HistoryTaking Physical Examination in Vascular Diseases Aim To

- Slides: 32
History-Taking & Physical Examination in Vascular Diseases
Aim – To reach for a Presumptive Diagnosis
How to take the History • Establish a rapport with patient introduce yourself. • Initiate by asking – what made him to seek medical advice. • Listen without interruption. • Wait for answers before asking another question.
Don’ts of history taking • • • Do not interrupt the patient. Do not use medical terminology. Do not ask irrelevent questions Do not ask leading questions. Do not be abrupt or impatient.
The Present Complains • Ask the patient to tell you what made him to seek medical advice. • Record the answer in patients words.
History of Presenting Complains • Details of the history of the main complaints. - when did it start - what was the first thing noticed - progress since then - ever had it before.
History of Presenting Complains • • S – Site O – Onset C – Character R – Radiation A – Association T – Timing/Duration E – Exacerbating & alleviating factors S - Severity
Direct Questioning • Specific questions about the diagnosis you have in mind. - Risk factors. - Review of relevant system.
• • • Past Medical History Drug History Family History Social History Habits
• Vascular Diseases - Arterial - Venous - Lymphatic
Arterial Diseases • Electively – Chronic Symptoms • Acutely – Limb threatening disorders • Pain Intermittent Claudication Rest pain • Tissue loss Ulcer Gangrene
• Acute arterial occlusion Sudden onset Severe, Shocking pain Diffuse Associated Symptoms
• Chronic Arterial Insuffciency: Intermittent Claudication Site – depends on the level & extent of arterial disease - Cramp like pain - Consistantly reproduced by same level of exercise - Completely & quickly relieved by rest - Claudication distance
• Rest Pain - continuous severe pain, aching in nature - occurs in distal part of foot - often relieved by putting the leg below the level of heart - movement or pressure causes exacerbn.
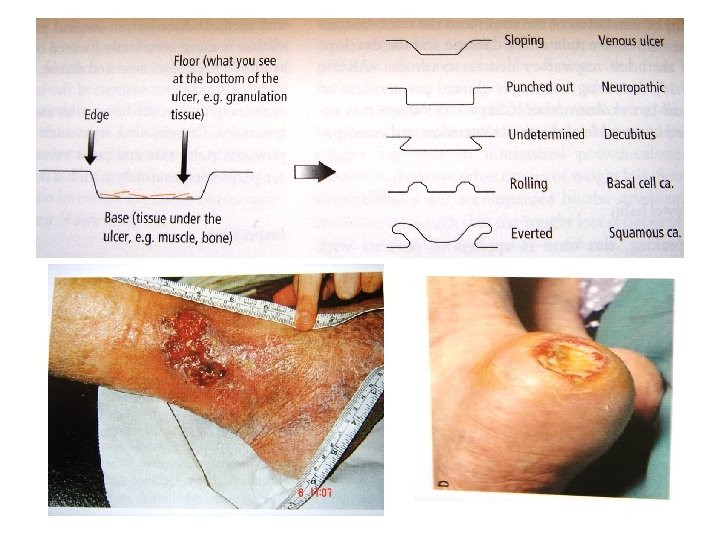
• Ulcer – area of discontinuity of surface epithelium • Gangrene – Dead tissue - Duration, Site. - what drew the patient’s attention to the ulcer - other symptoms - progression - persistance - multiplicity
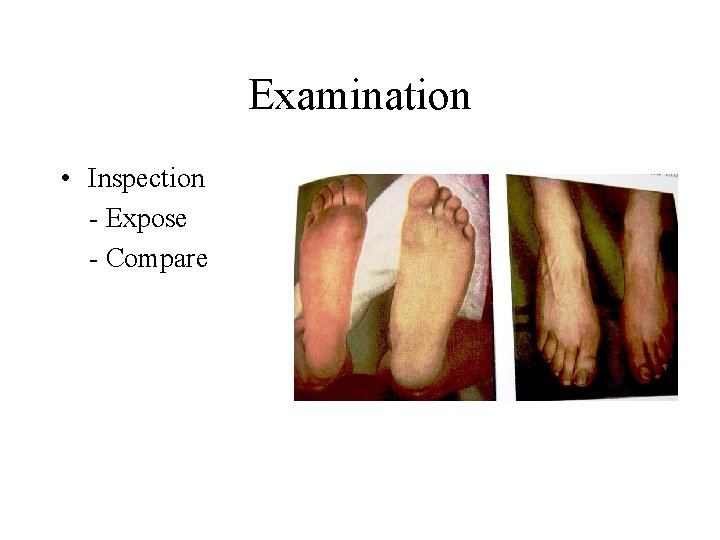
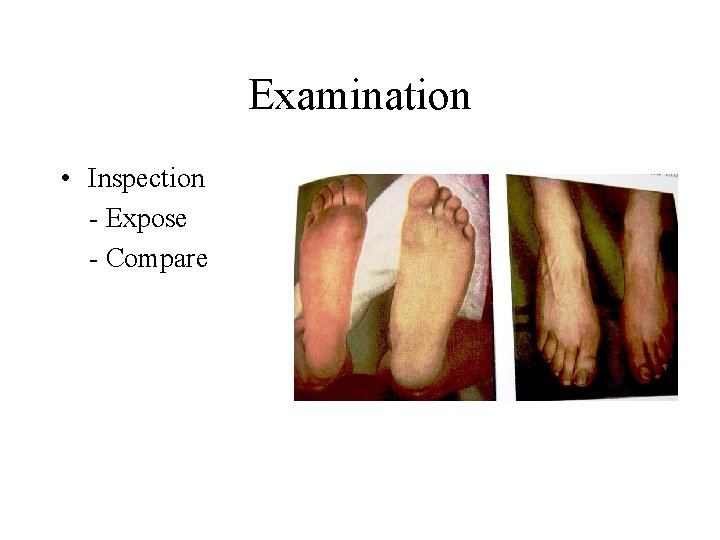
Examination • Inspection - Expose - Compare

• Look For
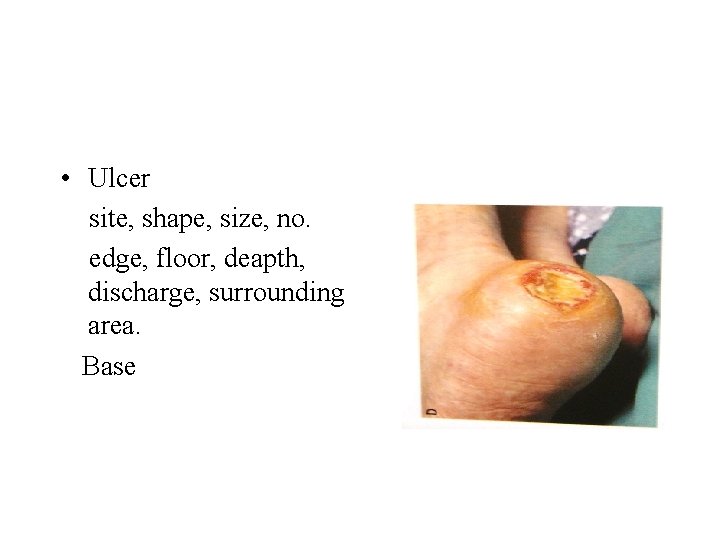
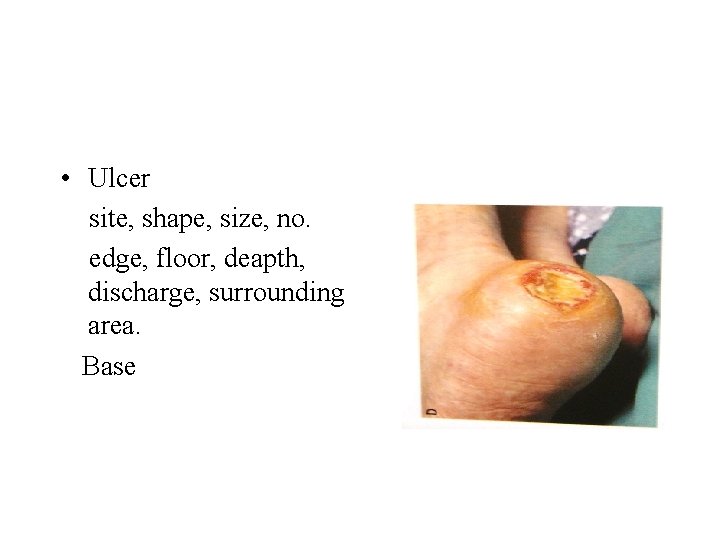
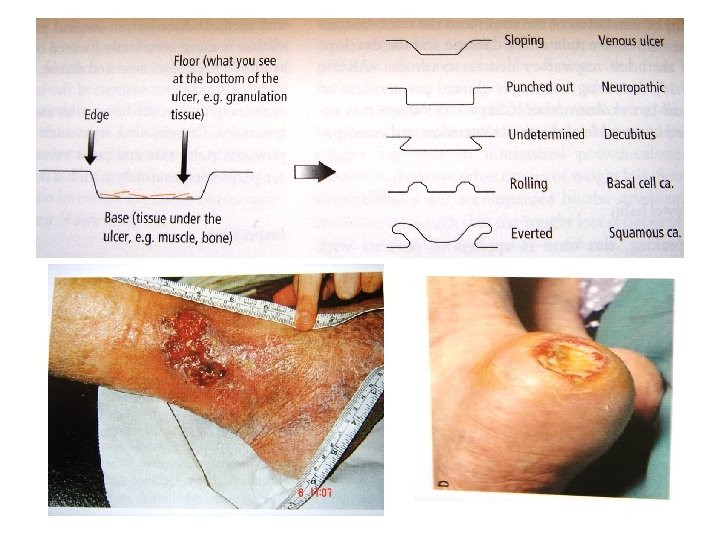
• Ulcer site, shape, size, no. edge, floor, deapth, discharge, surrounding area. Base
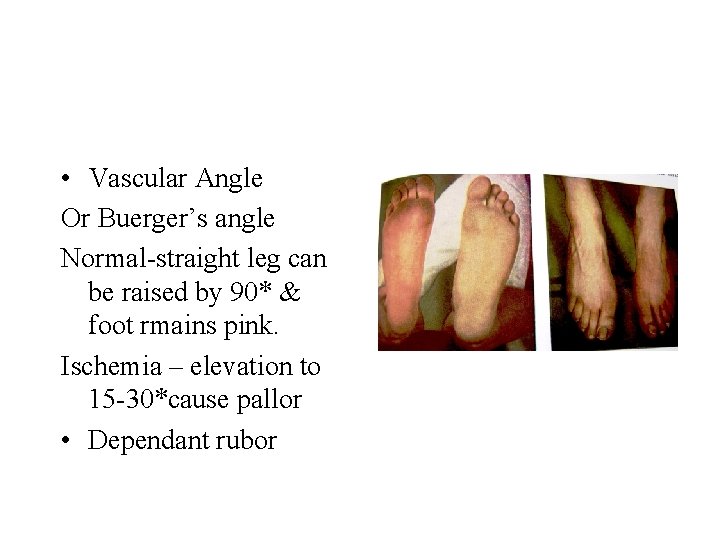
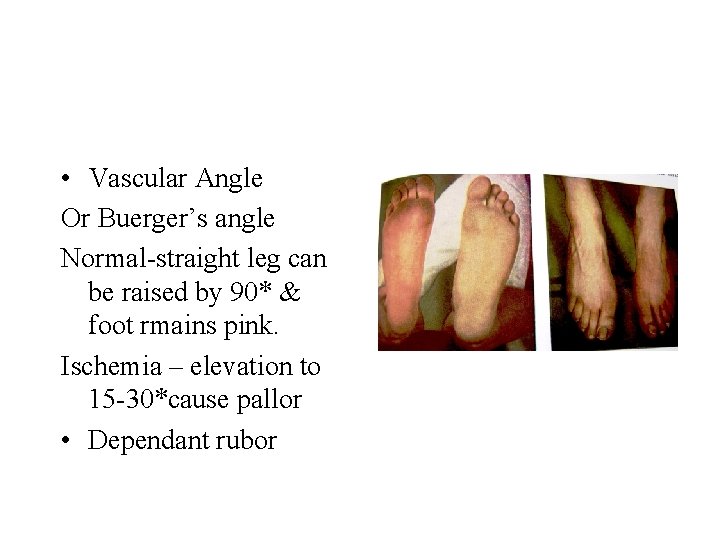
• Vascular Angle Or Buerger’s angle Normal-straight leg can be raised by 90* & foot rmains pink. Ischemia – elevation to 15 -30*cause pallor • Dependant rubor
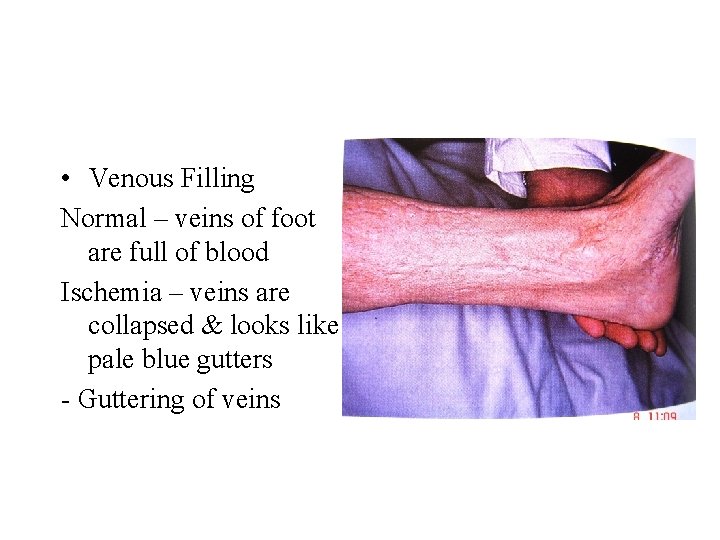
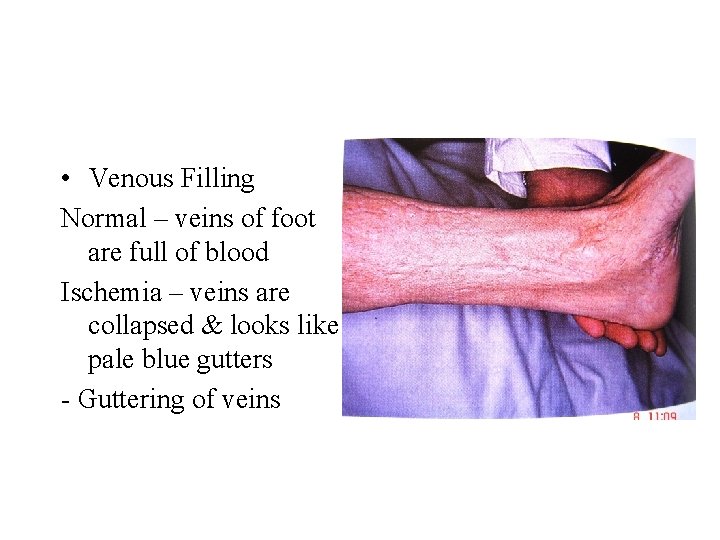
• Venous Filling Normal – veins of foot are full of blood Ischemia – veins are collapsed & looks like pale blue gutters - Guttering of veins
Palpation • Temperature which foot – warm/cold. level at which change occurs • Tenderness • Capillary filling
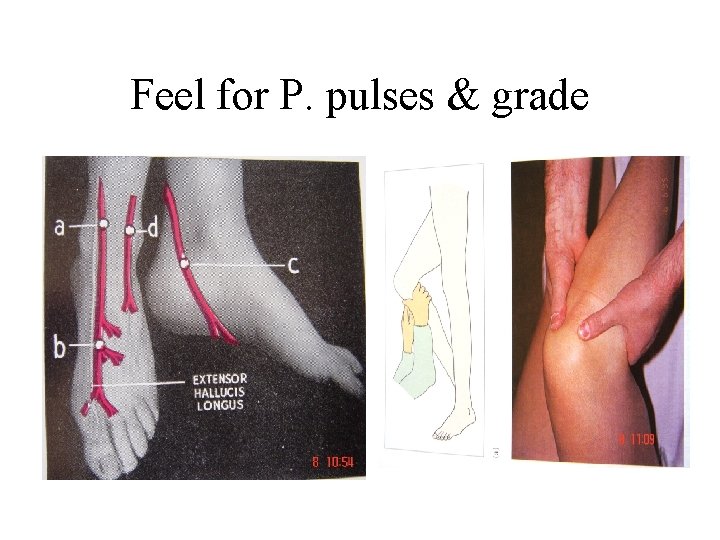
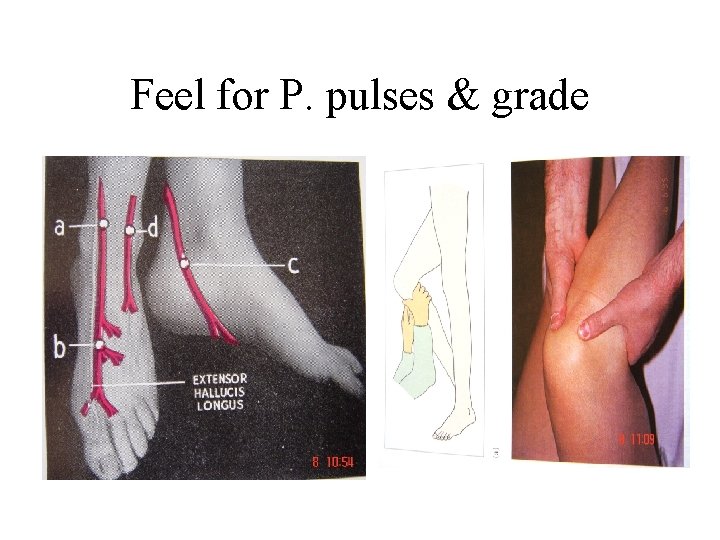
Feel for P. pulses & grade
• Peripheral Nerves Examination - Sensory - Motor • Auscultation - Bruit
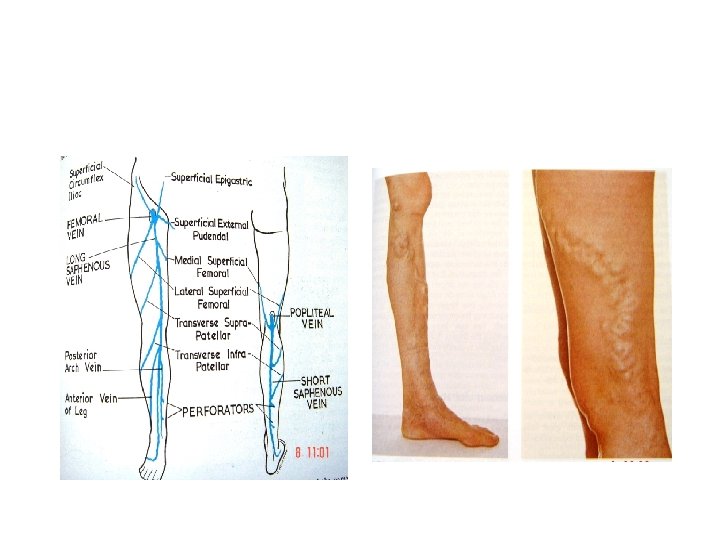
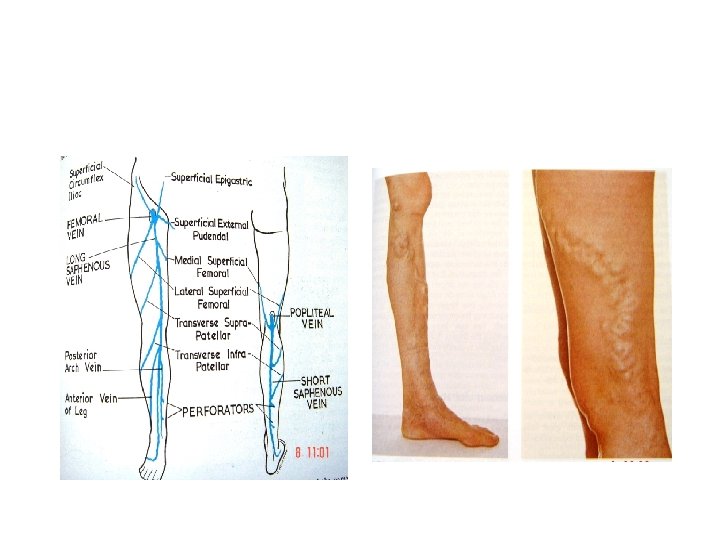
Venous diseases • Common Presentation - Varicose veins Asyptomatic, Cosmetic, Dull aching pains, Feeling of heaviness, Itching/Eczema, superficial thrombophlebitis, bleeding, Ulceration, Saphenavarix.
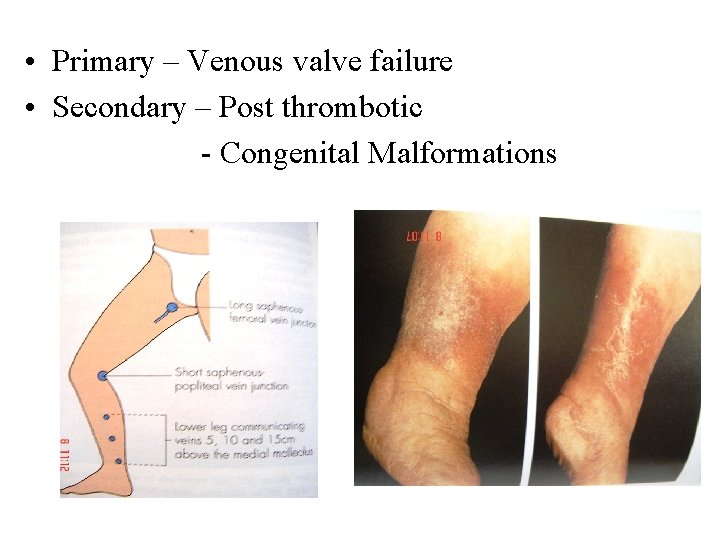
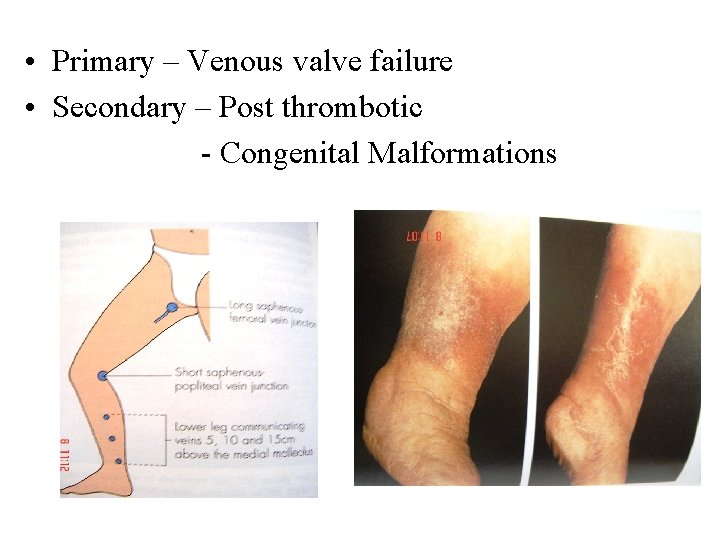
• Primary – Venous valve failure • Secondary – Post thrombotic - Congenital Malformations
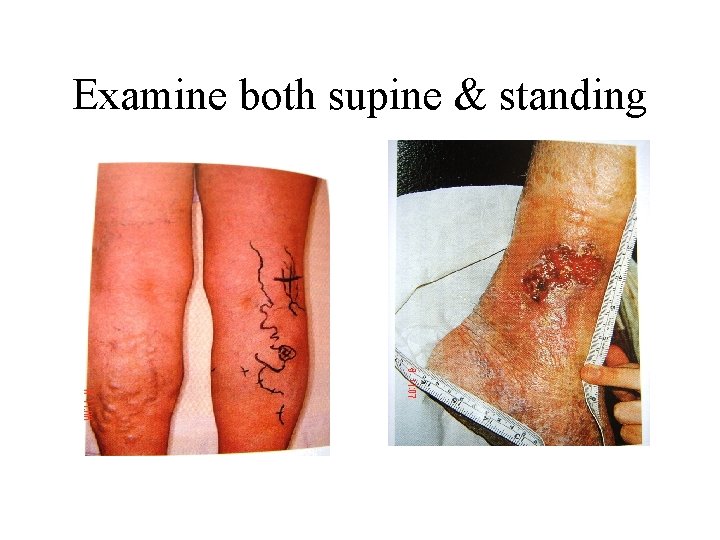
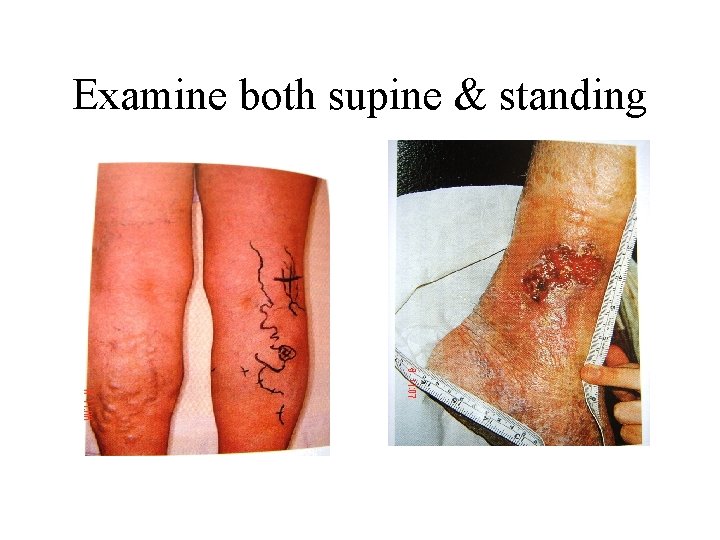
Examine both supine & standing
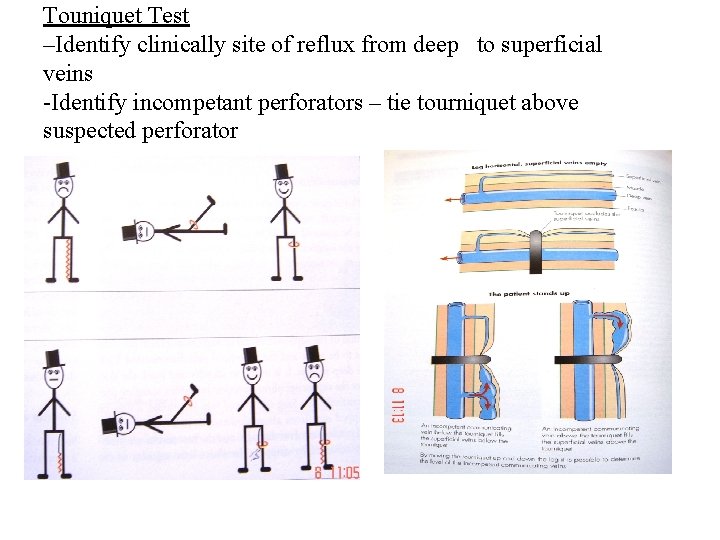
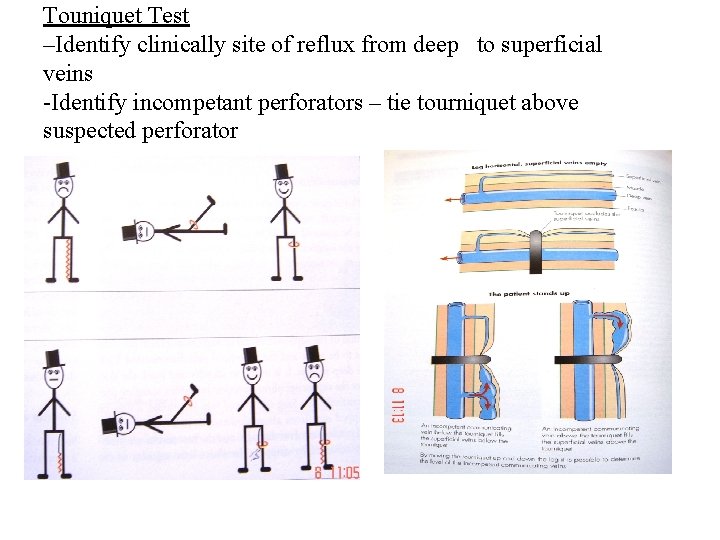
Touniquet Test –Identify clinically site of reflux from deep to superficial veins -Identify incompetant perforators – tie tourniquet above suspected perforator
Lymphatic diseases • Lymphangitis – inflamation of lymphatics. • Lymphedema – faiure of lymph drainage. Protein rich fluid accumulates in tissue
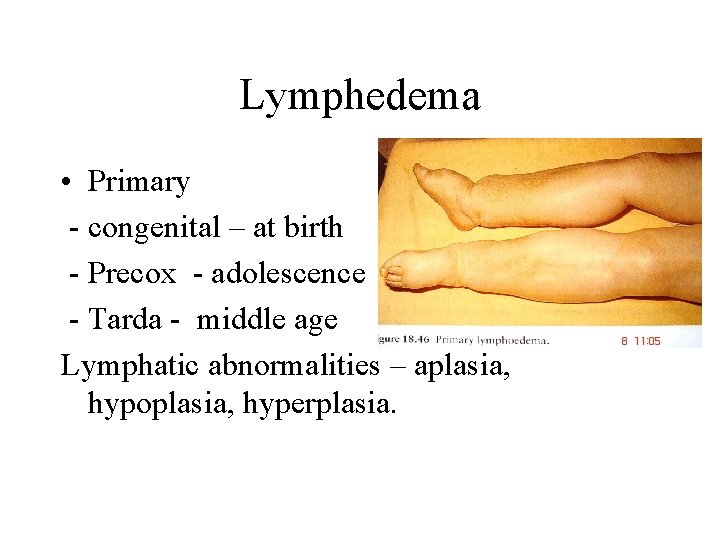
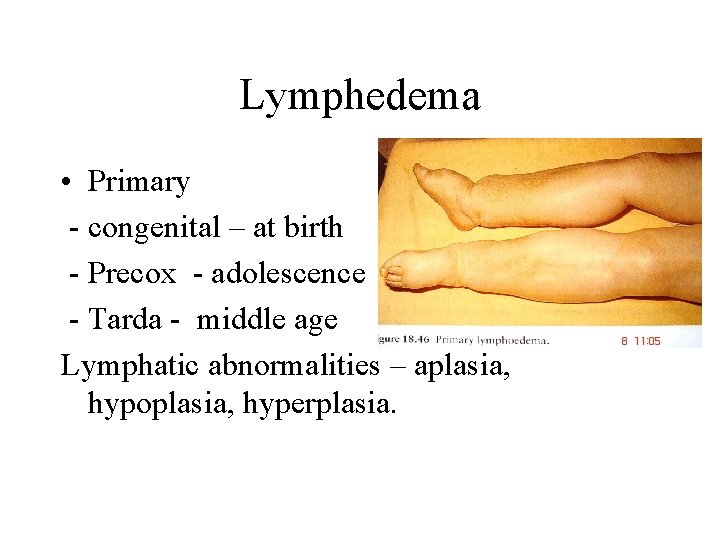
Lymphedema • Primary - congenital – at birth - Precox - adolescence - Tarda - middle age Lymphatic abnormalities – aplasia, hypoplasia, hyperplasia.
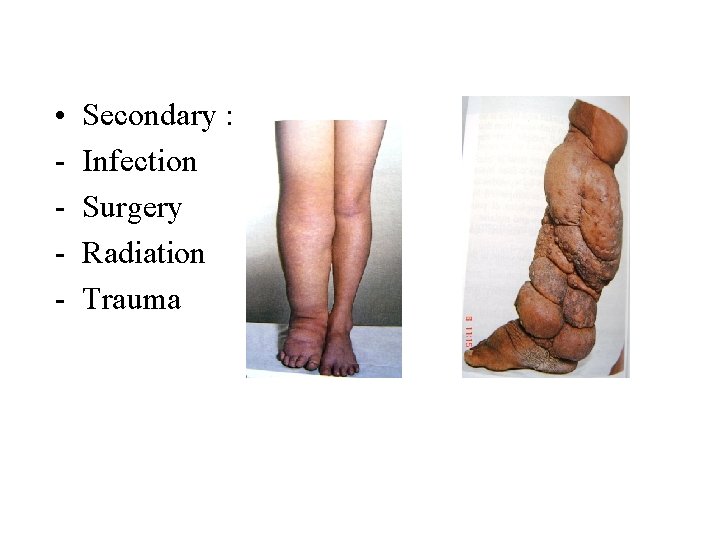
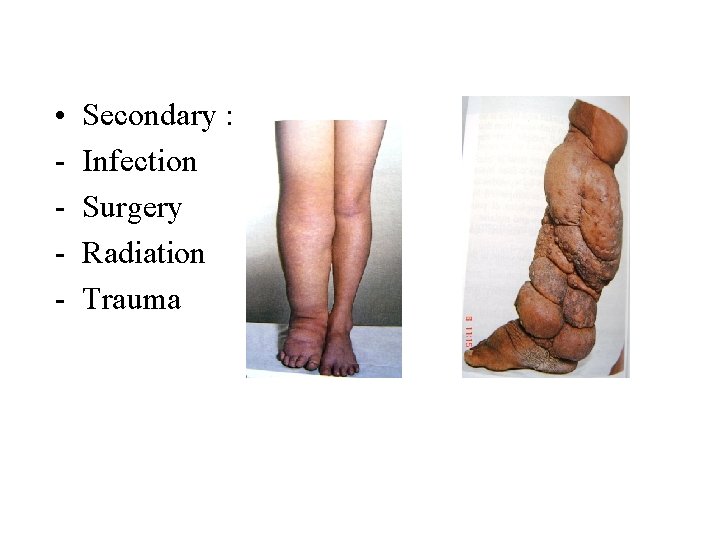
• - Secondary : Infection Surgery Radiation Trauma