HORMONAL METHODS OF CONTRACEPTION Created By Jason Barber

HORMONAL METHODS OF CONTRACEPTION Created By: Jason Barber, Laureen Watanabe, Sean Barnett, Tiare Palimoo

Types of Hormonal Methods Oral Contraceptives (Pills) Injection: Depo-Provera Contraceptive Patch: Ortho-Evra Contraceptive Implants: Implanon Vaginal Ring: Nuva. Ring Intrauterine Device (IUD)

Oral Contraceptives (Pills) Method of action: � Most common is the Combination Oral Contraceptive form (COC) – provides a constant elevated level of synthetic estrogen and progesterone (progestin) � Inhibits the pituitary release of follicle stimulating hormone (FSH) and luteinizing hormone (LH) � Result = no maturation or ovulation of egg along with uterine wall thinning and increased cervical mucus; preventing sperm reaching the egg

Other Oral Contraceptives Emergency Contraceptive Pills (ECPs): AKA The Morning After Pill 1. Plan B One Step - high dose progestinonly; stops release of egg and implantation; taken within 72 hours of unprotected sex; available OTC for 17+ years of age 2. Next Choice - higher level of progestin; two pills (one taken within 72 hours; second one 12 hours after first) 3. Higher dose - increased dose of regular (COC) oral birth control pills

Other Oral Contraceptives Cont. Mini Pill: � Progestin-only Pills (POPs) � Thickens cervical mucus and thins uterus lining – preventing sperm from reaching egg � Brand names: Micronor, Nora-BE, and Nor. QD � Prescription only � Taken daily

Oral Contraceptives (Pills) Instruction of use: � Most commonly taken daily: usually on a cycle of 3 weeks of active pills followed by 7 days of placebo pills. 3 Stages of Initiation: 1. Quick start - taking the first pill the same day as the clinical appointment, while using backup method for 7 days. 2. First day start - taking the first pill on the first day of the menstrual cycle (menses) 3. Sunday start - start the first pill on the first Sunday after the start of their menstrual period
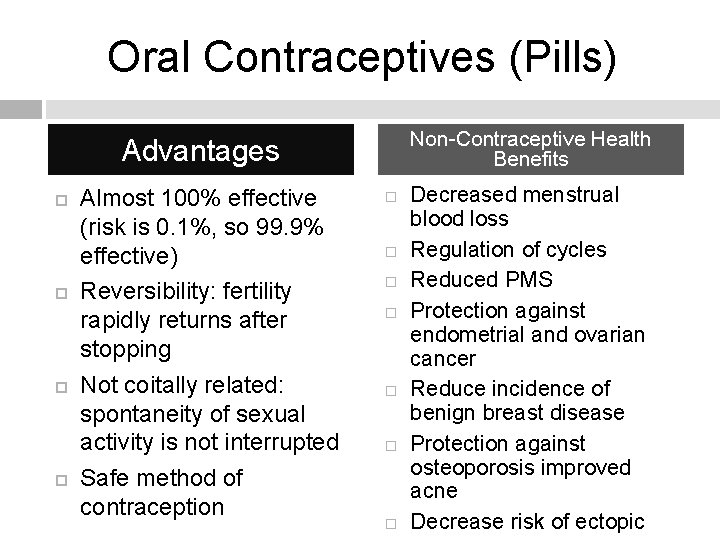
Oral Contraceptives (Pills) Non-Contraceptive Health Benefits Advantages Almost 100% effective (risk is 0. 1%, so 99. 9% effective) Reversibility: fertility rapidly returns after stopping Not coitally related: spontaneity of sexual activity is not interrupted Safe method of contraception Decreased menstrual blood loss Regulation of cycles Reduced PMS Protection against endometrial and ovarian cancer Reduce incidence of benign breast disease Protection against osteoporosis improved acne Decrease risk of ectopic

Oral Contraceptives (Pills) Disadvantages Pregnancy risk increases to 8% with missing one day of oral contraceptive No protection against STD/STIs Increased risk of cardiovascular disease Higher cost if not covered with insurance Having to remember to take the pill every day Adverse Effects/Side Effects Nausea and vomiting Menstrual spotting Headaches Depression Decreased libido Increased risk of gallstones Cigarette smoking while taking oral contraceptives increases the risk of: heart attacks, blood clots, and strokes (higher risk for women over 35 and heavy smokers of 15 or more

Oral Contraceptives (Pills) How much does Oral Contraceptives cost? � According to Planned Parenthood: Doctor’s visit: $35 - $250 depending on with or without insurance Cost per month: $15 - $50
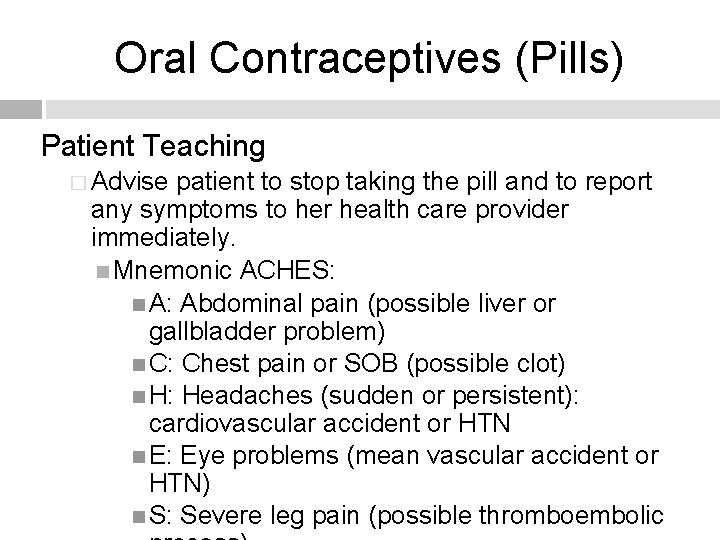
Oral Contraceptives (Pills) Patient Teaching � Advise patient to stop taking the pill and to report any symptoms to her health care provider immediately. Mnemonic ACHES: A: Abdominal pain (possible liver or gallbladder problem) C: Chest pain or SOB (possible clot) H: Headaches (sudden or persistent): cardiovascular accident or HTN E: Eye problems (mean vascular accident or HTN) S: Severe leg pain (possible thromboembolic
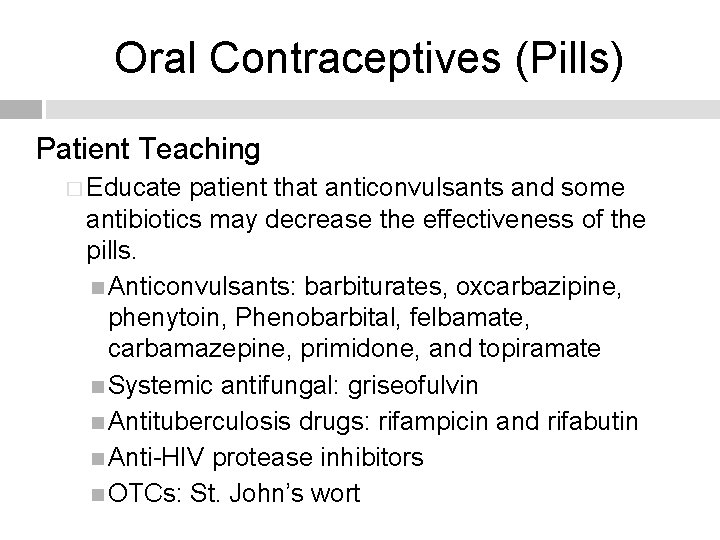
Oral Contraceptives (Pills) Patient Teaching � Educate patient that anticonvulsants and some antibiotics may decrease the effectiveness of the pills. Anticonvulsants: barbiturates, oxcarbazipine, phenytoin, Phenobarbital, felbamate, carbamazepine, primidone, and topiramate Systemic antifungal: griseofulvin Antituberculosis drugs: rifampicin and rifabutin Anti-HIV protease inhibitors OTCs: St. John’s wort
Oral Contraceptives (Pills) Patient Teaching � Educate the patient on the importance of taking pills daily at the same time. Suggestions: set an alarm or make it part of something the patient does already, like brushing teeth before bed. If a pill is missed: The patient should take it as soon as she remember. The next pill should be taken at the correct time. If the patient realize when taking a pill that one was skipped, the skipped pill must be taken

Injection: Depo-Provera What is the birth control injection? � Brand name: Depo-Provera � Injection of depot medroxyprogesterone acetate (DMPA) � Administered by a needle in the muscle of the arm or buttocks every 11 – 13 weeks � Provides protection against pregnancy for 3 months
Injection: Depo-Provera What is the birth control injection? � It is 99. 7% effective in preventing pregnancy Less than 1 out of 100 women will get pregnant each year if they always use the birth control shot as directed About 6 out of 100 women will get pregnant each year if they don’t always use the birth control shot as directed � Recommended for people who are unable to take other contraceptive methods � Not recommended for those with unexplained vaginal bleeding, breast cancer, liver disease, a history of blood-clotting problems, and risk factors

Injection: Depo-Provera How does the injection work? � Type of progestin � It works by stopping your ovaries from releasing an egg every month (ovulation) Pregnancy cannot happen if there is no egg to join the sperm � Thins the lining of the uterus Keeps sperm from getting to the eggs
Injection: Depo-Provera Instruction of use: � Injections are administered by the health care provider � First one is given within the first 5 days after the start of your menstrual periods � Becomes fully effective 24 hours after the injection � You must get the injection on time � Health care provider should avoid massaging injection site following administration to avoid accelerating medication absorption, which will shorten the duration of its effectiveness.

Injection: Depo-Provera Disadvantages Advantages Only have to think about it 4 times a year No daily pill to remember Reversible 50% of women will stop having periods all together within the first year of starting Decrease the risk of endometrial cancer Decrease the frequency of menstrual migraines Can be used while breastfeeding Decrease in bone density Can prolong amenorrhea Irregular bleeding during the first 6 -9 months of use Increases the risk of thromboembolism Weight gain Hair loss Headaches Nausea Weakness or fatigue
Injection: Depo-Provera How much does an injection cost? � Prescription is required � If an exam is needed, it may cost $35 - $250 � The cost per injection (lasts about 3 months) is about $35 - $100 � Medicaid or other state programs may lower the costs

Injection: Depo-Provera Patient Teaching � Advise patient to keep follow-up appointments. � Educate patient on the importance of maintaining an adequate intake of calcium and vitamin D. � Counsel patient about including exercise in their daily routine. � Inform patient that Depo-Provera is not a good birth control method if she’s thinking of getting pregnant soon. It can take anywhere from 6 – 10 months after getting last shot to become pregnant.
Injection: Depo-Provera Patient Teaching � Instruct patient to report any signs to the health care provider immediately: A new lump in the breast Major depression Migraine with aura – seeing bright, flashing zigzags, usually before a very bad headache Pus, pain for many days, or bleeding where the shot was given Unusually heavy or prolonged vaginal bleeding Yellowing of the skin or eyes
Contraceptive Patch What is the Patch? Small, beige, square-shaped patch Applied to skin Once-per-week application Contains norelgestromin (progesterone) and ethinyl estradiol (estrogen) (i. e. , Ortho Evra) Delivered into bloodstream through the skin

Contraceptive Patch How does it work? � Delivers continuous levels of progestin and estrogen � Prevents ovulation � Thickens the cervical mucus � Prevents pregnancy the same way as the birth control pill and other methods of hormonal contraception (99% effective when used correctly)
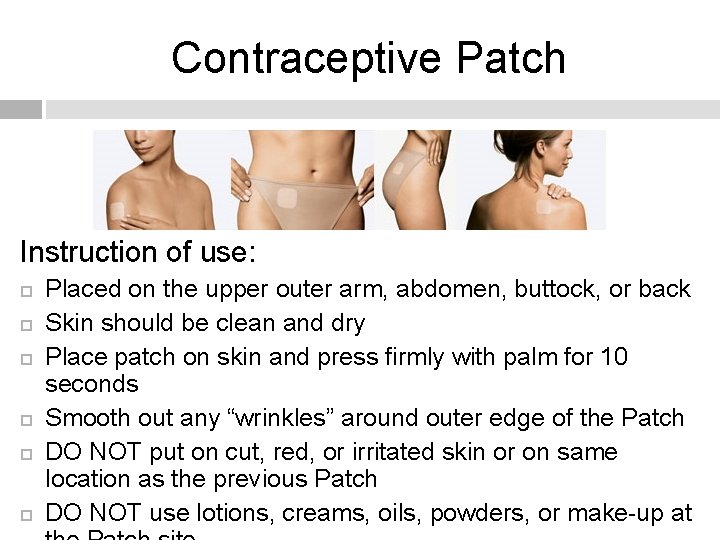
Contraceptive Patch Instruction of use: Placed on the upper outer arm, abdomen, buttock, or back Skin should be clean and dry Place patch on skin and press firmly with palm for 10 seconds Smooth out any “wrinkles” around outer edge of the Patch DO NOT put on cut, red, or irritated skin or on same location as the previous Patch DO NOT use lotions, creams, oils, powders, or make-up at
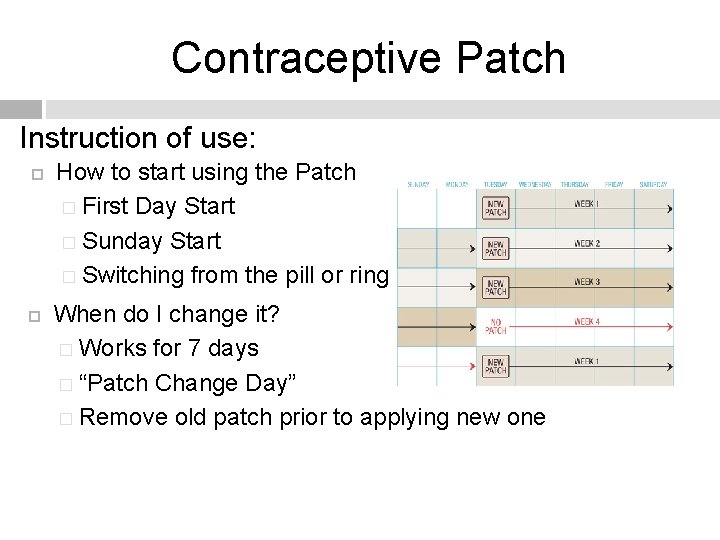
Contraceptive Patch Instruction of use: How to start using the Patch � First Day Start � Sunday Start � Switching from the pill or ring When do I change it? � Works for 7 days � “Patch Change Day” � Remove old patch prior to applying new one
Contraceptive Patch Disadvantages Advantages Convenient 99% effective Maintains consistent level of hormones Decreases risk of missing a dose More likely to use it consistently and correctly than those who use birth control pills Does not protect against STIs Skin reaction may occur from patch application Side effects: pain tenderness, and swelling in the breasts, headache, nausea, bleeding between periods Adverse effects: blood clots, stroke, heart attacks (greater risk if cigarette smoker and over the age of 35) May be less effective for women heavier than 198 lbs (90 kg) Certain medications and supplements make it less effective

Contraceptive Patch How do I get a Patch? � Available by prescription only by doctor What is the cost of the patch? � Medical exam: $35 - $250 � Patch: approximately $15 - $80/month � Covered by most major health insurance companies � Access 2 wellness
Contraceptive Patch Patient Teaching � Encourage the importance of consulting with a doctor when considering a new medication to fully understand risks and benefits and other possible options that are available � Have patient notify their doctor of all the medications (OTC and Rx) they are currently taking � Teach patient the proper way of applying the Patch � Provide a list of helpful ways to remember their “Patch Change Day” � Ensure patient is aware of the side effects and how to recognize adverse reactions and to seek medical
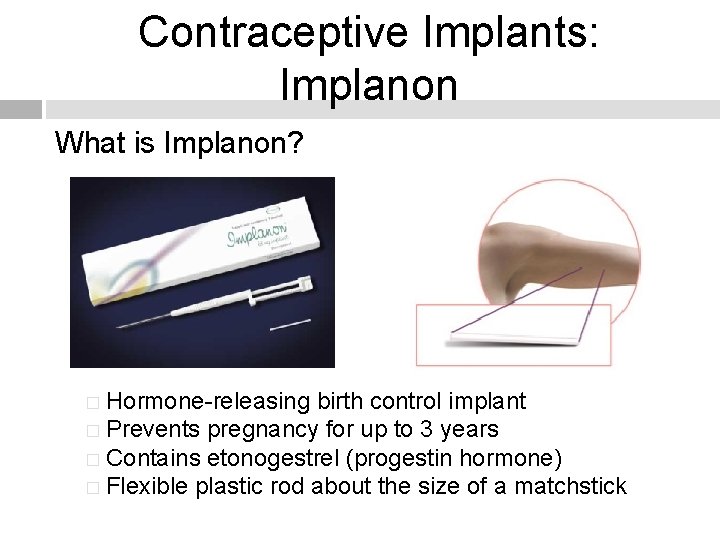
Contraceptive Implants: Implanon What is Implanon? � Hormone-releasing birth control implant � Prevents pregnancy for up to 3 years � Contains etonogestrel (progestin hormone) � Flexible plastic rod about the size of a matchstick
Contraceptive Implants: Implanon How does it work? � Prevents pregnancy by stopping release of an egg from the ovary � Thickens the cervical mucus to prevent the sperm from reaching the egg How is it inserted? � Your healthcare provider will insert the implant under the skin on the inner side of your upper arm � http: //www. youtube. com/watch? v=Wrl. N 6 UR_Dck
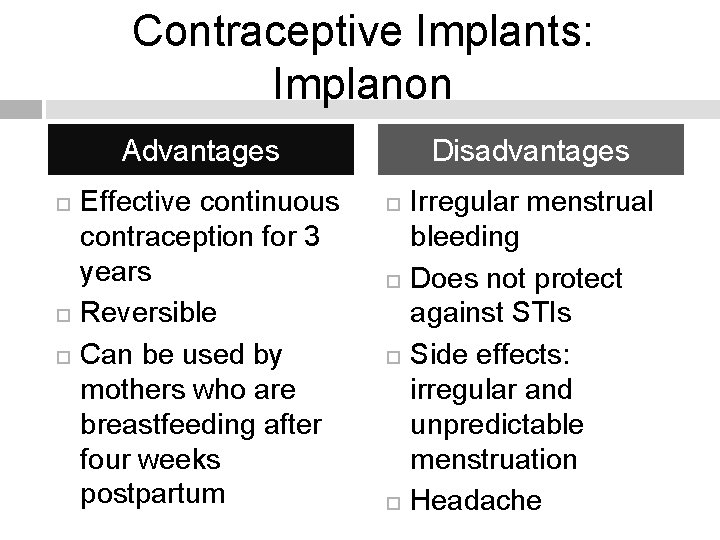
Contraceptive Implants: Implanon Disadvantages Advantages Effective continuous contraception for 3 years Reversible Can be used by mothers who are breastfeeding after four weeks postpartum Irregular menstrual bleeding Does not protect against STIs Side effects: irregular and unpredictable menstruation Headache
Contraceptive Implants: Implanon How much does it cost? � Exam, implant, and insertion: $400 - $800 � Removal: $100 - $300 � Total cost pays for pregnancy protection up to three years
Contraceptive Implants: Implanon Patient Teaching � Advise patient to avoid trauma to the area of implantation. � Teach patients the adverse side effects to be aware of and to notify their health care provider immediately � The implant must be removed if patient becomes pregnant or is diagnosed with breast cancer

Vaginal Ring: Nuva. Ring What is Nuva. Ring? � Flexible, plastic combined contraceptive vaginal ring � Contains a combination of a progestin and estrogen The hormones work by: keeping eggs from leaving the ovaries and making cervical mucus thicker
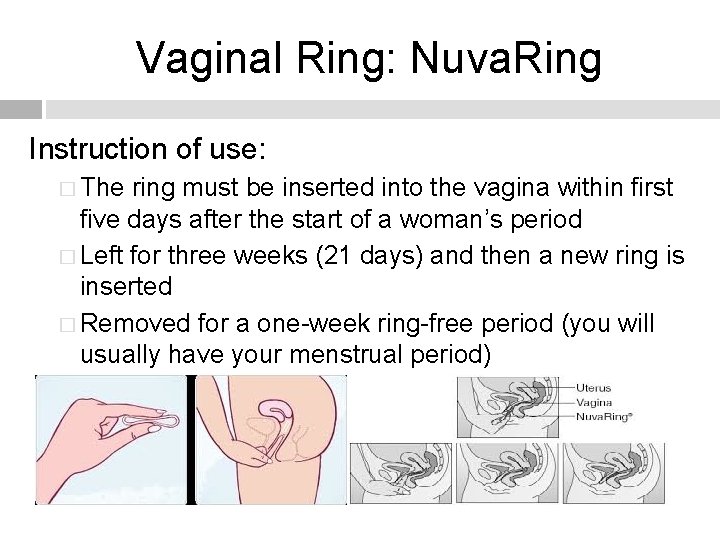
Vaginal Ring: Nuva. Ring Instruction of use: � The ring must be inserted into the vagina within first five days after the start of a woman’s period � Left for three weeks (21 days) and then a new ring is inserted � Removed for a one-week ring-free period (you will usually have your menstrual period)
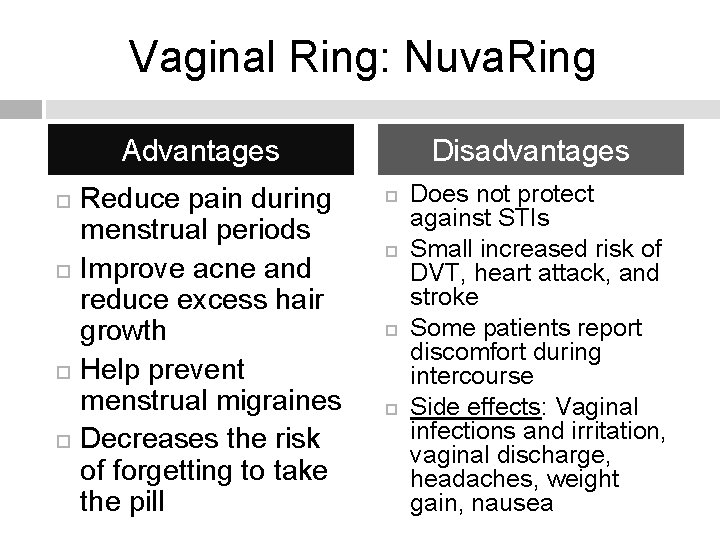
Vaginal Ring: Nuva. Ring Disadvantages Advantages Reduce pain during menstrual periods Improve acne and reduce excess hair growth Help prevent menstrual migraines Decreases the risk of forgetting to take the pill Does not protect against STIs Small increased risk of DVT, heart attack, and stroke Some patients report discomfort during intercourse Side effects: Vaginal infections and irritation, vaginal discharge, headaches, weight gain, nausea
Vaginal Ring: Nuva. Ring How much does the Nuva. Ring cost? � If exam is needed, exam costs $35 to $250 � Costs for ring: about $15 - $80 per month � May be purchased with a prescription at a drugstore or clinic
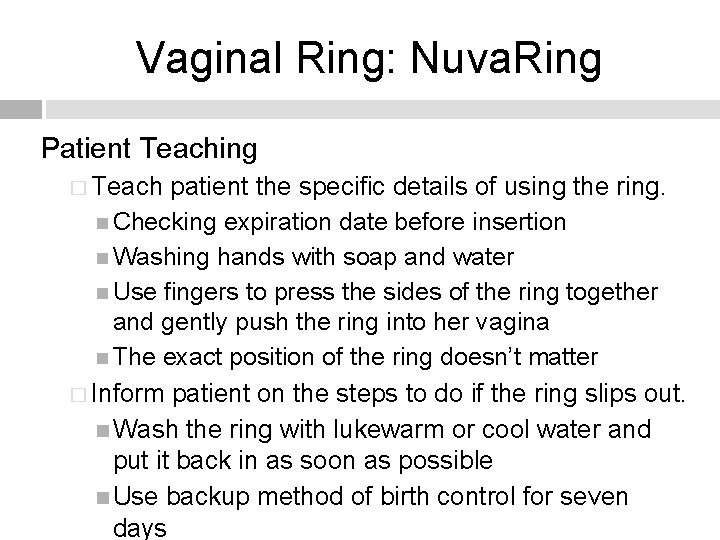
Vaginal Ring: Nuva. Ring Patient Teaching � Teach patient the specific details of using the ring. Checking expiration date before insertion Washing hands with soap and water Use fingers to press the sides of the ring together and gently push the ring into her vagina The exact position of the ring doesn’t matter � Inform patient on the steps to do if the ring slips out. Wash the ring with lukewarm or cool water and put it back in as soon as possible Use backup method of birth control for seven days
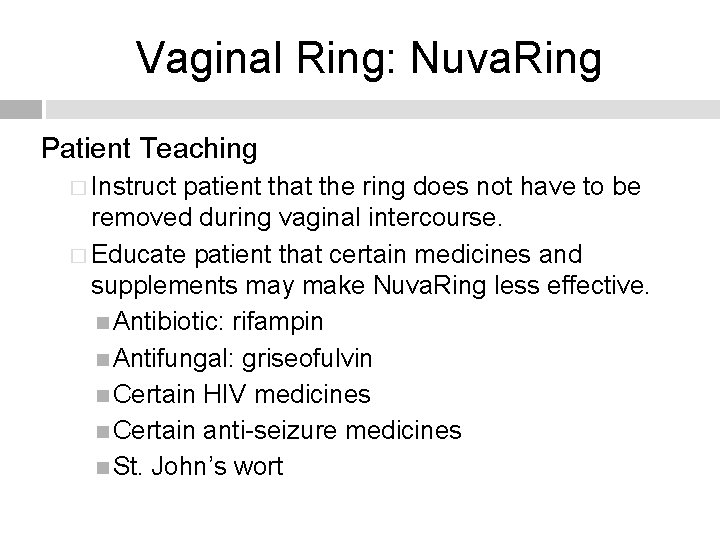
Vaginal Ring: Nuva. Ring Patient Teaching � Instruct patient that the ring does not have to be removed during vaginal intercourse. � Educate patient that certain medicines and supplements may make Nuva. Ring less effective. Antibiotic: rifampin Antifungal: griseofulvin Certain HIV medicines Certain anti-seizure medicines St. John’s wort
Intrauterine Device (IUD) What is an IUD? � Small, “T-shaped” device � Made of flexible plastic � Two types: copper (Para. Gard) and hormonal (Mirena or Skyla) � Hormonal IUD releases a small amount of progestin � Effective for 3 to 5 years � Less than 1 out of 100 women will get pregnant each year if they use an IUD
Intrauterine Device (IUD) The process of placement: � IUD must be fitted � Usually done towards the end of a period or shortly afterwards � Vaginal examination is performed � A small instrument is passed into your uterus to check its size and position where the IUD is then placed
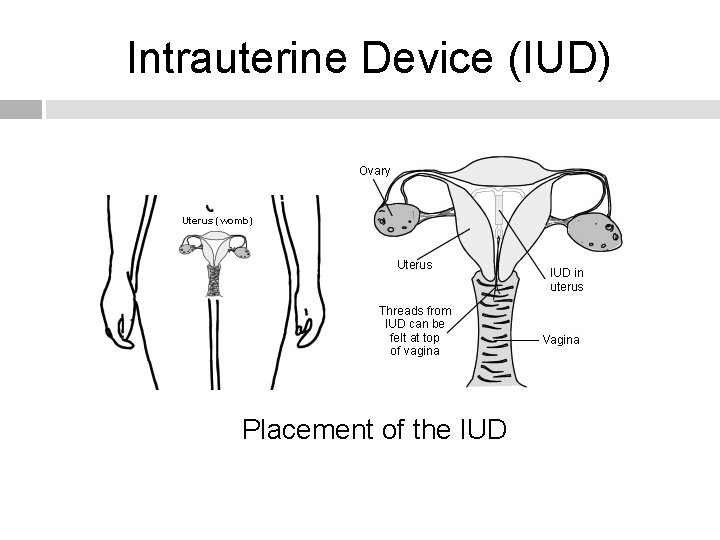
Intrauterine Device (IUD) Placement of the IUD
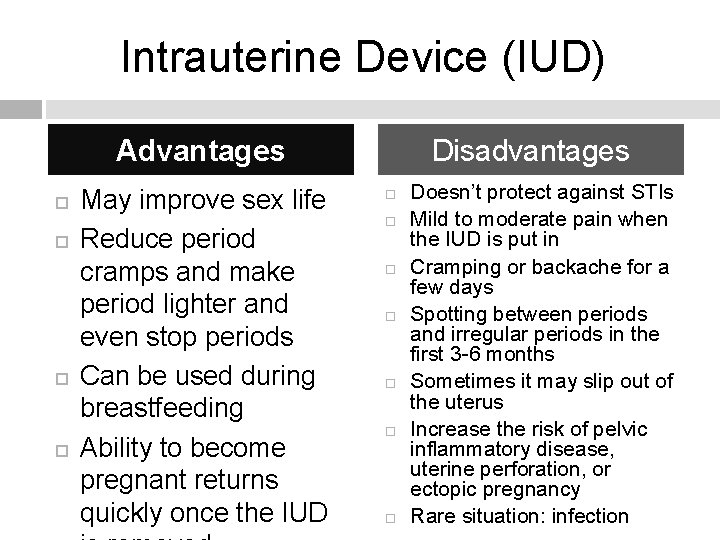
Intrauterine Device (IUD) Disadvantages Advantages May improve sex life Reduce period cramps and make period lighter and even stop periods Can be used during breastfeeding Ability to become pregnant returns quickly once the IUD Doesn’t protect against STIs Mild to moderate pain when the IUD is put in Cramping or backache for a few days Spotting between periods and irregular periods in the first 3 -6 months Sometimes it may slip out of the uterus Increase the risk of pelvic inflammatory disease, uterine perforation, or ectopic pregnancy Rare situation: infection
Intrauterine Device (IUD) How much does an IUD cost? � Most inexpensive long-term and reversible form of birth control � Only cost money in the beginning � The cost for the medical exam, the IUD, the insertion of the IUD, and follow-up visits can range from $500 to $1000 � The cost pays for protection that can last from 5 to 12 years
Intrauterine Device (IUD) Patient Teaching � Instruct patient it is common to feel some cramping and mild discomfort after the insertion of the IUD. Pain medication can be taken. � Advise patient to schedule a checkup after her first period. � Teach patient to check for the presence of the IUD strings after menstruation to rule out explosion of the device. Wash hands and either sit or squat down Put index or middle finger up into vagina until the cervix is felt (cervix will feel firm and somewhat rubbery) Feel the string ends that should be coming through.
Intrauterine Device (IUD) Patient Teaching � Teach patient to report to the primary care provider: late or abnormal spotting or bleeding, abdominal pain or pain with intercourse, abnormal or foul-smelling vaginal discharge, fever, chills, a change in string length, or if IUD cannot be located or is located outside of the cervix or in the vagina.
Lets See What You Remembered! 1. What is the percent (%) chance of getting pregnant while on birth control pills? 2. What is one disadvantage of getting the Depo. Provera shot? 3. Implanon provides continuous contraception for up to how many years? 4. What is the most inexpensive long-term contraception to use?
REFERENCES Janssen Pharmaceuticals, Inc. Orthro Evra. (2013). Retrieved from http: //www. orthoevra. com/index. html Lowdermilk, D. & Perry S. (2010). Maternity & Women’s Health Care (8 th ed. ). St. Louis: Mosby. Merck & Co. , Inc. Implanon. (2012). Retrieved from http: //www. implanonusa. com/en/ consumer/index. asp Planned parenthood Federation of America. Planned Parenthood. (2013). Retrieved from http: //www. plannedparenthood. org
- Slides: 48