HIV Cure Research Updates Dr Matthew Marsden Adj



- Slides: 55
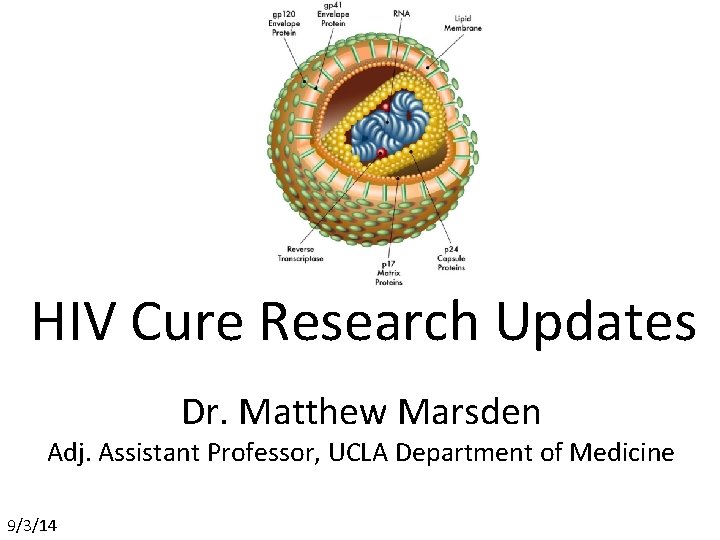
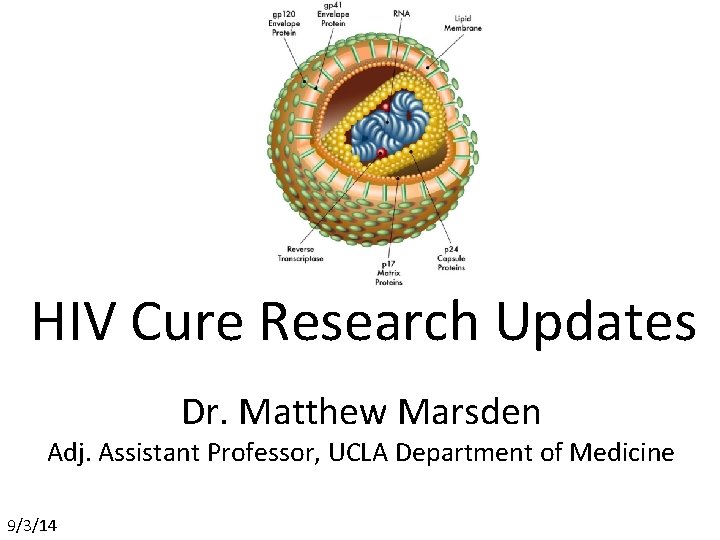
HIV Cure Research Updates Dr. Matthew Marsden Adj. Assistant Professor, UCLA Department of Medicine 9/3/14
http: //www. cnn. com/2013/03/18/health/hiv-functional-cure http: //www. nytimes. com/2011/11/29/health/new-hope-of-a-cure-forhiv. html? pagewanted=all http: //abcnews. go. com/Health/french-hiv-study-means-hivbabys-cure/story? id=18741318#. UZFht 7 VOQr. U
• Why is HIV difficult to cure? • Documented cases of apparent cures • New gene therapy/transplant approaches • Additional therapeutic approaches
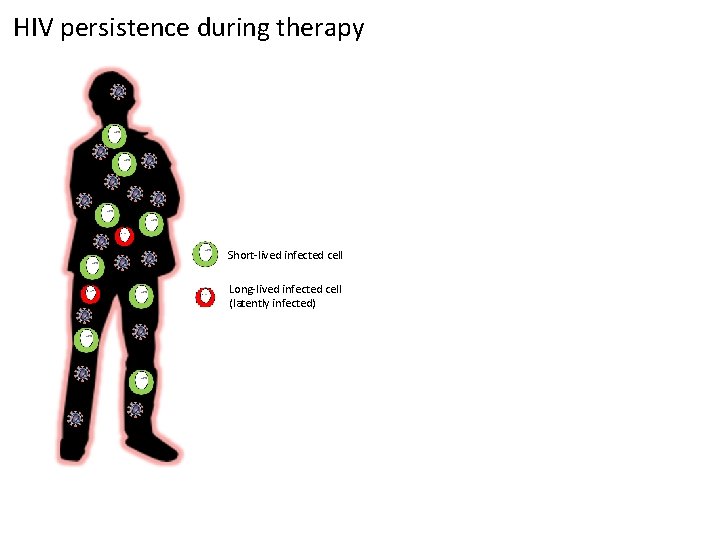
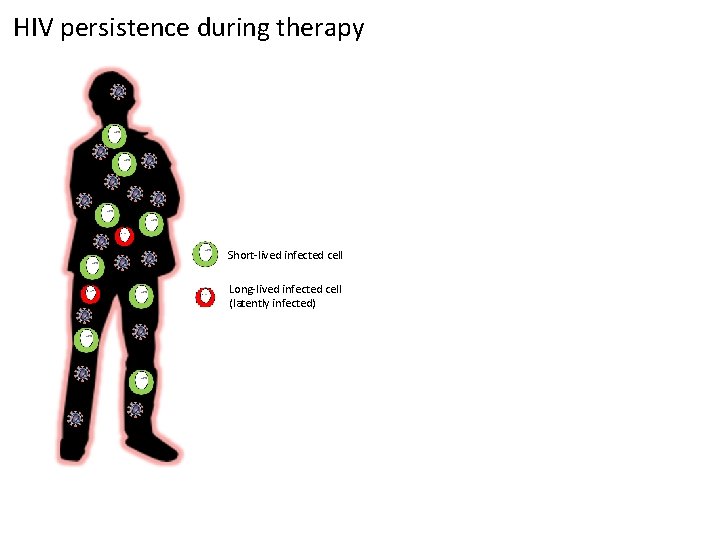
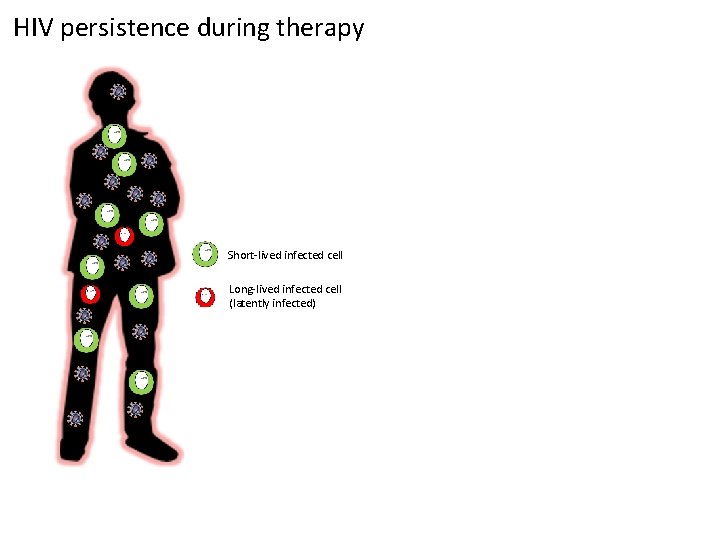
HIV persistence during therapy Short-lived infected cell Long-lived infected cell (latently infected)
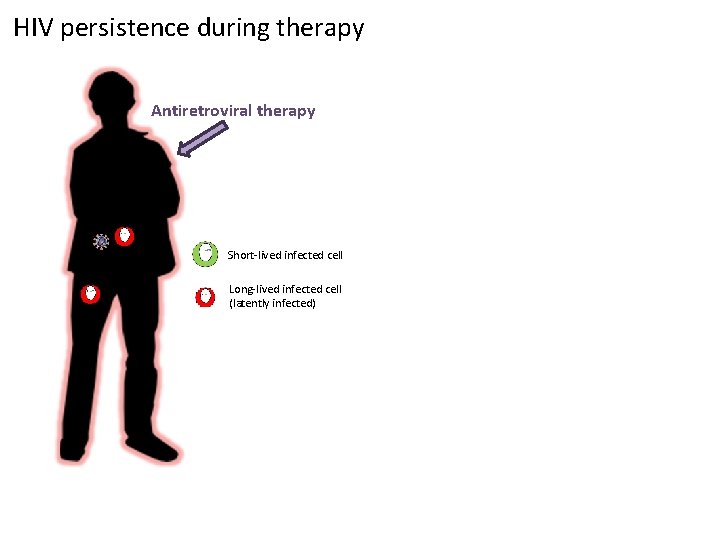
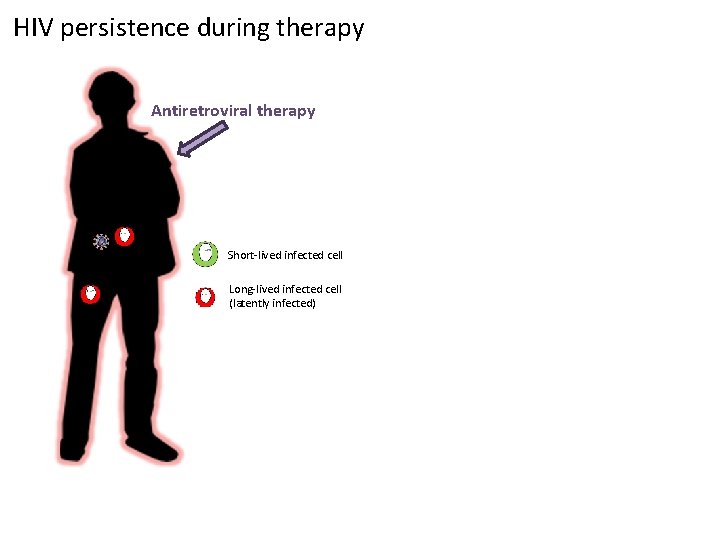
HIV persistence during therapy Antiretroviral therapy Short-lived infected cell Long-lived infected cell (latently infected)
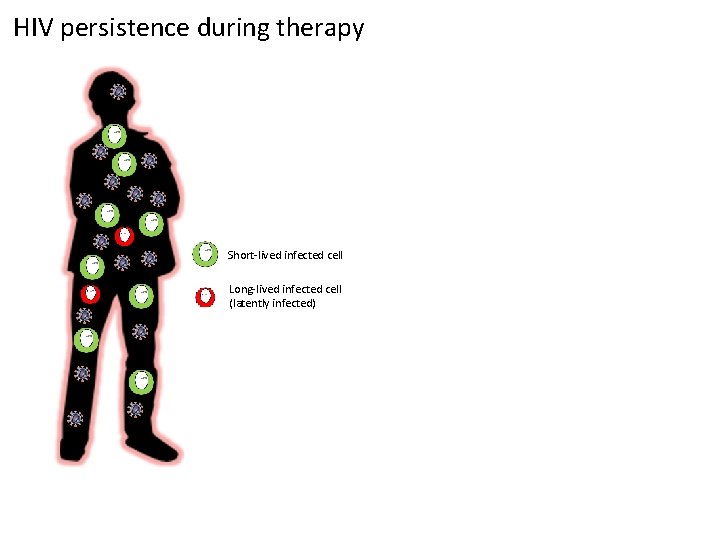
HIV persistence during therapy Short-lived infected cell Long-lived infected cell (latently infected)
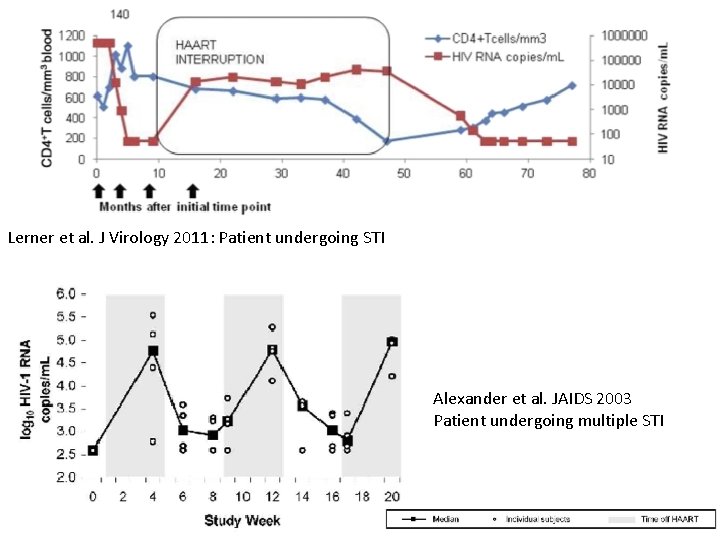
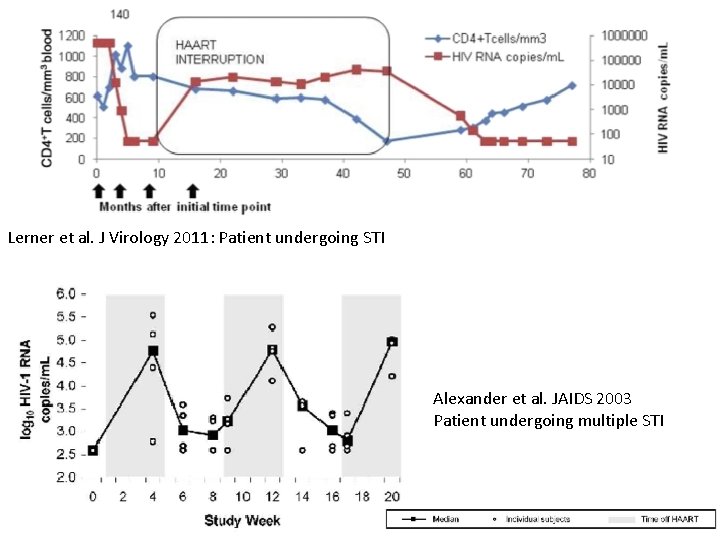
Lerner et al. J Virology 2011: Patient undergoing STI Alexander et al. JAIDS 2003 Patient undergoing multiple STI
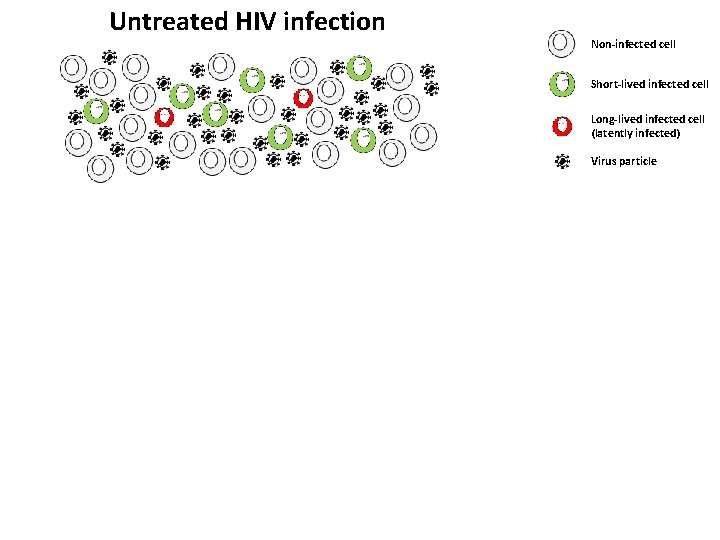
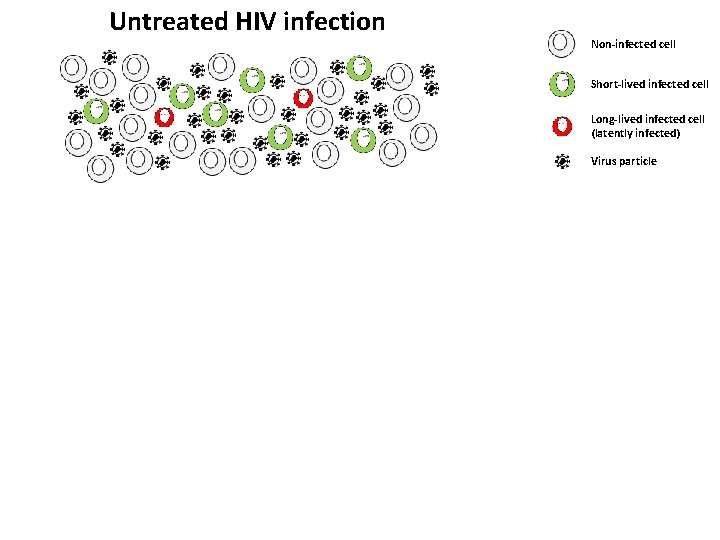
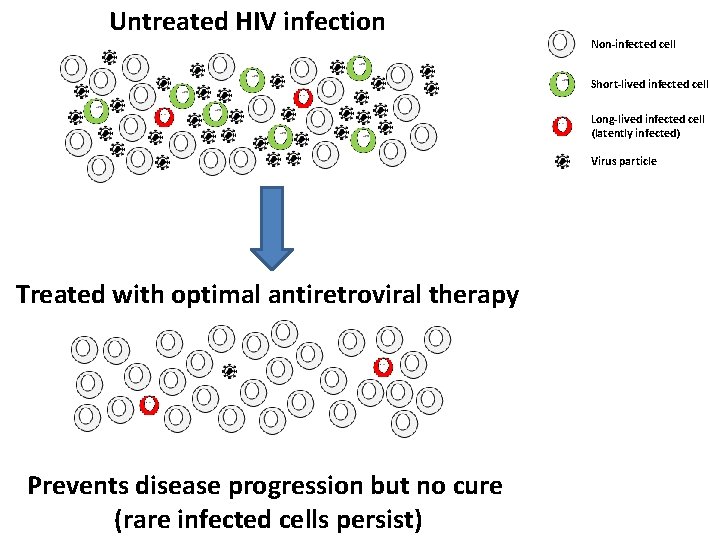
Untreated HIV infection Non-infected cell Short-lived infected cell Long-lived infected cell (latently infected) Virus particle
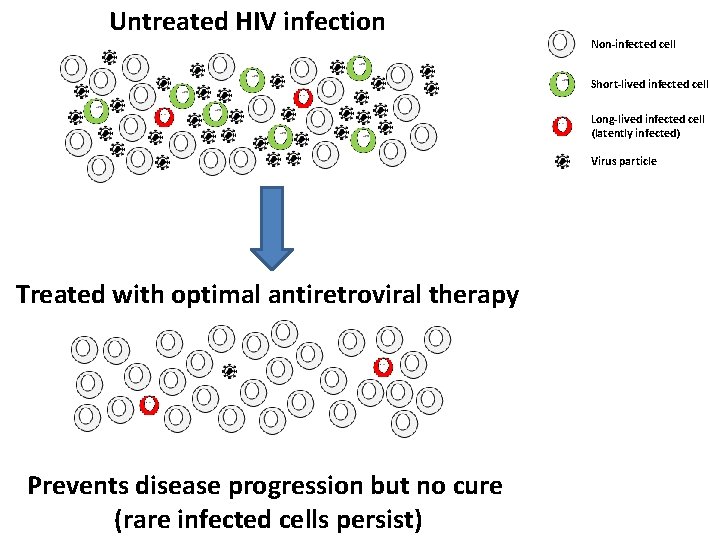
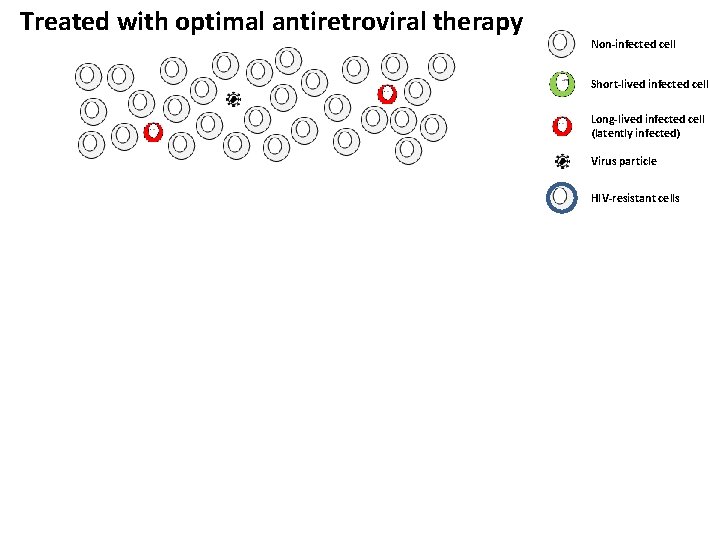
Untreated HIV infection Non-infected cell Short-lived infected cell Long-lived infected cell (latently infected) Virus particle Treated with optimal antiretroviral therapy Prevents disease progression but no cure (rare infected cells persist)
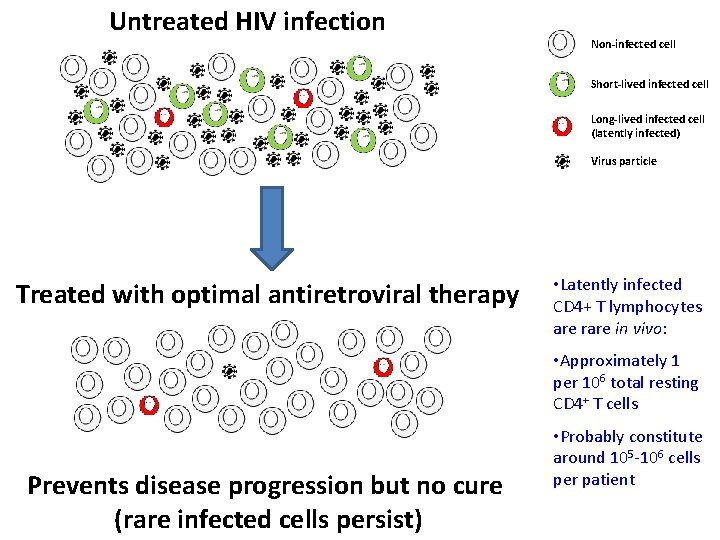
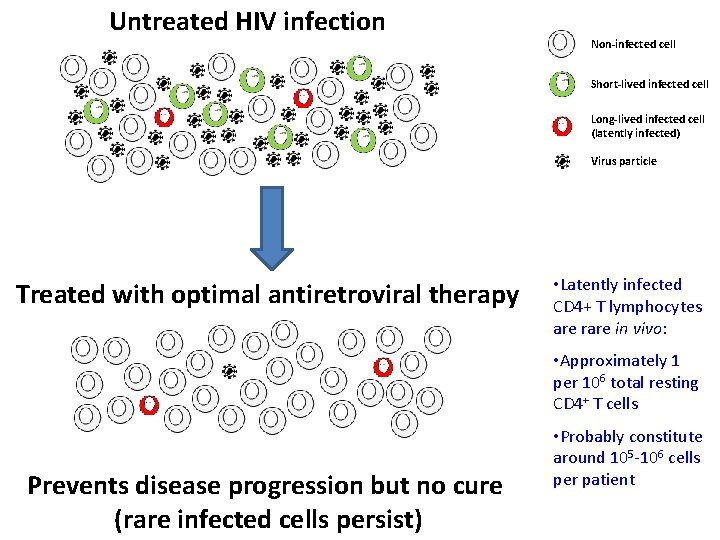
Untreated HIV infection Non-infected cell Short-lived infected cell Long-lived infected cell (latently infected) Virus particle Treated with optimal antiretroviral therapy • Latently infected CD 4+ T lymphocytes are rare in vivo: • Approximately 1 per 106 total resting CD 4+ T cells Prevents disease progression but no cure (rare infected cells persist) • Probably constitute around 105 -106 cells per patient
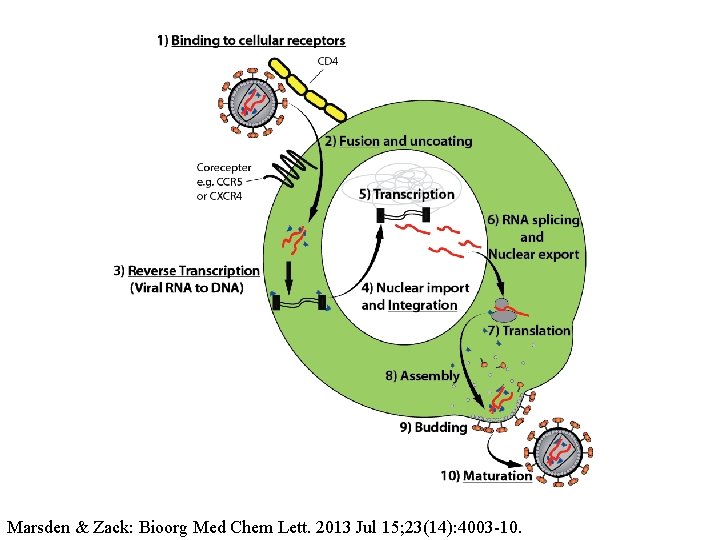
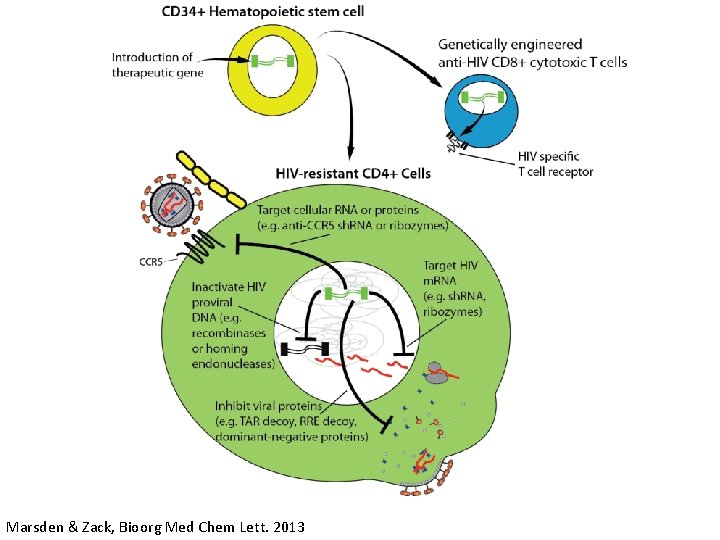
Marsden & Zack: Bioorg Med Chem Lett. 2013 Jul 15; 23(14): 4003 -10.
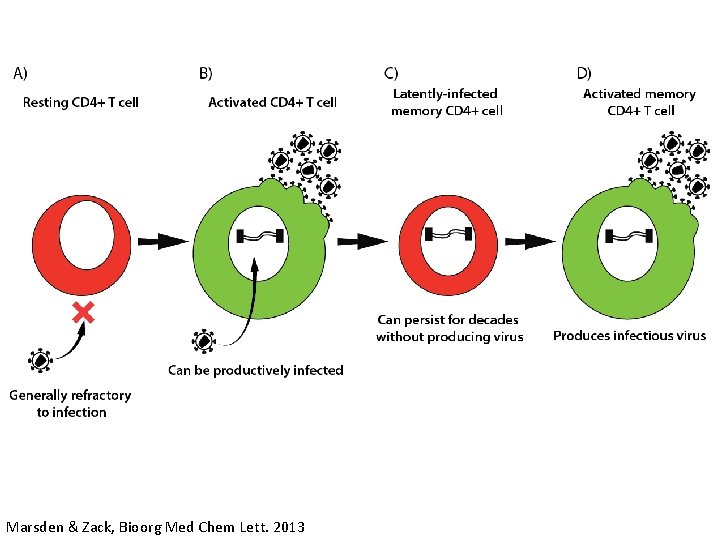
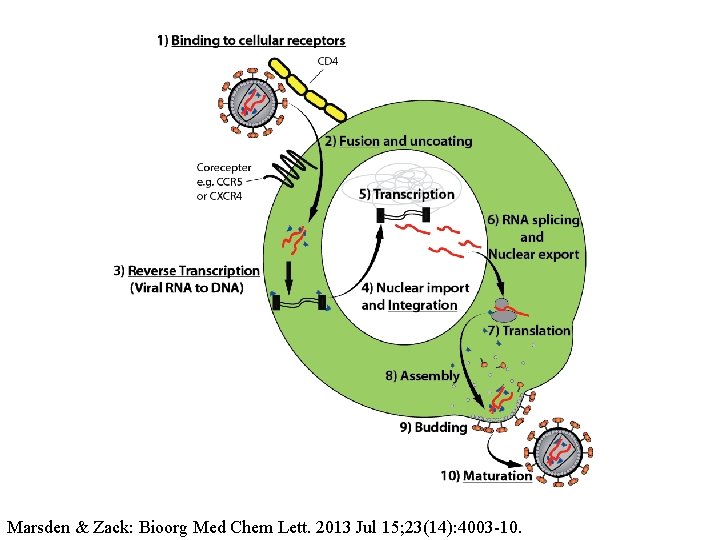
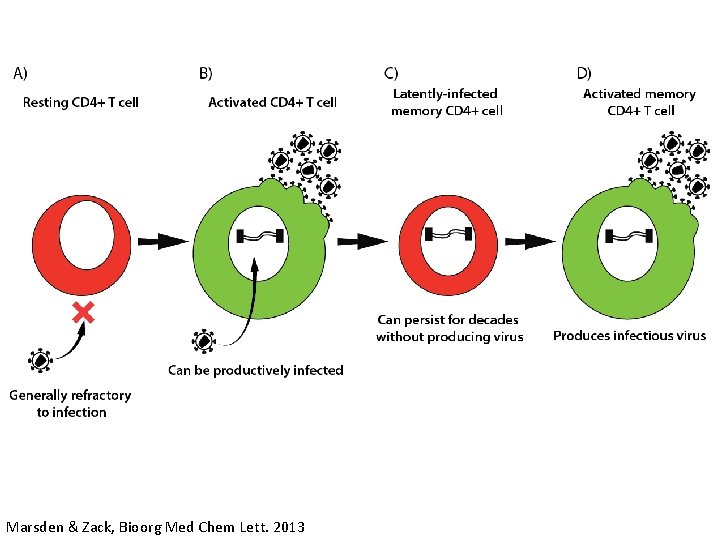
Marsden & Zack, Bioorg Med Chem Lett. 2013
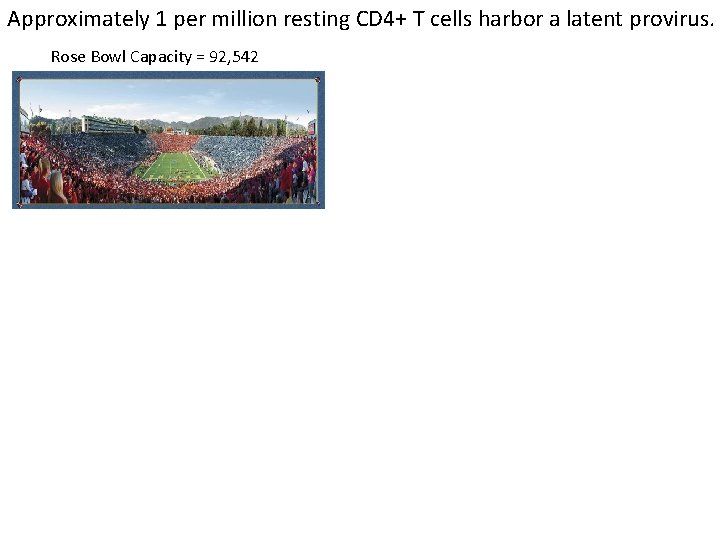
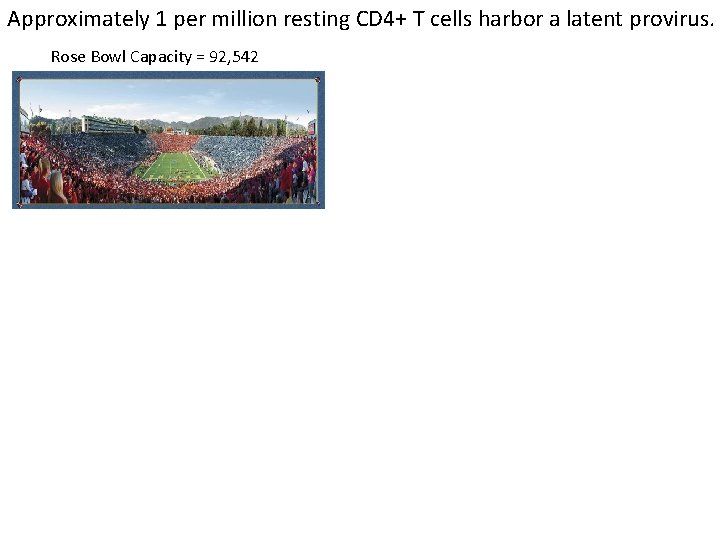
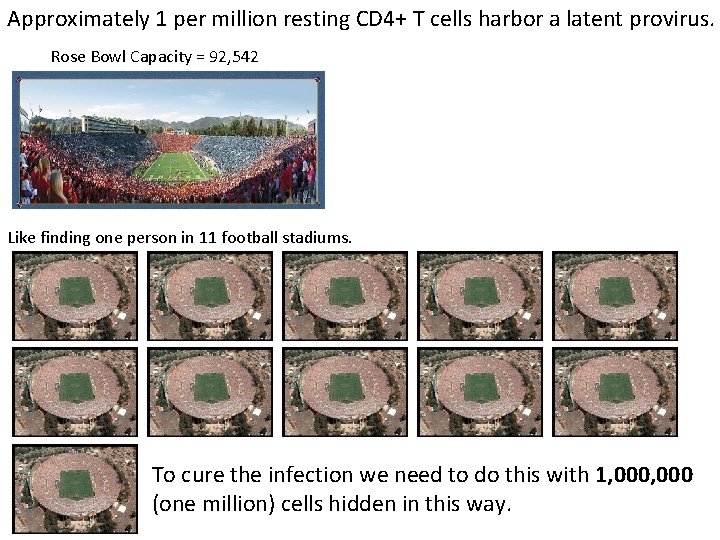
Approximately 1 per million resting CD 4+ T cells harbor a latent provirus. Rose Bowl Capacity = 92, 542
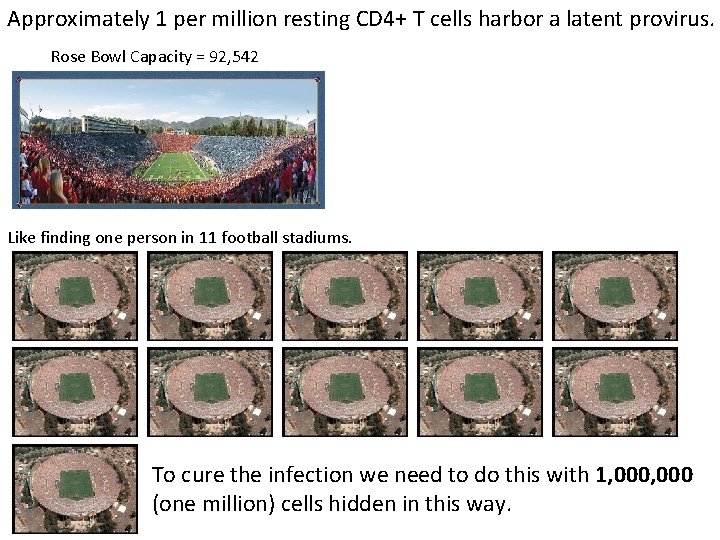
Approximately 1 per million resting CD 4+ T cells harbor a latent provirus. Rose Bowl Capacity = 92, 542 Like finding one person in 11 football stadiums. To cure the infection we need to do this with 1, 000 (one million) cells hidden in this way.
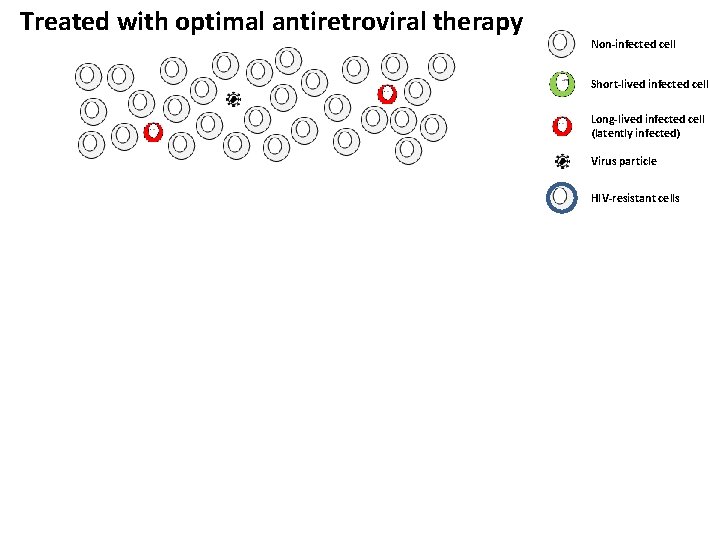
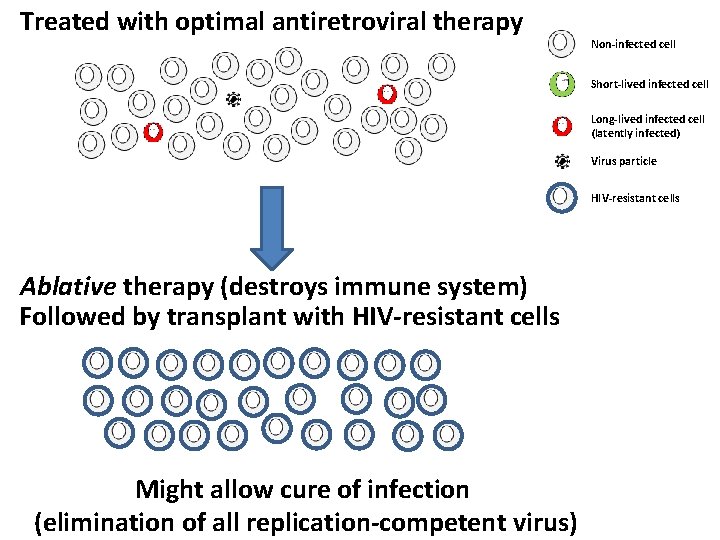
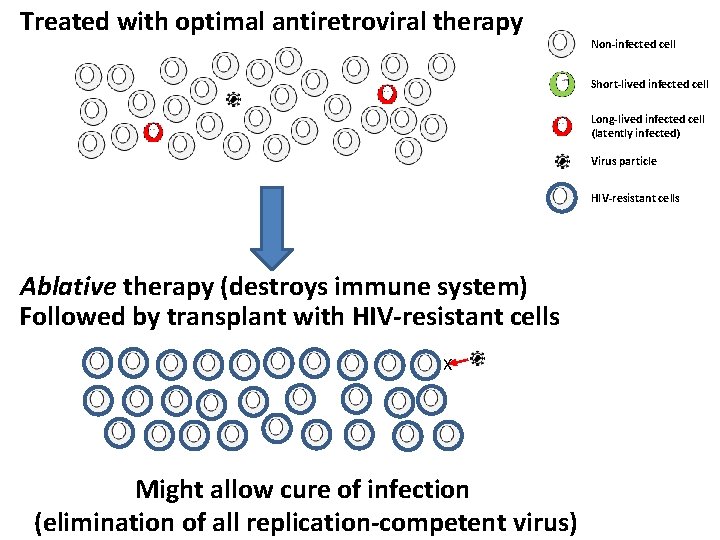
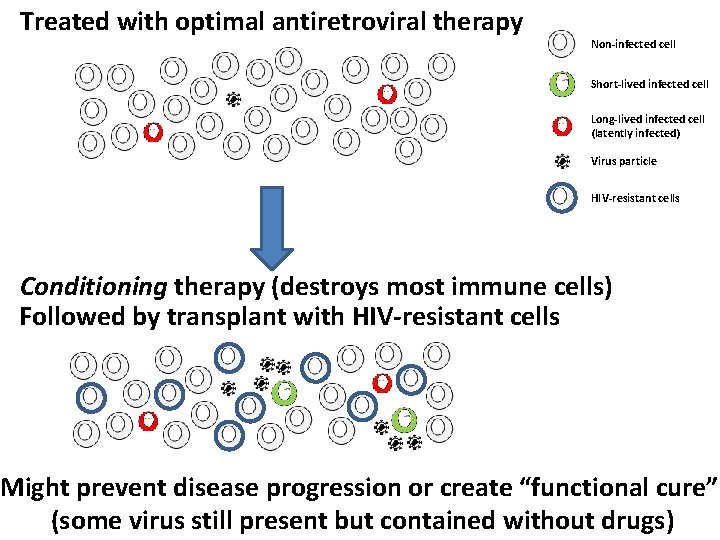
Treated with optimal antiretroviral therapy Non-infected cell Short-lived infected cell Long-lived infected cell (latently infected) Virus particle HIV-resistant cells
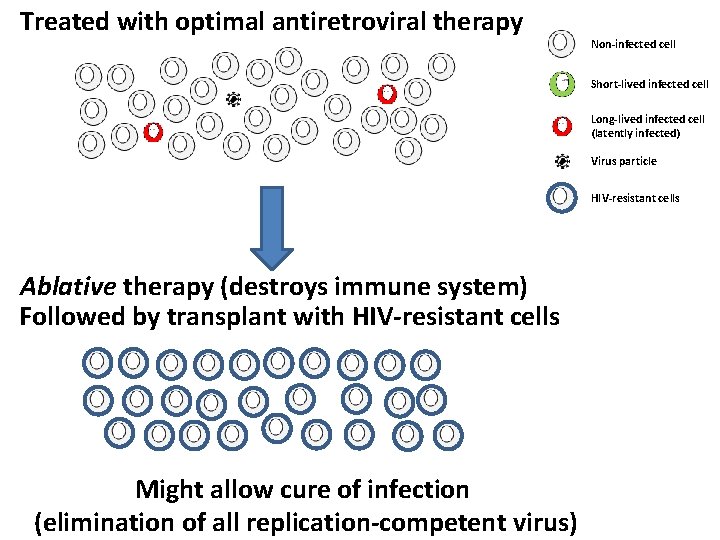
Treated with optimal antiretroviral therapy Non-infected cell Short-lived infected cell Long-lived infected cell (latently infected) Virus particle HIV-resistant cells Ablative therapy (destroys immune system) Followed by transplant with HIV-resistant cells Might allow cure of infection (elimination of all replication-competent virus)
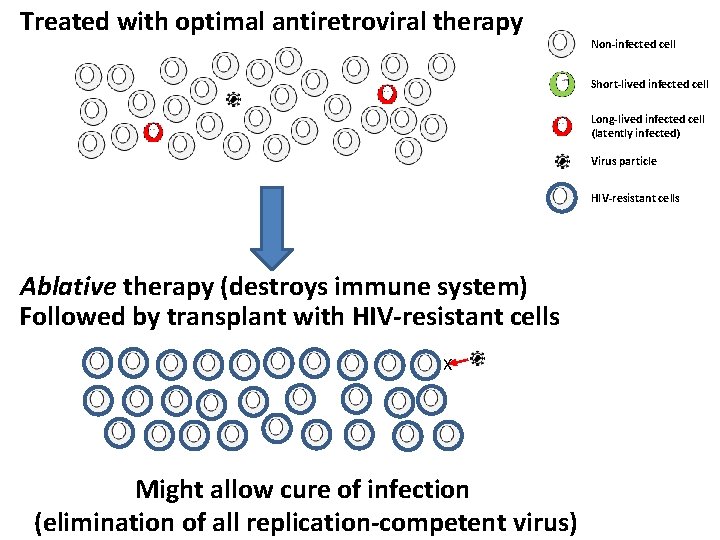
Treated with optimal antiretroviral therapy Non-infected cell Short-lived infected cell Long-lived infected cell (latently infected) Virus particle HIV-resistant cells Ablative therapy (destroys immune system) Followed by transplant with HIV-resistant cells X Might allow cure of infection (elimination of all replication-competent virus)
The “Berlin Patient” http: //pozmagazine. tumblr. com/post/5137593713/timothy-brown-a-k -a-the-berlin-patient-is-the
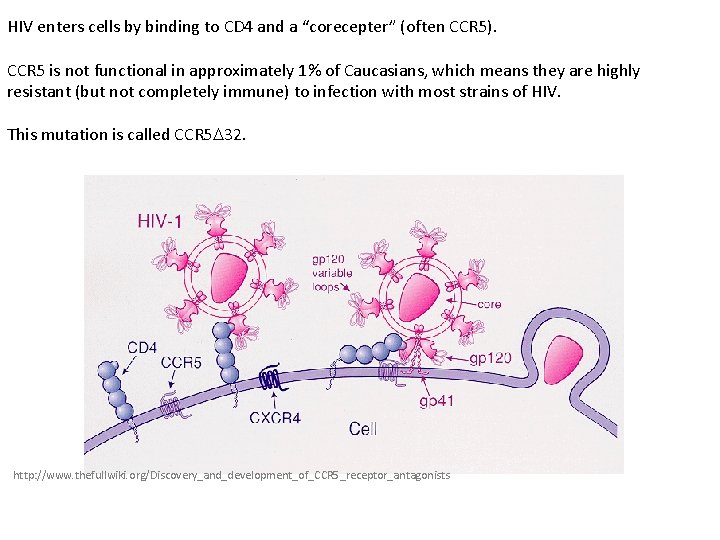
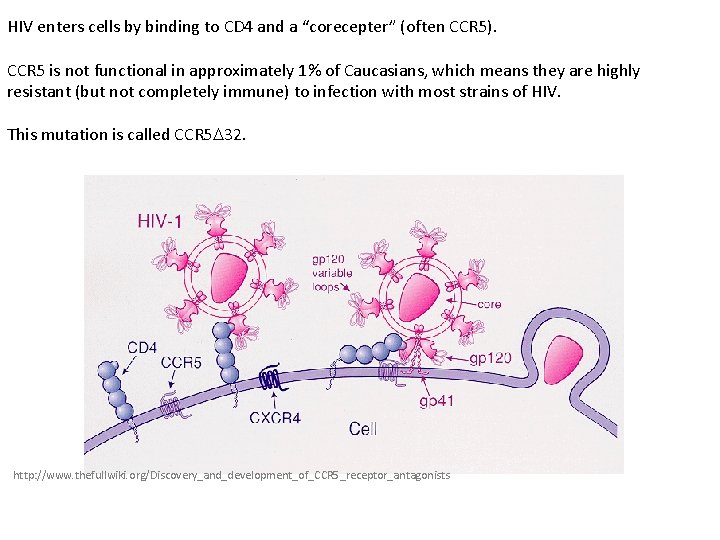
HIV enters cells by binding to CD 4 and a “corecepter” (often CCR 5). CCR 5 is not functional in approximately 1% of Caucasians, which means they are highly resistant (but not completely immune) to infection with most strains of HIV. This mutation is called CCR 5 32. http: //www. thefullwiki. org/Discovery_and_development_of_CCR 5_receptor_antagonists
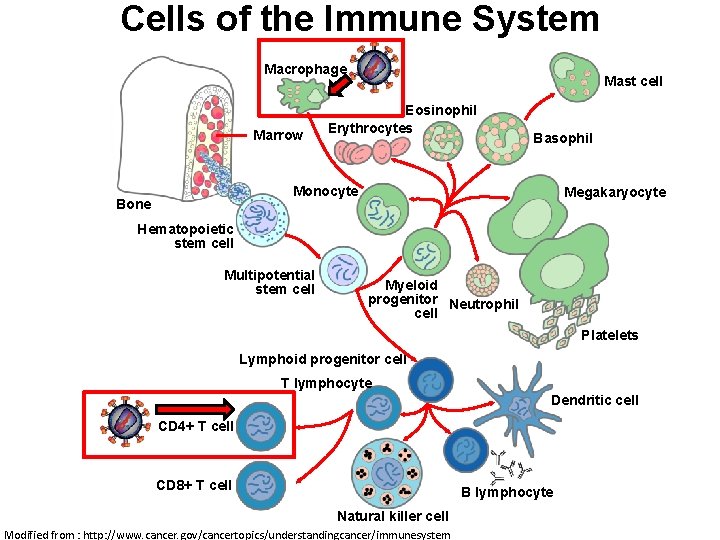
• The “Berlin Patient” was HIV positive and also developed leukemia. • He underwent aggressive chemotherapy to clear the leukemia, and in the process almost all the HIV+ cells in his body were also killed. • This patient then received two bone marrow transplants from a CCR 5 - 32 individual. • The new immune cells were not susceptible HIV, and the virus in currently undetectable more than seven years post-transplant.
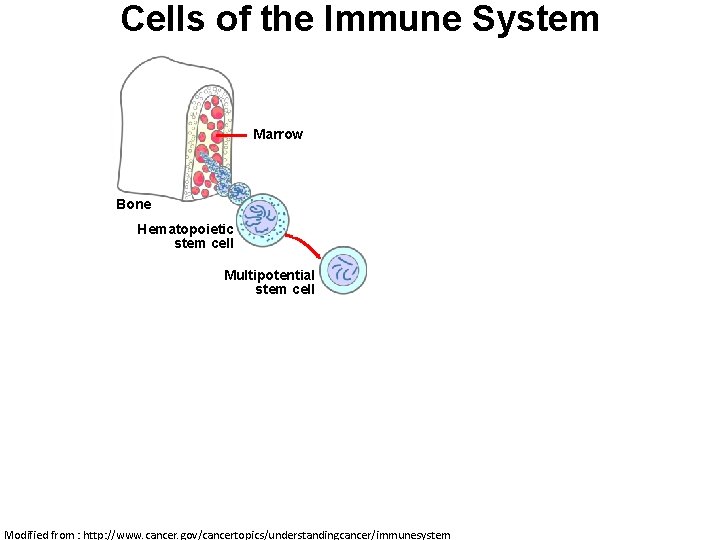
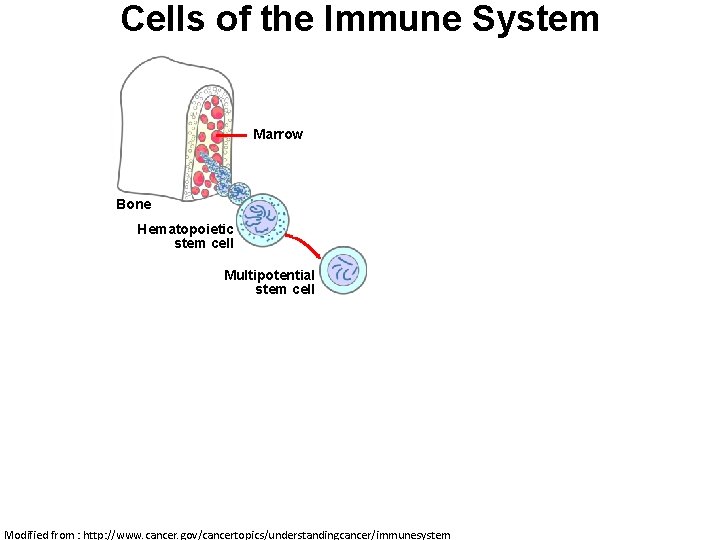
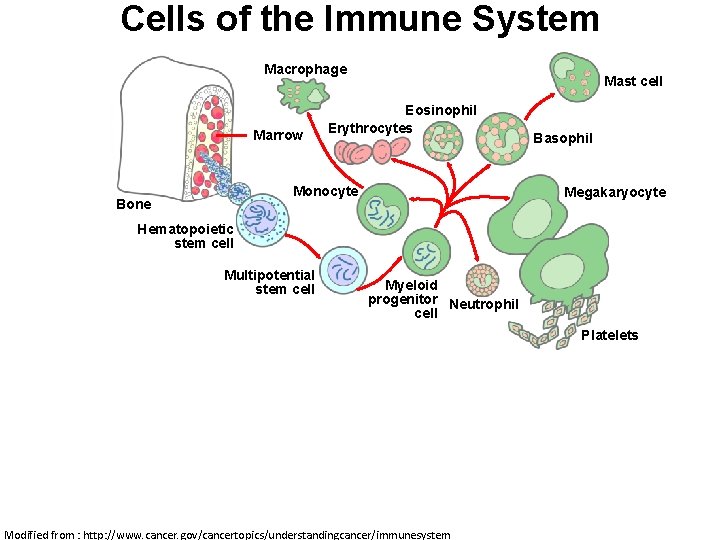
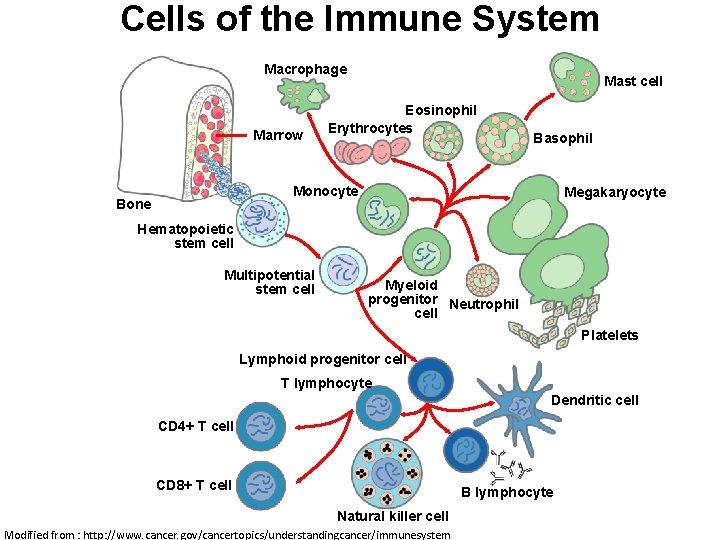
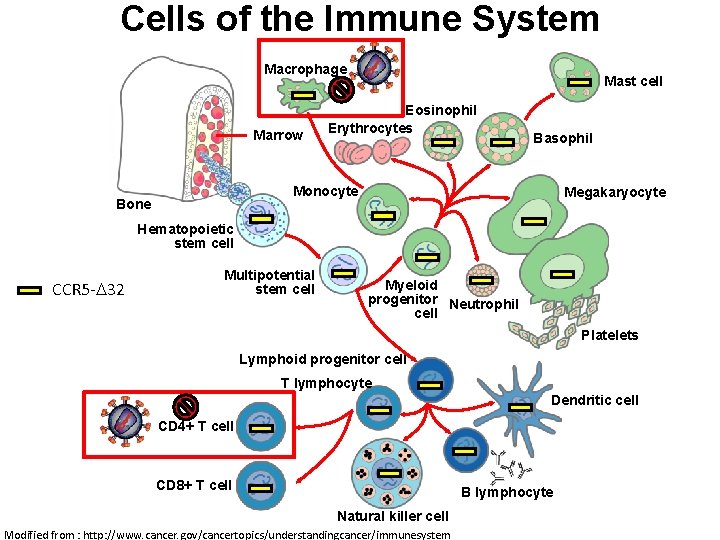
Cells of the Immune System Macrophage Marrow Mast cell Eosinophil Erythrocytes Basophil Monocyte Bone Megakaryocyte Hematopoietic stem cell Multipotential stem cell Myeloid progenitor Neutrophil cell Platelets Lymphoid progenitor cell T lymphocyte Dendritic cell CD 4+ T cell CD 8+ T cell B lymphocyte Natural killer cell Modified from : http: //www. cancer. gov/cancertopics/understandingcancer/immunesystem
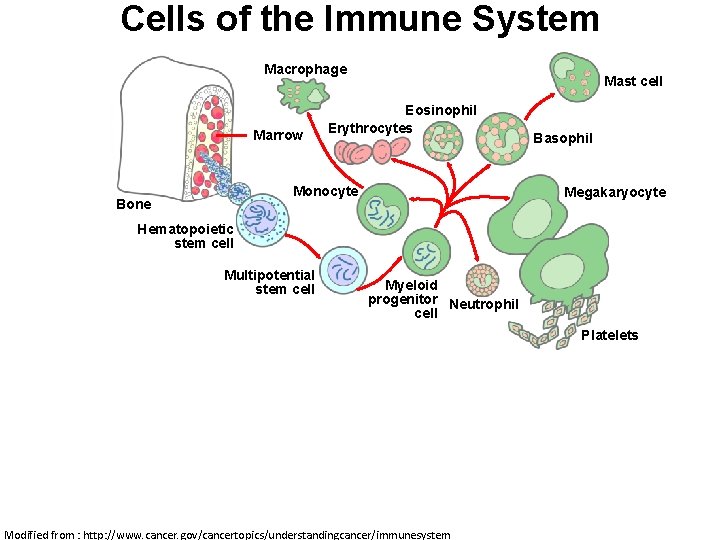
Cells of the Immune System Macrophage Marrow Mast cell Eosinophil Erythrocytes Basophil Monocyte Bone Megakaryocyte Hematopoietic stem cell Multipotential stem cell Myeloid progenitor Neutrophil cell Platelets Lymphoid progenitor cell T lymphocyte Dendritic cell CD 4+ T cell CD 8+ T cell B lymphocyte Natural killer cell Modified from : http: //www. cancer. gov/cancertopics/understandingcancer/immunesystem
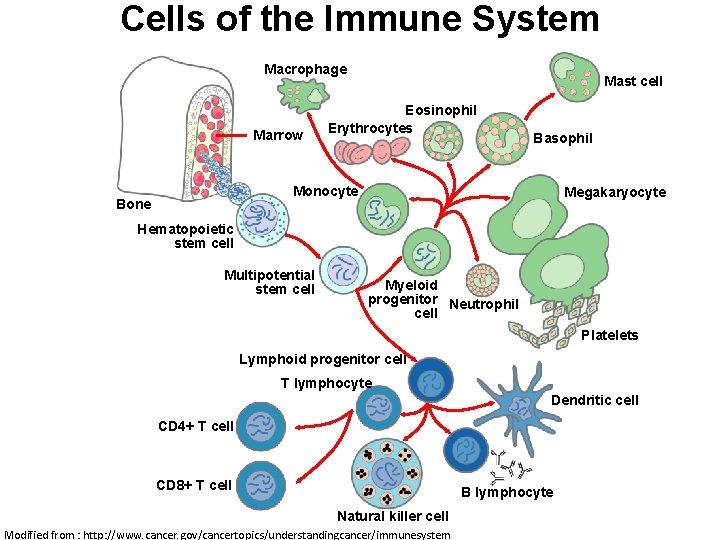
Cells of the Immune System Macrophage Marrow Mast cell Eosinophil Erythrocytes Basophil Monocyte Bone Megakaryocyte Hematopoietic stem cell Multipotential stem cell Myeloid progenitor Neutrophil cell Platelets Lymphoid progenitor cell T lymphocyte Dendritic cell CD 4+ T cell CD 8+ T cell B lymphocyte Natural killer cell Modified from : http: //www. cancer. gov/cancertopics/understandingcancer/immunesystem
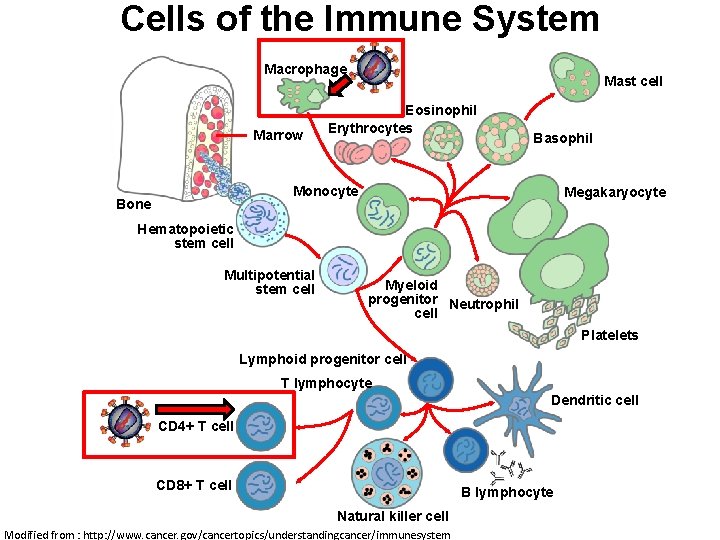
Cells of the Immune System Macrophage Marrow Mast cell Eosinophil Erythrocytes Basophil Monocyte Bone Megakaryocyte Hematopoietic stem cell Multipotential stem cell Myeloid progenitor Neutrophil cell Platelets Lymphoid progenitor cell T lymphocyte Dendritic cell CD 4+ T cell CD 8+ T cell B lymphocyte Natural killer cell Modified from : http: //www. cancer. gov/cancertopics/understandingcancer/immunesystem
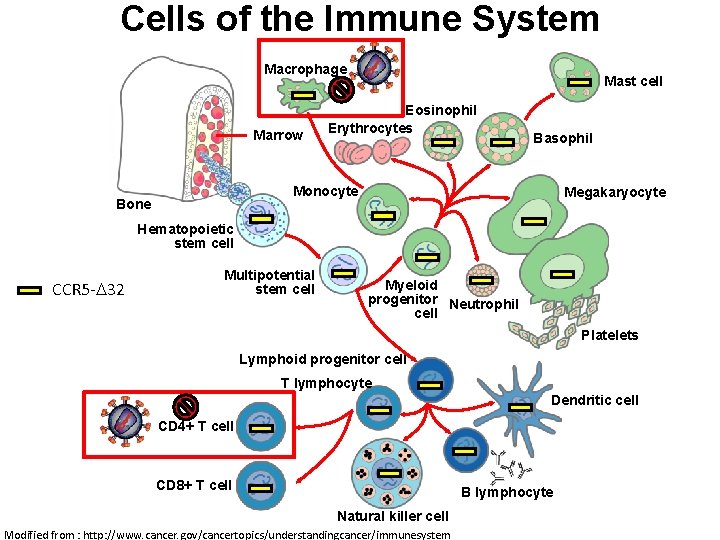
Cells of the Immune System Macrophage Marrow Mast cell Eosinophil Erythrocytes Basophil Monocyte Bone Megakaryocyte Hematopoietic stem cell CCR 5 - 32 Multipotential stem cell Myeloid progenitor Neutrophil cell Platelets Lymphoid progenitor cell T lymphocyte Dendritic cell CD 4+ T cell CD 8+ T cell B lymphocyte Natural killer cell Modified from : http: //www. cancer. gov/cancertopics/understandingcancer/immunesystem
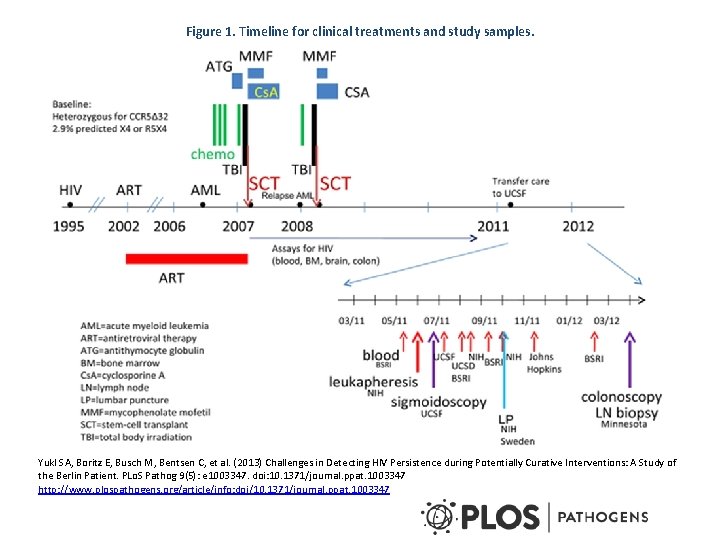
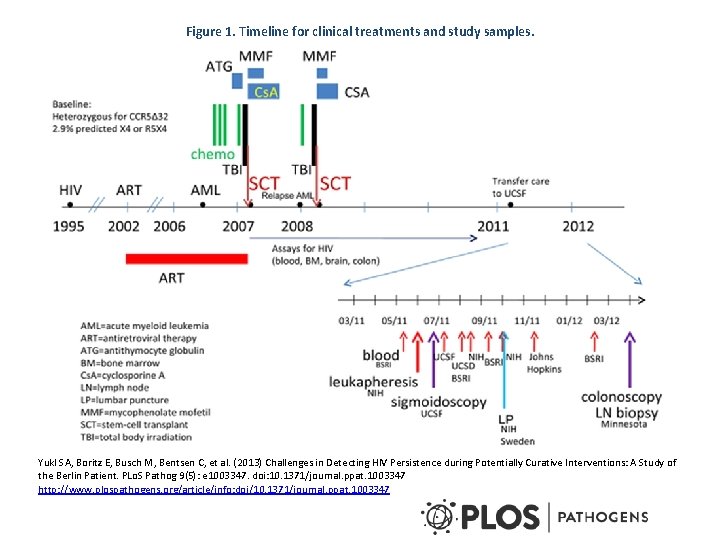
Figure 1. Timeline for clinical treatments and study samples. Yukl SA, Boritz E, Busch M, Bentsen C, et al. (2013) Challenges in Detecting HIV Persistence during Potentially Curative Interventions: A Study of the Berlin Patient. PLo. S Pathog 9(5): e 1003347. doi: 10. 1371/journal. ppat. 1003347 http: //www. plospathogens. org/article/info: doi/10. 1371/journal. ppat. 1003347
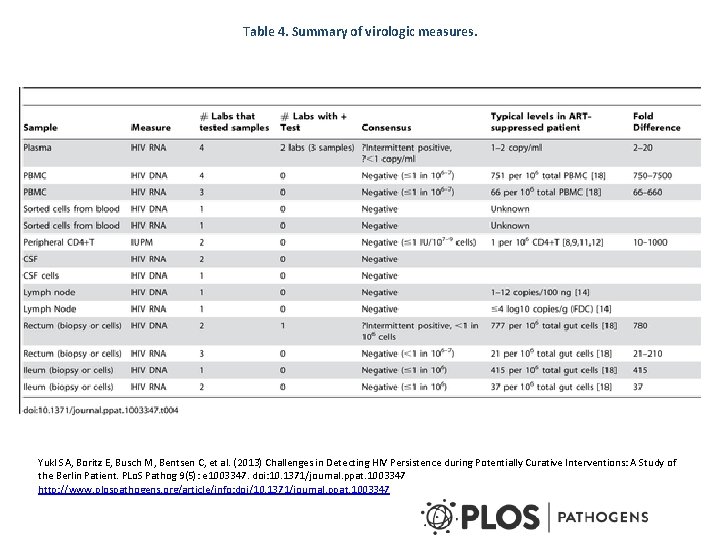
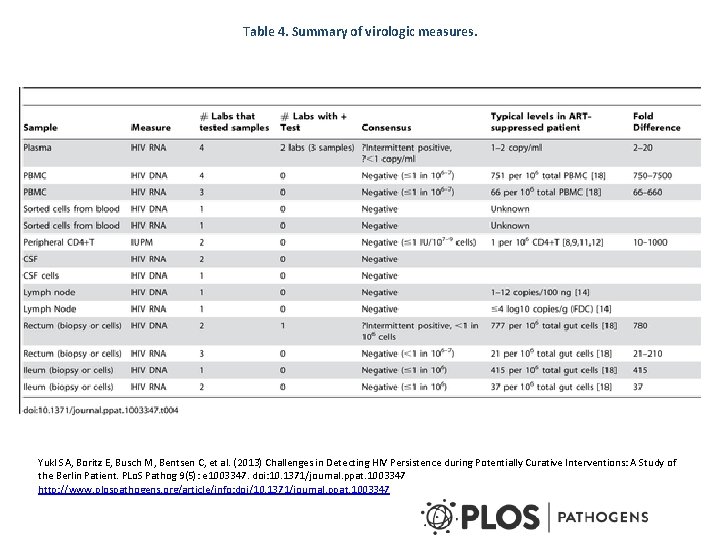
Table 4. Summary of virologic measures. Yukl SA, Boritz E, Busch M, Bentsen C, et al. (2013) Challenges in Detecting HIV Persistence during Potentially Curative Interventions: A Study of the Berlin Patient. PLo. S Pathog 9(5): e 1003347. doi: 10. 1371/journal. ppat. 1003347 http: //www. plospathogens. org/article/info: doi/10. 1371/journal. ppat. 1003347
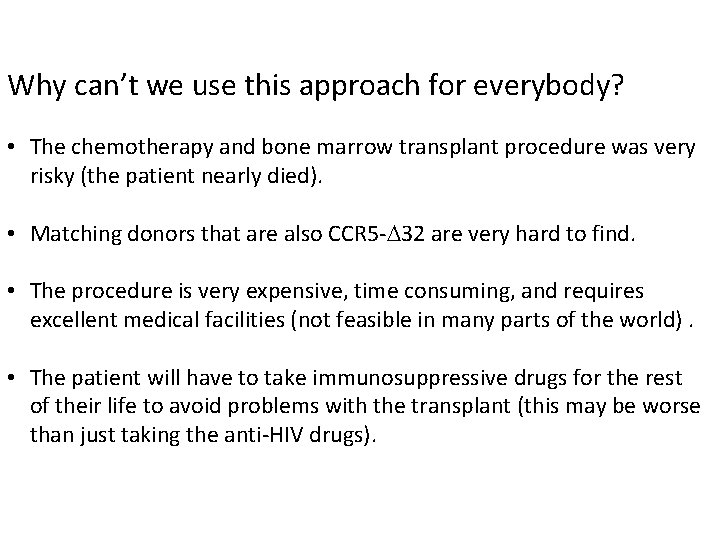
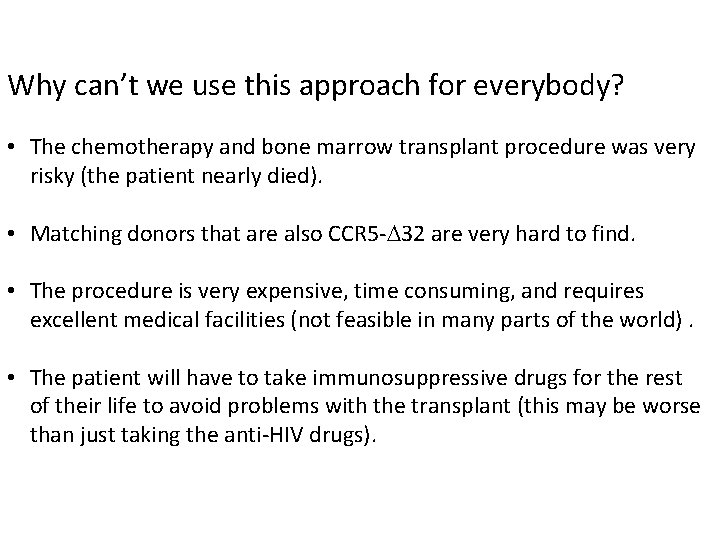
Why can’t we use this approach for everybody? • The chemotherapy and bone marrow transplant procedure was very risky (the patient nearly died). • Matching donors that are also CCR 5 - 32 are very hard to find. • The procedure is very expensive, time consuming, and requires excellent medical facilities (not feasible in many parts of the world). • The patient will have to take immunosuppressive drugs for the rest of their life to avoid problems with the transplant (this may be worse than just taking the anti-HIV drugs).
The “Boston Patients” Dr. Timothy Henrich of Brigham and Women's Hospital

Bone marrow transplant with unprotected (not HIV-resistant) donor cells “the 2 Boston Patients” delayed viral rebound…. . But did not prevent it. . . http: //www. cnn. com/2013/12/07/health/hiv-patients/
• The “Boston Patients” were HIV positive and also developed leukemia. • They underwent reduced-intensity chemotherapy to clear the leukemia (stayed on antiretroviral therapy during this process). • They then received a bone marrow transplants (not HIV-resistant cells). • Stayed on ART for 2. 6 and 4. 3 years and virus was not detectable. • Upon treatment interruption, viral rebound occurred after 3 and 8 months.
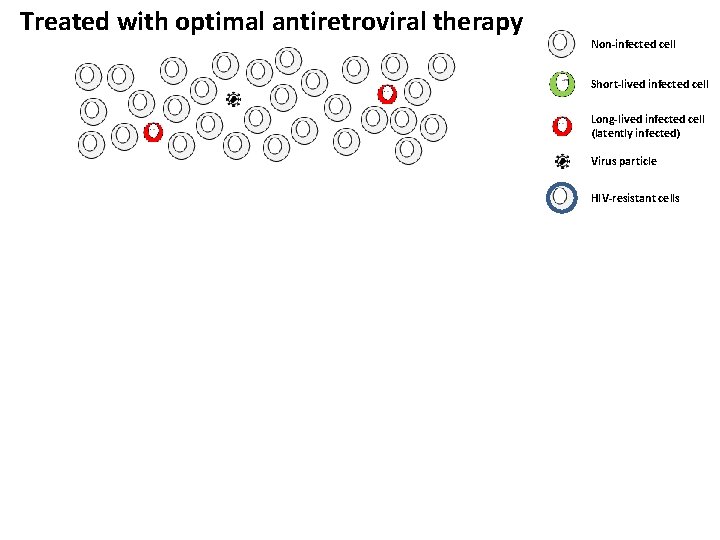
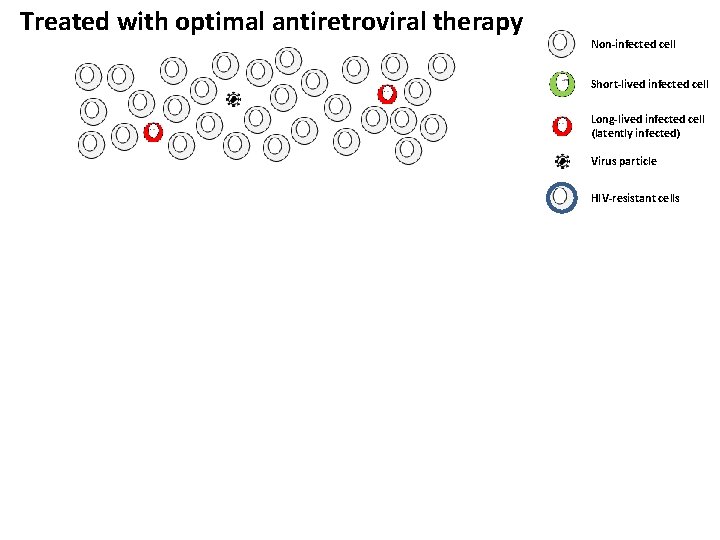
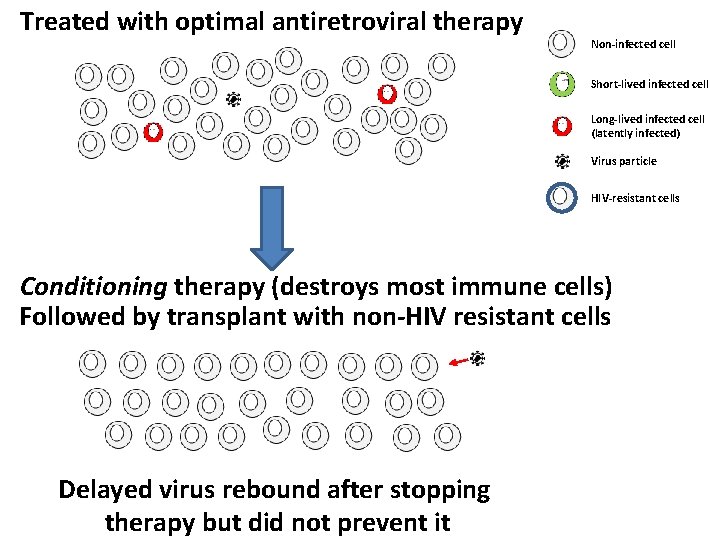
Treated with optimal antiretroviral therapy Non-infected cell Short-lived infected cell Long-lived infected cell (latently infected) Virus particle HIV-resistant cells
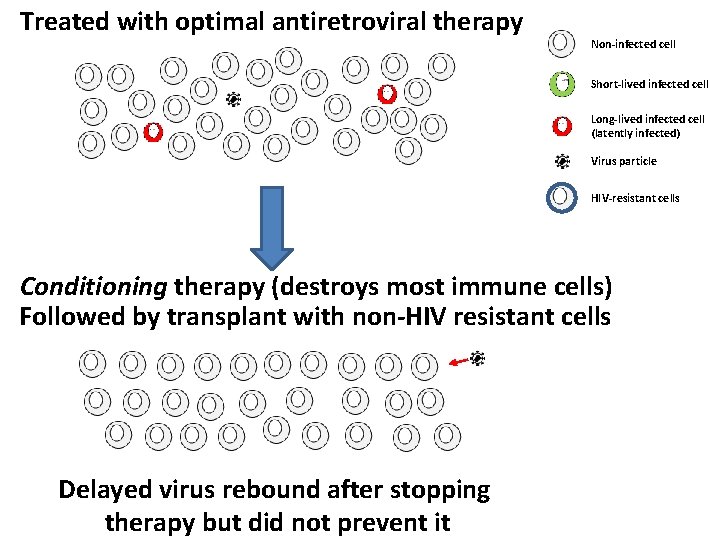
Treated with optimal antiretroviral therapy Non-infected cell Short-lived infected cell Long-lived infected cell (latently infected) Virus particle HIV-resistant cells Conditioning therapy (destroys most immune cells) Followed by transplant with non-HIV resistant cells Delayed virus rebound after stopping therapy but did not prevent it

The “Mississippi baby”
Detection of Human Immunodeficiency Virus Type 1 (HIV-1) Infection in the Child. Persaud D et al. N Engl J Med 2013; 369: 18281835. http: //www. nejm. org/doi/full/10. 1056/NEJMoa 1302976#t=article “An infant was born by spontaneous vaginal delivery at 35 weeks of gestation to a woman who had received no prenatal care. Rapid HIV-1 testing in the mother was positive during labor. Delivery occurred before antiretroviral prophylaxis was administered. Maternal HIV -1 infection was confirmed by means of Western blot testing. ” “ART was initiated in the infant at 30 hours of age. A three-drug regimen of zidovudine (at a dose of 2 mg per kilogram of body weight every 6 hours), lamivudine (at a dose of 4 mg per kilogram twice daily), and nevirapine (at a dose of 2 mg per kilogram twice daily) was selected to provide prophylaxis for high-risk HIV-1 exposure and to minimize the likelihood of generating resistant viral variants in the event that the infant had been infected in utero. ”
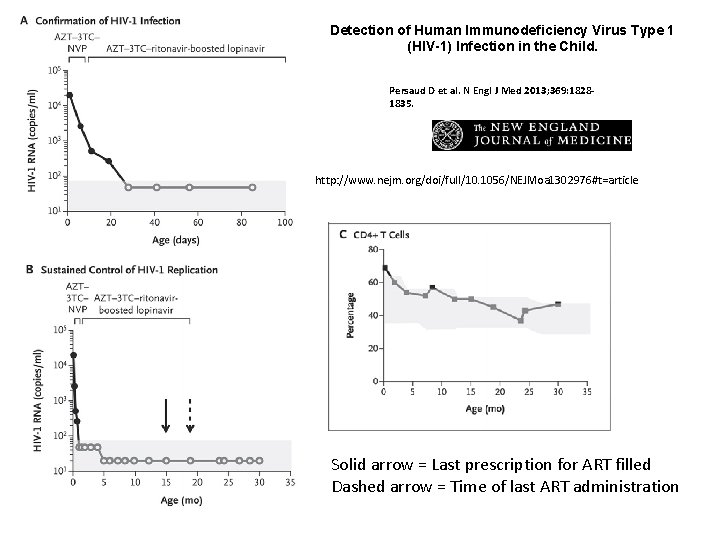
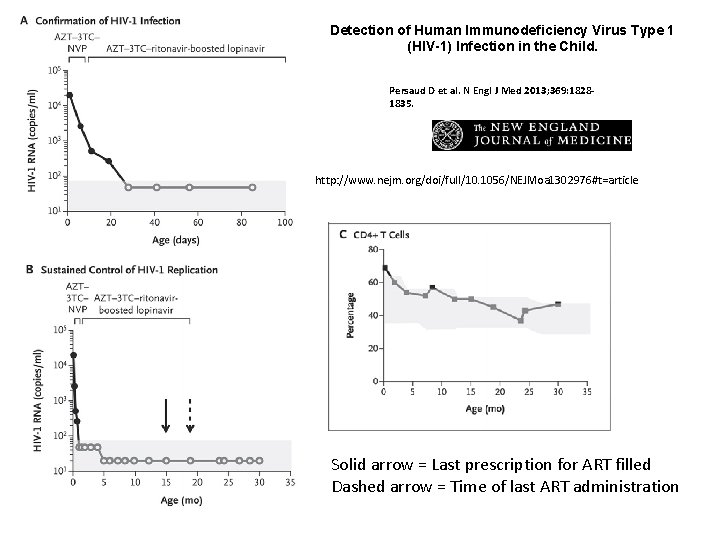
Detection of Human Immunodeficiency Virus Type 1 (HIV-1) Infection in the Child. Persaud D et al. N Engl J Med 2013; 369: 18281835. http: //www. nejm. org/doi/full/10. 1056/NEJMoa 1302976#t=article Solid arrow = Last prescription for ART filled Dashed arrow = Time of last ART administration
http: //www. usatoday. com/story/news/nation/2014/03/05/hiv-baby-cure/6081221/ The “LA Baby” has a similar story to the “Mississippi baby”, but has yet to undergo ART treatment interruption. “The girl was delivered at Miller Children's Hospital in Long Beach, California, last summer to a mother with HIV who had not received antiretroviral drugs during pregnancy. Doctors gave the baby high doses of three drugs -- AZT, 3 TC and Nevirapine -- four hours after birth. Eleven days later, the virus was undetectable in her body and remained undetectable eight months later. ” http: //www. cnn. com/2014/03/06/health/hiv-baby-cured/
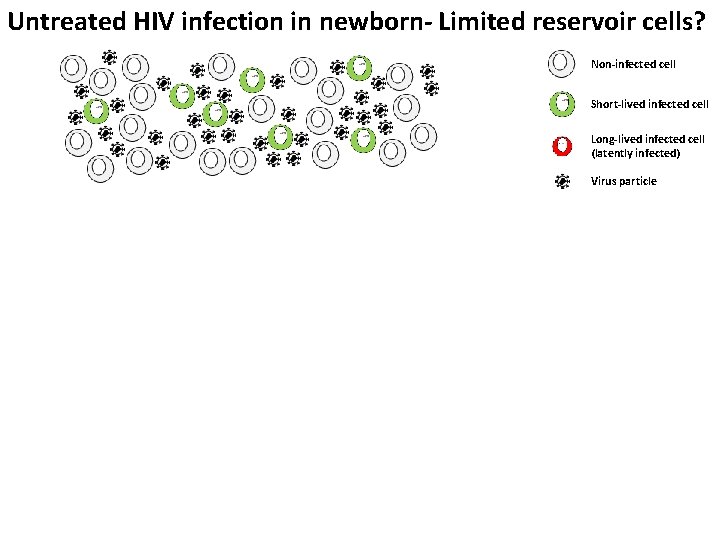
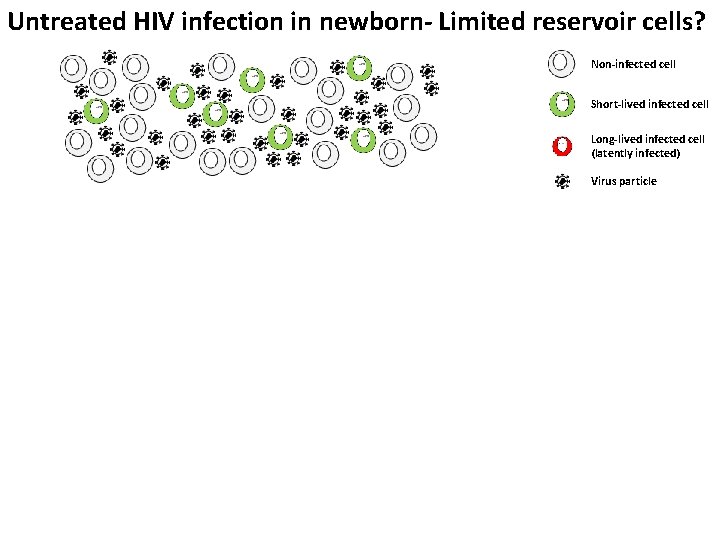
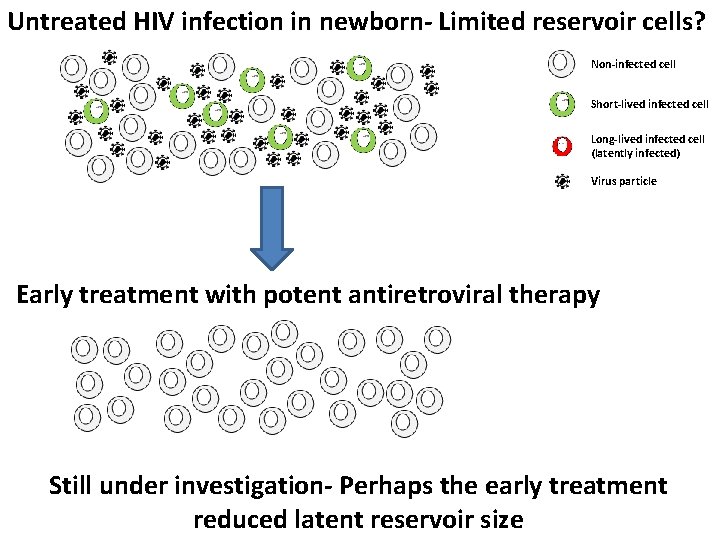
Untreated HIV infection in newborn- Limited reservoir cells? Non-infected cell Short-lived infected cell Long-lived infected cell (latently infected) Virus particle
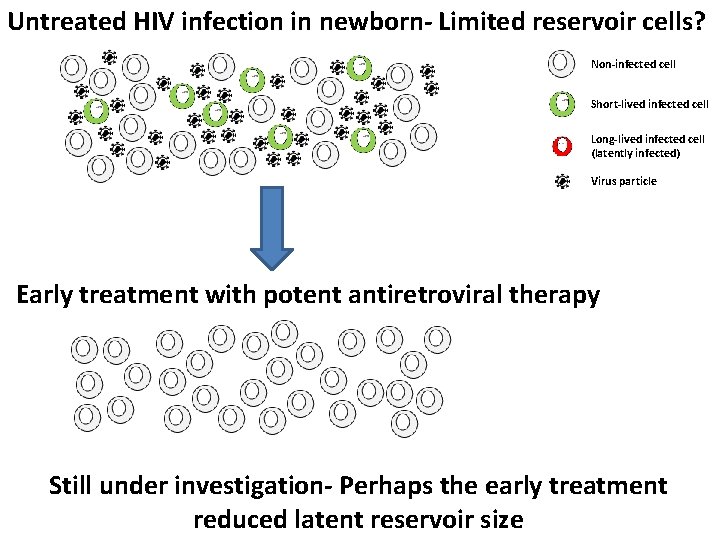
Untreated HIV infection in newborn- Limited reservoir cells? Non-infected cell Short-lived infected cell Long-lived infected cell (latently infected) Virus particle Early treatment with potent antiretroviral therapy Still under investigation- Perhaps the early treatment reduced latent reservoir size
The “VISCONTI cohort” Viro-Immunologic Sustained COntrol after Treatment Interruption “Functional cure” for some patients?
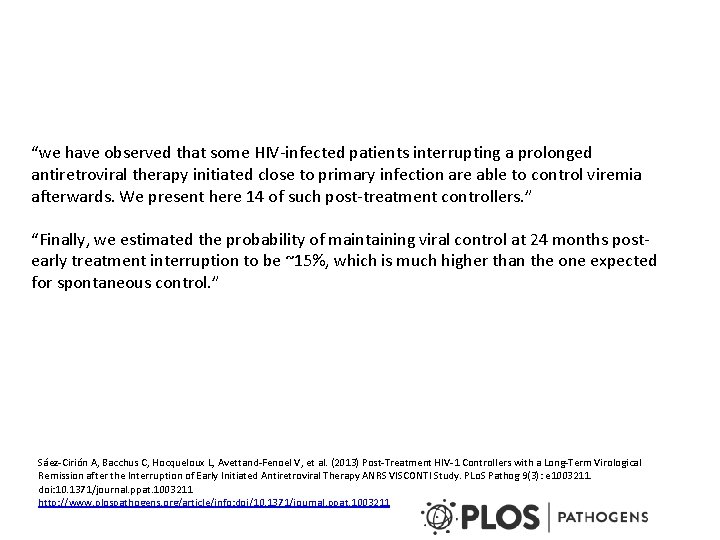
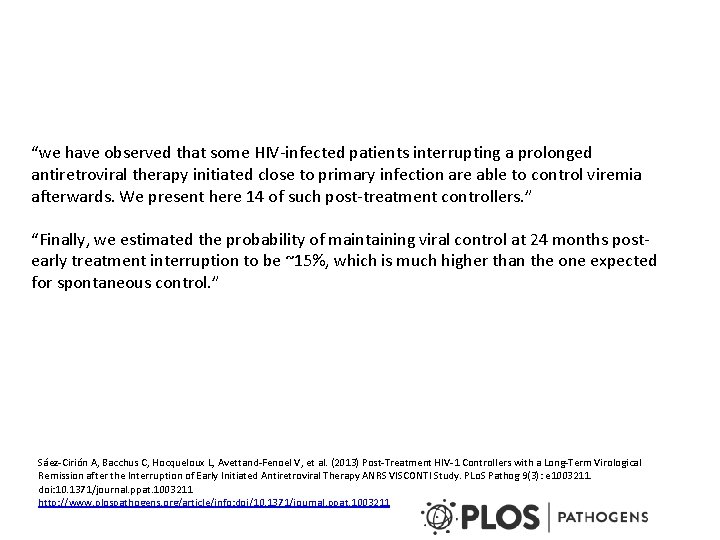
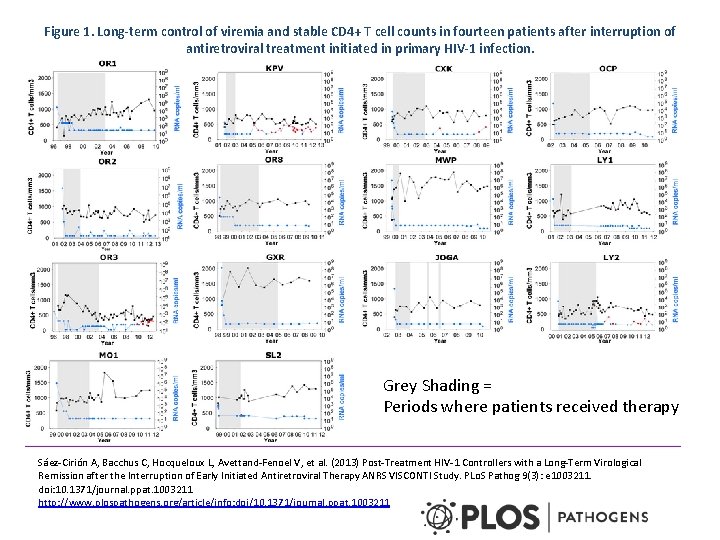
“we have observed that some HIV-infected patients interrupting a prolonged antiretroviral therapy initiated close to primary infection are able to control viremia afterwards. We present here 14 of such post-treatment controllers. ” “Finally, we estimated the probability of maintaining viral control at 24 months postearly treatment interruption to be ~15%, which is much higher than the one expected for spontaneous control. ” Sáez-Cirión A, Bacchus C, Hocqueloux L, Avettand-Fenoel V, et al. (2013) Post-Treatment HIV-1 Controllers with a Long-Term Virological Remission after the Interruption of Early Initiated Antiretroviral Therapy ANRS VISCONTI Study. PLo. S Pathog 9(3): e 1003211. doi: 10. 1371/journal. ppat. 1003211 http: //www. plospathogens. org/article/info: doi/10. 1371/journal. ppat. 1003211
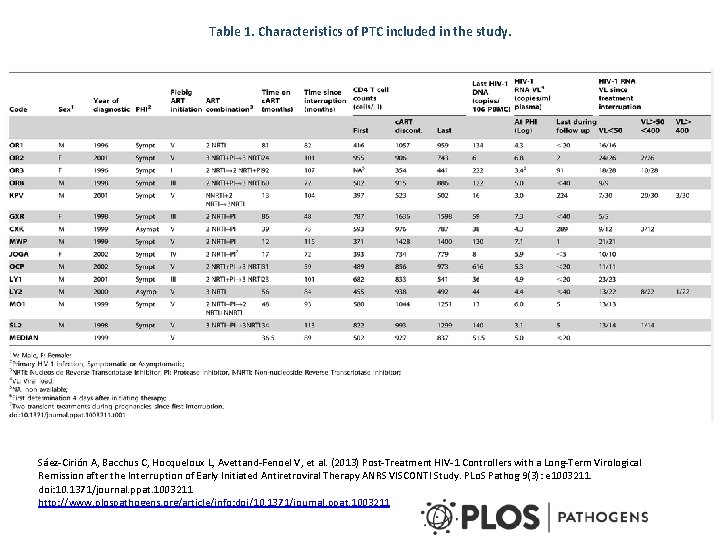
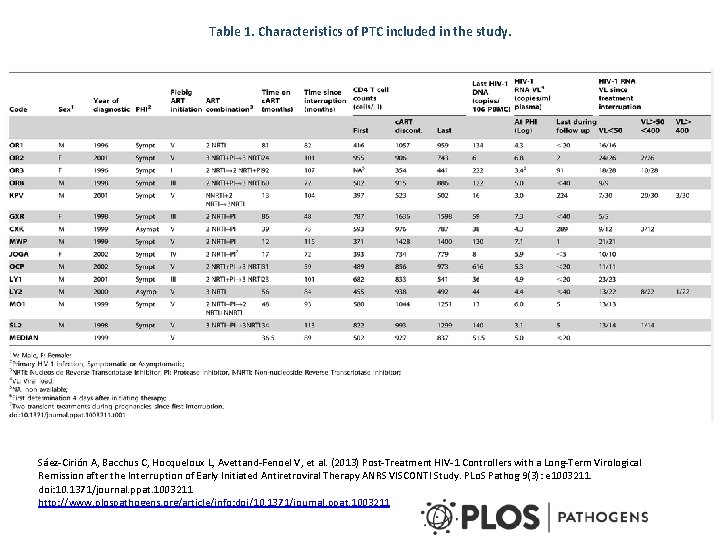
Table 1. Characteristics of PTC included in the study. Sáez-Cirión A, Bacchus C, Hocqueloux L, Avettand-Fenoel V, et al. (2013) Post-Treatment HIV-1 Controllers with a Long-Term Virological Remission after the Interruption of Early Initiated Antiretroviral Therapy ANRS VISCONTI Study. PLo. S Pathog 9(3): e 1003211. doi: 10. 1371/journal. ppat. 1003211 http: //www. plospathogens. org/article/info: doi/10. 1371/journal. ppat. 1003211
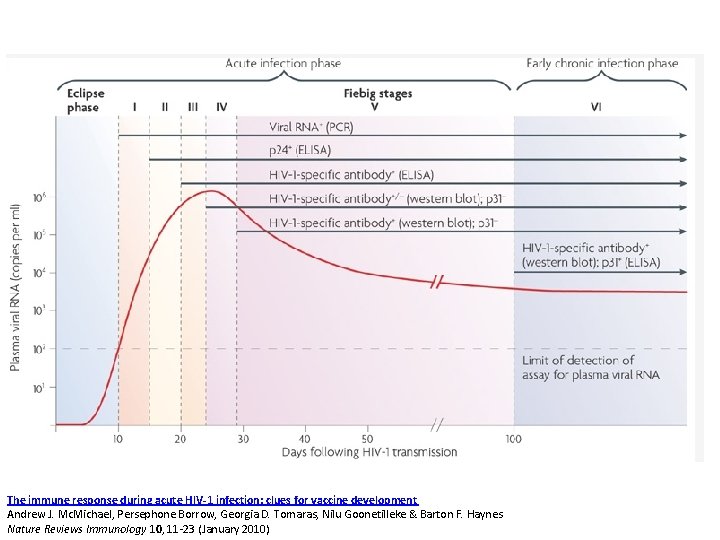
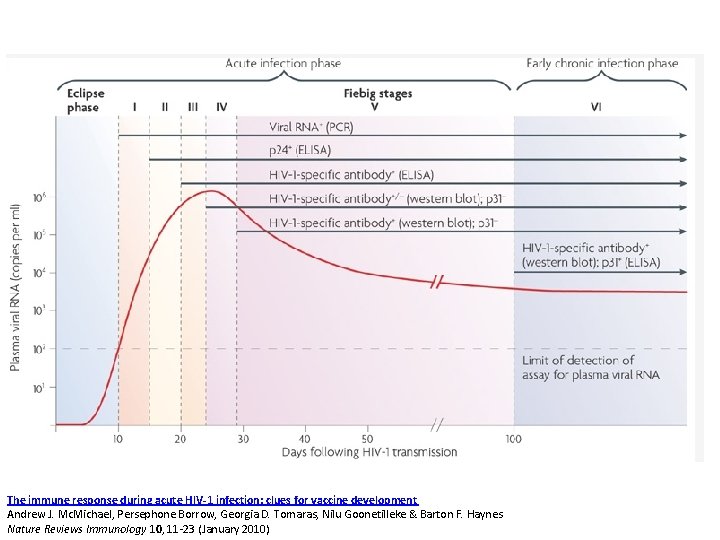
The immune response during acute HIV-1 infection: clues for vaccine development Andrew J. Mc. Michael, Persephone Borrow, Georgia D. Tomaras, Nilu Goonetilleke & Barton F. Haynes Nature Reviews Immunology 10, 11 -23 (January 2010)
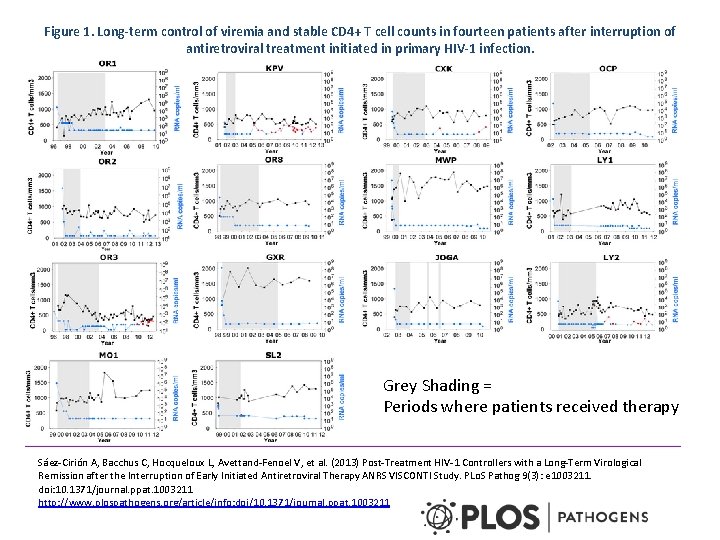
Figure 1. Long-term control of viremia and stable CD 4+ T cell counts in fourteen patients after interruption of antiretroviral treatment initiated in primary HIV-1 infection. Grey Shading = Periods where patients received therapy Sáez-Cirión A, Bacchus C, Hocqueloux L, Avettand-Fenoel V, et al. (2013) Post-Treatment HIV-1 Controllers with a Long-Term Virological Remission after the Interruption of Early Initiated Antiretroviral Therapy ANRS VISCONTI Study. PLo. S Pathog 9(3): e 1003211. doi: 10. 1371/journal. ppat. 1003211 http: //www. plospathogens. org/article/info: doi/10. 1371/journal. ppat. 1003211
New experimental gene therapy/transplantation cure approaches
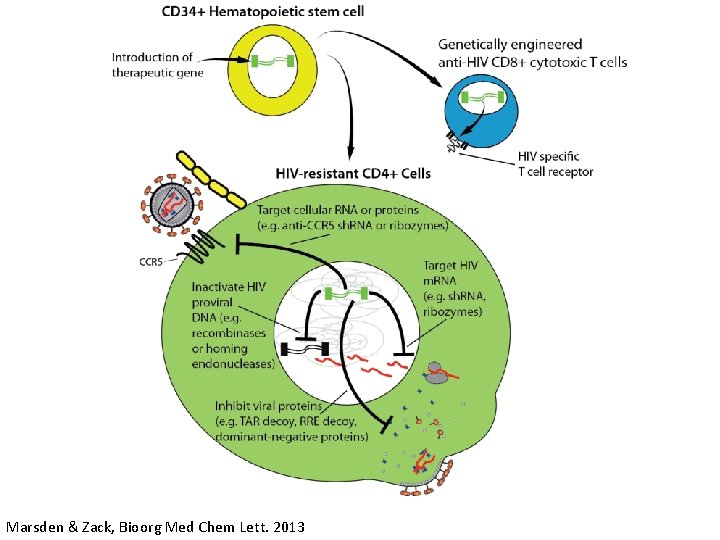
Marsden & Zack, Bioorg Med Chem Lett. 2013
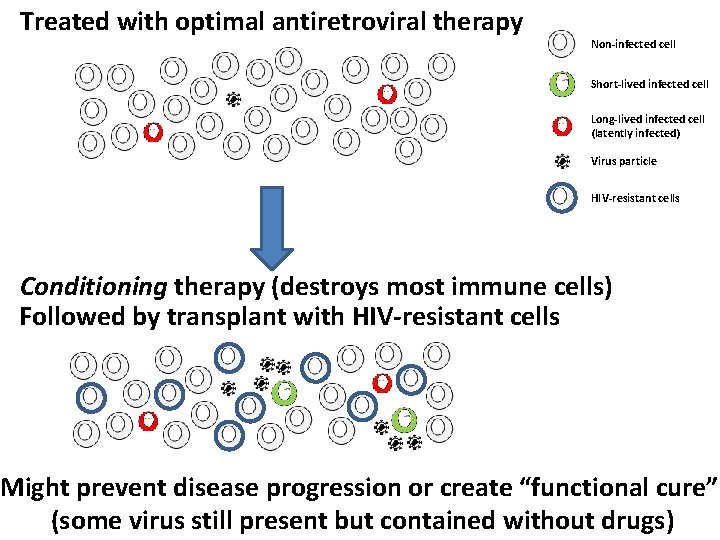
Treated with optimal antiretroviral therapy Non-infected cell Short-lived infected cell Long-lived infected cell (latently infected) Virus particle HIV-resistant cells Conditioning therapy (destroys most immune cells) Followed by transplant with HIV-resistant cells Might prevent disease progression or create “functional cure” (some virus still present but contained without drugs)
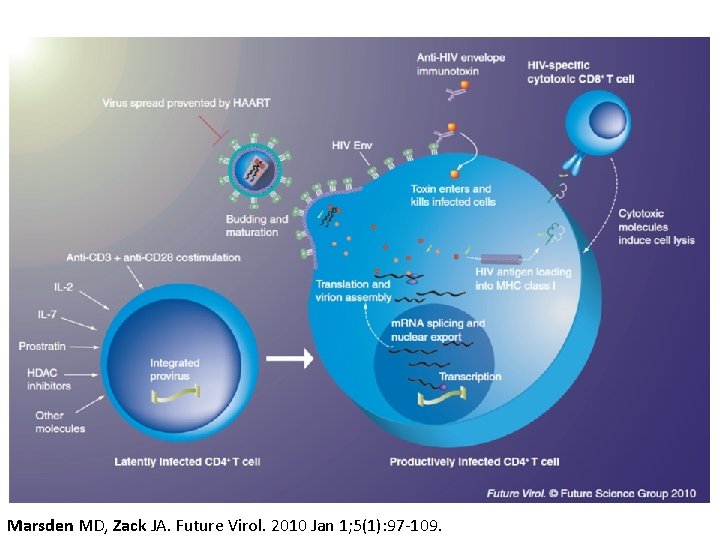
Experimental activation-elimination approaches to deplete latent HIV “Kick and Kill”
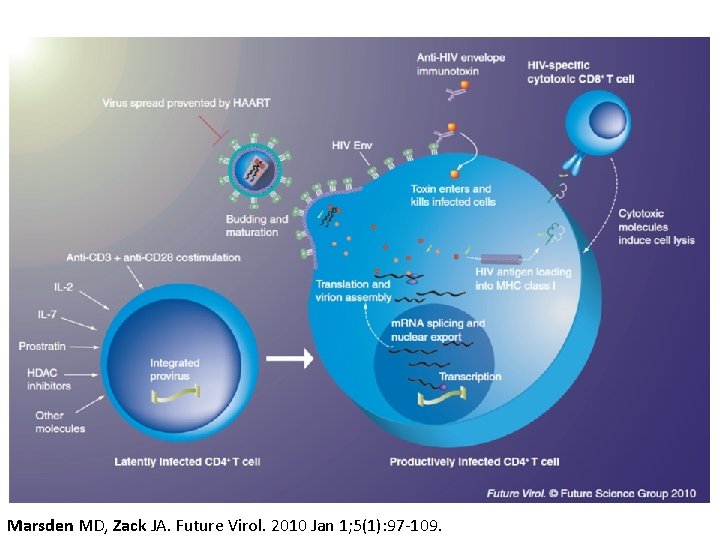
Marsden MD, Zack JA. Future Virol. 2010 Jan 1; 5(1): 97 -109.
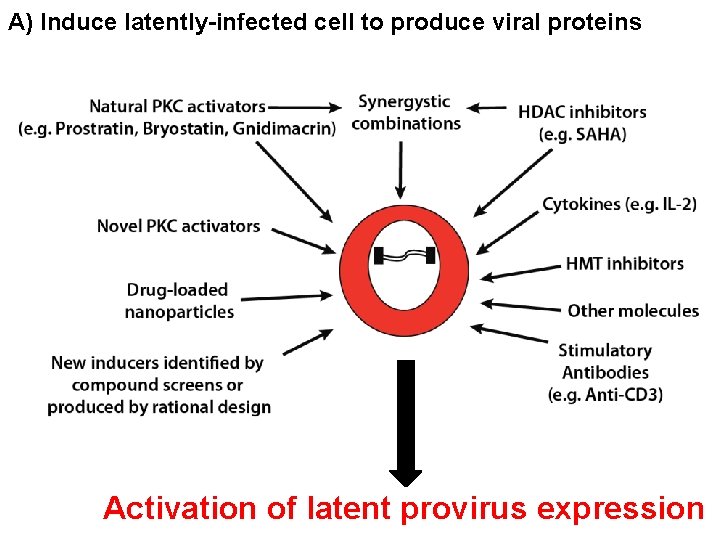
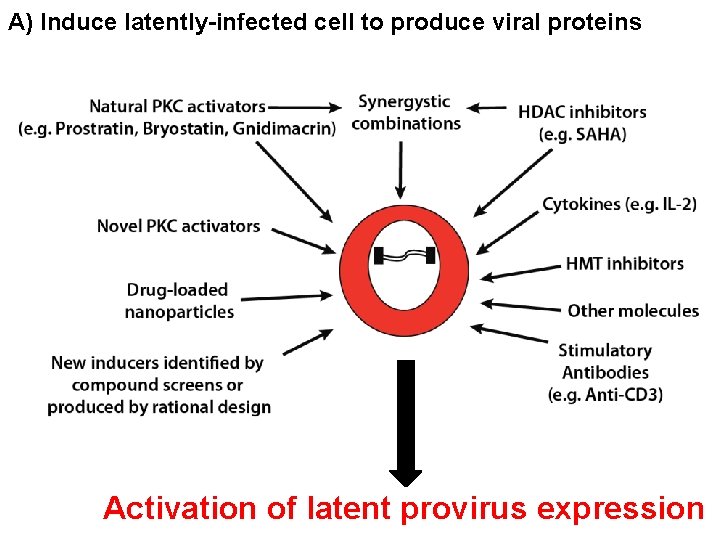
A) Induce latently-infected cell to produce viral proteins Activation of latent provirus expression
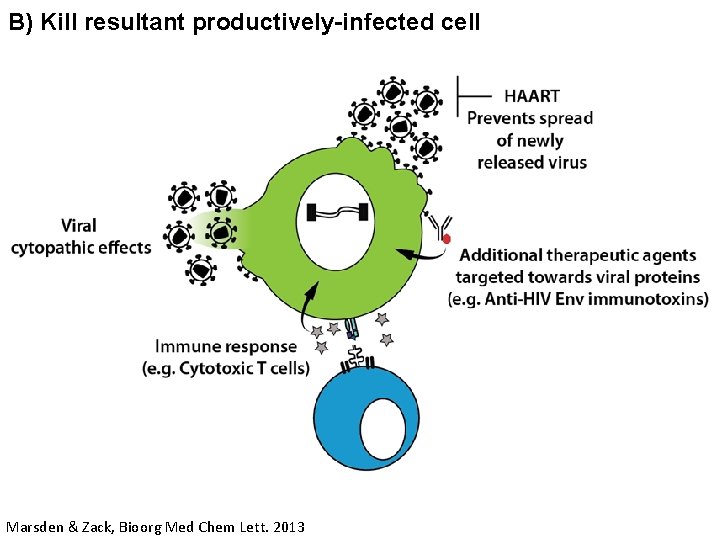
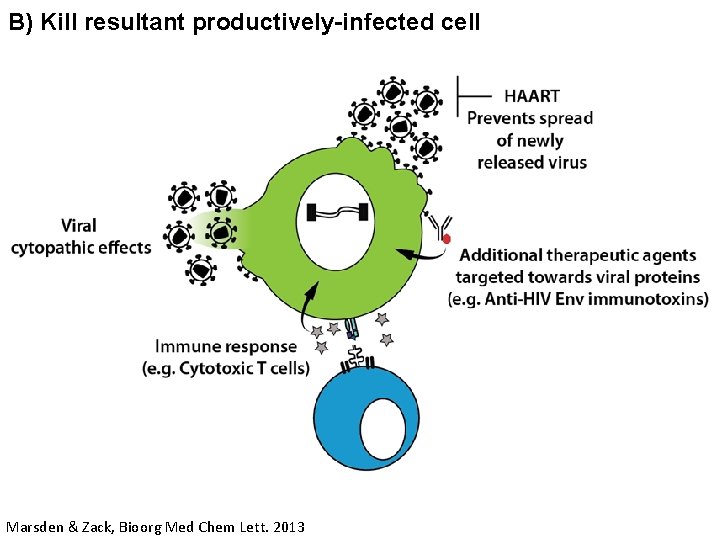
B) Kill resultant productively-infected cell Marsden & Zack, Bioorg Med Chem Lett. 2013
Headlines often don’t tell the full story! http: //boing. net/2009/08/30/how-science-reportin. html

Take-home points: • HIV cure research is a major focus of the scientific community and governmental funding agencies. • It is hard to definitively prove that a person is cured of HIV because virus may emerge from rare infected cells many years after stopping therapy. • However, there is a single case in which HIV might have been cured (Berlin Patient). • The circumstances of this cure is highly unusual (ablative therapy, GVHD, and bone marrow transplant with resistant cells), and therefore cannot be directly applied to all infected people. • Important as proof of concept for HIV cure. • More studies are being performed to develop new cure approaches that can be more widely used.
Thank You! Questions?