Histology of the Female Reproductive System Reproductive function


- Slides: 57
Histology of the Female Reproductive System
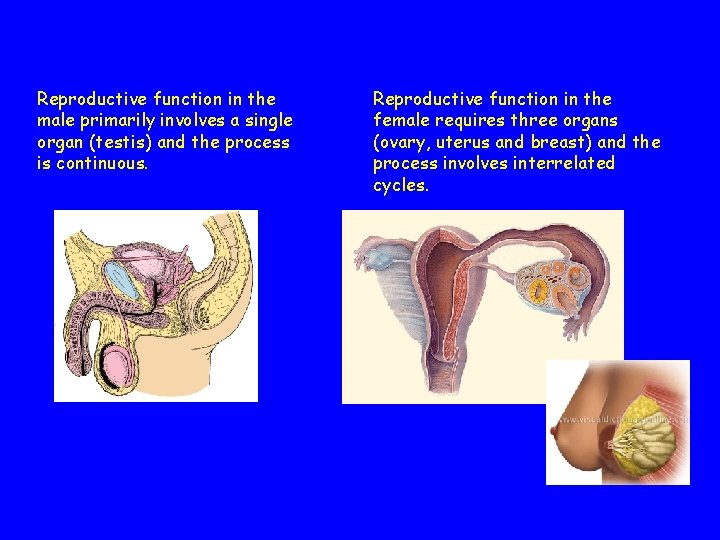
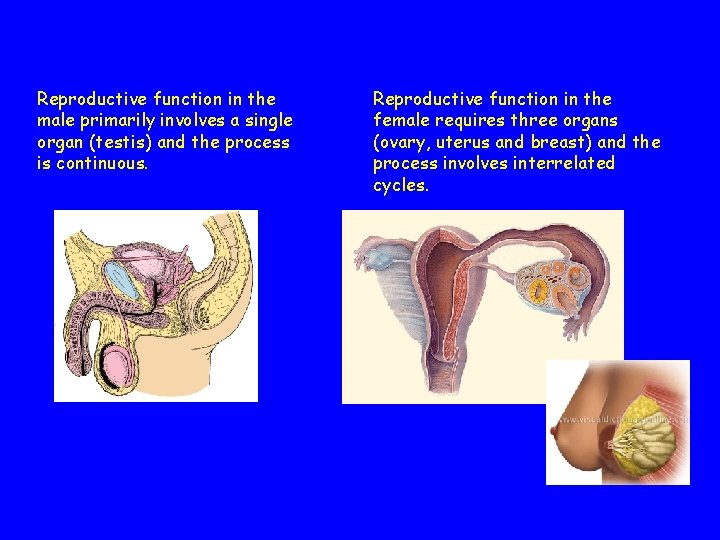
Reproductive function in the male primarily involves a single organ (testis) and the process is continuous. Reproductive function in the female requires three organs (ovary, uterus and breast) and the process involves interrelated cycles.
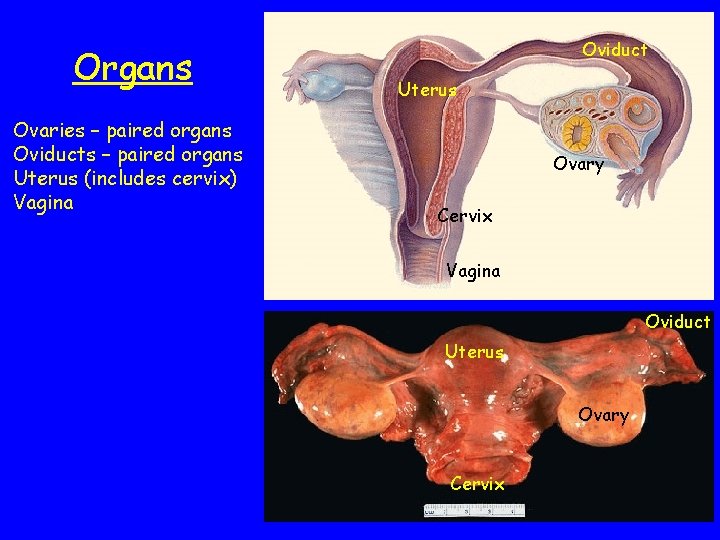
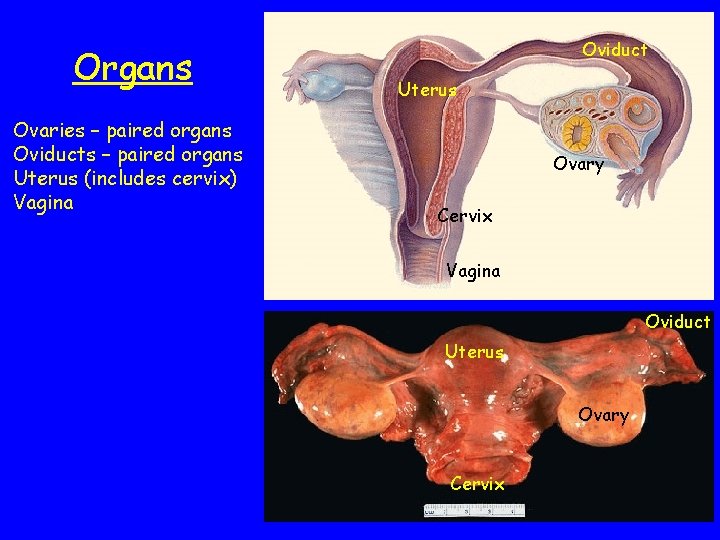
Organs Ovaries – paired organs Oviducts – paired organs Uterus (includes cervix) Vagina Oviduct Uterus Ovary Cervix
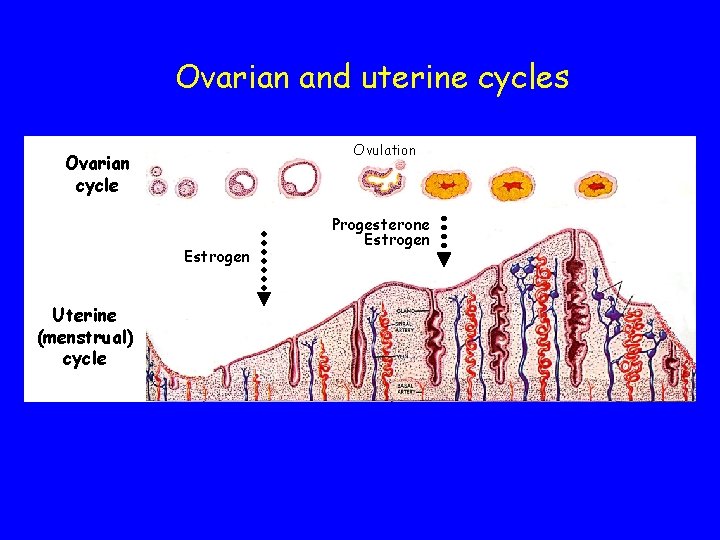
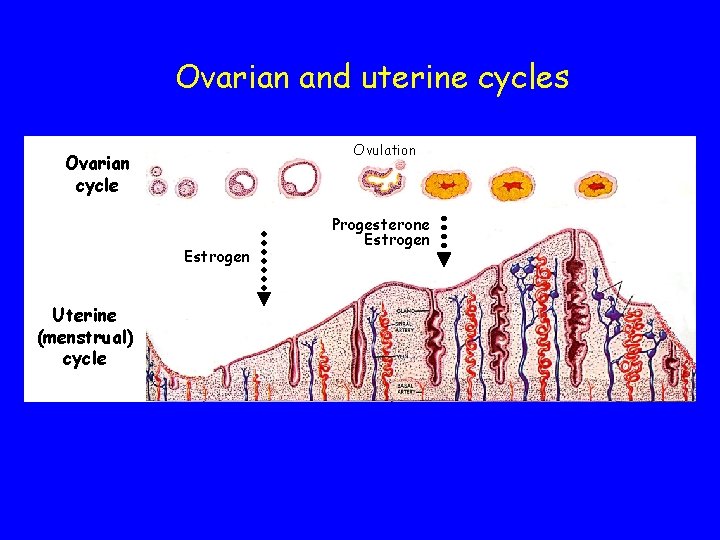
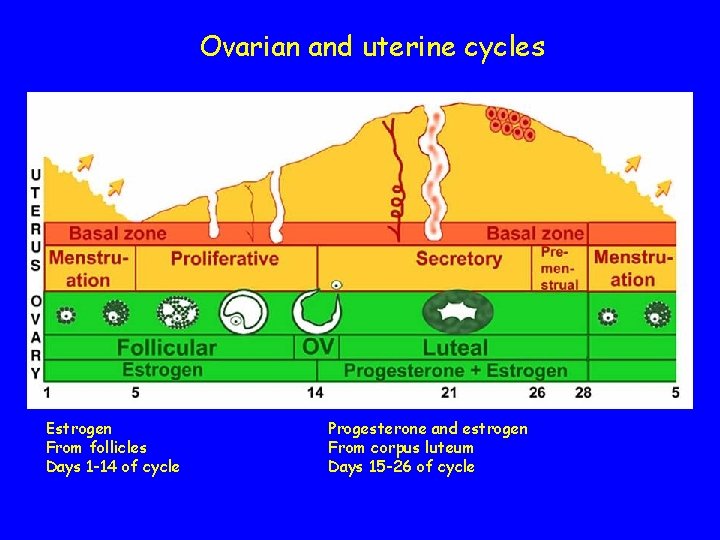
Ovarian and uterine cycles Ovulation Ovarian cycle Estrogen Uterine (menstrual) cycle Progesterone Estrogen

Ovarian and uterine cycles Ovarian cycle Estrogen Uterine (menstrual) cycle
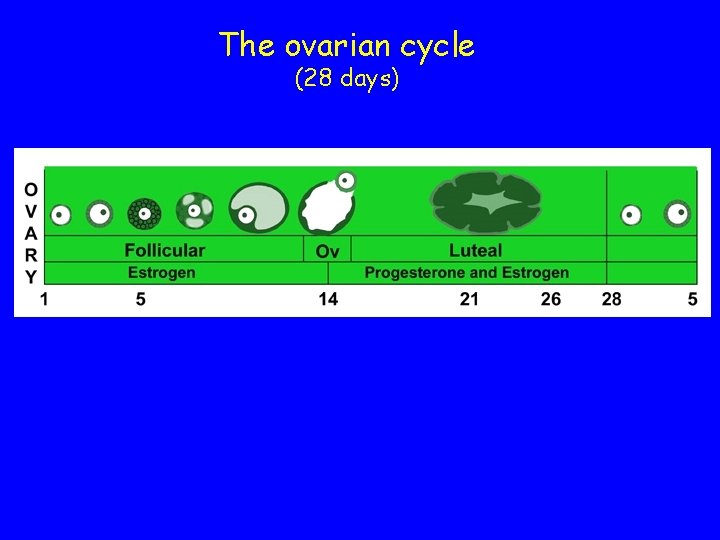
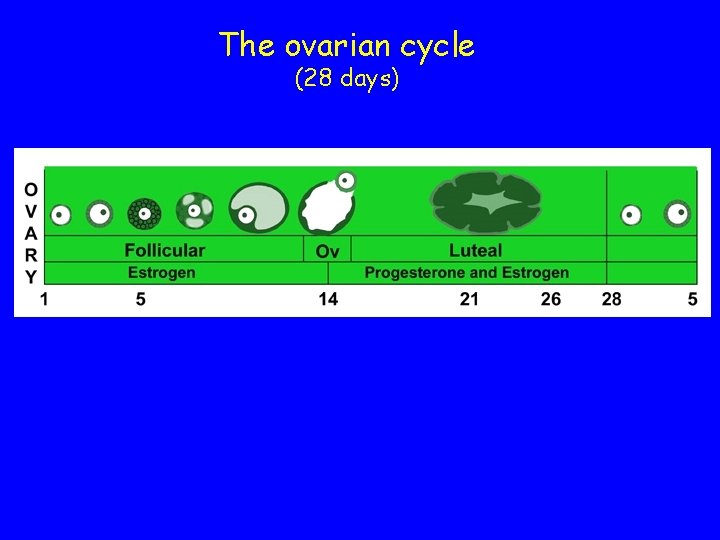
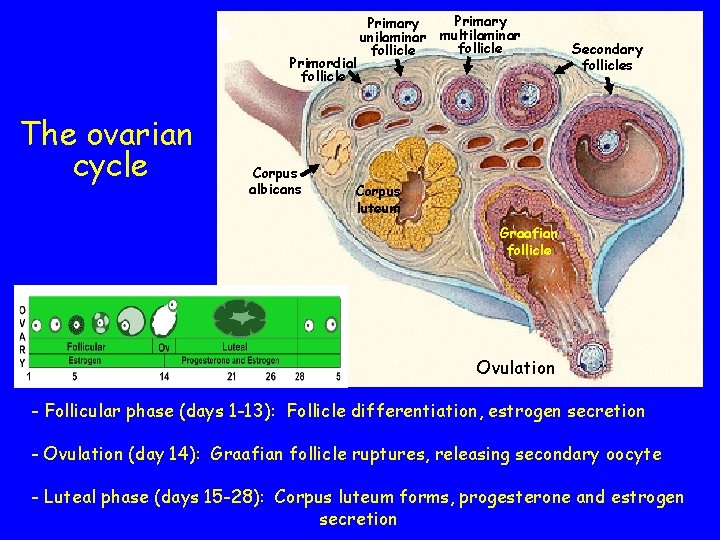
The ovarian cycle (28 days)
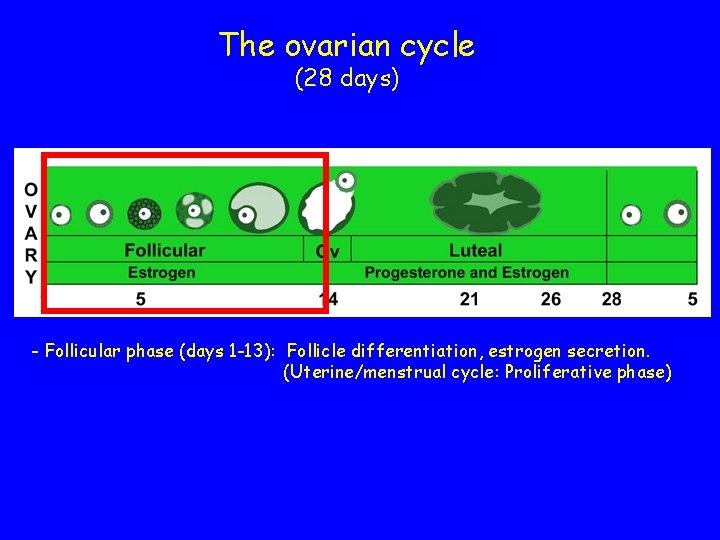
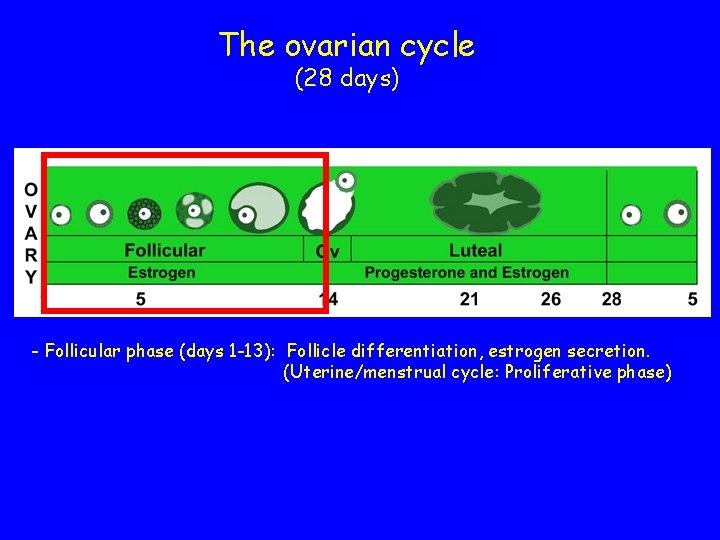
The ovarian cycle (28 days) - Follicular phase (days 1 -13): Follicle differentiation, estrogen secretion. (Uterine/menstrual cycle: Proliferative phase)
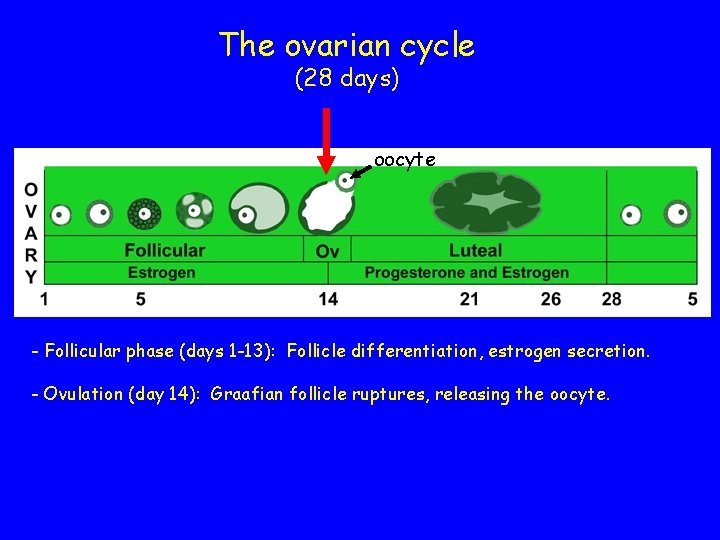
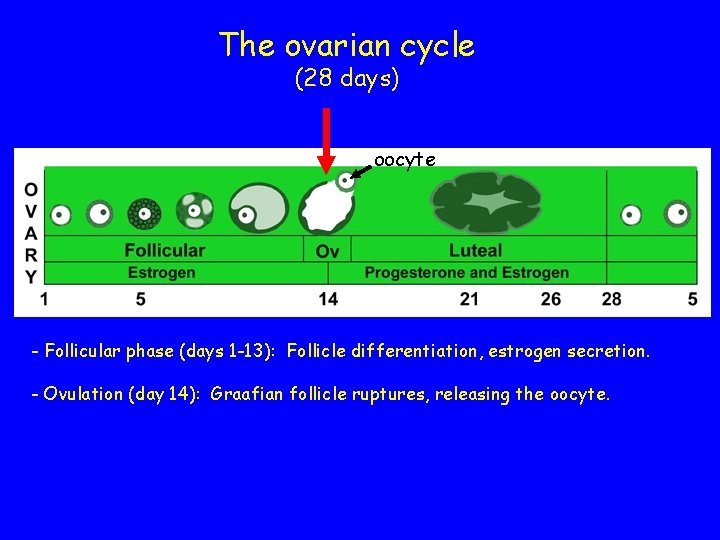
The ovarian cycle (28 days) oocyte - Follicular phase (days 1 -13): Follicle differentiation, estrogen secretion. - Ovulation (day 14): Graafian follicle ruptures, releasing the oocyte.
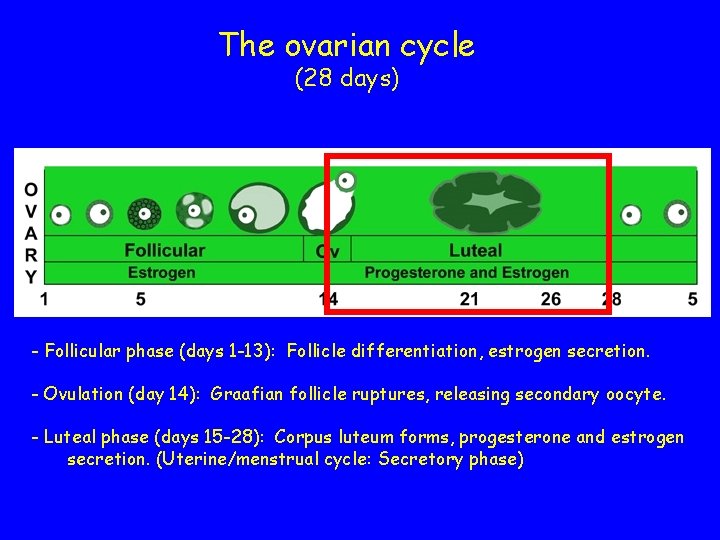
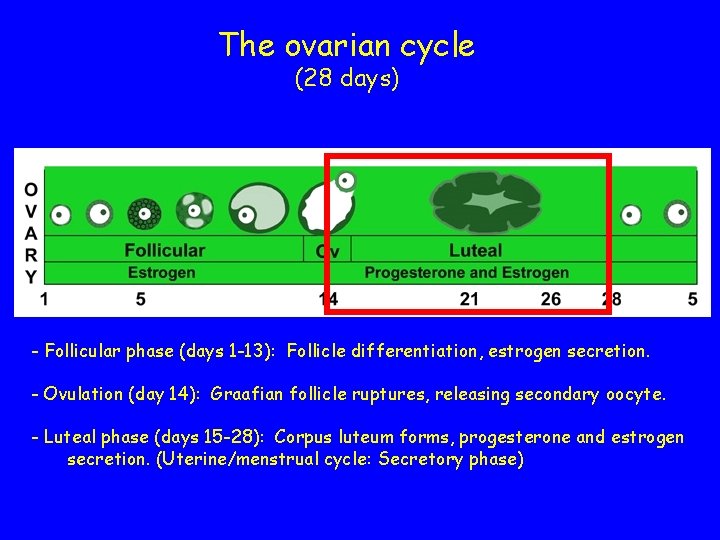
The ovarian cycle (28 days) - Follicular phase (days 1 -13): Follicle differentiation, estrogen secretion. - Ovulation (day 14): Graafian follicle ruptures, releasing secondary oocyte. - Luteal phase (days 15 -28): Corpus luteum forms, progesterone and estrogen secretion. (Uterine/menstrual cycle: Secretory phase)
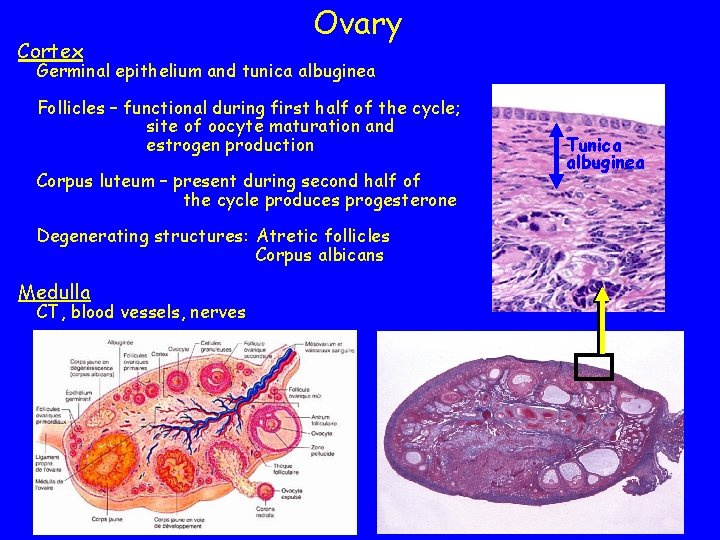
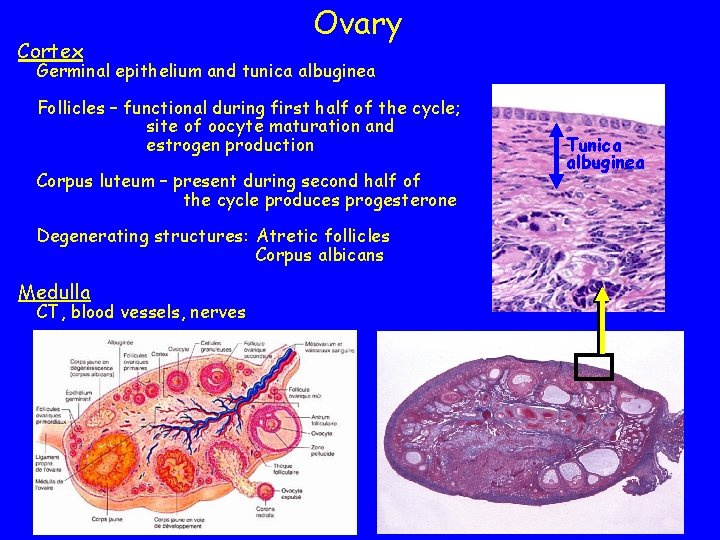
Cortex Ovary Germinal epithelium and tunica albuginea Follicles – functional during first half of the cycle; site of oocyte maturation and estrogen production Corpus luteum – present during second half of the cycle produces progesterone Degenerating structures: Atretic follicles Corpus albicans Medulla CT, blood vessels, nerves Tunica albuginea
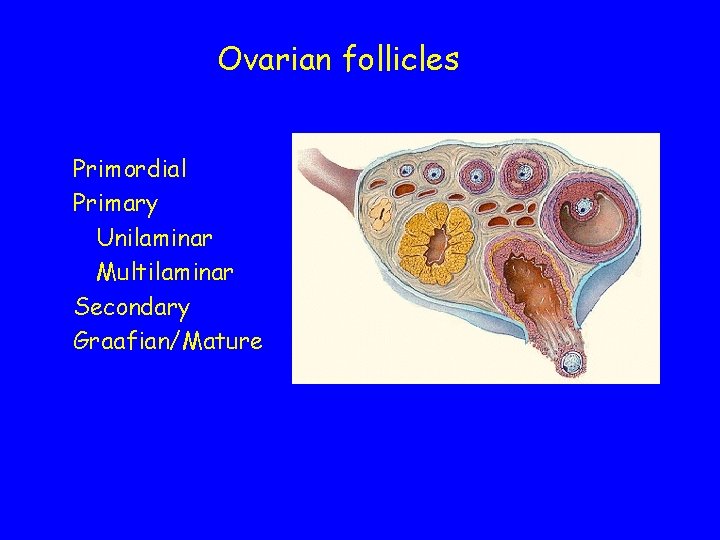
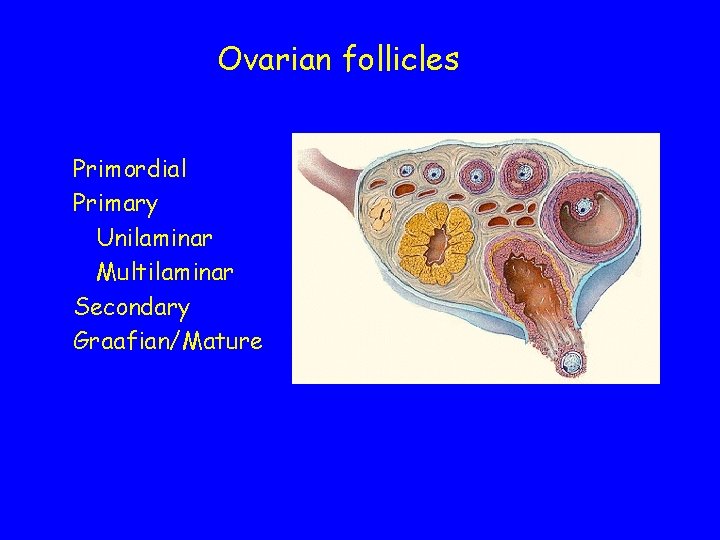
Ovarian follicles Primordial Primary Unilaminar Multilaminar Secondary Graafian/Mature
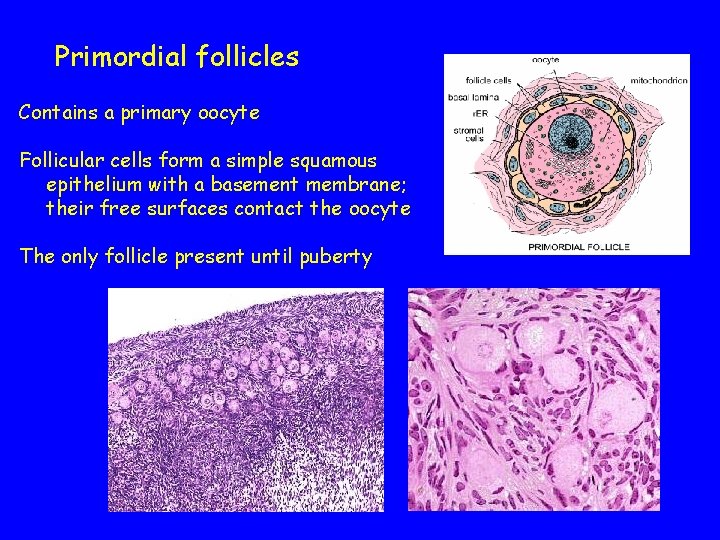
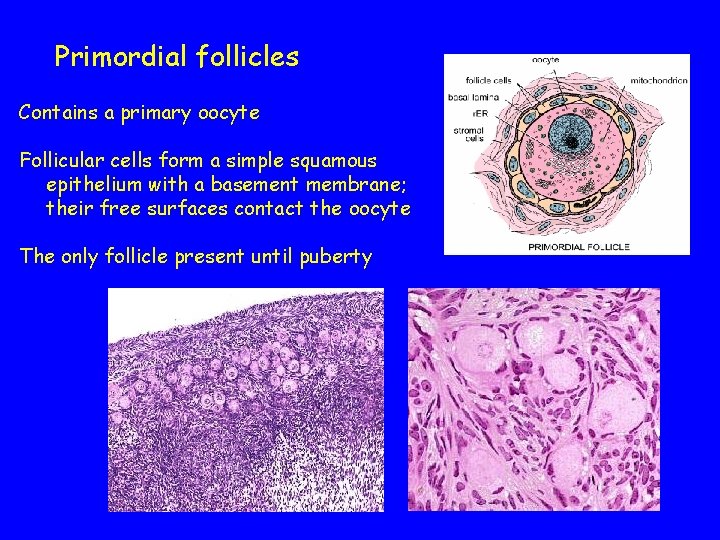
Primordial follicles Contains a primary oocyte Follicular cells form a simple squamous epithelium with a basement membrane; their free surfaces contact the oocyte The only follicle present until puberty
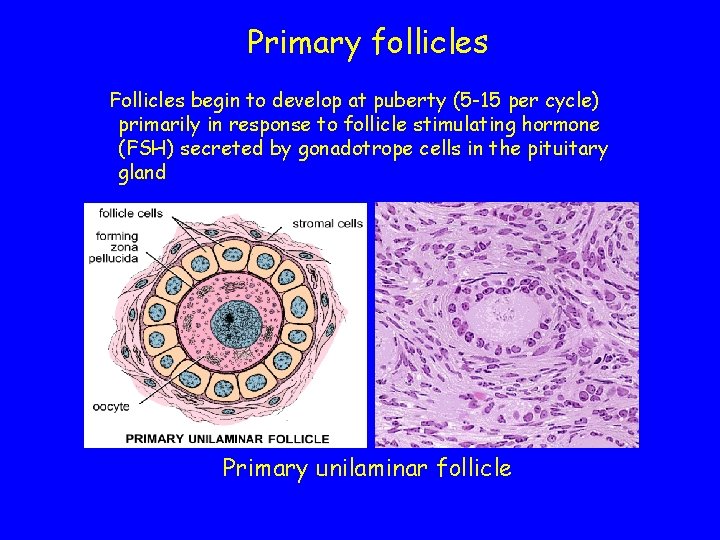
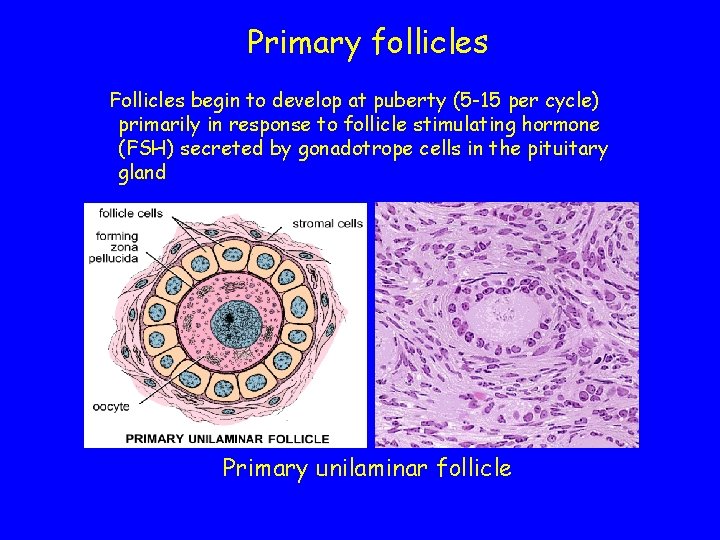
Primary follicles Follicles begin to develop at puberty (5 -15 per cycle) primarily in response to follicle stimulating hormone (FSH) secreted by gonadotrope cells in the pituitary gland Primary unilaminar follicle
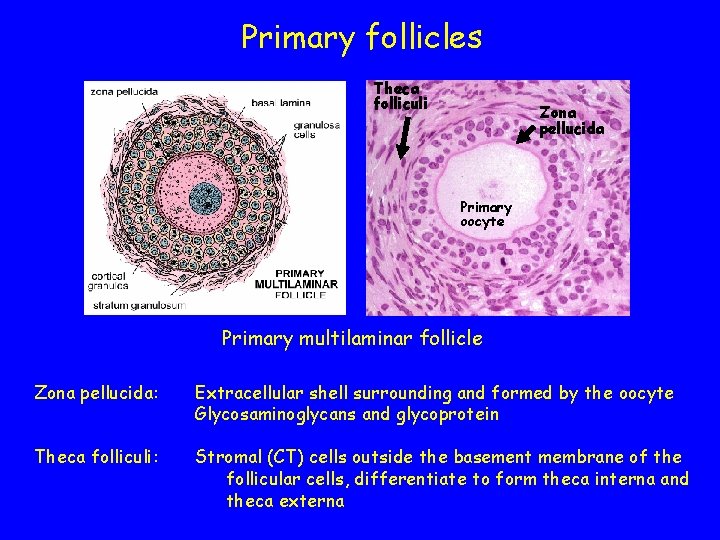
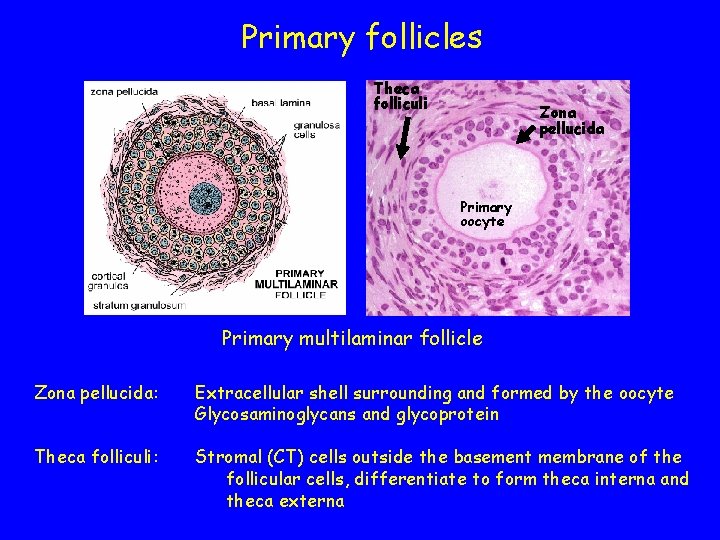
Primary follicles Theca folliculi Zona pellucida Primary oocyte Primary multilaminar follicle Zona pellucida: Extracellular shell surrounding and formed by the oocyte Glycosaminoglycans and glycoprotein Theca folliculi: Stromal (CT) cells outside the basement membrane of the follicular cells, differentiate to form theca interna and theca externa
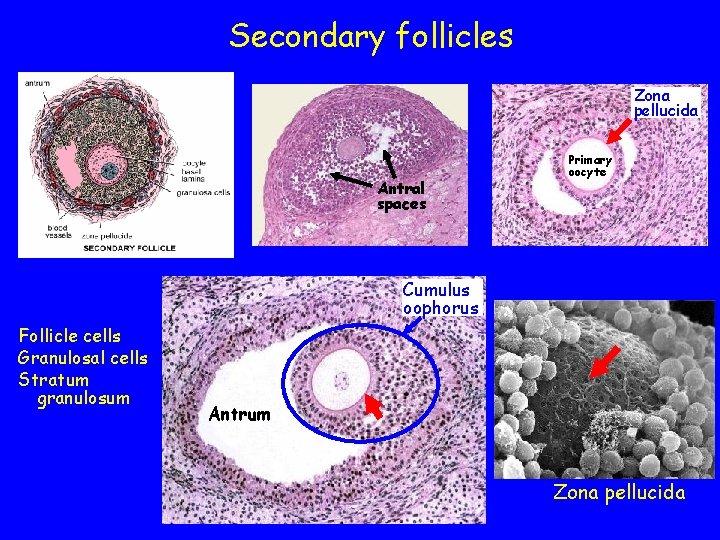
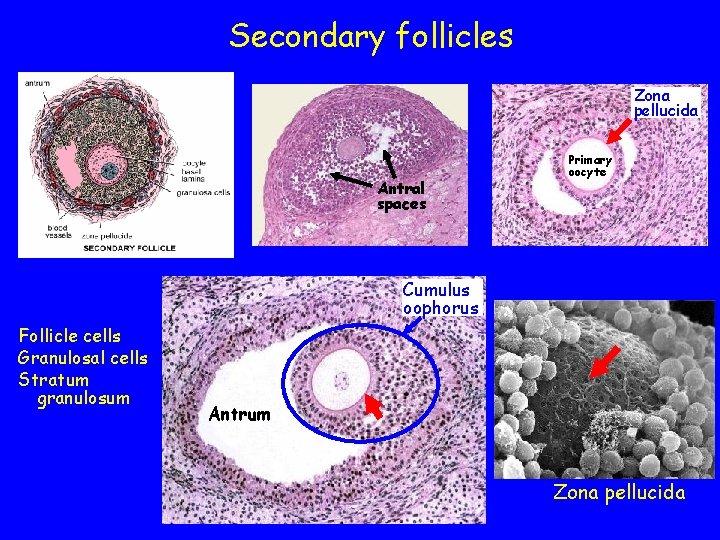
Secondary follicles Zona pellucida Antral spaces Primary oocyte Cumulus oophorus Follicle cells Granulosal cells Stratum granulosum Antrum Zona pellucida
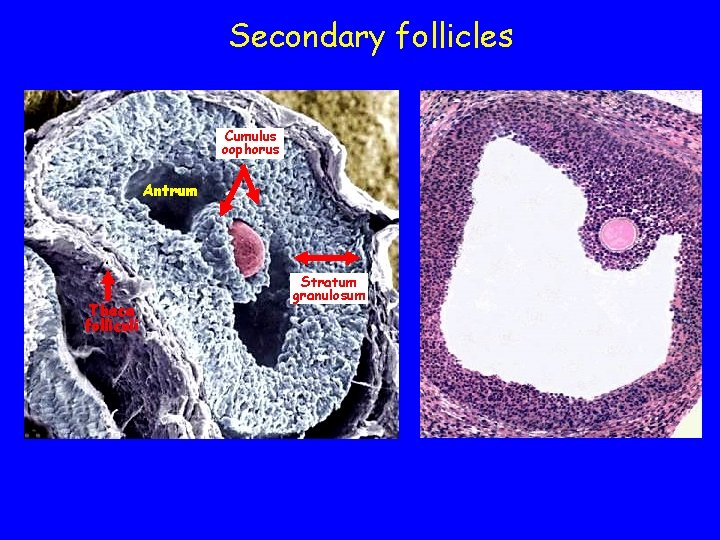
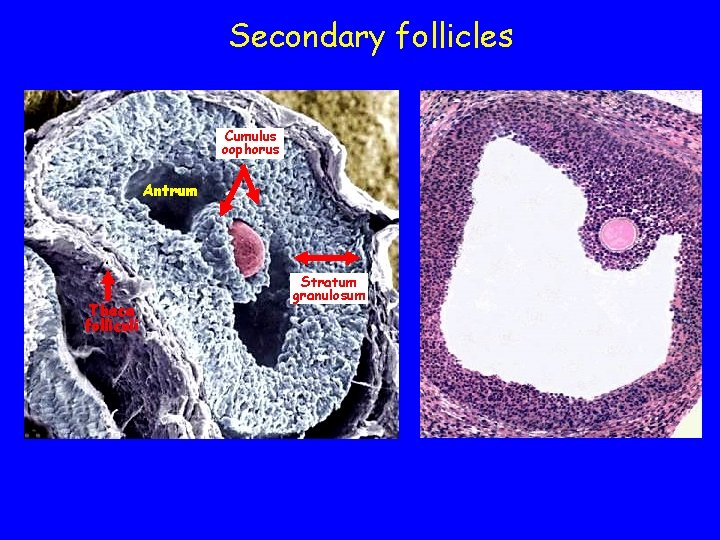
Secondary follicles Cumulus oophorus Antrum Theca folliculi Stratum granulosum
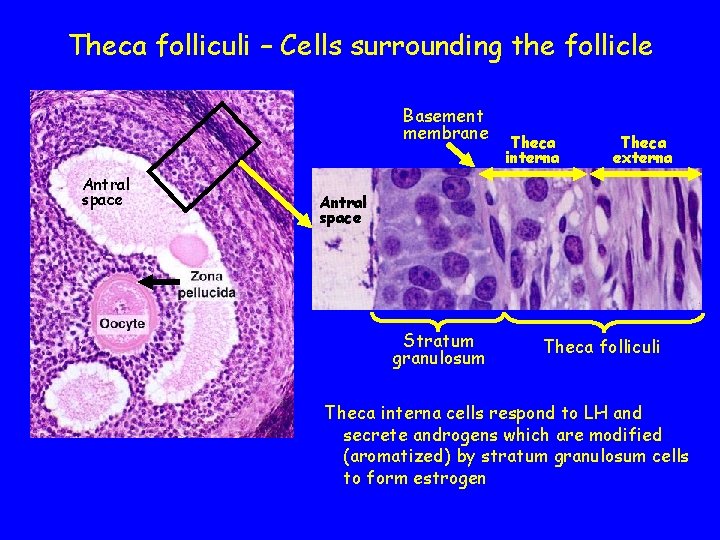
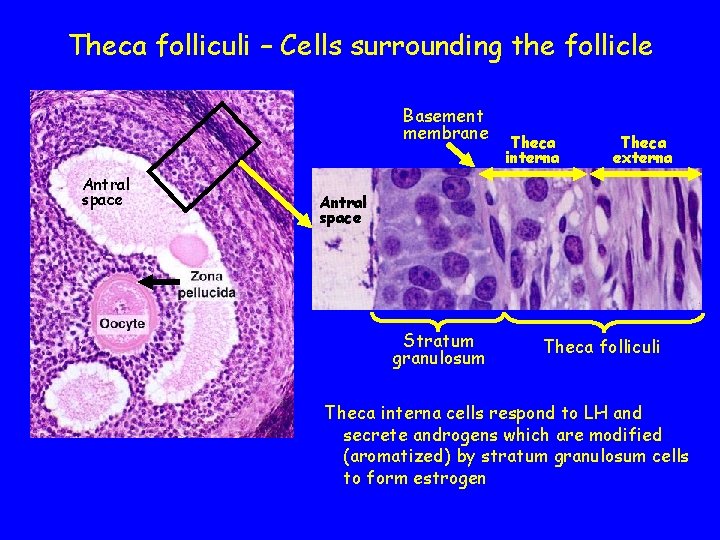
Theca folliculi – Cells surrounding the follicle Basement membrane Antral space Theca interna Theca externa Antral space Stratum granulosum Theca folliculi Theca interna cells respond to LH and secrete androgens which are modified (aromatized) by stratum granulosum cells to form estrogen
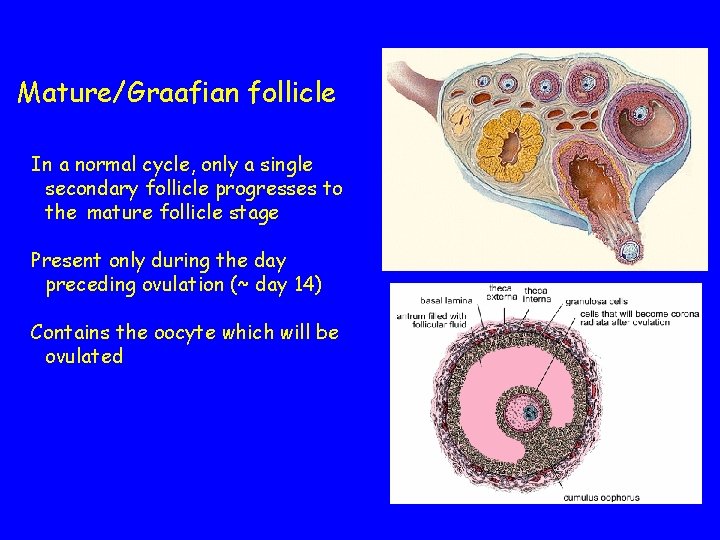
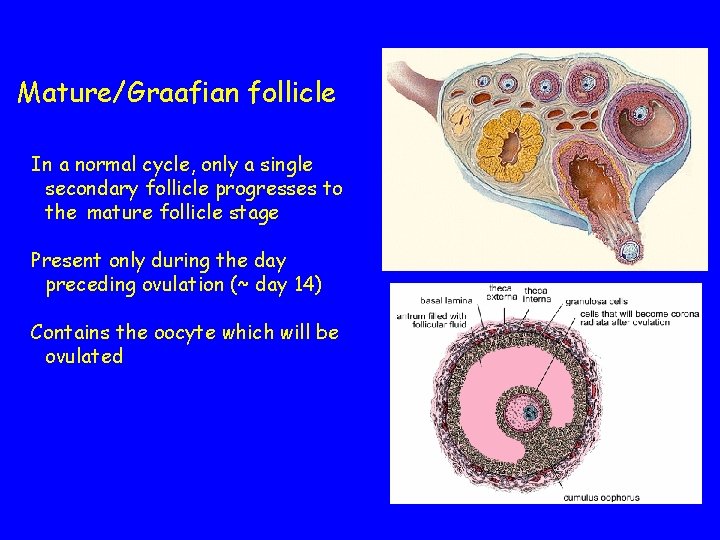
Mature/Graafian follicle In a normal cycle, only a single secondary follicle progresses to the mature follicle stage Present only during the day preceding ovulation (~ day 14) Contains the oocyte which will be ovulated
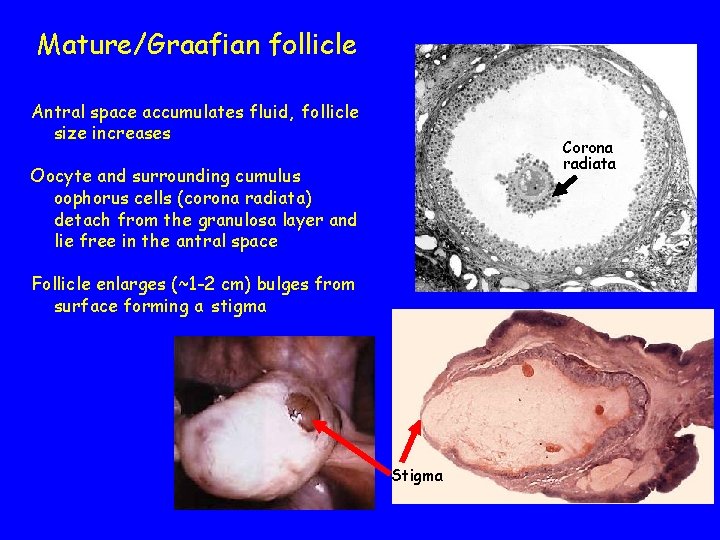
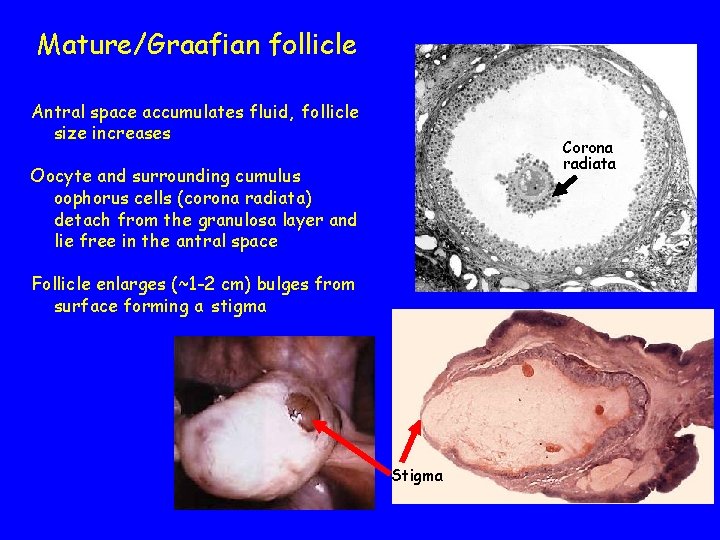
Mature/Graafian follicle Antral space accumulates fluid, follicle size increases Corona radiata Oocyte and surrounding cumulus oophorus cells (corona radiata) detach from the granulosa layer and lie free in the antral space Follicle enlarges (~1 -2 cm) bulges from surface forming a stigma Stigma
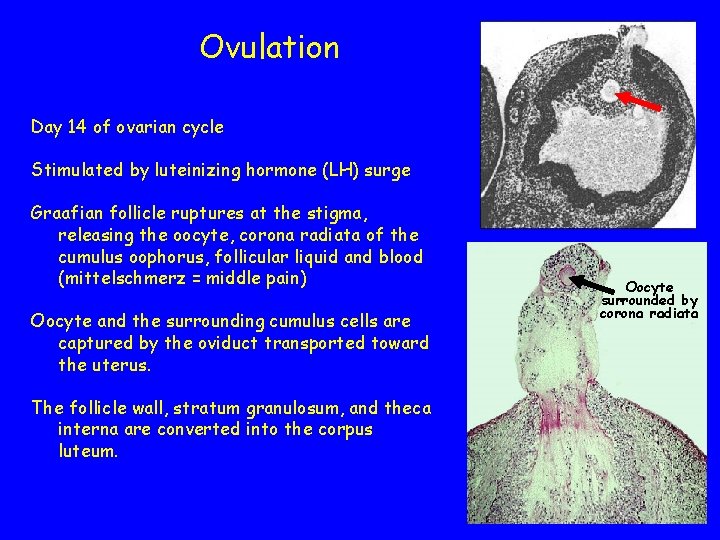
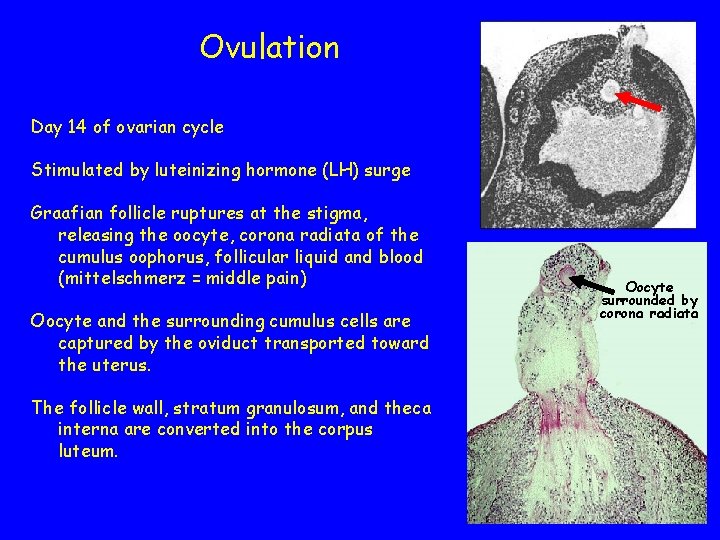
Ovulation Day 14 of ovarian cycle Stimulated by luteinizing hormone (LH) surge Graafian follicle ruptures at the stigma, releasing the oocyte, corona radiata of the cumulus oophorus, follicular liquid and blood (mittelschmerz = middle pain) Oocyte and the surrounding cumulus cells are captured by the oviduct transported toward the uterus. The follicle wall, stratum granulosum, and theca interna are converted into the corpus luteum. Oocyte surrounded by corona radiata
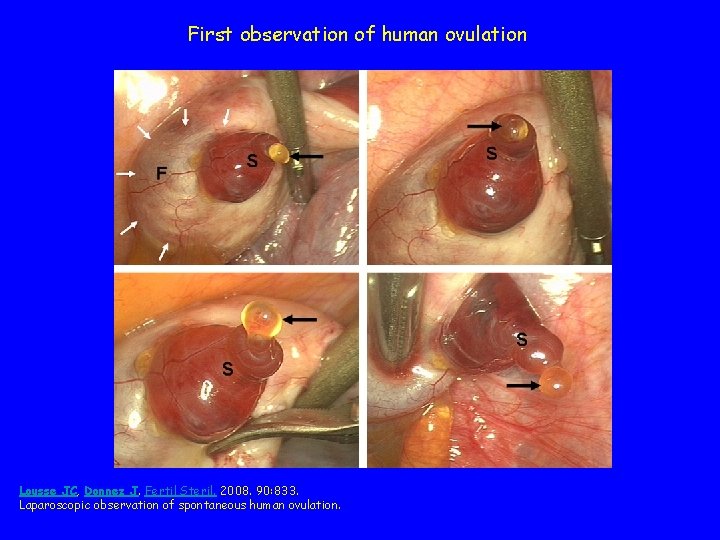
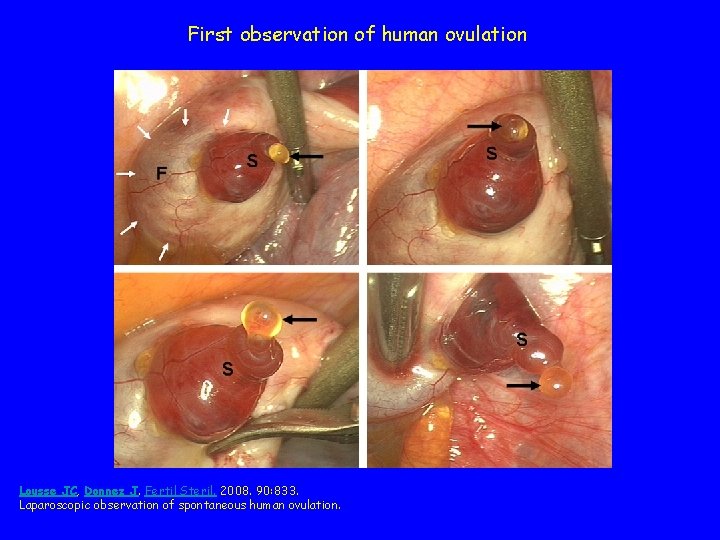
First observation of human ovulation Lousse JC, Donnez J. Fertil Steril. 2008. 90: 833. Laparoscopic observation of spontaneous human ovulation.
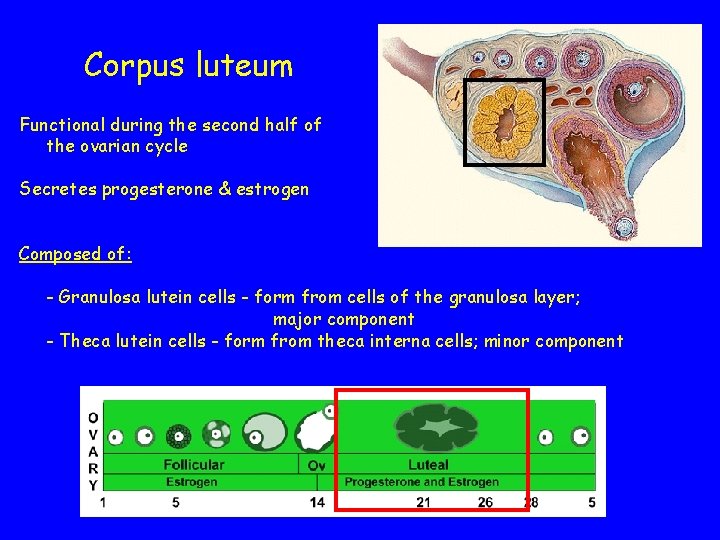
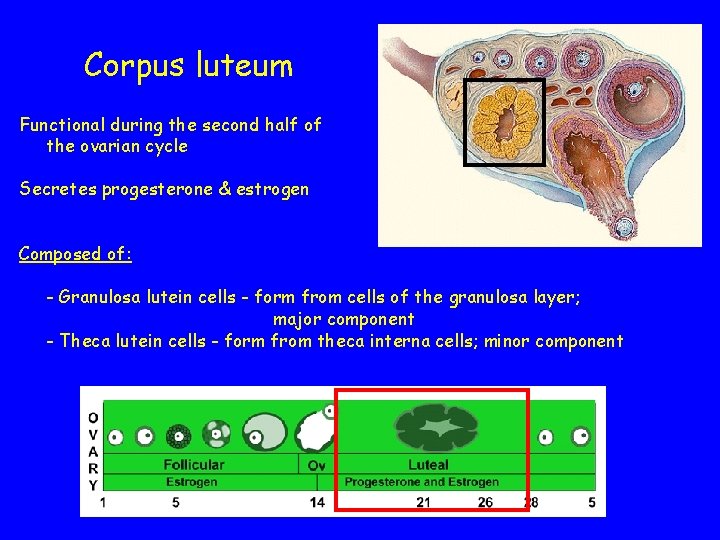
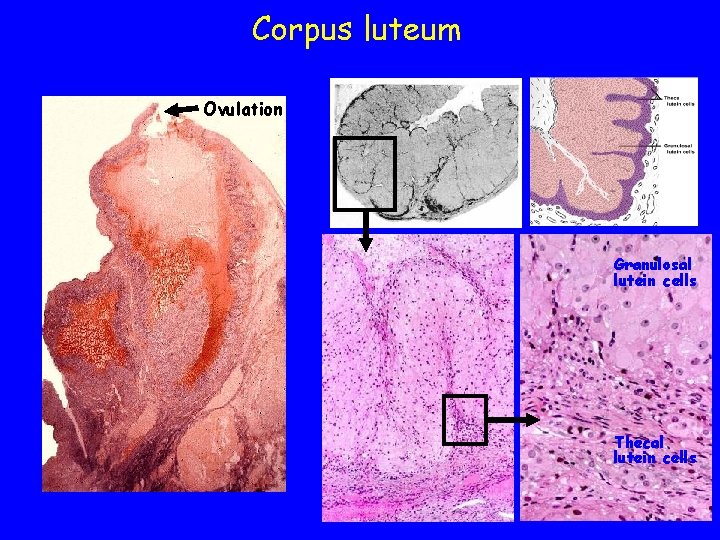
Corpus luteum Functional during the second half of the ovarian cycle Secretes progesterone & estrogen Composed of: - Granulosa lutein cells - form from cells of the granulosa layer; major component - Theca lutein cells - form from theca interna cells; minor component
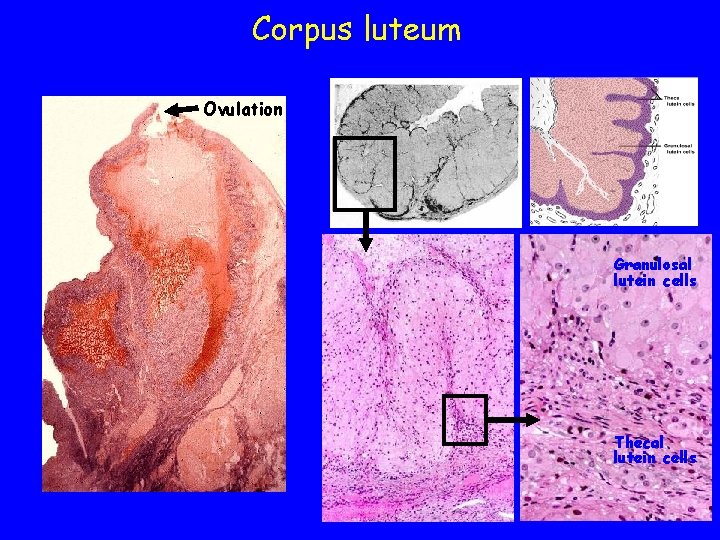
Corpus luteum Ovulation Granulosal lutein cells Thecal lutein cells
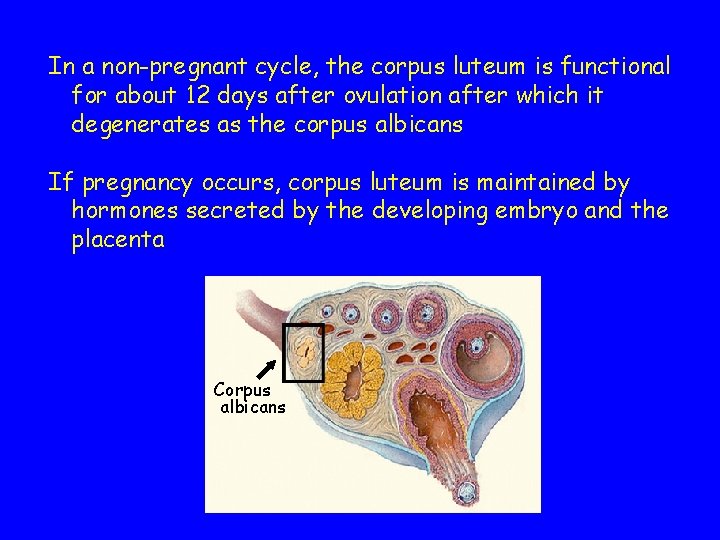
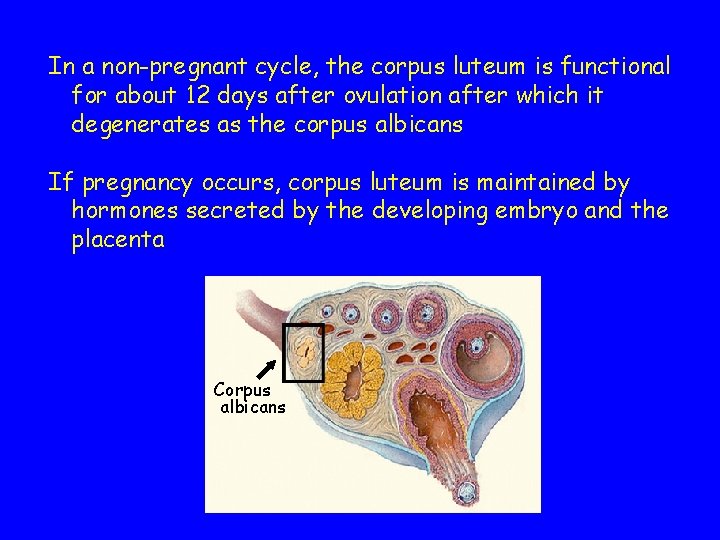
In a non-pregnant cycle, the corpus luteum is functional for about 12 days after ovulation after which it degenerates as the corpus albicans If pregnancy occurs, corpus luteum is maintained by hormones secreted by the developing embryo and the placenta Corpus albicans
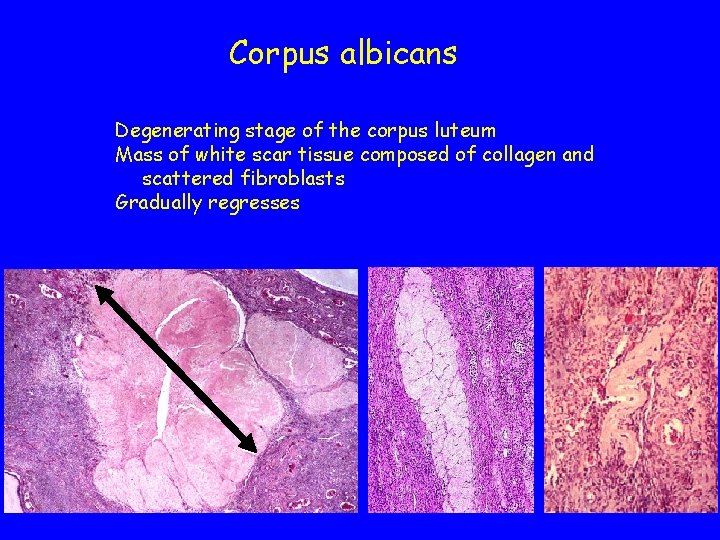
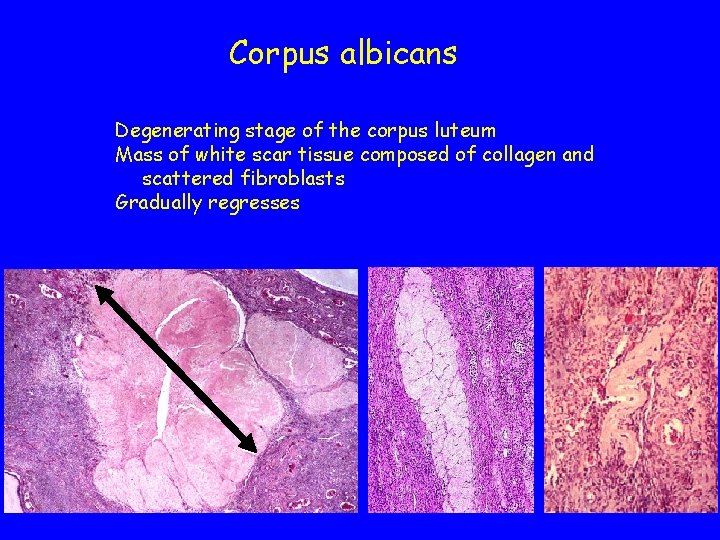
Corpus albicans Degenerating stage of the corpus luteum Mass of white scar tissue composed of collagen and scattered fibroblasts Gradually regresses
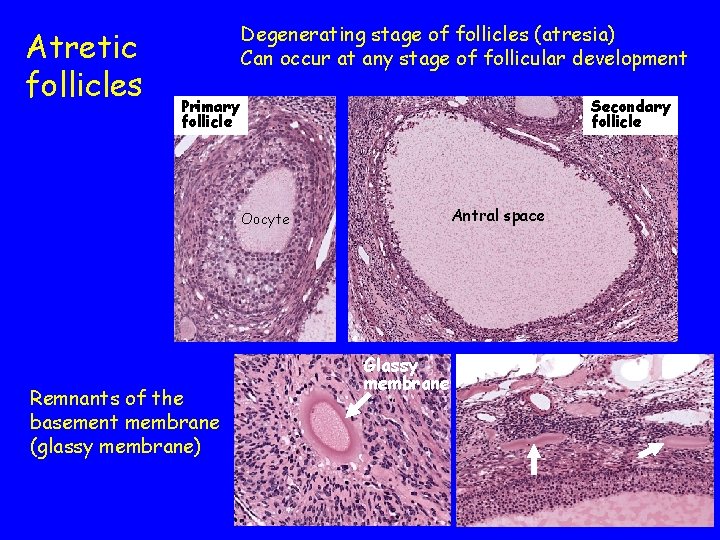
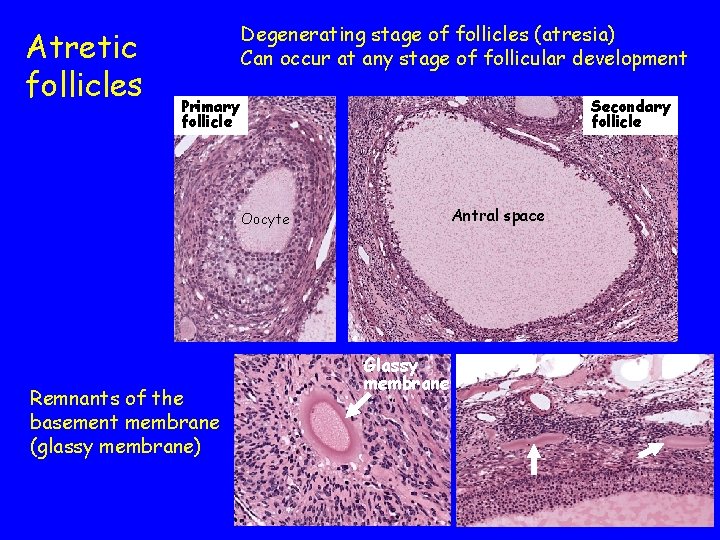
Atretic follicles Degenerating stage of follicles (atresia) Can occur at any stage of follicular development Primary follicle Secondary follicle Antral space Oocyte Remnants of the basement membrane (glassy membrane) Glassy membrane
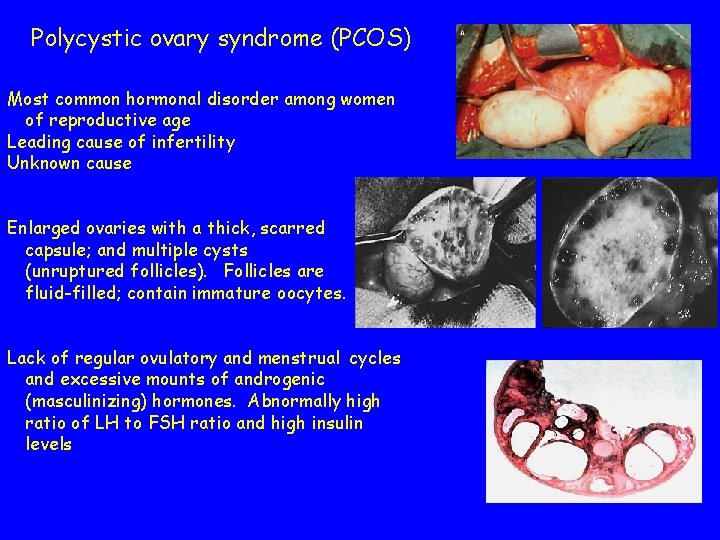
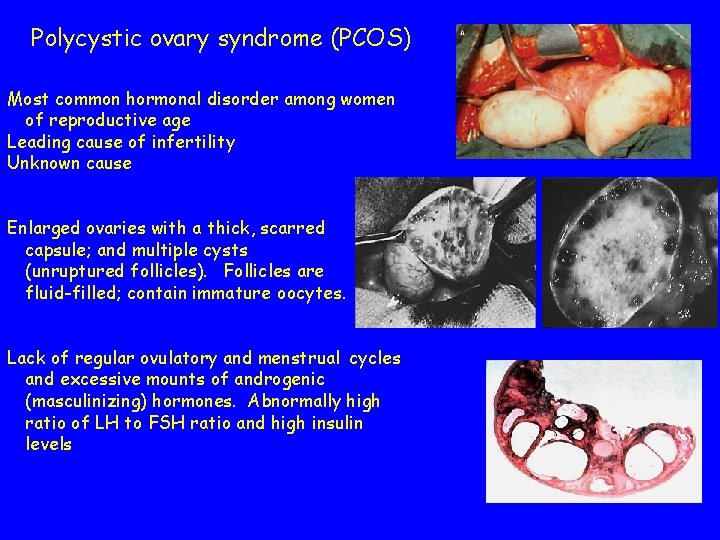
Polycystic ovary syndrome (PCOS) Most common hormonal disorder among women of reproductive age Leading cause of infertility Unknown cause Enlarged ovaries with a thick, scarred capsule; and multiple cysts (unruptured follicles). Follicles are fluid-filled; contain immature oocytes. Lack of regular ovulatory and menstrual cycles and excessive mounts of androgenic (masculinizing) hormones. Abnormally high ratio of LH to FSH ratio and high insulin levels
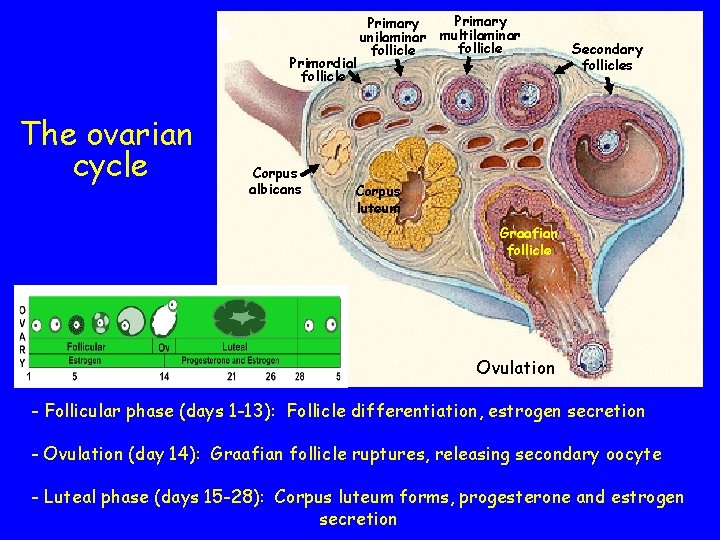
Primordial follicle The ovarian cycle Corpus albicans Primary multilaminar unilaminar follicle Secondary follicles Corpus luteum Graafian follicle Ovulation - Follicular phase (days 1 -13): Follicle differentiation, estrogen secretion - Ovulation (day 14): Graafian follicle ruptures, releasing secondary oocyte - Luteal phase (days 15 -28): Corpus luteum forms, progesterone and estrogen secretion
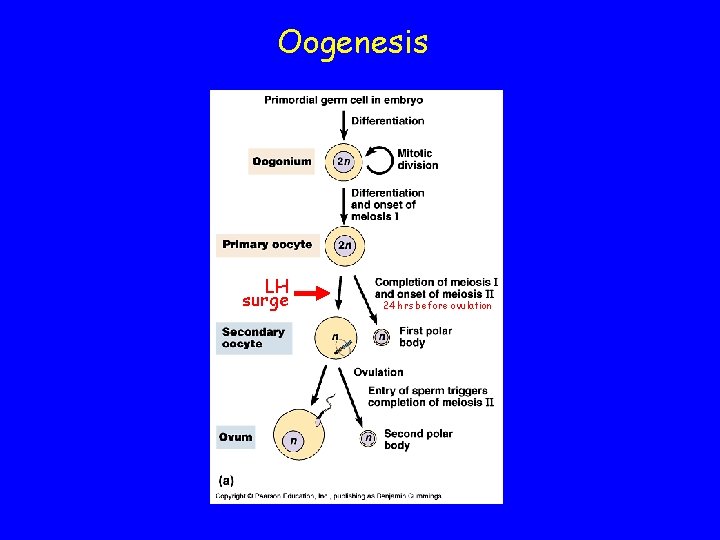
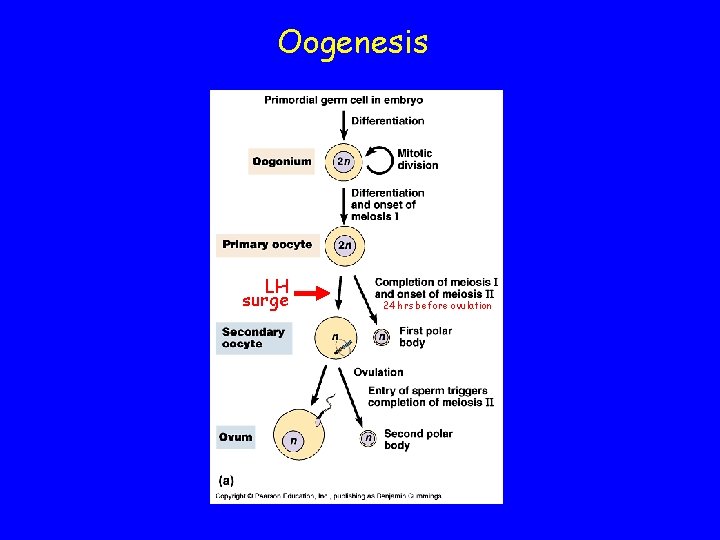
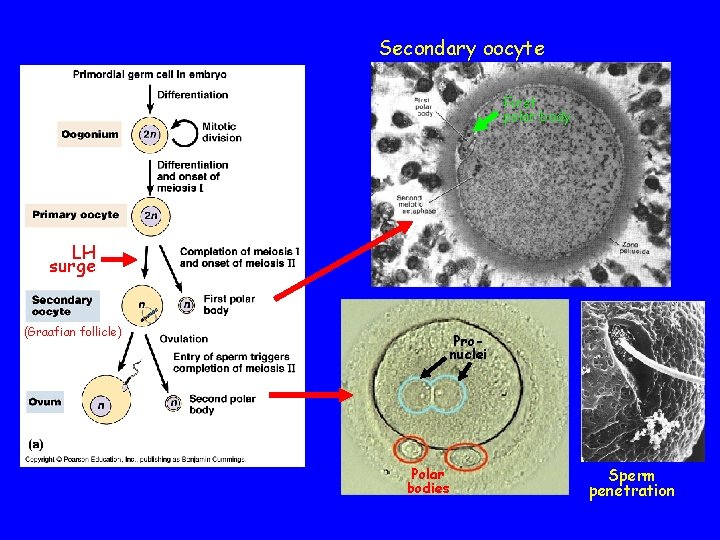
Oogenesis LH surge 24 hrs before ovulation
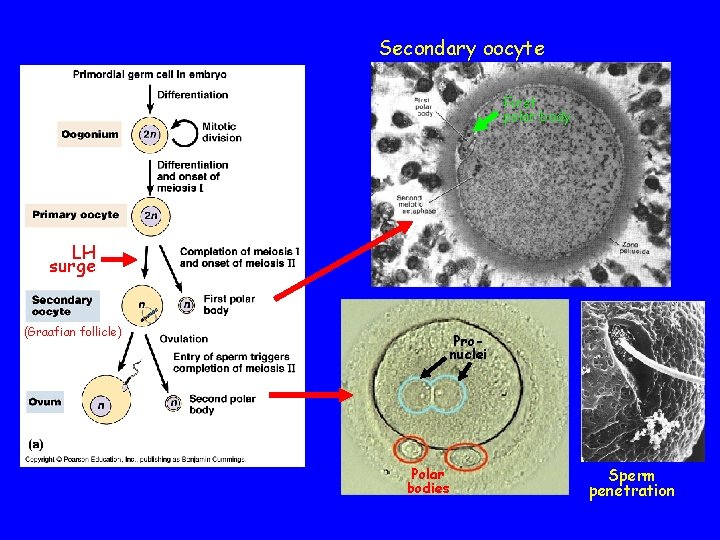
Secondary oocyte First polar body LH surge (Graafian follicle) Pronuclei Polar bodies Sperm penetration
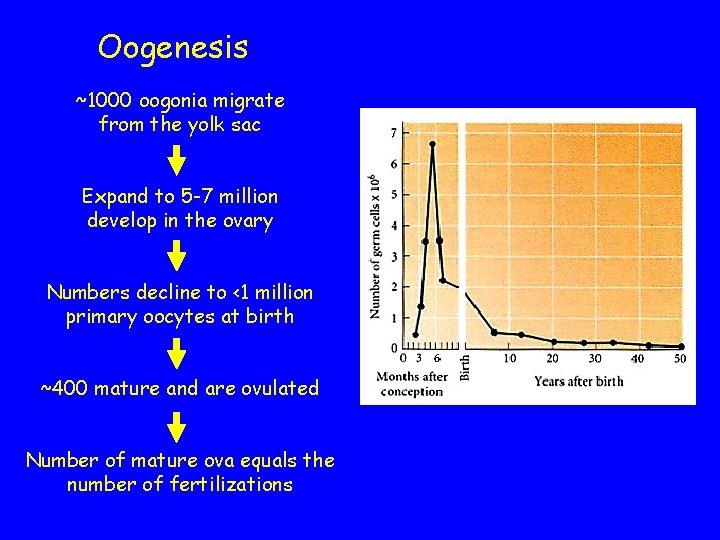
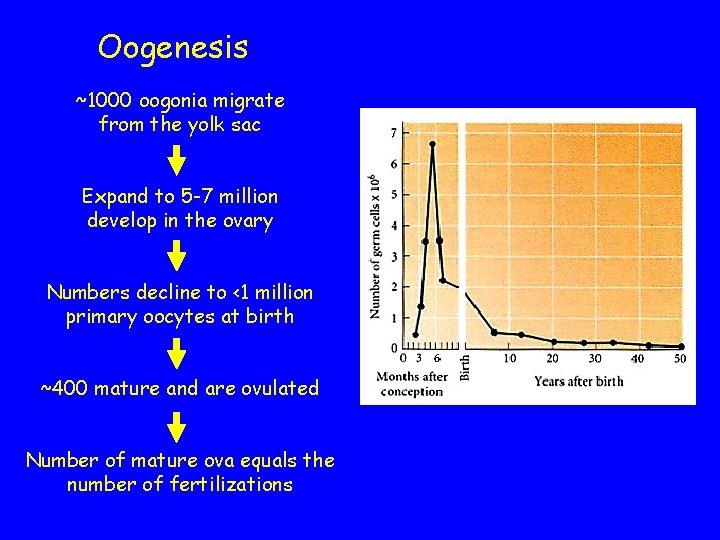
Oogenesis ~1000 oogonia migrate from the yolk sac Expand to 5 -7 million develop in the ovary Numbers decline to <1 million primary oocytes at birth ~400 mature and are ovulated Number of mature ova equals the number of fertilizations
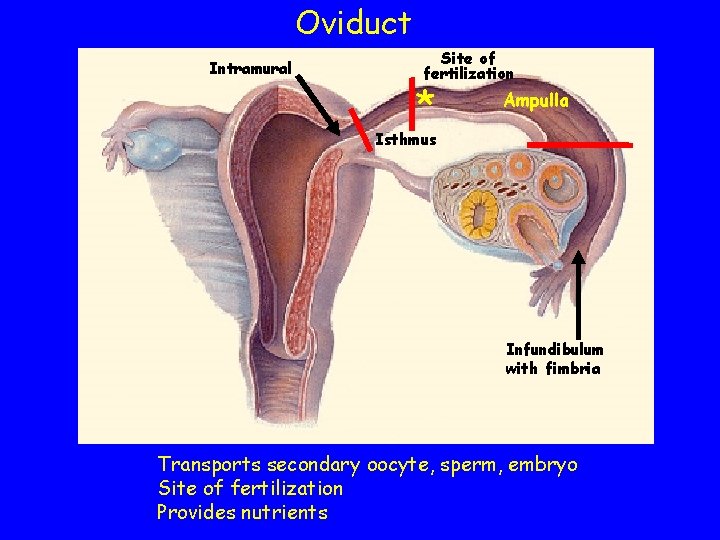
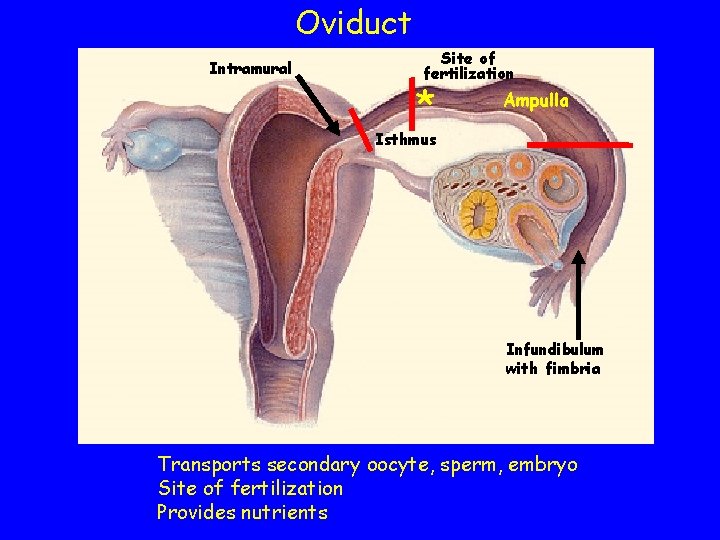
Oviduct Intramural Site of fertilization * Ampulla Isthmus Infundibulum with fimbria Transports secondary oocyte, sperm, embryo Site of fertilization Provides nutrients
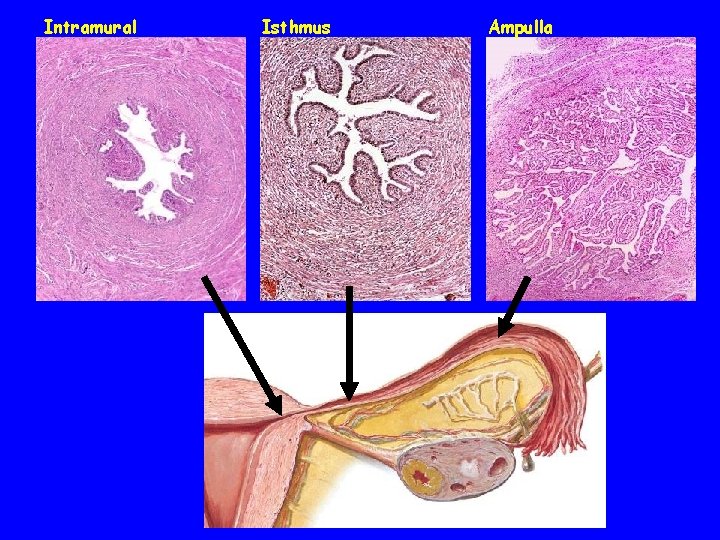
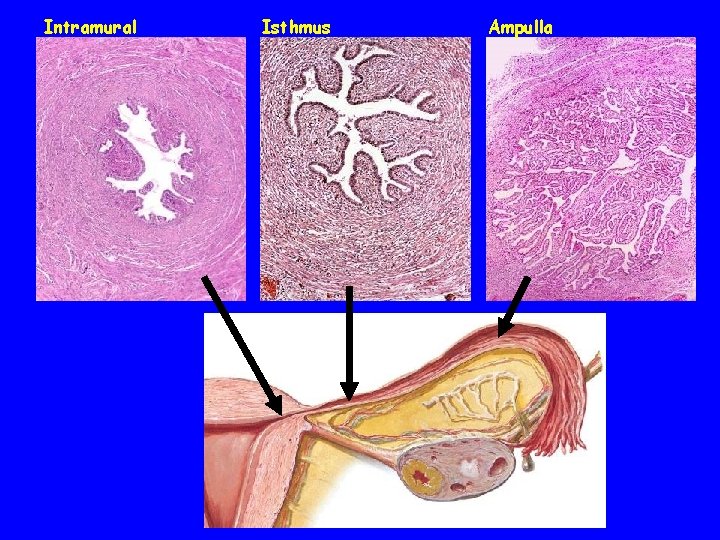
Intramural Isthmus Ampulla
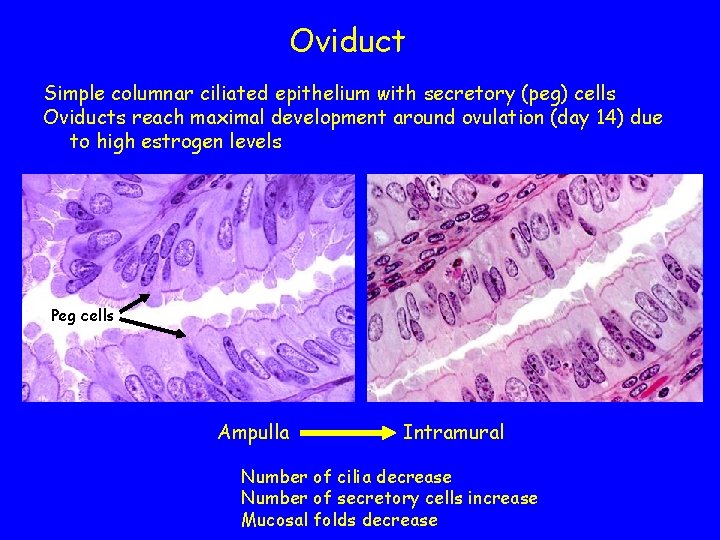
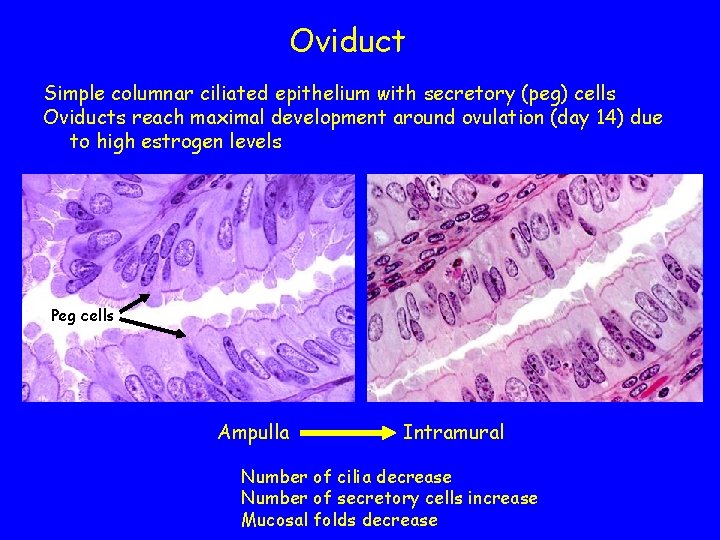
Oviduct Simple columnar ciliated epithelium with secretory (peg) cells Oviducts reach maximal development around ovulation (day 14) due to high estrogen levels Peg cells Ampulla Intramural Number of cilia decrease Number of secretory cells increase Mucosal folds decrease
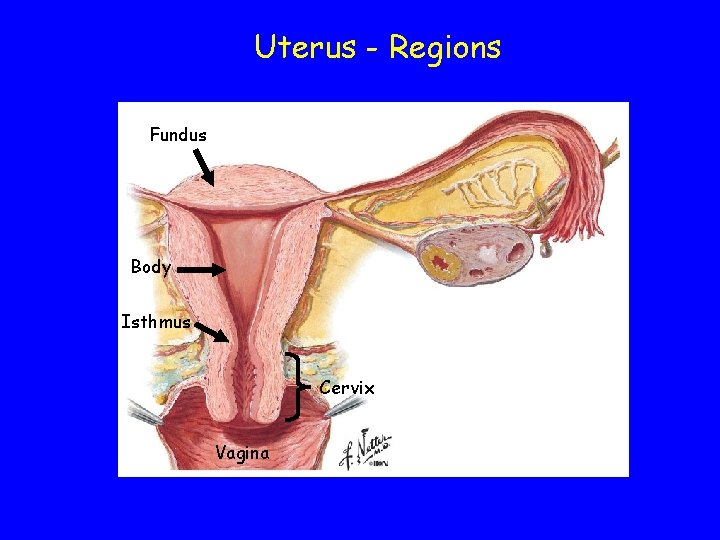
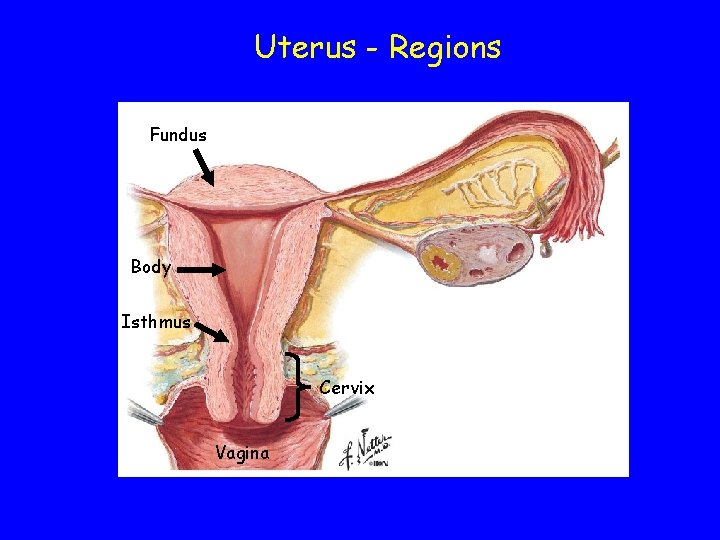
Uterus - Regions Fundus Body Isthmus Cervix Vagina
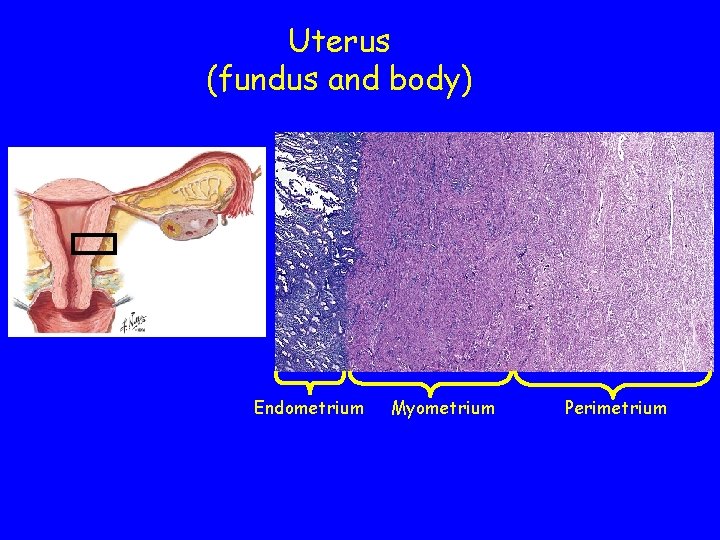
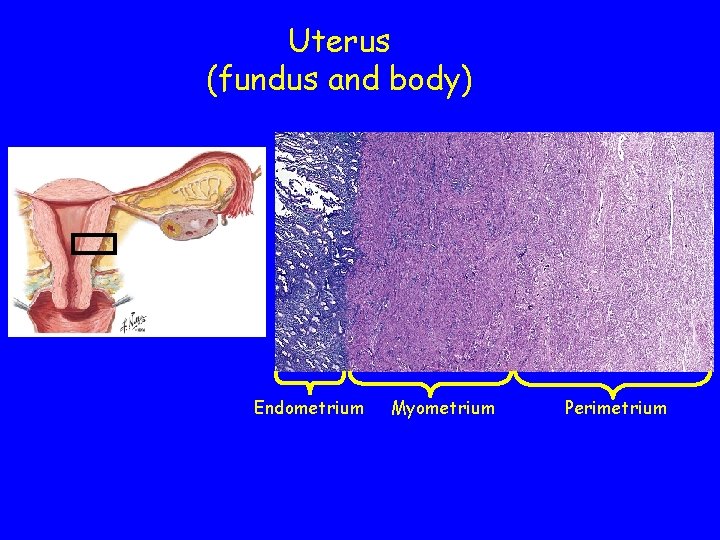
Uterus (fundus and body) Endometrium Myometrium Perimetrium
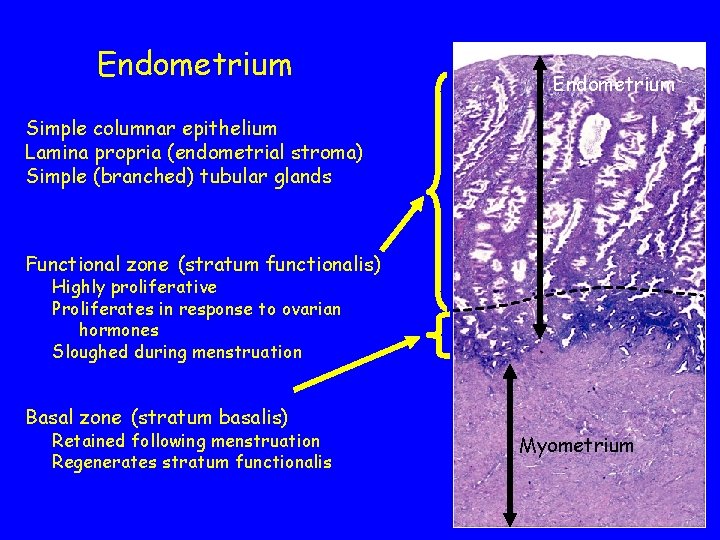
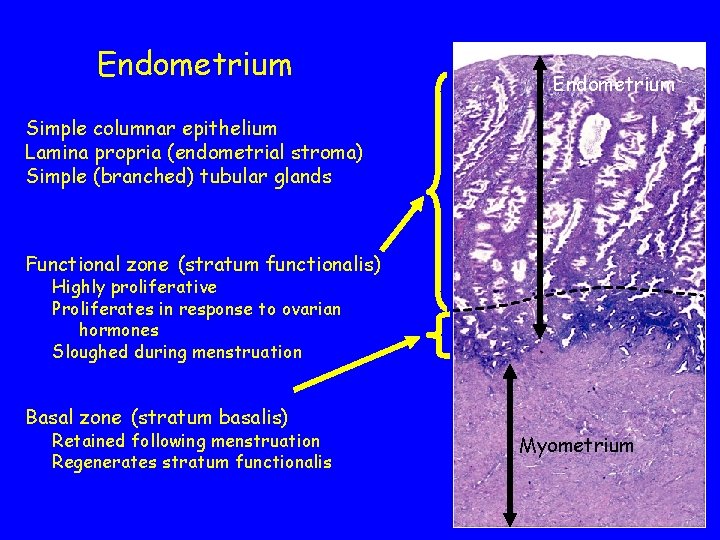
Endometrium Simple columnar epithelium Lamina propria (endometrial stroma) Simple (branched) tubular glands Functional zone (stratum functionalis) Highly proliferative Proliferates in response to ovarian hormones Sloughed during menstruation Basal zone (stratum basalis) Retained following menstruation Regenerates stratum functionalis Myometrium
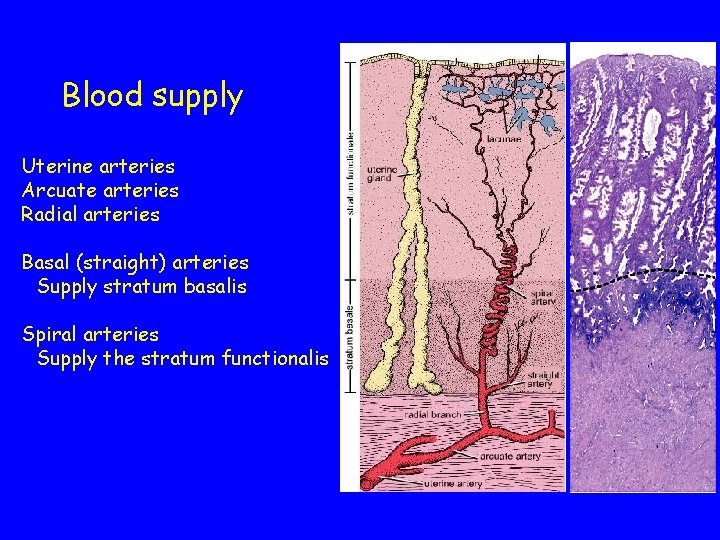
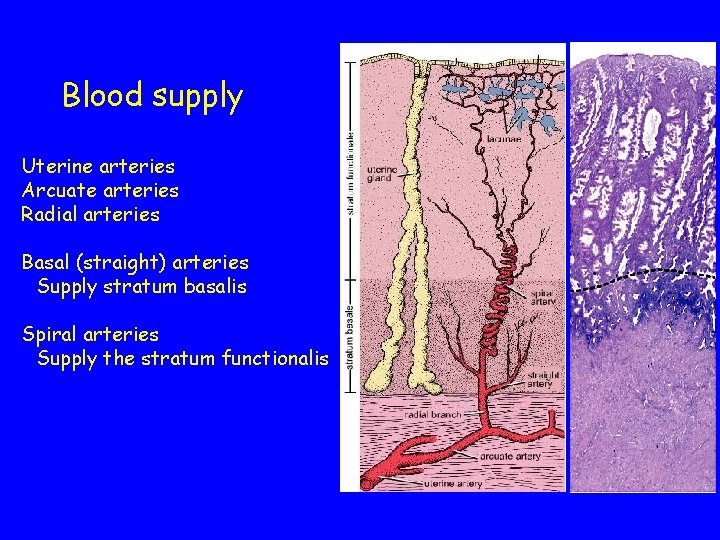
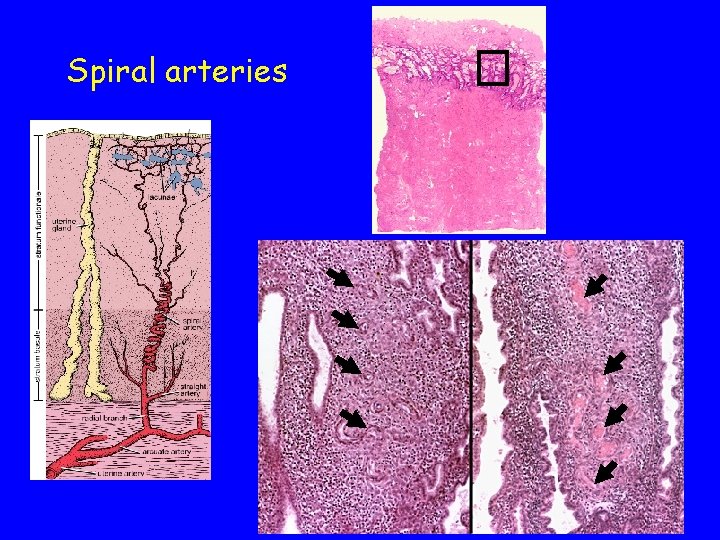
Blood supply Uterine arteries Arcuate arteries Radial arteries Basal (straight) arteries Supply stratum basalis Spiral arteries Supply the stratum functionalis
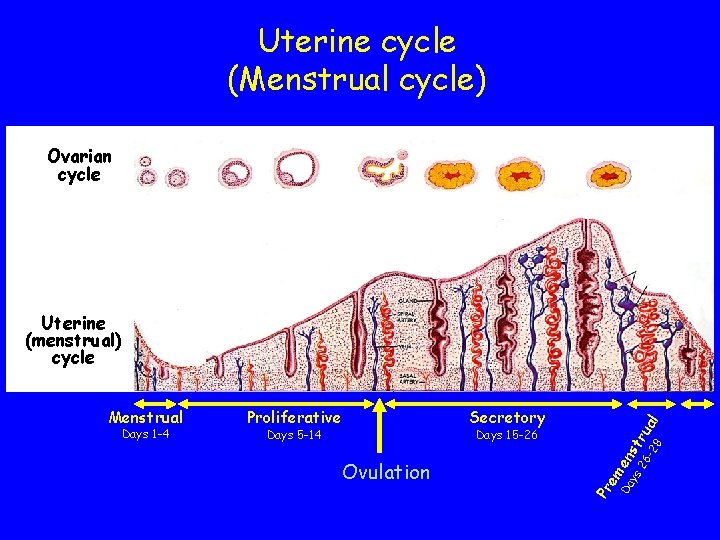
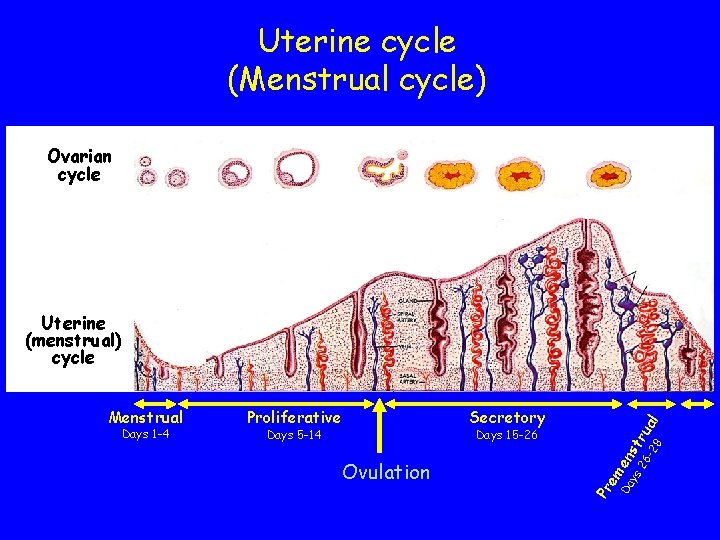
Uterine cycle (Menstrual cycle) Ovarian cycle Secretory Days 5 -14 Days 15 -26 Ovulation em Days 1 -4 Proliferative Pr Menstrual Da en ys st 26 ru -2 al 8 Uterine (menstrual) cycle
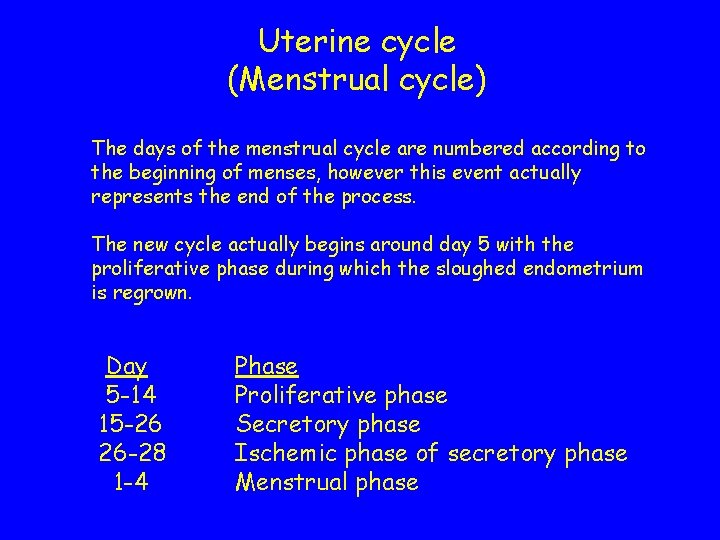
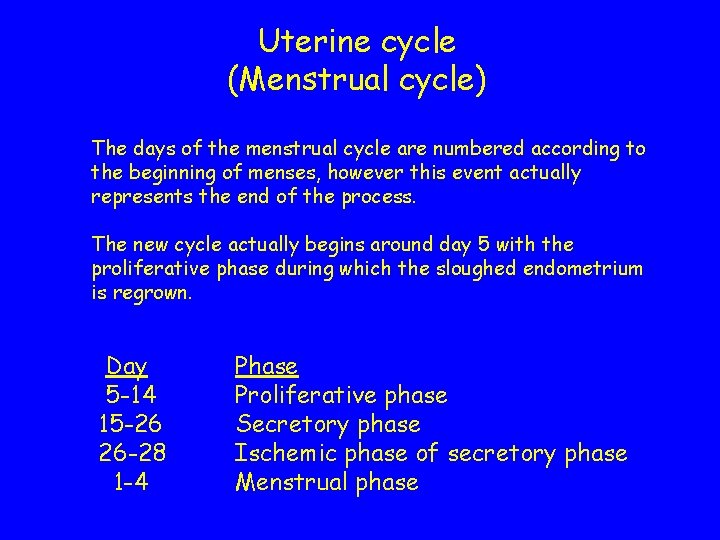
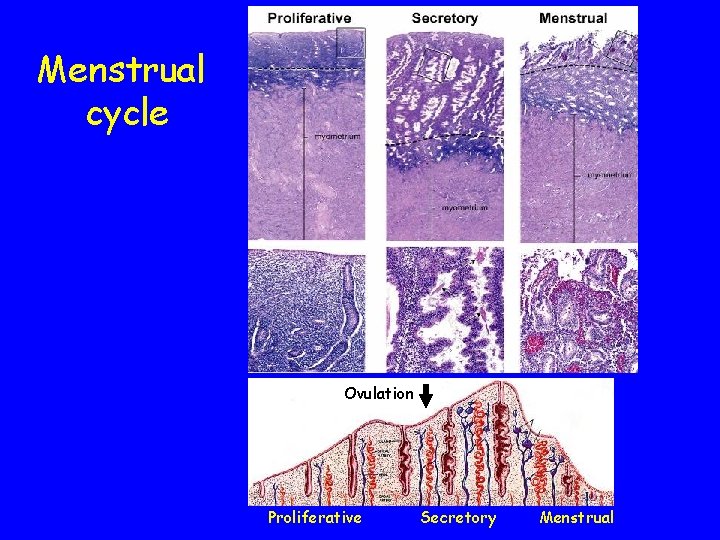
Uterine cycle (Menstrual cycle) The days of the menstrual cycle are numbered according to the beginning of menses, however this event actually represents the end of the process. The new cycle actually begins around day 5 with the proliferative phase during which the sloughed endometrium is regrown. Day 5 -14 15 -26 26 -28 1 -4 Phase Proliferative phase Secretory phase Ischemic phase of secretory phase Menstrual phase
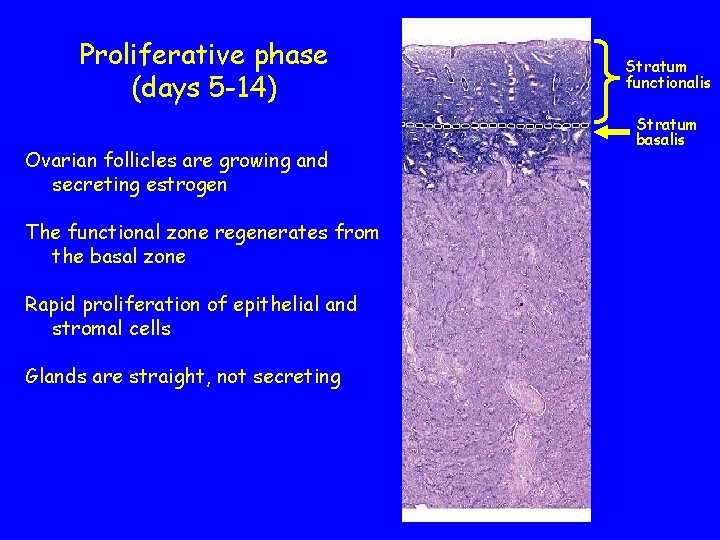
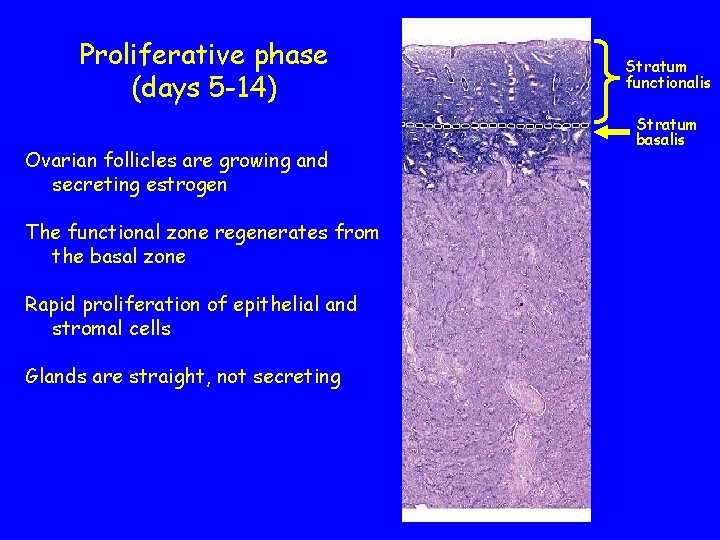
Proliferative phase (days 5 -14) Ovarian follicles are growing and secreting estrogen The functional zone regenerates from the basal zone Rapid proliferation of epithelial and stromal cells Glands are straight, not secreting Stratum functionalis Stratum basalis
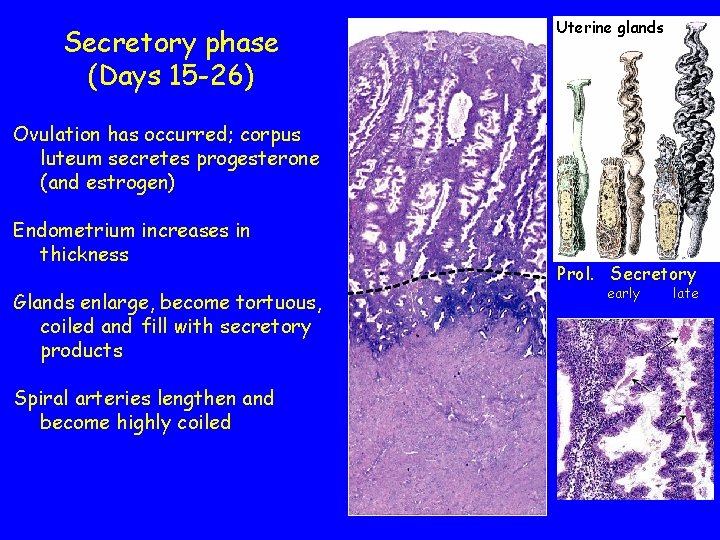
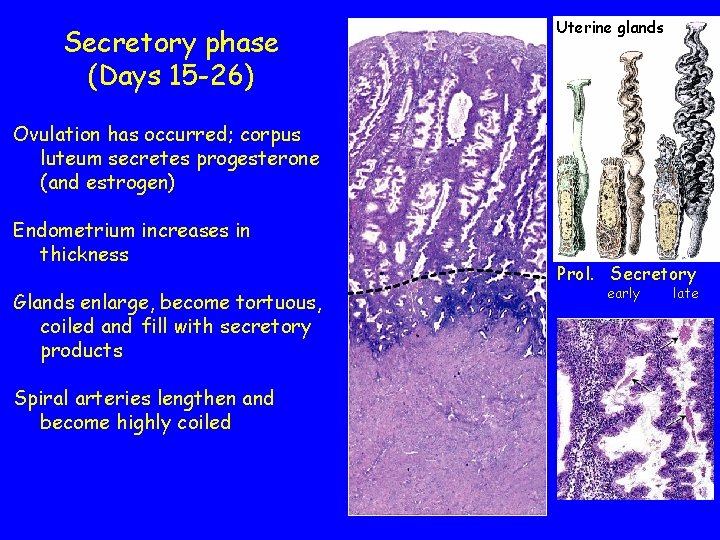
Secretory phase (Days 15 -26) Uterine glands Ovulation has occurred; corpus luteum secretes progesterone (and estrogen) Endometrium increases in thickness Glands enlarge, become tortuous, coiled and fill with secretory products Spiral arteries lengthen and become highly coiled Prol. Secretory early late
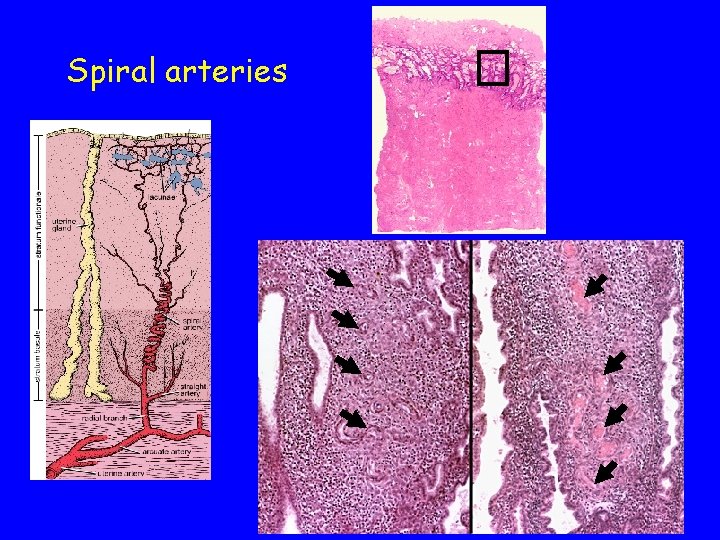
Spiral arteries
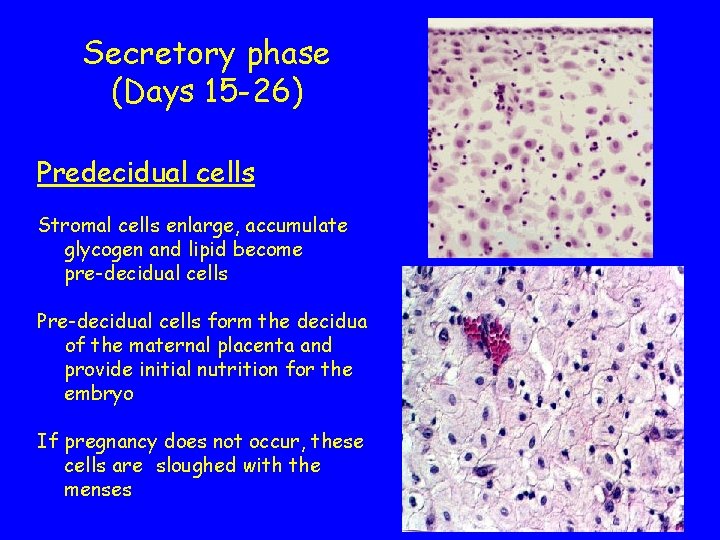
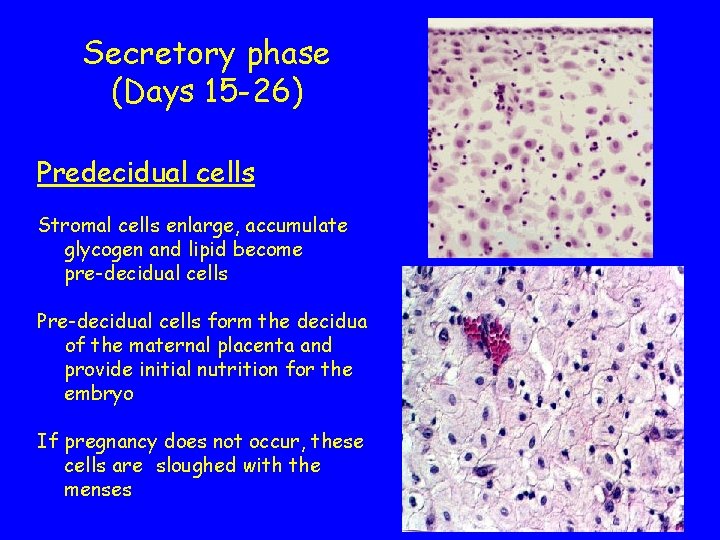
Secretory phase (Days 15 -26) Predecidual cells Stromal cells enlarge, accumulate glycogen and lipid become pre-decidual cells Pre-decidual cells form the decidua of the maternal placenta and provide initial nutrition for the embryo If pregnancy does not occur, these cells are sloughed with the menses
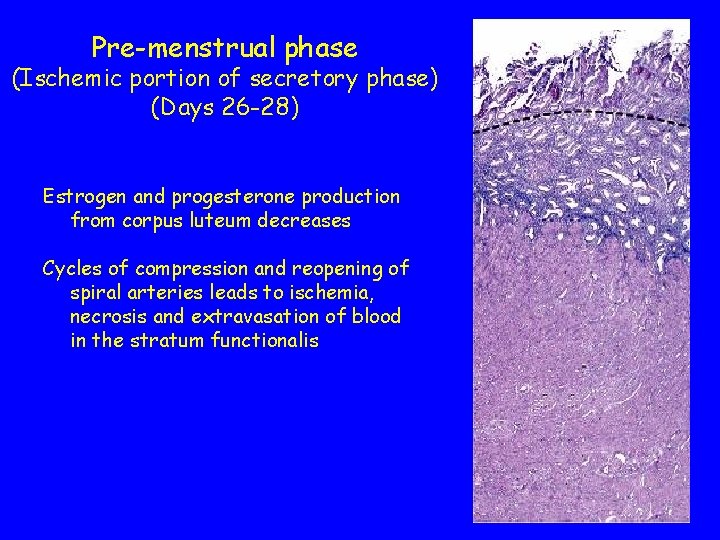
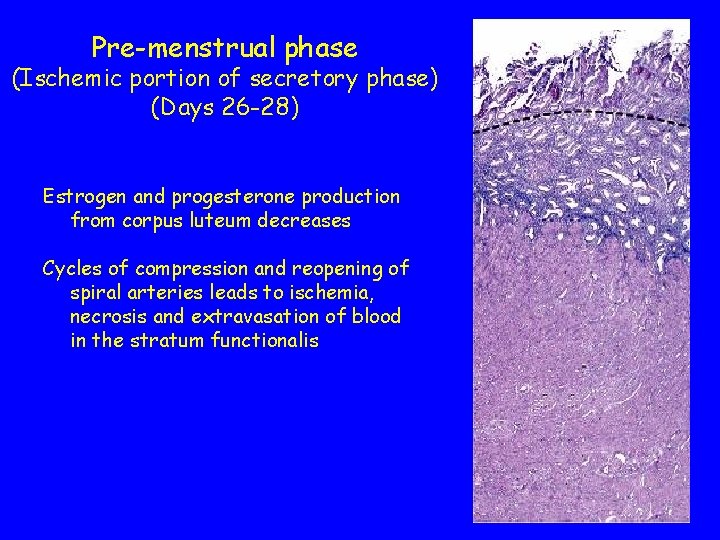
Pre-menstrual phase (Ischemic portion of secretory phase) (Days 26 -28) Estrogen and progesterone production from corpus luteum decreases Cycles of compression and reopening of spiral arteries leads to ischemia, necrosis and extravasation of blood in the stratum functionalis
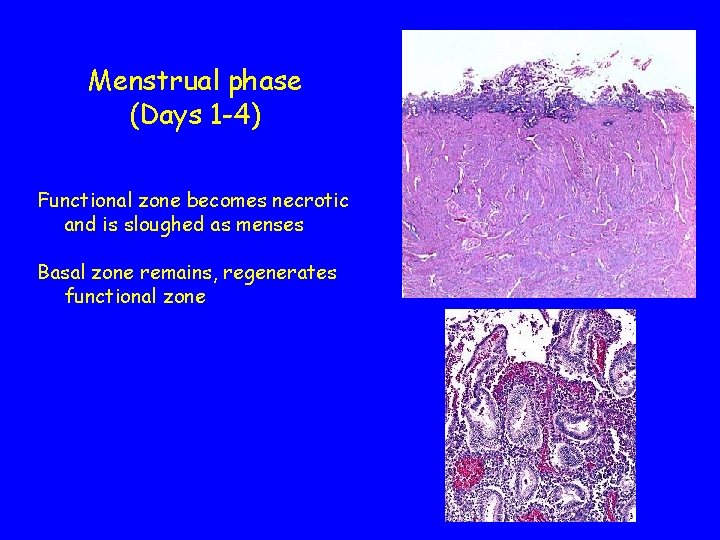
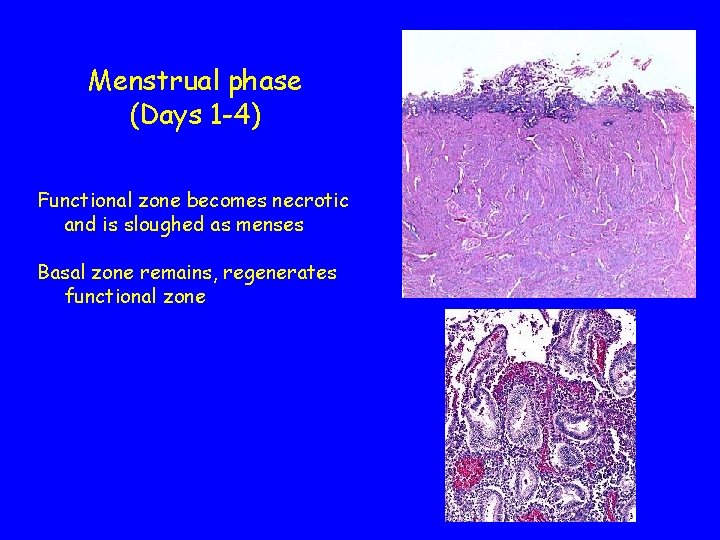
Menstrual phase (Days 1 -4) Functional zone becomes necrotic and is sloughed as menses Basal zone remains, regenerates functional zone
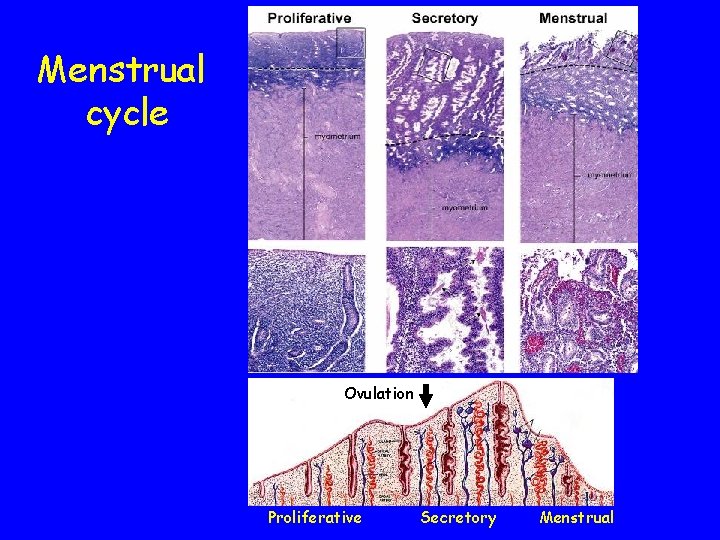
Menstrual cycle Ovulation Proliferative Secretory Menstrual
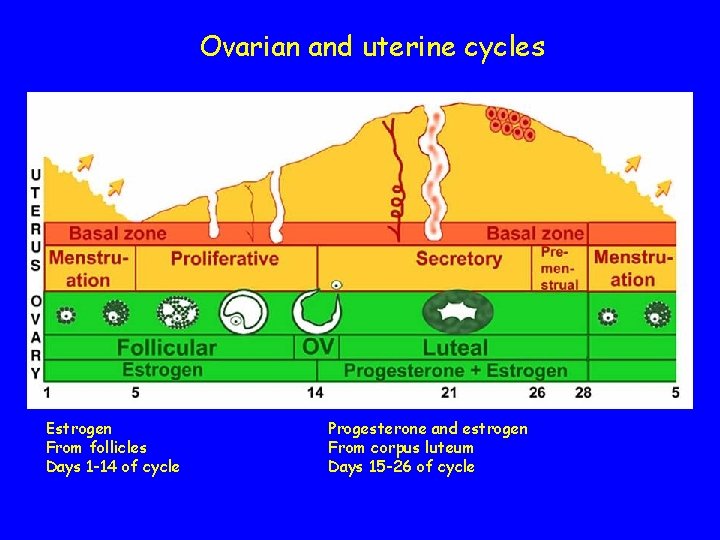
Ovarian and uterine cycles Estrogen From follicles Days 1 -14 of cycle Progesterone and estrogen From corpus luteum Days 15 -26 of cycle
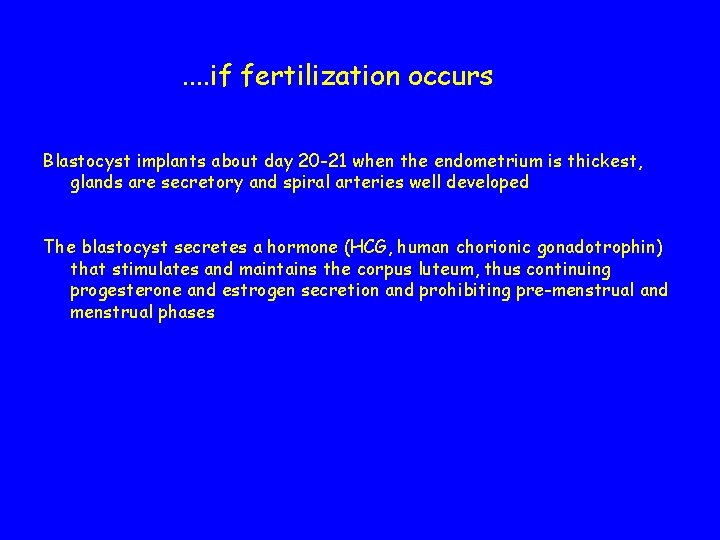
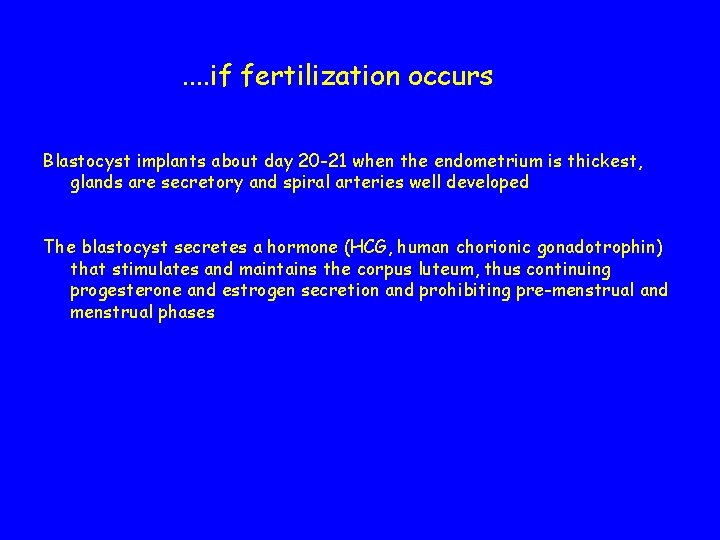
. . if fertilization occurs Blastocyst implants about day 20 -21 when the endometrium is thickest, glands are secretory and spiral arteries well developed The blastocyst secretes a hormone (HCG, human chorionic gonadotrophin) that stimulates and maintains the corpus luteum, thus continuing progesterone and estrogen secretion and prohibiting pre-menstrual and menstrual phases
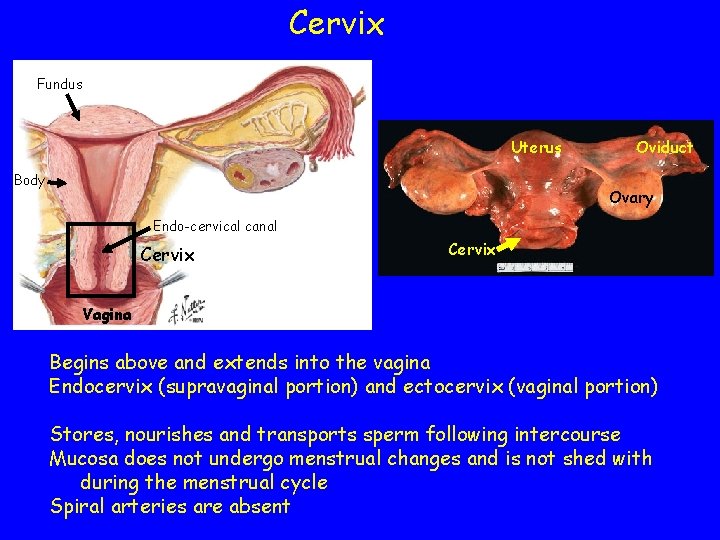
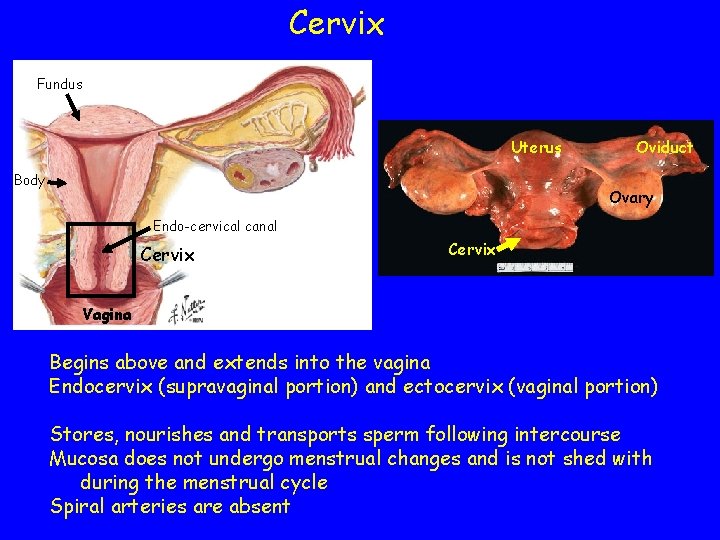
Cervix Fundus Uterus Body Oviduct Ovary Endo-cervical canal Cervix Vagina Begins above and extends into the vagina Endocervix (supravaginal portion) and ectocervix (vaginal portion) Stores, nourishes and transports sperm following intercourse Mucosa does not undergo menstrual changes and is not shed with during the menstrual cycle Spiral arteries are absent
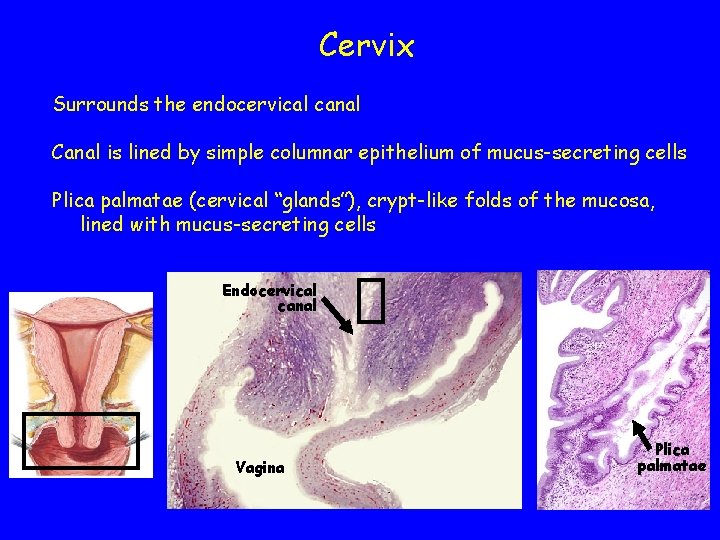
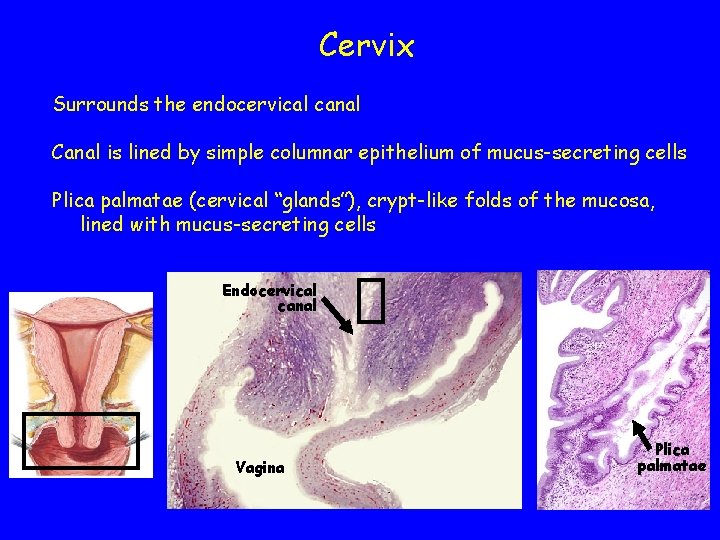
Cervix Surrounds the endocervical canal Canal is lined by simple columnar epithelium of mucus-secreting cells Plica palmatae (cervical “glands”), crypt-like folds of the mucosa, lined with mucus-secreting cells Endocervical canal Vagina Plica palmatae
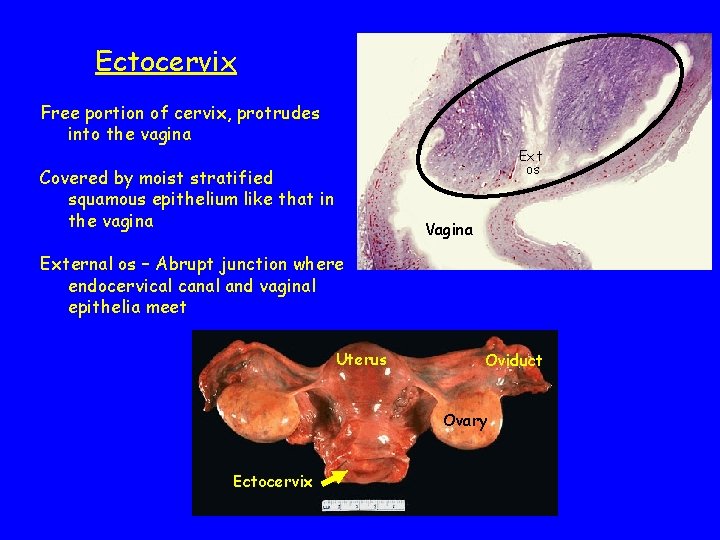
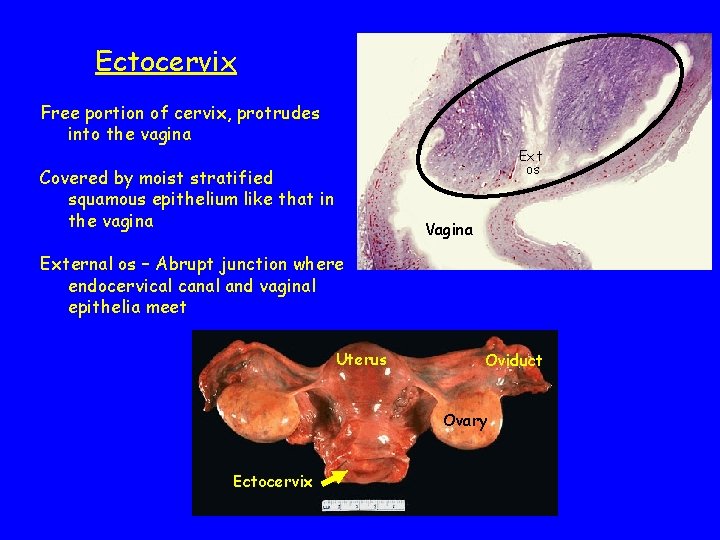
Ectocervix Free portion of cervix, protrudes into the vagina Ext os Covered by moist stratified squamous epithelium like that in the vagina Vagina External os – Abrupt junction where endocervical canal and vaginal epithelia meet Uterus Oviduct Ovary Ectocervix

External os Endocervix Ectocervix External os
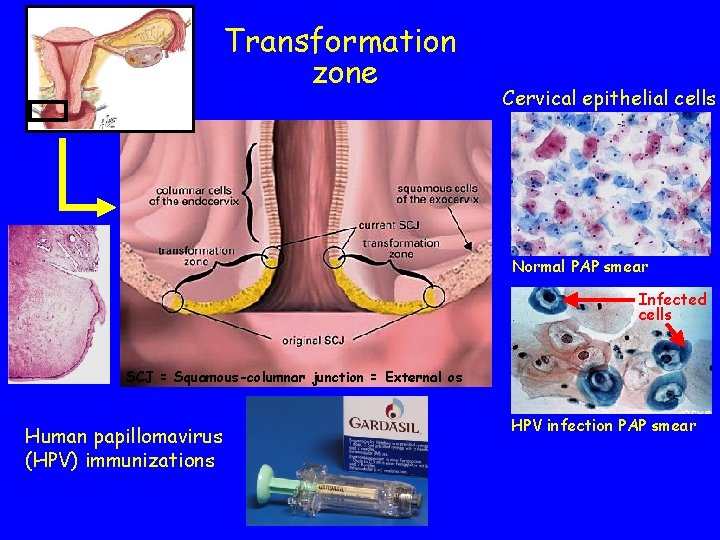
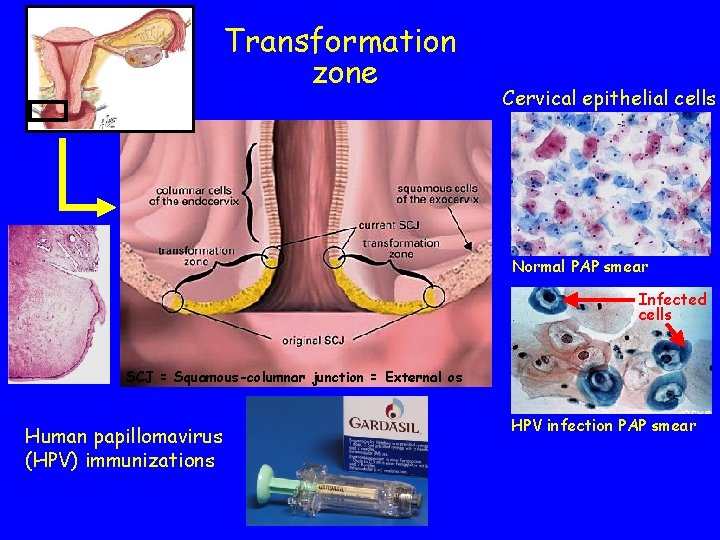
Transformation zone Cervical epithelial cells Normal PAP smear Infected cells SCJ = Squamous-columnar junction = External os Human papillomavirus (HPV) immunizations HPV infection PAP smear
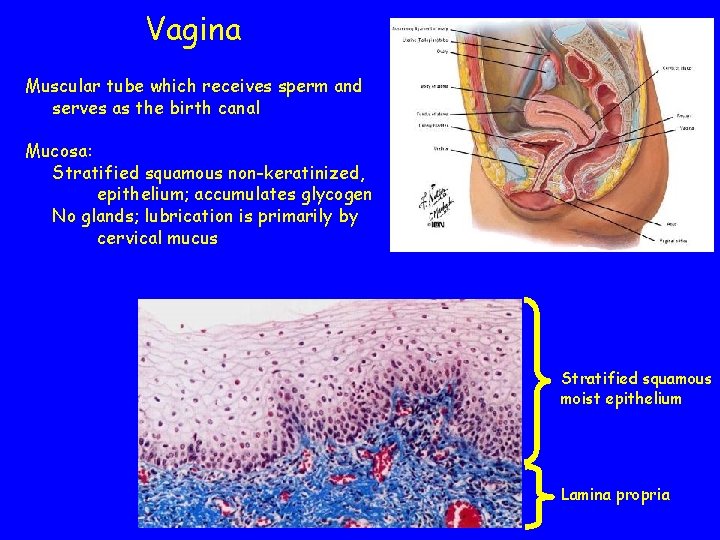
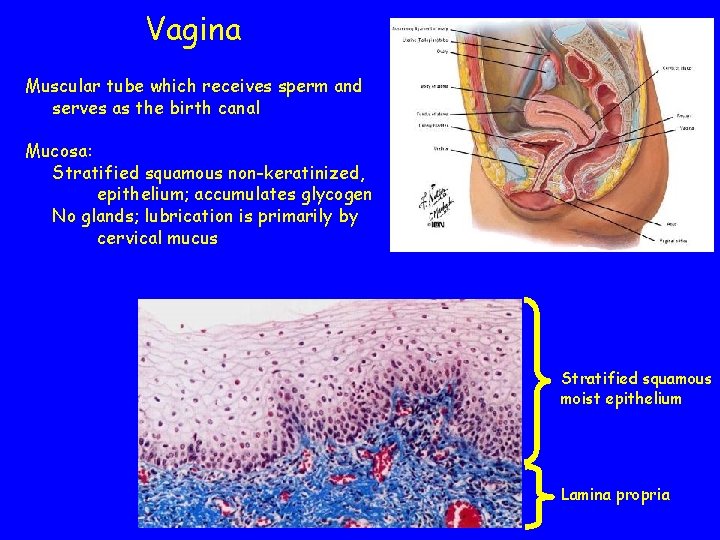
Vagina Muscular tube which receives sperm and serves as the birth canal Mucosa: Stratified squamous non-keratinized, epithelium; accumulates glycogen No glands; lubrication is primarily by cervical mucus Stratified squamous moist epithelium Lamina propria
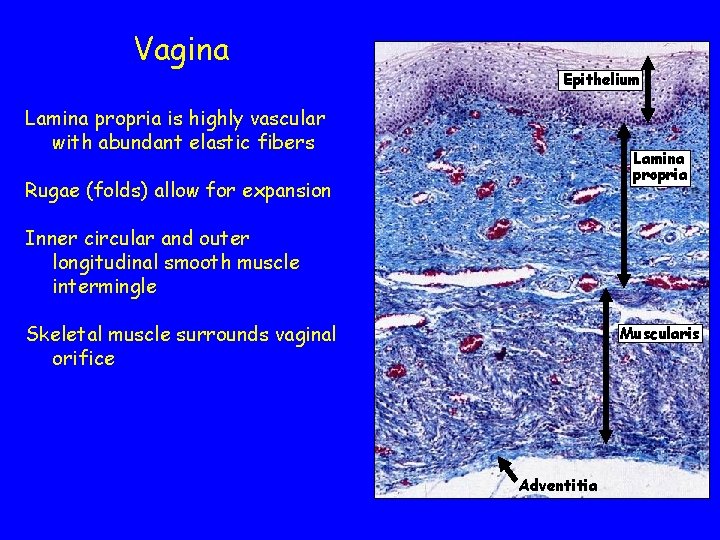
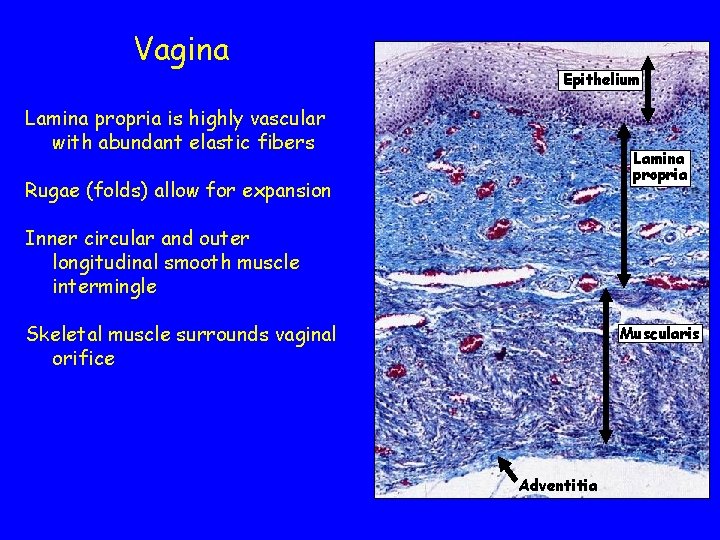
Vagina Epithelium Lamina propria is highly vascular with abundant elastic fibers Lamina propria Rugae (folds) allow for expansion Inner circular and outer longitudinal smooth muscle intermingle Skeletal muscle surrounds vaginal orifice Muscularis Adventitia
Vaginal epithelium Epithelial cells synthesize and accumulate glycogen Bacterial flora in the vagina generate lactic acid from the glycogen, creating an acidic environment (p. H = 4) which protects against vaginal infections.