Holes Essentials of Human Anatomy Physiology Unit 5
- Slides: 35
Hole’s Essentials of Human Anatomy & Physiology Unit 5: Chapter 7 Skeletal System
Functions of Bone Tissue · Support of the body tissues · Legs & pelvis support body’s weight · Atlas supports the skull · Protection of underlying organs · Skull – protects the brain, eyes, ears · Rib cage & shoulder girdle – protects heart and lungs · Pelvic girdle – protects lower abdominal organs and internal reproductive organs · Movement · Skeletal muscles attached to bones by tendons serve to move bones · Muscles use bones to work in opposition to cause movement
Functions of Bone Tissue · Mineral Homeostasis · Bones store many minerals including: · Calcium salts, mainly calcium phosphate · Magnesium, sodium, potassium, carbonate ions · Harmful minerals stored: · Lead, radium, strontium · Energy storage · Yellow marrow in the shaft of long bones · Serves as an important chemical energy storage (fat) · Can convert back to red marrow if blood cells are needed and revert back to yellow marrow when there is a blood cell surplus
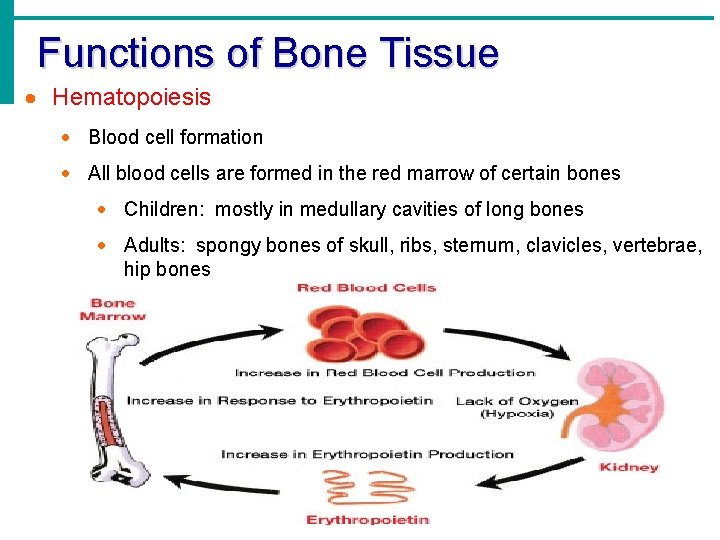
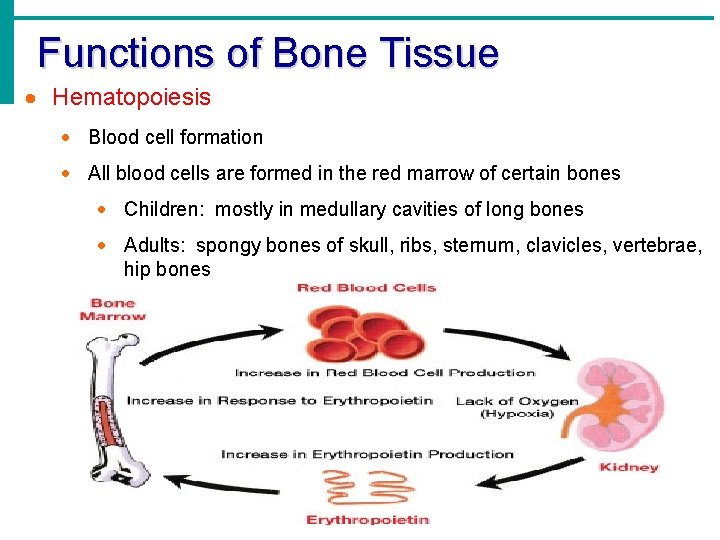
Functions of Bone Tissue · Hematopoiesis · Blood cell formation · All blood cells are formed in the red marrow of certain bones · Children: mostly in medullary cavities of long bones · Adults: spongy bones of skull, ribs, sternum, clavicles, vertebrae, hip bones
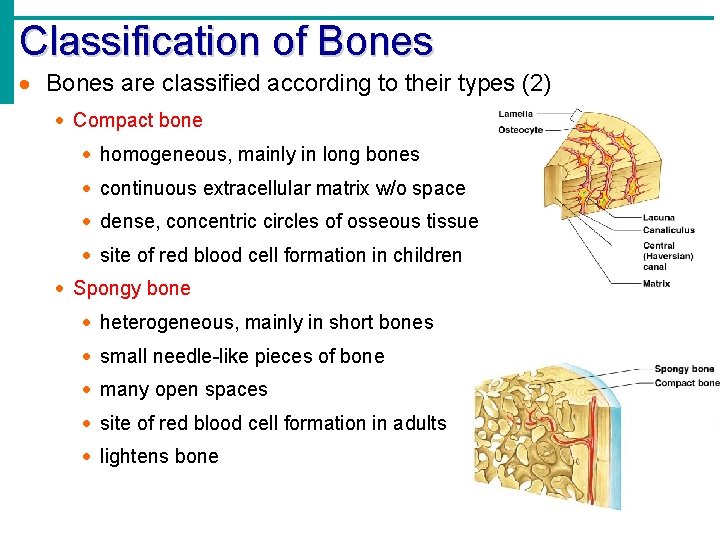
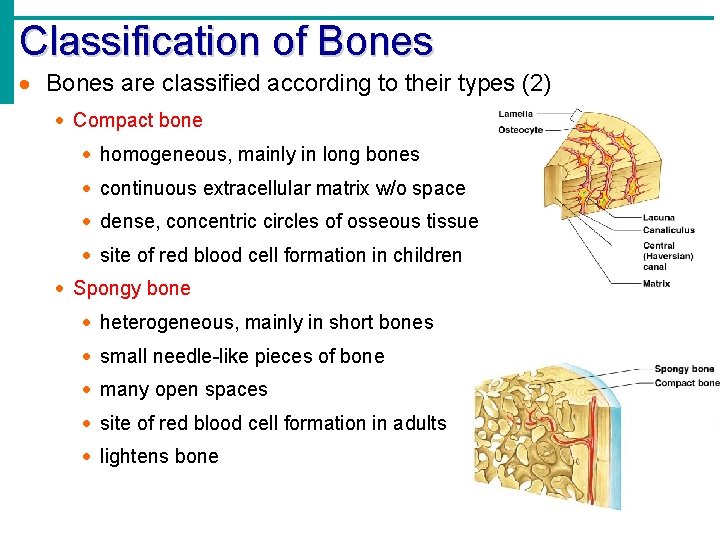
Classification of Bones · Bones are classified according to their types (2) · Compact bone · homogeneous, mainly in long bones · continuous extracellular matrix w/o space · dense, concentric circles of osseous tissue · site of red blood cell formation in children · Spongy bone · heterogeneous, mainly in short bones · small needle-like pieces of bone · many open spaces · site of red blood cell formation in adults · lightens bone
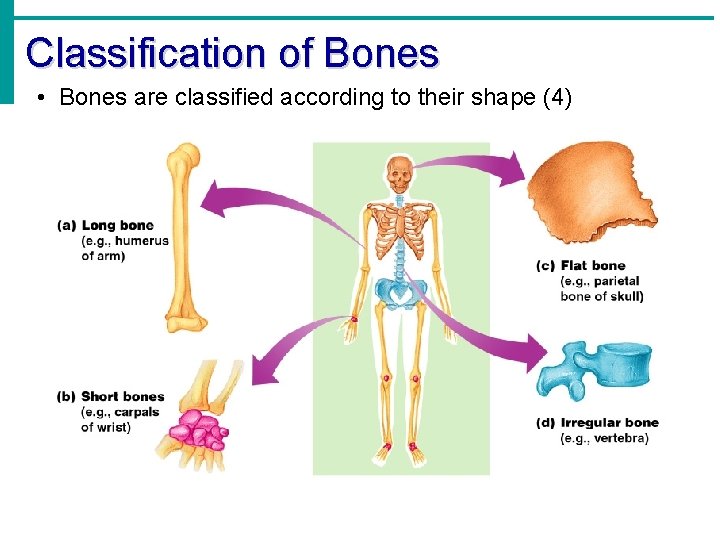
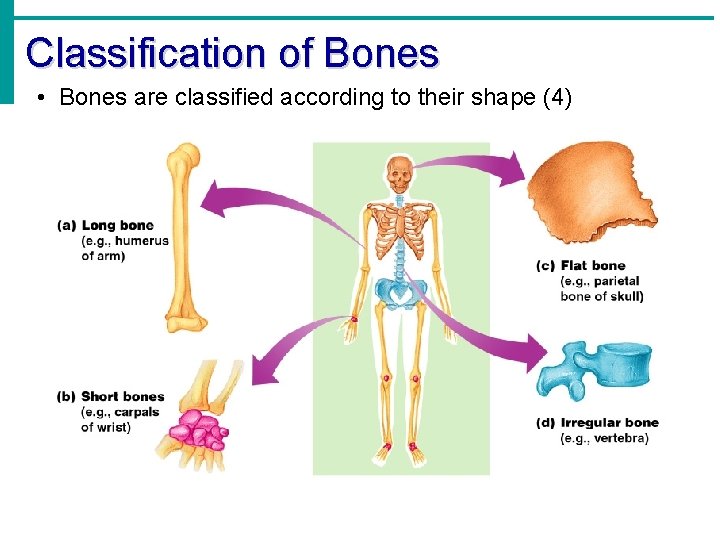
Classification of Bones • Bones are classified according to their shape (4)
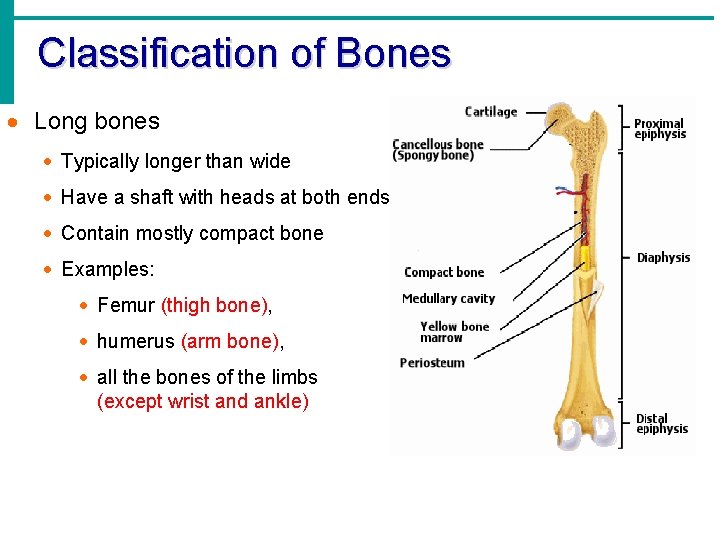
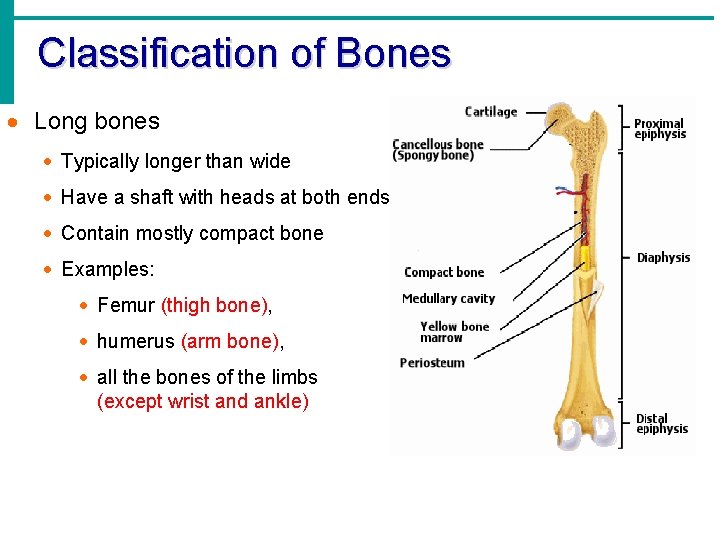
Classification of Bones · Long bones · Typically longer than wide · Have a shaft with heads at both ends · Contain mostly compact bone · Examples: · Femur (thigh bone), · humerus (arm bone), · all the bones of the limbs (except wrist and ankle)
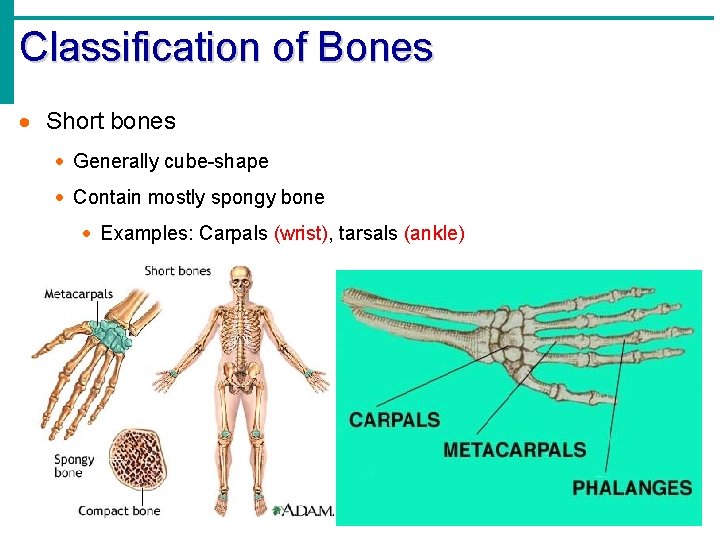
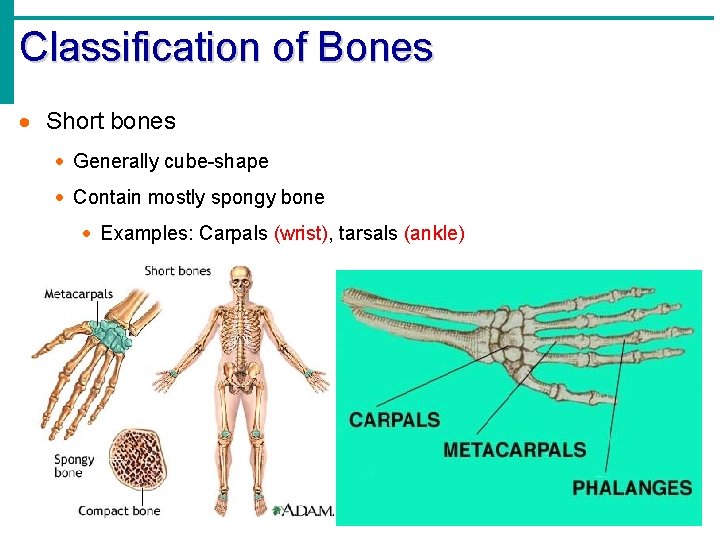
Classification of Bones · Short bones · Generally cube-shape · Contain mostly spongy bone · Examples: Carpals (wrist), tarsals (ankle)
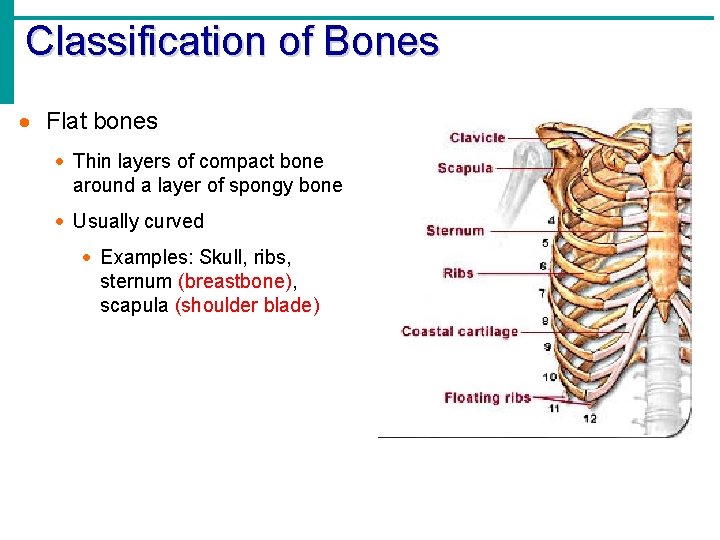
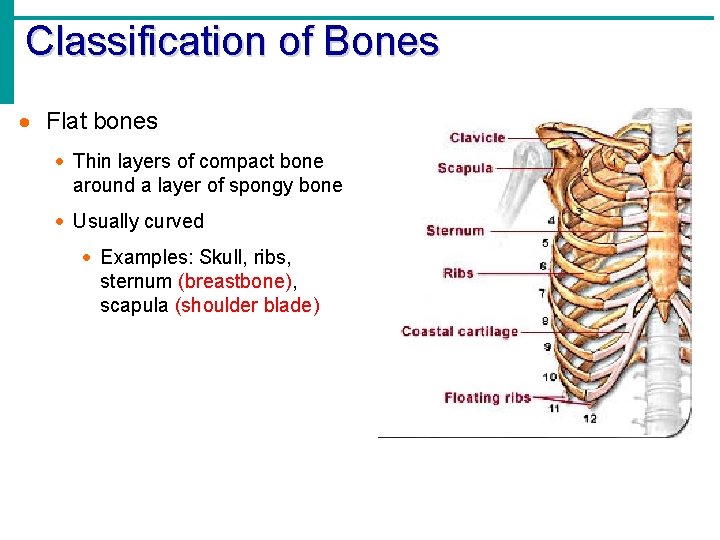
Classification of Bones · Flat bones · Thin layers of compact bone around a layer of spongy bone · Usually curved · Examples: Skull, ribs, sternum (breastbone), scapula (shoulder blade)
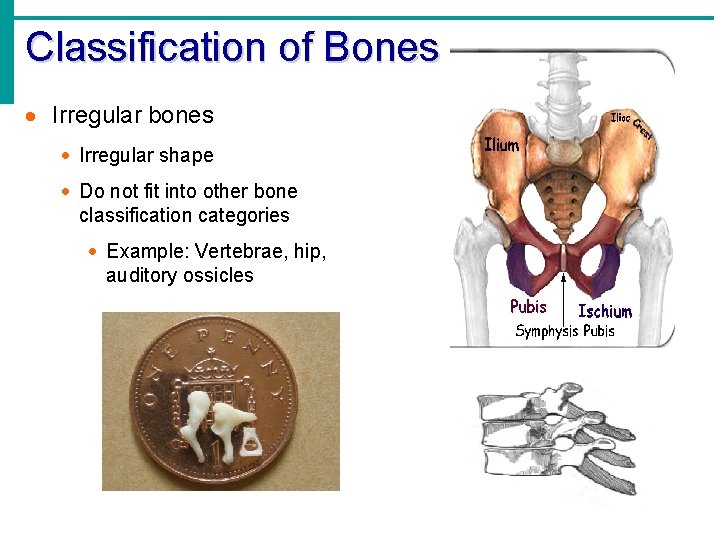
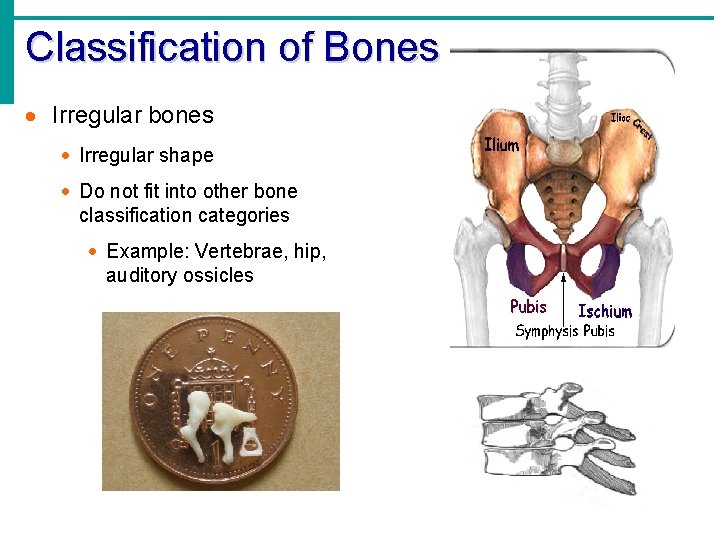
Classification of Bones · Irregular bones · Irregular shape · Do not fit into other bone classification categories · Example: Vertebrae, hip, auditory ossicles
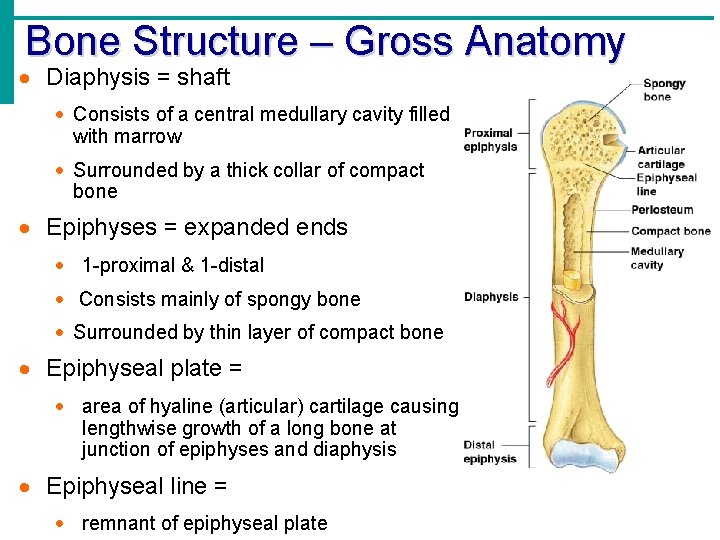
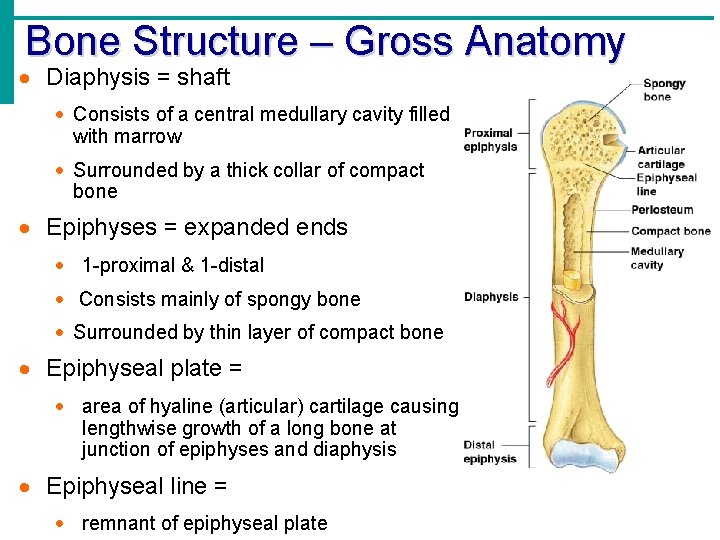
Bone Structure – Gross Anatomy · Diaphysis = shaft · Consists of a central medullary cavity filled with marrow · Surrounded by a thick collar of compact bone · Epiphyses = expanded ends · 1 -proximal & 1 -distal · Consists mainly of spongy bone · Surrounded by thin layer of compact bone · Epiphyseal plate = · area of hyaline (articular) cartilage causing lengthwise growth of a long bone at junction of epiphyses and diaphysis · Epiphyseal line = · remnant of epiphyseal plate
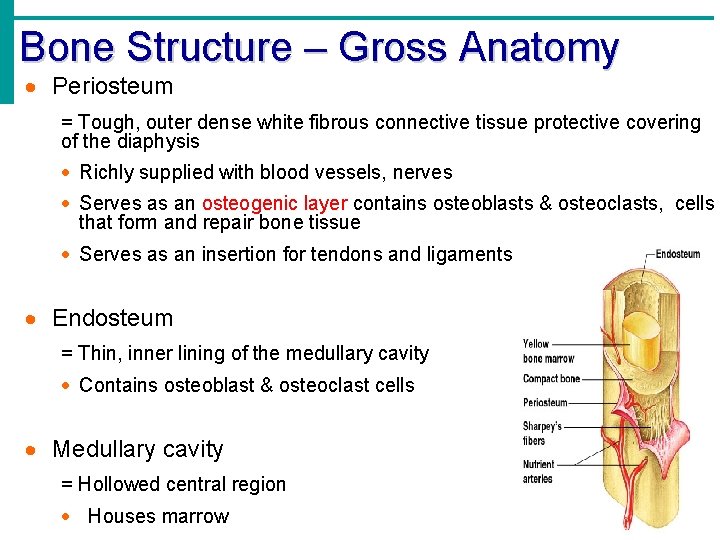
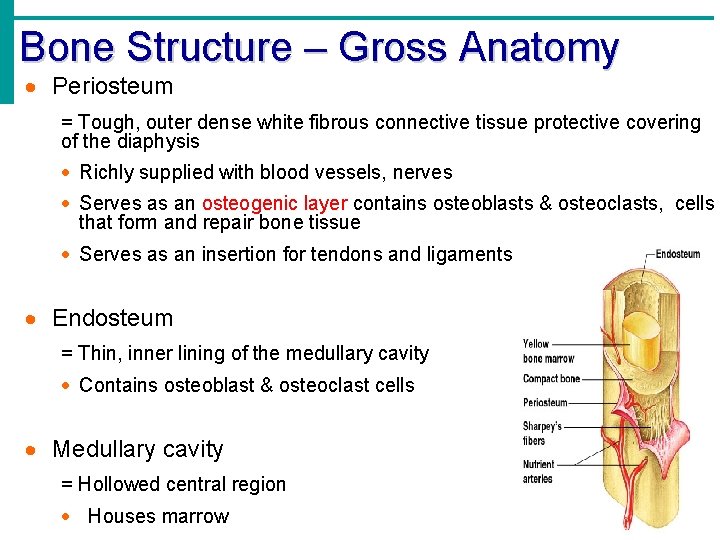
Bone Structure – Gross Anatomy · Periosteum = Tough, outer dense white fibrous connective tissue protective covering of the diaphysis · Richly supplied with blood vessels, nerves · Serves as an osteogenic layer contains osteoblasts & osteoclasts, cells that form and repair bone tissue · Serves as an insertion for tendons and ligaments · Endosteum = Thin, inner lining of the medullary cavity · Contains osteoblast & osteoclast cells · Medullary cavity = Hollowed central region · Houses marrow
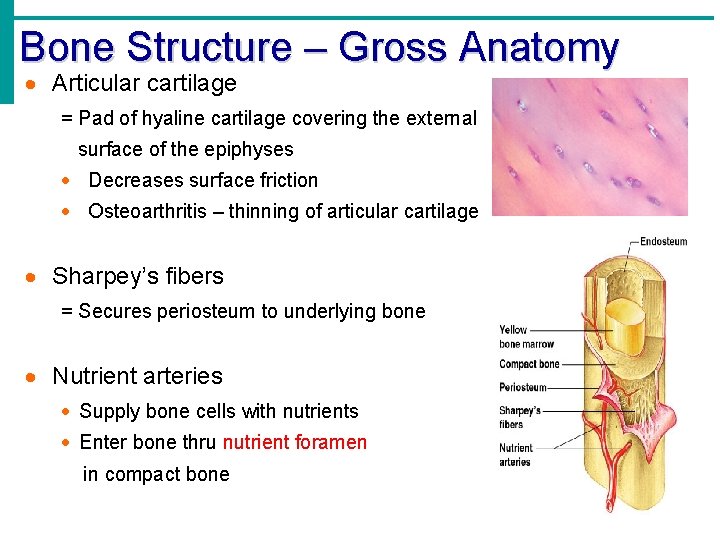
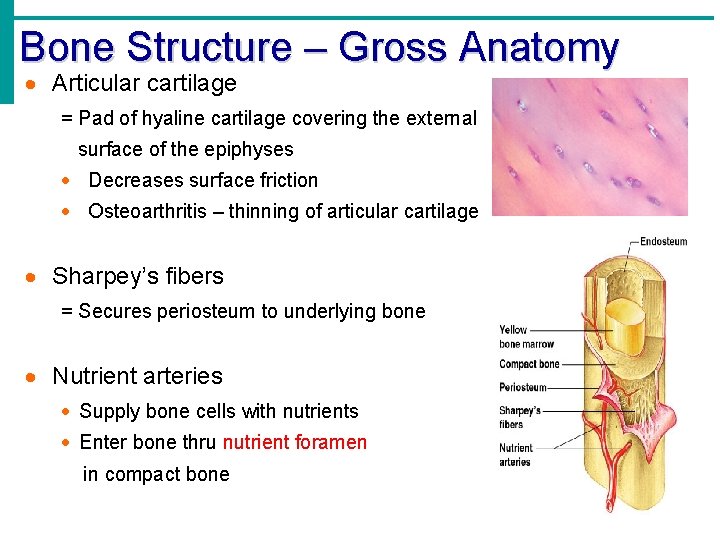
Bone Structure – Gross Anatomy · Articular cartilage = Pad of hyaline cartilage covering the external surface of the epiphyses · Decreases surface friction · Osteoarthritis – thinning of articular cartilage · Sharpey’s fibers = Secures periosteum to underlying bone · Nutrient arteries · Supply bone cells with nutrients · Enter bone thru nutrient foramen in compact bone
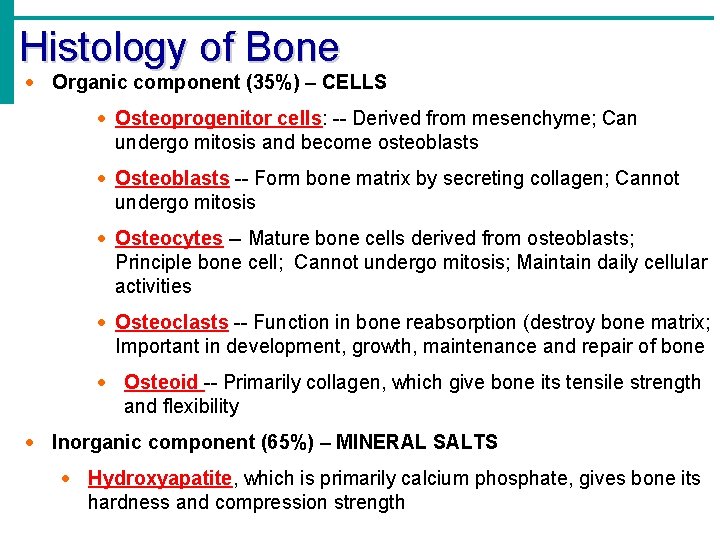
Histology of Bone · Organic component (35%) – CELLS · Osteoprogenitor cells: -- Derived from mesenchyme; Can undergo mitosis and become osteoblasts · Osteoblasts -- Form bone matrix by secreting collagen; Cannot undergo mitosis · Osteocytes -- Mature bone cells derived from osteoblasts; Principle bone cell; Cannot undergo mitosis; Maintain daily cellular activities · Osteoclasts -- Function in bone reabsorption (destroy bone matrix; Important in development, growth, maintenance and repair of bone · Osteoid -- Primarily collagen, which give bone its tensile strength and flexibility · Inorganic component (65%) – MINERAL SALTS · Hydroxyapatite, which is primarily calcium phosphate, gives bone its hardness and compression strength
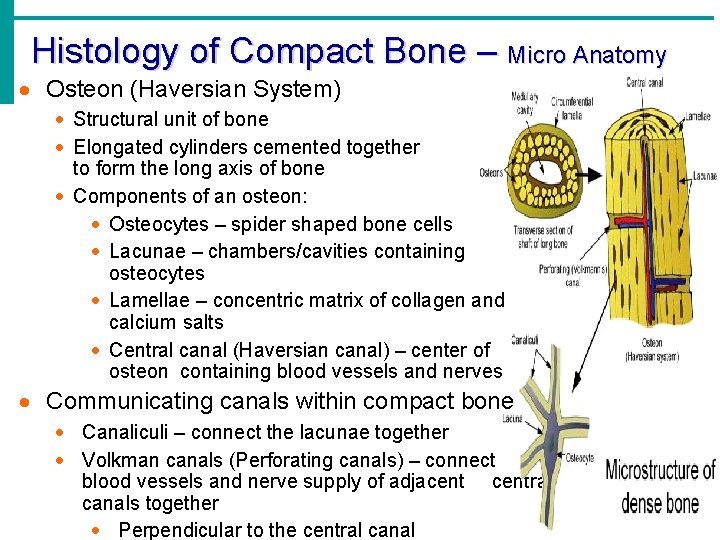
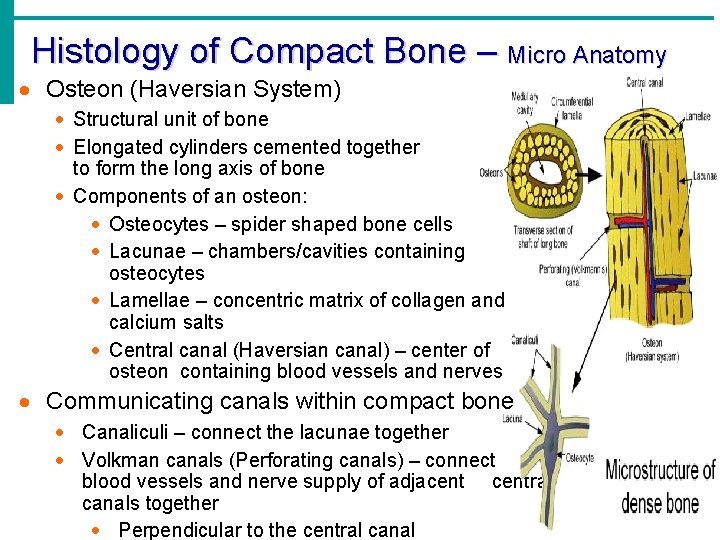
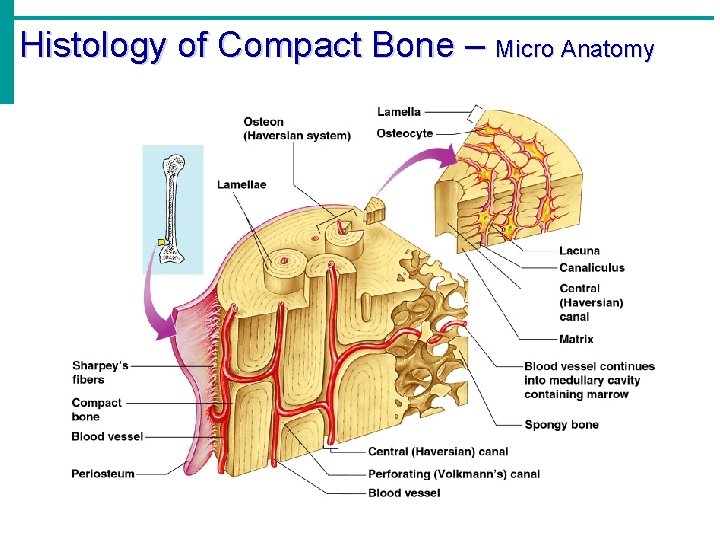
Histology of Compact Bone – Micro Anatomy · Osteon (Haversian System) · Structural unit of bone · Elongated cylinders cemented together to form the long axis of bone · Components of an osteon: · Osteocytes – spider shaped bone cells · Lacunae – chambers/cavities containing osteocytes · Lamellae – concentric matrix of collagen and calcium salts · Central canal (Haversian canal) – center of osteon containing blood vessels and nerves · Communicating canals within compact bone · Canaliculi – connect the lacunae together · Volkman canals (Perforating canals) – connect blood vessels and nerve supply of adjacentral canals together · Perpendicular to the central canal
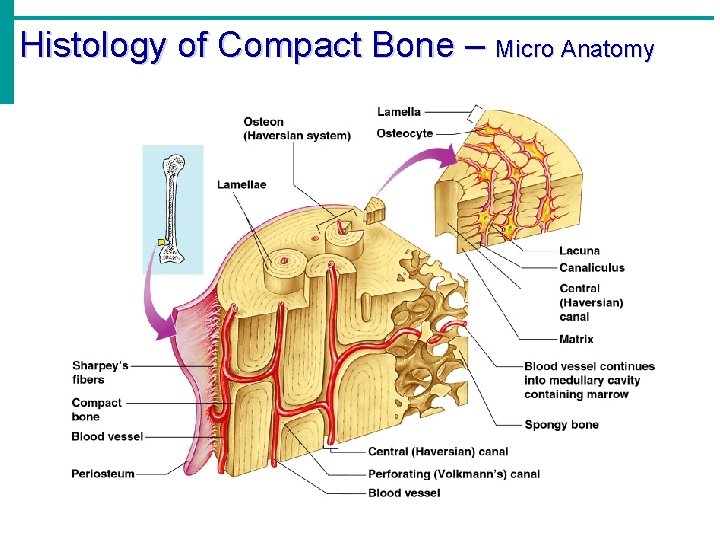
Histology of Compact Bone – Micro Anatomy
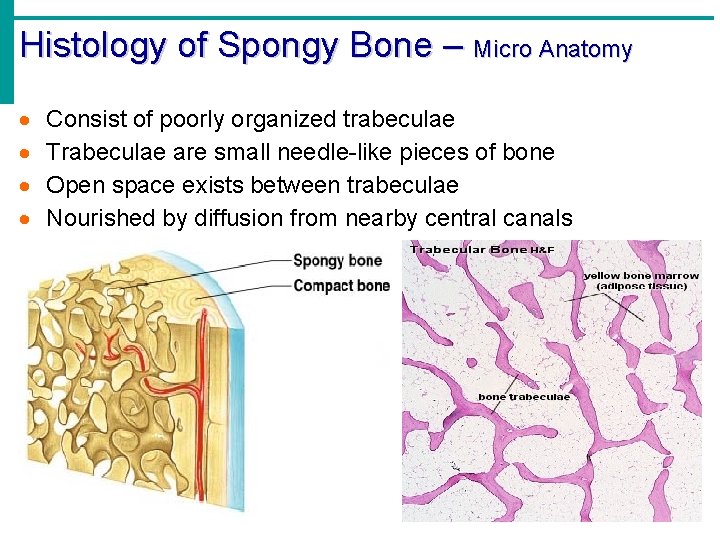
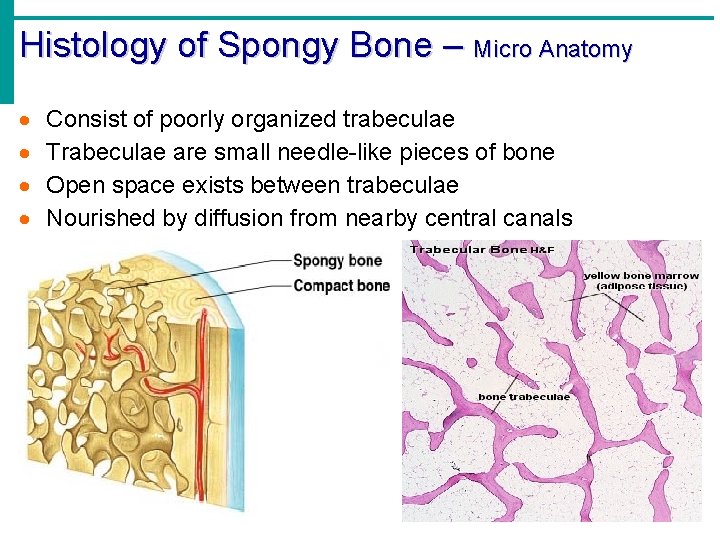
Histology of Spongy Bone – Micro Anatomy · · Consist of poorly organized trabeculae Trabeculae are small needle-like pieces of bone Open space exists between trabeculae Nourished by diffusion from nearby central canals
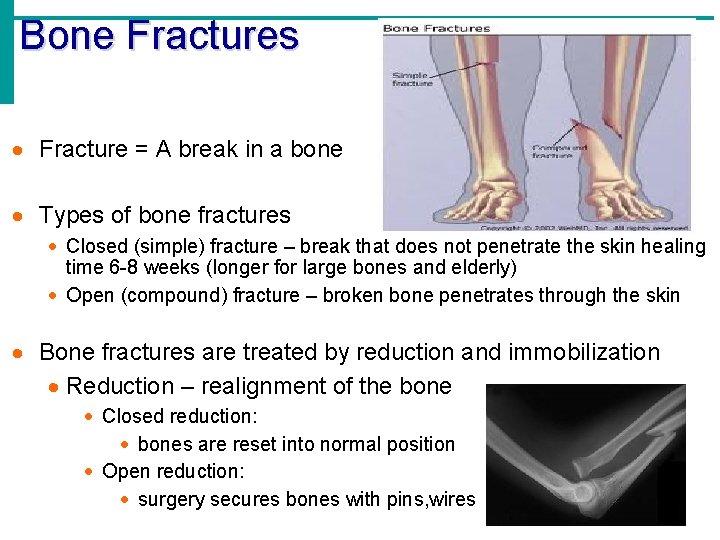
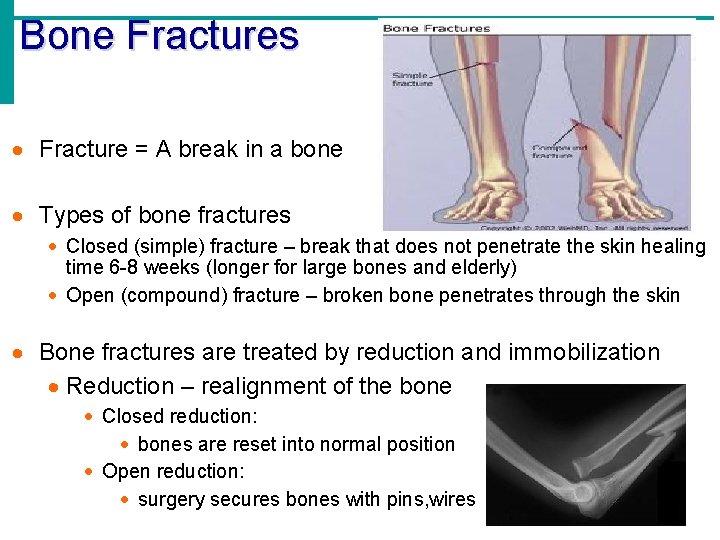
Bone Fractures · Fracture = A break in a bone · Types of bone fractures · Closed (simple) fracture – break that does not penetrate the skin healing time 6 -8 weeks (longer for large bones and elderly) · Open (compound) fracture – broken bone penetrates through the skin · Bone fractures are treated by reduction and immobilization · Reduction – realignment of the bone · Closed reduction: · bones are reset into normal position · Open reduction: · surgery secures bones with pins, wires
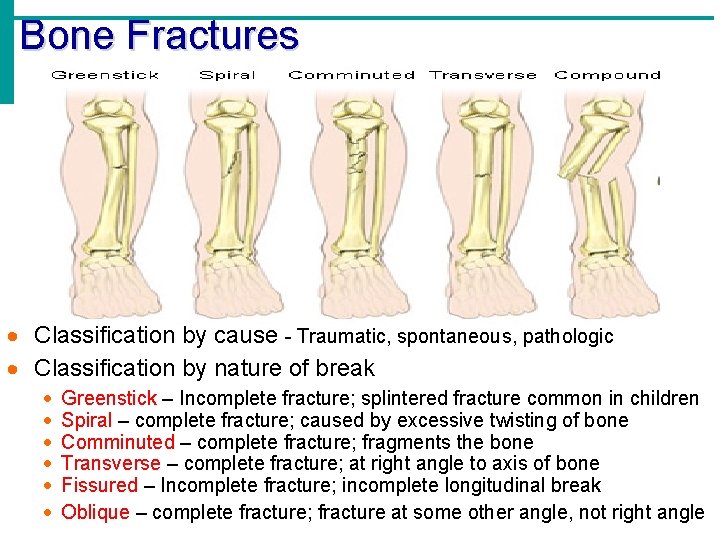
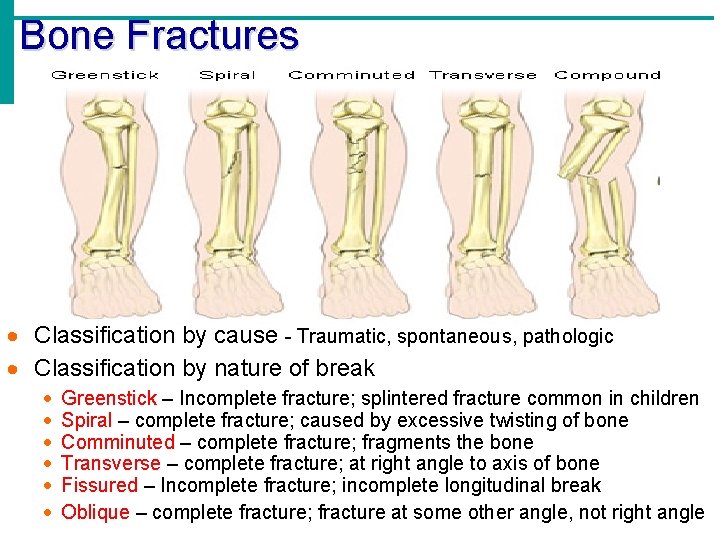
Bone Fractures · Classification by cause - Traumatic, spontaneous, pathologic · Classification by nature of break · · · Greenstick – Incomplete fracture; splintered fracture common in children Spiral – complete fracture; caused by excessive twisting of bone Comminuted – complete fracture; fragments the bone Transverse – complete fracture; at right angle to axis of bone Fissured – Incomplete fracture; incomplete longitudinal break Oblique – complete fracture; fracture at some other angle, not right angle
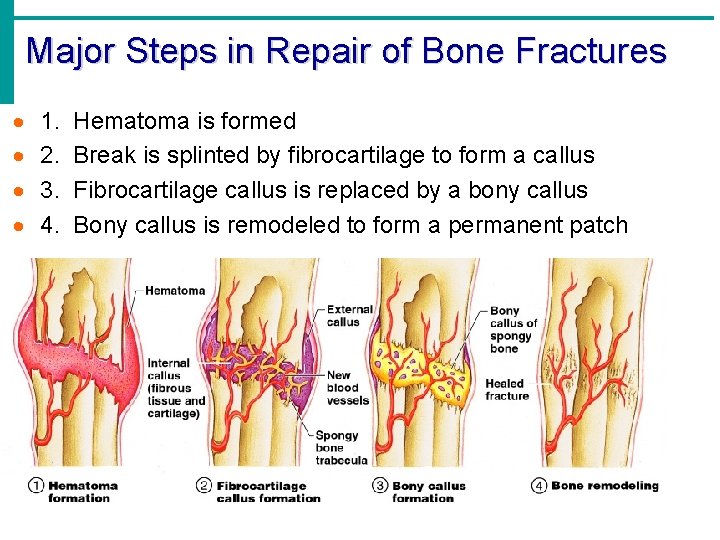
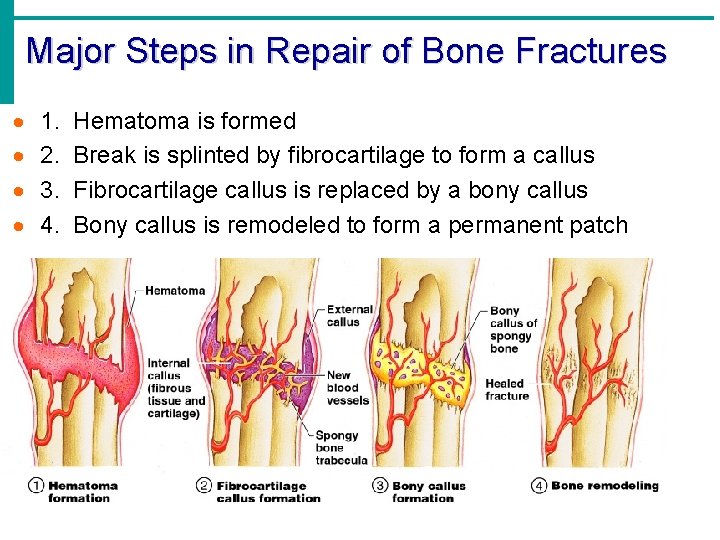
Major Steps in Repair of Bone Fractures · · 1. 2. 3. 4. Hematoma is formed Break is splinted by fibrocartilage to form a callus Fibrocartilage callus is replaced by a bony callus Bony callus is remodeled to form a permanent patch
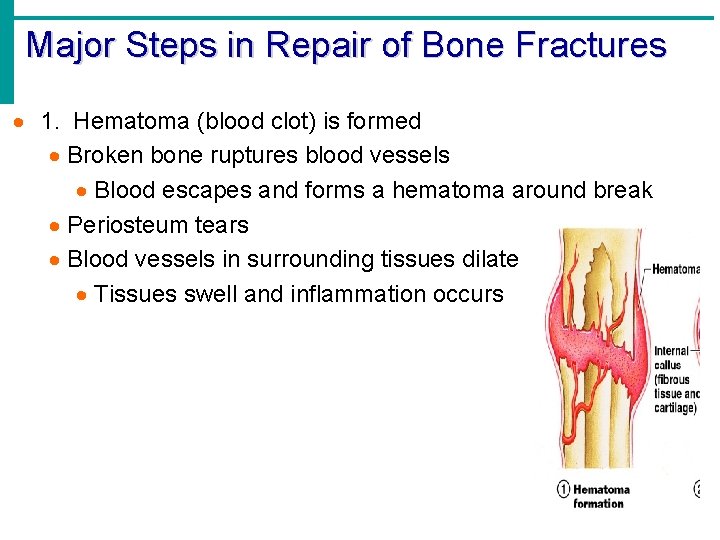
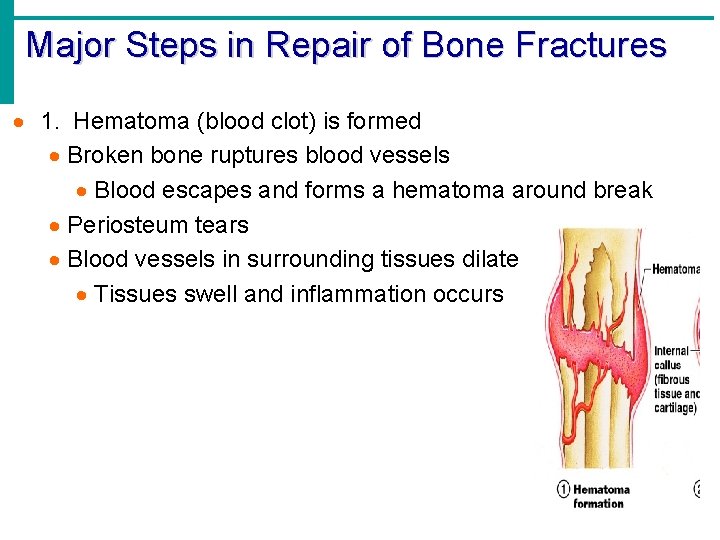
Major Steps in Repair of Bone Fractures · 1. Hematoma (blood clot) is formed · Broken bone ruptures blood vessels · Blood escapes and forms a hematoma around break · Periosteum tears · Blood vessels in surrounding tissues dilate · Tissues swell and inflammation occurs
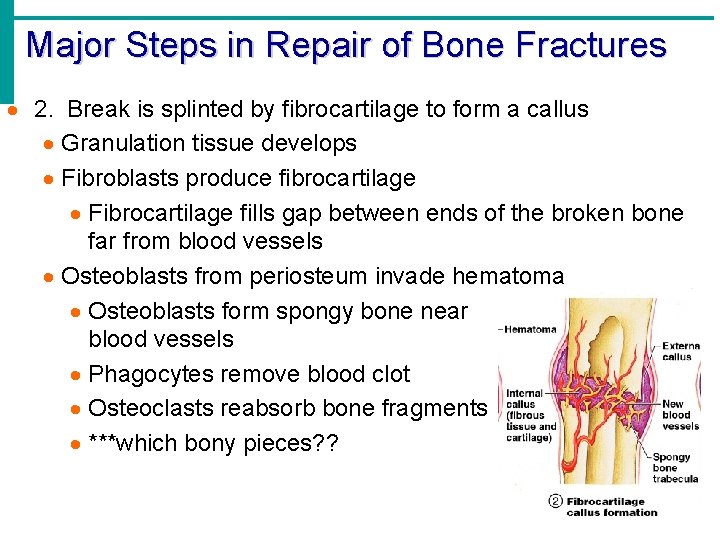
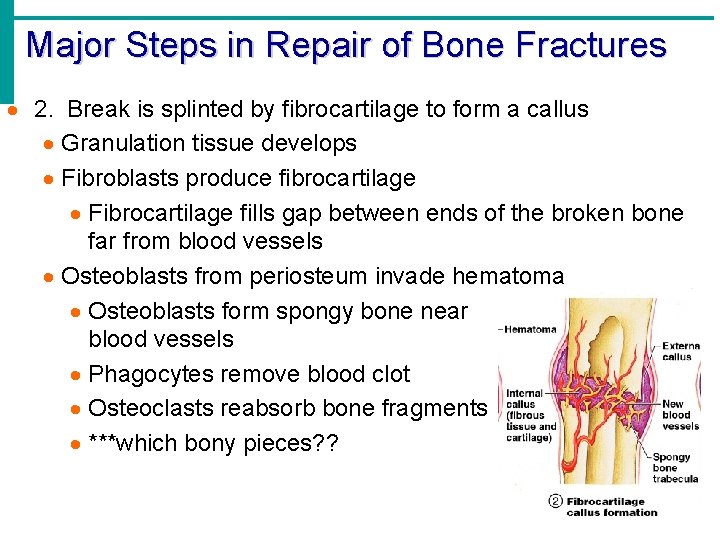
Major Steps in Repair of Bone Fractures · 2. Break is splinted by fibrocartilage to form a callus · Granulation tissue develops · Fibroblasts produce fibrocartilage · Fibrocartilage fills gap between ends of the broken bone far from blood vessels · Osteoblasts from periosteum invade hematoma · Osteoblasts form spongy bone near blood vessels · Phagocytes remove blood clot · Osteoclasts reabsorb bone fragments · ***which bony pieces? ?
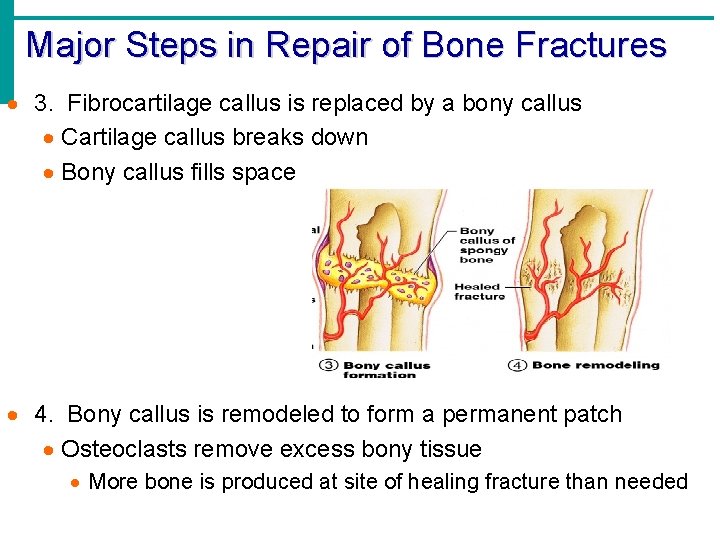
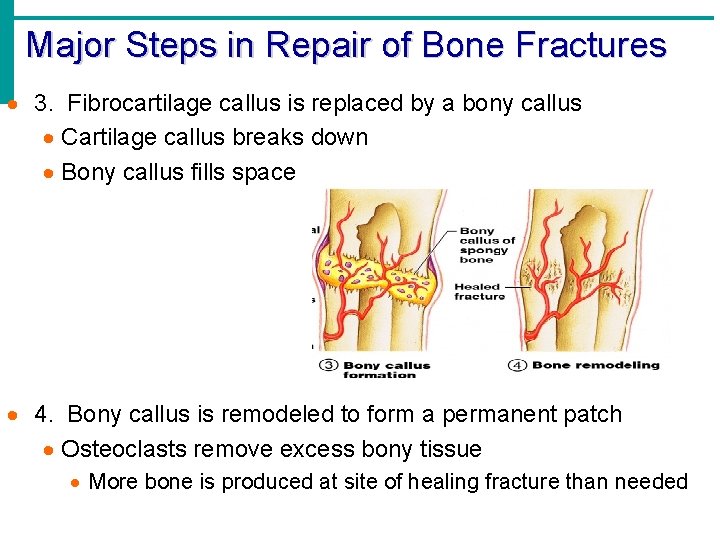
Major Steps in Repair of Bone Fractures · 3. Fibrocartilage callus is replaced by a bony callus · Cartilage callus breaks down · Bony callus fills space · 4. Bony callus is remodeled to form a permanent patch · Osteoclasts remove excess bony tissue · More bone is produced at site of healing fracture than needed
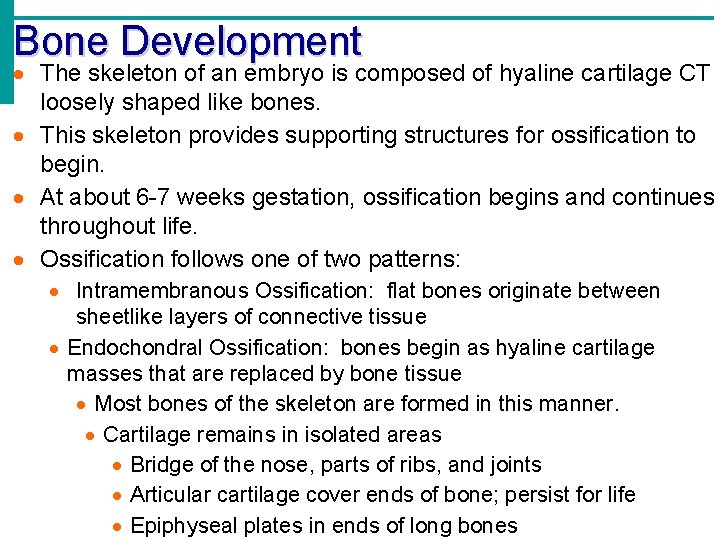
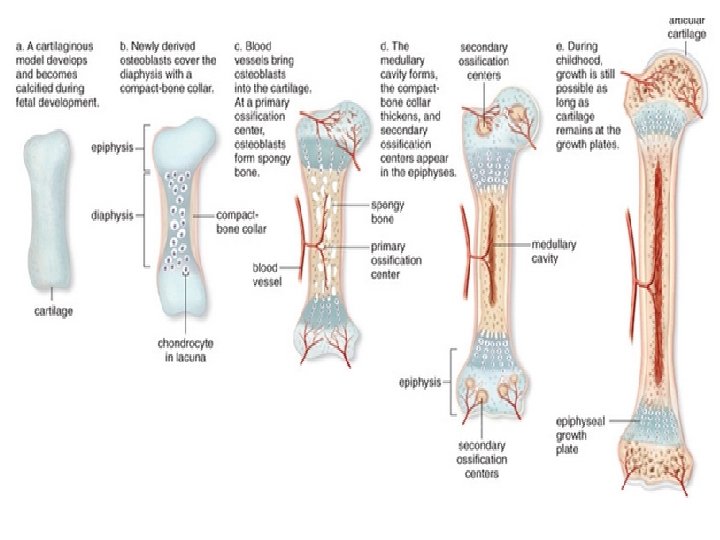
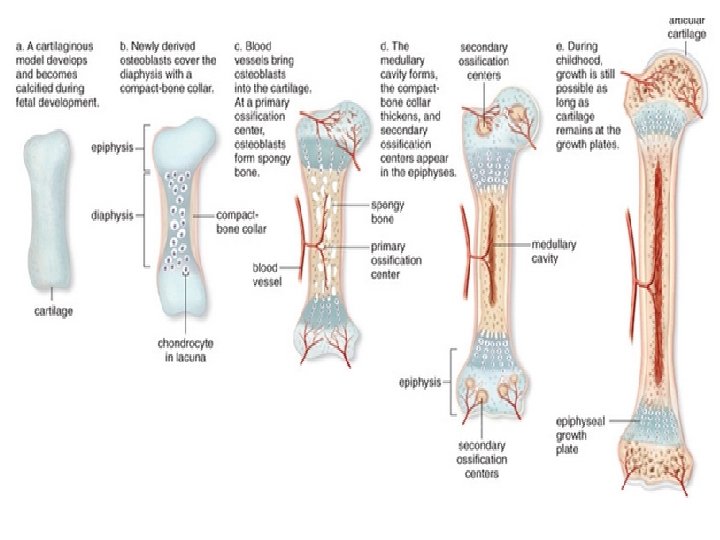
Bone Development · The skeleton of an embryo is composed of hyaline cartilage CT loosely shaped like bones. · This skeleton provides supporting structures for ossification to begin. · At about 6 -7 weeks gestation, ossification begins and continues throughout life. · Ossification follows one of two patterns: · Intramembranous Ossification: flat bones originate between sheetlike layers of connective tissue · Endochondral Ossification: bones begin as hyaline cartilage masses that are replaced by bone tissue · Most bones of the skeleton are formed in this manner. · Cartilage remains in isolated areas · Bridge of the nose, parts of ribs, and joints · Articular cartilage cover ends of bone; persist for life · Epiphyseal plates in ends of long bones
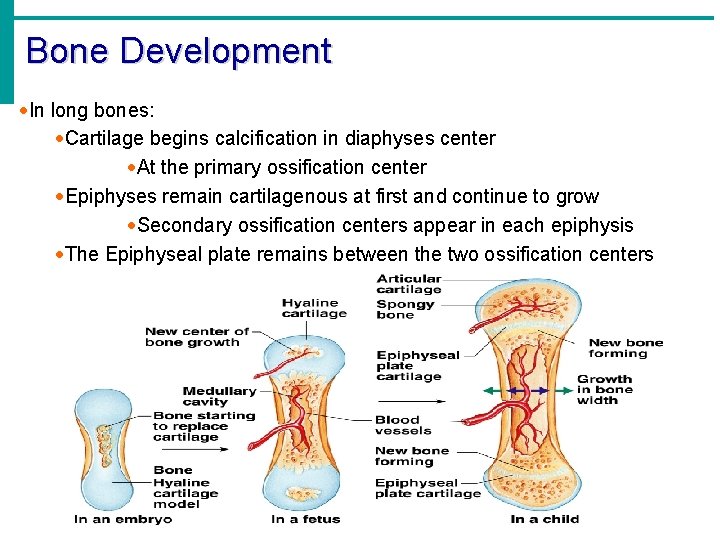
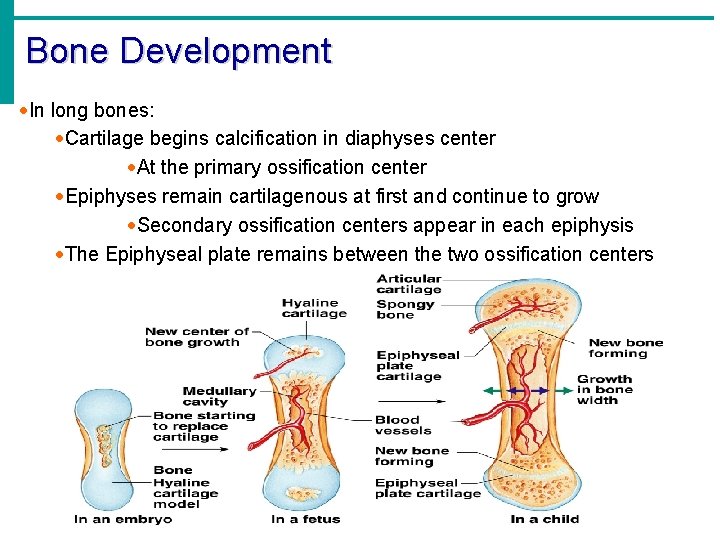
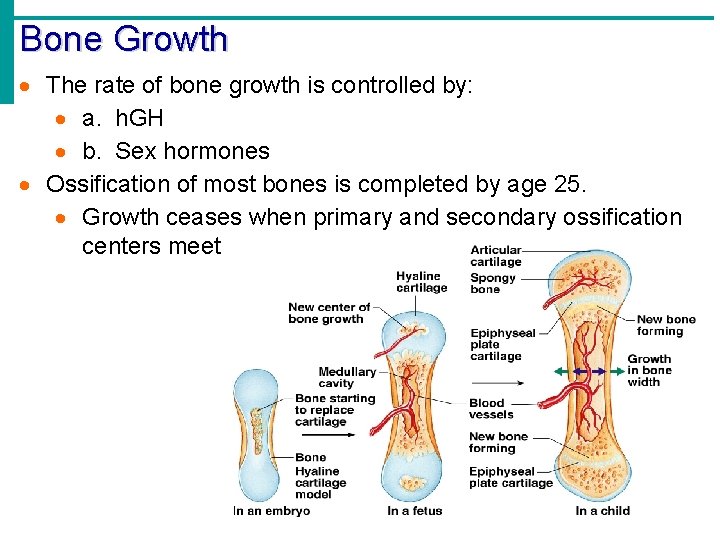
Bone Development ·In long bones: ·Cartilage begins calcification in diaphyses center ·At the primary ossification center ·Epiphyses remain cartilagenous at first and continue to grow ·Secondary ossification centers appear in each epiphysis ·The Epiphyseal plate remains between the two ossification centers
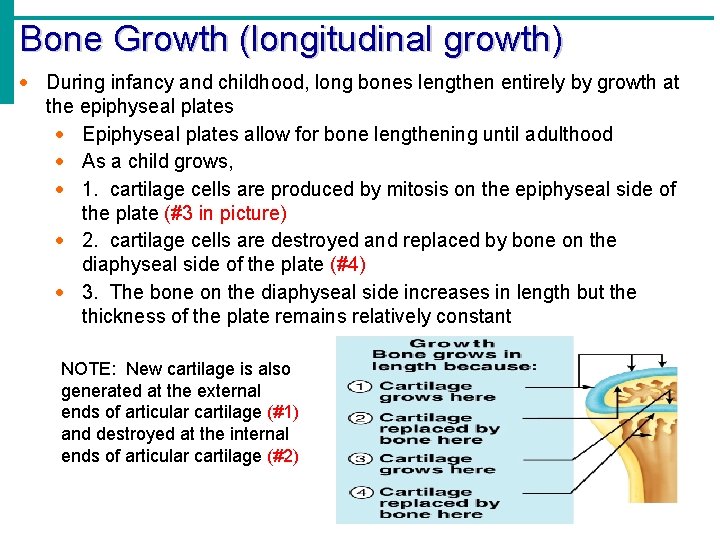
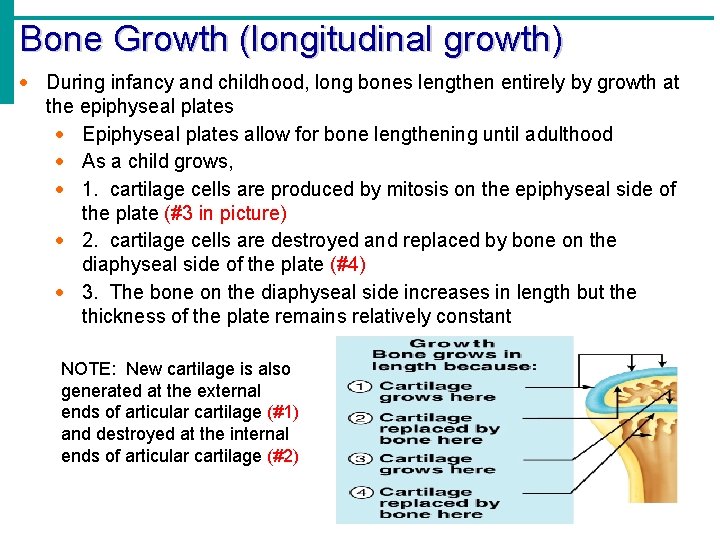
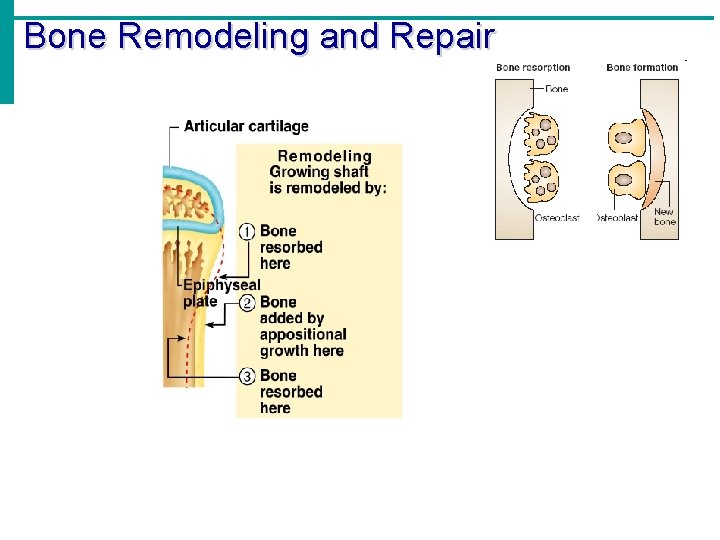
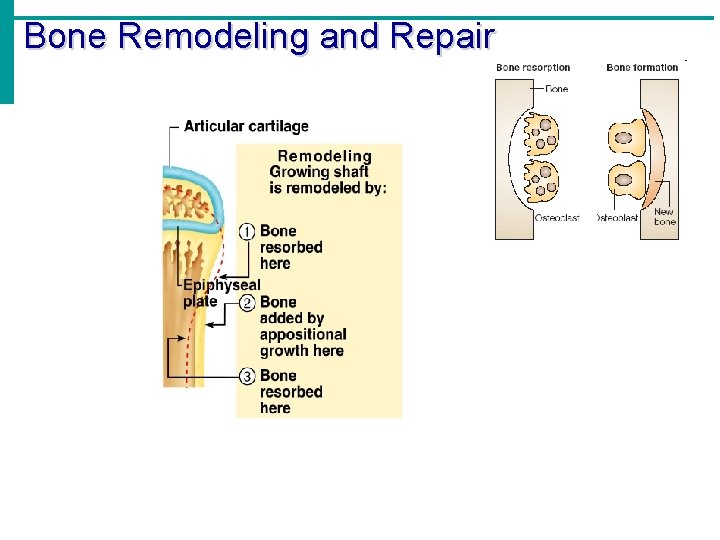
Bone Growth (longitudinal growth) · During infancy and childhood, long bones lengthen entirely by growth at the epiphyseal plates · Epiphyseal plates allow for bone lengthening until adulthood · As a child grows, · 1. cartilage cells are produced by mitosis on the epiphyseal side of the plate (#3 in picture) · 2. cartilage cells are destroyed and replaced by bone on the diaphyseal side of the plate (#4) · 3. The bone on the diaphyseal side increases in length but the thickness of the plate remains relatively constant NOTE: New cartilage is also generated at the external ends of articular cartilage (#1) and destroyed at the internal ends of articular cartilage (#2)
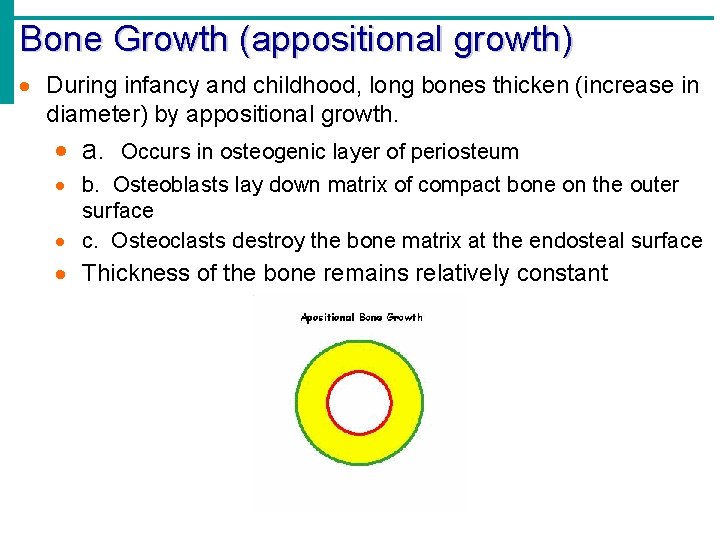
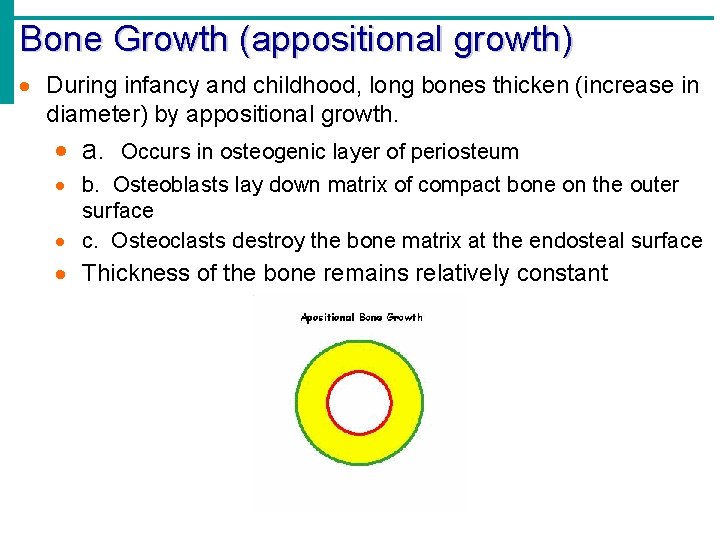
Bone Growth (appositional growth) · During infancy and childhood, long bones thicken (increase in diameter) by appositional growth. · a. Occurs in osteogenic layer of periosteum · b. Osteoblasts lay down matrix of compact bone on the outer surface · c. Osteoclasts destroy the bone matrix at the endosteal surface · Thickness of the bone remains relatively constant
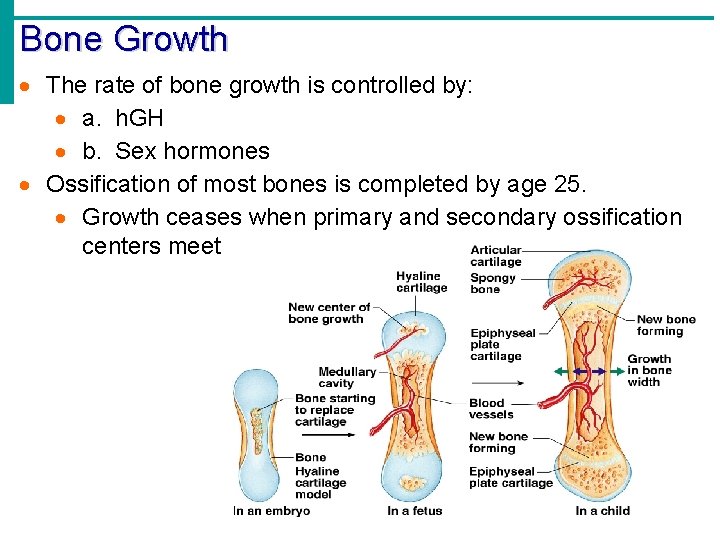
Bone Growth · The rate of bone growth is controlled by: · a. h. GH · b. Sex hormones · Ossification of most bones is completed by age 25. · Growth ceases when primary and secondary ossification centers meet
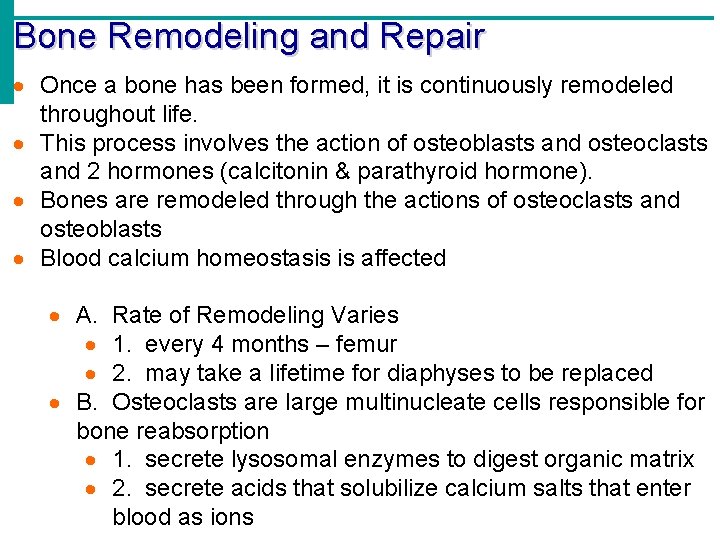
Bone Remodeling and Repair · Once a bone has been formed, it is continuously remodeled throughout life. · This process involves the action of osteoblasts and osteoclasts and 2 hormones (calcitonin & parathyroid hormone). · Bones are remodeled through the actions of osteoclasts and osteoblasts · Blood calcium homeostasis is affected · A. Rate of Remodeling Varies · 1. every 4 months – femur · 2. may take a lifetime for diaphyses to be replaced · B. Osteoclasts are large multinucleate cells responsible for bone reabsorption · 1. secrete lysosomal enzymes to digest organic matrix · 2. secrete acids that solubilize calcium salts that enter blood as ions
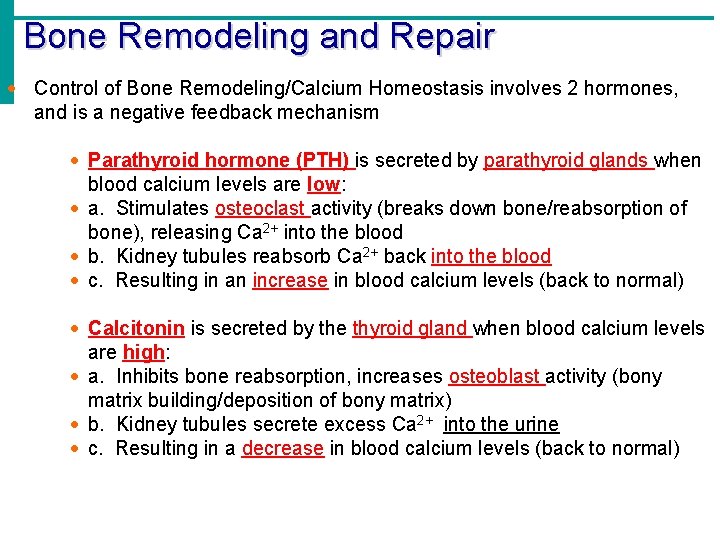
Bone Remodeling and Repair · Control of Bone Remodeling/Calcium Homeostasis involves 2 hormones, and is a negative feedback mechanism · Parathyroid hormone (PTH) is secreted by parathyroid glands when blood calcium levels are low: · a. Stimulates osteoclast activity (breaks down bone/reabsorption of bone), releasing Ca 2+ into the blood · b. Kidney tubules reabsorb Ca 2+ back into the blood · c. Resulting in an increase in blood calcium levels (back to normal) · Calcitonin is secreted by the thyroid gland when blood calcium levels are high: · a. Inhibits bone reabsorption, increases osteoblast activity (bony matrix building/deposition of bony matrix) · b. Kidney tubules secrete excess Ca 2+ into the urine · c. Resulting in a decrease in blood calcium levels (back to normal)
Bone Remodeling and Repair
Bone Remodeling and Repair · Minerals needed for bone remodeling: · Calcium – component of hydroxyapatite · Phosphorus – component of hydroxyapatite · Magnesium – needed for osteoblast activity · Boron – inhibits calcium loss · Manganese – needed for development of new matrix · Vitamins needed for bone growth, remodeling, repair: · Vitamin D – greatly increases intestinal absorption of dietary calcium and slows its urine loss · Deficiency causes rickets in children and osteomalacia in adults · Vitamin C – helps maintain bone matrix (collagen synthesis) · Deficiency causes scurvy · Vitamin A – required for bone reabsorption, controls the activity, distribution and coordination of osteoblasts & osteoclasts during development · Vitamin B 12 – plays a role in osteoblast activity
Bone Remodeling and Repair · Hormones needed for bone growth and remodeling: · human Growth Hormone (h. GH) · Secreted by the pituitary gland · Responsible for general growth of all tissues · Stimulates reproduction of cartilage cells at epiphyseal plate · (Acromegaly – picture next slide) · Sex hormones · Estrogen and Androgens (testosterone) · Aid osteoblast activity to promote new bone growth · Degenerates cartilage cells in epiphyseal plate (closes the plate) · Estrogen effect is greater than androgen (testosterone) effect, though synergistic in males · Thyroid hormones T 3 and T 4 · T 3 = triiodothreonine · T 4 = thyroxine · stimulates replacement of cartilage by bone in plate · PTH & Calcitonin – already discussed
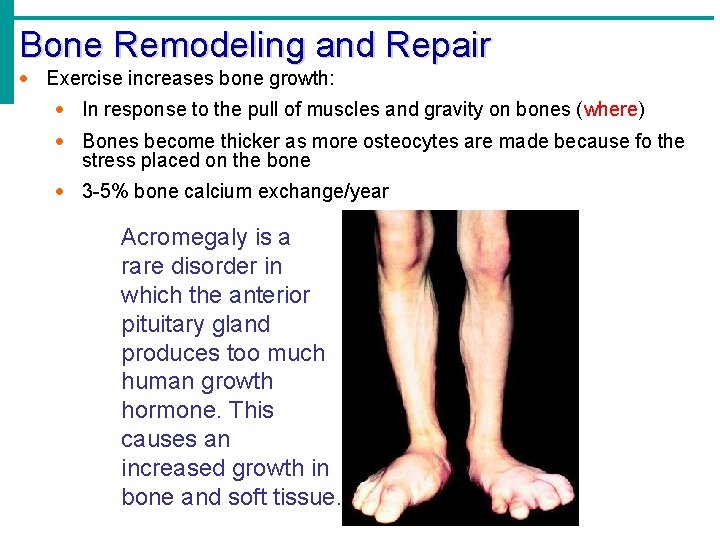
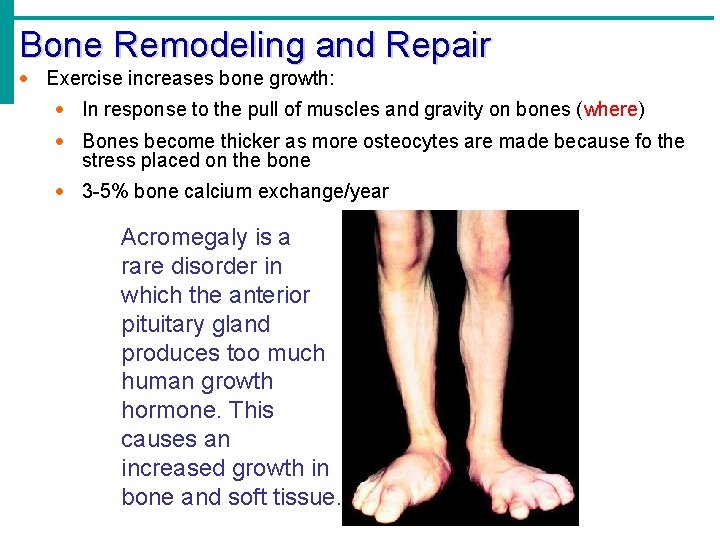
Bone Remodeling and Repair · Exercise increases bone growth: · In response to the pull of muscles and gravity on bones (where) · Bones become thicker as more osteocytes are made because fo the stress placed on the bone · 3 -5% bone calcium exchange/year Acromegaly is a rare disorder in which the anterior pituitary gland produces too much human growth hormone. This causes an increased growth in bone and soft tissue.
 Holes essential of human anatomy and physiology
Holes essential of human anatomy and physiology Holes anatomy and physiology chapter 1
Holes anatomy and physiology chapter 1 3 layers of muscle
3 layers of muscle Waistline
Waistline Chapter 1 introduction to anatomy and physiology
Chapter 1 introduction to anatomy and physiology Chapter 2 human reproductive anatomy and physiology
Chapter 2 human reproductive anatomy and physiology Human anatomy and physiology 10th edition
Human anatomy and physiology 10th edition Human anatomy & physiology edition 9
Human anatomy & physiology edition 9 Teks anatomy and physiology
Teks anatomy and physiology Anatomy and physiology unit 7 cardiovascular system
Anatomy and physiology unit 7 cardiovascular system Unit 26 animal anatomy physiology and nutrition
Unit 26 animal anatomy physiology and nutrition Unit 5 anatomy and physiology
Unit 5 anatomy and physiology Physiology of esophagus
Physiology of esophagus Unit 8 physiology of human body systems assignment 1
Unit 8 physiology of human body systems assignment 1 Lower respiratory tract
Lower respiratory tract Tattoo anatomy and physiology
Tattoo anatomy and physiology Anatomy science olympiad
Anatomy science olympiad External parts of a leaf
External parts of a leaf Anatomy and physiology of bone
Anatomy and physiology of bone Duodenal ulcer anatomy
Duodenal ulcer anatomy Sheep liver lobes
Sheep liver lobes Podbřišek
Podbřišek Iliac regions
Iliac regions Google com
Google com Chapter 14 anatomy and physiology
Chapter 14 anatomy and physiology Http://anatomy and physiology
Http://anatomy and physiology Anatomy and physiology of appendicitis
Anatomy and physiology of appendicitis Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Anatomical planes
Anatomical planes Anatomy and physiology chapter 8 special senses
Anatomy and physiology chapter 8 special senses Chapter 13 anatomy and physiology of pregnancy
Chapter 13 anatomy and physiology of pregnancy Science olympiad anatomy and physiology 2020 cheat sheet
Science olympiad anatomy and physiology 2020 cheat sheet Chapter 2 basic chemistry anatomy and physiology
Chapter 2 basic chemistry anatomy and physiology Contraction
Contraction Pancreas anatomy and physiology
Pancreas anatomy and physiology