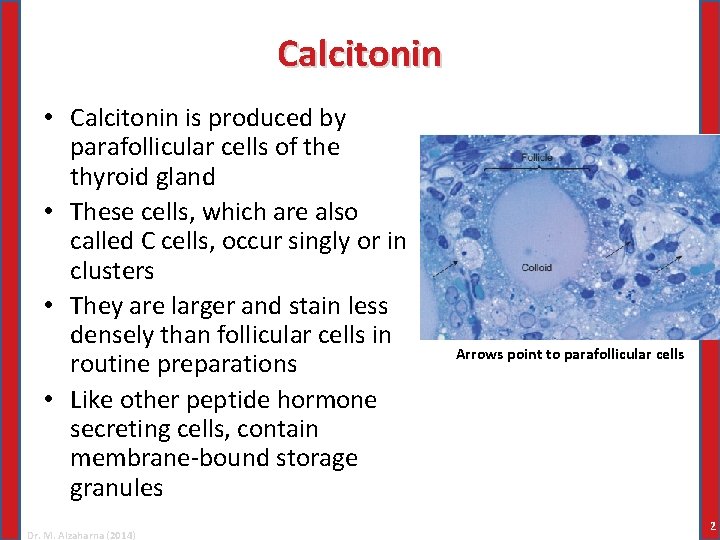
Calcitonin • Calcitonin is produced by parafollicular cells of the thyroid gland • These cells, which are also called C cells, occur singly or in clusters • They are larger and stain less densely than follicular cells in routine preparations • Like other peptide hormone secreting cells, contain membrane-bound storage granules Dr. M. Alzaharna (2014) Arrows point to parafollicular cells 2
Biosynthesis, Secretion, and Metabolism • Calcitonin consists of 32 amino acids • The active hormone has a half-life in plasma of about 5 to 10 minutes and is cleared from the blood primarily by the kidney • The gene that encodes calcitonin also encodes a neuropeptide called calcitonin gene related peptide (CGRP) Dr. M. Alzaharna (2014) 3
Physiological Actions of Calcitonin • No obvious derangement in calcium balance or other homeostatic function results from deficient or excessive production • Thyroidectomy does not produce a tendency toward hypercalcemia, and thyroid tumors that secrete massive amounts of calcitonin do not cause hypocalcemia • Calcitonin quickly and dramatically lowers the blood calcium concentration in many experimental animals • Calcitonin is not a major factor in calcium homeostasis in humans, and does not participate in minute-to minute regulation of blood calcium concentrations • Rather, the importance of calcitonin may be limited to protection against excessive bone resorption Dr. M. Alzaharna (2014) 4
Actions on Bone • Calcitonin lowers blood calcium and phosphate primarily, and perhaps exclusively, by inhibiting osteoclastic activity • Osteoclasts are the principal, and probably only, target cells for calcitonin in bone • Although they express an abundance of receptors for calcitonin, osteoclasts quickly become insensitive to the hormone because continued stimulation results in massive down regulation of receptors Dr. M. Alzaharna (2014) 5
Actions on Kidney • At high concentrations calcitonin may increase urinary excretion of calcium and phosphorus, probably by acting on the proximal tubules • In humans these effects are small, last only a short while, and are not physiologically important for lowering blood calcium • Renal control of calcium is not disrupted in patients with thyroid tumors that secrete large amounts of calcitonin • Kidney cells “escape” from prolonged stimulation with calcitonin and become refractory to it, probably as a result of downregulation of receptors Dr. M. Alzaharna (2014) 6
Regulation of Secretion • Circulating concentrations of calcitonin are quite low when blood calcium is in the normal range or below, but are increased when ionized calcium concentrations is high and exceeds a threshold limit • Parafollicular cells respond directly to ionized calcium in blood and express the same G-protein coupled calcium sensing receptor in their surface membranes as the parathyroid chief cells • Both cell types respond to extracellular calcium over the same concentration range, but their secretory responses are opposite Dr. M. Alzaharna (2014) 7
Regulation of Secretion • In addition to the direct stimulation by high concentrations of calcium, calcitonin secretion may also increase after eating • Gastrin, produced by the gastric mucosa stimulates parafollicular cells to secrete calcitonin • Other gastrointestinal hormones have similar effects, but gastrin is the most potent • Secretion of calcitonin in anticipation of an influx of calcium from the intestine is a feed-forward mechanism that may guard against excessive concentrations of plasma calcium after calcium ingestion by decreasing osteoclastic activity Dr. M. Alzaharna (2014) 8
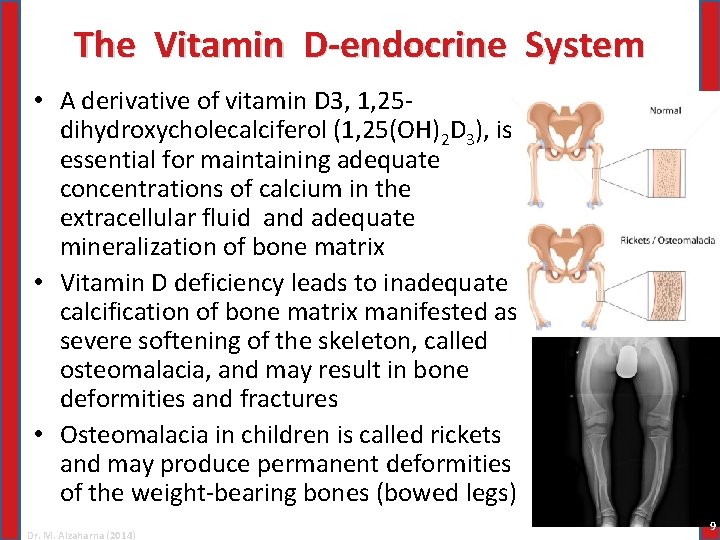
The Vitamin D-endocrine System • A derivative of vitamin D 3, 1, 25 dihydroxycholecalciferol (1, 25(OH)2 D 3), is essential for maintaining adequate concentrations of calcium in the extracellular fluid and adequate mineralization of bone matrix • Vitamin D deficiency leads to inadequate calcification of bone matrix manifested as severe softening of the skeleton, called osteomalacia, and may result in bone deformities and fractures • Osteomalacia in children is called rickets and may produce permanent deformities of the weight-bearing bones (bowed legs) Dr. M. Alzaharna (2014) 9
The Vitamin D-endocrine System • One important distinction between hormones and vitamins is that hormones are synthesized within the body from simple precursors, but vitamins must be provided in the diet • Actually, vitamin D 3 can be synthesized endogenously in humans, but the rate is limited by a nonenzymatic reaction that requires radiant energy in the form of light • The immediate precursor for vitamin D 3 , 7 dehydrocholesterol, is synthesized from acetyl coenzyme A (Co. A) and is stored in skin Dr. M. Alzaharna (2014) 10
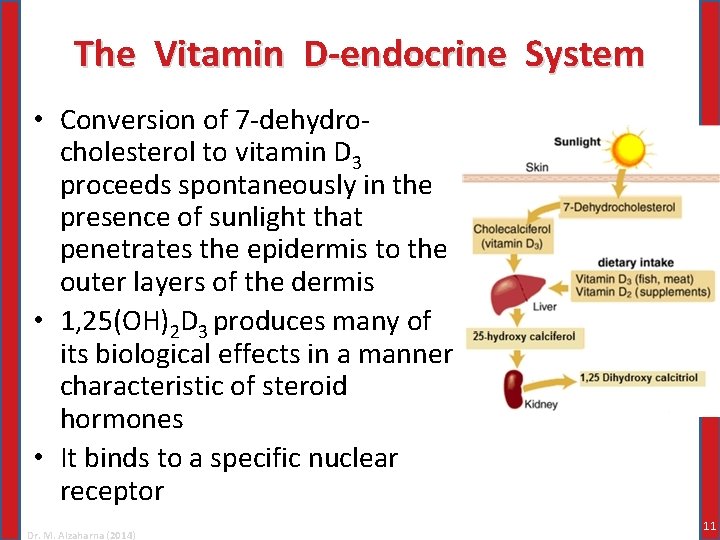
The Vitamin D-endocrine System • Conversion of 7 -dehydrocholesterol to vitamin D 3 proceeds spontaneously in the presence of sunlight that penetrates the epidermis to the outer layers of the dermis • 1, 25(OH)2 D 3 produces many of its biological effects in a manner characteristic of steroid hormones • It binds to a specific nuclear receptor Dr. M. Alzaharna (2014) 11
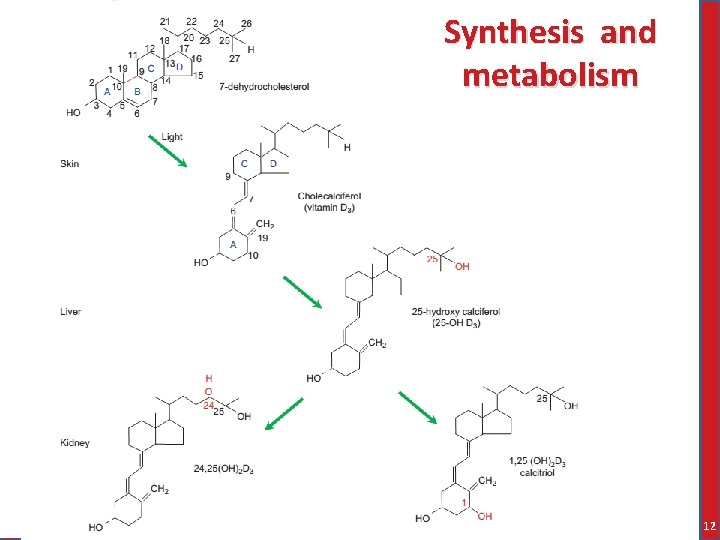
Synthesis and metabolism 12
Physiological Actions of 1, 25(OH)2 D 3 • Overall, the principal physiological actions of 1, 25(OH)2 D 3 increase calcium and phosphate concentrations in extracellular fluid • These effects are exerted primarily on intestine and bone, and to a lesser extent on kidney Dr. M. Alzaharna (2014) 13
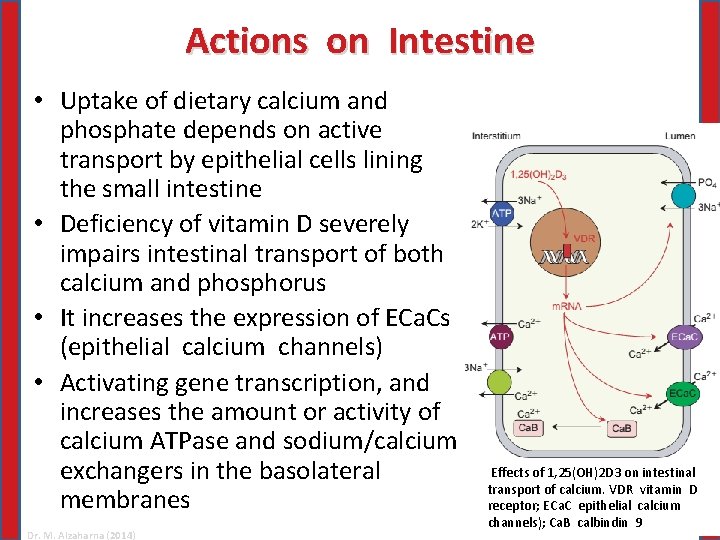
Actions on Intestine • Uptake of dietary calcium and phosphate depends on active transport by epithelial cells lining the small intestine • Deficiency of vitamin D severely impairs intestinal transport of both calcium and phosphorus • It increases the expression of ECa. Cs (epithelial calcium channels) • Activating gene transcription, and increases the amount or activity of calcium ATPase and sodium/calcium exchangers in the basolateral membranes Dr. M. Alzaharna (2014) Effects of 1, 25(OH)2 D 3 on intestinal transport of calcium. VDR vitamin D receptor; ECa. C epithelial calcium channels); Ca. B calbindin 9 14
Actions on Bone • Although the most obvious consequence of vitamin D deficiency is decreased mineralization of bone, 1, 25(OH)2 D 3 is not directly required for bone formation or calcium phosphate deposition in osteoid • Rather, mineralization of osteoid occurs spontaneously when adequate amounts of these ions are available • Ultimately, increased bone mineralization is made possible by increased intestinal absorption of calcium and phosphate • Paradoxically, like PTH, 1, 25(OH)2 D 3 increases both the number and activity of osteoclasts Dr. M. Alzaharna (2014) 15
Actions on Kidney • When given to vitamin D-deficient subjects, 1, 25(OH)2 D 3 increases reabsorption of both calcium and phosphate from the glomerular filtrate • PTH secretion is increased in vitamin D deficiency, and hence tubular reabsorption of phosphate is restricted • Replenishment of 1, 25(OH)2 D 3 decreases the secretion of PTH and thus allows proximal tubular reabsorption of phosphate to increase Dr. M. Alzaharna (2014) 16
Actions on the Parathyroid Glands • The chief cells of the parathyroid glands are physiological targets for 1, 25(OH)2 D 3 and respond to it in a manner that is characteristic of negative feedback • Negative feedback is exerted at the level of synthesis rather than secretion • The promoter region of the PTH gene contains a vitamin D response element Dr. M. Alzaharna (2014) 17
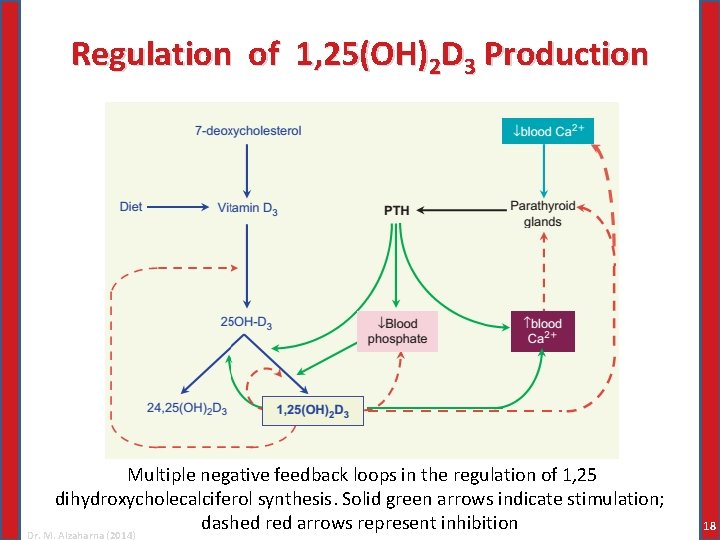
Regulation of 1, 25(OH)2 D 3 Production Multiple negative feedback loops in the regulation of 1, 25 dihydroxycholecalciferol synthesis. Solid green arrows indicate stimulation; dashed red arrows represent inhibition Dr. M. Alzaharna (2014) 18
Regulation of 1, 25(OH)2 D 3 Production • PTH increases synthesis of 1, 25(OH)2 D 3, which exerts a powerful inhibitory effect on PTH gene expression in the parathyroid chief cells • The most important regulatory step in 1, 25(OH)2 D 3 synthesis is the hydroxylation of carbon 1 by cells in the proximal tubules of the kidney • In the absence of PTH, the concentration of 1 α-hydroxylase in renal cells quickly falls • PTH regulates transcription of the gene that codes for the 1 α-hydroxylase Dr. M. Alzaharna (2014) 19
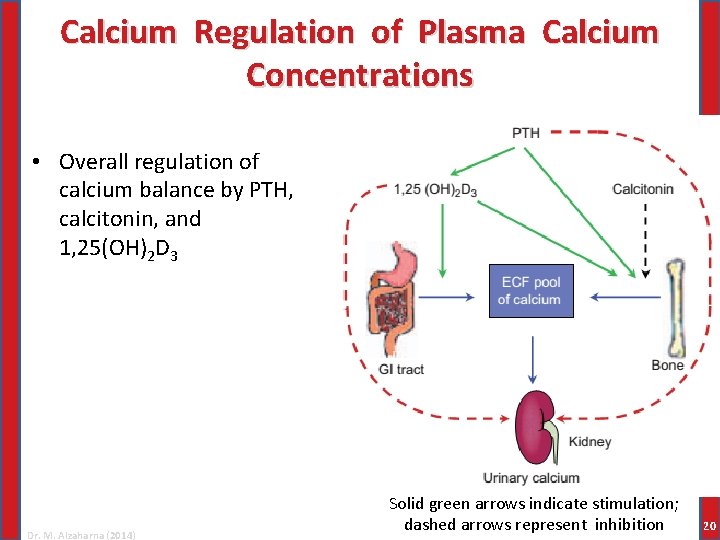
Calcium Regulation of Plasma Calcium Concentrations • Overall regulation of calcium balance by PTH, calcitonin, and 1, 25(OH)2 D 3 Dr. M. Alzaharna (2014) Solid green arrows indicate stimulation; dashed arrows represent inhibition 20
Integrated Actions of Calcitropic Hormones • Response to a hypocalcemic challenge: – Because some calcium is always lost in urine, even a short period of total fasting can produce a mild hypocalcemic challenge – More severe challenges are produced by a diet deficient in calcium or anything that might interfere with calcium absorption by renal tubules or the intestine – The parathyroid glands are delicately sensitive to even a small decrease in ionized calcium and promptly increase PTH secretion Dr. M. Alzaharna (2014) 21
Integrated Actions of Calcitropic Hormones – The first line of defense against a hypocalcemic challenge is: • Effects of PTH on calcium reabsorption from the glomerular filtrate coupled with some calcium mobilization from bone – After about 12 to 24 hours, increased formation of 1, 25(OH)2 D 3 increases the efficiency of calcium absorption from the gut – Osteoclastic bone resorption in response to both PTH and 1, 25(OH)2 D 3 affect vast reserves of calcium in the skeleton – If calcium intake remains inadequate, skeletal integrity may be sacrificed in favor of maintaining blood calcium concentrations Dr. M. Alzaharna (2014) 22
Response to a Hypercalcemic Challenge • Hypercalcemia is rarely seen under normal physiological circumstances, but it may be a complication of a variety of pathological conditions usually accompanied by increased blood concentrations of PTH or PTHrp • Although some calcium phosphate may crystallize in demineralized osteoid, renal loss of calcium is the principal means of lowering blood calcium • The rate of renal loss by PTH sensitive mechanisms, however, is limited to only about 10% of the calcium present in the glomerular filtrate • Decreased reabsorption of calcium in the ascending limb triggered by the calcium sensing receptor, however, would quickly facilitate further calcium excretion Dr. M. Alzaharna (2014) 23
Other Hormones That Influence Calcium Balance • Many other endocrine and paracrine factors influence calcium balance • Most of the calcium reabsorbed from the glomerular filtrate is by passive processes driven by active reabsorption of sodium • Therefore, renal conservation of calcium is intimately related to sodium balance • Adjustments of sodium reabsorption are accompanied by changes in renal calcium reabsorption Dr. M. Alzaharna (2014) 24
Other Hormones That Influence Calcium Balance • For example, volume expansion results in increased glomerular filtration and decreased sodium reabsorption in the proximal tubule • The proximal tubule accounts for the bulk of the calcium reabsorbed, and hence even small changes at this level can result insignificant calcium loss • Volume contraction secondarily increases calcium reabsorption through increased reabsorption of sodium and water resulting from increased production of angiotensin II and ADH Dr. M. Alzaharna (2014) 25
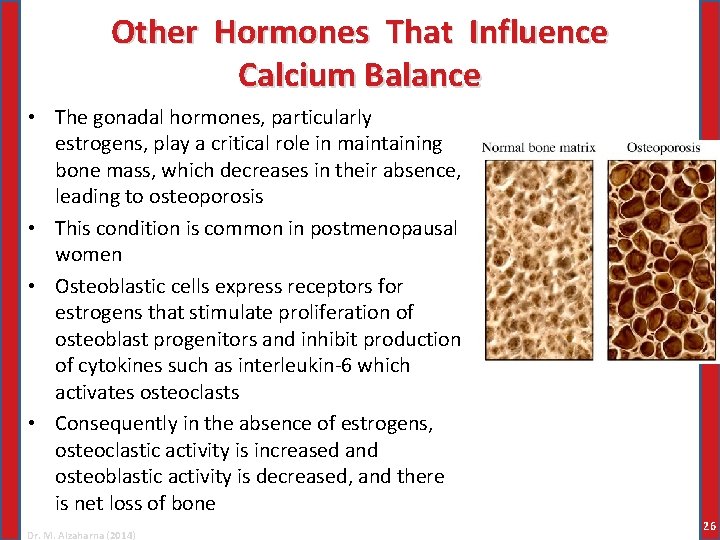
Other Hormones That Influence Calcium Balance • The gonadal hormones, particularly estrogens, play a critical role in maintaining bone mass, which decreases in their absence, leading to osteoporosis • This condition is common in postmenopausal women • Osteoblastic cells express receptors for estrogens that stimulate proliferation of osteoblast progenitors and inhibit production of cytokines such as interleukin-6 which activates osteoclasts • Consequently in the absence of estrogens, osteoclastic activity is increased and osteoblastic activity is decreased, and there is net loss of bone Dr. M. Alzaharna (2014) 26
Other Hormones That Influence Calcium Balance • Excessive thyroid hormone accelerates activity of both the osteoclasts and osteoblasts and often results in net bone resorption and a decrease in bone density • Excessive glucocorticoid concentrations also decrease skeletal mass by increasing PTH synthesis and secretion Dr. M. Alzaharna (2014) 27
HYPERCALCEMIA & HYPOCALCEMIA 28
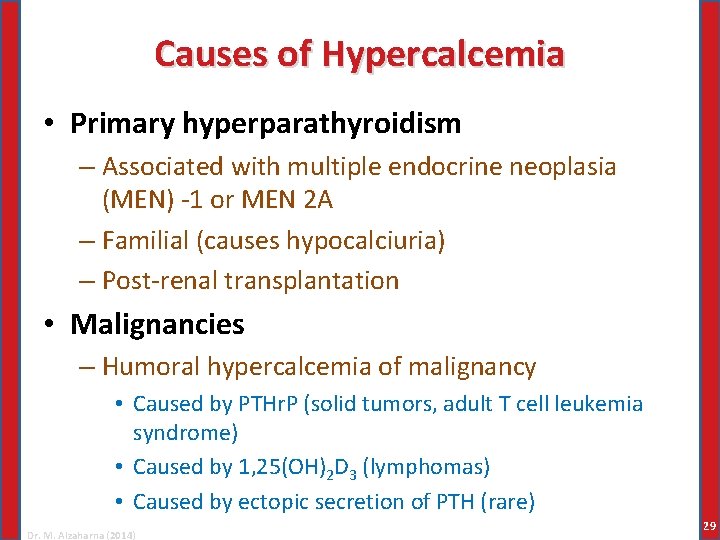
Causes of Hypercalcemia • Primary hyperparathyroidism – Associated with multiple endocrine neoplasia (MEN) -1 or MEN 2 A – Familial (causes hypocalciuria) – Post-renal transplantation • Malignancies – Humoral hypercalcemia of malignancy • Caused by PTHr. P (solid tumors, adult T cell leukemia syndrome) • Caused by 1, 25(OH)2 D 3 (lymphomas) • Caused by ectopic secretion of PTH (rare) Dr. M. Alzaharna (2014) 29
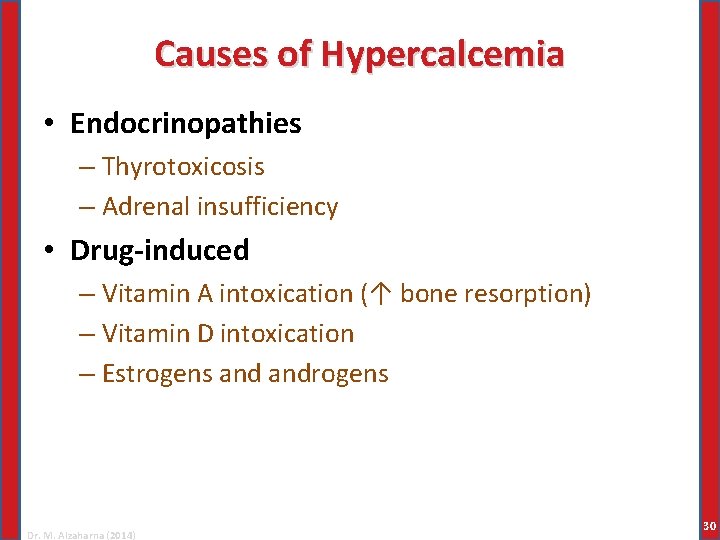
Causes of Hypercalcemia • Endocrinopathies – Thyrotoxicosis – Adrenal insufficiency • Drug-induced – Vitamin A intoxication (↑ bone resorption) – Vitamin D intoxication – Estrogens androgens Dr. M. Alzaharna (2014) 30
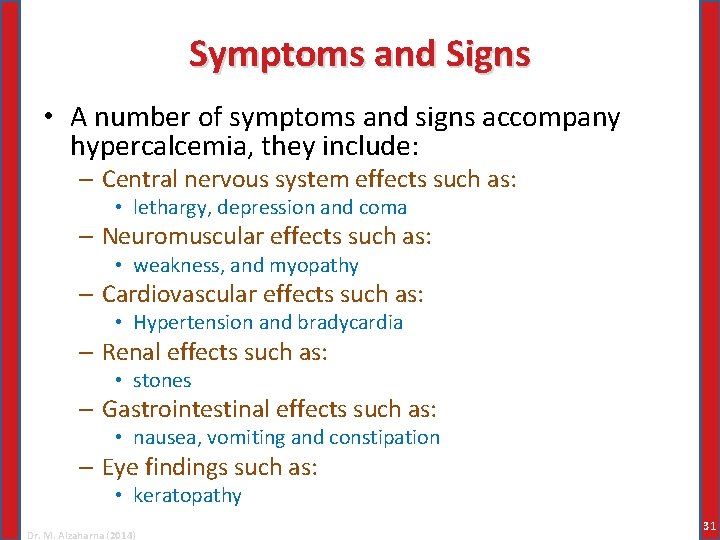
Symptoms and Signs • A number of symptoms and signs accompany hypercalcemia, they include: – Central nervous system effects such as: • lethargy, depression and coma – Neuromuscular effects such as: • weakness, and myopathy – Cardiovascular effects such as: • Hypertension and bradycardia – Renal effects such as: • stones – Gastrointestinal effects such as: • nausea, vomiting and constipation – Eye findings such as: • keratopathy Dr. M. Alzaharna (2014) 31
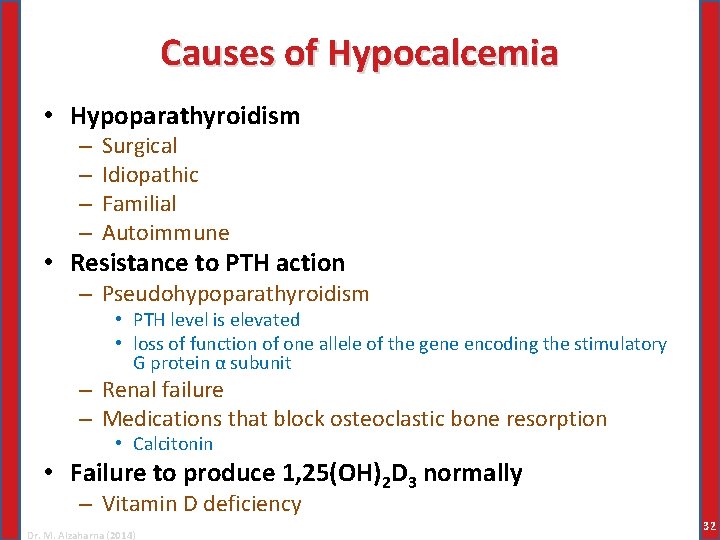
Causes of Hypocalcemia • Hypoparathyroidism – – Surgical Idiopathic Familial Autoimmune • Resistance to PTH action – Pseudohypoparathyroidism • PTH level is elevated • loss of function of one allele of the gene encoding the stimulatory G protein α subunit – Renal failure – Medications that block osteoclastic bone resorption • Calcitonin • Failure to produce 1, 25(OH)2 D 3 normally – Vitamin D deficiency Dr. M. Alzaharna (2014) 32
Causes of Hypocalcemia • Acute complexation or deposition of calcium – Acute hyperphosphatemia – Acute pancreatitis – Citrated blood transfusion • complexation of calcium as calcium citrate – Rapid, excessive skeletal mineralization • Osteoblastic metastasis • Vitamin D therapy for vitamin D deficiency Dr. M. Alzaharna (2014) 33
Symptoms & Signs • Chronic moderate hypocalcemia may be completely asymptomatic • Acute hypocalcemia causes: – Increased neuromuscular irritability – The clinical manifestation is tetany – Milder forms of neuromuscular irritability is numbness of the fingertips – Prolonged contraction of the respiratory muscles causes cyanosis Dr. M. Alzaharna (2014) 34
- Slides: 34