Histology for Pathology Gastrointestinal System and Exocrine Pancreas
- Slides: 25
Histology for Pathology Gastrointestinal System and Exocrine Pancreas Theresa Kristopaitis, MD Associate Professor Director of Mechanisms of Human Disease Kelli A. Hutchens, MD, FCAP Assistant Professor Assistant Director of Mechanisms of Human Disease Loyola Stritch School of Medicine
Objectives • On H&E stained sections, identify the four general layers of the digestive tract organs (esophagus, stomach, small bowel, colon): Mucosa; submucosa; muscularis externa, and adventitia/serosa • On H&E stained sections identify the following components of the mucosa: epithelium, lamina propria, muscularis mucosa • Describe the components of the submucosal layer of the digestive organs • Explain the location of Meissner plexus vs Auerbach plexus and describe the function of each • Name the type of epithelium comprising the mucosa of the esophagus, stomach, small bowel, appendix, colon and anal canal. • Identify submucosal glands in the esophagus and describe their function. • Describe the composition of the esophagogastric junction • Name the four parts of the stomach. • Identify gastric pits and explain their function. • On high power H&E stained sections distinguish parietal cells from chief cells. List the substances secreted by each of the cells.
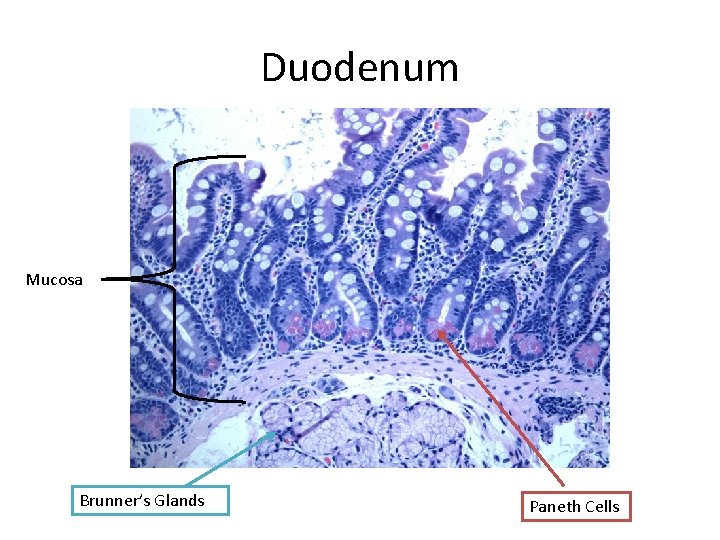
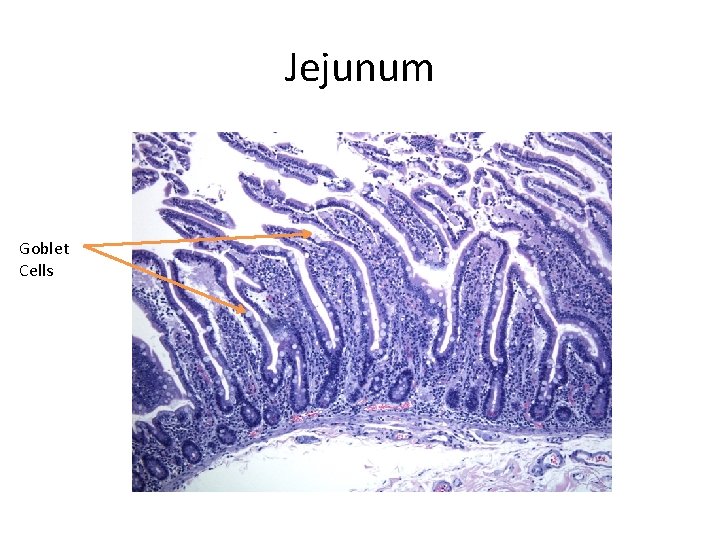
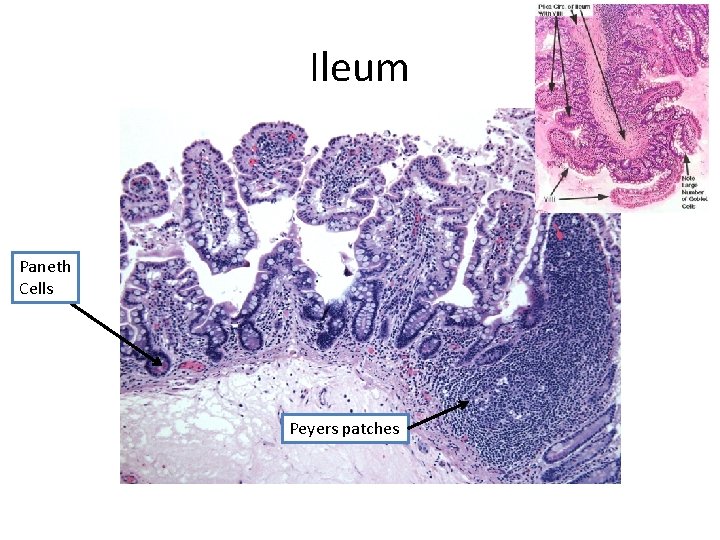
Objectives Identify the following key components of the small intestine: Duodenum: villi, Brunner glands Jejunum: villi, goblet cells Ileum: villi, goblet cells, Peyer patches Define Crypts (or Glands) of Lieberkuhn. Contrast vili vs plicae circulares On H&E stained sections distinguish colon from small intestine. Define taenia coli. In H&E stained sections of pancreas distinguish the endocrine components of the pancreas from the exocrine components. • In H&E stained sections of pancreas identify pancreatic acinar cells vs ducts. • • •
Oral Cavity • Inner surface of the lips, cheeks, soft palate, surface of tongue, and floor of the mouth – Nonkeratinized stratified squamous epithelium – Lamina propria – Submucosa • Gingiva and hard palate – Keratinized stratified squamous epithelium – Lamina propria • Tongue: specialized mucosa with papillae
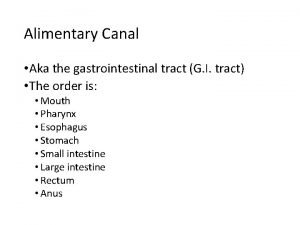
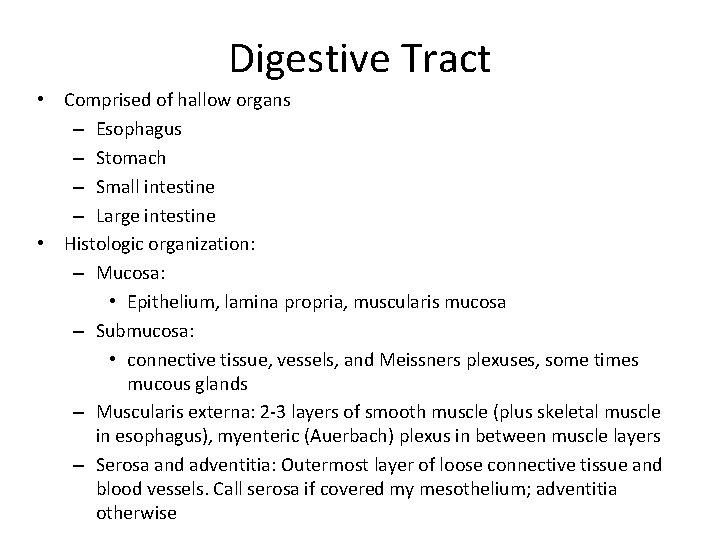
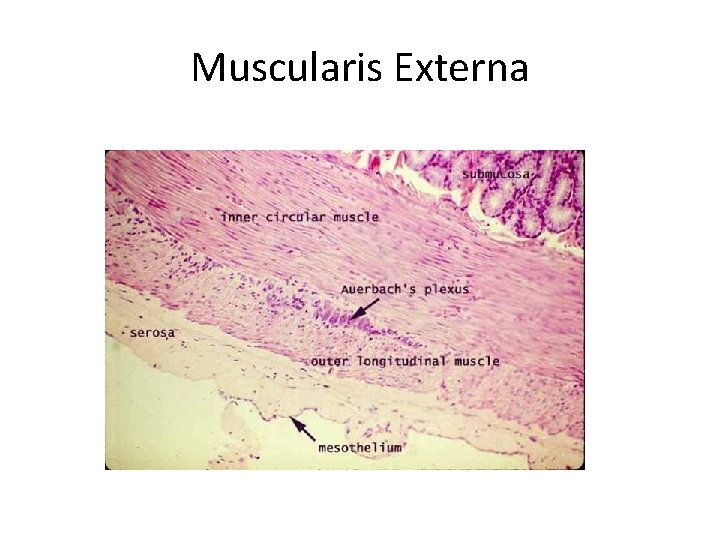
Digestive Tract • Comprised of hallow organs – Esophagus – Stomach – Small intestine – Large intestine • Histologic organization: – Mucosa: • Epithelium, lamina propria, muscularis mucosa – Submucosa: • connective tissue, vessels, and Meissners plexuses, some times mucous glands – Muscularis externa: 2 -3 layers of smooth muscle (plus skeletal muscle in esophagus), myenteric (Auerbach) plexus in between muscle layers – Serosa and adventitia: Outermost layer of loose connective tissue and blood vessels. Call serosa if covered my mesothelium; adventitia otherwise
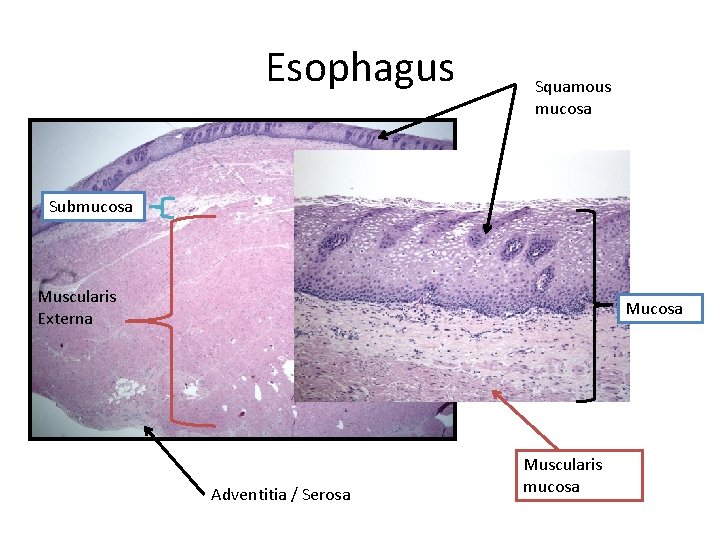
Esophagus • Mucosa: non-keratinizing stratified squamous • Submucosa: contains mucous glands – Increased mucous glands at lower esophagus (GE junction) to protect esophagus from gastric juices • Muscularis externa: inner circular and outer longitudinal – Contains skeletal muscle fibers
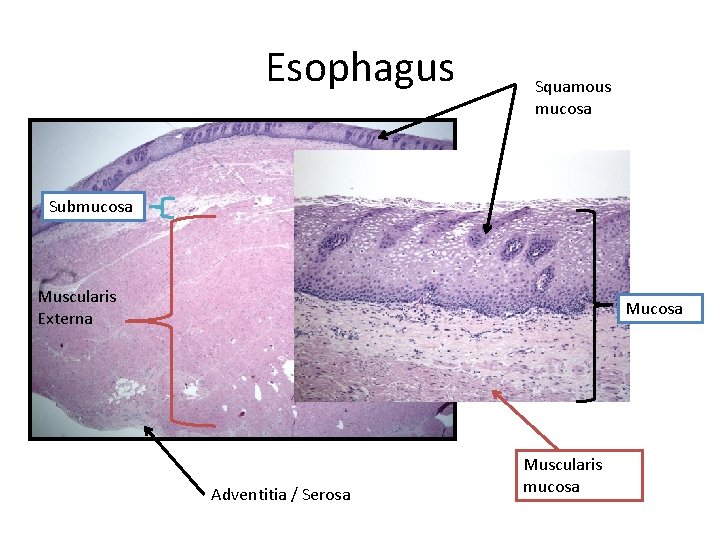
Esophagus Squamous mucosa Submucosa Muscularis Externa Mucosa Adventitia / Serosa Muscularis mucosa
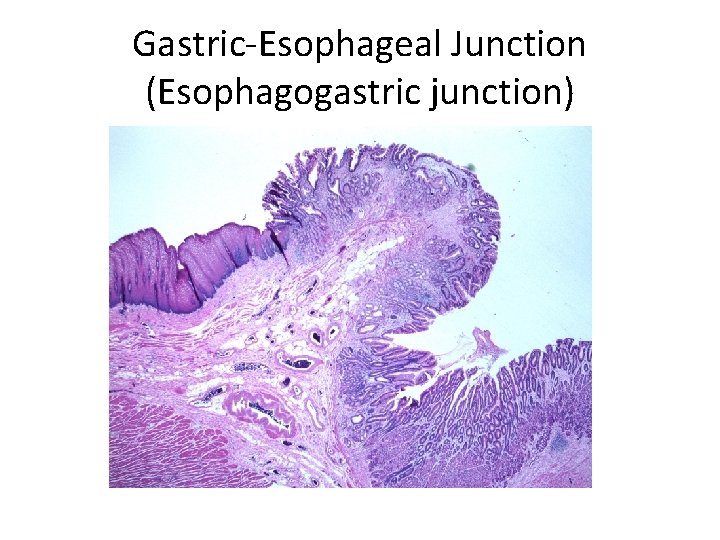
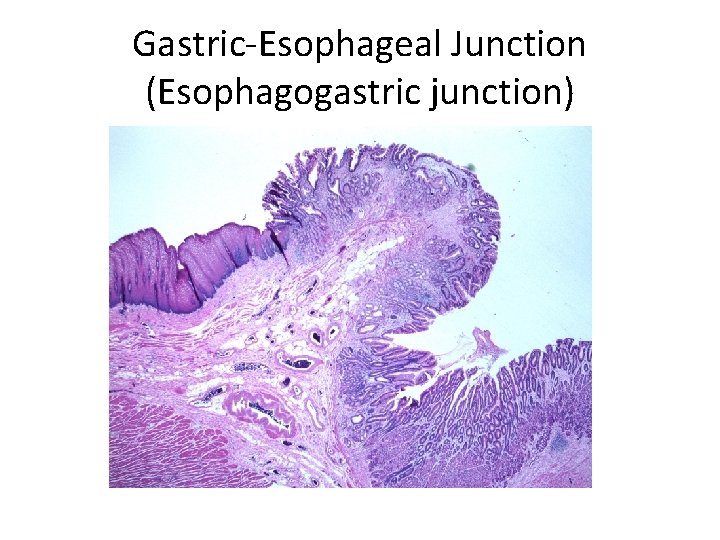
Gastric-Esophageal Junction (Esophagogastric junction)
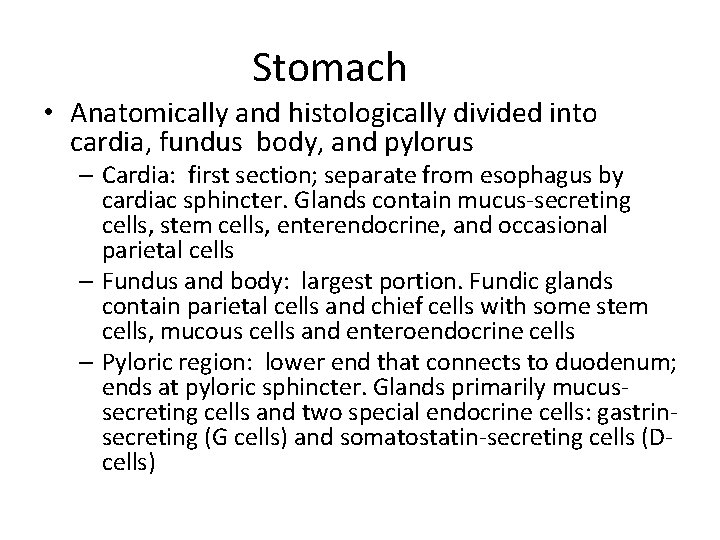
Stomach • Anatomically and histologically divided into cardia, fundus body, and pylorus – Cardia: first section; separate from esophagus by cardiac sphincter. Glands contain mucus-secreting cells, stem cells, enterendocrine, and occasional parietal cells – Fundus and body: largest portion. Fundic glands contain parietal cells and chief cells with some stem cells, mucous cells and enteroendocrine cells – Pyloric region: lower end that connects to duodenum; ends at pyloric sphincter. Glands primarily mucussecreting cells and two special endocrine cells: gastrinsecreting (G cells) and somatostatin-secreting cells (Dcells)
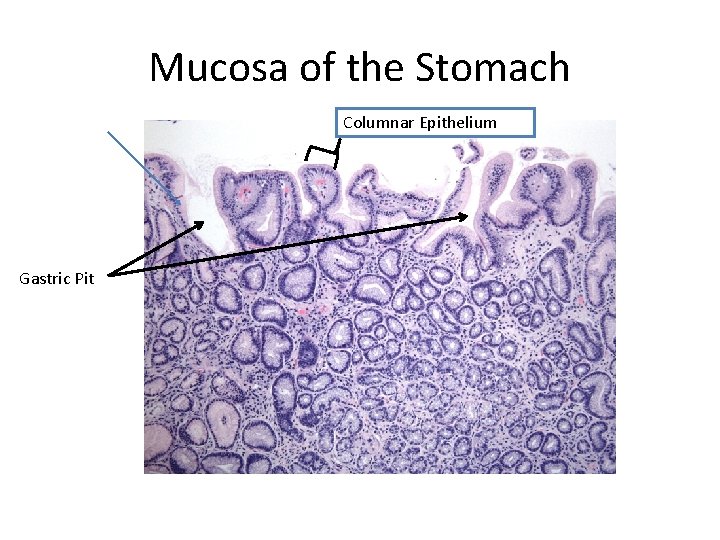
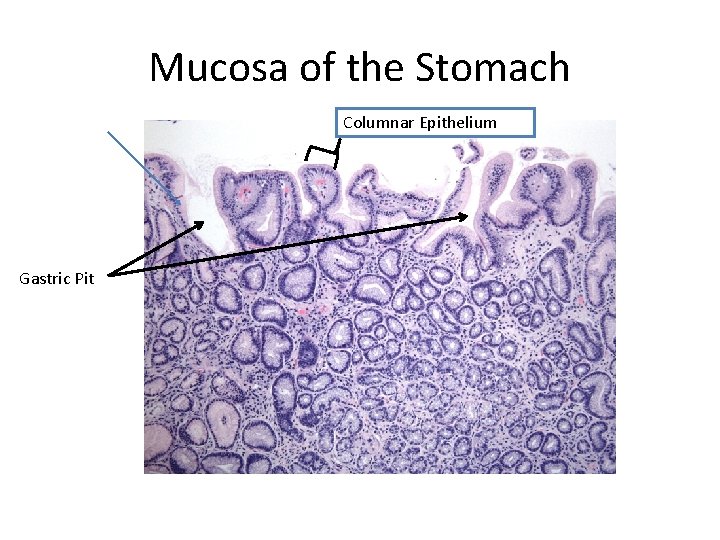
Mucosa of the Stomach Columnar Epithelium Gastric Pit
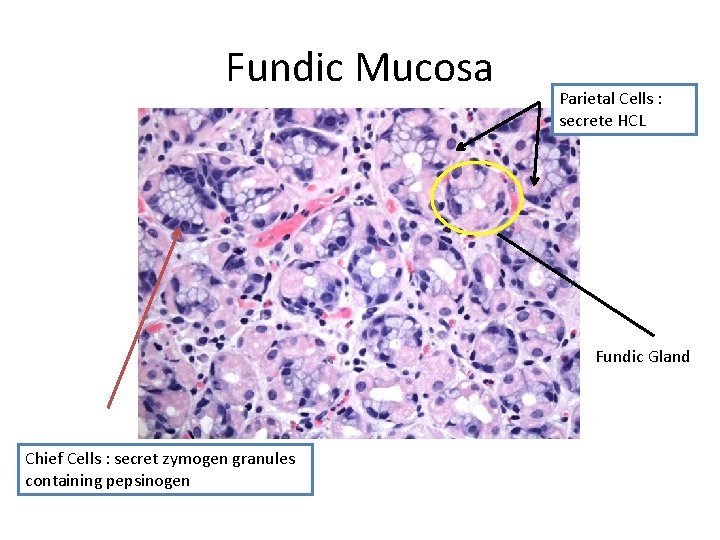
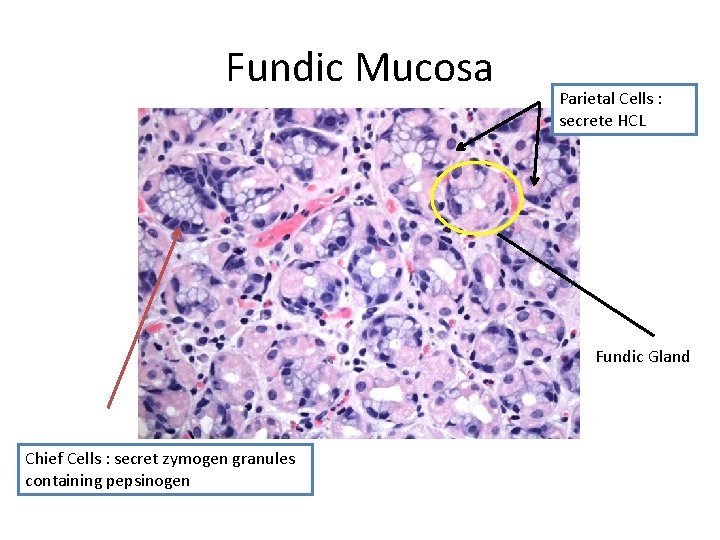
Fundic Mucosa Parietal Cells : secrete HCL Fundic Gland Chief Cells : secret zymogen granules containing pepsinogen
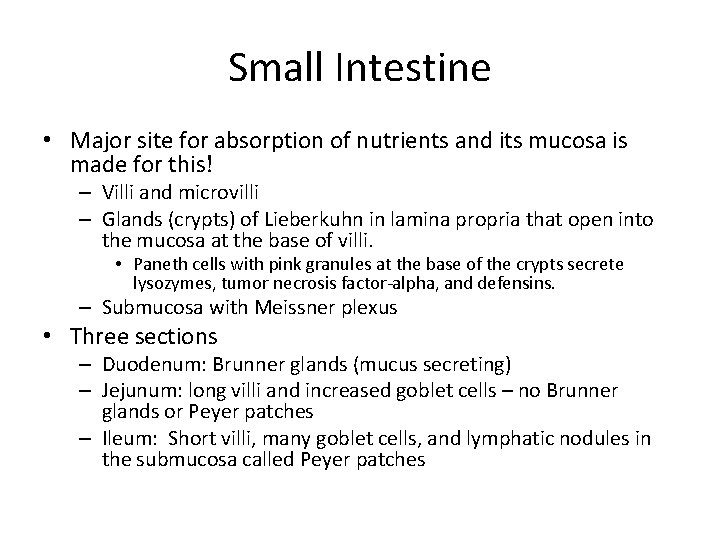
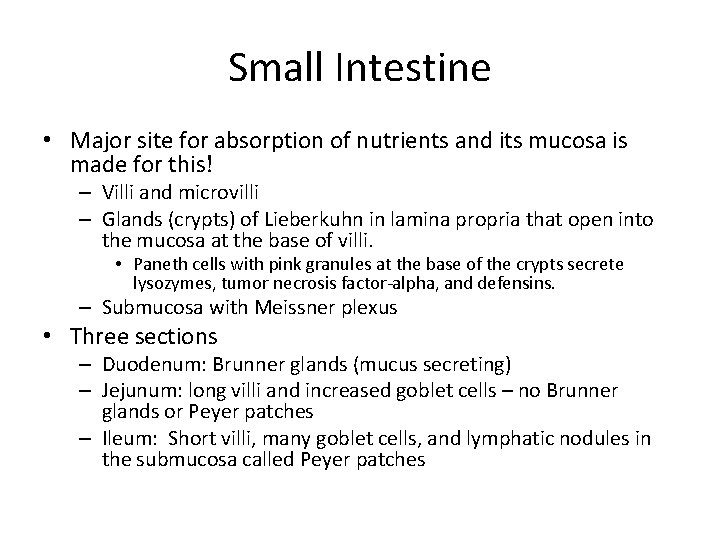
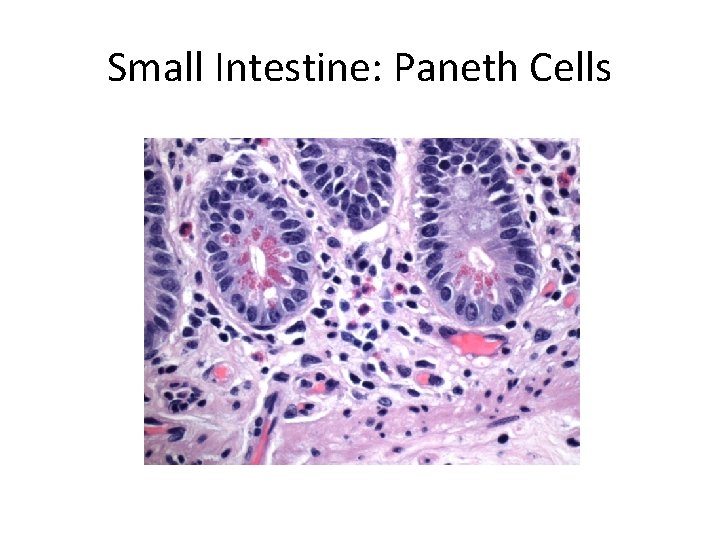
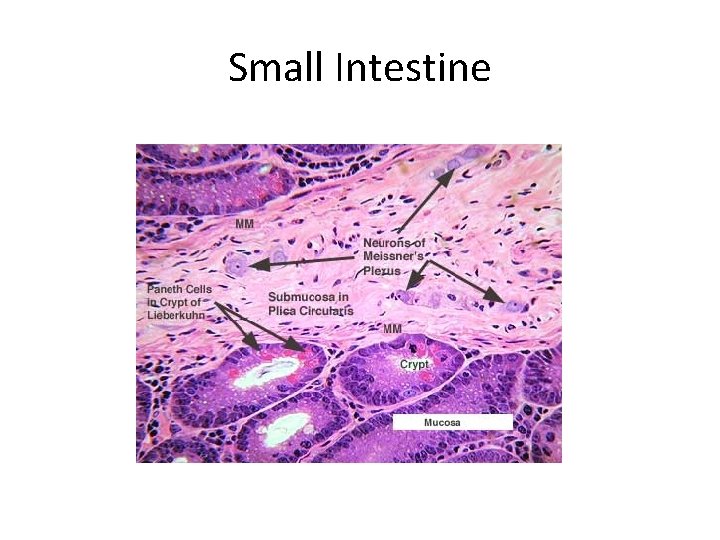
Small Intestine • Major site for absorption of nutrients and its mucosa is made for this! – Villi and microvilli – Glands (crypts) of Lieberkuhn in lamina propria that open into the mucosa at the base of villi. • Paneth cells with pink granules at the base of the crypts secrete lysozymes, tumor necrosis factor-alpha, and defensins. – Submucosa with Meissner plexus • Three sections – Duodenum: Brunner glands (mucus secreting) – Jejunum: long villi and increased goblet cells – no Brunner glands or Peyer patches – Ileum: Short villi, many goblet cells, and lymphatic nodules in the submucosa called Peyer patches
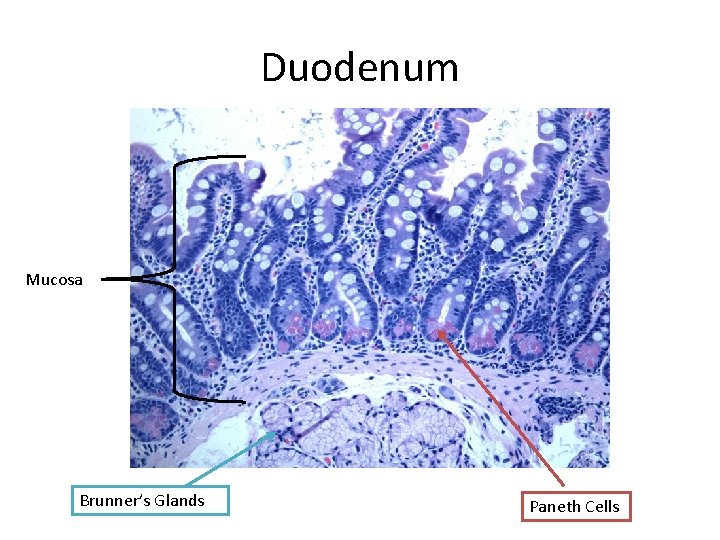
Duodenum Mucosa Brunner’s Glands Paneth Cells
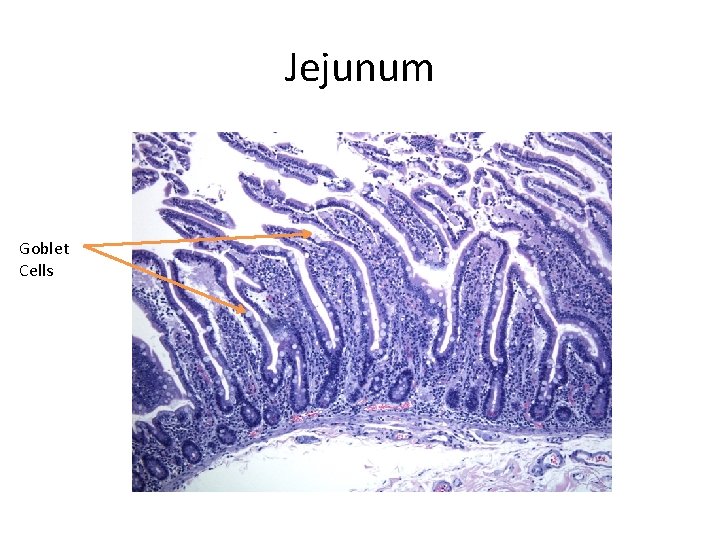
Jejunum Goblet Cells
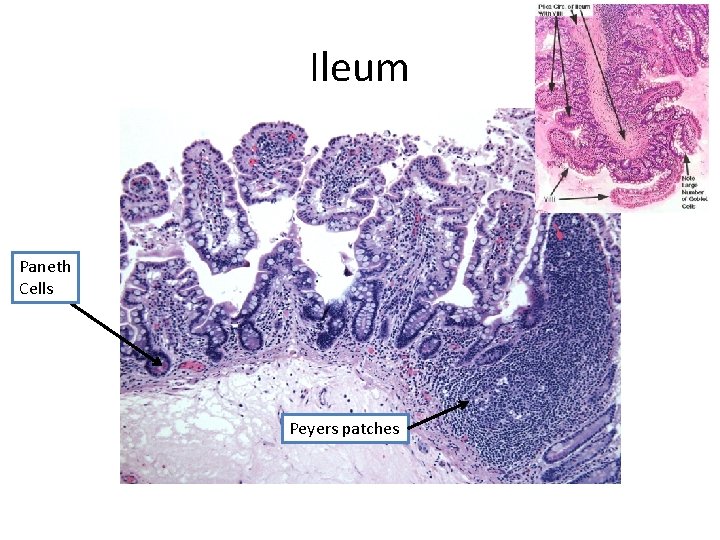
Ileum Paneth Cells Peyers patches
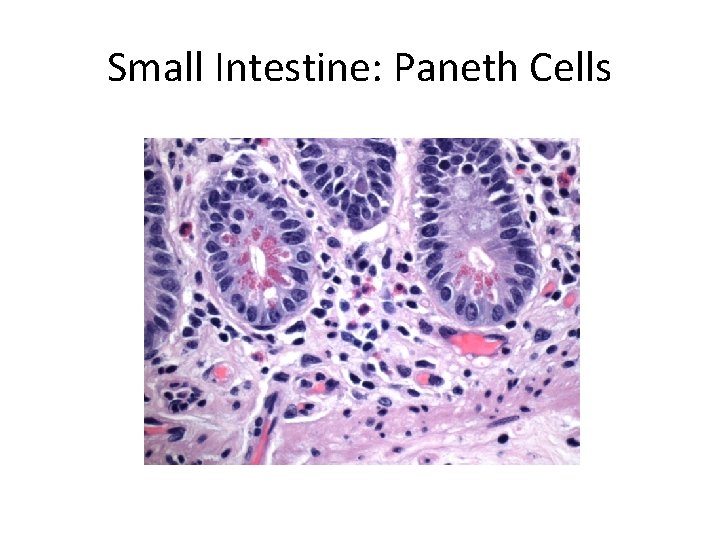
Small Intestine: Paneth Cells
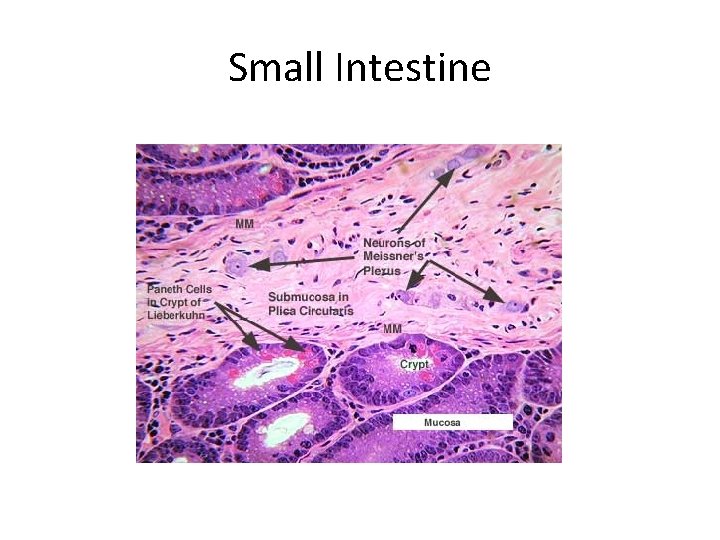
Small Intestine
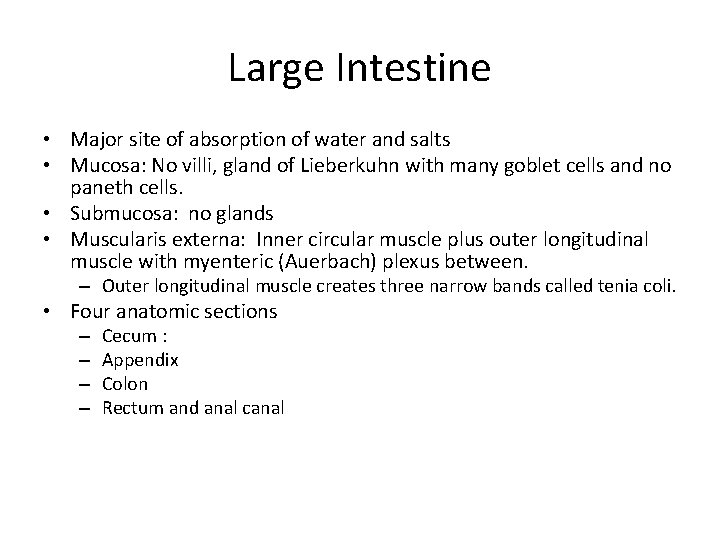
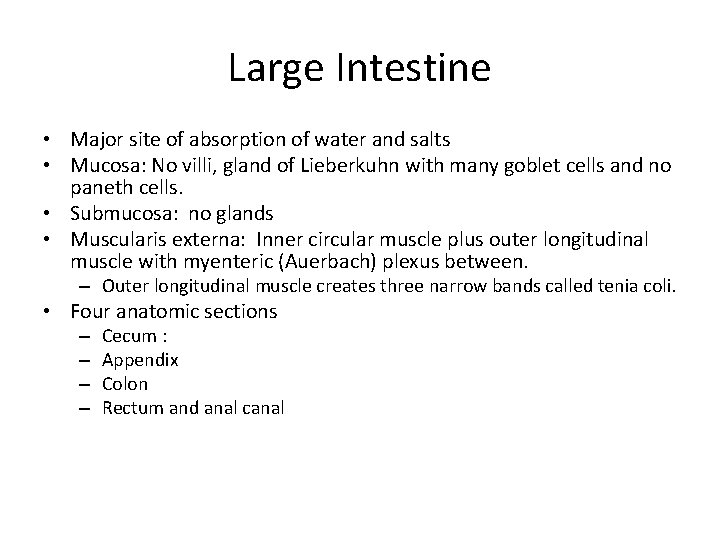
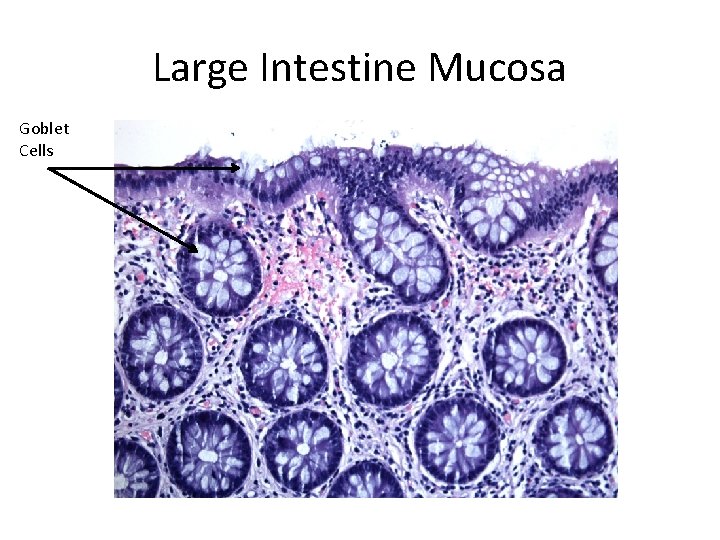
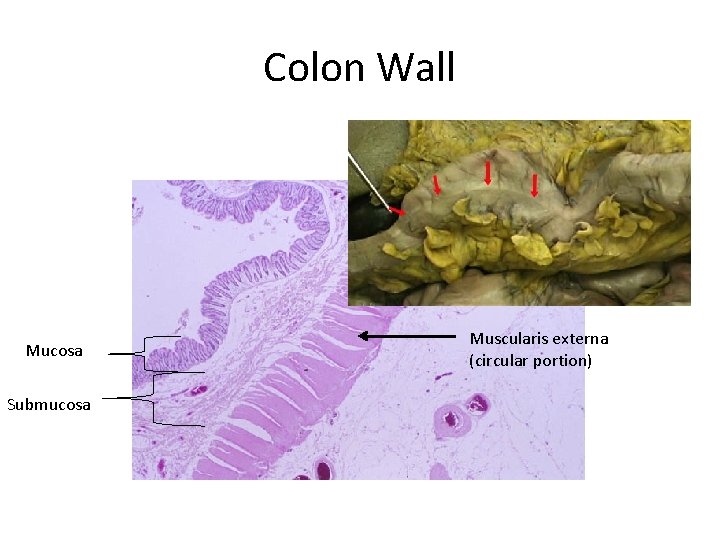
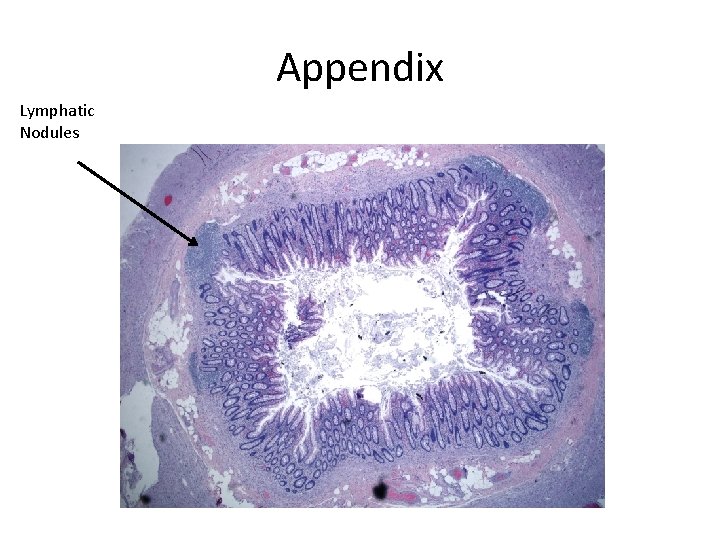
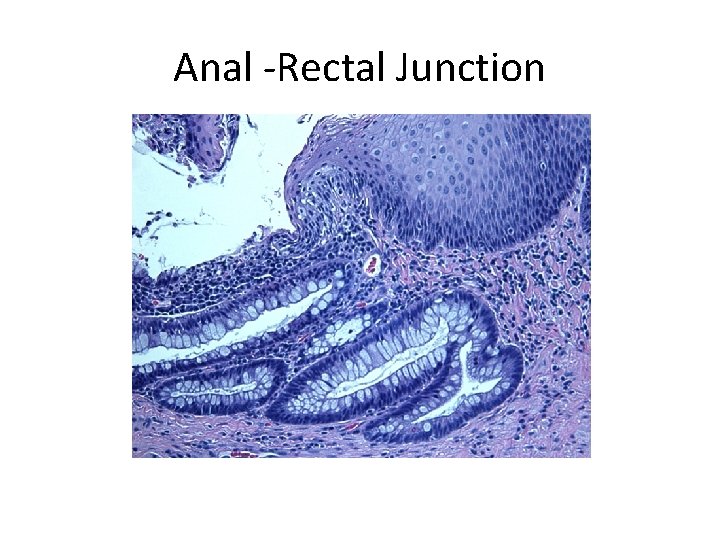
Large Intestine • Major site of absorption of water and salts • Mucosa: No villi, gland of Lieberkuhn with many goblet cells and no paneth cells. • Submucosa: no glands • Muscularis externa: Inner circular muscle plus outer longitudinal muscle with myenteric (Auerbach) plexus between. – Outer longitudinal muscle creates three narrow bands called tenia coli. • Four anatomic sections – – Cecum : Appendix Colon Rectum and anal canal
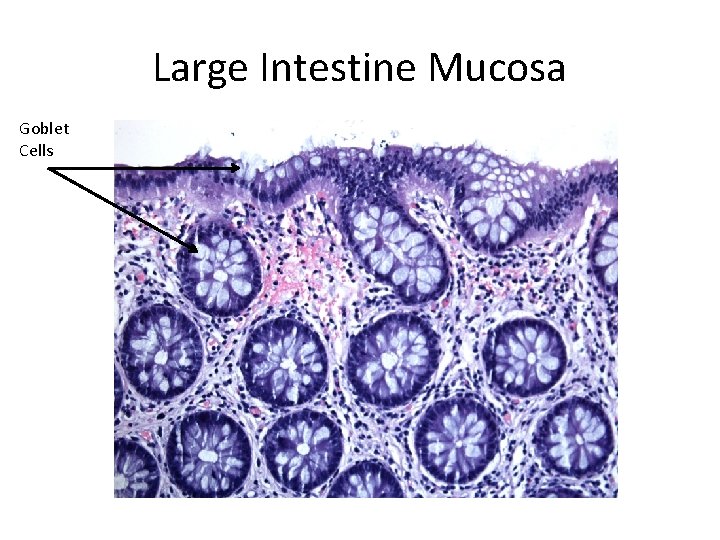
Large Intestine Mucosa Goblet Cells
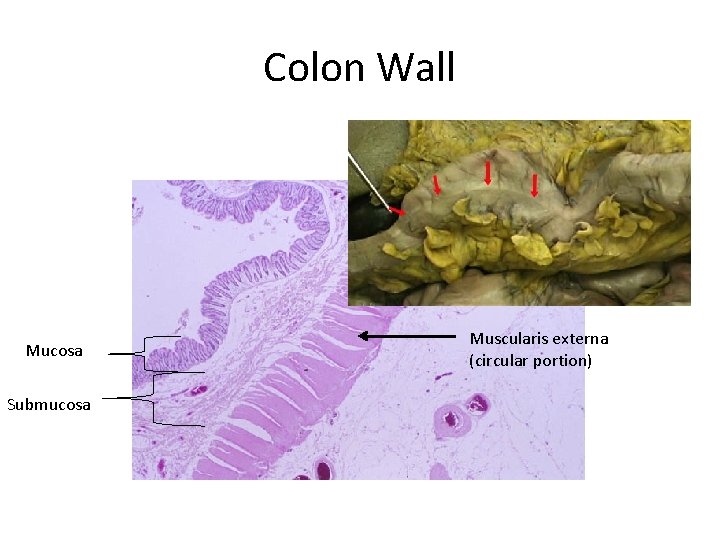
Colon Wall Mucosa Submucosa Muscularis externa (circular portion)
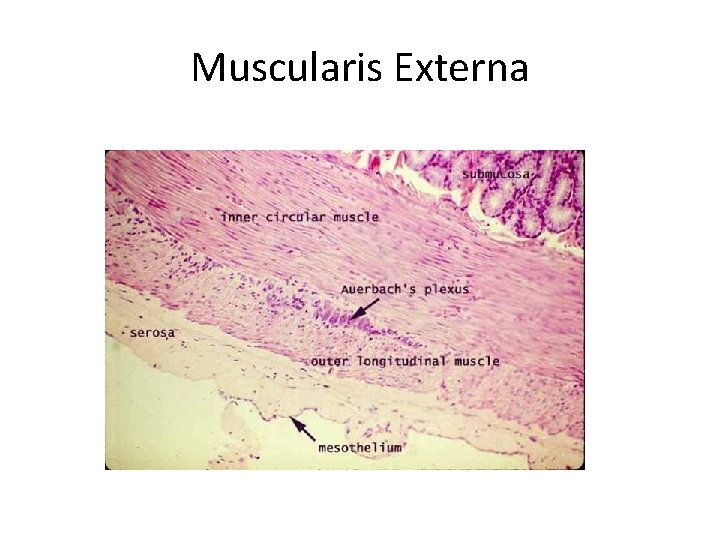
Muscularis Externa
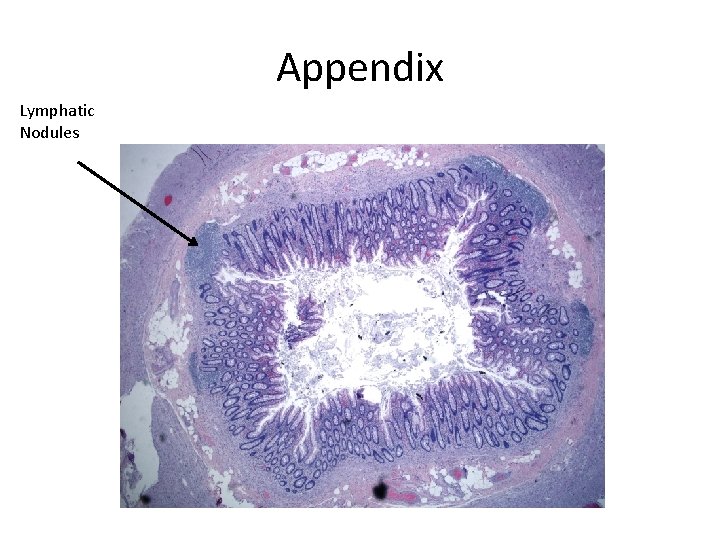
Appendix Lymphatic Nodules
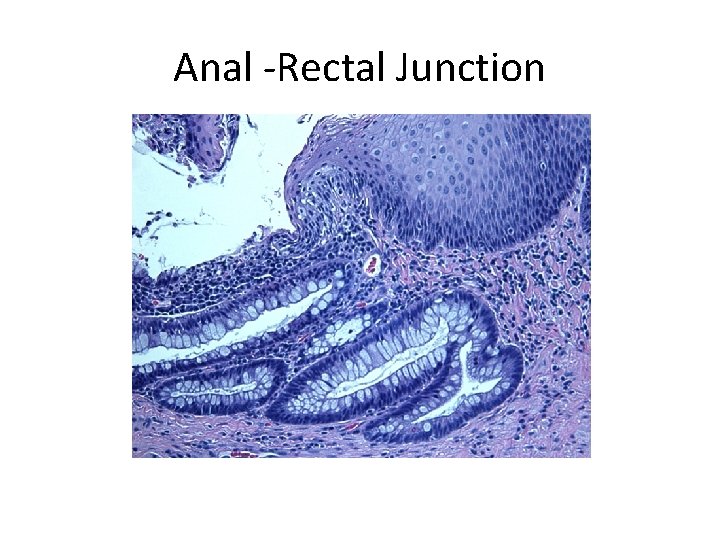
Anal -Rectal Junction
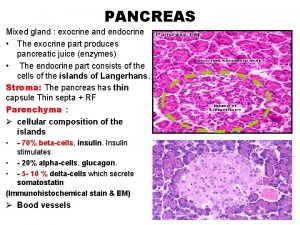
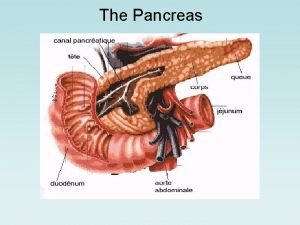
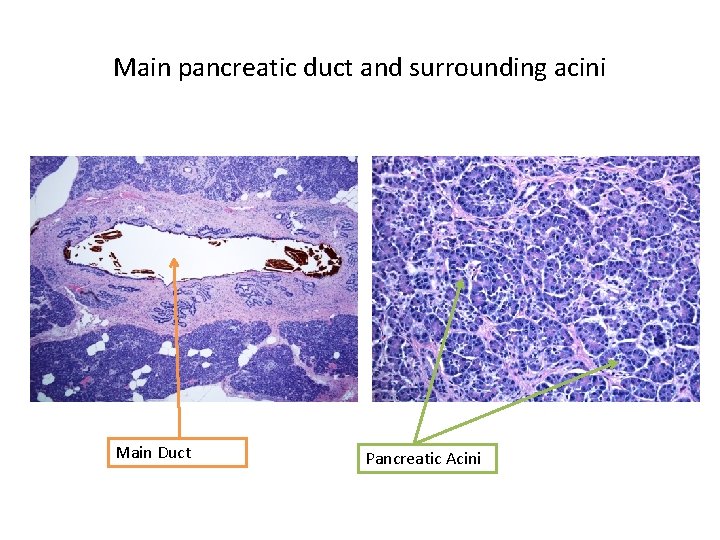
Exocrine Pancreas • Many serous secretory cells (pancreatic acinar cells) form acinar structures. – Cytoplasm contains zymogen granules • Secretions carried by main duct to join bile duct at the ampulla in the duodenum
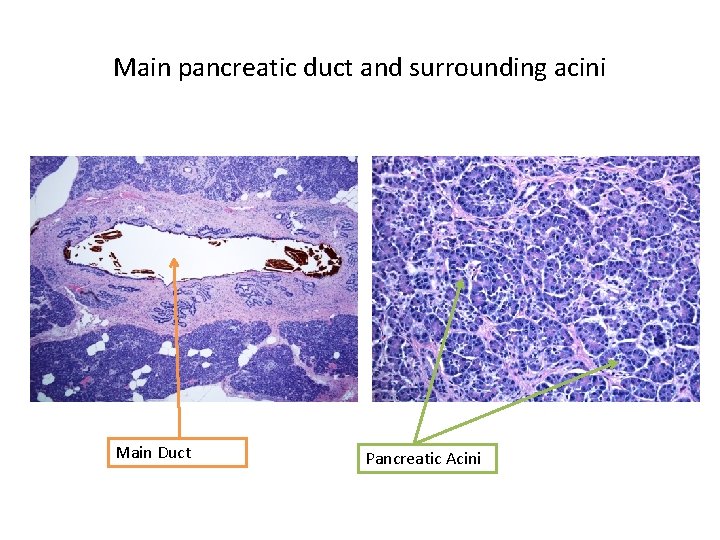
Main pancreatic duct and surrounding acini Main Duct Pancreatic Acini
 Ipmn
Ipmn Where is bile juice produced
Where is bile juice produced Pancreasitis
Pancreasitis Fungiform papillae histology
Fungiform papillae histology Pancreas anatomy and physiology
Pancreas anatomy and physiology Pancreatic carcinoma risk factors
Pancreatic carcinoma risk factors Chapter 15 the gastrointestinal system
Chapter 15 the gastrointestinal system Emt chapter 18 gastrointestinal and urologic emergencies
Emt chapter 18 gastrointestinal and urologic emergencies Difference between endocrine and exocrine glands
Difference between endocrine and exocrine glands Whats the difference between endocrine and exocrine glands
Whats the difference between endocrine and exocrine glands Embriologia del sistema gastrointestinal
Embriologia del sistema gastrointestinal Gastrointestinal tract
Gastrointestinal tract Chemotrypsinogen
Chemotrypsinogen Gastrointestinal hormones
Gastrointestinal hormones Malrotasi traktus gastrointestinal
Malrotasi traktus gastrointestinal Espectro equimótico
Espectro equimótico Gastrointestinal sistem hormonları
Gastrointestinal sistem hormonları Gastrointestinal medical terminology breakdown
Gastrointestinal medical terminology breakdown Focused physical assessment
Focused physical assessment Foregut
Foregut Composition of stomach
Composition of stomach Motilidad gastrointestinal
Motilidad gastrointestinal Upper gi bleeding management
Upper gi bleeding management Pré-molares
Pré-molares Anatomia rim
Anatomia rim Gastrointestinal disease
Gastrointestinal disease