HISTOLOGY OF LIVER LIVER 2 nd largest organ

- Slides: 37

HISTOLOGY OF LIVER
LIVER 2 nd largest organ of the body Largest gland Location Receives blood from: Portal vein Hepatic artery Drains to: IVC
FUNCTIONS OF LIVER Detoxification of metabolic waste products e. g. de-amination of amino acids to produce urea Destruction of spent RBC’s Synthesis & secretion of bile Synthesis of plasma proteins including albumin & clotting factors Synthesis of plasma lipoproteins Metabolic functions e. g. glycogen synthesis, gluconeogenesis, storage of glycogen, some vitamins & lipids Detoxification of various drugs & toxins e. g. alcohol
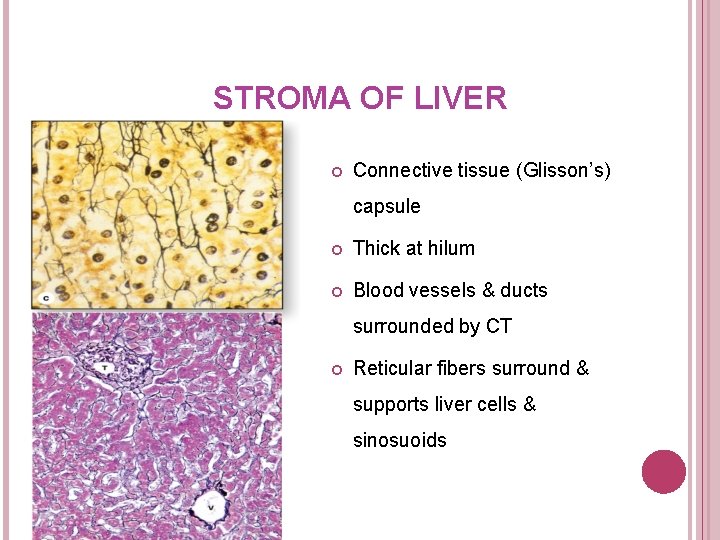
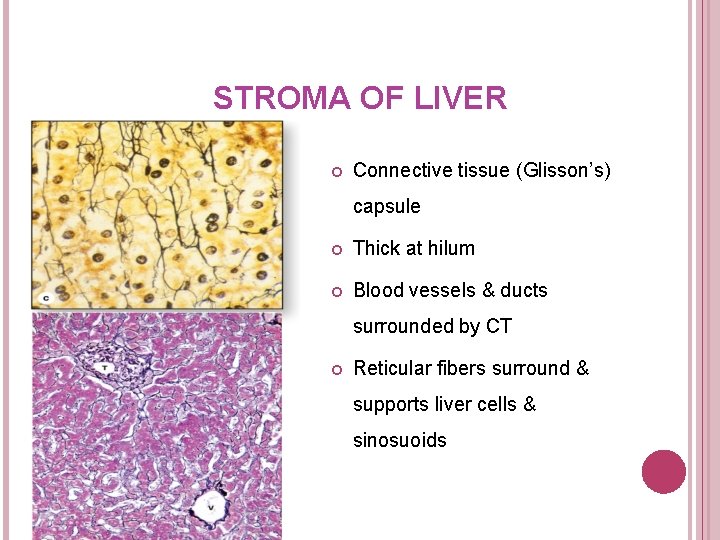
STROMA OF LIVER Connective tissue (Glisson’s) capsule Thick at hilum Blood vessels & ducts surrounded by CT Reticular fibers surround & supports liver cells & sinosuoids
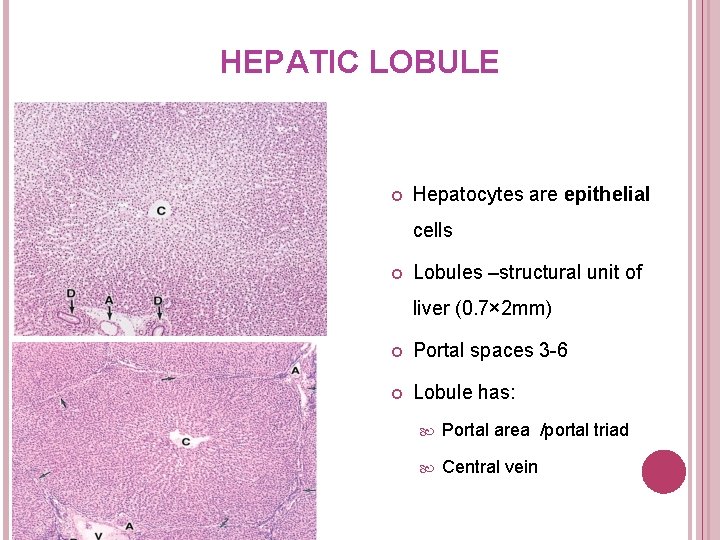
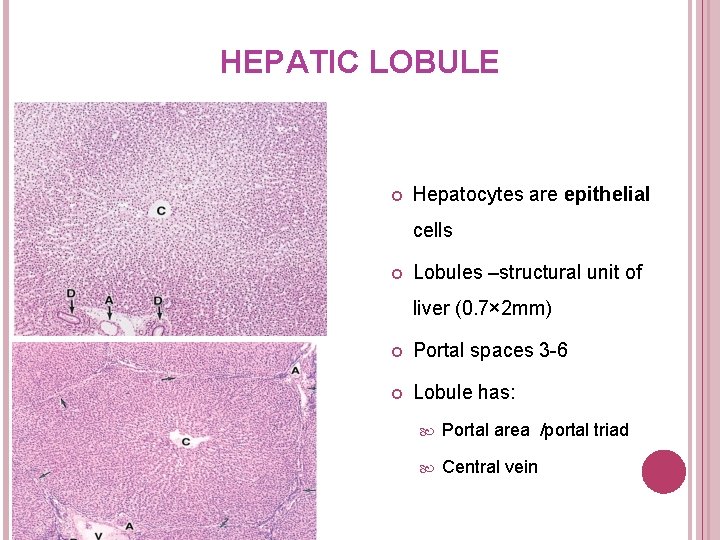
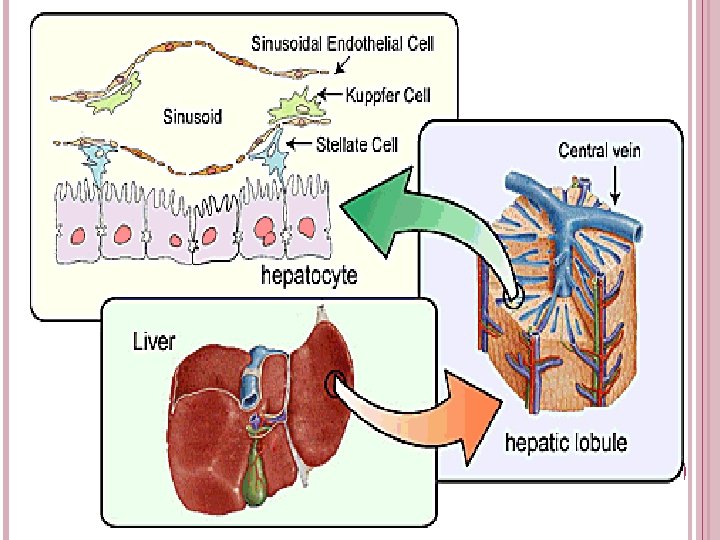
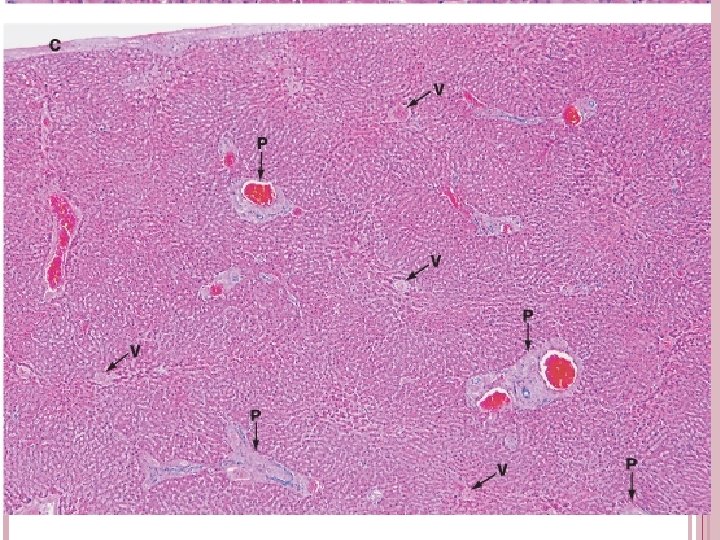
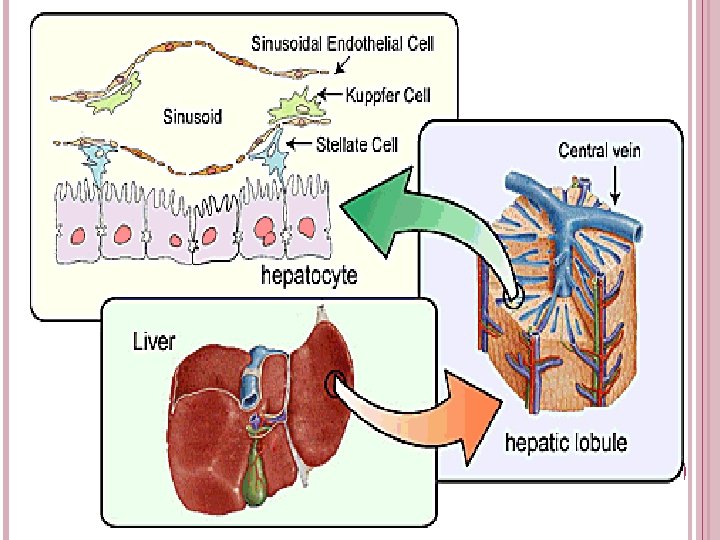
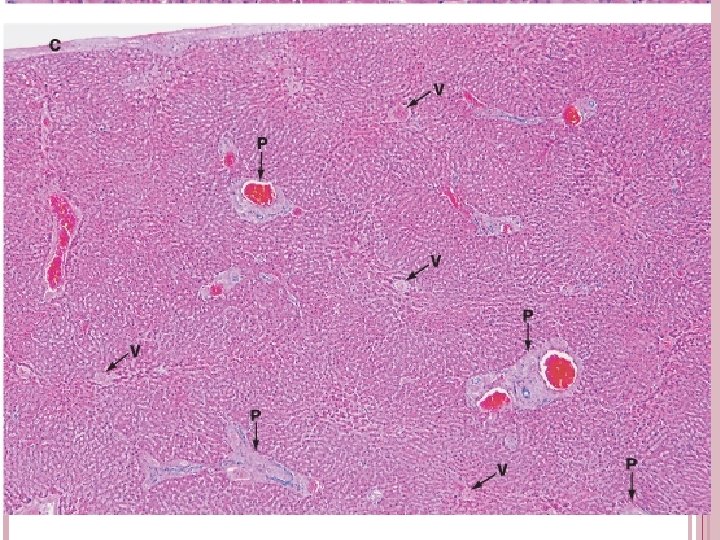
HEPATIC LOBULE Hepatocytes are epithelial cells Lobules –structural unit of liver (0. 7× 2 mm) Portal spaces 3 -6 Lobule has: Portal area /portal triad Central vein
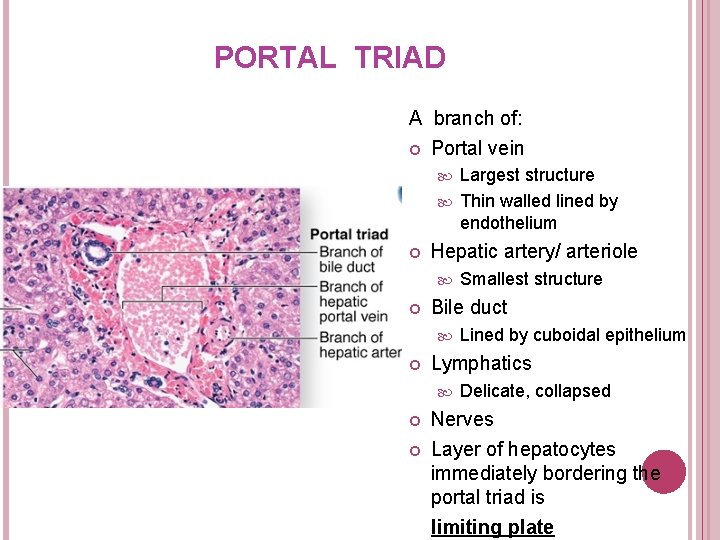
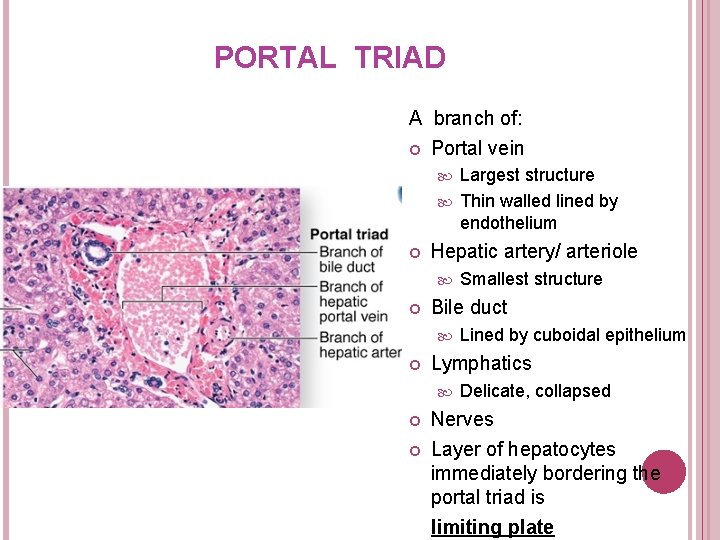
PORTAL TRIAD A branch of: Portal vein Largest structure Thin walled lined by endothelium Hepatic artery/ arteriole Bile duct Lined by cuboidal epithelium Lymphatics Smallest structure Delicate, collapsed Nerves Layer of hepatocytes immediately bordering the portal triad is limiting plate
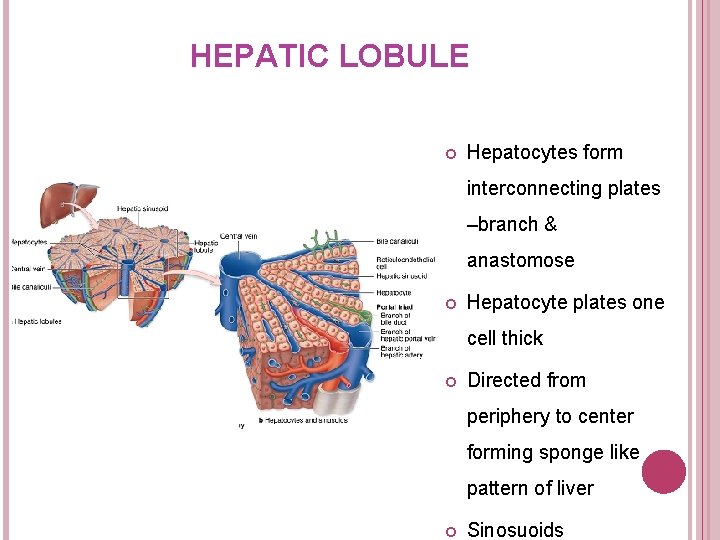
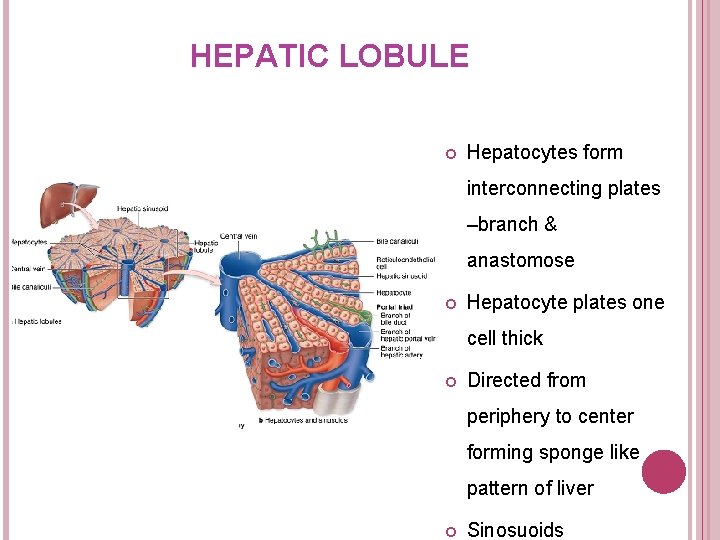
HEPATIC LOBULE Hepatocytes form interconnecting plates –branch & anastomose Hepatocyte plates one cell thick Directed from periphery to center forming sponge like pattern of liver Sinosuoids
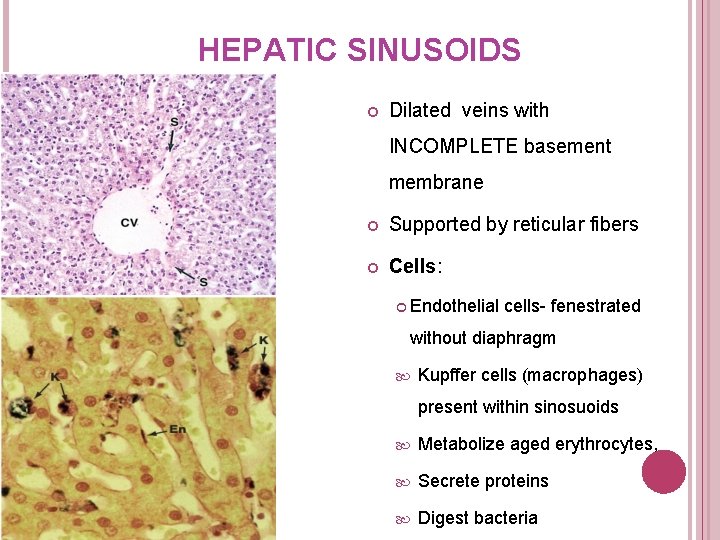
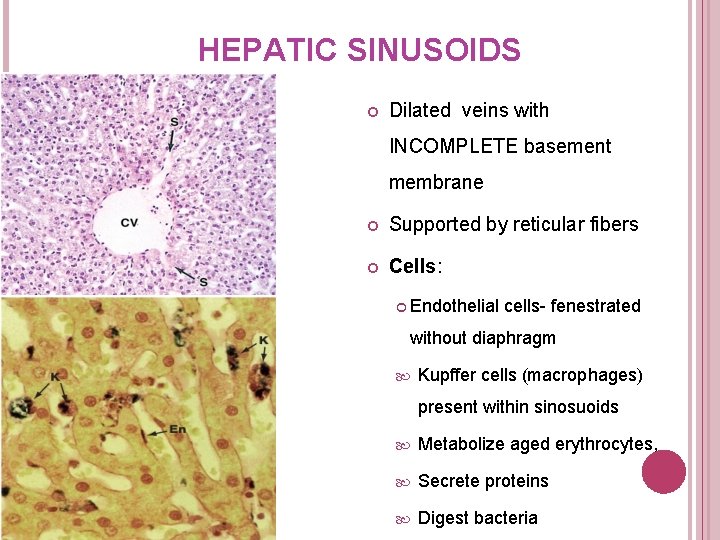
HEPATIC SINUSOIDS Dilated veins with INCOMPLETE basement membrane Supported by reticular fibers Cells: Endothelial cells- fenestrated without diaphragm Kupffer cells (macrophages) present within sinosuoids Metabolize aged erythrocytes, Secrete proteins Digest bacteria
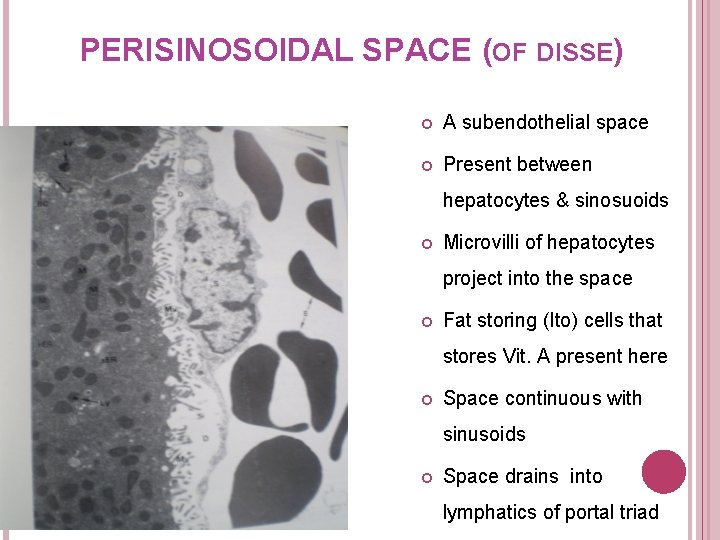
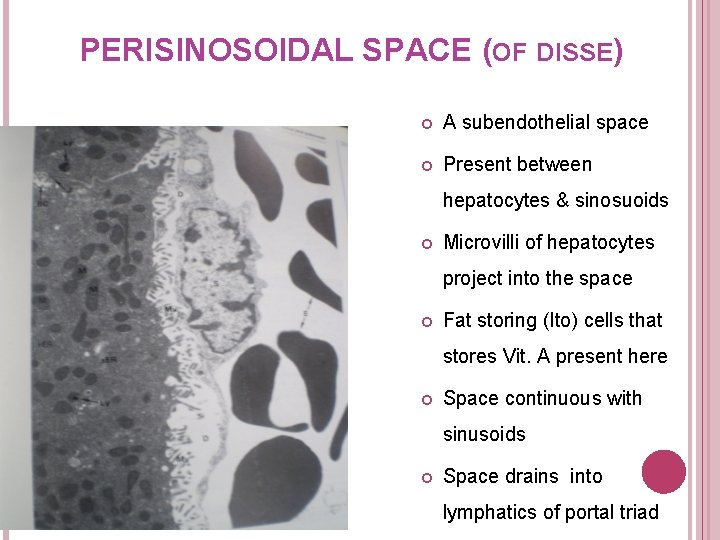
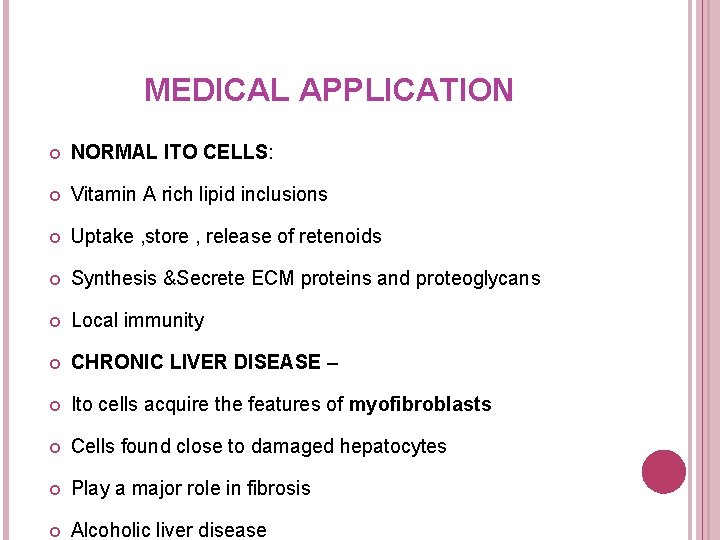
PERISINOSOIDAL SPACE (OF DISSE) A subendothelial space Present between hepatocytes & sinosuoids Microvilli of hepatocytes project into the space Fat storing (Ito) cells that stores Vit. A present here Space continuous with sinusoids Space drains into lymphatics of portal triad
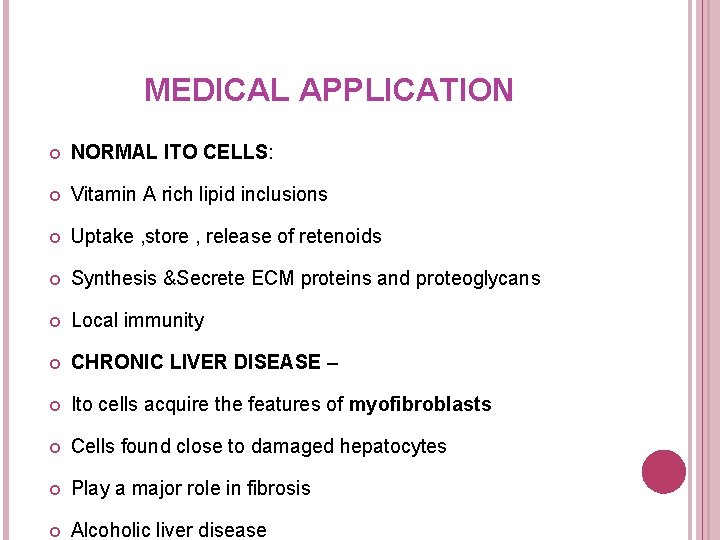
MEDICAL APPLICATION NORMAL ITO CELLS: Vitamin A rich lipid inclusions Uptake , store , release of retenoids Synthesis &Secrete ECM proteins and proteoglycans Local immunity CHRONIC LIVER DISEASE – Ito cells acquire the features of myofibroblasts Cells found close to damaged hepatocytes Play a major role in fibrosis Alcoholic liver disease
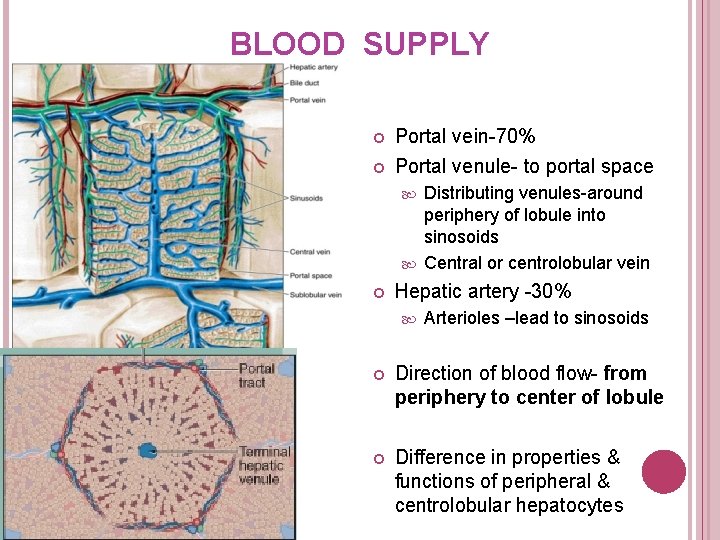
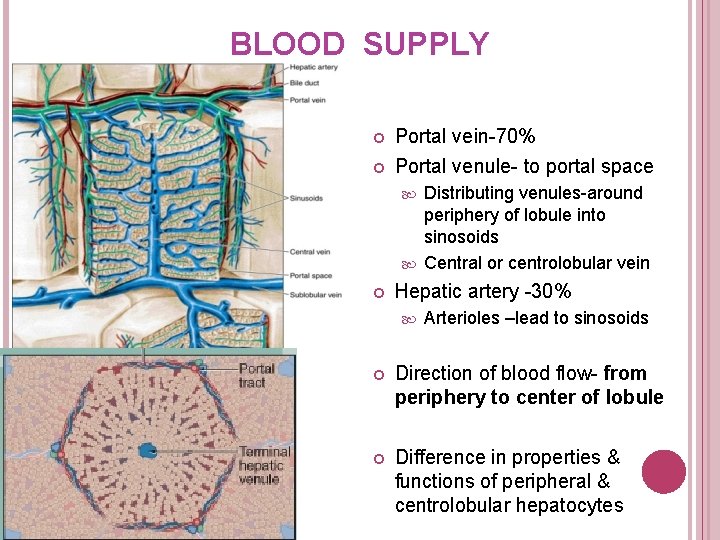
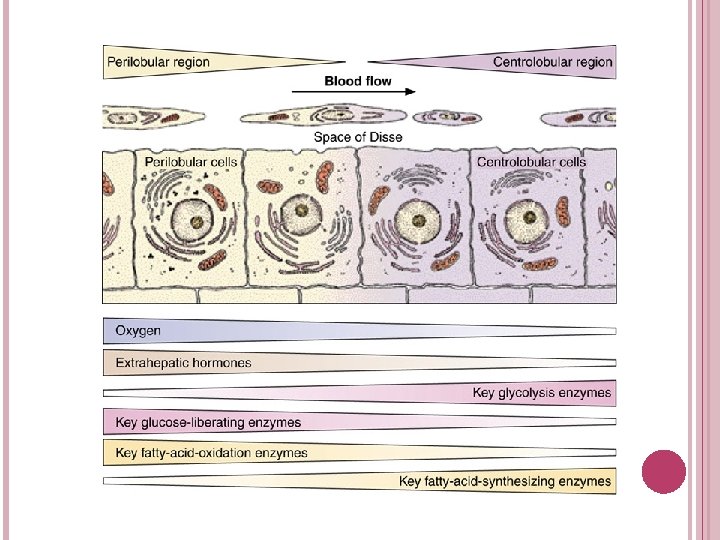
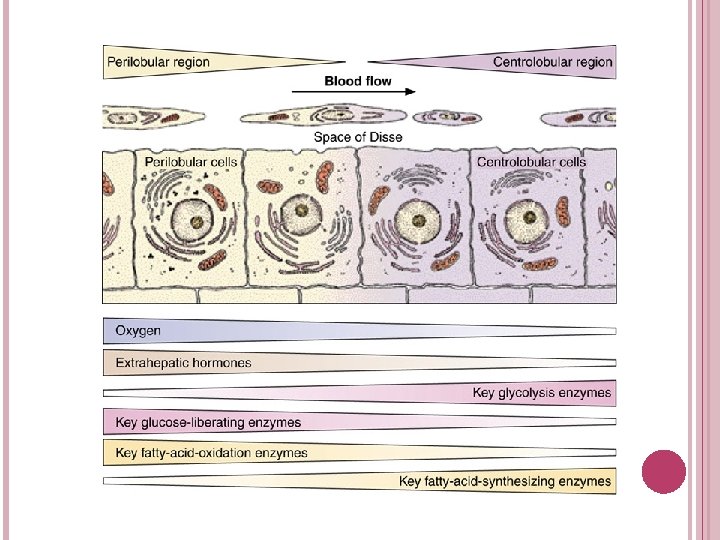
BLOOD SUPPLY Portal vein-70% Portal venule- to portal space Distributing venules-around periphery of lobule into sinosoids Central or centrolobular vein Hepatic artery -30% Arterioles –lead to sinosoids Direction of blood flow- from periphery to center of lobule Difference in properties & functions of peripheral & centrolobular hepatocytes
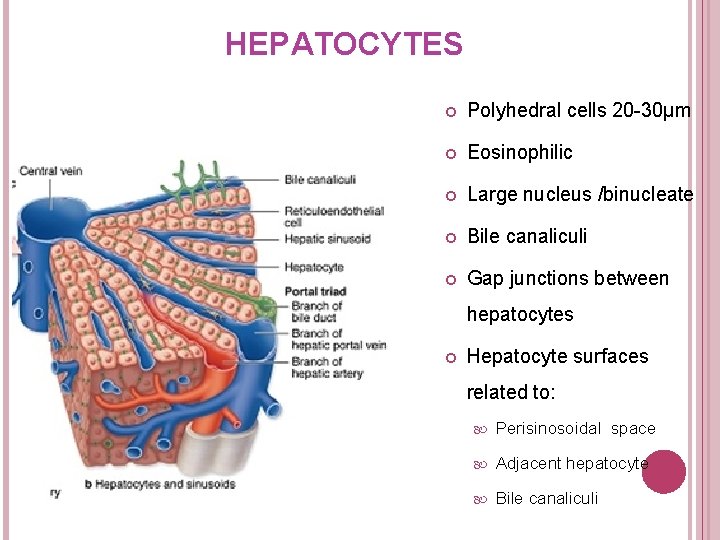
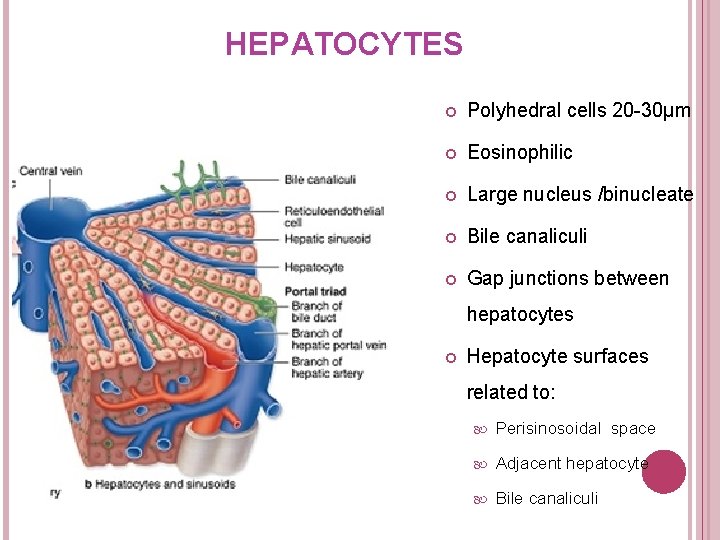
HEPATOCYTES Polyhedral cells 20 -30µm Eosinophilic Large nucleus /binucleate Bile canaliculi Gap junctions between hepatocytes Hepatocyte surfaces related to: Perisinosoidal space Adjacent hepatocyte Bile canaliculi
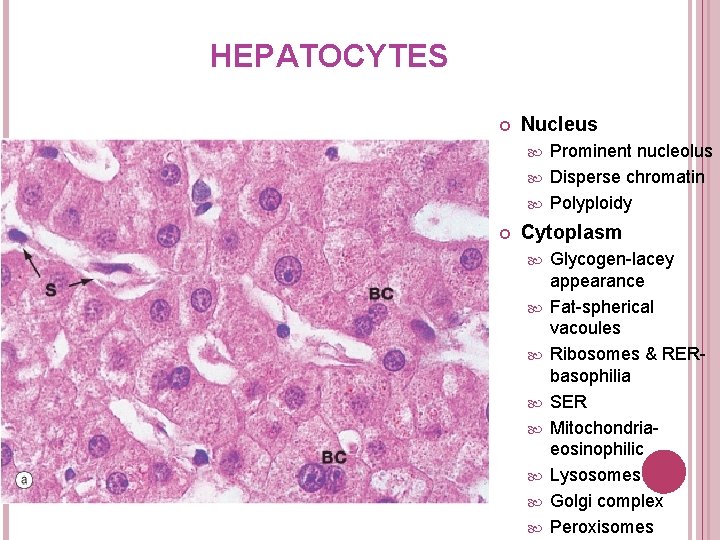
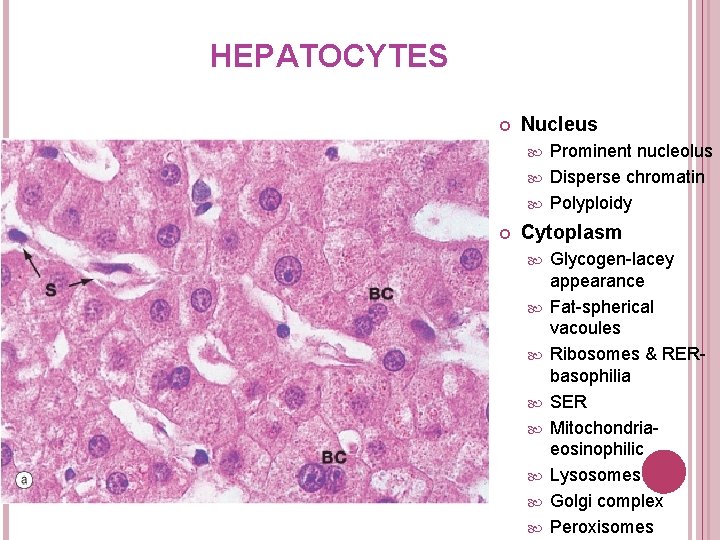
HEPATOCYTES Nucleus Prominent nucleolus Disperse chromatin Polyploidy Cytoplasm Glycogen-lacey appearance Fat-spherical vacoules Ribosomes & RERbasophilia SER Mitochondriaeosinophilic Lysosomes Golgi complex Peroxisomes
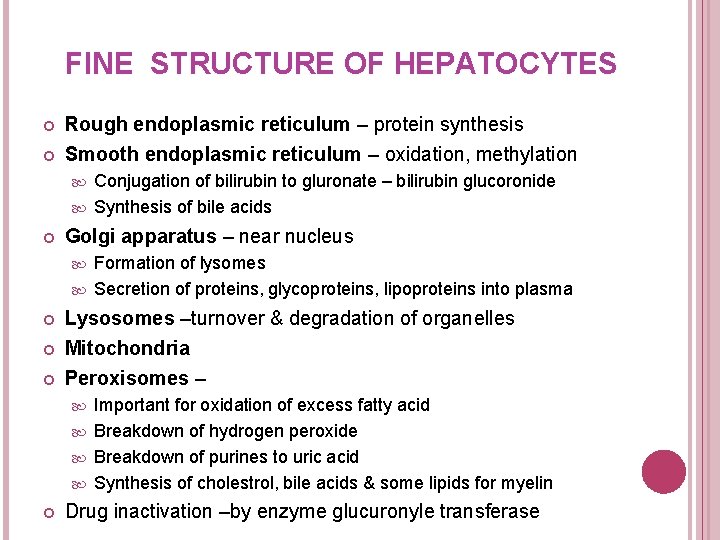
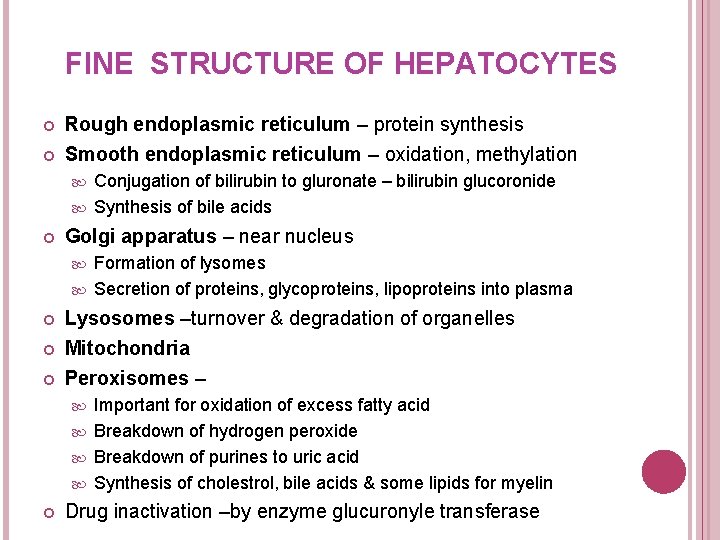
FINE STRUCTURE OF HEPATOCYTES Rough endoplasmic reticulum – protein synthesis Smooth endoplasmic reticulum – oxidation, methylation Conjugation of bilirubin to gluronate – bilirubin glucoronide Synthesis of bile acids Golgi apparatus – near nucleus Formation of lysomes Secretion of proteins, glycoproteins, lipoproteins into plasma Lysosomes –turnover & degradation of organelles Mitochondria Peroxisomes – Important for oxidation of excess fatty acid Breakdown of hydrogen peroxide Breakdown of purines to uric acid Synthesis of cholestrol, bile acids & some lipids for myelin Drug inactivation –by enzyme glucuronyle transferase
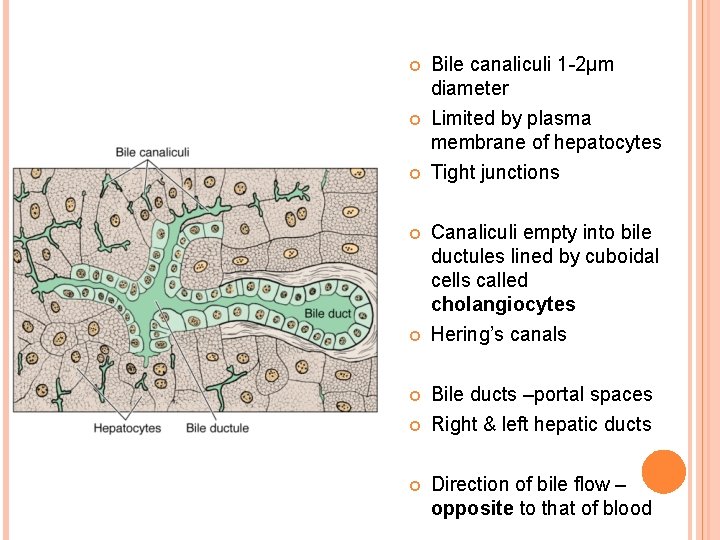
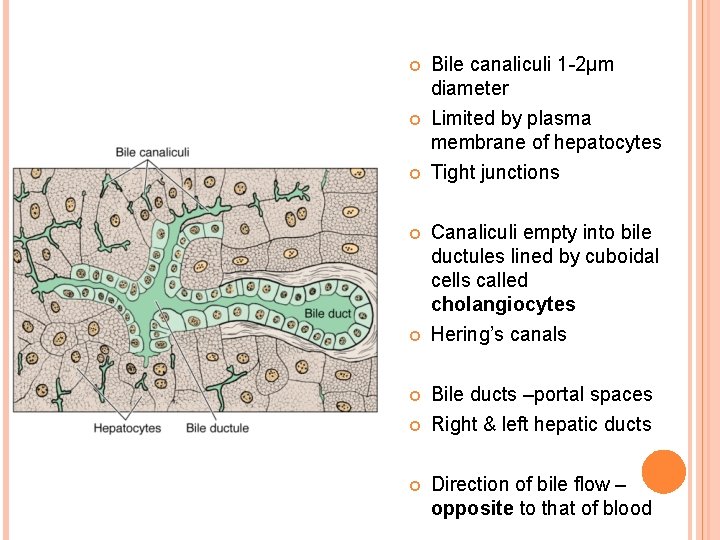
Bile canaliculi 1 -2µm diameter Limited by plasma membrane of hepatocytes Tight junctions Canaliculi empty into bile ductules lined by cuboidal cells called cholangiocytes Hering’s canals Bile ducts –portal spaces Right & left hepatic ducts Direction of bile flow – opposite to that of blood
MEDICAL APPLICATION DISORDER OF PEROXISOME FUNCTION Inherited disorder Mutation of enzymes in peroxisomes. Adrenoleukodystrophy (X-ALD) results from failure to metabolize fatty acids properly Result: Deterioration of myelin sheath of neurons
RBC – heme – unconjugated bilirubin + plasma albumin absrobed by hepatocytes – bilirubin released from albumin – bilirubin + glucoronic acid – bilirubin glucoronide (water soluble) – bile canaliculi Conjugated bilirubin (bilirubin glucoronide) – urobilinogen – urine Urobilinogen – stercobilinogen - intestines
MEDICAL APPLICATION When bilirubin or bilirubin glucuronide is not excreted properly various diseases characterized by JAUNDICE occur Neonatal hyperbilirubinemia – jaundice in newborn Underdeveloped smooth ER Treatment – blue light exposure Unconjugated bilirubin transformed into water soluble photoisomer that can be excreted by kidneys
BILE Exocrine function of liver Consists of: Bile acids – emulsify fats Cholesterol Phospholipids Bilirubin Electrolytes
MEDICAL APPLICATION Gall stone formation (cholelithiasis) Causes Obstructs bile flow Jaundice – presence of bilirubin in blood Rupture of tight junctions around bile canaliculi
MEDICAL APPLICATION Drugs inactivated by liver can induce increase in smooth ER in hepatocytes e. g. barbiturates Barbiturates can increase synthesis of glucuronyltransferase synthesis Use barbiturates in glucuronyltransferase deficiency
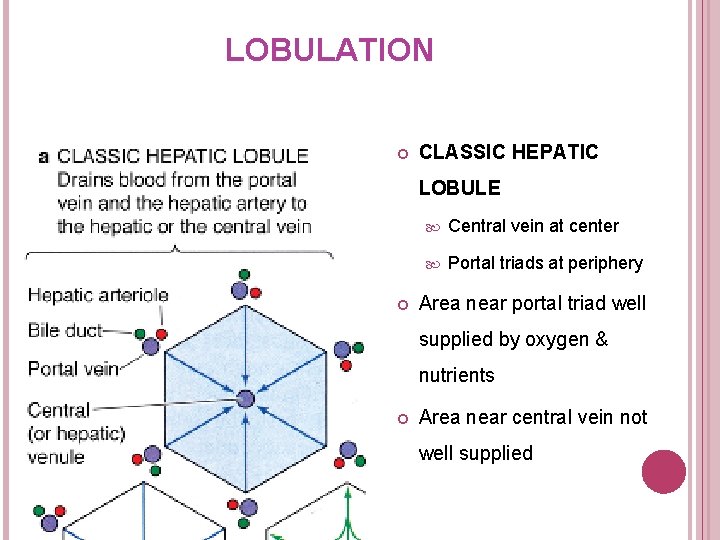
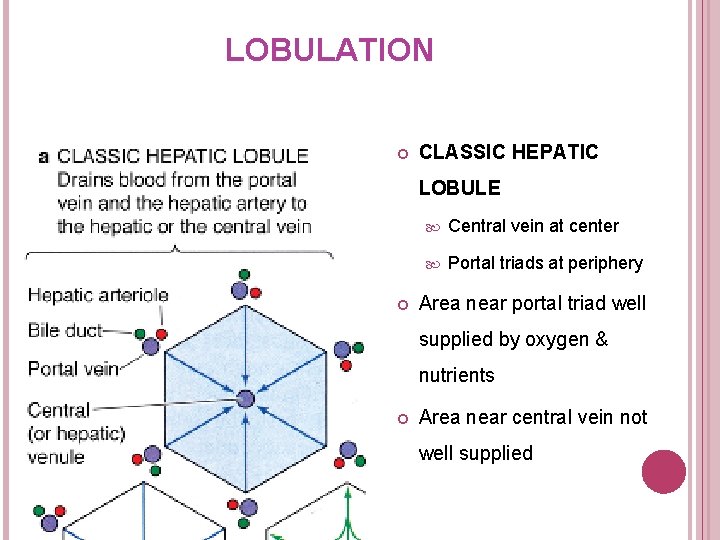
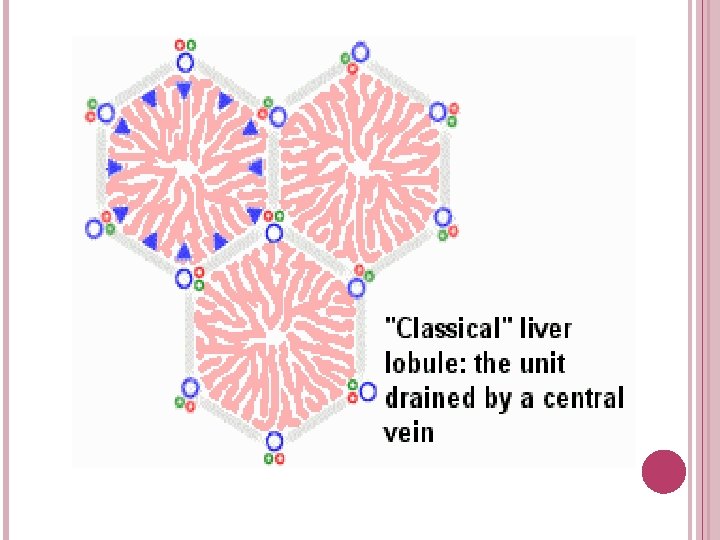
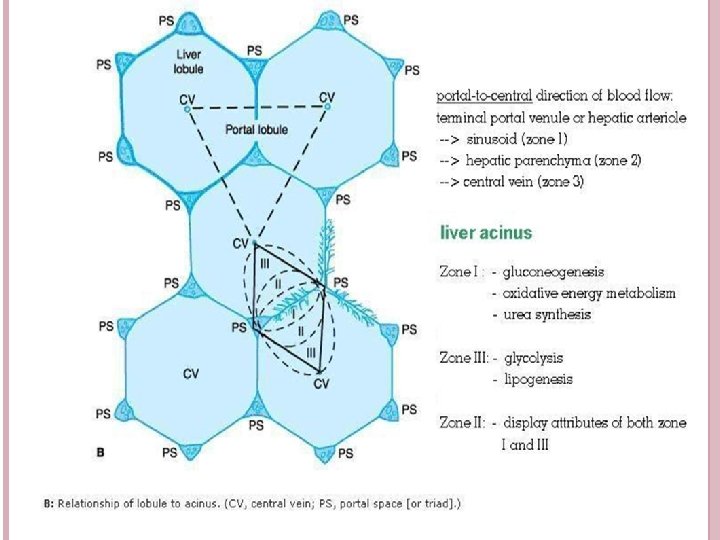
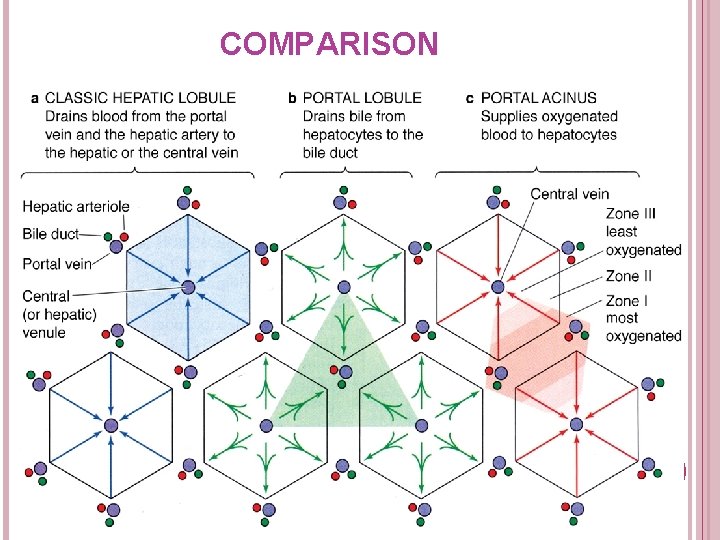
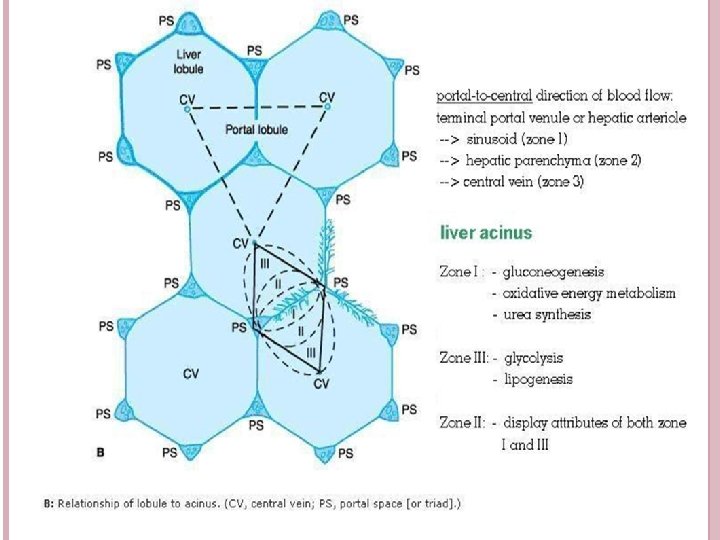
LOBULATION CLASSIC HEPATIC LOBULE Central vein at center Portal triads at periphery Area near portal triad well supplied by oxygen & nutrients Area near central vein not well supplied
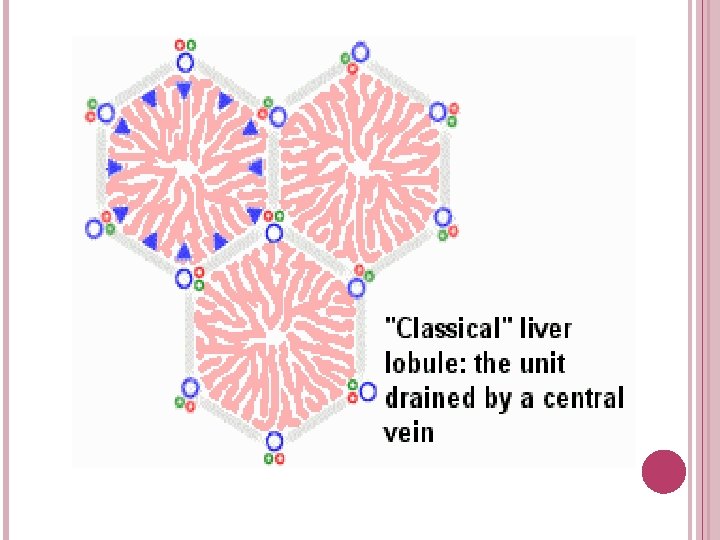
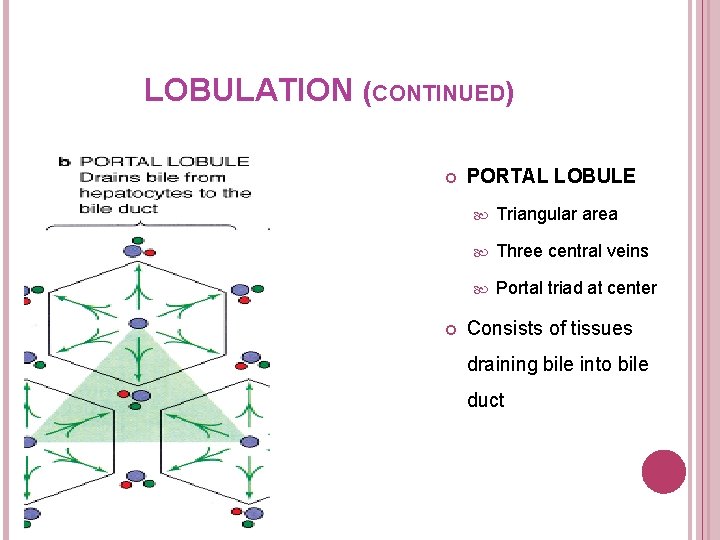
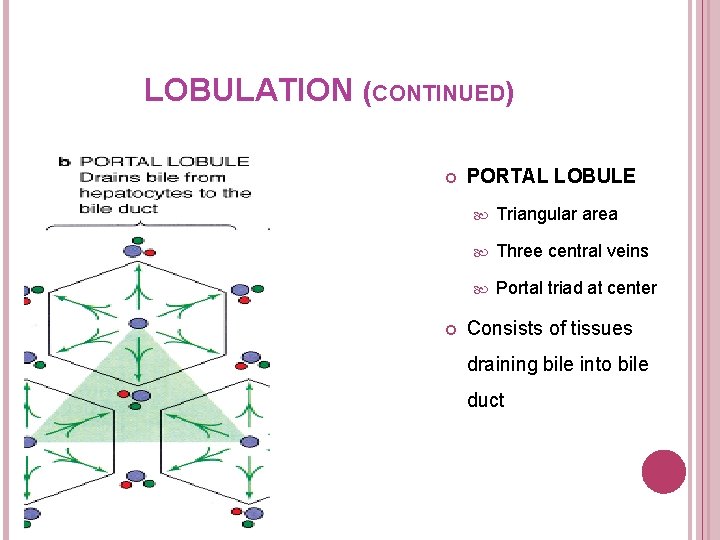
LOBULATION (CONTINUED) PORTAL LOBULE Triangular area Three central veins Portal triad at center Consists of tissues draining bile into bile duct
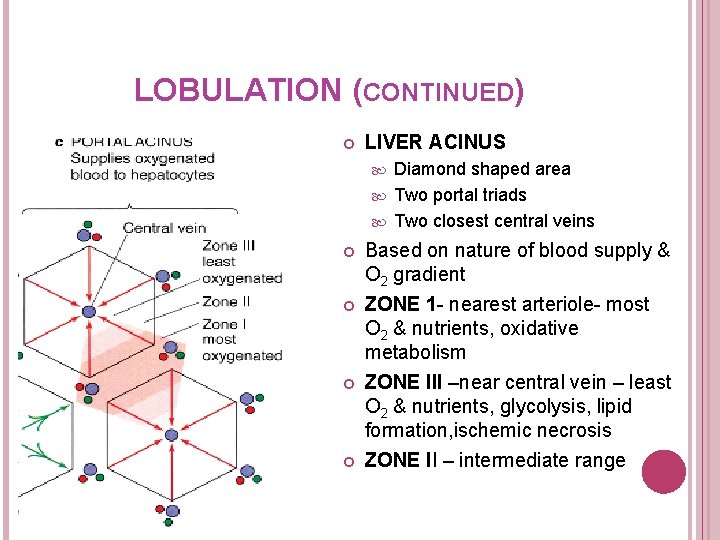
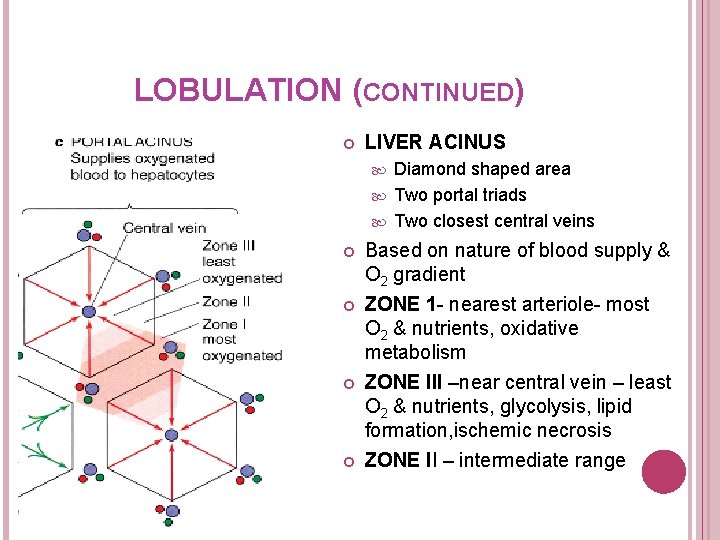
LOBULATION (CONTINUED) LIVER ACINUS Diamond shaped area Two portal triads Two closest central veins Based on nature of blood supply & O 2 gradient ZONE 1 - nearest arteriole- most O 2 & nutrients, oxidative metabolism ZONE III –near central vein – least O 2 & nutrients, glycolysis, lipid formation, ischemic necrosis ZONE II – intermediate range
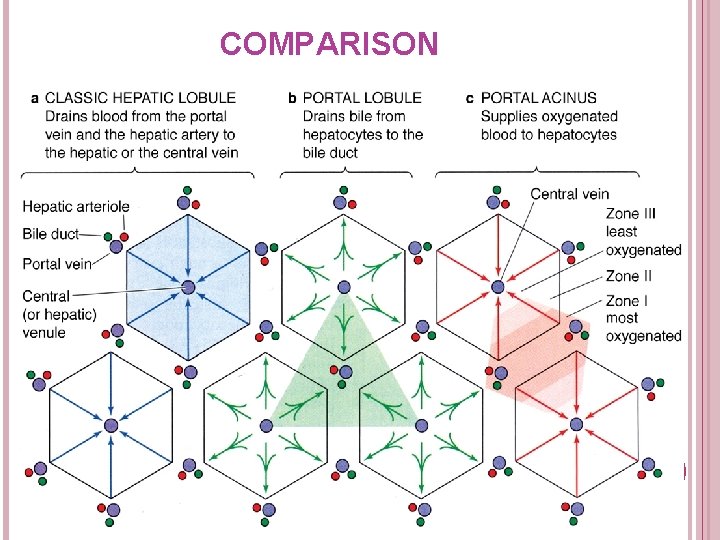
COMPARISON
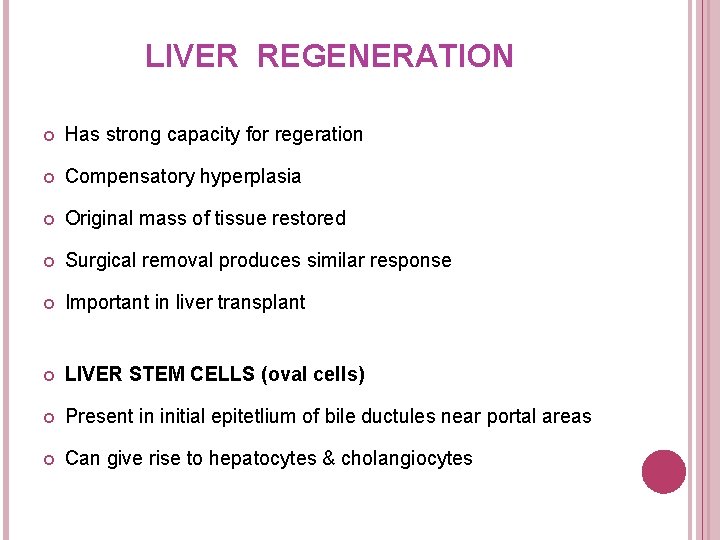
LIVER REGENERATION Has strong capacity for regeration Compensatory hyperplasia Original mass of tissue restored Surgical removal produces similar response Important in liver transplant LIVER STEM CELLS (oval cells) Present in initial epitetlium of bile ductules near portal areas Can give rise to hepatocytes & cholangiocytes
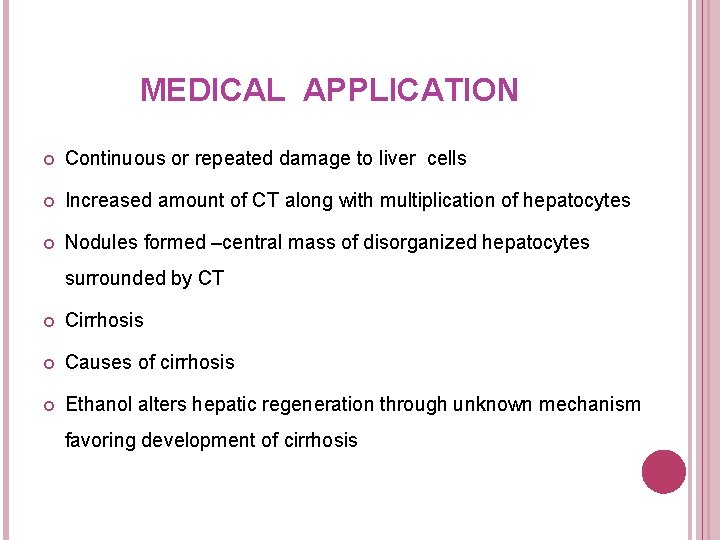
MEDICAL APPLICATION Continuous or repeated damage to liver cells Increased amount of CT along with multiplication of hepatocytes Nodules formed –central mass of disorganized hepatocytes surrounded by CT Cirrhosis Causes of cirrhosis Ethanol alters hepatic regeneration through unknown mechanism favoring development of cirrhosis
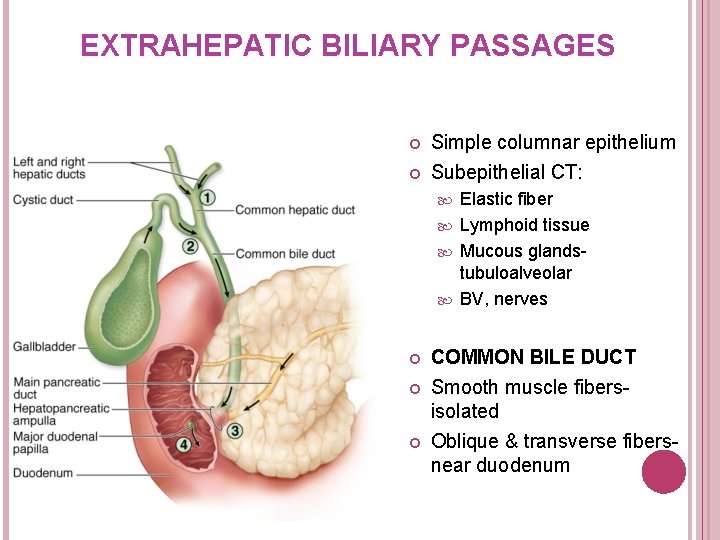
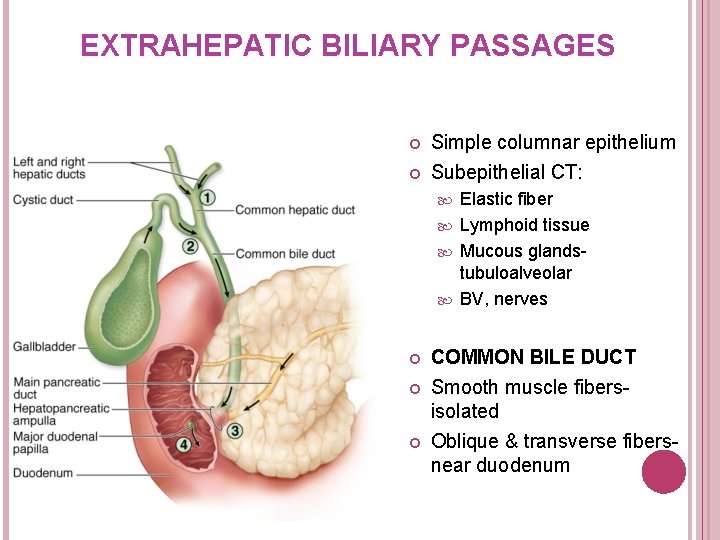
EXTRAHEPATIC BILIARY PASSAGES Simple columnar epithelium Subepithelial CT: Elastic fiber Lymphoid tissue Mucous glandstubuloalveolar BV, nerves COMMON BILE DUCT Smooth muscle fibersisolated Oblique & transverse fibersnear duodenum
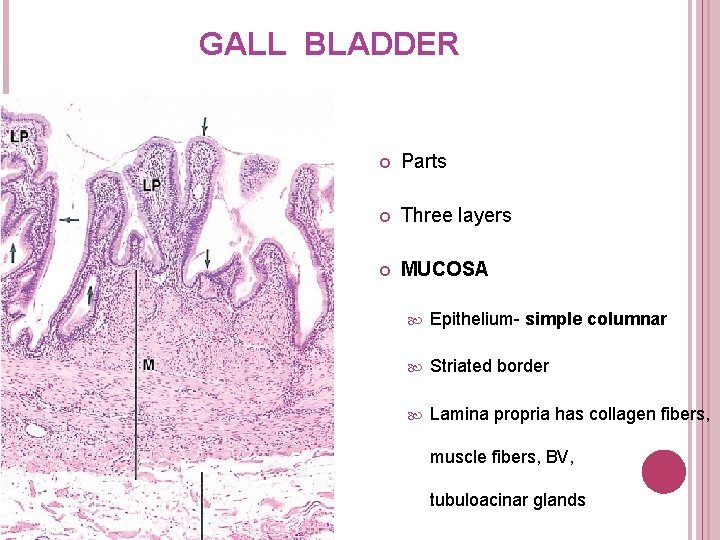
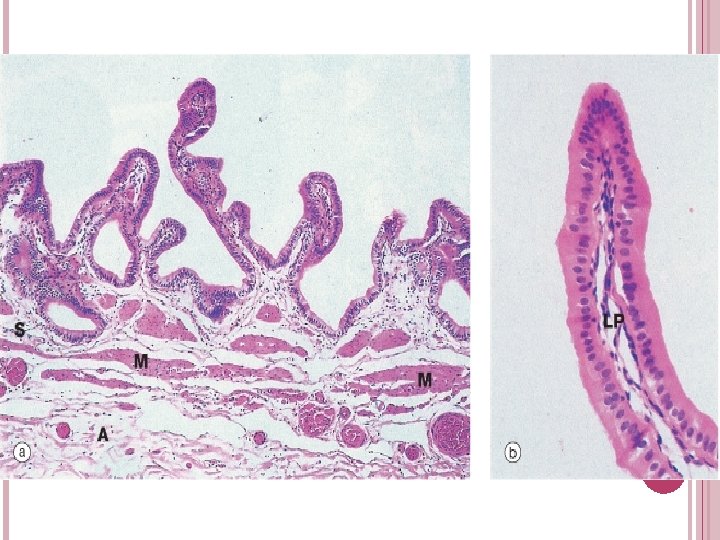
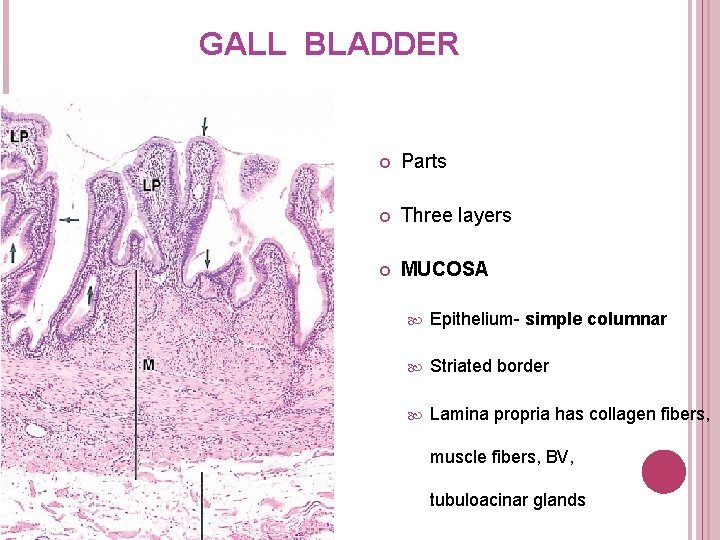
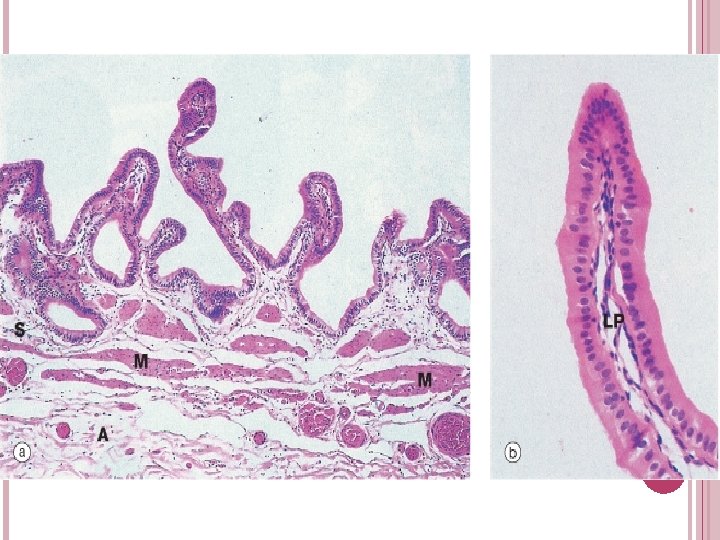
GALL BLADDER Parts Three layers MUCOSA Epithelium- simple columnar Striated border Lamina propria has collagen fibers, muscle fibers, BV, tubuloacinar glands
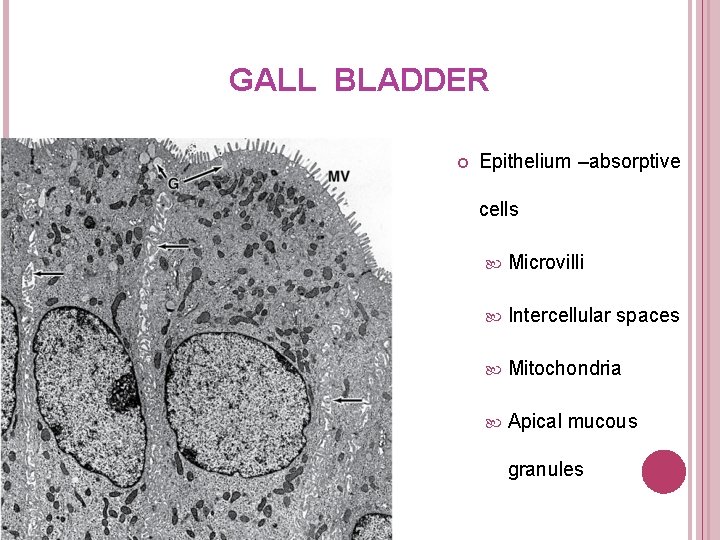
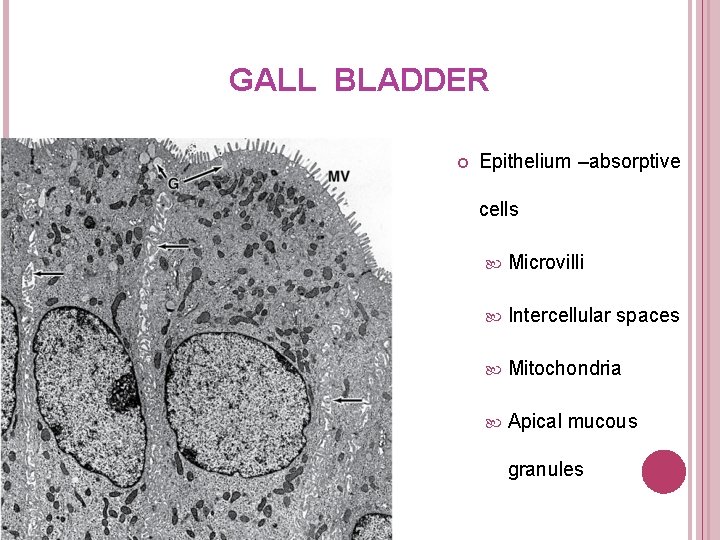
GALL BLADDER Epithelium –absorptive cells Microvilli Intercellular spaces Mitochondria Apical mucous granules
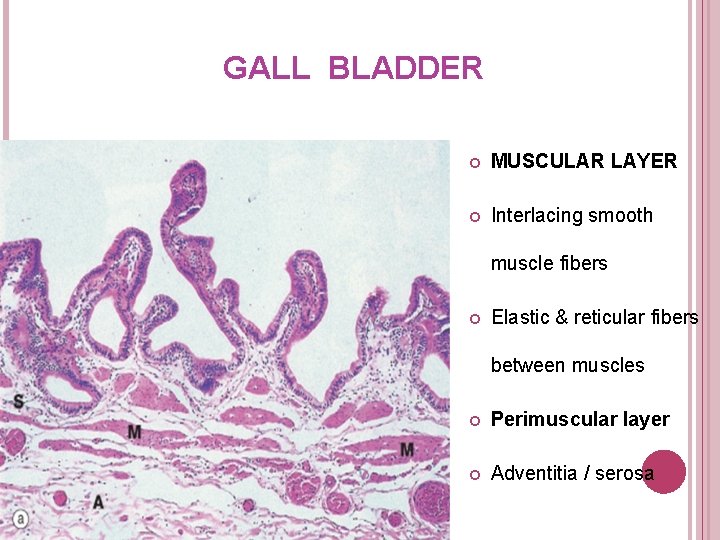
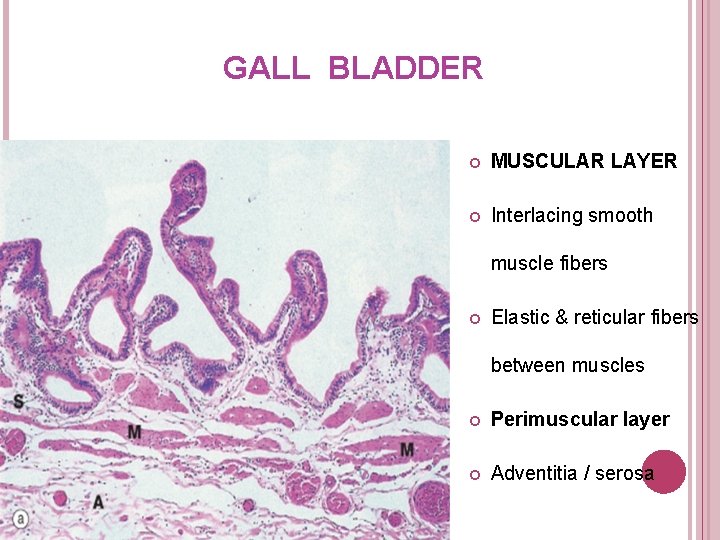
GALL BLADDER MUSCULAR LAYER Interlacing smooth muscle fibers Elastic & reticular fibers between muscles Perimuscular layer Adventitia / serosa