HIV1 Rapid Test for Recent Infection Maxim Swift











- Slides: 41
HIV-1 Rapid Test for Recent Infection: Maxim Swift Recent Infection Assay (RIA) SPECIMEN COLLECTION AND STEP-WISE PROCEDURE FOR MAXIM SWIFT RIA International Laboratory Branch Division of Global HIV/AIDS & Tuberculosis Centers for Disease Control and Prevention

2 Outline • Describe the procedure for collection of whole blood specimens • Venous • Finger prick • Dried blood spots (DBS, for VL testing only) • Explain the specimen handling and storage requirements • Understand the stepwise procedure for Asante testing and interpretation of results
SPECIMEN COLLECTION: WHOLE BLOOD
4 Different Procedures for Whole Blood Collection Venous Blood Finger Prick
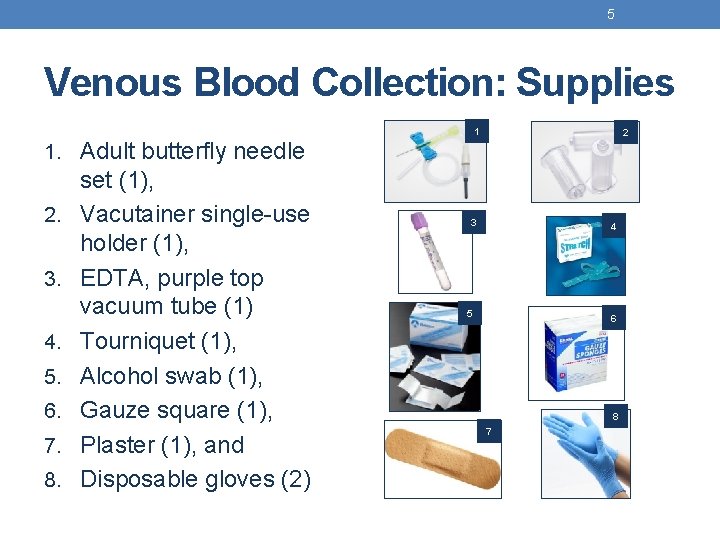
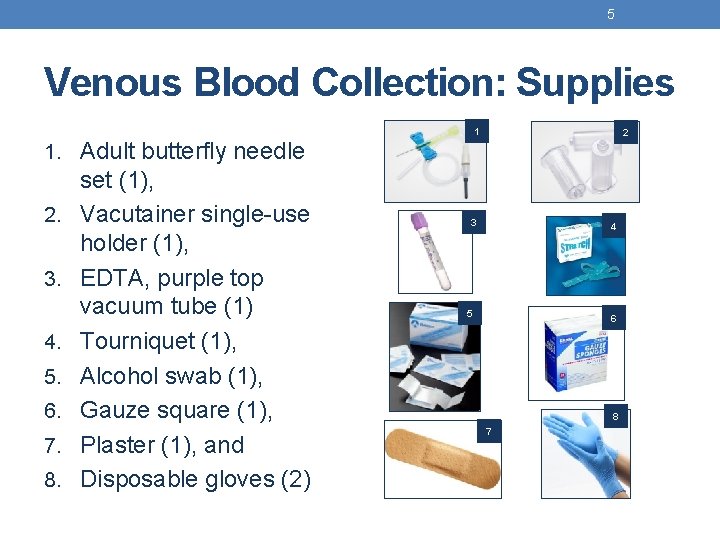
5 Venous Blood Collection: Supplies 1 2 1. Adult butterfly needle 2. 3. 4. 5. 6. 7. 8. set (1), Vacutainer single-use holder (1), EDTA, purple top vacuum tube (1) Tourniquet (1), Alcohol swab (1), Gauze square (1), Plaster (1), and Disposable gloves (2) 3 4 5 6 8 7
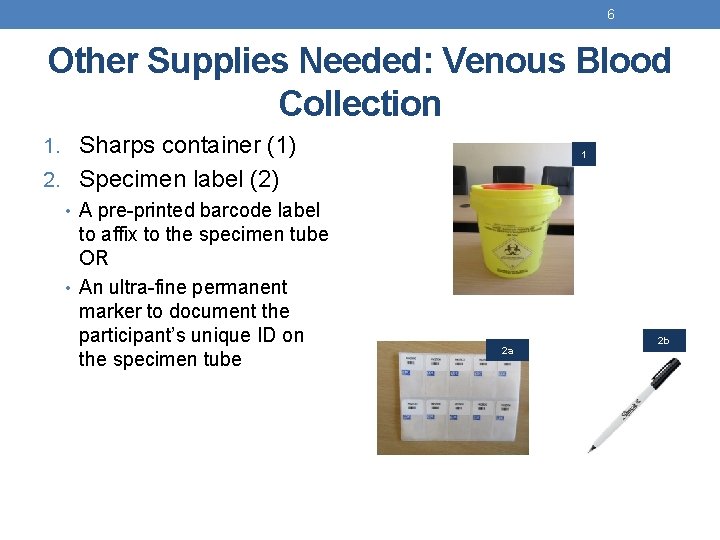
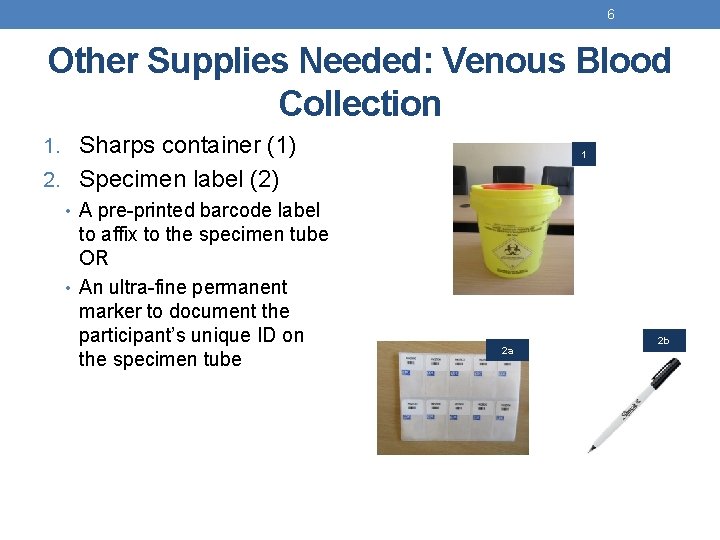
6 Other Supplies Needed: Venous Blood Collection 1. Sharps container (1) 2. Specimen label (2) • A pre-printed barcode label to affix to the specimen tube OR • An ultra-fine permanent marker to document the participant’s unique ID on the specimen tube 1 2 a 2 b
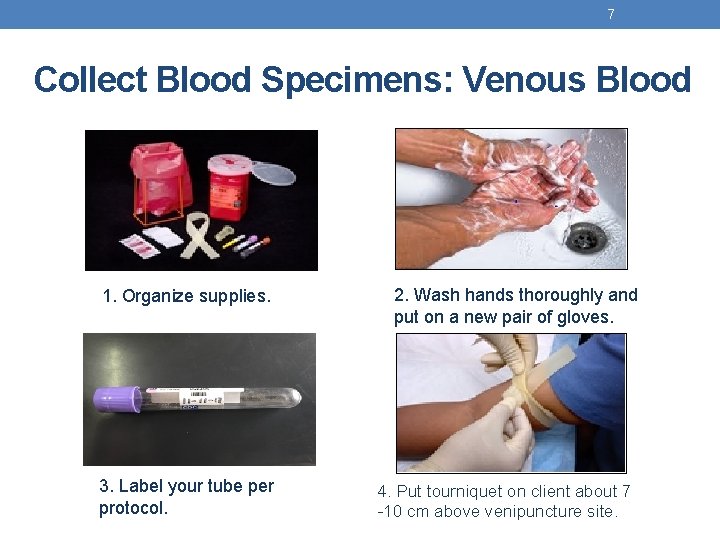
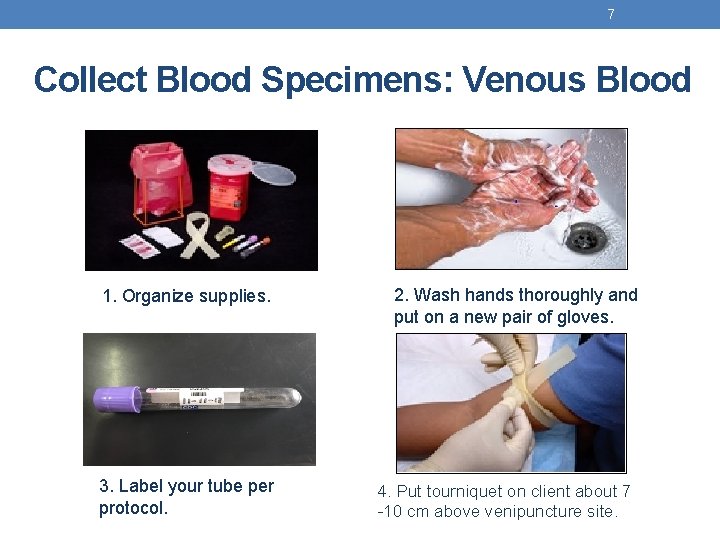
7 Collect Blood Specimens: Venous Blood 1. Organize supplies. 3. Label your tube per protocol. 2. Wash hands thoroughly and put on a new pair of gloves. 4. Put tourniquet on client about 7 -10 cm above venipuncture site.
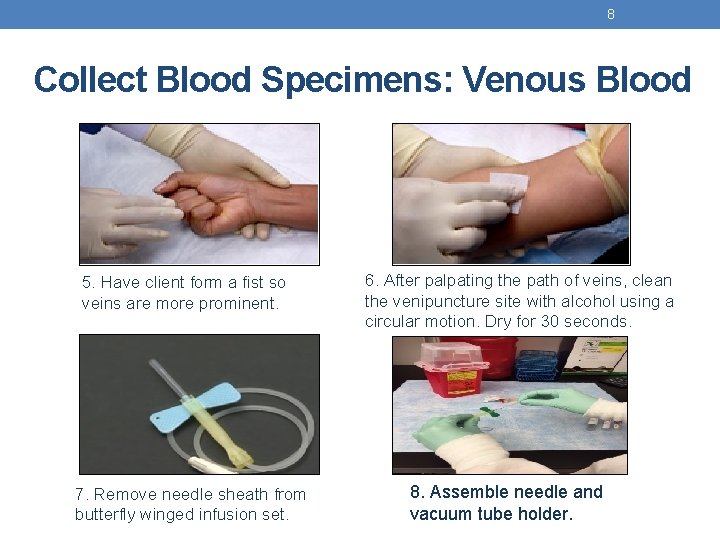
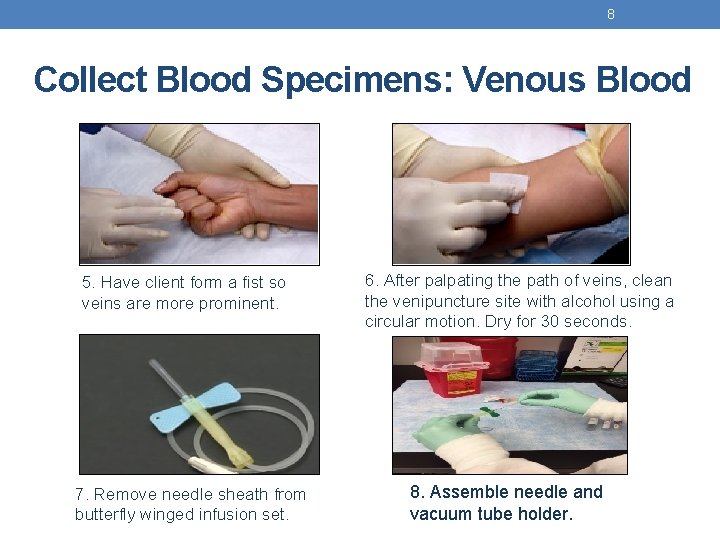
8 Collect Blood Specimens: Venous Blood 5. Have client form a fist so veins are more prominent. 7. Remove needle sheath from butterfly winged infusion set. 6. After palpating the path of veins, clean the venipuncture site with alcohol using a circular motion. Dry for 30 seconds. 8. Assemble needle and vacuum tube holder.

9 Collect Blood Specimens: Venous Blood 9. Use your thumb to pull skin tight, 1 -2” below venipuncture site. 11. Push the vacutainer tube completely into the needle. Blood should begin to flow into the tube. 10. Insert the needle, bevel side up into the vein. A “flash” of blood will enter the tubing. 12. Have participant relax the fist, and release the tourniquet.
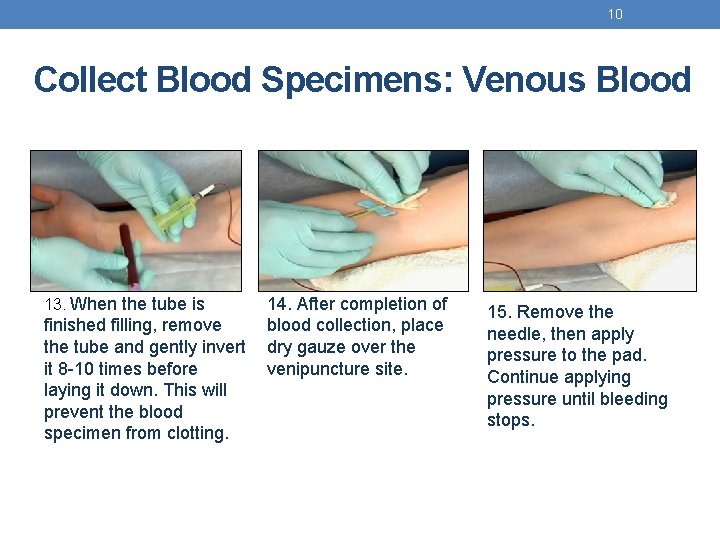
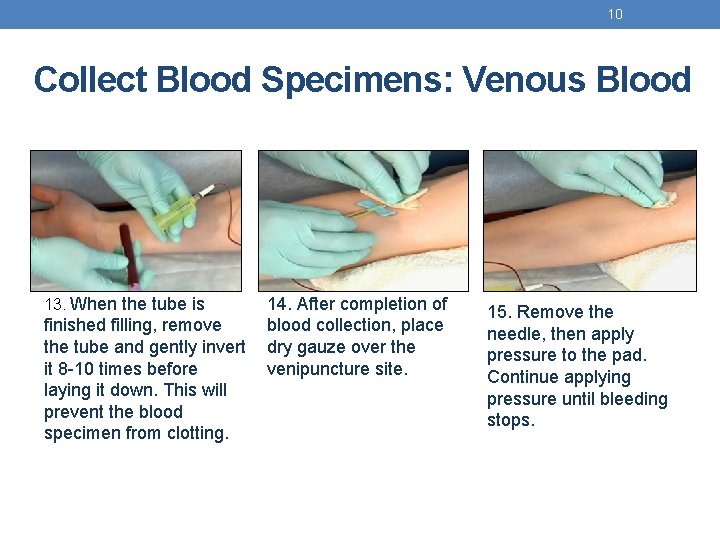
10 Collect Blood Specimens: Venous Blood 13. When the tube is finished filling, remove the tube and gently invert it 8 -10 times before laying it down. This will prevent the blood specimen from clotting. 14. After completion of blood collection, place dry gauze over the venipuncture site. 15. Remove the needle, then apply pressure to the pad. Continue applying pressure until bleeding stops.
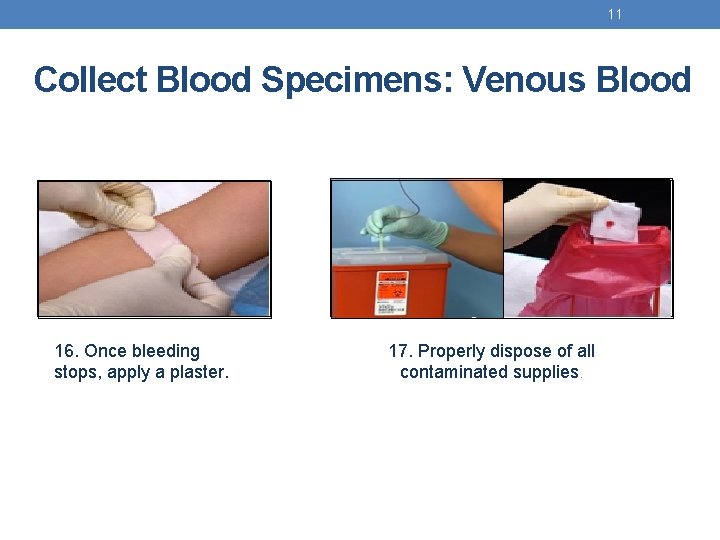
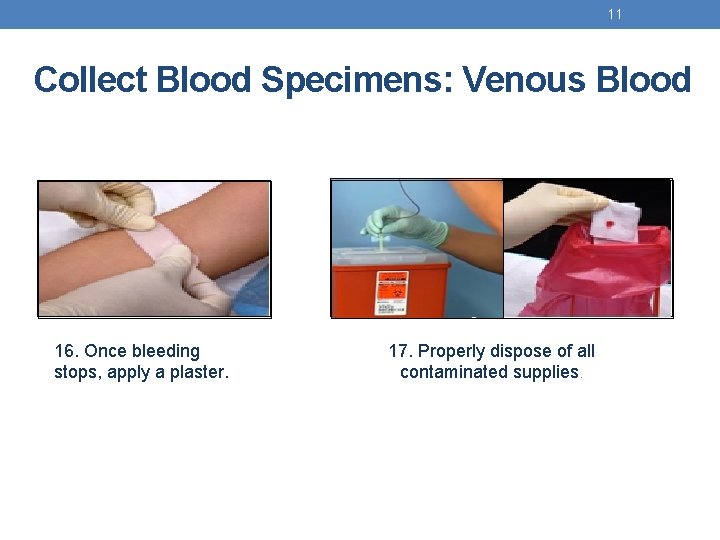
11 Collect Blood Specimens: Venous Blood 16. Once bleeding stops, apply a plaster. 17. Properly dispose of all contaminated supplies.

Venous Puncture Job Aid q For use with vacutainer tubes. q Always use universal safety precautions when handling specimens. q Keep work areas clean and organized. 1 Collect supplies 7 Remove needle sheath from butterfly winged infusion set. 13 Gently invert it 8 -10 times before laying tube down to prevent the blood from clotting. 2 3 Wash hands thoroughly and put on a new pair of gloves. 8 Assemble needle and vacuum tube holder. 14 After completion of blood collection, place dry gauze over the venipuncture site. Label tube with the client identification number. 9 Use your thumb to pull skin tight, 1 -2” below venipuncture site. 15 Remove the needle and apply pressure to the pad until bleeding stops. 4 5 Put tourniquet on client about 3 -4” above venipuncture site. Have client form a fist so veins are more prominent. 10 Insert the needle, bevel side up into the vein. A “flash” of blood will enter the tubing. 16 Once bleeding stops, apply a plaster. 6 After palpating the path of the vein, clean the venipuncture site w/alcohol using a circular motion. Allow the area to dry. 11 12 Push the vacutainer tube completely into the needle. Blood should begin to flow into the tube. Have participant relax the fist, and release the tourniquet. 17 Properly dispose of all contaminated supplies.
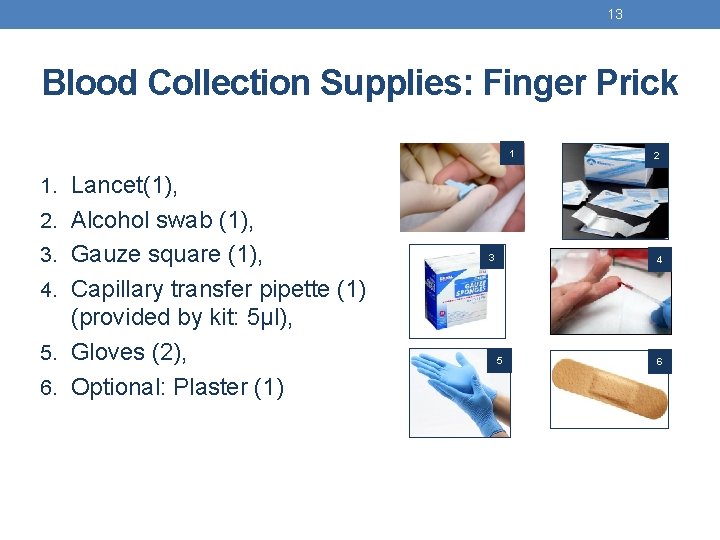
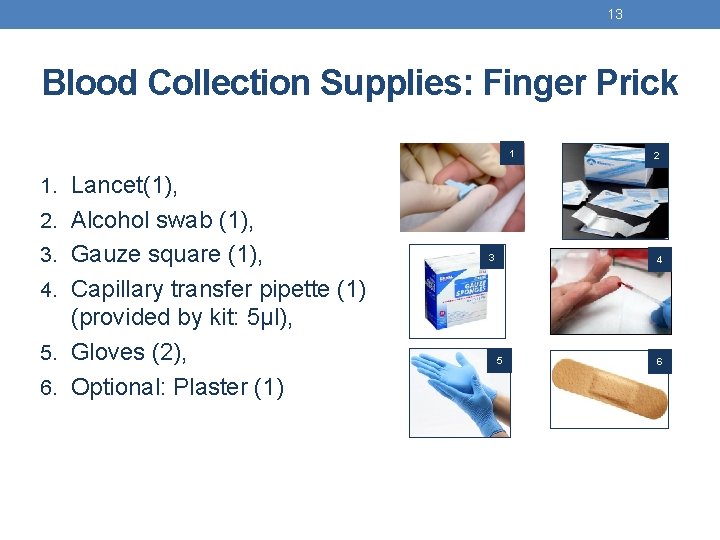
13 Blood Collection Supplies: Finger Prick 1 2 1. Lancet(1), 2. Alcohol swab (1), 3. Gauze square (1), 3 4 4. Capillary transfer pipette (1) (provided by kit: 5µl), 5. Gloves (2), 6. Optional: Plaster (1) 5 6
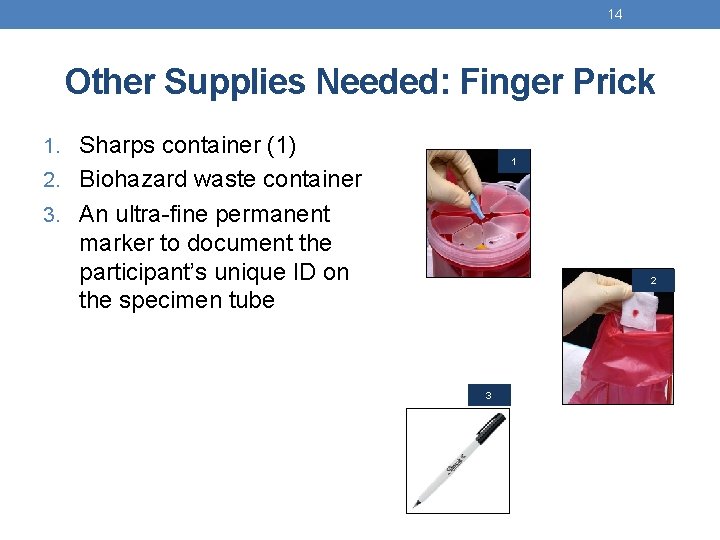
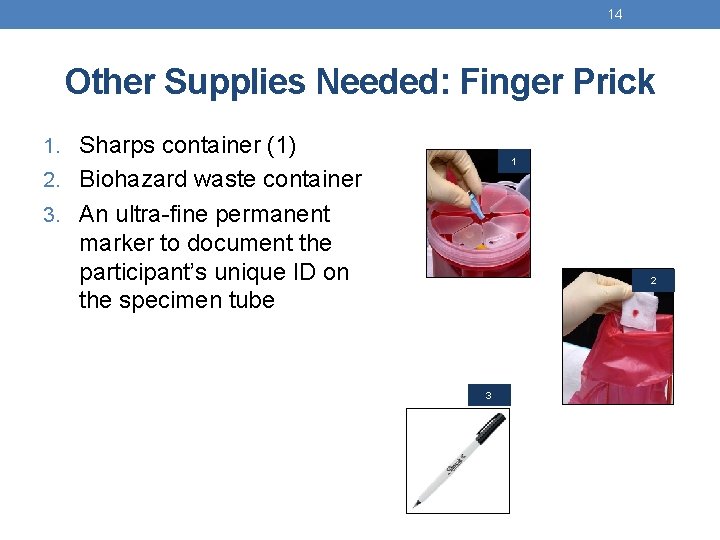
14 Other Supplies Needed: Finger Prick 1. Sharps container (1) 1 2. Biohazard waste container 3. An ultra-fine permanent marker to document the participant’s unique ID on the specimen tube 2 3
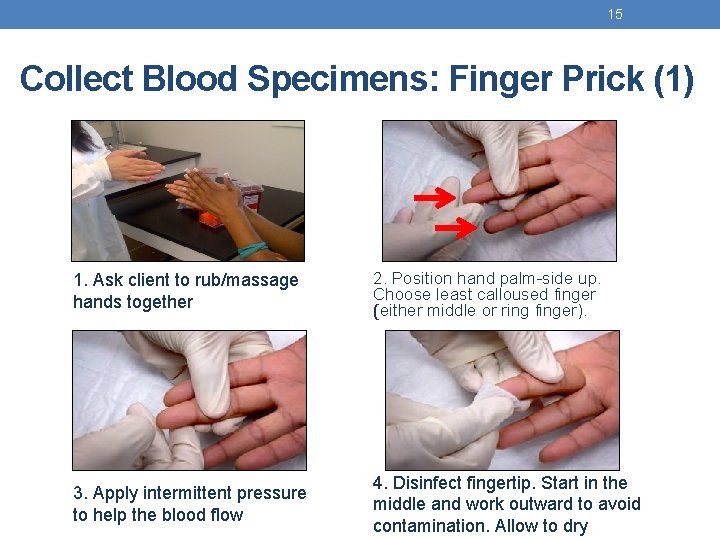
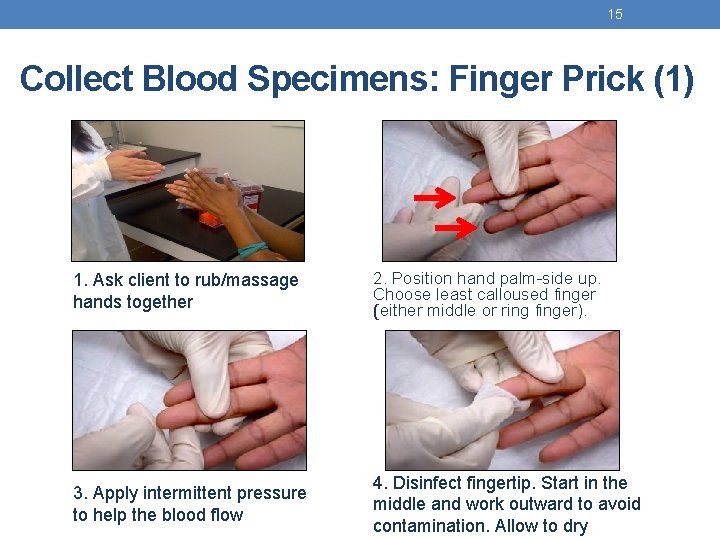
15 Collect Blood Specimens: Finger Prick (1) 1. Ask client to rub/massage hands together 2. Position hand palm-side up. Choose least calloused finger (either middle or ring finger). 3. Apply intermittent pressure to help the blood flow 4. Disinfect fingertip. Start in the middle and work outward to avoid contamination. Allow to dry
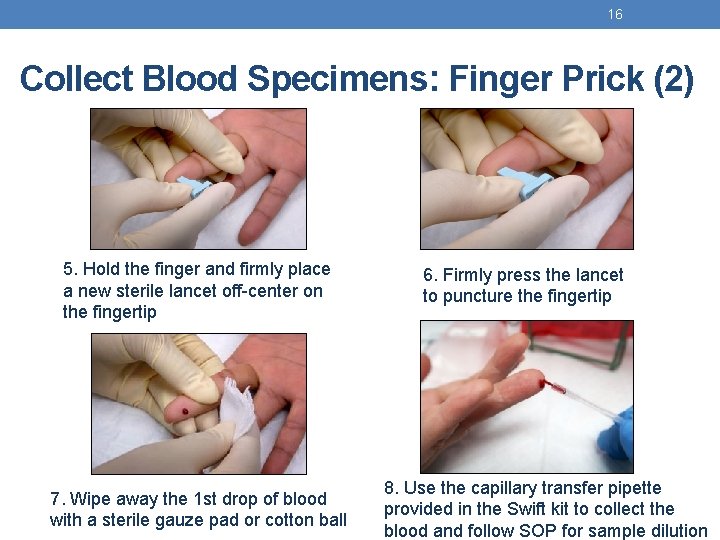
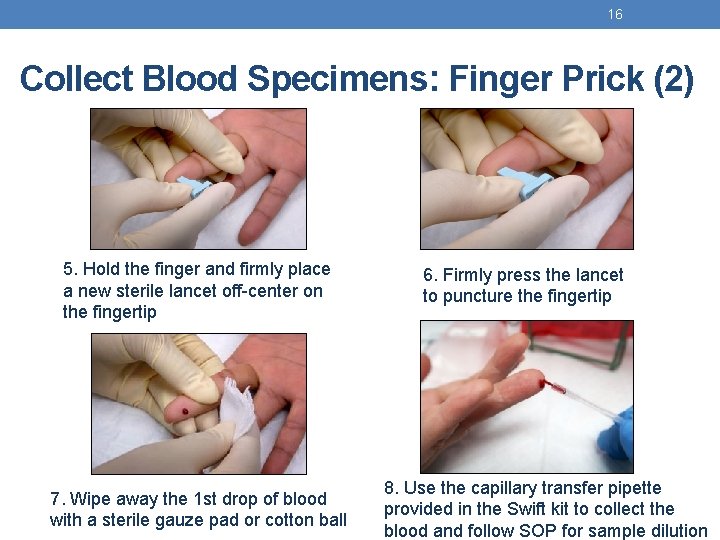
16 Collect Blood Specimens: Finger Prick (2) 5. Hold the finger and firmly place a new sterile lancet off-center on the fingertip 7. Wipe away the 1 st drop of blood with a sterile gauze pad or cotton ball 6. Firmly press the lancet to puncture the fingertip 8. Use the capillary transfer pipette provided in the Swift kit to collect the blood and follow SOP for sample dilution
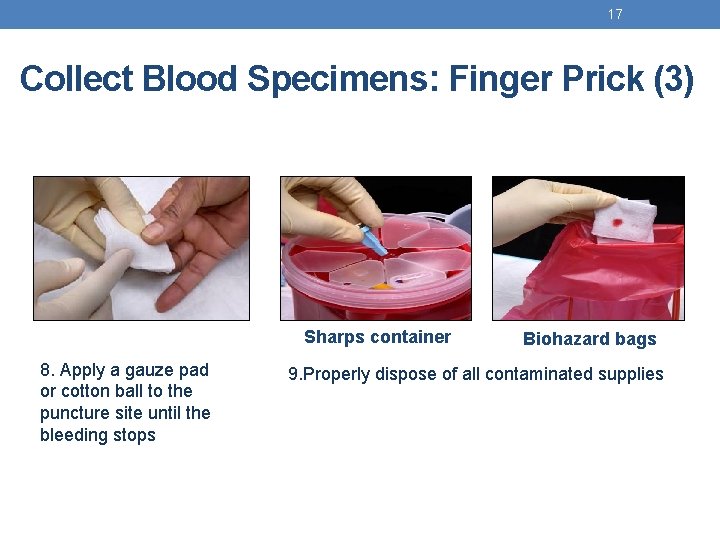
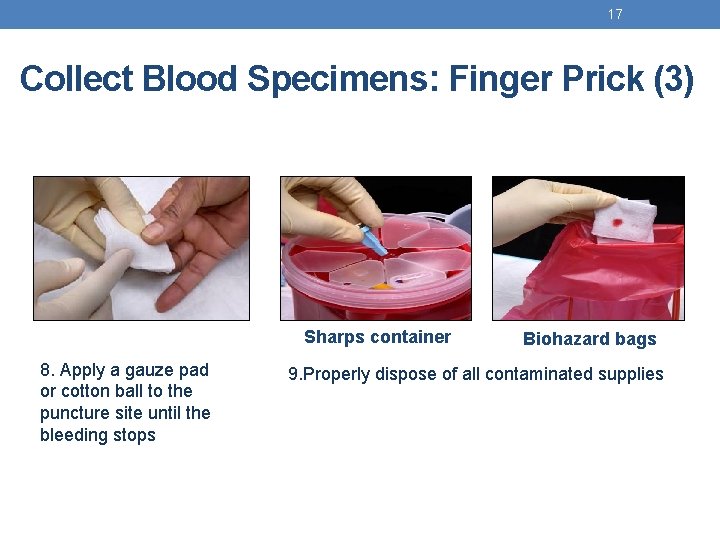
17 Collect Blood Specimens: Finger Prick (3) Sharps container 8. Apply a gauze pad or cotton ball to the puncture site until the bleeding stops Biohazard bags 9. Properly dispose of all contaminated supplies

Finger Prick Job Aid q Always use universal safety precautions when handling specimens. q Keep work areas clean and organized. 1 Ask client to rub/massage hands together. Ensure the clients hands are warm to touch. 6 Firmly press the lancet to puncture the fingertip 2 3 Position hand palmside up. Choose least calloused finger (either middle or ring finger). Apply intermittent pressure to help the blood flow. 7 8 Wipe away the 1 st drop of blood with a sterile gauze pad or cotton ball Use the capillary transfer pipette provided in the Swift kit to collect the blood. 4 Disinfect fingertip. Start in the middle and work outward to avoid contamination. Allow to dry. 9 Apply a gauze pad or cotton ball to the puncture site until the bleeding stops 5 Hold the finger and firmly place a new sterile lancet off-center on the fingertip. 10 Properly dispose of all contaminated supplies.
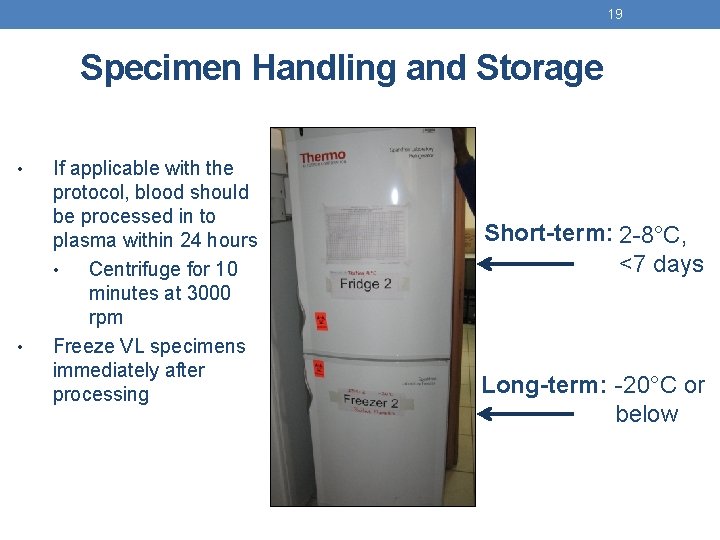
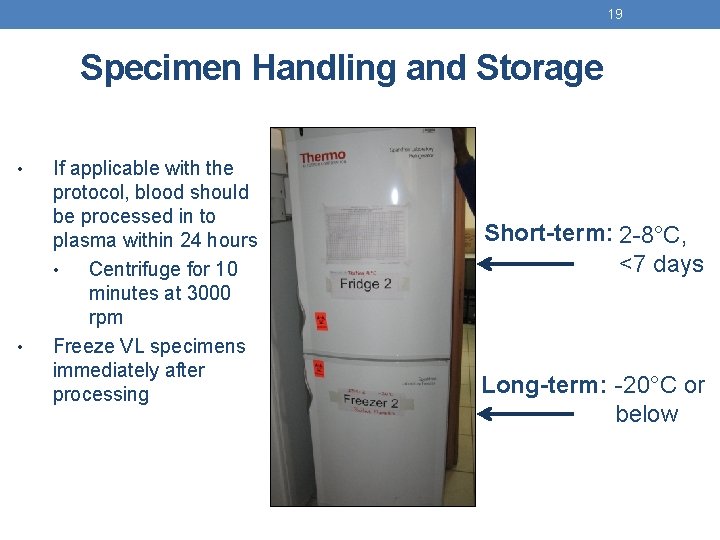
19 Specimen Handling and Storage • • If applicable with the protocol, blood should be processed in to plasma within 24 hours • Centrifuge for 10 minutes at 3000 rpm Freeze VL specimens immediately after processing Short-term: 2 -8°C, <7 days Long-term: -20°C or below
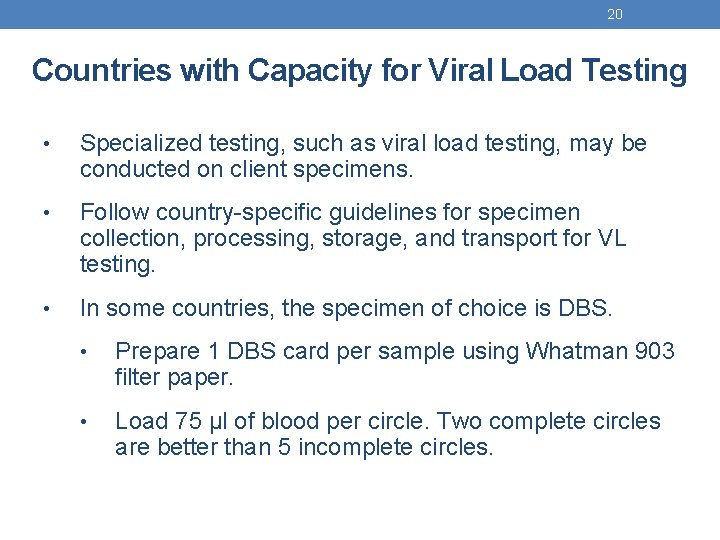
20 Countries with Capacity for Viral Load Testing • Specialized testing, such as viral load testing, may be conducted on client specimens. • Follow country-specific guidelines for specimen collection, processing, storage, and transport for VL testing. • In some countries, the specimen of choice is DBS. • Prepare 1 DBS card per sample using Whatman 903 filter paper. • Load 75 µl of blood per circle. Two complete circles are better than 5 incomplete circles.

Dried Blood Spot (DBS) Job Aid q Always use universal safety precautions when handling specimens. q Keep work areas clean and organized. q Uniformly saturate spots on Whatman 903 filter paper. Two complete circles are better than 5 incomplete circles. q Do not heat, stack or allow DBS to touch other surfaces during the drying process. q Store DBS away from direct sunlight, dust, insects. 1 Spotting Rack Drying Rack 6 Drying Rack 3 Wash hands thoroughly and put on a new pair of gloves. Collect supplies. Spotting Rack 2 7 Move card from spotting Place dry DBS cards rack to drying rack. Allow between sheets of weighing paper. blood to fully air dry horizontally (at least 4 hours) at room temperature. Avoid touching or smearing the blood. 8 Insert into sealable plastic bag. 4 Label your DBS card with the client identification number. 9 Add 3 desiccant packs into the bag for every 1 humidity card. Remove excess air from the bag prior to sealing. 5 Follow finger prick procedure. Remember to wipe away 1 st drop of blood with gauze. 10 Before shipment insert bundled DBS and appropriate documentation into ripresistant envelope Apply blood to card to uniformly saturate entire circle.
STEP-BY-STEP PROCEDURE FOR MAXIM SWIFT RTRI
23 Before You Start Testing… • Check kit before use, use only kits that have not expired and test devices that are not damaged. • Keep kits stored at 2 - 30°C • If kits were stored below room temperature, bring them to room temperature before testing • Bring stored specimens from refrigerator to room temperature prior to use. • Always use universal safety precautions when handling specimens. • Keep work areas clean and organized.
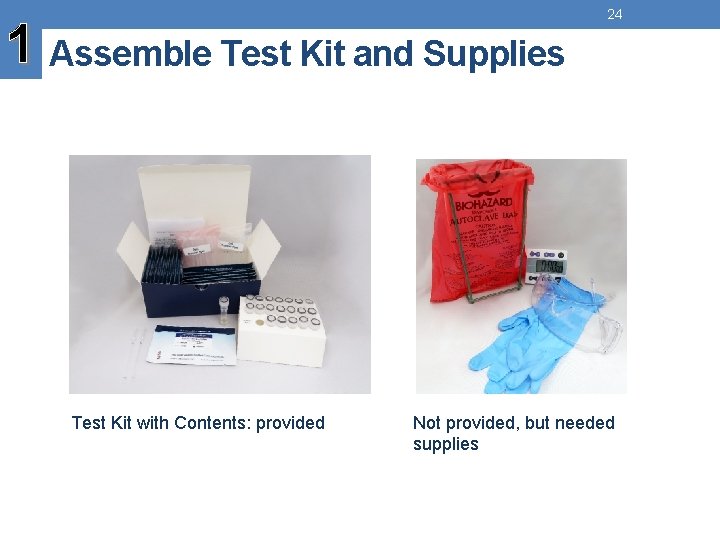
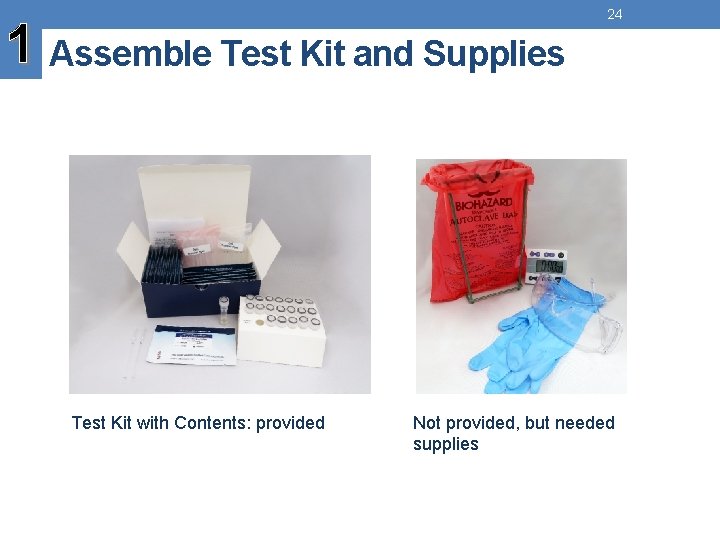
1 Assemble Test Kit and Supplies Test Kit with Contents: provided 24 Not provided, but needed supplies
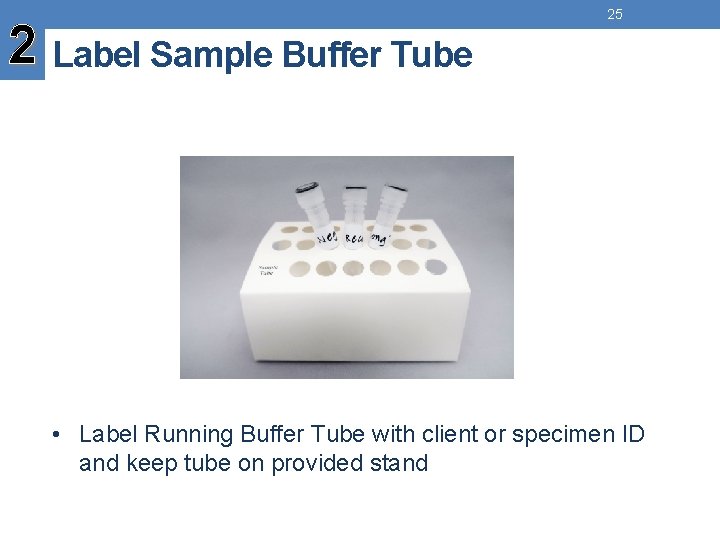
2 Label Sample Buffer Tube 25 • Label Running Buffer Tube with client or specimen ID and keep tube on provided stand
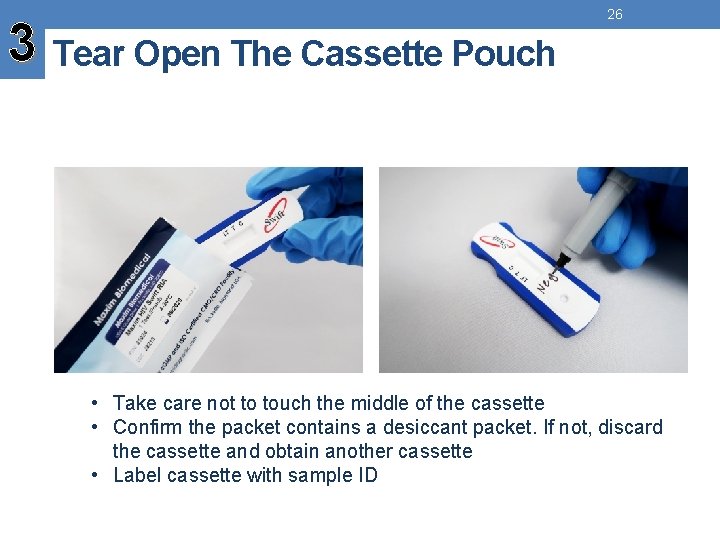
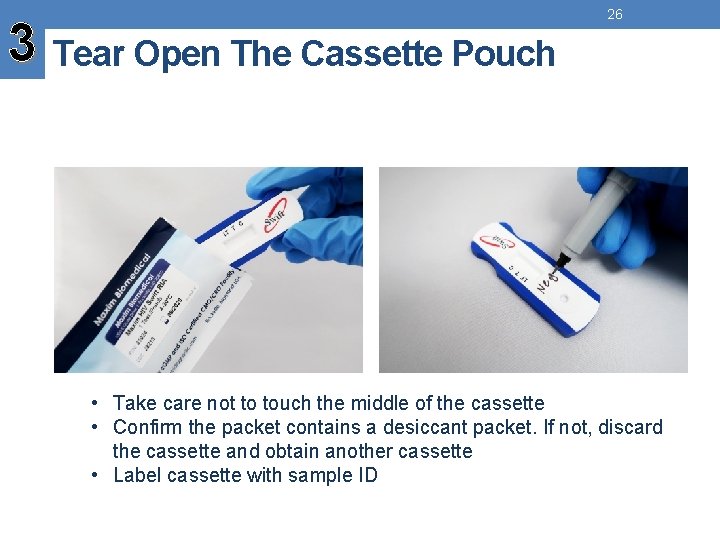
3 Tear Open The Cassette Pouch 26 • Take care not to touch the middle of the cassette • Confirm the packet contains a desiccant packet. If not, discard the cassette and obtain another cassette • Label cassette with sample ID
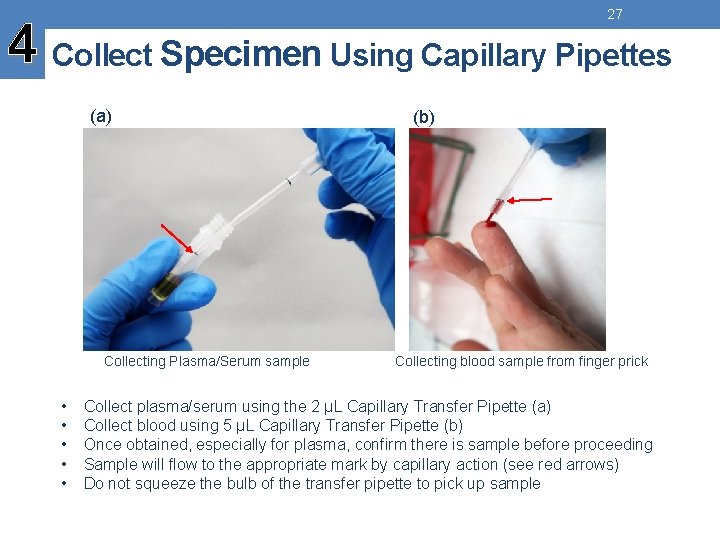
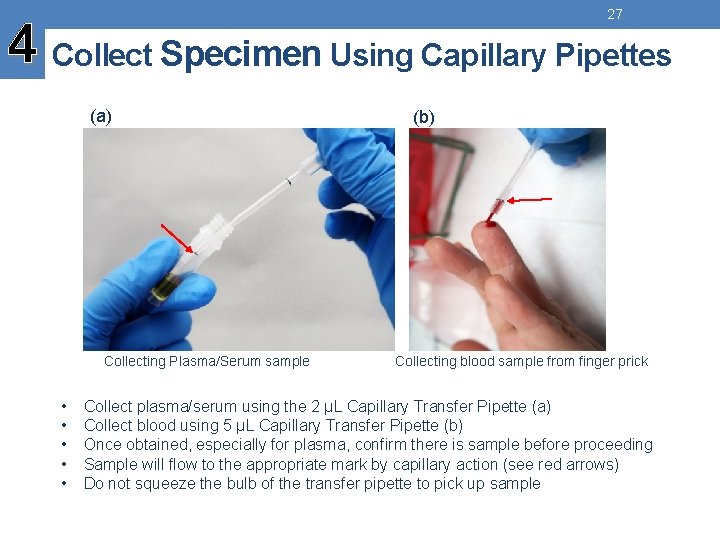
27 4 Collect Specimen Using Capillary Pipettes (a) Collecting Plasma/Serum sample • • • (b) Collecting blood sample from finger prick Collect plasma/serum using the 2 µL Capillary Transfer Pipette (a) Collect blood using 5 µL Capillary Transfer Pipette (b) Once obtained, especially for plasma, confirm there is sample before proceeding Sample will flow to the appropriate mark by capillary action (see red arrows) Do not squeeze the bulb of the transfer pipette to pick up sample

5 Transfer Sample into the Running 28 Buffer Tube and Mix • Transfer sample directly into the labelled Running Buffer Tube • Gently squeeze and release the bulb of capillary transfer pipette several times to thoroughly mix the specimen into the Running Buffer • Minimize the introduction of air bubbles into the buffer as much as possible while mixing
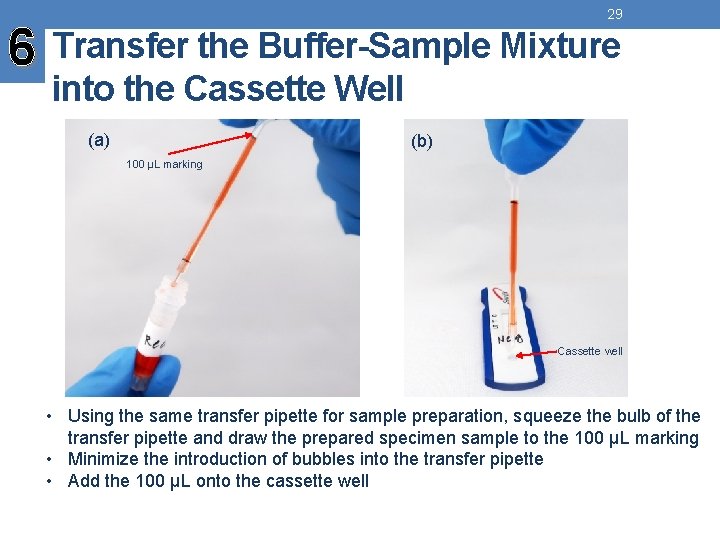
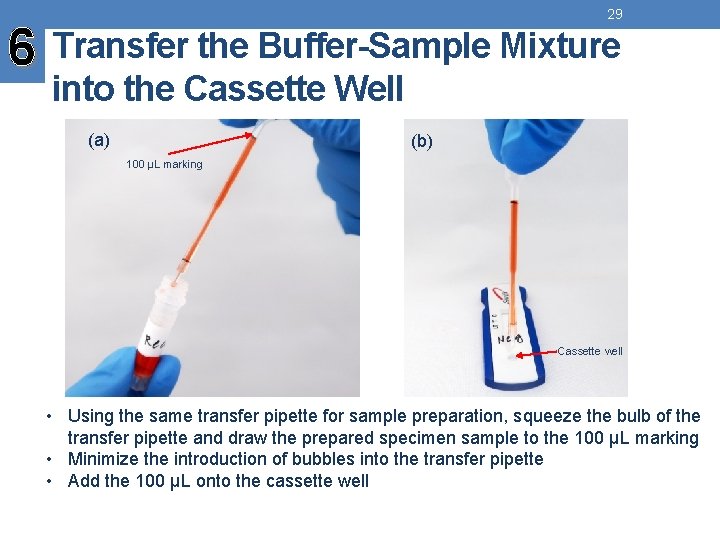
29 6 Transfer the Buffer-Sample Mixture into the Cassette Well (a) (b) 100 µL marking Cassette well • Using the same transfer pipette for sample preparation, squeeze the bulb of the transfer pipette and draw the prepared specimen sample to the 100 µL marking • Minimize the introduction of bubbles into the transfer pipette • Add the 100 µL onto the cassette well

30 7 Discard the Capillary Pipette into a Biohazard Bag

8 Start Timer (20 Minutes) 31
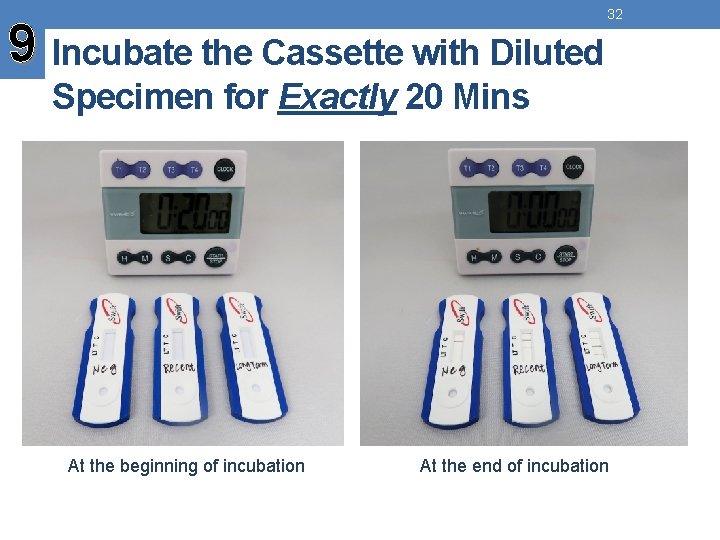
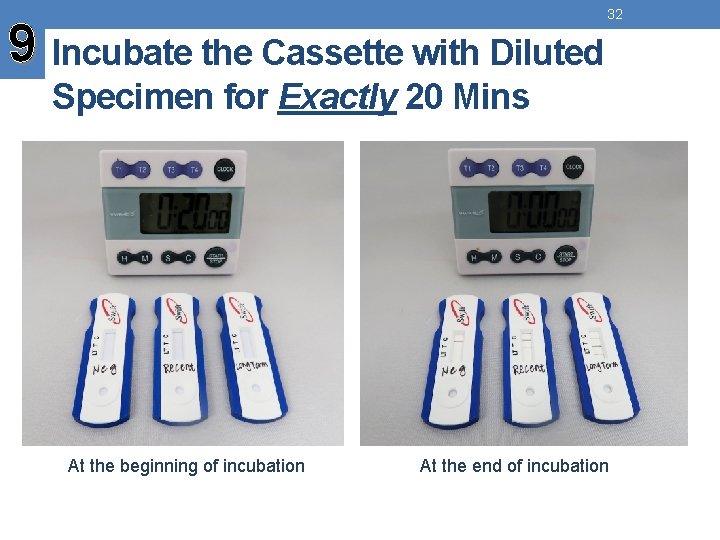
9 Incubate the Cassette with Diluted 32 Specimen for Exactly 20 Mins At the beginning of incubation At the end of incubation
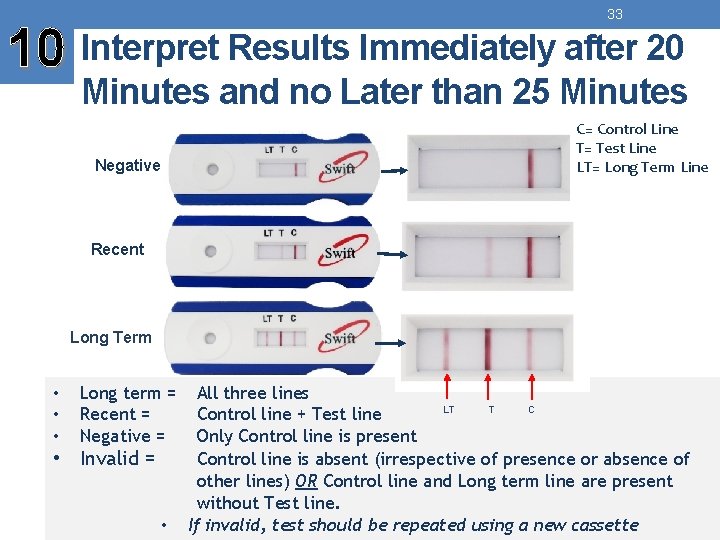
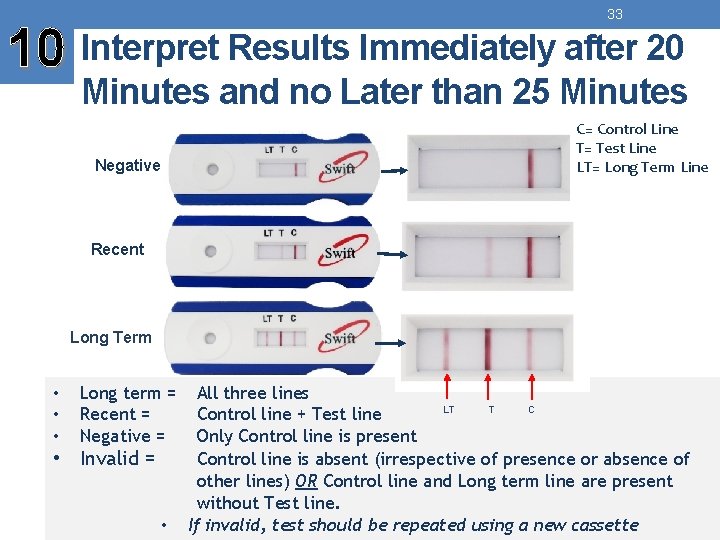
33 10 Interpret Results Immediately after 20 Minutes and no Later than 25 Minutes Negative C= Control Line T= Test Line LT= Long Term Line Recent Long Term • • • Long term = Recent = Negative = • Invalid = • All three lines C LT T Control line + Test line Only Control line is present Control line is absent (irrespective of presence or absence of other lines) OR Control line and Long term line are present without Test line. If invalid, test should be repeated using a new cassette

34 Examples: Long-Term (varying intensities) C= Control Line T= Test Line LT= Long Term Line
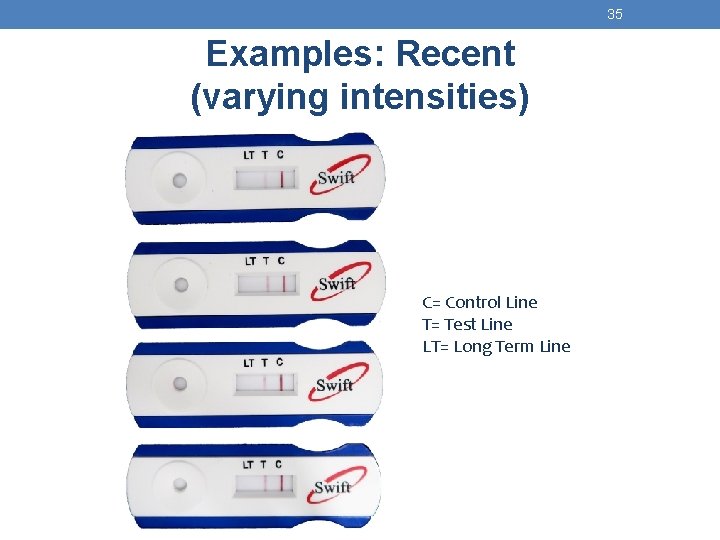
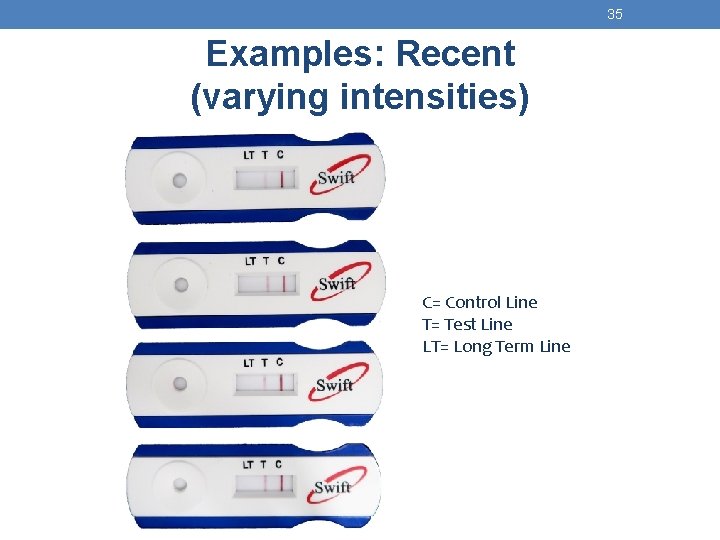
35 Examples: Recent (varying intensities) C= Control Line T= Test Line LT= Long Term Line
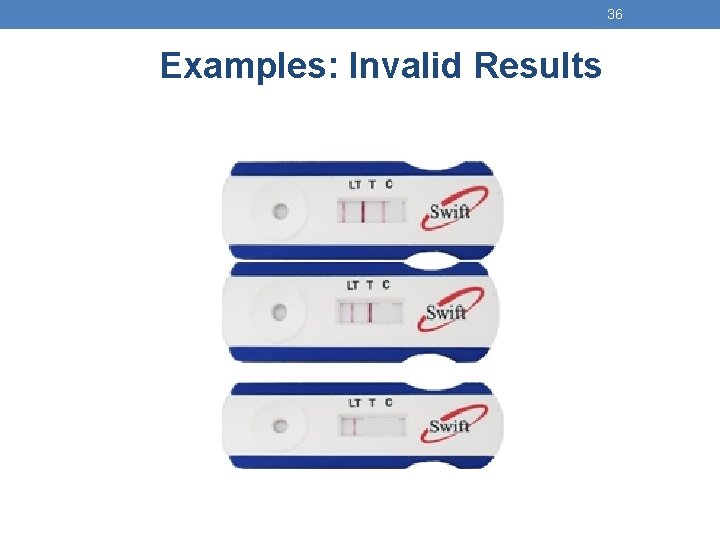
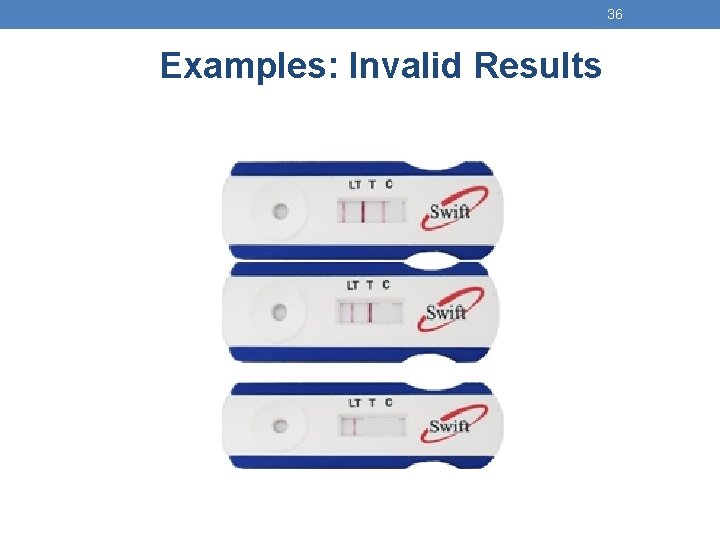
36 Examples: Invalid Results
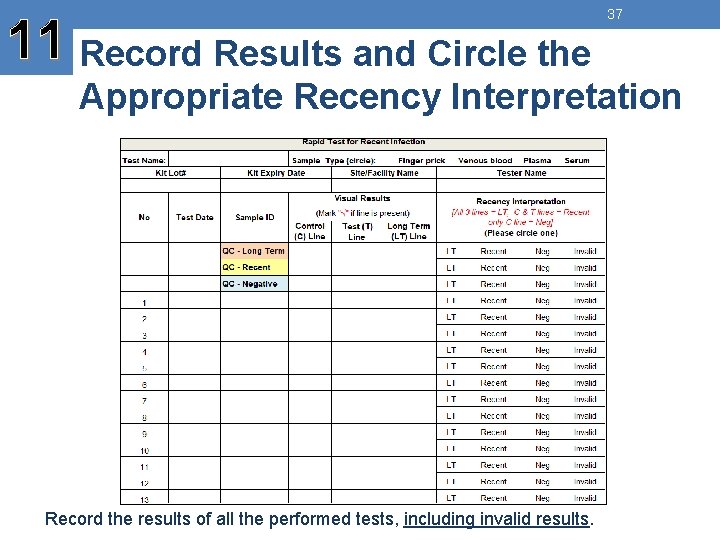
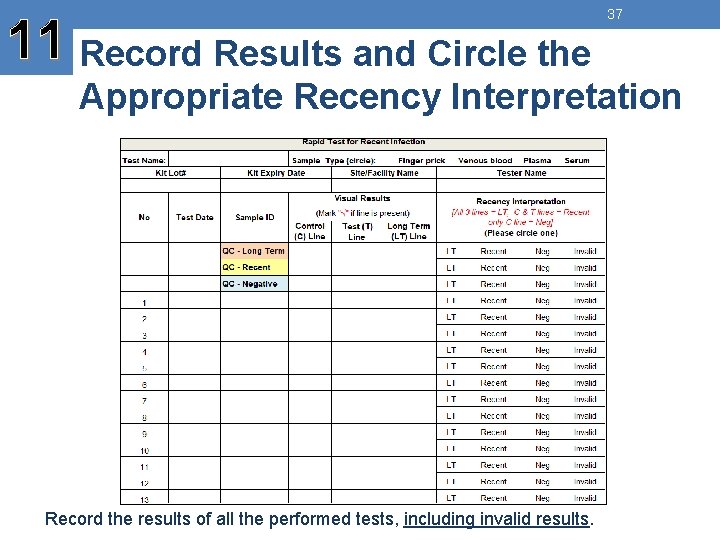
11 Record Results and Circle the 37 Appropriate Recency Interpretation Record the results of all the performed tests, including invalid results.
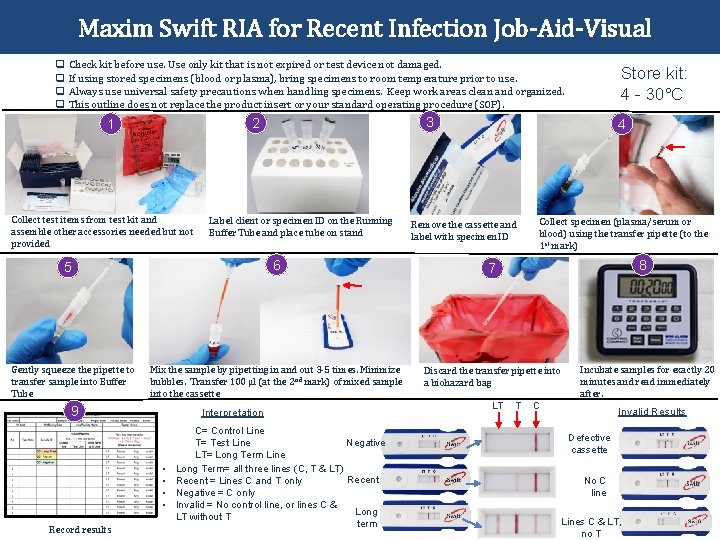
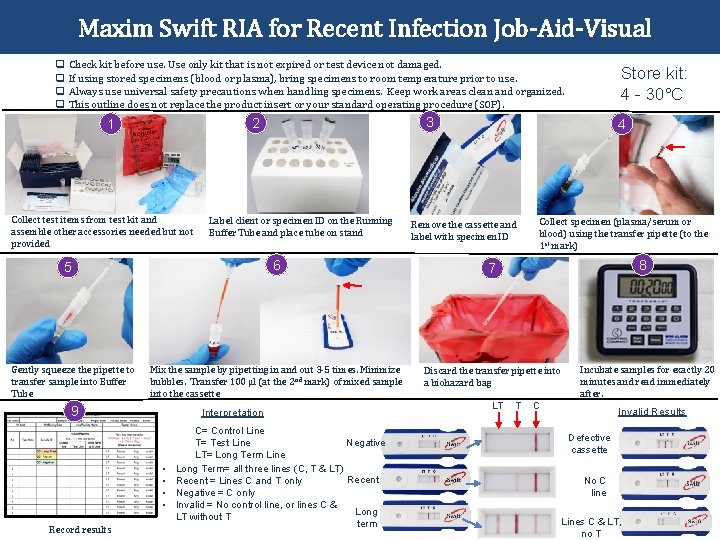
Maxim Swift RIA for Recent Infection Job-Aid-Visual q Check kit before use. Use only kit that is not expired or test device not damaged. q If using stored specimens (blood or plasma), bring specimens to room temperature prior to use. q Always use universal safety precautions when handling specimens. Keep work areas clean and organized. q This outline does not replace the product insert or your standard operating procedure (SOP). Collect test items from test kit and assemble other accessories needed but not provided Label client or specimen ID on the Running Buffer Tube and place tube on stand Remove the cassette and label with specimen ID Collect specimen (plasma/serum or blood) using the transfer pipette (to the 1 st mark) 8 7 Mix the sample by pipetting in and out 3 -5 times. Minimize bubbles. Transfer 100 µl (at the 2 nd mark) of mixed sample into the cassette Discard the transfer pipette into a biohazard bag 9 Interpretation • • Record results 4 6 5 Gently squeeze the pipette to transfer sample into Buffer Tube 3 2 1 Store kit: 4 - 30°C C= Control Line T= Test Line Negative LT= Long Term Line Long Term= all three lines (C, T & LT) Recent = Lines C and T only Negative = C only Invalid = No control line, or lines C & Long LT without T term LT T Incubate samples for exactly 20 minutes and read immediately after. C Invalid Results Defective cassette No C line Lines C & LT, no T

39 Training Panel Data Capture Form: Example Expected, acceptable Not expected, not acceptable Pass • • • Pass Fail Few specimens are known to flip-flop between recent and long term (TP-10, TP-16 and TP-17) No specimen should flip-flop between positive and negative Advise trainee to retest in case wrong specimen was used
40 Review • What methods are used to collect whole blood? • What are the techniques used to collect whole blood from a finger prick? • At what temperature, and for how long, should specimens be stored? • When would DBS specimens be collected? • What are the steps when performing the Maxim Swift recent infection assay?

Thank You!
 Unit test swift
Unit test swift Suede-like and downy surface
Suede-like and downy surface Lexia rapid test
Lexia rapid test Dilisi rapid test
Dilisi rapid test Biozek corona rapid test
Biozek corona rapid test Amnisure package insert
Amnisure package insert Hiv test results
Hiv test results Quickvue rapid strep test instructions
Quickvue rapid strep test instructions Recent trends in ic engine
Recent trends in ic engine Recent developments in ict
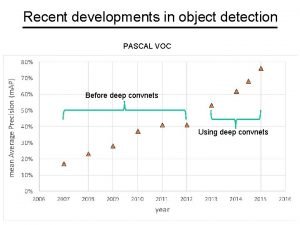
Recent developments in ict Recent developments in object detection
Recent developments in object detection Is college worth it synthesis essay
Is college worth it synthesis essay Modern trends of foreign trade in india
Modern trends of foreign trade in india What is skimming and scanning
What is skimming and scanning Trends in project portfolio management
Trends in project portfolio management Recent demographic changes in the uk
Recent demographic changes in the uk Myips.clever
Myips.clever Biotaphonomy
Biotaphonomy Jose has just played a long bruising football game
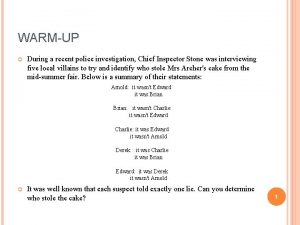
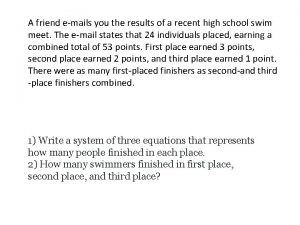
Jose has just played a long bruising football game A friend emails you the results of a recent high school
A friend emails you the results of a recent high school Recent advances in dental ceramics
Recent advances in dental ceramics Sports news in passive voice
Sports news in passive voice Http drive google com
Http drive google com Can backdated udin be generated
Can backdated udin be generated Emerging trends in mis
Emerging trends in mis Comait
Comait Formuö
Formuö Typiska novell drag
Typiska novell drag Tack för att ni lyssnade bild
Tack för att ni lyssnade bild Returpilarna
Returpilarna Shingelfrisyren
Shingelfrisyren En lathund för arbete med kontinuitetshantering
En lathund för arbete med kontinuitetshantering Kassaregister ideell förening
Kassaregister ideell förening Vilotidsbok
Vilotidsbok A gastrica
A gastrica Vad är densitet
Vad är densitet Datorkunskap för nybörjare
Datorkunskap för nybörjare Tack för att ni lyssnade bild
Tack för att ni lyssnade bild Mall för debattartikel
Mall för debattartikel Autokratiskt ledarskap
Autokratiskt ledarskap Nyckelkompetenser för livslångt lärande
Nyckelkompetenser för livslångt lärande Påbyggnader för flakfordon
Påbyggnader för flakfordon