HIV in Education in Emergency Presentation to Education




- Slides: 19
HIV in Education in Emergency Presentation to Education Cluster 20 October 2014
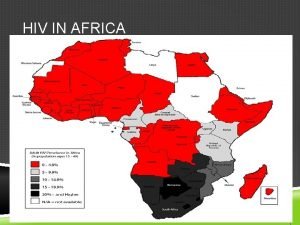
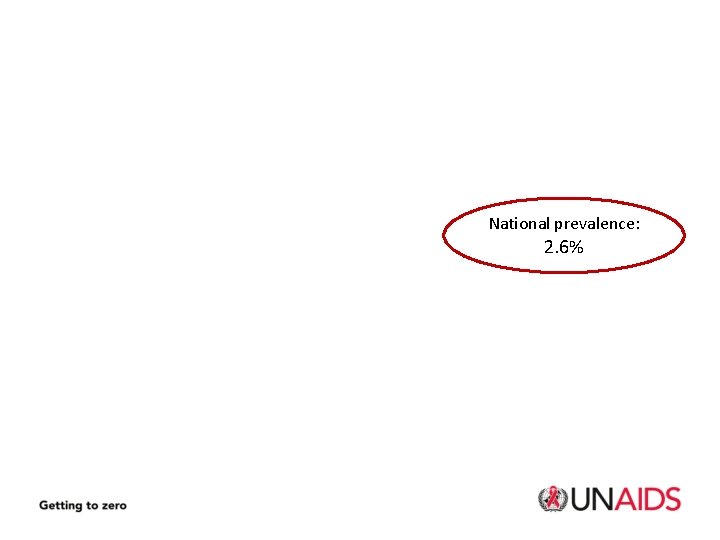
National prevalence: 2. 6%
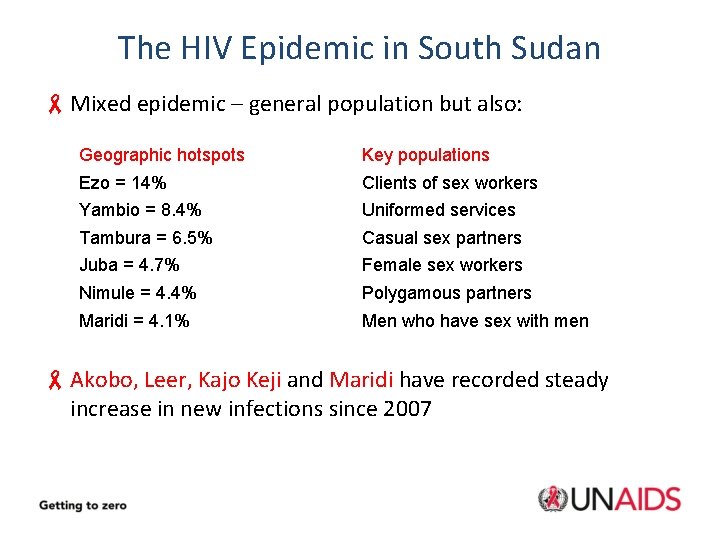
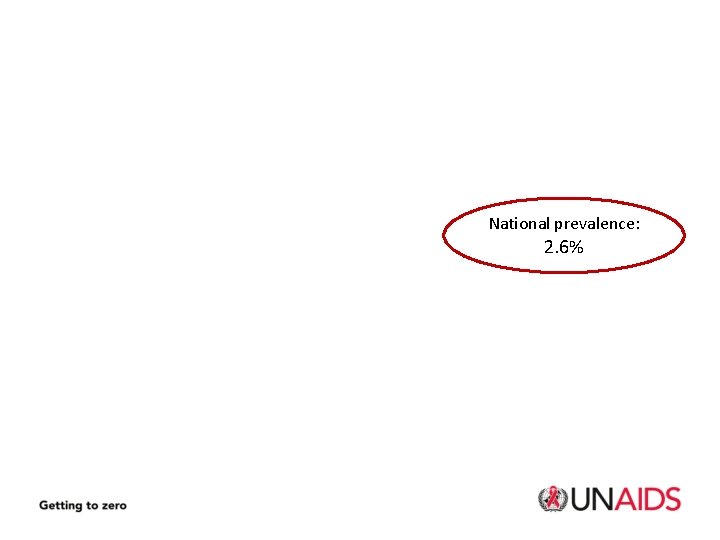
The HIV Epidemic in South Sudan - Mixed epidemic – general population but also: Geographic hotspots Key populations Ezo = 14% Clients of sex workers Yambio = 8. 4% Uniformed services Tambura = 6. 5% Casual sex partners Juba = 4. 7% Female sex workers Nimule = 4. 4% Polygamous partners Maridi = 4. 1% Men who have sex with men - Akobo, Leer, Kajo Keji and Maridi have recorded steady increase in new infections since 2007
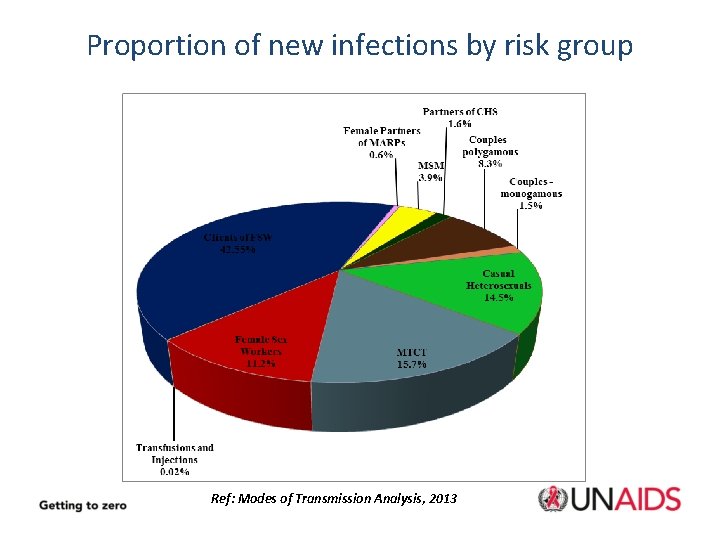
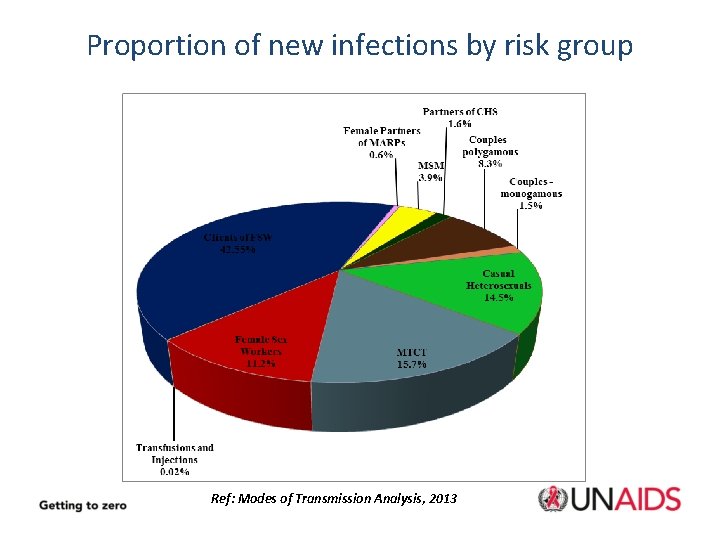
Proportion of new infections by risk group Ref: Modes of Transmission Analysis, 2013
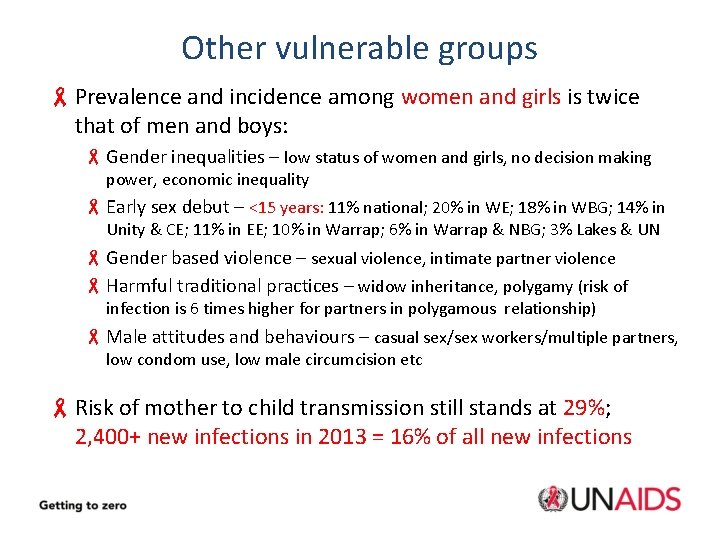
Other vulnerable groups - Prevalence and incidence among women and girls is twice that of men and boys: - Gender inequalities – low status of women and girls, no decision making power, economic inequality - Early sex debut – <15 years: 11% national; 20% in WE; 18% in WBG; 14% in Unity & CE; 11% in EE; 10% in Warrap; 6% in Warrap & NBG; 3% Lakes & UN - Gender based violence – sexual violence, intimate partner violence - Harmful traditional practices – widow inheritance, polygamy (risk of infection is 6 times higher for partners in polygamous relationship) - Male attitudes and behaviours – casual sex/sex workers/multiple partners, low condom use, low male circumcision etc - Risk of mother to child transmission still stands at 29%; 2, 400+ new infections in 2013 = 16% of all new infections

Young People - South Sudan is a young population: 72% under 30 years, 51% under 18 years - 20, 000 young people <15 years living with HIV - Most young people do not have access to sexual and reproductive health information and services - Risk factors include early sex, inter-generational sex, gender based violence, no access to condoms etc - 2010 KAP study in Greater Equatoria: -21% early sex debut, mean age of 10. 75 -Very low comprehensive knowledge of HIV (11. 3%) -Low knowledge of correct condom use (31%)
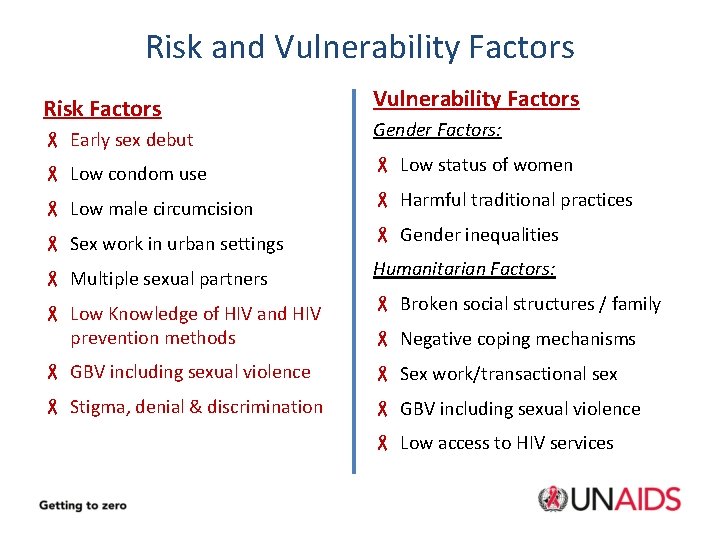
Risk and Vulnerability Factors Risk Factors Vulnerability Factors - Early sex debut Gender Factors: - Low condom use - Low status of women - Low male circumcision - Harmful traditional practices - Sex work in urban settings - Gender inequalities - Multiple sexual partners Humanitarian Factors: - Low Knowledge of HIV and HIV prevention methods - Broken social structures / family - GBV including sexual violence - Sex work/transactional sex - Stigma, denial & discrimination - GBV including sexual violence - Negative coping mechanisms - Low access to HIV services
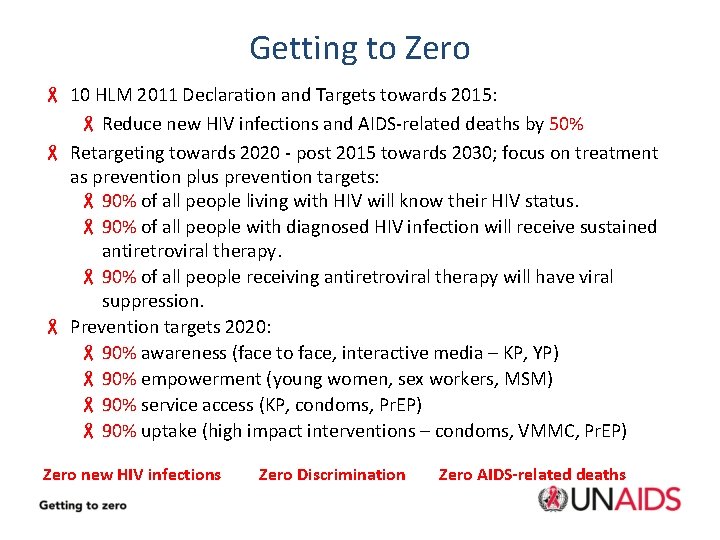
Getting to Zero - 10 HLM 2011 Declaration and Targets towards 2015: - Reduce new HIV infections and AIDS-related deaths by 50% - Retargeting towards 2020 - post 2015 towards 2030; focus on treatment as prevention plus prevention targets: - 90% of all people living with HIV will know their HIV status. - 90% of all people with diagnosed HIV infection will receive sustained antiretroviral therapy. - 90% of all people receiving antiretroviral therapy will have viral suppression. - Prevention targets 2020: - 90% awareness (face to face, interactive media – KP, YP) - 90% empowerment (young women, sex workers, MSM) - 90% service access (KP, condoms, Pr. EP) - 90% uptake (high impact interventions – condoms, VMMC, Pr. EP) Zero new HIV infections Zero Discrimination Zero AIDS-related deaths

HIV Response in South Sudan - Ratio of newly infected to initiated on treatment 4: 1 (Africa avg ≈2: 1); 20: 1 ratio of new infections to ever enrolled on treatment - Less than 5% of PLHIV are on treatment (9% at CD 4 count 350) - Only 20% of HIV positive pregnant women are able to access prevention of mother to child transmission services - Mo. H estimates 50, 000 people test for HIV every year, we need to reach 700, 000 a year to scale up treatment - About 10 million condoms are reported to be distributed annually, about 8% of what is required (110 million) to have an impact on new infections
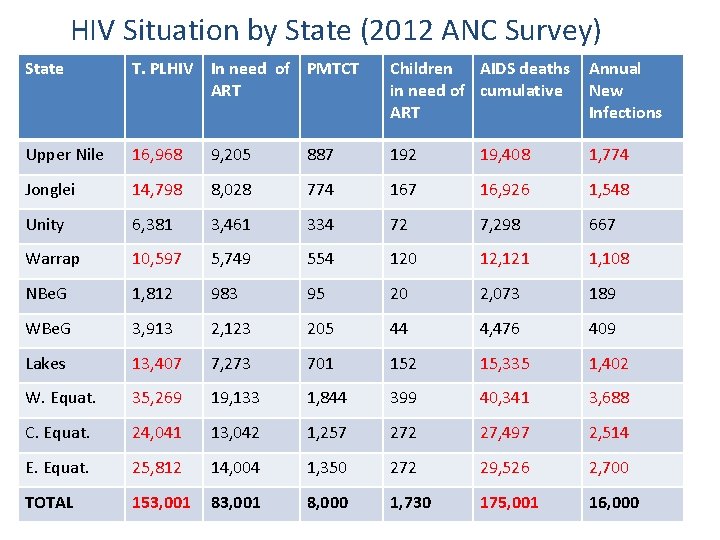
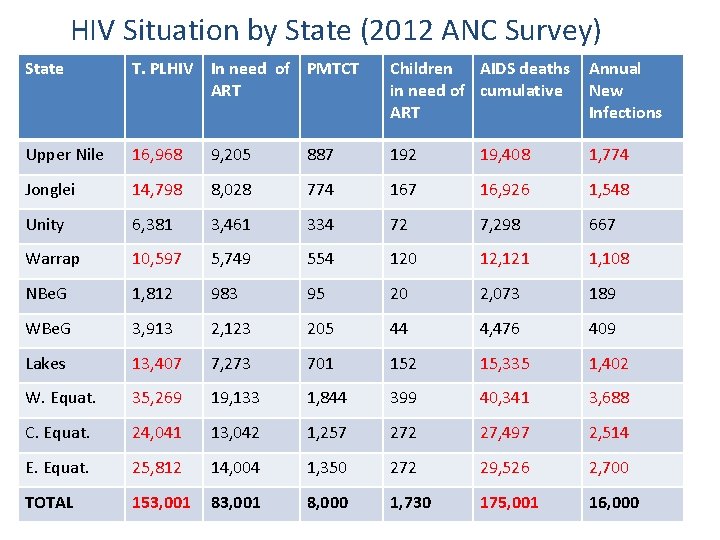
HIV Situation by State (2012 ANC Survey) State T. PLHIV In need of PMTCT ART Children AIDS deaths in need of cumulative ART Annual New Infections Upper Nile 16, 968 9, 205 887 192 19, 408 1, 774 Jonglei 14, 798 8, 028 774 167 16, 926 1, 548 Unity 6, 381 3, 461 334 72 7, 298 667 Warrap 10, 597 5, 749 554 120 12, 121 1, 108 NBe. G 1, 812 983 95 20 2, 073 189 WBe. G 3, 913 2, 123 205 44 4, 476 409 Lakes 13, 407 7, 273 701 152 15, 335 1, 402 W. Equat. 35, 269 19, 133 1, 844 399 40, 341 3, 688 C. Equat. 24, 041 13, 042 1, 257 272 27, 497 2, 514 E. Equat. 25, 812 14, 004 1, 350 272 29, 526 2, 700 TOTAL 153, 001 8, 000 1, 730 175, 001 16, 000
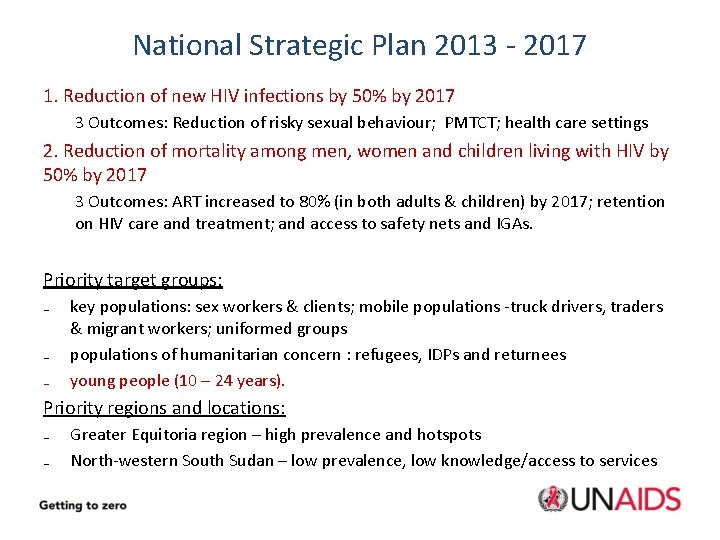
National Strategic Plan 2013 - 2017 1. Reduction of new HIV infections by 50% by 2017 3 Outcomes: Reduction of risky sexual behaviour; PMTCT; health care settings 2. Reduction of mortality among men, women and children living with HIV by 50% by 2017 3 Outcomes: ART increased to 80% (in both adults & children) by 2017; retention on HIV care and treatment; and access to safety nets and IGAs. Priority target groups: ₋ ₋ ₋ key populations: sex workers & clients; mobile populations -truck drivers, traders & migrant workers; uniformed groups populations of humanitarian concern : refugees, IDPs and returnees young people (10 – 24 years). Priority regions and locations: ₋ ₋ Greater Equitoria region – high prevalence and hotspots North-western South Sudan – low prevalence, low knowledge/access to services
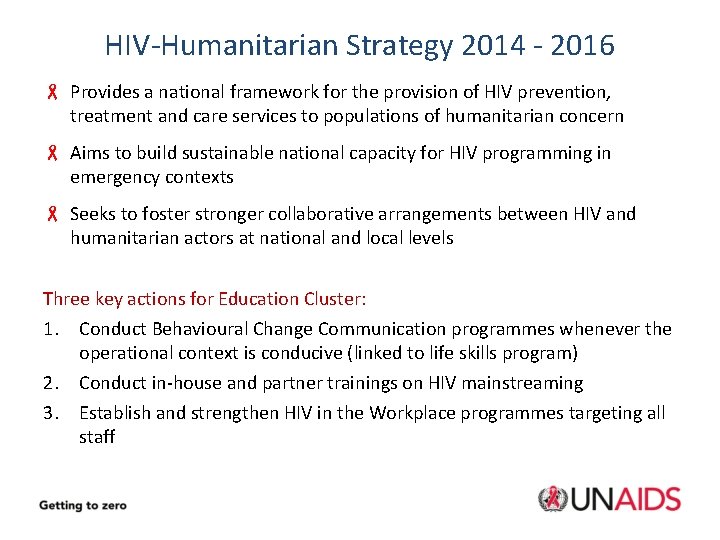
HIV-Humanitarian Strategy 2014 - 2016 - Provides a national framework for the provision of HIV prevention, treatment and care services to populations of humanitarian concern - Aims to build sustainable national capacity for HIV programming in emergency contexts - Seeks to foster stronger collaborative arrangements between HIV and humanitarian actors at national and local levels Three key actions for Education Cluster: 1. Conduct Behavioural Change Communication programmes whenever the operational context is conducive (linked to life skills program) 2. Conduct in-house and partner trainings on HIV mainstreaming 3. Establish and strengthen HIV in the Workplace programmes targeting all staff

IASC Guidelines: HIV in Education - Children and young people with access to education are also more likely to delay onset of sexual activity and avoid alcohol and substance abuse - Education can provide life-saving knowledge, skills and services to children and young people vulnerable to HIV infection - Education can provide additional protection for those already infected and affected - Education can help raise awareness in the larger community IASC Guidelines: http: //www. humanitarianinfo. org - IASC Products: HIV/AIDS Also INEE Minimum Standards Toolkit: HIV/AIDS www. ineesite. org/uploads/documents/store/doc_1_INEE_toolkit_-_HIV-AIDS. pdf
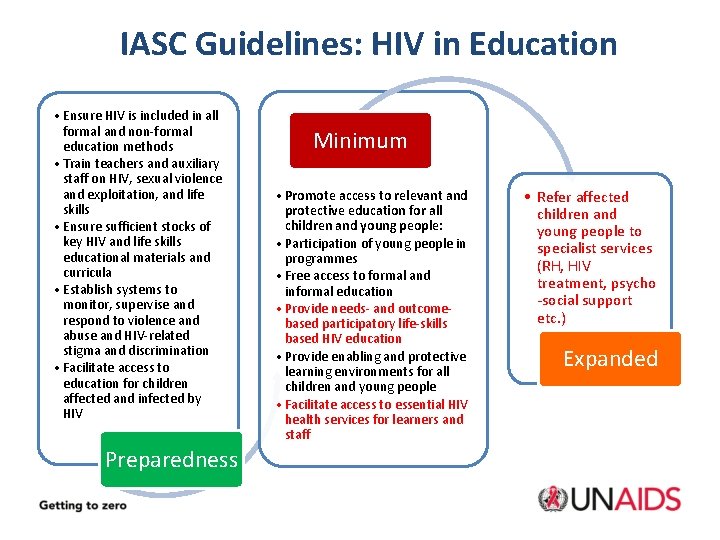
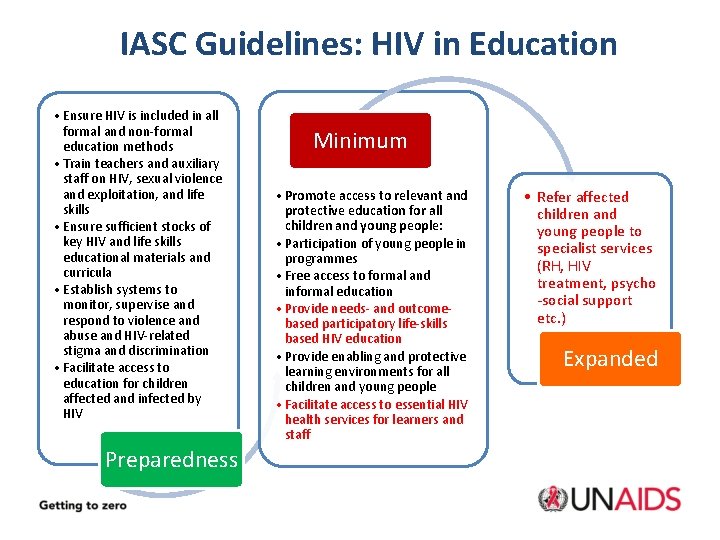
IASC Guidelines: HIV in Education • Ensure HIV is included in all formal and non-formal education methods • Train teachers and auxiliary staff on HIV, sexual violence and exploitation, and life skills • Ensure sufficient stocks of key HIV and life skills educational materials and curricula • Establish systems to monitor, supervise and respond to violence and abuse and HIV-related stigma and discrimination • Facilitate access to education for children affected and infected by HIV Preparedness Minimum • Promote access to relevant and protective education for all children and young people: • Participation of young people in programmes • Free access to formal and informal education • Provide needs- and outcomebased participatory life-skills based HIV education • Provide enabling and protective learning environments for all children and young people • Facilitate access to essential HIV health services for learners and staff • Refer affected children and young people to specialist services (RH, HIV treatment, psycho -social support etc. ) Expanded

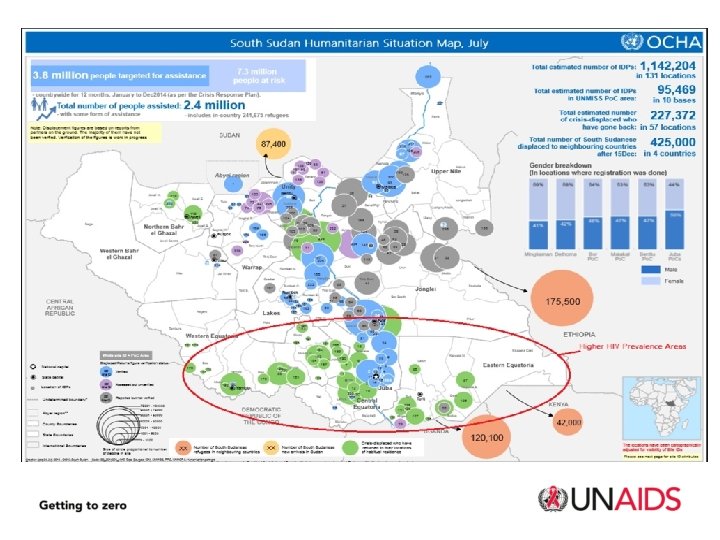
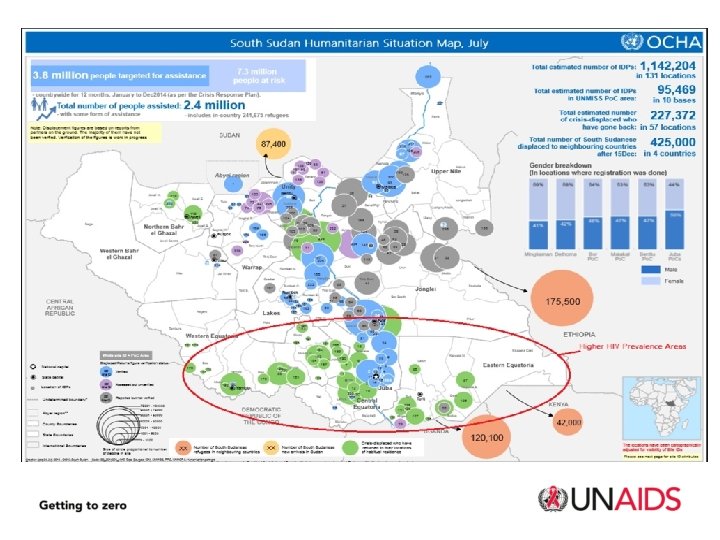
HIV situation stemming from crisis ≈ 40, 000 PLHIV affected with little to no access to treatment, care and support networks ≈ 25, 000 PLHIV displaced and likely in urgent need of HIV treatment, care and support services ≈ 1, 000 PLHIV have interrupted treatment Vulnerability factors: - Family separation – high risk sexual behaviors, especially among young men - GBV - rape, sexual exploitation, intimate partner violence - Negative coping mechanisms – transactional sex, sex work - Little knowledge of HIV and HIV prevention - Low access to HIV services and prevention commodities (condoms) - Displacement to higher HIV prevalence locations
HIV in humanitarian response -Tracing and referring clients on ART, CTX and TB treatment -Provision of HIV services in IDP sites: -Awareness/behavioral change communication – HIV, GBV -Condom promotion -HIV counseling and testing -Prevention of mother to child transmission -Mobile and referral for treatment -SRH and MNCH linkages, including PSS and PEP for GBV survivors, and STI management -Resource mobilisation – GFATM, Humanitarian?
Opportunity for integration: IEC materials for BCC Five sets developed and approved, in English and Arabic: 1. 2. 3. 4. 5. HIV Basic Information HIV Counseling and Testing Prevention of mother to child transmission Stigma and Discrimination Snakes and Ladders Game for young people For your own sets, contact Mango Tree: Mathias Mwene – Country Manager, MT South Sudan mmwene@mangotreeuganda. org Tel South Sudan: +211927221638 Uganda: +256 703 071 172 / +256 312 263 Cost: ≈ USD 250 for all 5 sets HIV IEC materials developed for UN staff also available for work place programme
www. aidsandemergencies. org Mumtaz Mia – Program Adviser Email: miam@unaids. org Mobile: 0912 112 299 Omar Dia – Humanitarian Adviser Email: diao@unaids. org Mobile: 0912 154 719 www. unaids. org
 Emergency medicine case presentation
Emergency medicine case presentation Answer site
Answer site Quang trung
Quang trung Hiv reverse transcription
Hiv reverse transcription Test wiedzy o hiv i aids
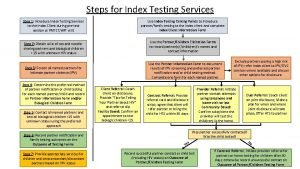
Test wiedzy o hiv i aids Approche index testing
Approche index testing Prognas kb
Prognas kb Phdp in hiv
Phdp in hiv Kuchecheudzwa
Kuchecheudzwa Hcv window period
Hcv window period Why do the bodys antibodies fail to protect people from hiv
Why do the bodys antibodies fail to protect people from hiv Iris syndrome
Iris syndrome Where did hiv come from
Where did hiv come from Hiv risk factors
Hiv risk factors Asante hiv-1 rapid recency assay
Asante hiv-1 rapid recency assay Fiebig hiv
Fiebig hiv Hiv case-based surveillance in ethiopia
Hiv case-based surveillance in ethiopia Triệu chứng nhiễm hiv
Triệu chứng nhiễm hiv A bacterial std that usually affects mucous membranes
A bacterial std that usually affects mucous membranes Chapter 24 sexually transmitted diseases and hiv/aids
Chapter 24 sexually transmitted diseases and hiv/aids