History and Physical Examination of Older Adults Elizabeth
History and Physical Examination of Older Adults Elizabeth Galik, Ph. D, CRNP
Objectives • At the completion of this seminar, the student will: 1. Discuss strategies to overcome challenges to conducting a comprehensive health history and physical exam of an older adult. 2. Recommend appropriate health screening and immunizations for older adults.

Domains of a Comprehensive Assessment of Older Adults • • Physical Socio-economic Psychological Function (central focus) • Domains interact in complex ways to influence health • Importance of interdisciplinary team
Challenges to the Comprehensive Assessment of Older Adults • Sensory impairment (hearing, vision, etc. ) • Restricted mobility • Slowed response time/communication difficulties (aphasia) • Cognitive impairment • Tendency to underreport or minimize symptoms • Lengthy medical histories • Present with disease in an atypical fashion
Challenges (continued) • Chief complaints may be multiple, overlapping, vague, non-specific • Older adults typically manifest disease with functional decline (stop eating, stay in bed, become confused, fall, etc. )
Atypical presentation of illness in older adults 1. Vague presentation of illness 2. Altered presentation of illness 3. Under-reporting of illness Ham, Sloane, & Warshaw (2002)
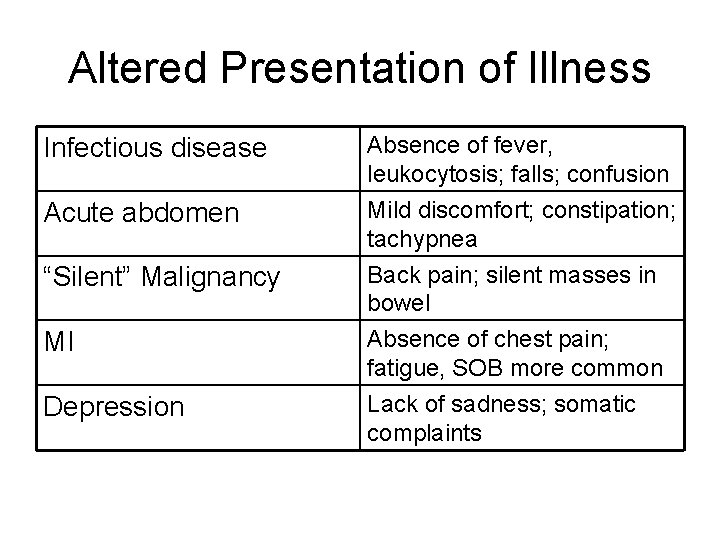
Altered Presentation of Illness Infectious disease Absence of fever, leukocytosis; falls; confusion Acute abdomen Mild discomfort; constipation; tachypnea Back pain; silent masses in bowel “Silent” Malignancy MI Depression Absence of chest pain; fatigue, SOB more common Lack of sadness; somatic complaints
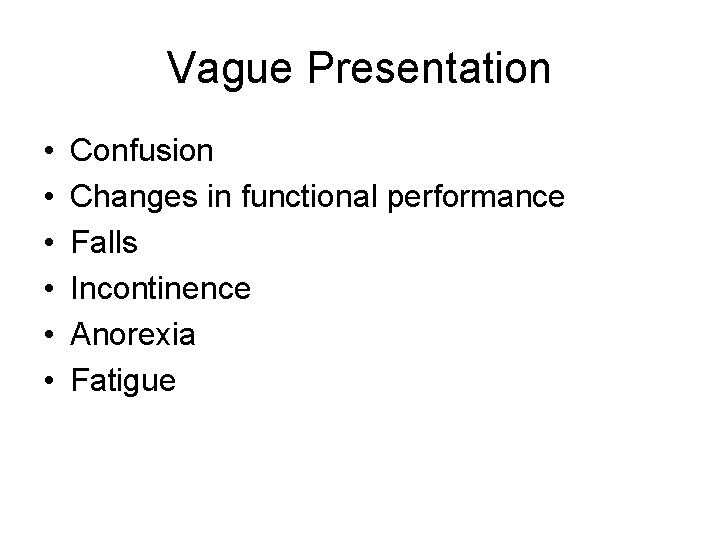
Vague Presentation • • • Confusion Changes in functional performance Falls Incontinence Anorexia Fatigue
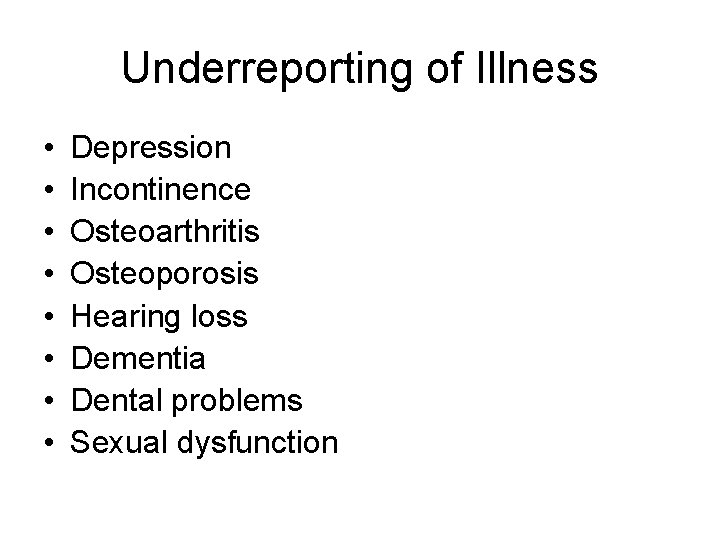
Underreporting of Illness • • Depression Incontinence Osteoarthritis Osteoporosis Hearing loss Dementia Dental problems Sexual dysfunction
Factors that contribute to underreporting • Insidious onset and vague symptoms • Viewed as “normal aging” by patients and families • Concerned about being ignored or generating burdensome diagnostic testing • Communication deficits (hearing, vision, speech)
Strategies • Schedule more than one session for the initial patient history • Bring medications and supplements in a brown bag • Get collateral history from family/caregiver • Attempt to minimize the impact of sensory deficits (adequate lighting, minimize ambient noise)
Strategies • Structure the interview to overcome patient disability (ex. Yes or no questions for an aphasic patient, attention to non-verbal cues) • BE OBSERVANT!!! Integrate functional assessment into the exam
Social History • Home/living arrangements • Relationship with family & friends • Expectations of family/caregivers • Economic status • Ability to perform ADLs • Social activities/hobbies/past occupation • Spiritual/religious • Transportation • Advanced Directives
Past Medical History • • Previous surgical procedures Major illnesses and hospitalizations Previous transfusions TB history and testing • Immunizations status – – Influenza Pneumococcal Tetanus Herpes zoster (shingles)
Past Medical History (continued) • Preventive Health Measures – Mammography (Q 2 years age 50 -75, then stop at 75 (USPSTF) or 85 (AGS) – Fecal occult blood (Q year) – Pap smear USPSTF, AGS, ACS no screening >65 if all negative tests in past and no risk factors for cervical ca. No prior pap, 2 negative tests – Flexible sigmoidoscopy (Q 5 yrs) – Colonoscopy (Q 10 years, from age 50 -75)
Preventive Health Measures (cont) • Bone mass measurement Q 2 years • DRE & PSA (ACS: consider for men over 50 based on risks and life expectancy; USPSTF against screening • DM screening (2 times a year with risk factors) • Physical examination (Welcome to Medicare) within first 6 months of getting Medicare Part B
Past Medical History (continued) • • • Medications (brown bag) Previous allergies/intolerances Knowledge of current medication regimen Adherence Perceived beneficial or adverse drug effects
Review of Systems: System and Key Symptoms for Older Adults • Skin – New lesion, rash • HEENT – Change in hearing or vision, difficulty chewing • Respiratory – Dyspnea, persistent cough • Cardiovascular – Orthopnea, edema, angina, claudication palpitations, dizziness, syncope
Review of Systems • Gastrointestinal – Dysphagia, abdominal pain, change in bowel habit • Genitourinary – Frequency, urgency, nocturia, hesitancy, intermittent stream, incontinence, hematuria, vaginal bleeding • Musculoskeletal – Focal or diffuse pain and/or weakness • Neurological – Unsteadiness, falls, weakness, bradykinesia, tremor, gait changes • Psychological – Depression, anxiety, paranoia, forgetfulness, confusion
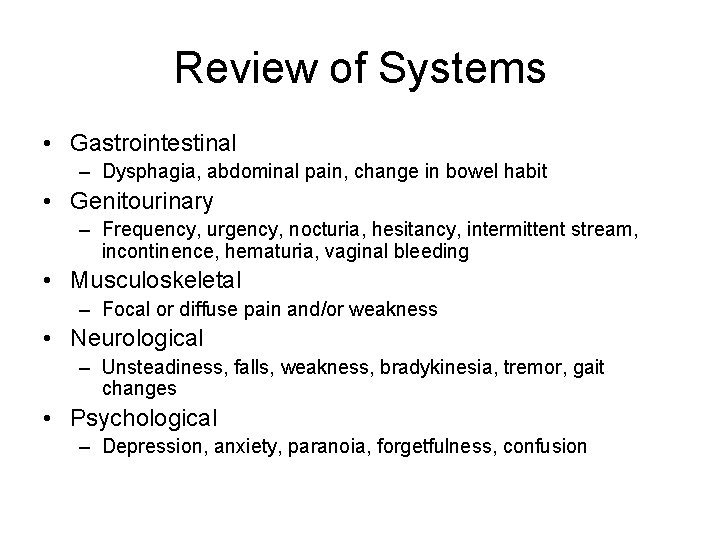
Physical Exam: Skin • • Thin Less elasticity Decreased skin turgor Dry skin (fewer sweat glands) • Less vasculature • Less subcutaneous fat
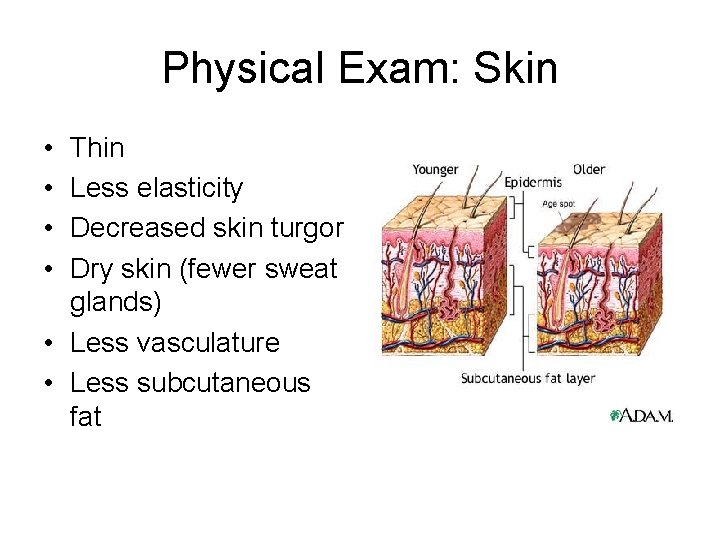
Seborrheic Keratoses
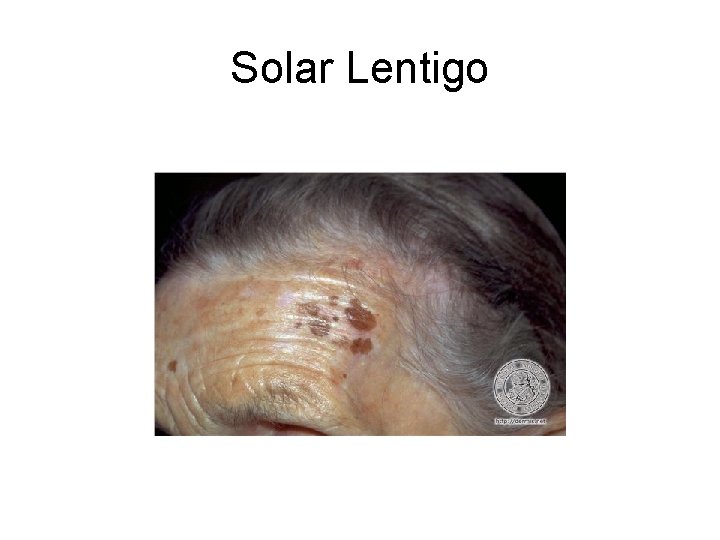
Solar Lentigo
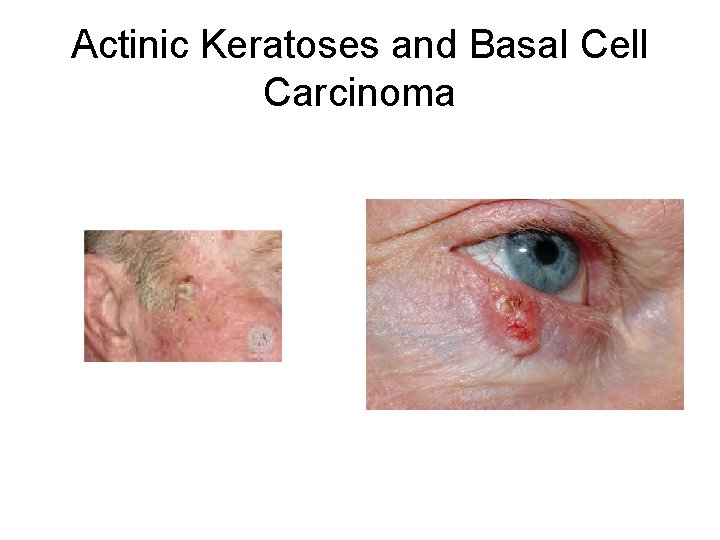
Actinic Keratoses and Basal Cell Carcinoma
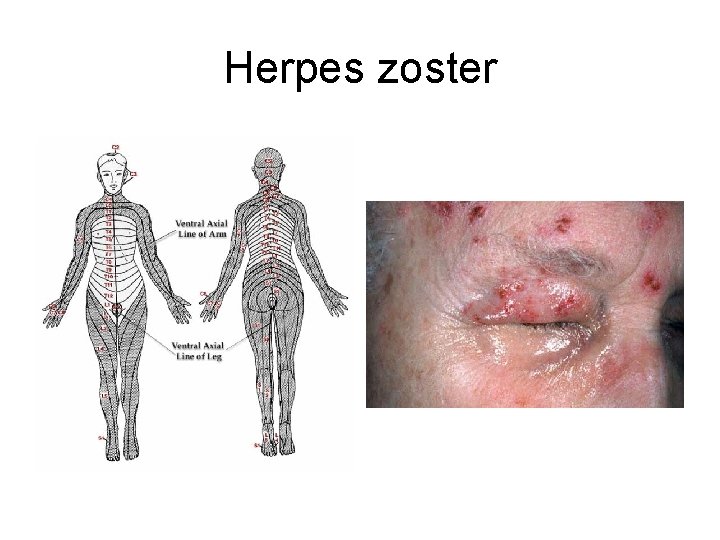
Herpes zoster
Physical Exam: Eyes • • Slower pupillary reflex (still symmetric) Decreased tearing Decreased adaptation to light Pupils may be irregularly shaped after iridectomy • Decreased visual acuity • Cataracts may make fundoscopic examination often difficult and limited
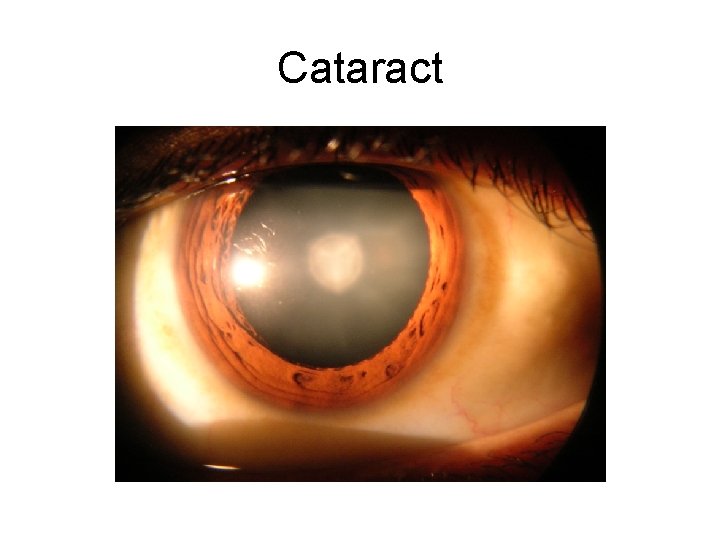
Cataract
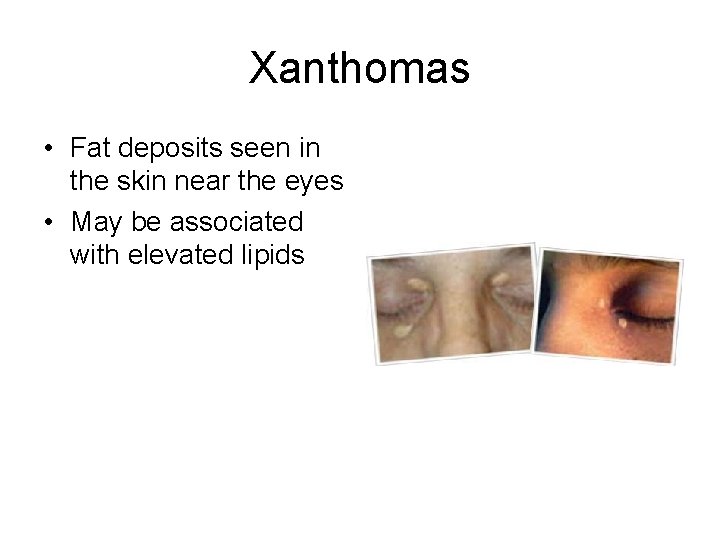
Xanthomas • Fat deposits seen in the skin near the eyes • May be associated with elevated lipids
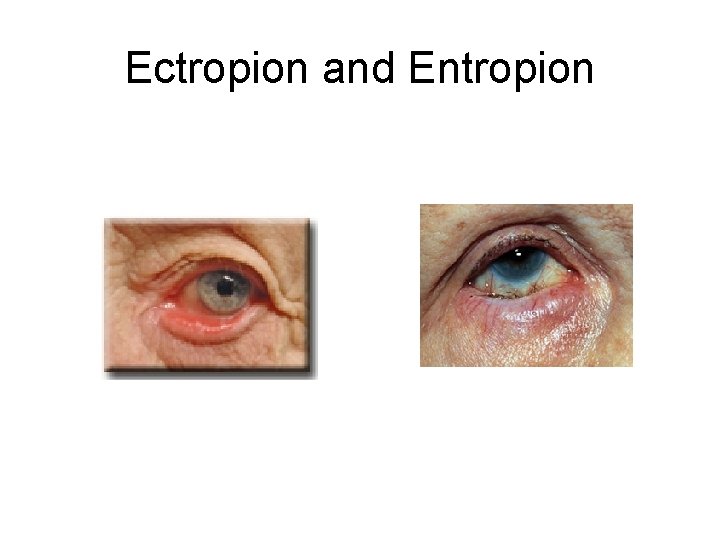
Ectropion and Entropion
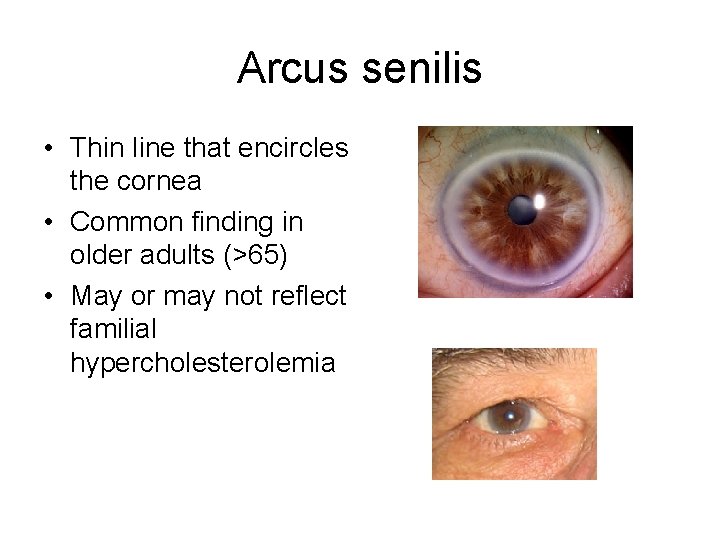
Arcus senilis • Thin line that encircles the cornea • Common finding in older adults (>65) • May or may not reflect familial hypercholesterolemia
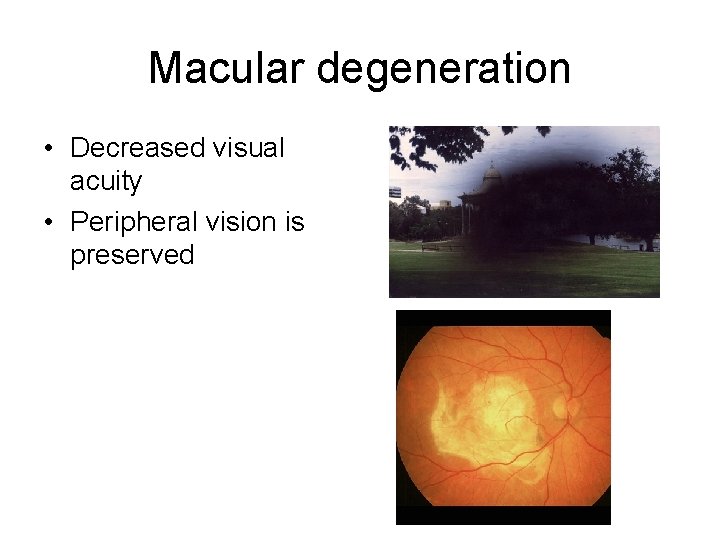
Macular degeneration • Decreased visual acuity • Peripheral vision is preserved
Physical Exam: Ears • Hearing Loss – Sensorineural Hearing loss (high frequency loss) – Conductive Hearing Loss (cerumen impaction) – Presbycusis
Physical Exam: Mouth • Tooth loss and periodontal disease are common • 50% of those 65 years and older are edentulous • Area under the tongue is a common site for early malignancies

Oral Cancer
Physical Exam: Lungs • Age Associated Changes – Decreased lung tissue elasticity – Atrophy of cilia – Decrease in respiratory strength • Associated Signs and Symptoms – In COPD: Lung fields may be hyperresonant – May have a difficult time with multiple “deep breaths” (Decreased FEV 1) – Decreased sound at bases
Respiratory • Crackles can be heard in the absence of pulmonary disease and heart failure; often indicates atelectasis
Physical Exam: Cardiovascular • Age Associated Changes – – Decreased beta-adrenergic stimulation Decreased cardiac output Calcification of valves Decreased baroreceptor response • Associated Signs and Symptoms – – – Reduced stroke volume and output Left ventricular hypertrophy Increased systolic BP Orthostatic hypotension Systolic ejection murmurs are common S 4 is commonly heard
Cardiovascular: Common abnormal findings • • Irregular rhythms Systolic murmurs Vascular bruits Diminished distal pulses
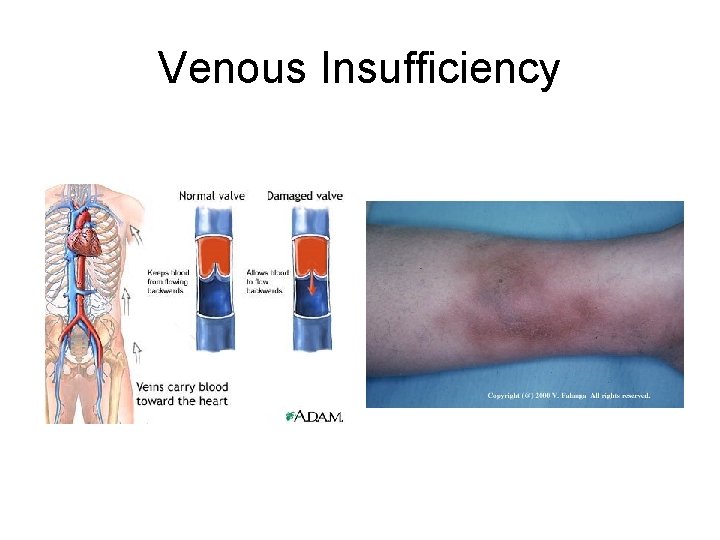
Venous Insufficiency
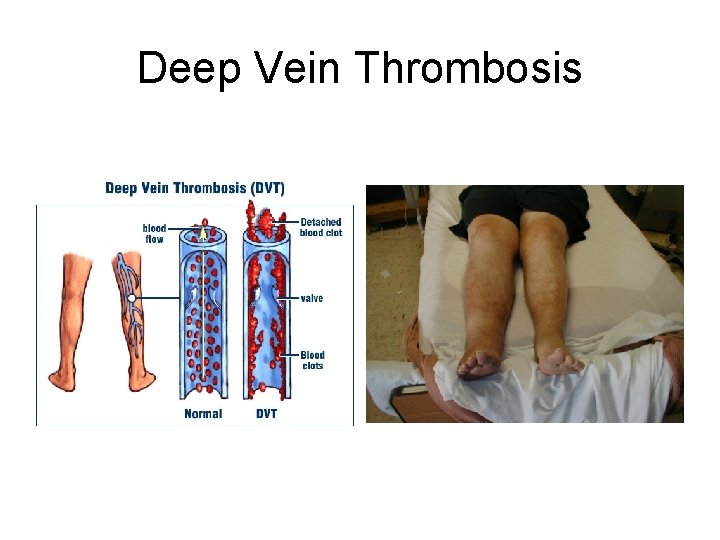
Deep Vein Thrombosis

Arterial and Venous ulcers
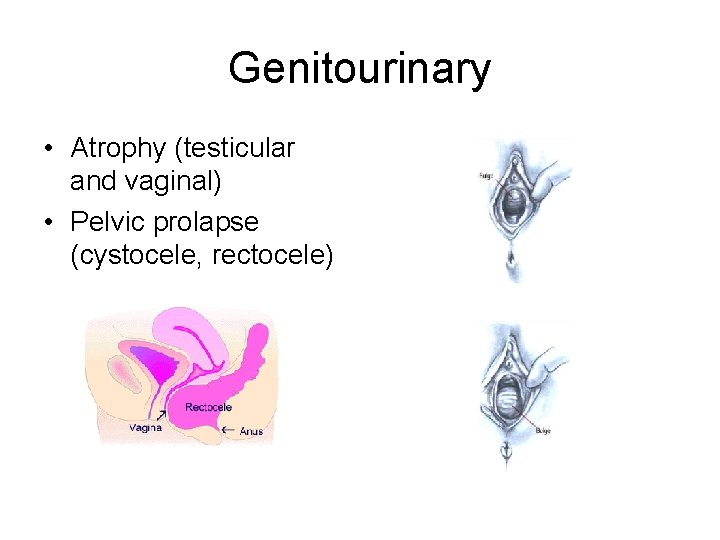
Genitourinary • Atrophy (testicular and vaginal) • Pelvic prolapse (cystocele, rectocele)
Neurologic and Mental Status • Weakness (arm drift may be the only sign of residual weakness from a stroke; check for proximal weakness ie difficulty getting out of a chair) • Tremor • Bradykinesia
Gait and Balance • Get Up and Go: Sit, rise from a chair, walk 8 feet and turn around, and sit back down • Check for speed, agility, balance
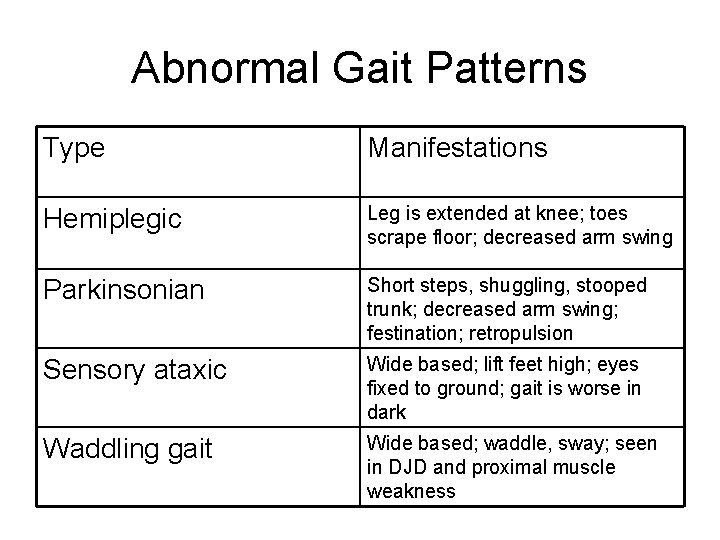
Abnormal Gait Patterns Type Manifestations Hemiplegic Leg is extended at knee; toes scrape floor; decreased arm swing Parkinsonian Short steps, shuggling, stooped trunk; decreased arm swing; festination; retropulsion Sensory ataxic Wide based; lift feet high; eyes fixed to ground; gait is worse in dark Waddling gait Wide based; waddle, sway; seen in DJD and proximal muscle weakness
Mental Status Exam • • • Appearance and grooming Speech and language Mood and affect Thought process Cognition
Why we work with older adults • Older adults are vulnerable to reversible problems that contribute to disability, so even small improvements in physical, mental, social, and/or functional status can have a significant positive impact on patients and their families/caregivers
- Slides: 46