Honors Anatomy Physiology INTEGUMENTARY SYSTEM ESSENTIAL QUESTION What





































- Slides: 110

Honors Anatomy & Physiology INTEGUMENTARY SYSTEM
ESSENTIAL QUESTION � What body? are the ways skin protects the
INTEGUMENTARY SYSTEM � functions: 1. 2. 3. 4. 5. 6. protecting the body helping to regulate body temperature allows you to sense stimuli in your environment stores blood synthesis of vit. D excretion & absorption of materials
STRUCTURE OF THE SKIN � skin = cutaneous membrane � largest organ of body � in � 2 1. 2. 3. adults: covers ~ 2 m² & weighs ~ 4. 5 – 5 kg (10 – 11 lb) parts: epidermis sub Q below dermis & not technically part of skin: contains fat (insulation), & blood vessels, nerves that supply the skin
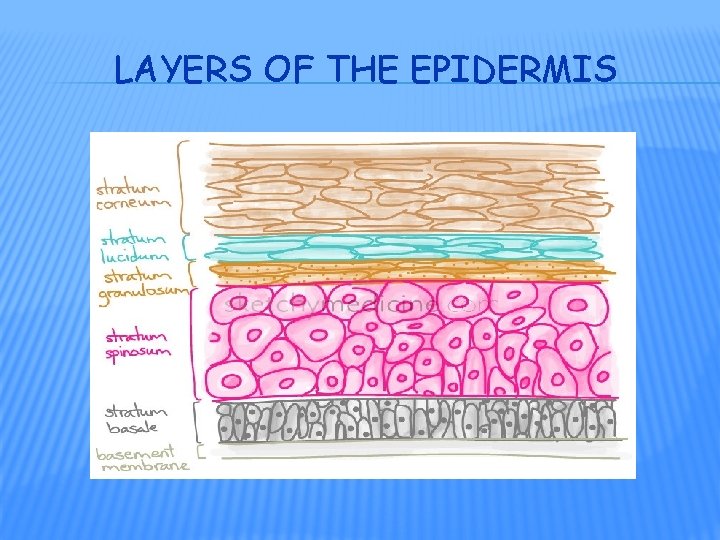
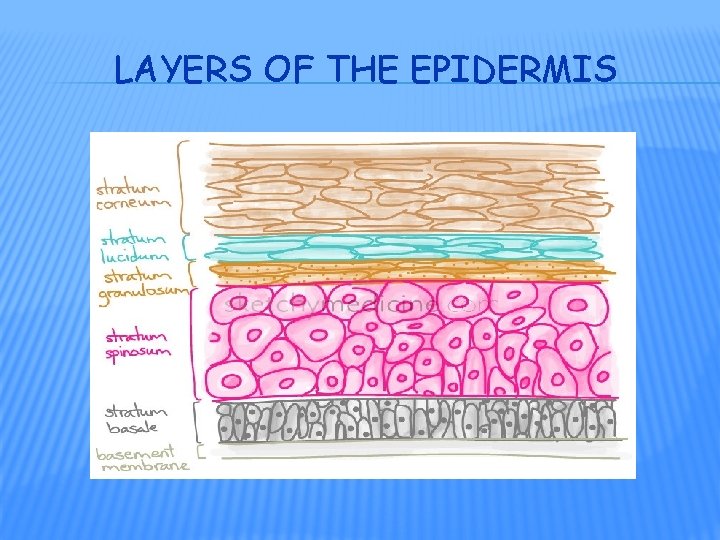
LAYERS OF THE EPIDERMIS
EPIDERMIS � keratinzed stratified squamous epithelium � 4 main cell types: 1. keratinocytes 2. melanocytes 3. Langerhans cells 4. Merkel cells
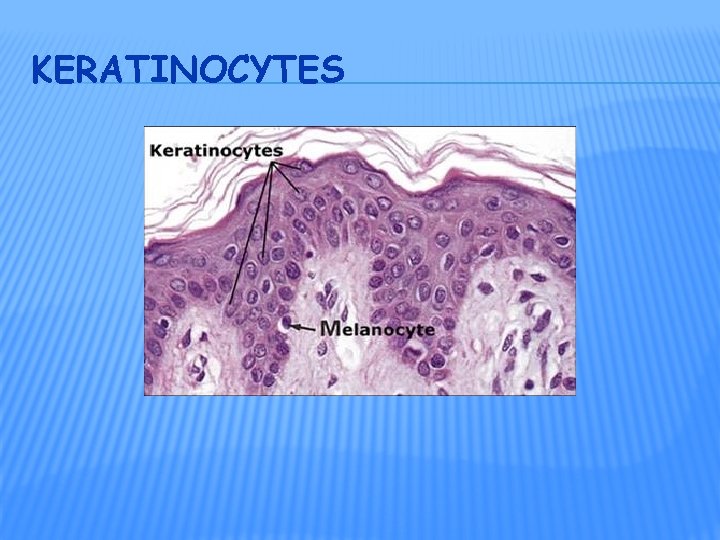
KERATINOCYTES �~ 90% of all epidermal cells � produce fibrous protein: keratin: � protects � heat skin & underlying tissue from � microbes � chemicals � also release a water-repellant sealant from lamellar granules � decreases water entry/loss � inhibits entry of foreign materials
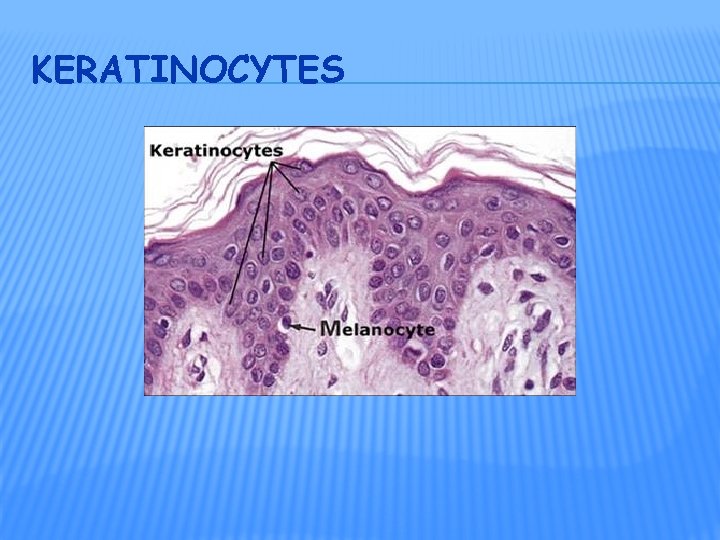
KERATINOCYTES

MELANOCYTES � ~8% of epidermal cells � produce melanin keratinocytes � pigment (yellow-red to brown-black) that contributes to skin color � * absorbs UV radiation � “covers” nucleus in keratinocyte

LANGERHANS CELLS � arise in red bone marrow then migrate to epidermis � easily damaged by UV radiation � function: immune response vs. microbes that invade


MERKEL CELLS � least numerous of epidermal cells (>1%) � deep in epidermis � in contact with Merkel disc (tactile disc) � together detect different aspects of touch


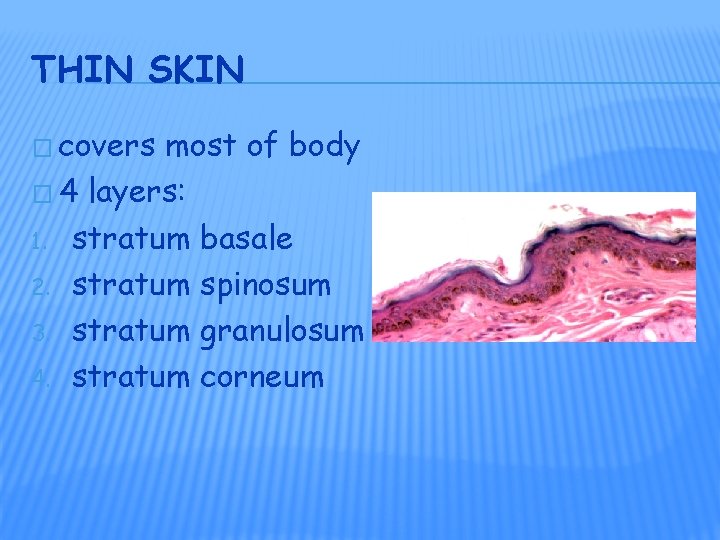
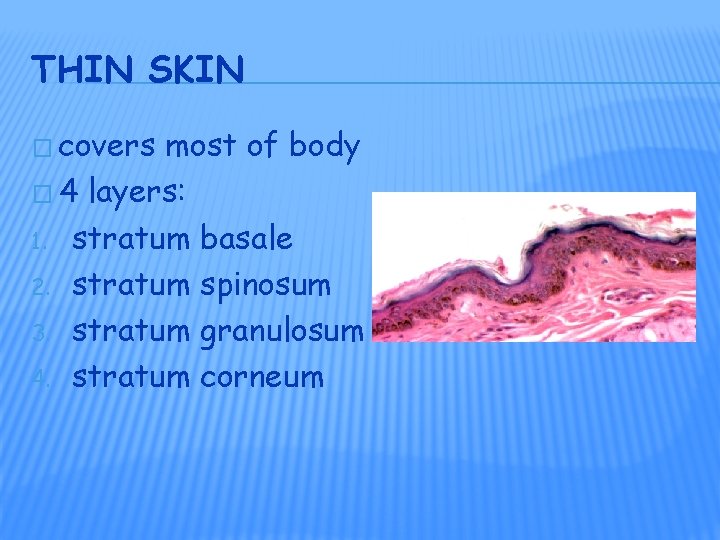
THIN SKIN � covers most of body � 4 layers: 1. stratum basale 2. stratum spinosum 3. stratum granulosum 4. stratum corneum
THICK SKIN � found in areas where exposure to friction is the greatest � “thick” because has 1 extra layer: � stratum lucidum (between stratgum granulosa & a thicker stratum corneum)

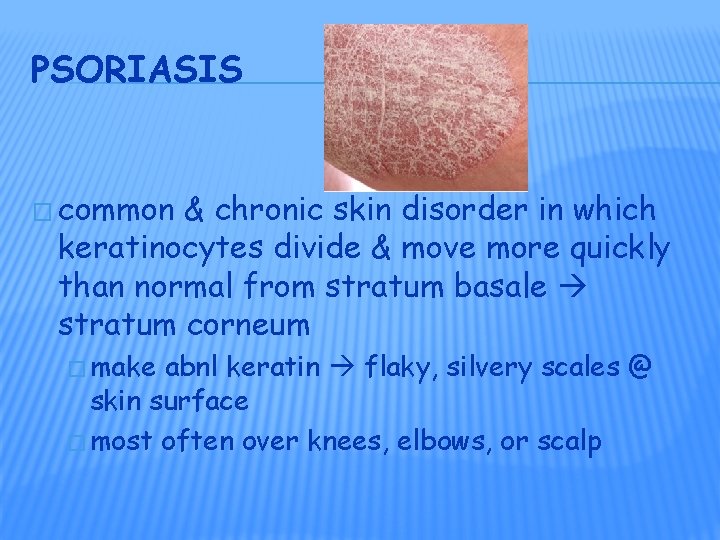
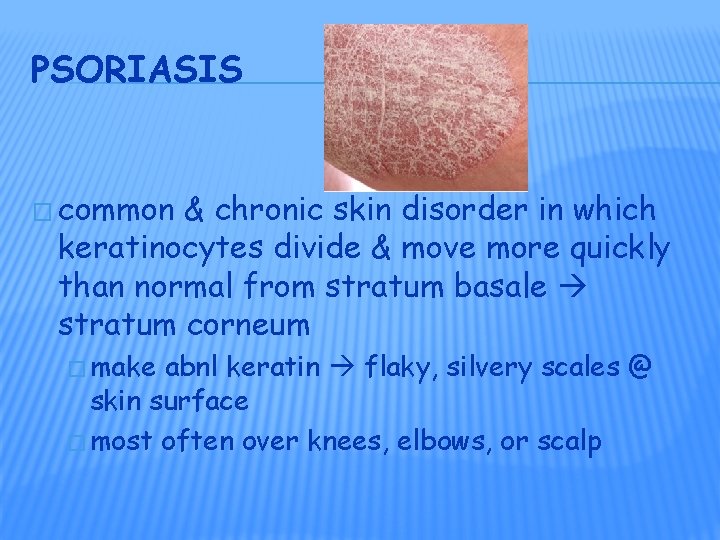
PSORIASIS � common & chronic skin disorder in which keratinocytes divide & move more quickly than normal from stratum basale stratum corneum � make abnl keratin flaky, silvery scales @ skin surface � most often over knees, elbows, or scalp


DERMIS � 2 nd, deeper layer of skin � composed mostly of CT � 2 regions: 1. papillary region 2. reticular region
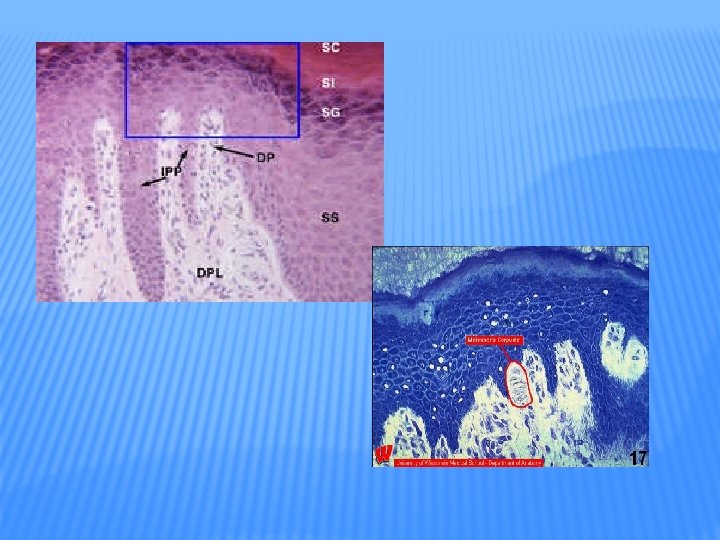
PAPILLARY REGION OF DERMIS �~ 1/5 th of total dermis � surface area greatly increased by fingerlike structures: dermal papillae that project into epidermis � contain: � capillary loops � tactile receptors: Meissner corpuscles � free nerve endings (temp, pain, tickle, itch)
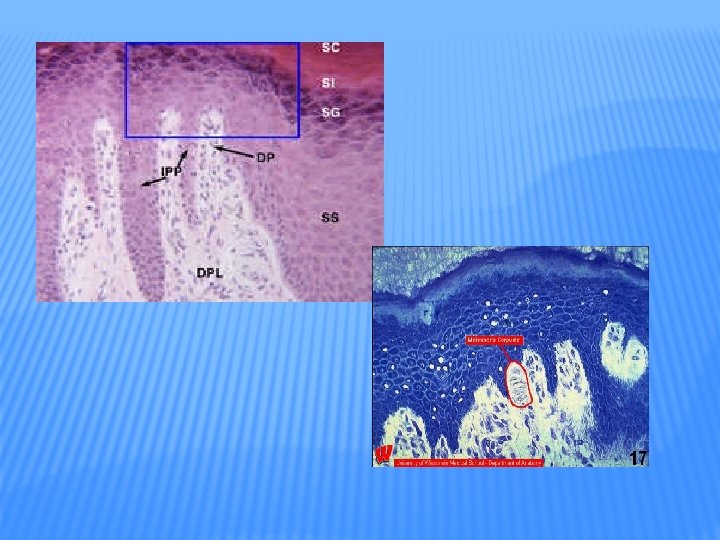
EPIDERMAL RIDGES � develop during 3 rd month of fetal development � pattern is genetically determined & unique to individuals (x identical twins) � on finger tips ridges deeper finger prints � allow you to grasp things by increasing surface area


RETICULAR REGION OF DERMIS � attached to subcutaneous layer beneath � contains: � dense irregular CT � hair follicles � sebaceous glands � sudoriferous (sweat) glands � collagen & elastic fibers (gives skin its elasticity, strength): extreme stretching striae (stretch marks)



BASIS OF SKIN COLOR � 3 1. 2. 3. pigments contribute: Melanin Hemoglobin (hgb) Carotene
MELANIN � made from a. a. tyrosine using enzyme tyrosinase then stored in organelle called a melanosome � exposure to UV light increases enzymatic activity & more (& darker) melanin produced � melanin absorbs UV radiation preventing it from damaging DNA which skin cancer
HEMOGLOBIN � in RBCs rosy color to lighter skinned individuals � blushing: due to increased blood flow (autonomic nervous system at work)
CAROTENE � yellow-orange pigment � precursor of vit. A
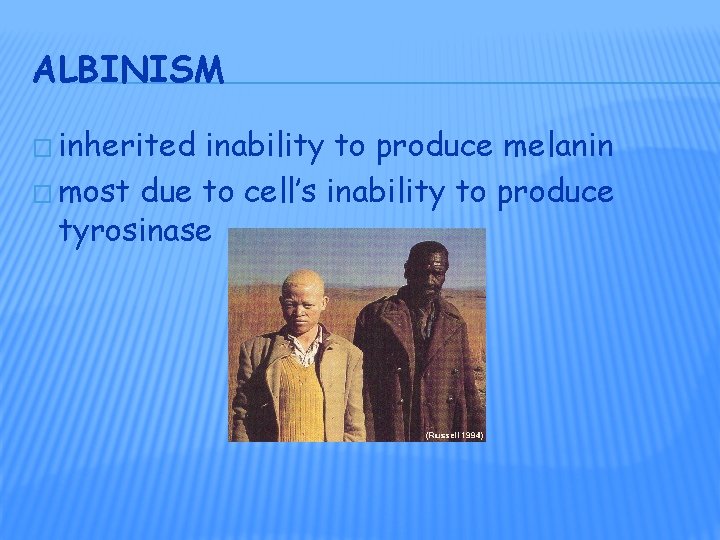
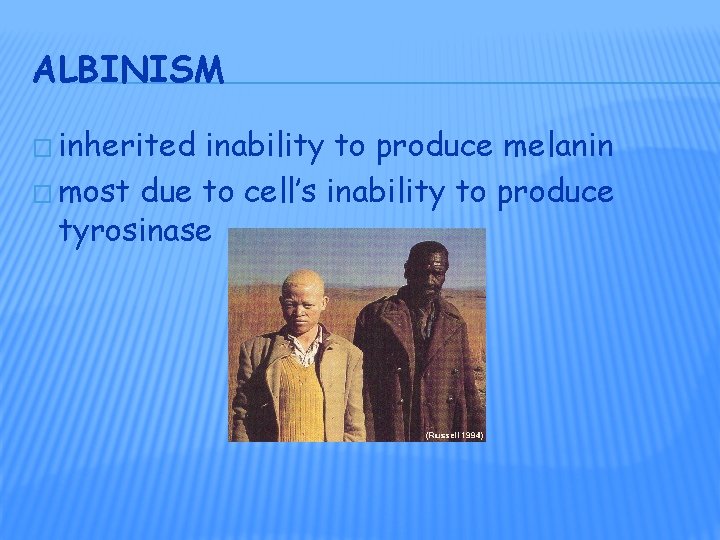
ALBINISM � inherited inability to produce melanin � most due to cell’s inability to produce tyrosinase

VITILIGO � partial or complete lack of melanocytes from patches of skin produces irregular white spots � ? Immune system malfunction?
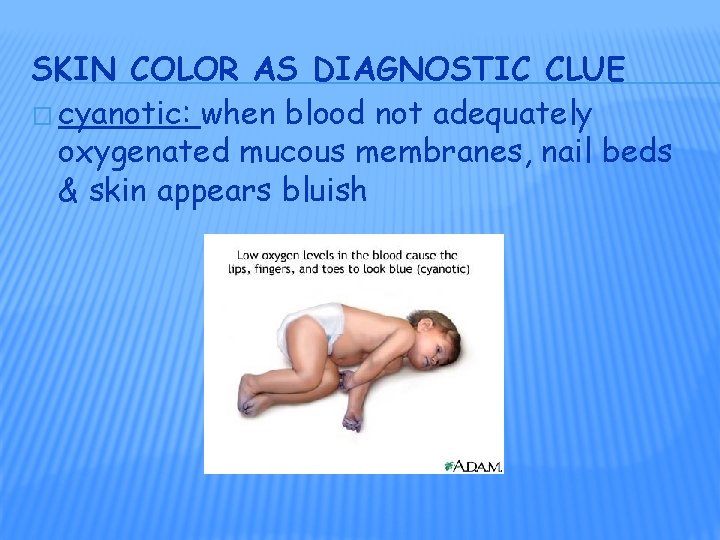
SKIN COLOR AS DIAGNOSTIC CLUE � cyanotic: when blood not adequately oxygenated mucous membranes, nail beds & skin appears bluish
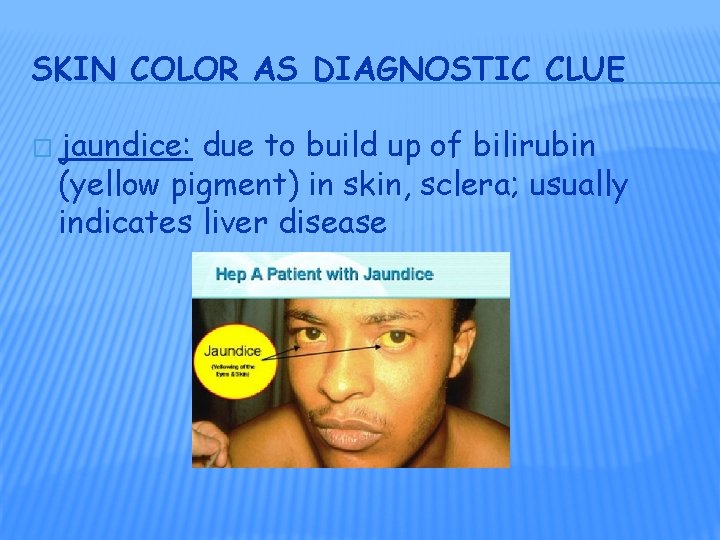
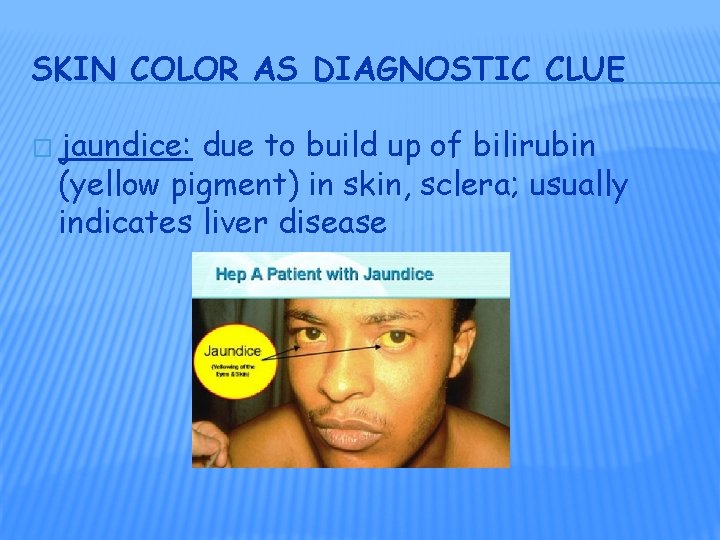
SKIN COLOR AS DIAGNOSTIC CLUE � jaundice: due to build up of bilirubin (yellow pigment) in skin, sclera; usually indicates liver disease
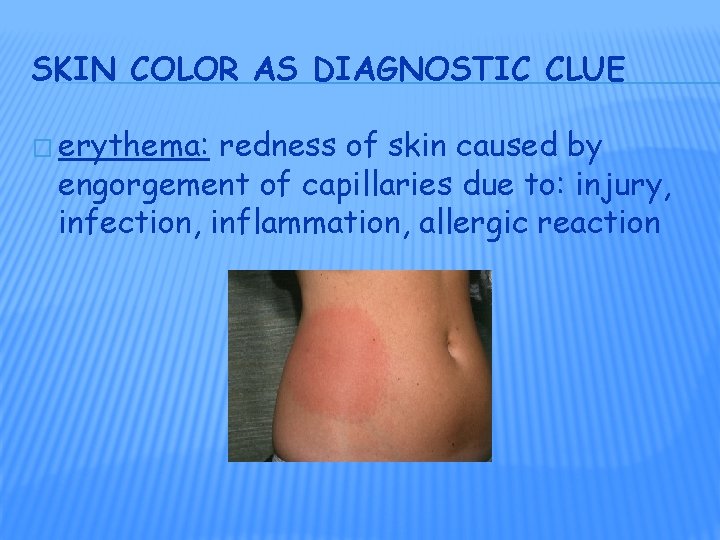
SKIN COLOR AS DIAGNOSTIC CLUE � erythema: redness of skin caused by engorgement of capillaries due to: injury, infection, inflammation, allergic reaction
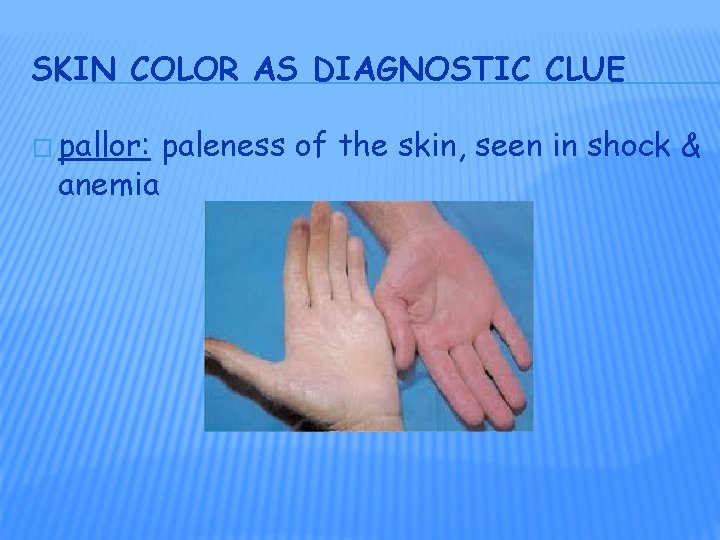
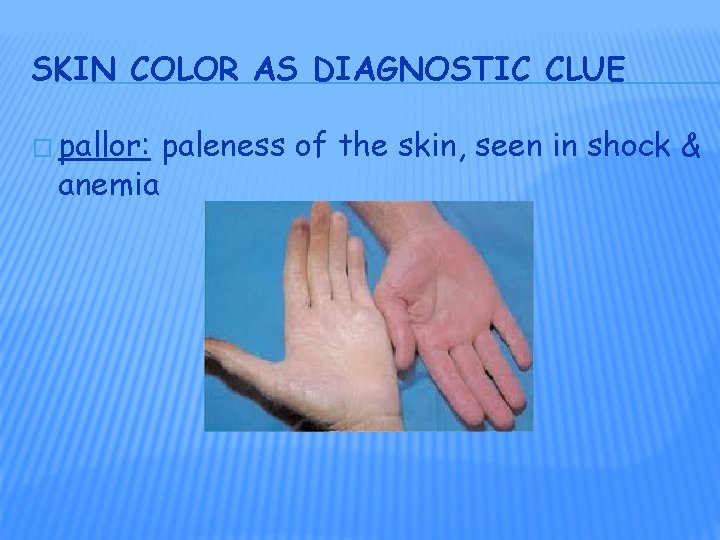
SKIN COLOR AS DIAGNOSTIC CLUE � pallor: anemia paleness of the skin, seen in shock &


ACCESSORY STRUCTURES OF THE SKIN � all develop from embryonic epidermis � include: � Hair � Nails � Glands
HAIR (PILI) � present on most skin surfaces x palmar surfaces of hands, soles & plantar surfaces of feet � genetic & hormonal influences determine thickness & pattern of distribution of hair
HAIR � functions: � protection � scalp, eyebrows, eyelashes: from getting foreign objects in eyes � nose, ear canals: trap foreign objects � sensitive � touch to light touch receptors in hair root plexus
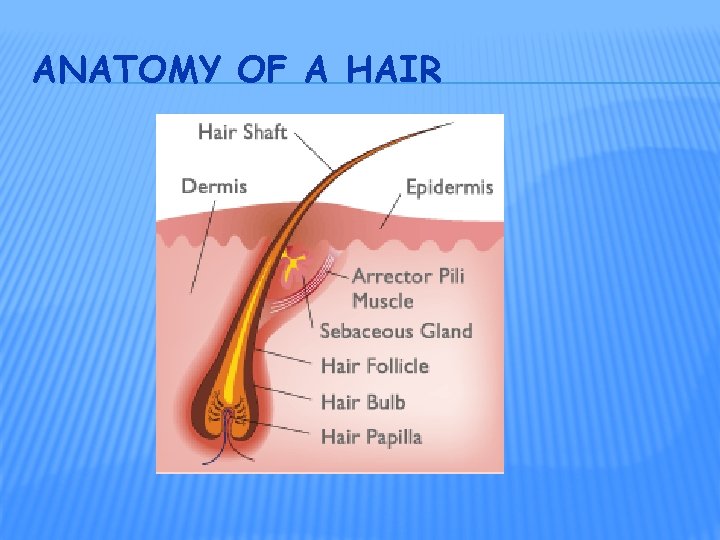
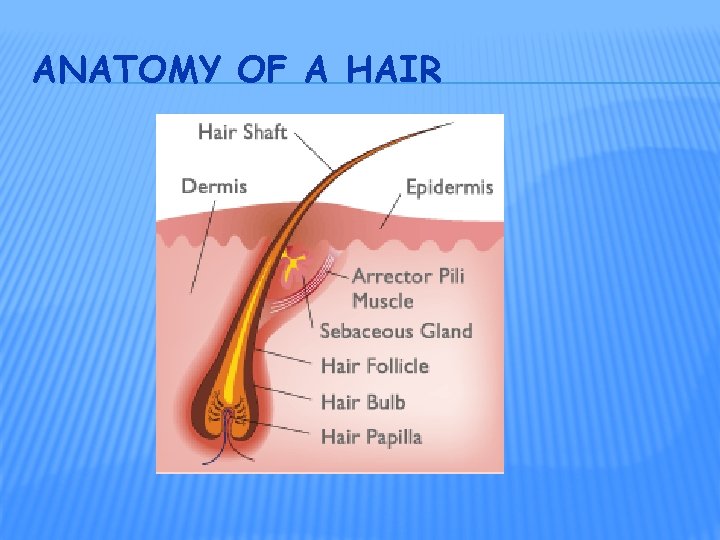
ANATOMY OF A HAIR
HAIR � composed of columns of dead, keratinized cells bonded together by extracellular proteins
ANATOMY OF A HAIR � shaft: portion of hair that projects from scalp � root: portion below scalp � follicle: surrounds root of hair � arector pili: smooth muscle extends from side of hair follicle superficial dermis
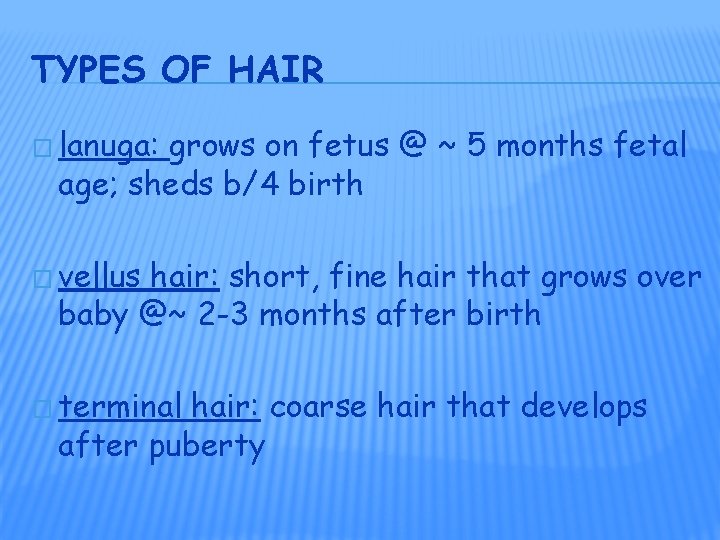
TYPES OF HAIR � lanuga: grows on fetus @ ~ 5 months fetal age; sheds b/4 birth � vellus hair: short, fine hair that grows over baby @~ 2 -3 months after birth � terminal hair: coarse hair that develops after puberty

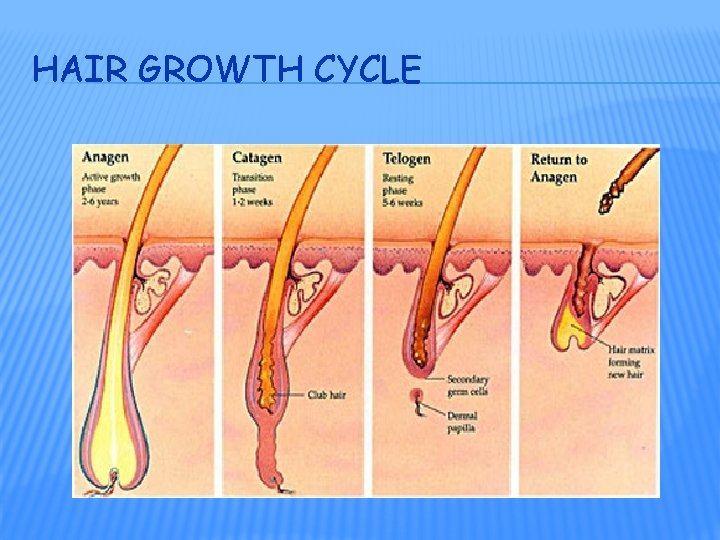
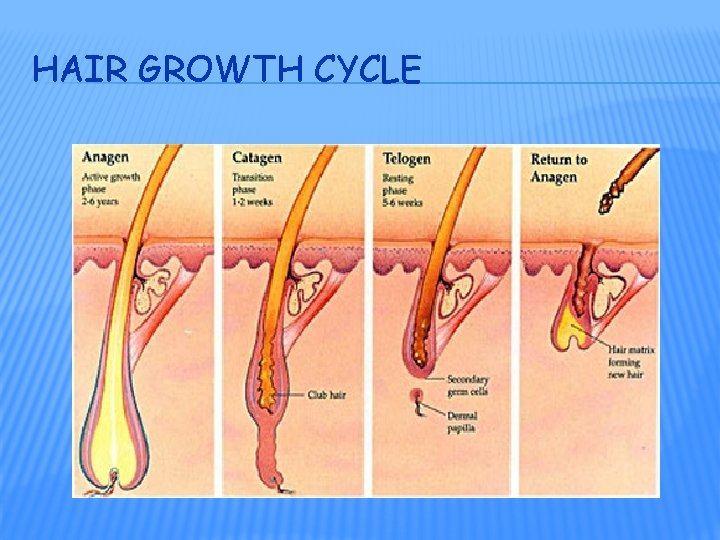
HAIR GROWTH CYCLE
HAIR COLOR � mostly due to amt & type of melanin in keratinzed cells � dark hair has eumelanin � blondes & redheads have pheomelanin � gray: loss of melanin � white: loss of melanin + air bubbles in shaft of hair


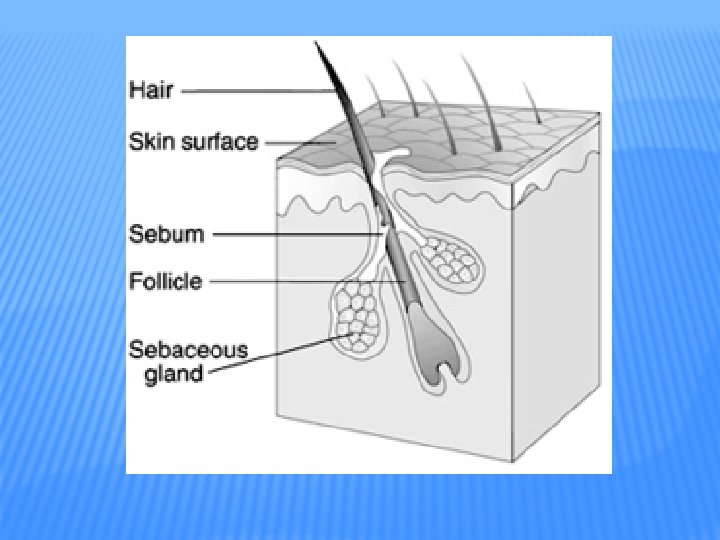
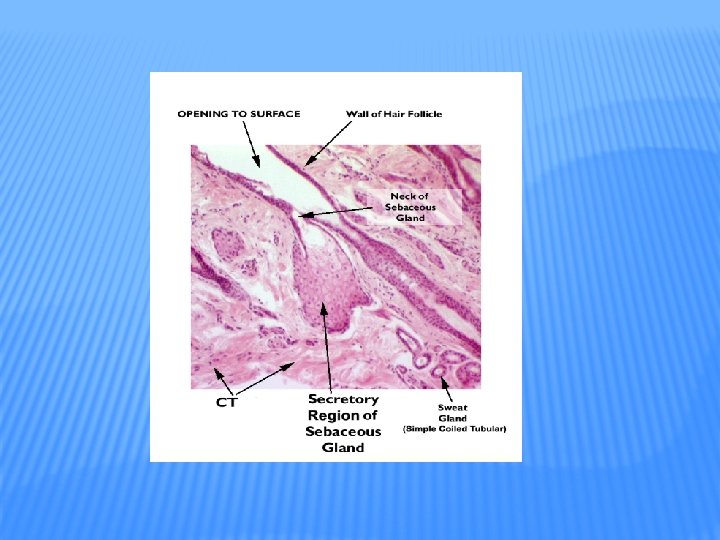
SKIN GLANDS � exocrine 1. 2. glands ass’c with the skin: sebaceous glands sudoriferous glands � � eccrine sweat glands apocrine sweat glands
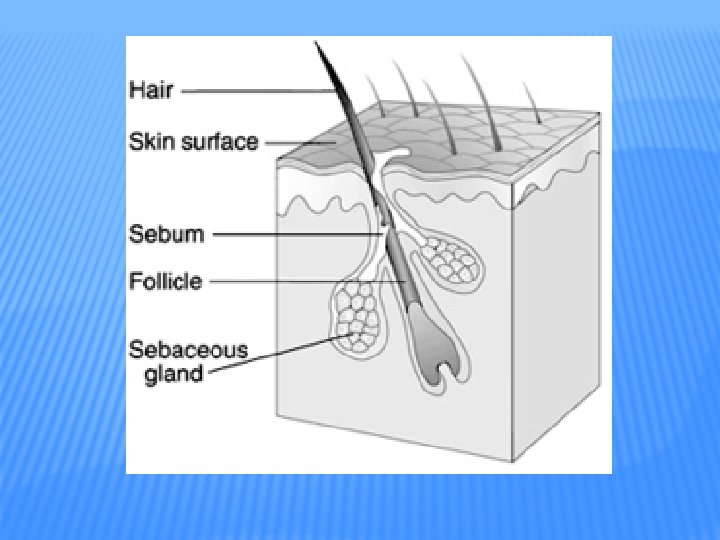
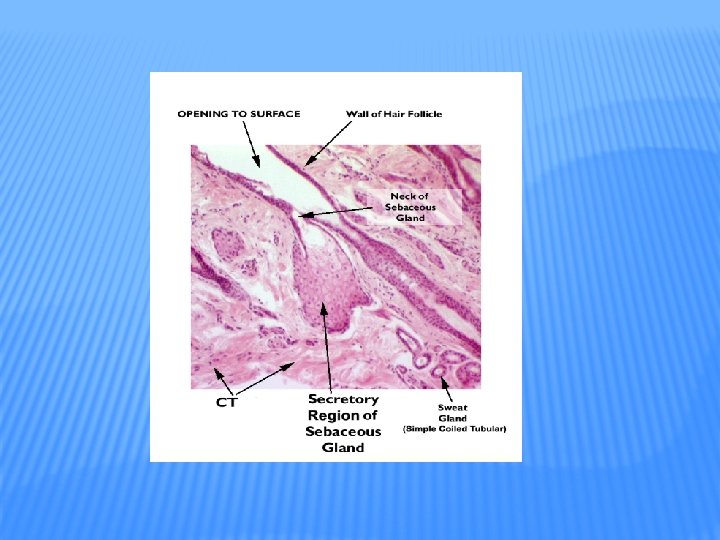
SEBACEOUS GLANDS � “oil” glands � most connected to hair follicles � rest secrete directly onto surface of skin (lips, eyelids, genitals) � secrete oily substance called sebum onto hair � keeps hair from getting brittle
ACNE � inflammation of sebaceous glands colonized with bacteria � infection cyst which destroys epidermal cells (cystic acne) � acne is not caused by eating chocolate or fried foods

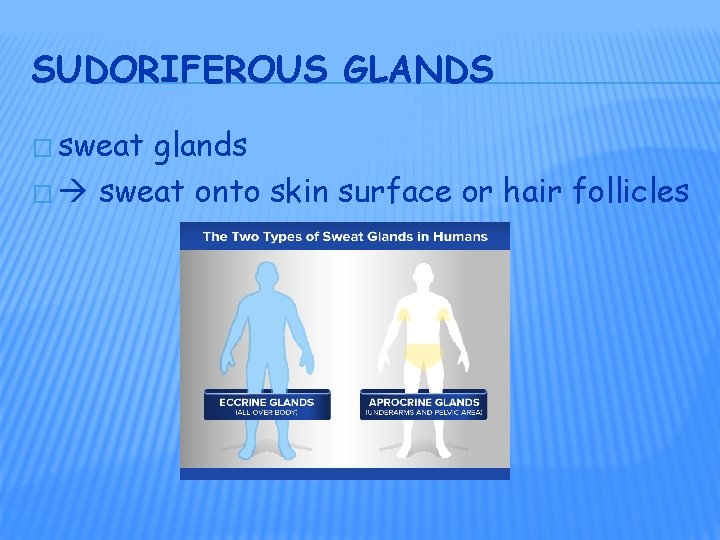
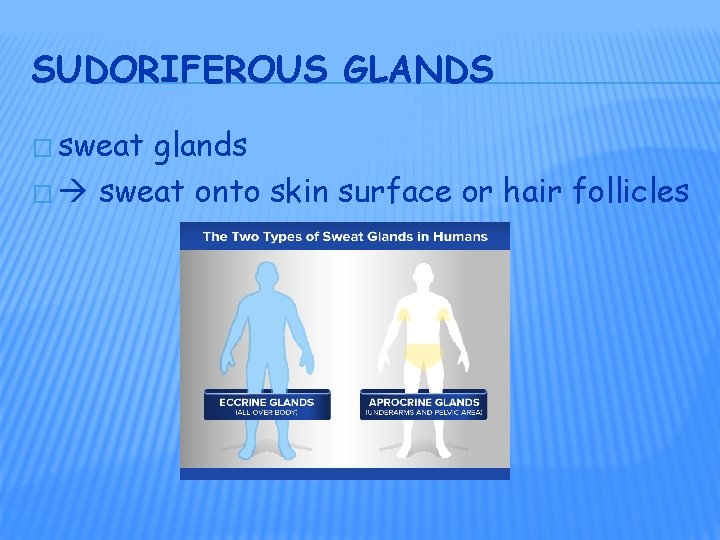
SUDORIFEROUS GLANDS � sweat glands � sweat onto skin surface or hair follicles
CERUMINOUS GLANDS � modified sweat glands in external ear canal skin (sub. Q layer) � secrete cerumen (ear wax � provides a sticky barrier that impedes entrance of foreign bodies

NAILS � plates of tightly packed, hard, dead, keratinized epidermal cells that form a clear, solid covering over the dorsal surfaces of the distal portions of the 20 digits � average growth ~ 0. 04 in/wk � fingernails grow slightly faster than toe nails
FUNCTIONS OF A NAIL � help us grasp & manipulate small objects � protect ends of digits � allows scratching
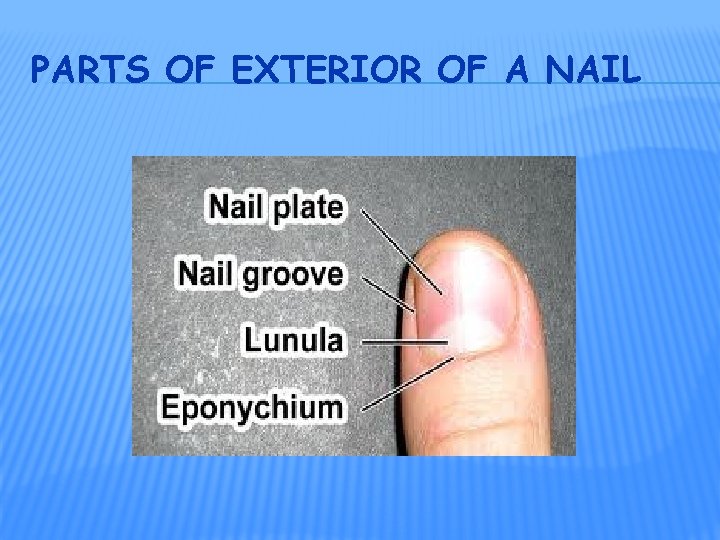
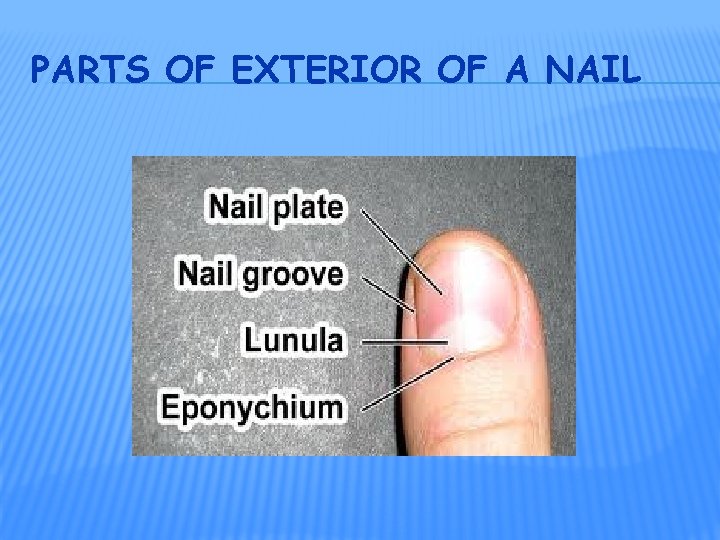
PARTS OF EXTERIOR OF A NAIL
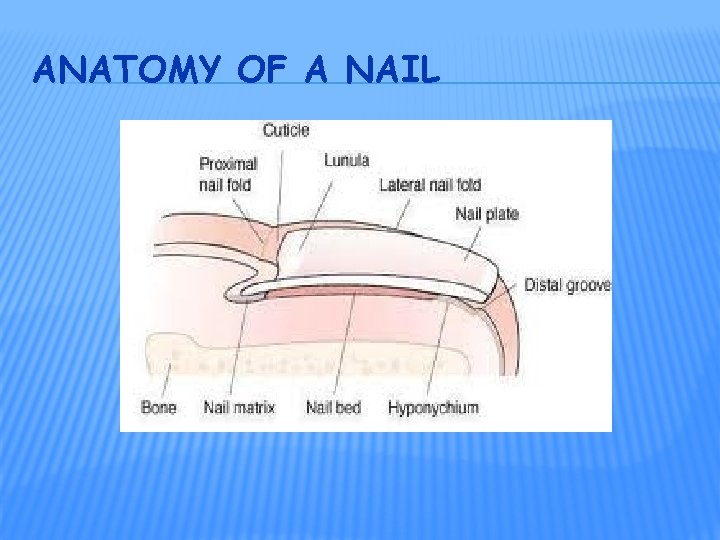
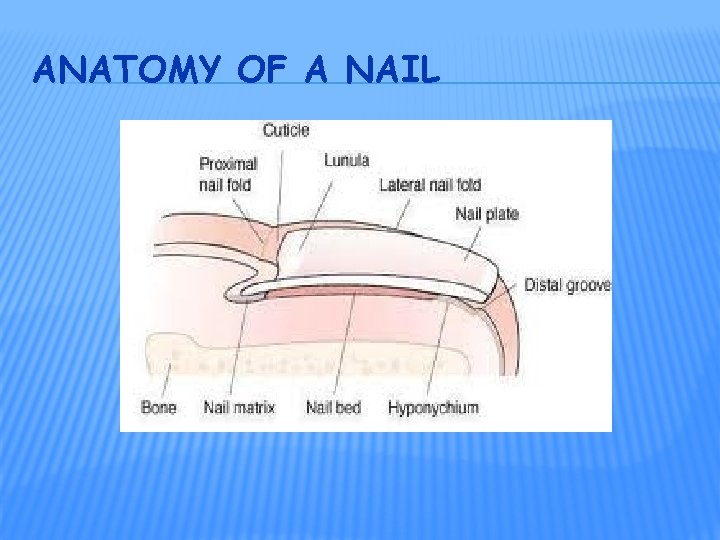
ANATOMY OF A NAIL
PARTS OF A NAIL � body: visible part � root: part buried � matrix: where cells divide to produce growth

FUNCTIONS OF THE SKIN (#7) 1. Thermoregulation � � 1. the homeostatic regulation of body temperature skin achieves this in 2 ways: sweating � 2. evaporation of sweat requires nrg (body heat) so body cools down as sweat evaporates adjusting flow of blood in dermis � � vessels dilate when body too warm vessels constrict when body too cold
FUNCTIONS OF THE SKIN 2. Blood Reservoir � skin carries ~ 8 – 10% of total blood flow in resting adult
FUNCTIONS OF THE SKIN 3. Protection � � � keratin protects underlying tissues from microbes, abrasion, heat, & chemicals lipids released retard evaporation of water from skin surface guarding vs. dehydration & retard water from entering thru skin sebum moistens skin & has antibacterial properties acidic p. H of sweat bacteriostatic melanin protects DNA in skin cells from UV damage Langerhans cells alert immune system if microbes does attack / macrophages ingest microbes
FUNCTIONS OF THE SKIN 4. Cutaneous Sensations � skin contains variety of nerve endings & receptors � touch � pressure � vibration � tickle � pain � temperature
FUNCTIONS OF THE SKIN 5. Excretion � elimination of wastes from the body � only small amt substances excreted from skin � ~400 m. L water/day ~200 m. L sweat (sedentary adult) � small amts salts, CO 2, NH 3, & urea �
FUNCTIONS OF THE SKIN 6. Absorption passage of materials from external environment body cells � absorption of water-soluble materials negligible � lipid-soluble materials do absorb: � fat-soluble vitamins (A, D, E, K) � certain drugs (can be administered transdermally) � gases: O 2 & CO 2 � toxins: acetone, CCl 4, salts of Hg, Pb, Ar, substances in poison ivy & poison oak �

FUNCTIONS OF THE SKIN 7. Synthesis of Vitamin D requires activation of a precursor molecule in the skin by UV rays in sunlight modified by enzymes in liver & kidneys producing calcitriol the most active form of vit. D � calcitriol: aids in absorption of calcium in GI tract �
SKIN WOUND HEALING � skin damage sets in motion a sequence of events that repairs the skin to as normal as it can in both structure & function � depending on depth of wound 1 of 2 processes occur � epidemal wound healing � deep wound healing
EPIDERMAL WOUND HEALING � abrasion: away � portion of skin has been scraped in response to injury: basal cells of nearby uninjured skin break contact with bm, enlarge, & migrate across the wound migration continues across wound until meet cells advancing from other side of wound � contact inhibition: cells stop migrating when touch another cell �
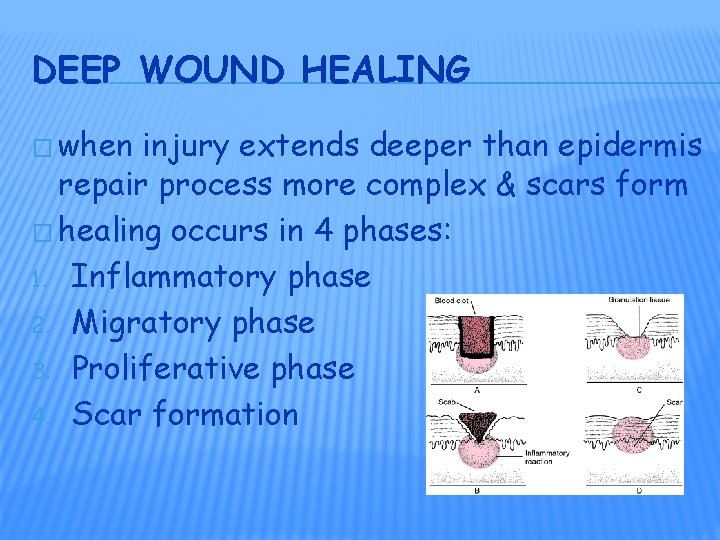
DEEP WOUND HEALING � when injury extends deeper than epidermis repair process more complex & scars form � healing occurs in 4 phases: 1. Inflammatory phase 2. Migratory phase 3. Proliferative phase 4. Scar formation
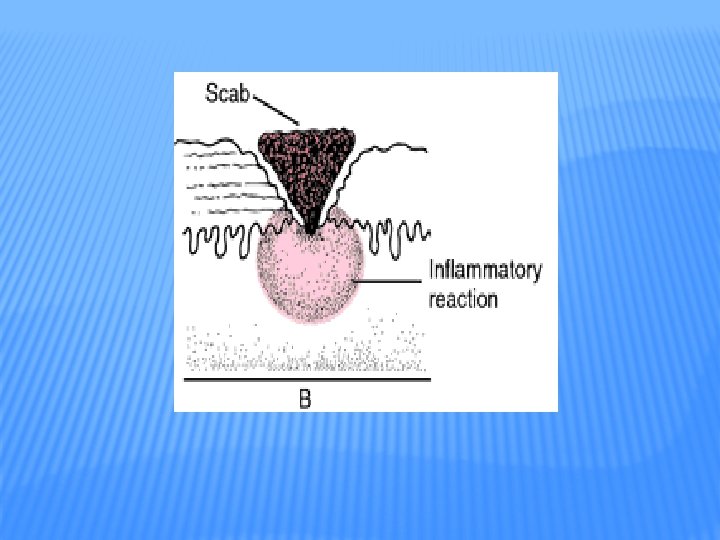
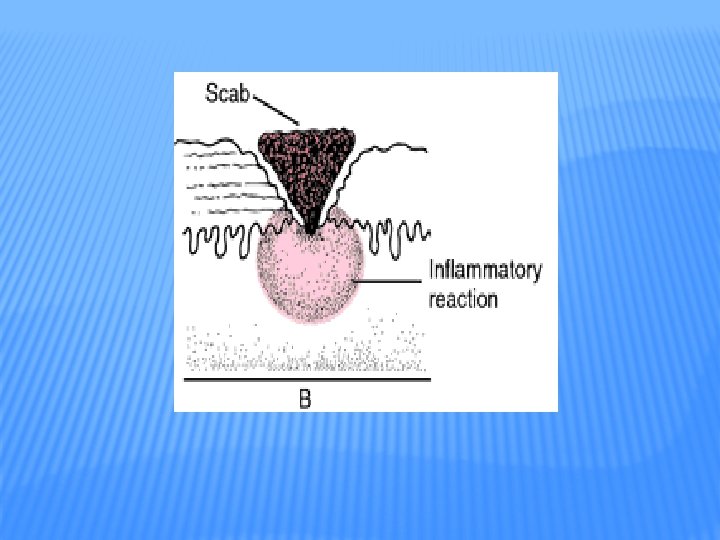
INFLAMMATORY PHASE � blood clot forms � loosely unites edges of wound � inflammation � vascular response � vasodilation � cellular develops & increased permeability of vessels response � phagocytic � fibroblasts WBCs (neutrophils), macrophages


MIGRATORY PHASE � clot scab � epithelial cells migrate beneath scab to bridge wound � fibroblasts begin secreting collagen & glycoproteins scar � *tissue filling wound called granulation tissue
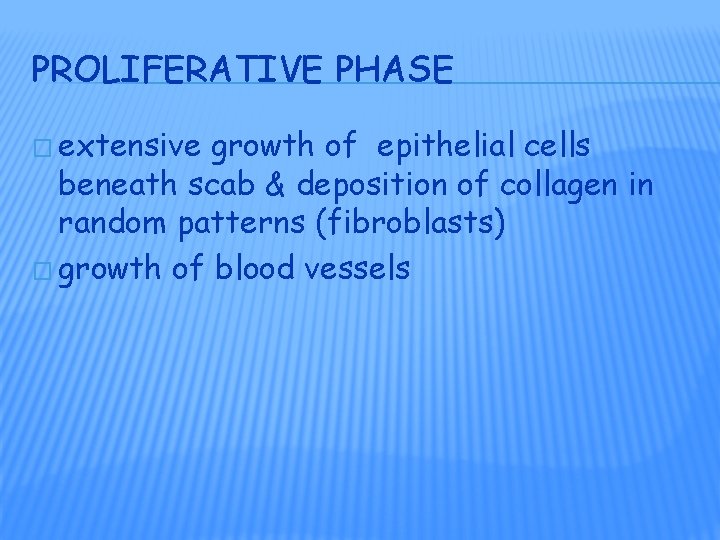
PROLIFERATIVE PHASE � extensive growth of epithelial cells beneath scab & deposition of collagen in random patterns (fibroblasts) � growth of blood vessels

SCAR FORMATION � aka maturation phase � scab falls off � epidermis restored � collagen fibers become more organized � fibroblasts disappear � blood vessels restored to normal � scar tissue less elastic, fewer blood vessels, +/- accessory structures of skin

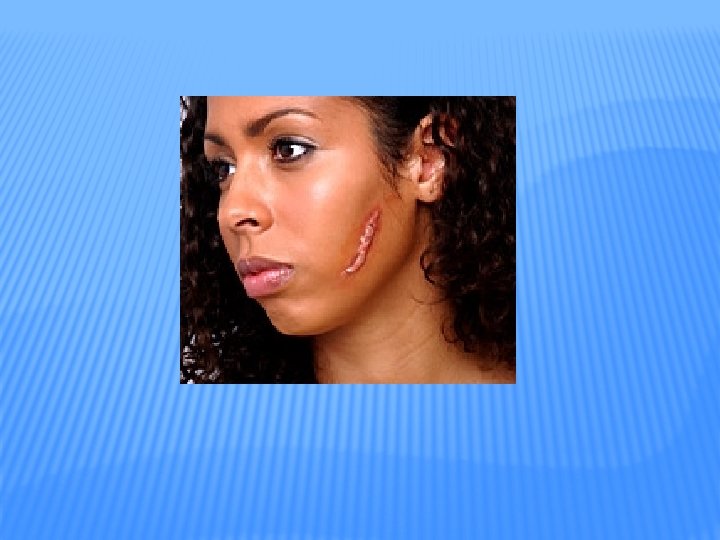
SCARS � fibrosis: process of scar formation � 2 types raised scars 1. hypertrophic scar � 2. scar remains w/in boundaries of wound keloid � extends boundaries of wound site
SCAR FORMATION � aka maturation phase � scab falls off � epidermis restored � collagen fibers become more organized � fibroblasts disappear � blood vessels restored to normal � scar tissue less elastic, fewer blood vessels, +/- accessory structures of skin

BURNS � tissue damage caused by excessive heat, electricity, radioactivity, or corrosive chemicals that denature proteins in skin cells � destroy skin’s ability to maintain homeostasis � graded by their severity: 1 st & 2 nd degree = partial thickness burns; 3 rd degree = full thickness
1 ST DEGREE BURNS � only epidermis is damaged � example: sunburn � symptoms: � localized � tx: redness, swelling, & pain immediate flushing with cool water (lessens pain) � healing: 3 – 6 days +/- peeling of skin � results: normal
2 ND DEGREE BURN � epidermis & upper dermis damaged, some skin function lost, ass’c structures not damaged � symptoms: � same as 1 st degree + blisters (epidermis separates from dermis due to accumulation of tissue fluid) � example: any burn with blisters

2 ND DEGREE BURNS � tx: if 2° infection: antibiotics � lasts: 3 – 4 wks with +/- scarring � AVOID: WEAR SUNSCREEN!

3 RD DEGREE BURNS � destroys epidermis, & sub. Q � no initial edema or pain or sensations (receptors destroyed) � most skin functions lost � as healing starts marked edema � regeneration: months, + scarring � tx: +/- skin grafting

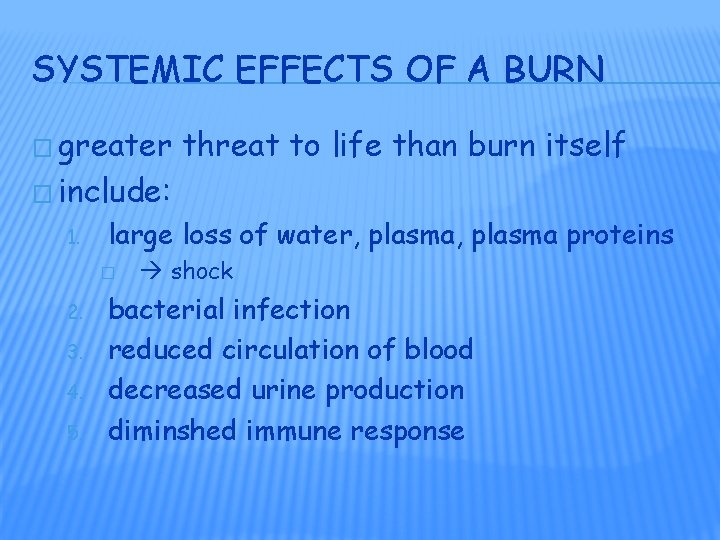
SYSTEMIC EFFECTS OF A BURN � greater threat to life than burn itself � include: 1. large loss of water, plasma proteins � 2. 3. 4. 5. shock bacterial infection reduced circulation of blood decreased urine production diminshed immune response

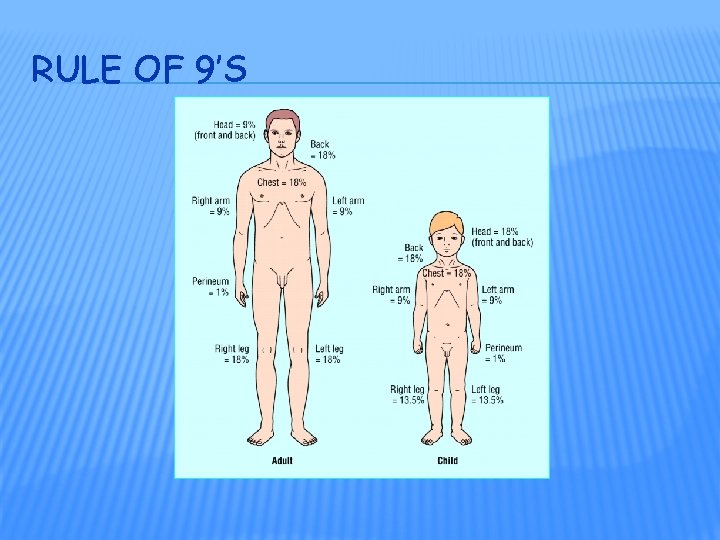
MAJOR BURNS � used to estimate extent & severity of burns � major burn considered a 3° burn that covers > 10% of body or a 2° burn that covers > 25% of surface area of body or any 3° burn on face, hands, feet, or perineum � if burn > 70% surface area > ½ patients die
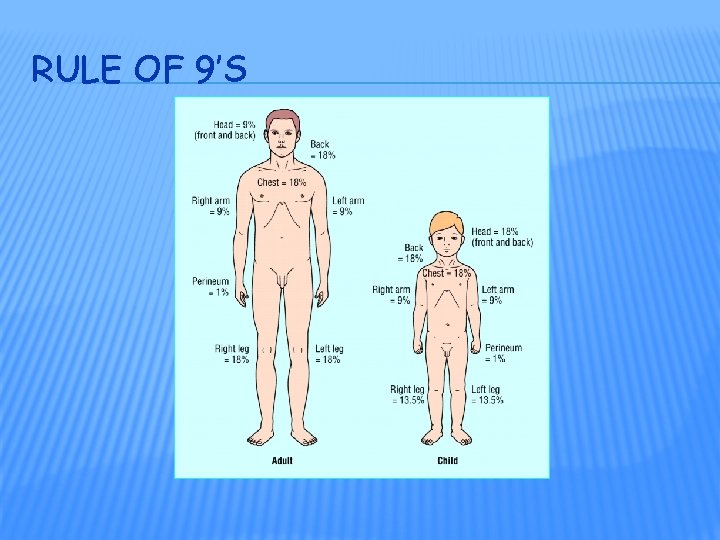
RULE OF 9’S

SKIN CANCER � 3 3. common forms: Basal cell carcinoma Squamous cell carcinoma Malignant melanoma � 1 & 2 50% more common in males 1. 2.
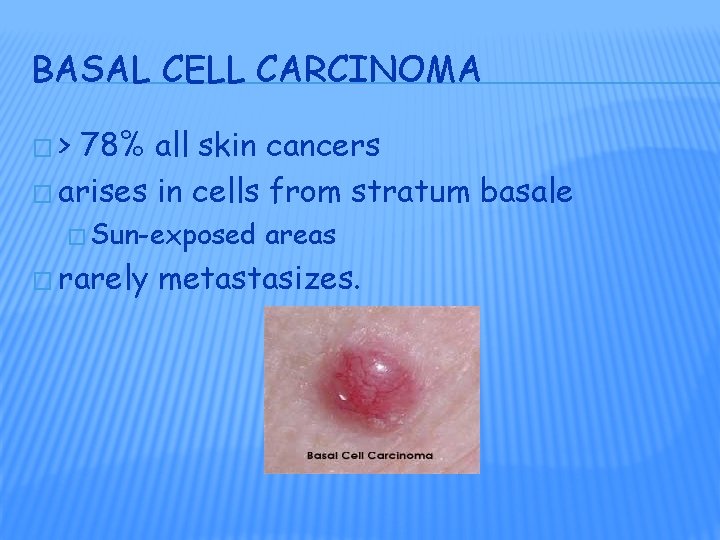
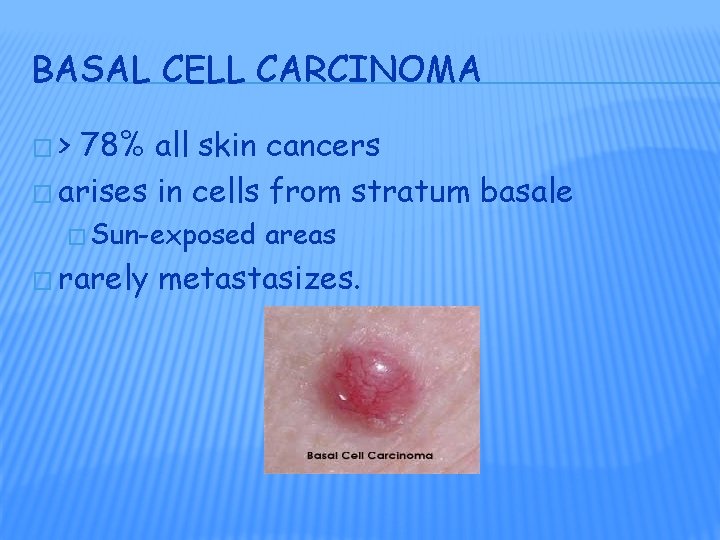
BASAL CELL CARCINOMA �> 78% all skin cancers � arises in cells from stratum basale � Sun-exposed � rarely areas metastasizes.
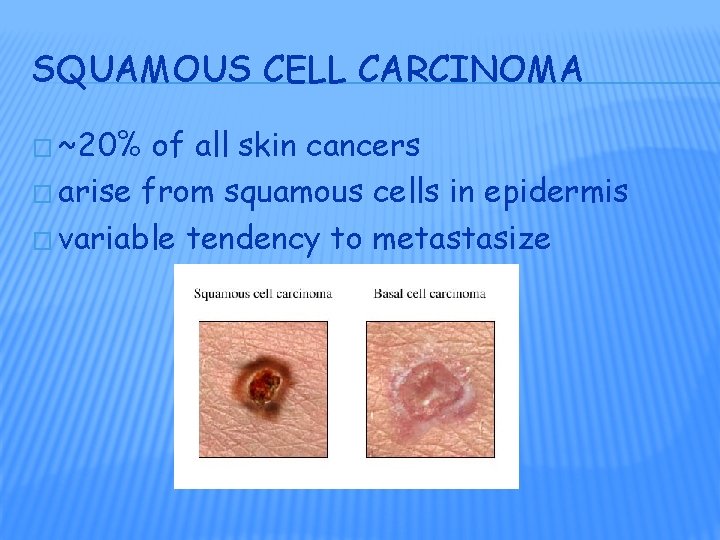
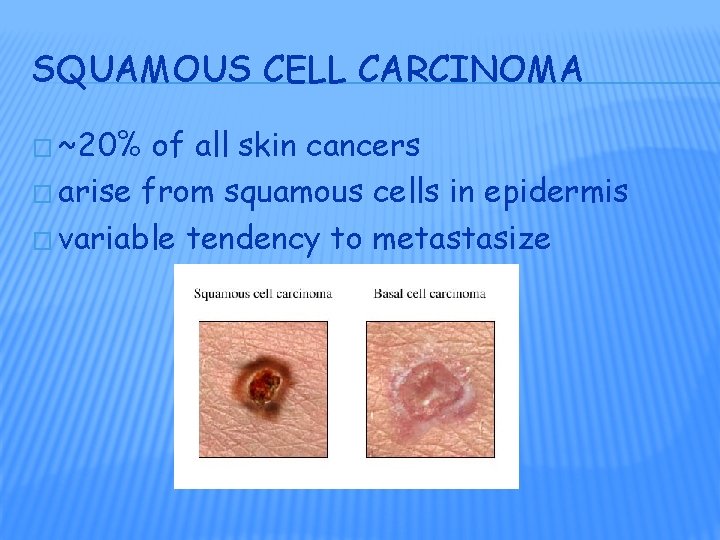
SQUAMOUS CELL CARCINOMA � ~20% of all skin cancers � arise from squamous cells in epidermis � variable tendency to metastasize
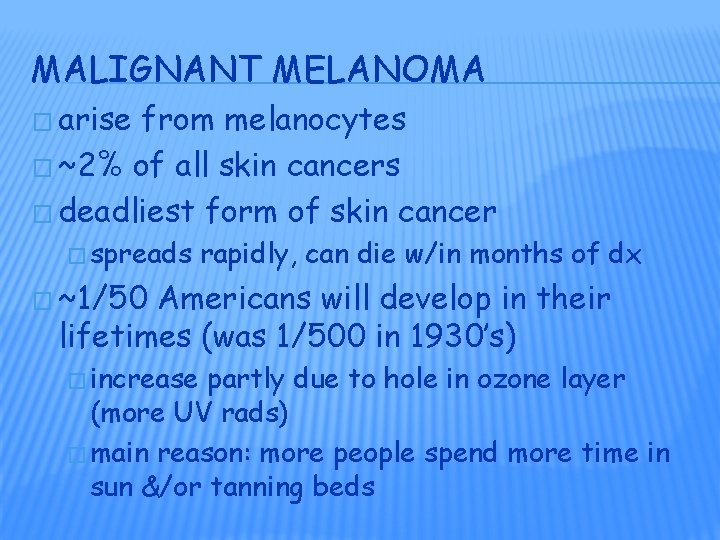
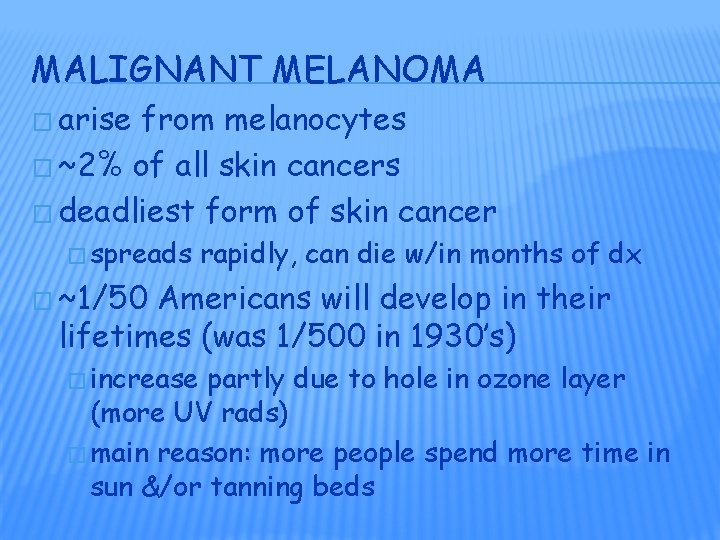
MALIGNANT MELANOMA � arise from melanocytes � ~2% of all skin cancers � deadliest form of skin cancer � spreads rapidly, can die w/in months of dx � ~1/50 Americans will develop in their lifetimes (was 1/500 in 1930’s) � increase partly due to hole in ozone layer (more UV rads) � main reason: more people spend more time in sun &/or tanning beds
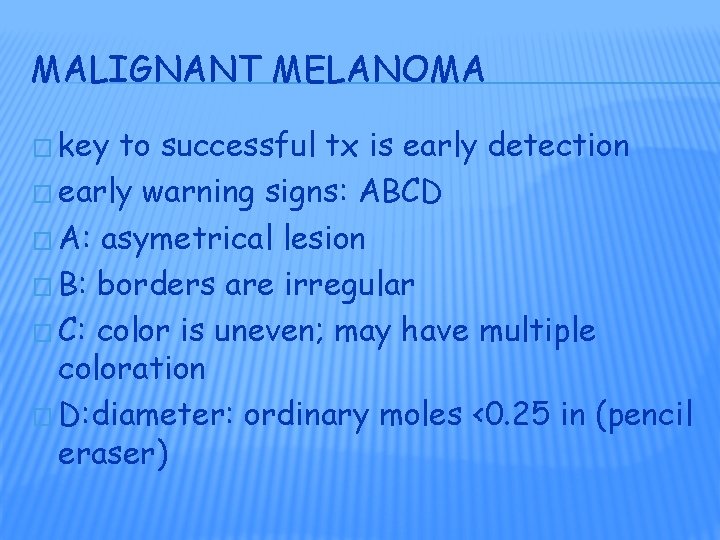
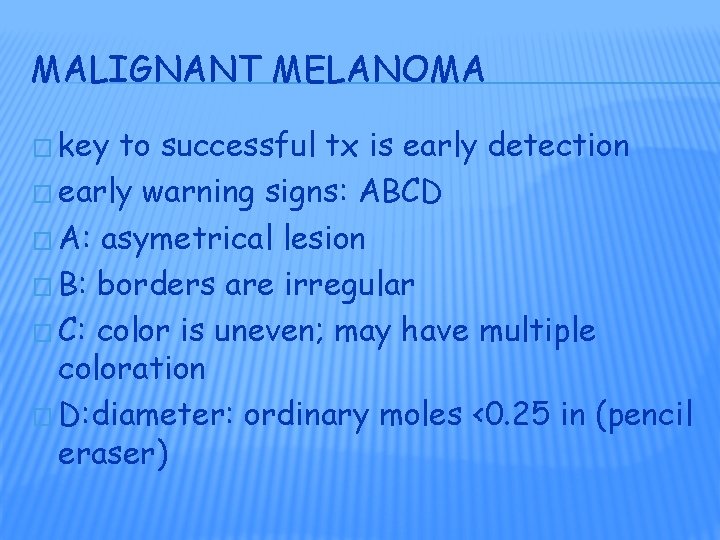
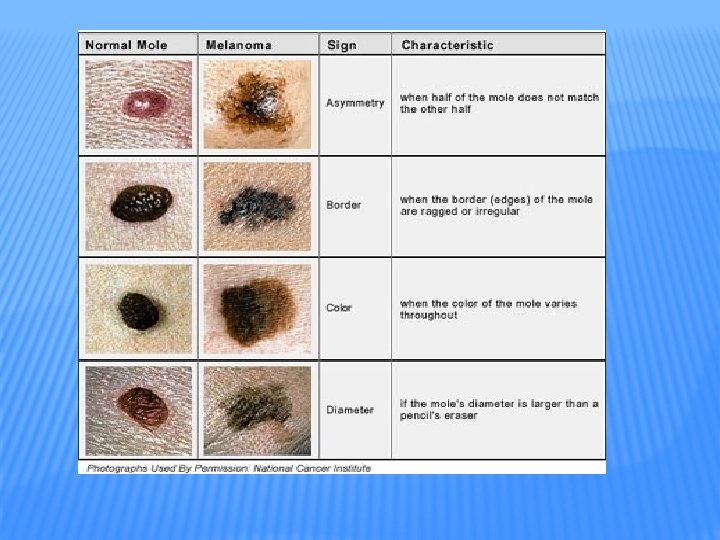
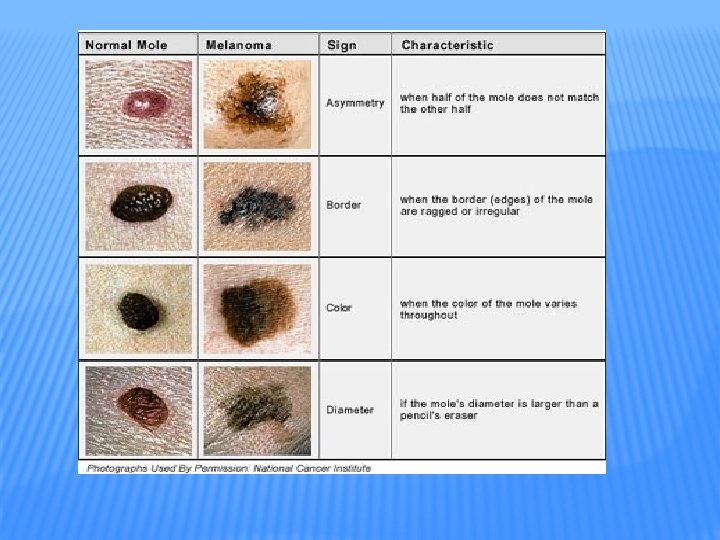
MALIGNANT MELANOMA � key to successful tx is early detection � early warning signs: ABCD � A: asymetrical lesion � B: borders are irregular � C: color is uneven; may have multiple coloration � D: diameter: ordinary moles <0. 25 in (pencil eraser)

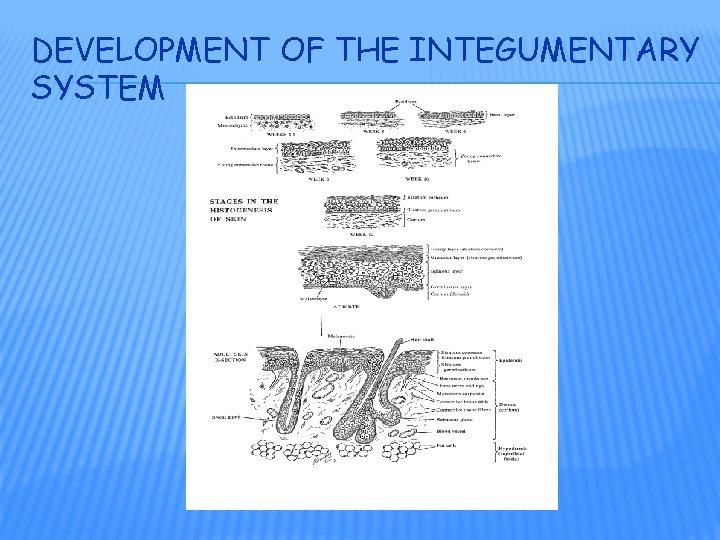
DEVELOPMENT OF THE INTEGUMENTARY SYSTEM
