Histology Elongated branching cells containing 1 2 central
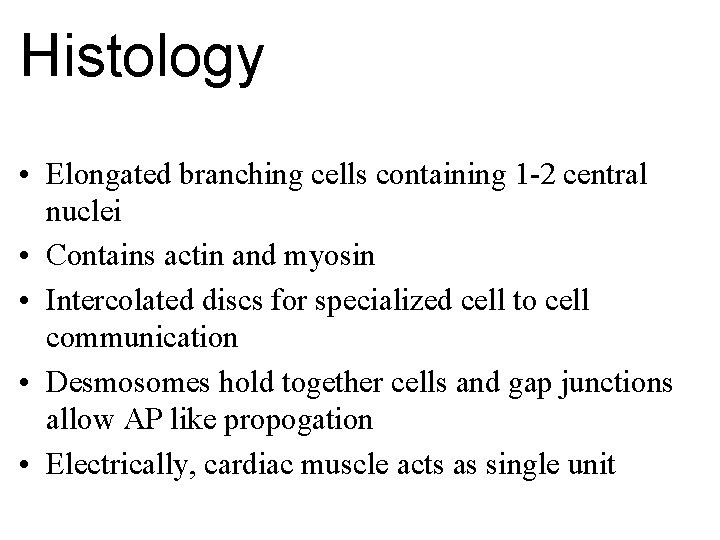
Histology • Elongated branching cells containing 1 -2 central nuclei • Contains actin and myosin • Intercolated discs for specialized cell to cell communication • Desmosomes hold together cells and gap junctions allow AP like propogation • Electrically, cardiac muscle acts as single unit
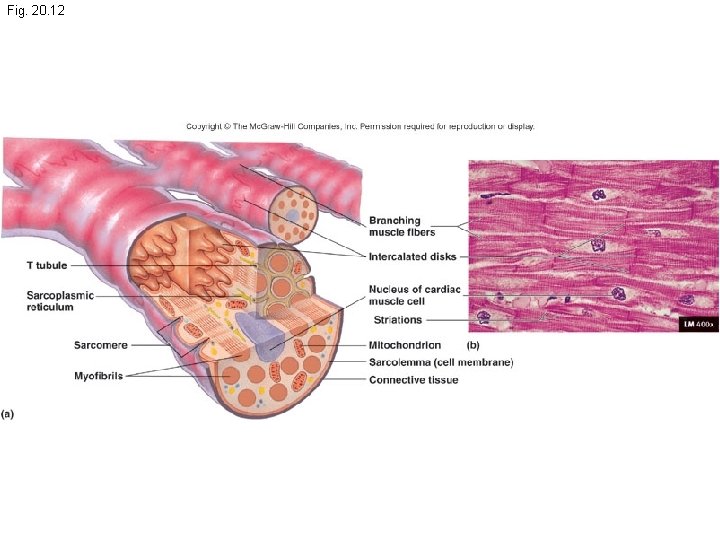
Fig. 20. 12
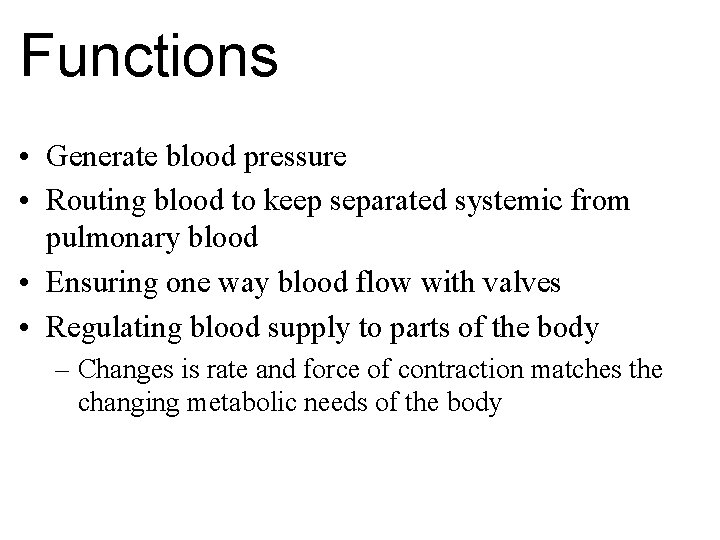
Functions • Generate blood pressure • Routing blood to keep separated systemic from pulmonary blood • Ensuring one way blood flow with valves • Regulating blood supply to parts of the body – Changes is rate and force of contraction matches the changing metabolic needs of the body
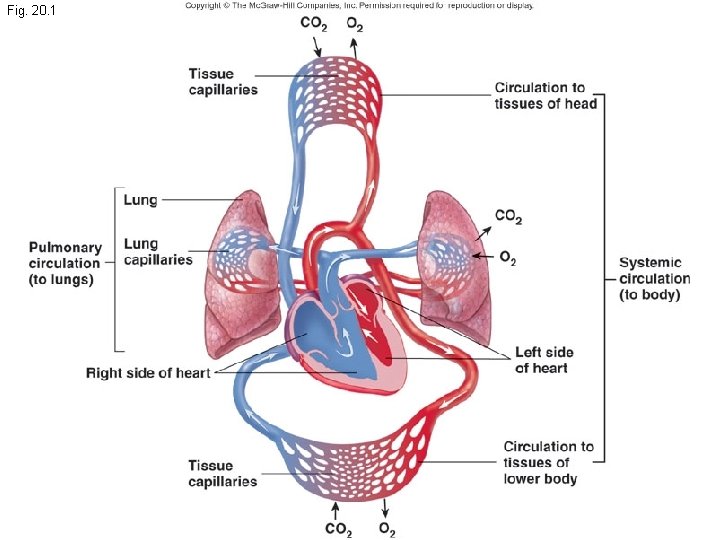
Fig. 20. 1

Anatomy • Pericardial Sac - parietal pericardium – Fibrous Layer – outer layer consisting of tough, fibrous connective tissue • prevents over distension of the heart • provides a protective membrane • anchors the heart in the mediastinum – Serous Layer - 2 layers - (parietal and visceral layer) continuous with the epicardium - adheres to the heart • Pericardial Cavity - a space between the parietal and the visceral layer of the heart filled with pericardial fluid - helps to prevent friction
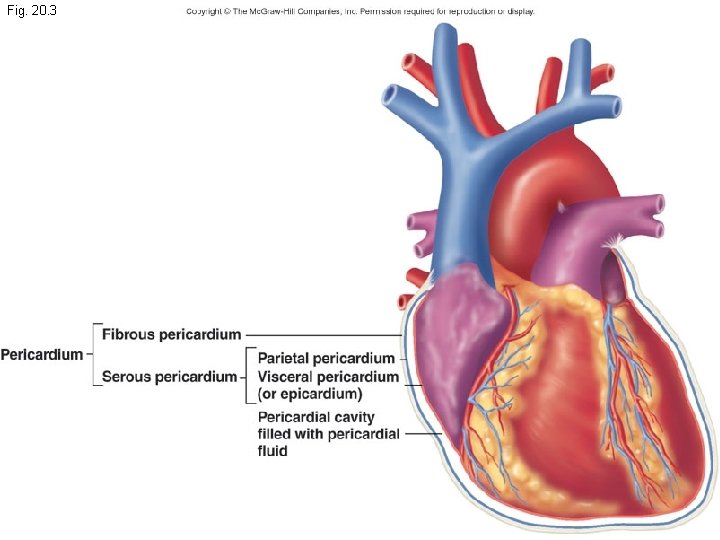
Fig. 20. 3
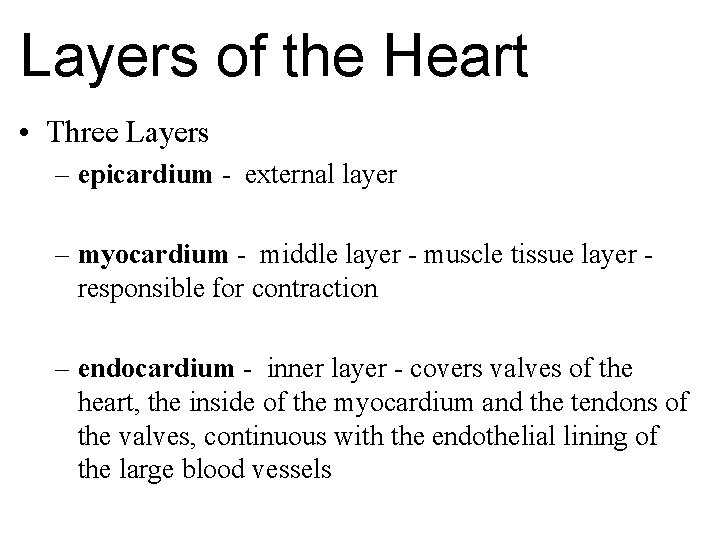
Layers of the Heart • Three Layers – epicardium - external layer – myocardium - middle layer - muscle tissue layer responsible for contraction – endocardium - inner layer - covers valves of the heart, the inside of the myocardium and the tendons of the valves, continuous with the endothelial lining of the large blood vessels
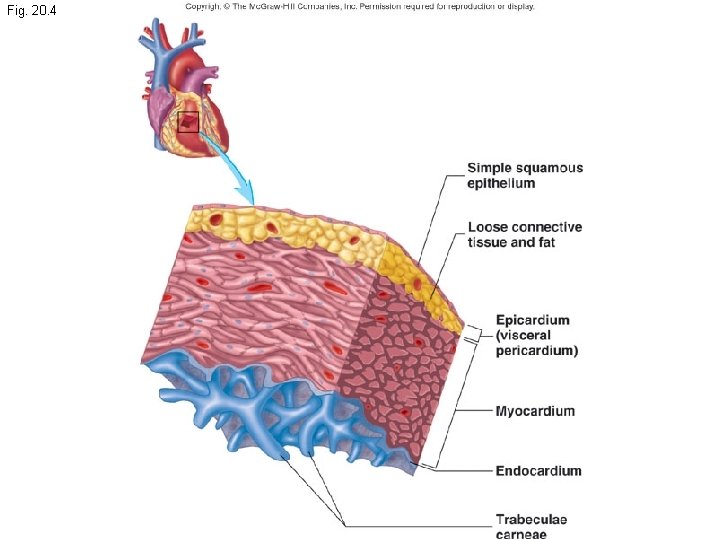
Fig. 20. 4
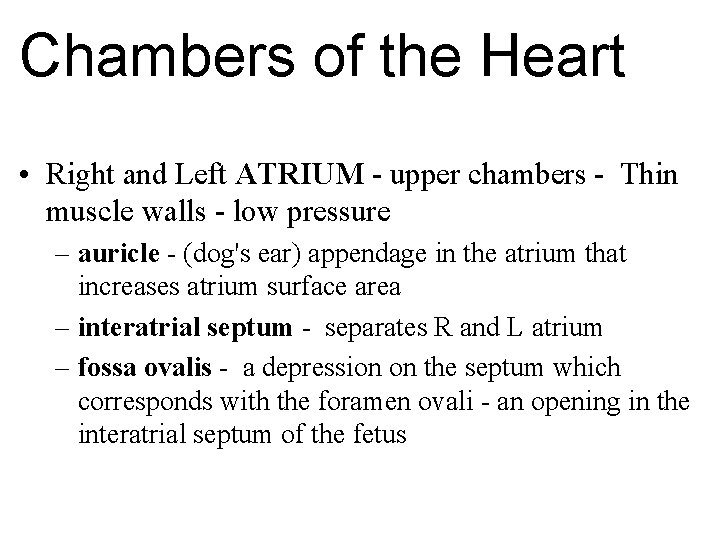
Chambers of the Heart • Right and Left ATRIUM - upper chambers - Thin muscle walls - low pressure – auricle - (dog's ear) appendage in the atrium that increases atrium surface area – interatrial septum - separates R and L atrium – fossa ovalis - a depression on the septum which corresponds with the foramen ovali - an opening in the interatrial septum of the fetus

Chambers of the Heart • Right and Left VENTRICLES - lower chambers much greater pressure – interventricular septum - separates R and L ventricles – L walls are even thicker than the R walls because it must pump blood through the 1000's miles of blood vessels
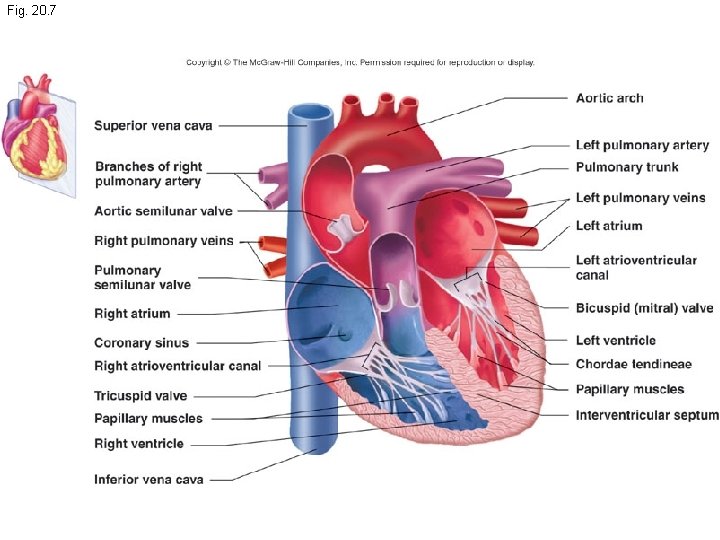
Fig. 20. 7
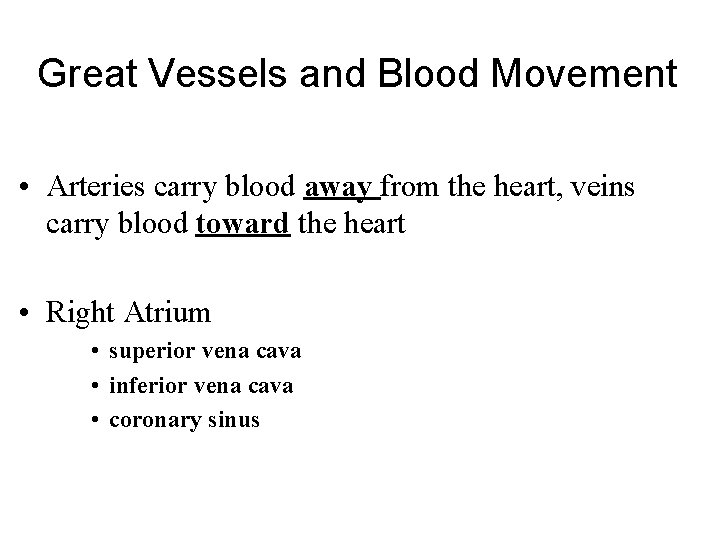
Great Vessels and Blood Movement • Arteries carry blood away from the heart, veins carry blood toward the heart • Right Atrium • superior vena cava • inferior vena cava • coronary sinus
Blood Flow • Blood travels through the right Atrioventricular valve (A-V , Tricuspid) into the R ventricle. The R ventricle contracts and pumps the blood through the pulmonary semilunar valve into the pulmonary trunk, the pulmonary trunk divides into the R and L pulmonary arteries, which lead to the lungs
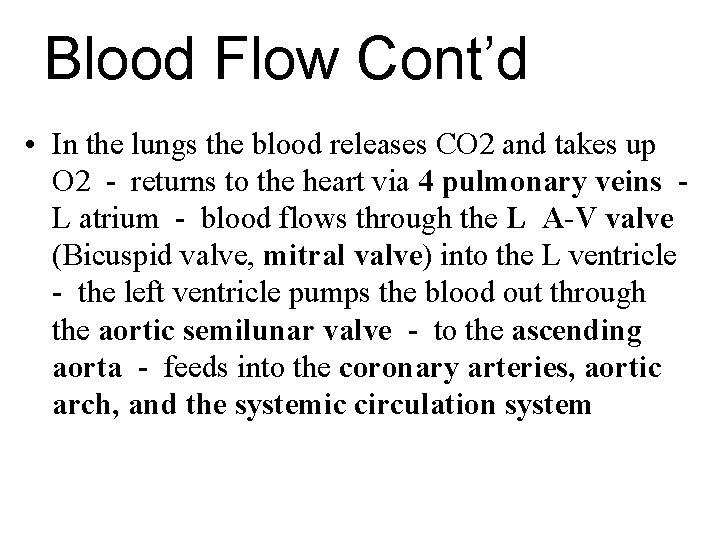
Blood Flow Cont’d • In the lungs the blood releases CO 2 and takes up O 2 - returns to the heart via 4 pulmonary veins L atrium - blood flows through the L A-V valve (Bicuspid valve, mitral valve) into the L ventricle - the left ventricle pumps the blood out through the aortic semilunar valve - to the ascending aorta - feeds into the coronary arteries, aortic arch, and the systemic circulation system
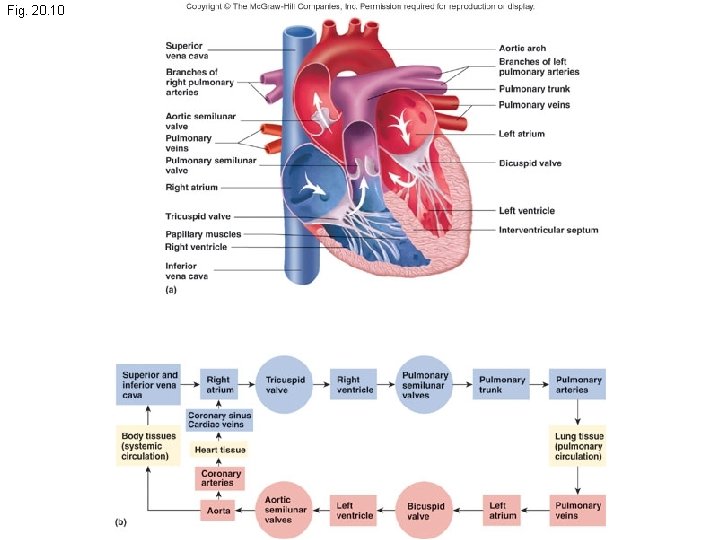
Fig. 20. 10
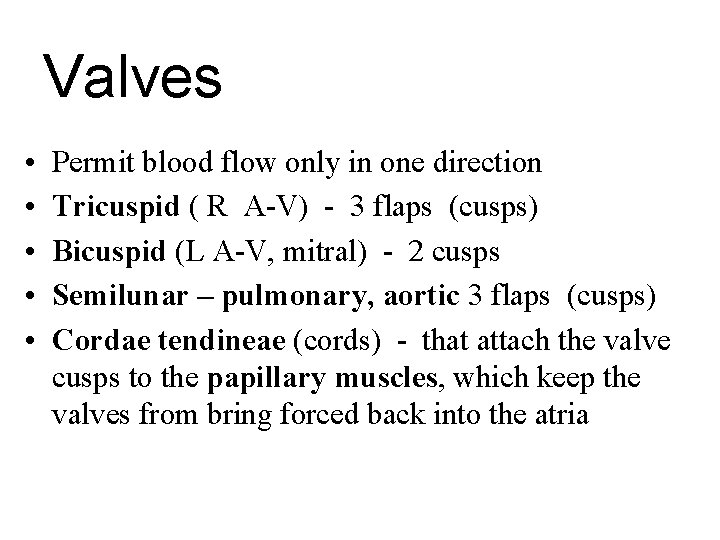
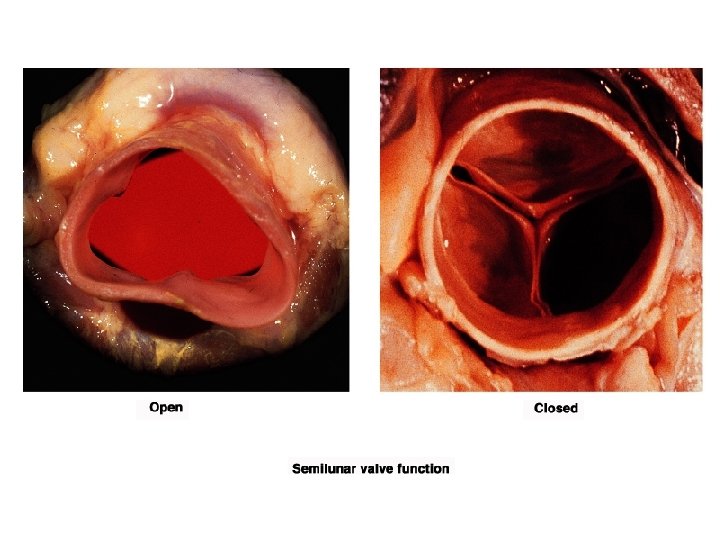
Valves • • • Permit blood flow only in one direction Tricuspid ( R A-V) - 3 flaps (cusps) Bicuspid (L A-V, mitral) - 2 cusps Semilunar – pulmonary, aortic 3 flaps (cusps) Cordae tendineae (cords) - that attach the valve cusps to the papillary muscles, which keep the valves from bring forced back into the atria
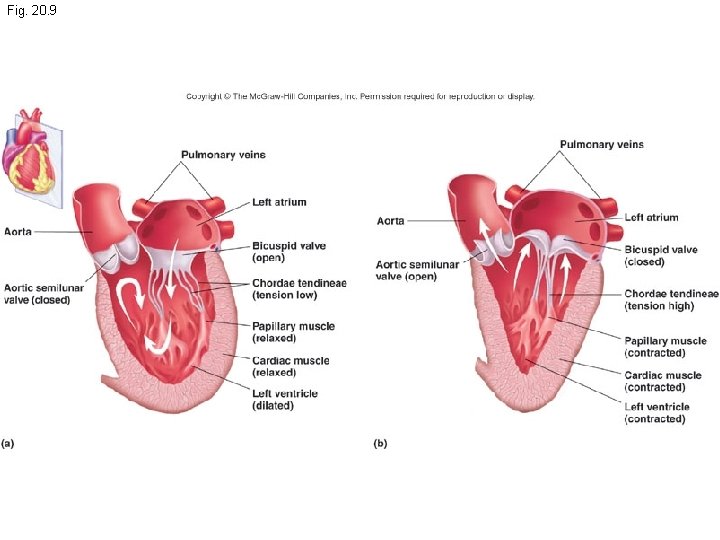
Fig. 20. 9
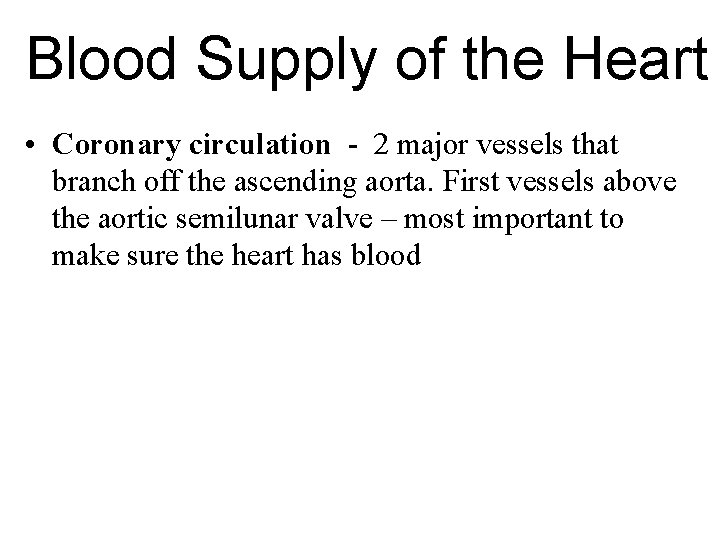
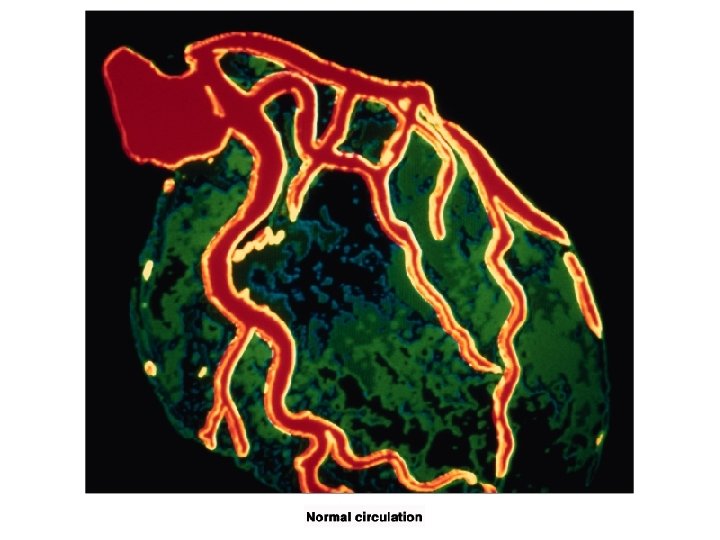
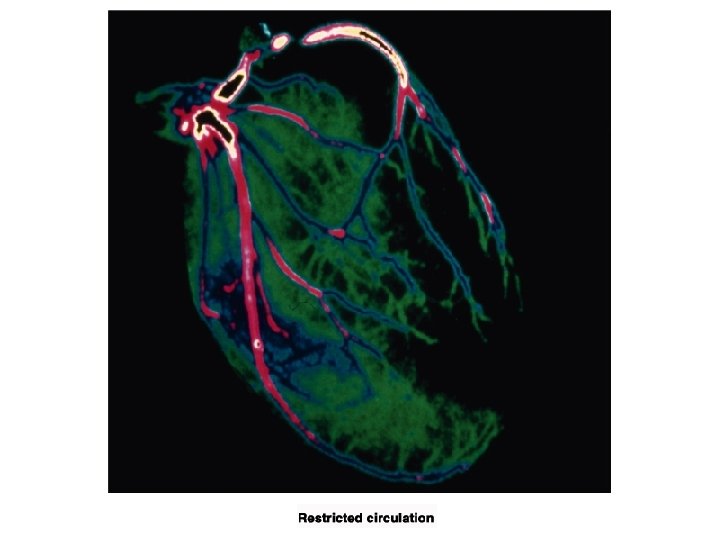
Blood Supply of the Heart • Coronary circulation - 2 major vessels that branch off the ascending aorta. First vessels above the aortic semilunar valve – most important to make sure the heart has blood
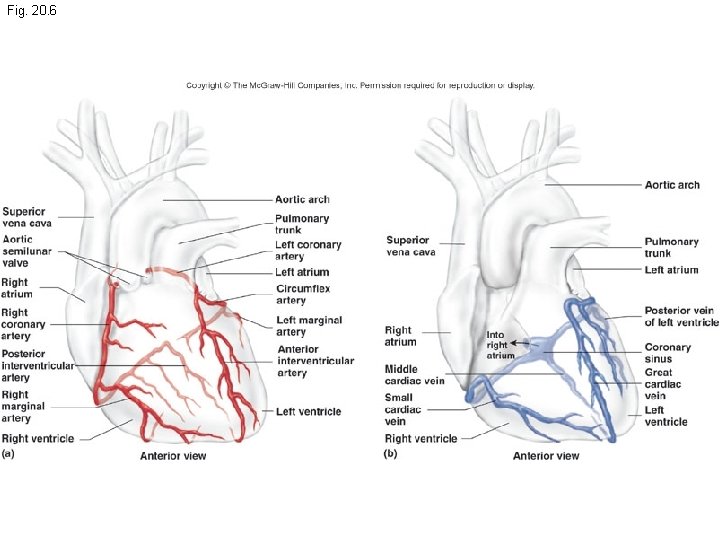
Fig. 20. 6
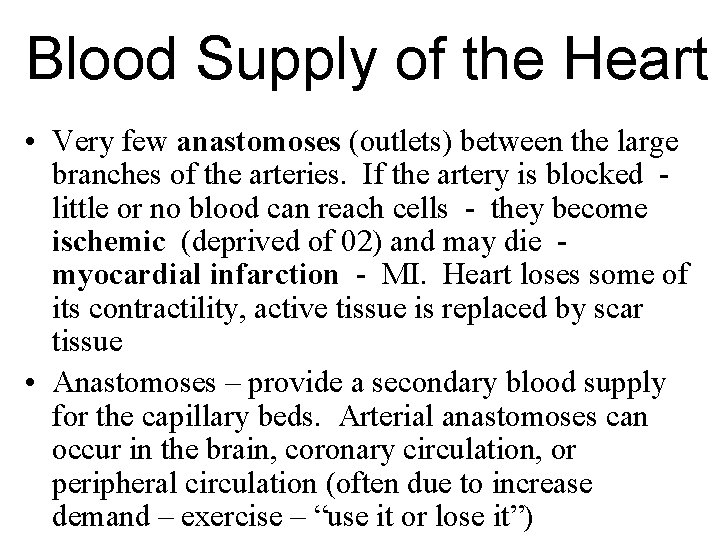
Blood Supply of the Heart • Very few anastomoses (outlets) between the large branches of the arteries. If the artery is blocked little or no blood can reach cells - they become ischemic (deprived of 02) and may die myocardial infarction - MI. Heart loses some of its contractility, active tissue is replaced by scar tissue • Anastomoses – provide a secondary blood supply for the capillary beds. Arterial anastomoses can occur in the brain, coronary circulation, or peripheral circulation (often due to increase demand – exercise – “use it or lose it”)
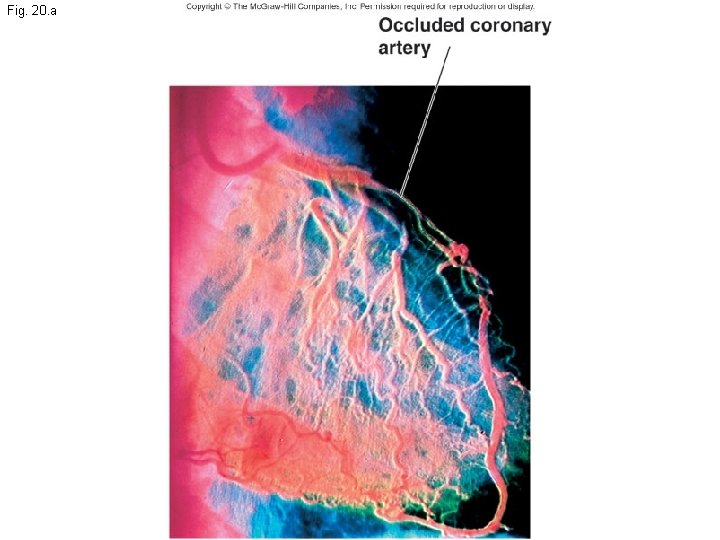
Fig. 20. a
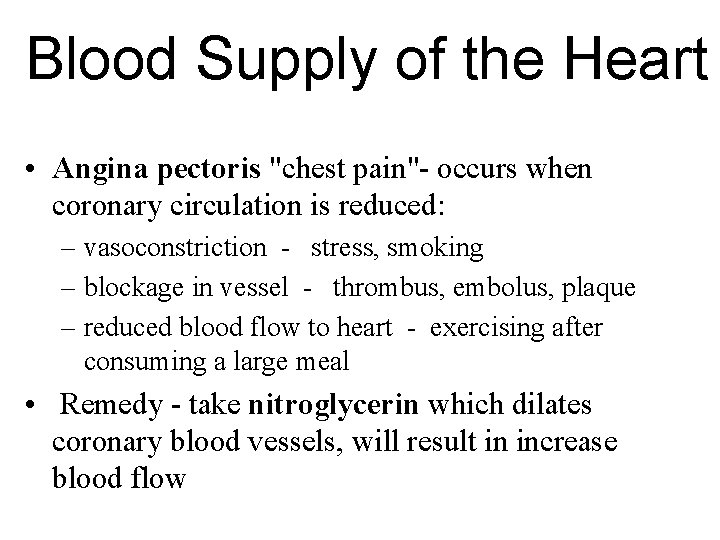
Blood Supply of the Heart • Angina pectoris "chest pain"- occurs when coronary circulation is reduced: – vasoconstriction - stress, smoking – blockage in vessel - thrombus, embolus, plaque – reduced blood flow to heart - exercising after consuming a large meal • Remedy - take nitroglycerin which dilates coronary blood vessels, will result in increase blood flow
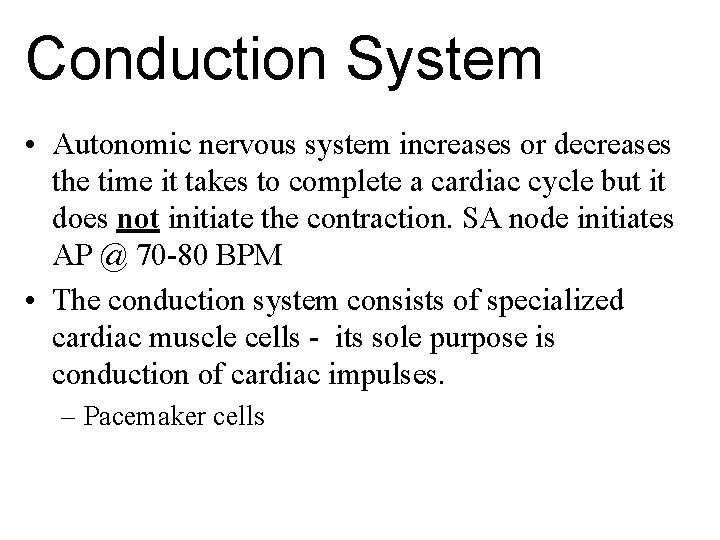
Conduction System • Autonomic nervous system increases or decreases the time it takes to complete a cardiac cycle but it does not initiate the contraction. SA node initiates AP @ 70 -80 BPM • The conduction system consists of specialized cardiac muscle cells - its sole purpose is conduction of cardiac impulses. – Pacemaker cells
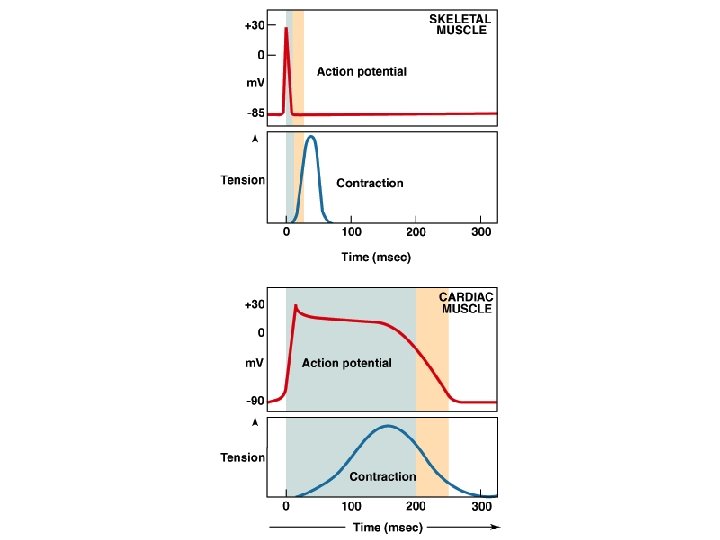

Conduction System • Sinoatrial Node - SA node - pacemaker – 100's of cells located in R atrium near the opening of the superior vena cava – Possess an intrinsic rhythm – They initiate each cardiac cycle – The impulse the SA node initiates spreads out over both atria causing them to contract and also depolarizing the AV node
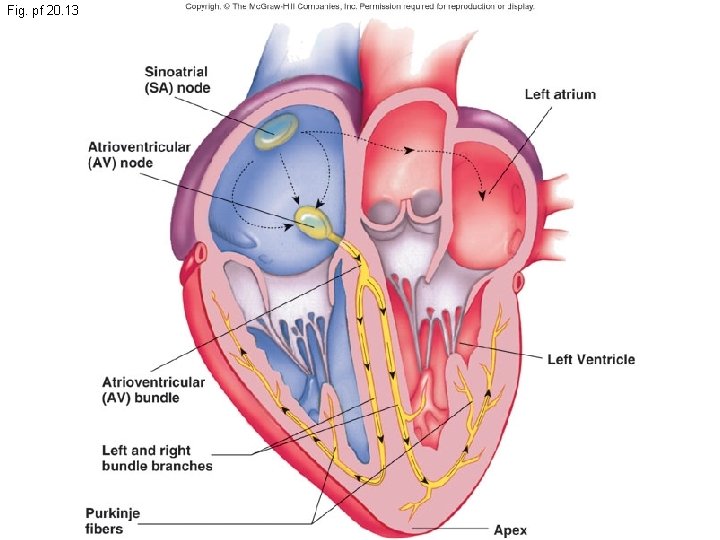
Fig. pf 20. 13

Conduction System • Atrioventricular node - AV node - located near the inferior portion of the interatrial septum one of the last parts of the R atrium to be depolarized • Atrioventricular Bundle - AV bundle (Bundle of His) • Purkinje Fibers
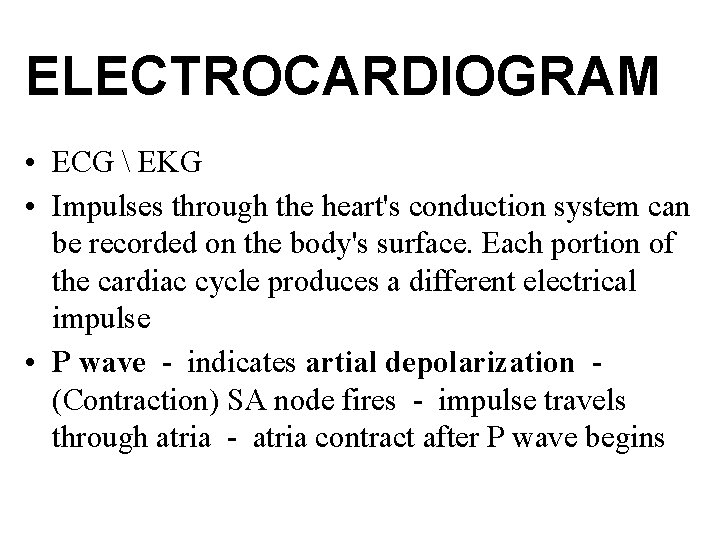
ELECTROCARDIOGRAM • ECG EKG • Impulses through the heart's conduction system can be recorded on the body's surface. Each portion of the cardiac cycle produces a different electrical impulse • P wave - indicates artial depolarization (Contraction) SA node fires - impulse travels through atria - atria contract after P wave begins
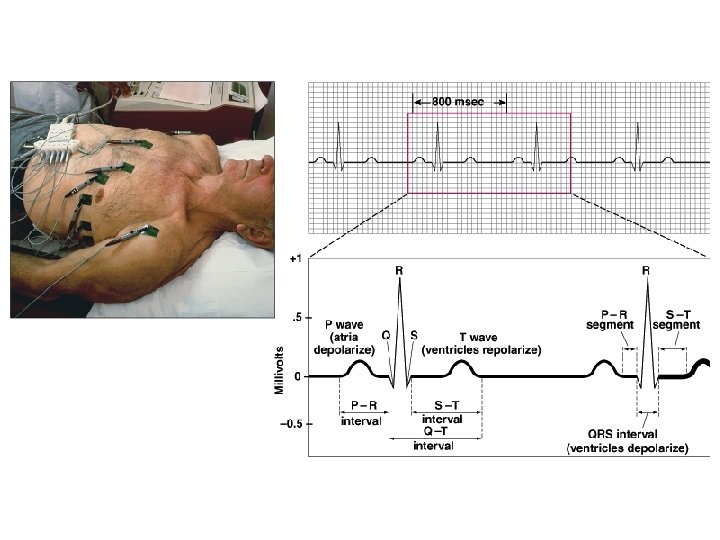
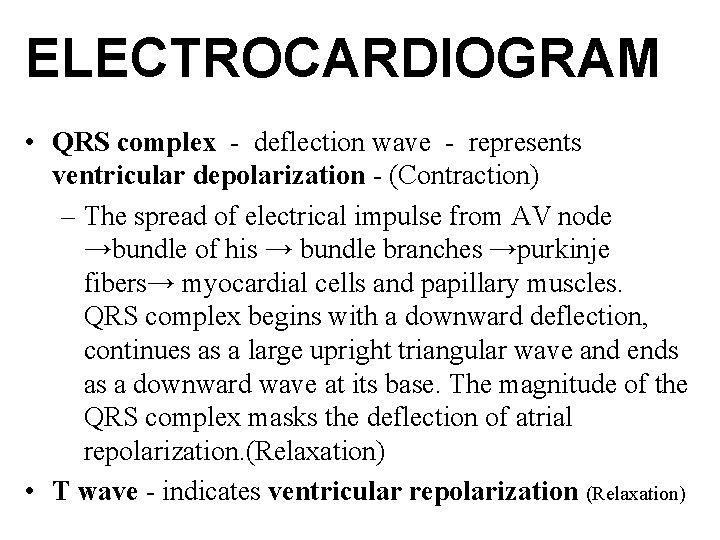
ELECTROCARDIOGRAM • QRS complex - deflection wave - represents ventricular depolarization - (Contraction) – The spread of electrical impulse from AV node →bundle of his → bundle branches →purkinje fibers→ myocardial cells and papillary muscles. QRS complex begins with a downward deflection, continues as a large upright triangular wave and ends as a downward wave at its base. The magnitude of the QRS complex masks the deflection of atrial repolarization. (Relaxation) • T wave - indicates ventricular repolarization (Relaxation)
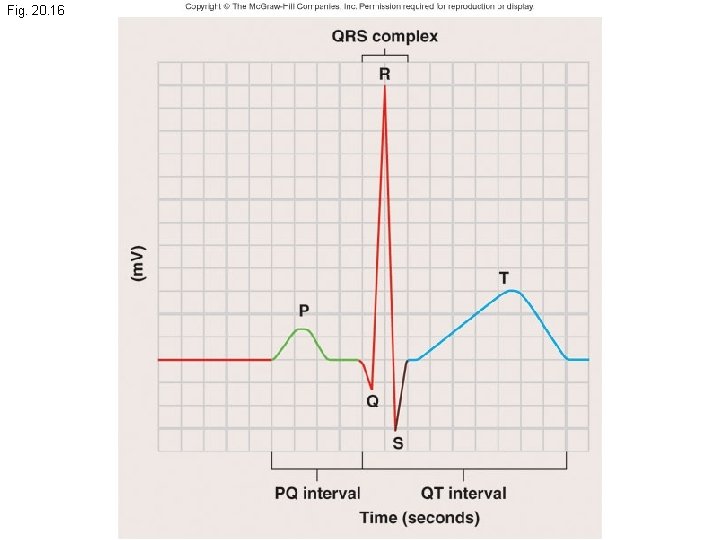
Fig. 20. 16
Fig. 20. 17 b
Cardiac Cycle • Heart is two pumps that work together, right and left half • Repetitive contraction (systole) and relaxation (diastole) of heart chambers • Blood moves through circulatory system from areas of higher to lower pressure. – Contraction of heart produces the pressure
Starling's Law of the Heart • Increasing the length of the cardiac muscle fibers intensifies the force of the ventricular contraction. During exercise: ↑blood flow = ↑ fiber length = ↑ contraction strength • “More in = more out”, Blood flow can increase from 4 -6 L/M to 18 -30 L/M during exercise
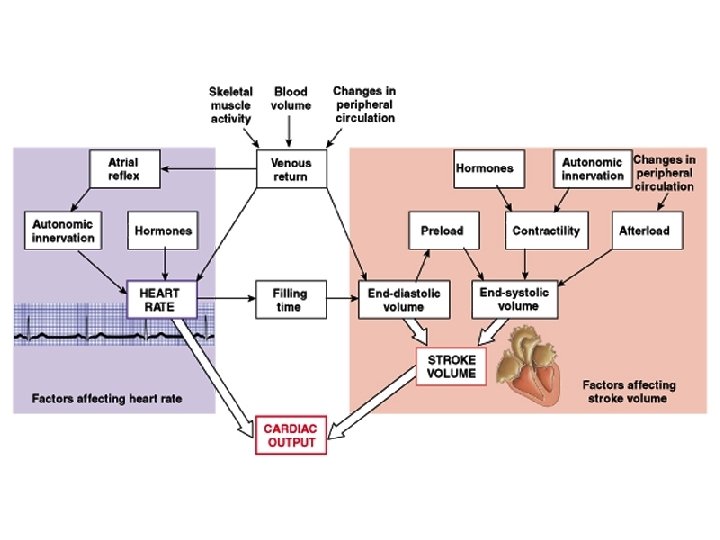
Regulation of Heart Rate • Cardioaccelatory center - located in medulla sympathetic fibers - release of norepinephrine causes an increase in heart rate and contractility (NE increases the force of contraction) • Cardioinhibitory center - located in medulla parasympathetic fibers - release acetylcholine which causes a decrease in HR and contractility. – Bradycardia - HR less than 60 BPM
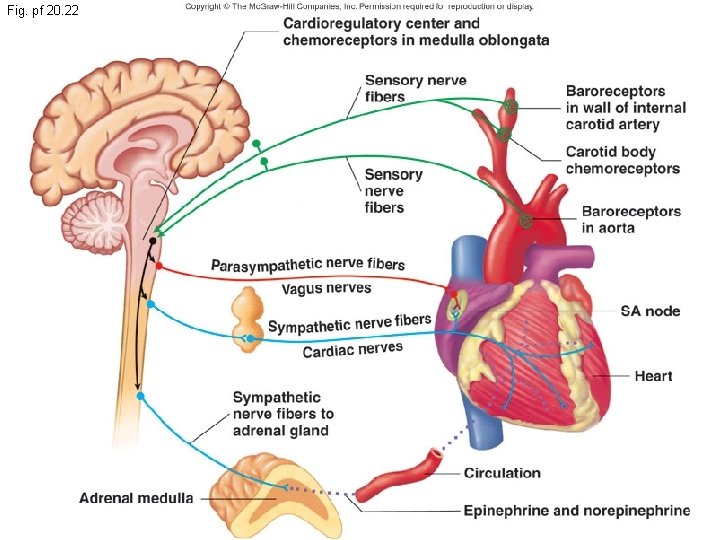
Fig. pf 20. 22
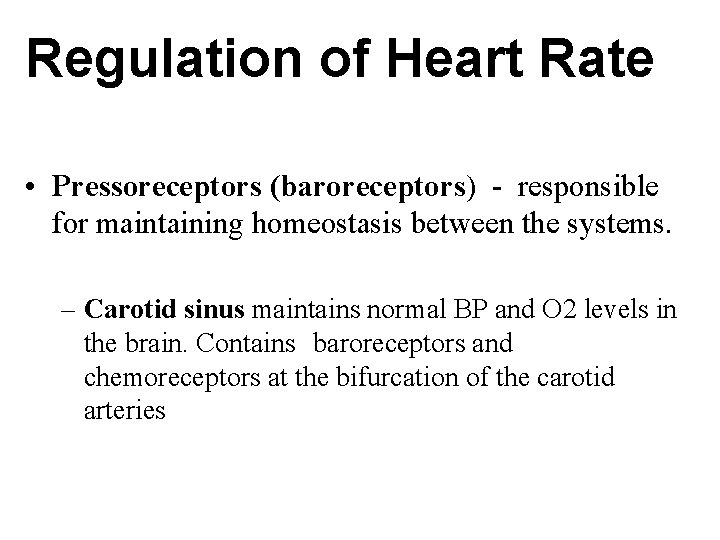
Regulation of Heart Rate • Pressoreceptors (baroreceptors) - responsible for maintaining homeostasis between the systems. – Carotid sinus maintains normal BP and O 2 levels in the brain. Contains baroreceptors and chemoreceptors at the bifurcation of the carotid arteries
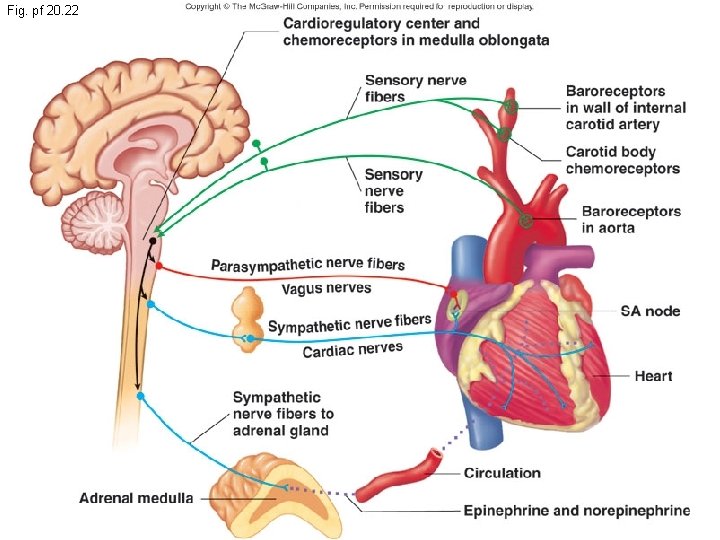
Fig. pf 20. 22
Cardiac Arrhythmias • Tachycardia: Heart rate in excess of 100 bpm • Bradycardia: Heart rate less than 60 bpm • Sinus arrhythmia: Heart rate varies 5% during respiratory cycle and up to 30% during deep respiration • Premature atrial contractions: Occasional shortened intervals between one contraction and succeeding, frequently occurs in healthy people
Effects of Aging on the Heart • Gradual changes in heart function, minor under resting condition, more significant during exercise • Hypertrophy of left ventricle • Maximum heart rate decreases • Increased tendency for valves to function abnormally and arrhythmias to occur • Increased oxygen consumption required to pump same amount of blood
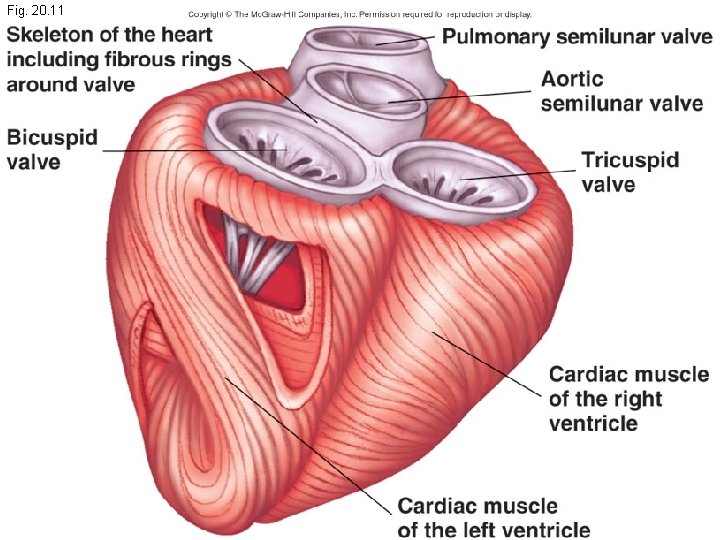
Fig. 20. 11
- Slides: 46