HIV Human Immunodeficiency Virus AIDS Acquired Immune Deficiency







- Slides: 30
HIV (Human Immunodeficiency Virus) & AIDS Acquired Immune Deficiency Syndrome Immunology Unit Department of Pathology King Saud University
Objectives To know the modes of transmission of HIV To understand HIV interactions with CD 4 positive helper lymphocytes To understand the mechanisms involved in immunodeficiency associated with HIV To know the course of immunological events from the time of infection with HIV until the development of AIDS

Transmission Modes of infection Sexual transmission at genital or colonic mucosa Blood transfusion Mother to infant Accidental occupational exposure
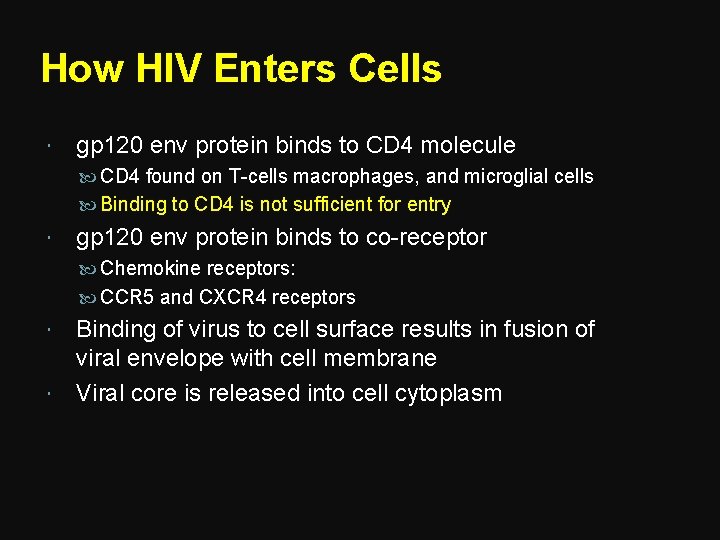
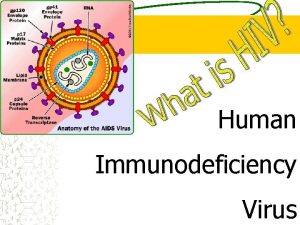
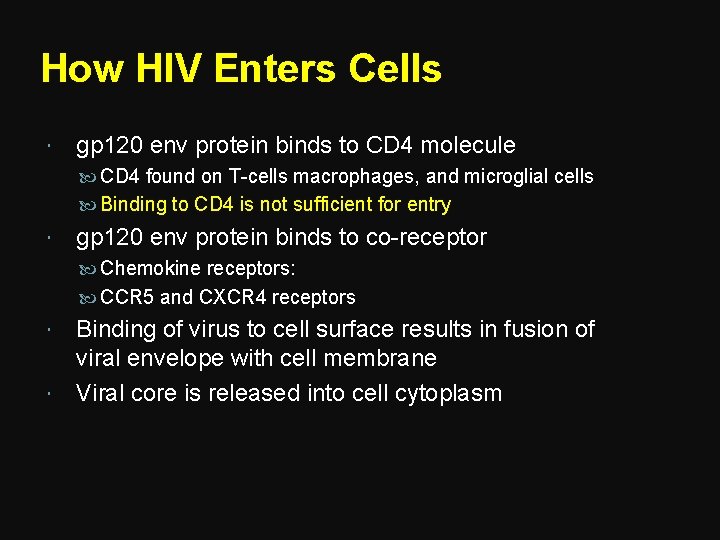
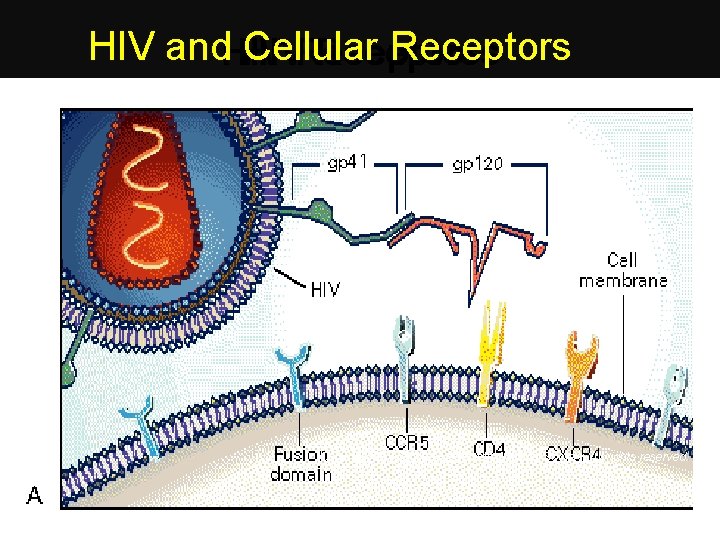
How HIV Enters Cells gp 120 env protein binds to CD 4 molecule CD 4 found on T-cells macrophages, and microglial cells Binding to CD 4 is not sufficient for entry gp 120 env protein binds to co-receptor Chemokine receptors: CCR 5 and CXCR 4 receptors Binding of virus to cell surface results in fusion of viral envelope with cell membrane Viral core is released into cell cytoplasm
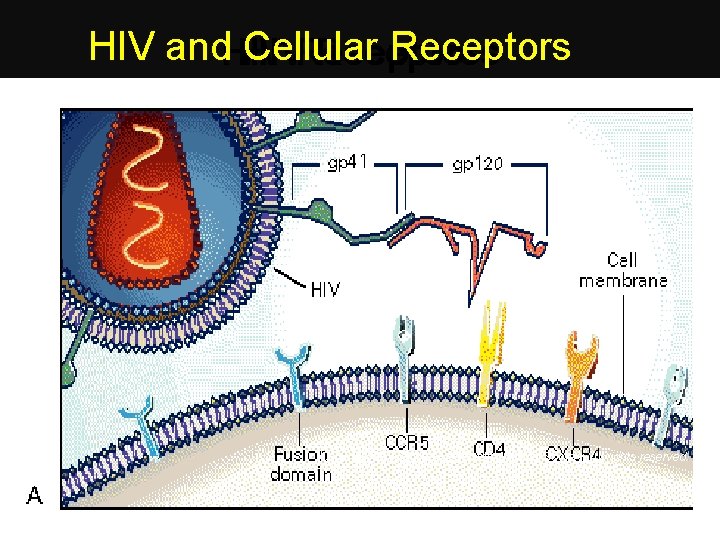
HIV and. HIV Cellular Receptors HIV Receptors Copyright © 1996 Massachusetts Medical Society. All rights reserved.
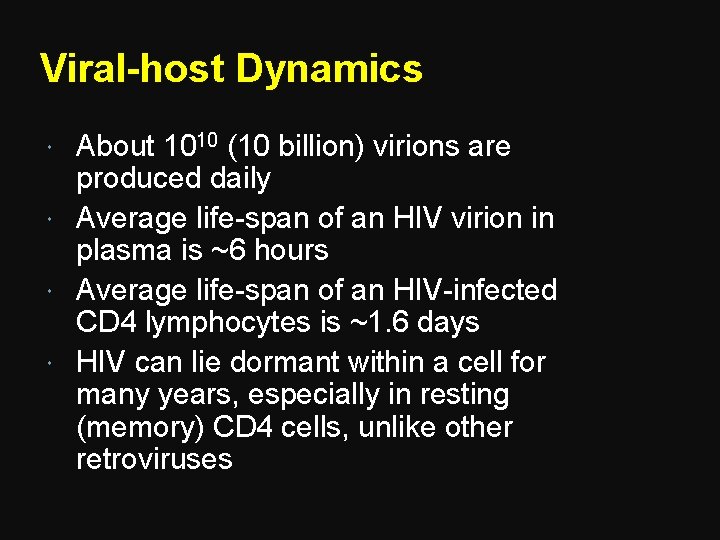
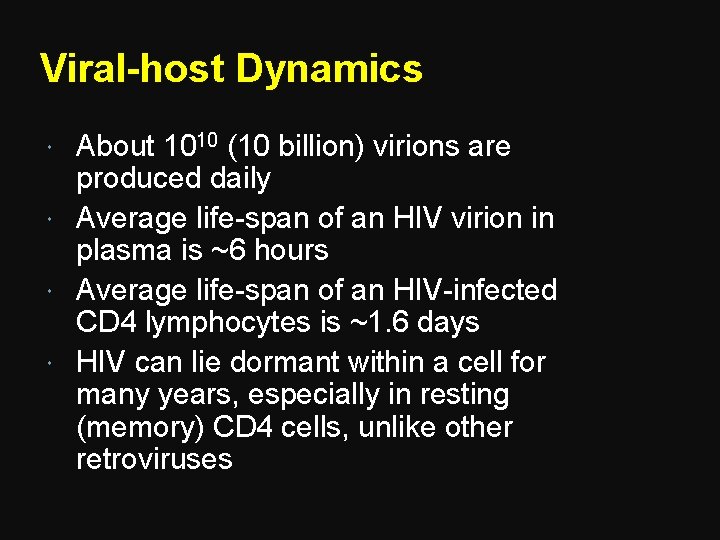
Viral-host Dynamics About 1010 (10 billion) virions are produced daily Average life-span of an HIV virion in plasma is ~6 hours Average life-span of an HIV-infected CD 4 lymphocytes is ~1. 6 days HIV can lie dormant within a cell for many years, especially in resting (memory) CD 4 cells, unlike other retroviruses

1. HIV (retrovirus) enters cell 2. Reverse Transcriptase makes DNA copy of RNA 3. Viral DNA forms provirus with host DNA Viral DNA makes m. RNA makes HIV proteins become HIV capsid m. RNA is collected inside of HIV capsid forming new HIV New HIV leaves cell and wraps itself in host membrane (envelope)
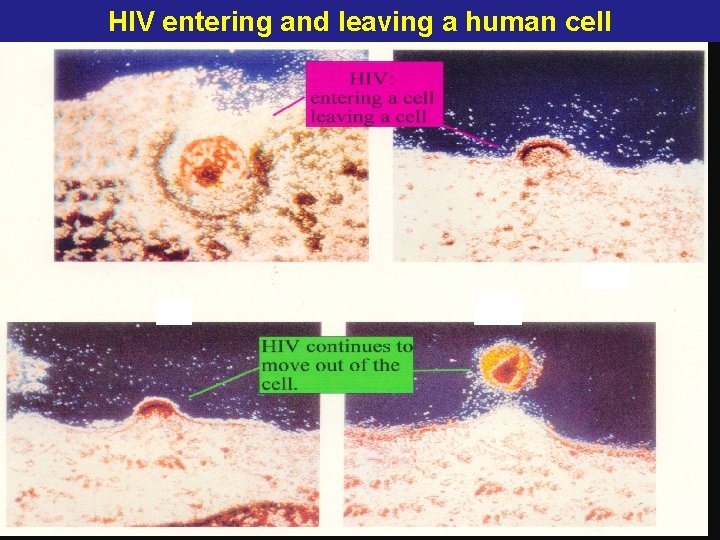
HIV entering and leaving a human cell
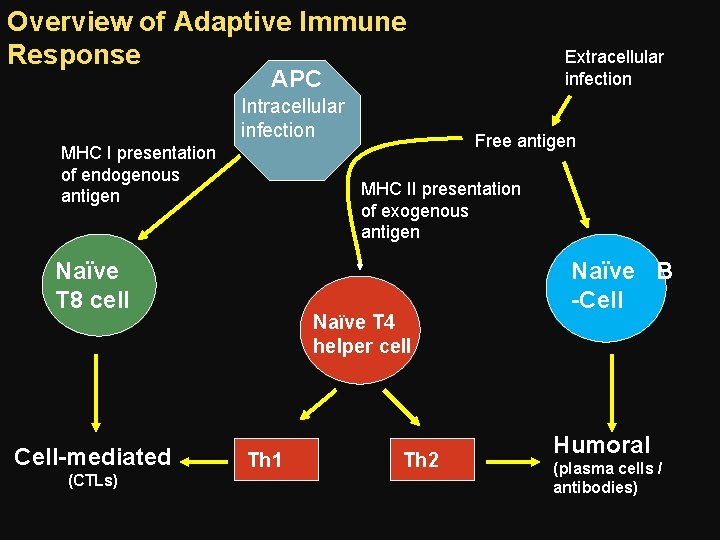
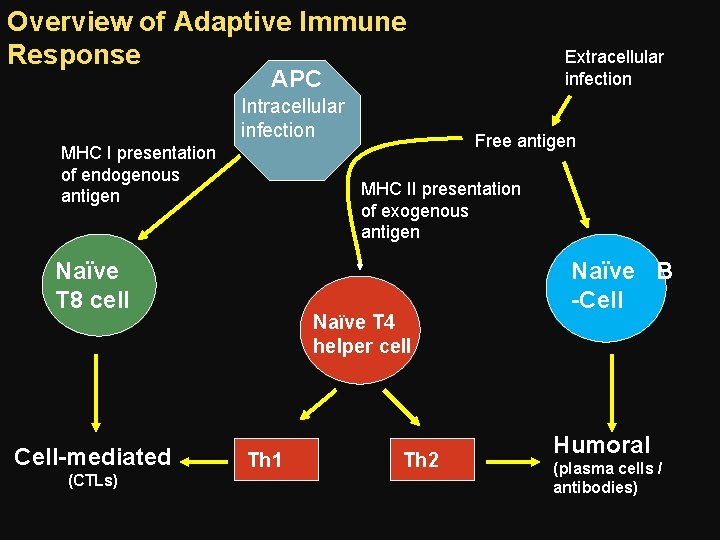
Overview of Adaptive Immune Response Extracellular infection APC Intracellular infection MHC I presentation of endogenous antigen MHC II presentation of exogenous antigen Naïve T 8 cell Cell-mediated (CTLs) Free antigen Naïve T 4 helper cell Th 1 Th 2 Naïve B -Cell Humoral (plasma cells / antibodies)
General Principles of Viral-host Interactions Host: mounts HIV-specific immune responses Cellular (cell-mediated) - most important Humoral (antibody-mediated) Virus: subverts the immune system Infects CD 4 cells that control normal immune responses Integrates into host DNA High rate of mutation Hides in tissue not readily accessible to immune system

Cellular Immune Responses to HIV CD 8 Cytotoxic T lymphocyte (CTL) Derived from naïve T 8 cells, which recognize viral antigens in context of MHC class I presentation Directly destroy infected cell Activity augmented by Th 1 response
Cellular Immune Responses to HIV CD 4 Helper T Lymphocyte (Th) Plays an important role in cell-mediated response Recognizes viral antigens by an antigen presenting cell (APC) ○ Utilizes major histocompatibility complex (MHC) class II Differentiated according to the type of “help” ○ Th 1 - activate Tc (CD 8) lymphocytes, promoting cell-mediated immunity ○ Th 2 - activate B lymphocytes, promoting antibody mediated immunity
Humoral Immune Response to HIV Neutralization Antibodies bind to surface of virus to prevent attachment to target cell Antibody-dependent cell-mediated cytotoxicity (ADCC) Fc portion of antibody binds to NK cell Stimulates NK cell to destroy infected cell

Cells Infected by HIV Numerous organ systems are infected by HIV: Brain: macrophages and glial cells Lymph nodes and thymus: lymphocytes and dendritic cells Blood, semen, vaginal fluids: macrophages Bone marrow: lymphocytes Skin: langerhans cells Colon, duodenum, rectum: chromaffin cells Lung: alveolar macrophages
General Principles of Immune Dysfunction in HIV All elements of immune system are affected Advanced stages of HIV are associated with substantial disruption of lymphoid tissue Impaired ability to mount immune response to new antigen Impaired ability to maintain memory responses Susceptibility to opportunistic infections

Mechanisms of CD 4 Depletion and Dysfunction Direct Elimination of HIV-infected cells by virus- specific immune responses Loss of plasma membrane integrity because of viral budding Indirect Syncytium formation Apoptosis Autoimmunity
Syncytium Formation Observed in HIV infection, most commonly in the brain Uninfected cells may then bind to infected cells due to viral gp 120 This results in fusion of the cell membranes and subsequent syncytium formation. These syncytia are highly unstable and die quickly
Role of Cellular Activation in Pathogenesis of HIV induces immune activation Which may seem paradoxical because HIV ultimately results in severe immunosuppression Activated T-cells support HIV replication Intercurrent infections are associated with transient increases in viremia Accounts for why TB worsens underlying HIV disease
Role of Cytokine Dysregulation in Pathogenesis of HIV is associated with increased expression of pro-inflammatory cytokines TNF-alpha, IL-1, IL-6, IL-10, IFN-gamma HIV results in disruption and loss of immunoregulatory cytokines IL-2, IL-12 Necessary for modulating effective cell- mediated immune responses (CTLs and NK cells)
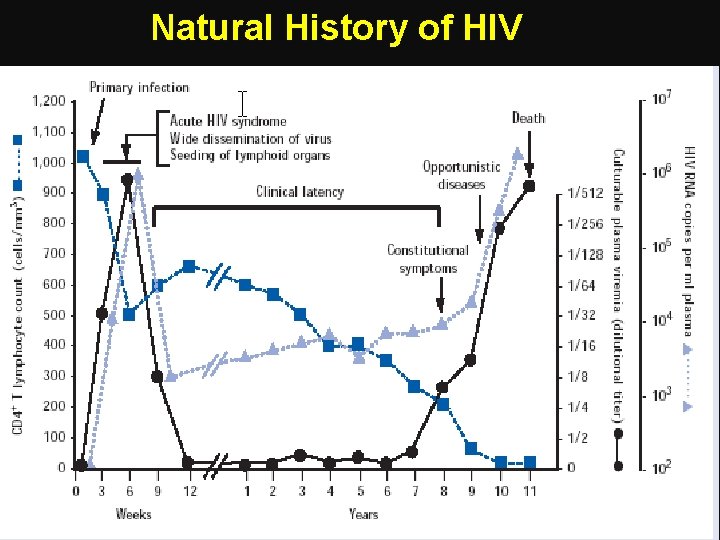
Primary Infection 70 -80% symptomatic, 3 -12 weeks after exposure Fever, rash, cervical lymphadenopathy, aseptic meningitis, encephalitis, myelitis, polyneuritis Surge in viral RNA copies to >1 million Fall in CD 4 count to 300 -400 Recovery in 7 -14 days

Seroconversion Median 8 weeks after infection Level of viral load post sero-conversion correlates with risk of progression of disease Asymptomatic Phase Remain well with no evidence of HIV disease except for generalized lymphadenopathy Fall of CD 4 count by about 50 -150 cells per year
CD 4 T-cell Count and Progression to AIDS Gradual reduction in number of circulating CD 4 cells is inversely correlated with the viral load Any depletion in numbers of CD 4 cells renders the body susceptible to opportunistic infections

Window Period: Untreated Clinical Course Acute HIV syndrome Primary HIV infection Asymptomatic antibody viremia ----------------------PCR P 24 ELISA a 0 b Time from a to b is the window period 2 3 4 years Weeks since infection Source: S Conway and J. G Bartlett, 2003
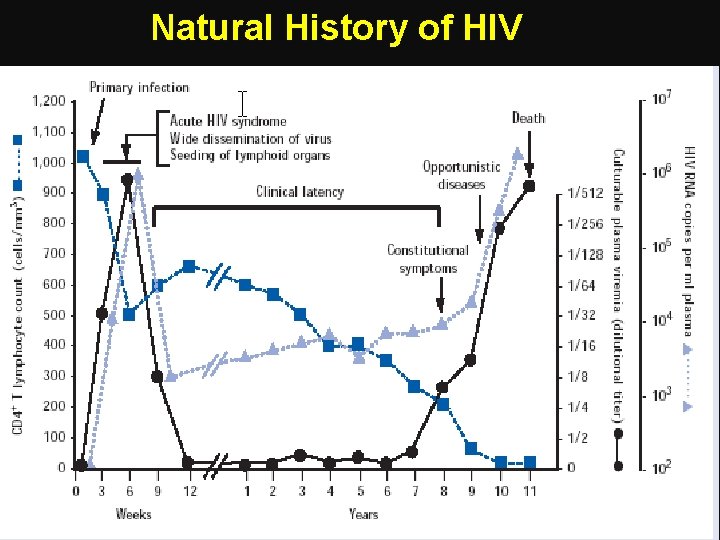
Natural History of HIV Fauci As, 1996
Laboratory Markers of HIV Infection Viral load Marker of HIV replication rate CD 4 count Marker of immunologic damage
Diagnosis Antibody test, ELISA Western blot HIV RNA viral load
Management Treatment recommended when symptomatic or CD 4 count below 200 Earlier if high viral load, rapidly falling CD 4 count, hepatitis C co-infection Antiviral therapy Reverse transcriptase inhibitors Protease inhibitors Fusion inhibitors
Take Home Message Infection with HIV usually occurs by sexual transmission, blood transfusion, mother to infant or accidental exposure HIV targets the immune system and primarily infects CD 4 positive lymphocytes Immunodeficiency associated with HIV infections is mainly due to reduction in CD 4 positive helper lymphocyte numbers Increased viral load, significant reduction in CD 4 lymphocytes and opportunistic infections are the hallmarks of progression to AIDS
Thank you
 A subsequent
A subsequent What are deficiency
What are deficiency Severe combined immunodeficiency
Severe combined immunodeficiency Test wiedzy o aids z odpowiedziami
Test wiedzy o aids z odpowiedziami Chapter 25 sexually transmitted infections and hiv/aids
Chapter 25 sexually transmitted infections and hiv/aids Chapter 24 sexually transmitted diseases and hiv/aids
Chapter 24 sexually transmitted diseases and hiv/aids Causative organism of hiv/aids
Causative organism of hiv/aids Recognize developmental disorders of the dentition
Recognize developmental disorders of the dentition Kasus hiv aids
Kasus hiv aids Stadium hiv menurut who
Stadium hiv menurut who Hiv virus
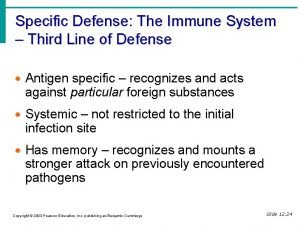
Hiv virus What is the third line of defense in the immune system
What is the third line of defense in the immune system Complete the flow chart
Complete the flow chart Any substance capable of provoking an immune response
Any substance capable of provoking an immune response Hydrops fetalis
Hydrops fetalis Primary vs secondary immune response
Primary vs secondary immune response Second line of defense immune system
Second line of defense immune system Chapter 35 immune system and disease
Chapter 35 immune system and disease Chapter 55 care of the patient with an immune disorder
Chapter 55 care of the patient with an immune disorder Primary vs secondary immune response
Primary vs secondary immune response Ap bio immune system
Ap bio immune system Chapter 24 the immune and lymphatic systems and cancer
Chapter 24 the immune and lymphatic systems and cancer Lesson 12 blood and immune system
Lesson 12 blood and immune system Lesson 12 blood and immune system
Lesson 12 blood and immune system Immune checkpoint inhibitors mechanism of action
Immune checkpoint inhibitors mechanism of action Immune reconstitution inflammatory syndrome
Immune reconstitution inflammatory syndrome Dr adria rusli
Dr adria rusli Immune system lymph nodes
Immune system lymph nodes Immune system def
Immune system def Immune complex glomerulonephritis
Immune complex glomerulonephritis Overreactions of the immune system
Overreactions of the immune system