Histamine And Antihistamine Drugs Department of Pharmacology Chalapathi





- Slides: 27

Histamine And Antihistamine Drugs Department of Pharmacology Chalapathi Institute of Pharmaceutical Sciences Guntur
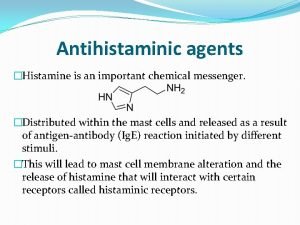
AUTACOIDS DEFINITION: � “Self-remedy, Referring to the Action of Local Hormones”
What Are Autacoids ? �Histamine �Serotonin �Endogenous Peptides �Prostaglandins �Leukotrienes
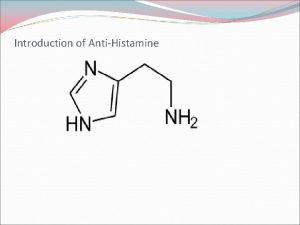
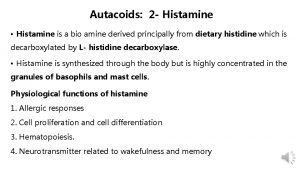
HISTAMINE v Histamine ü is A naturally occurring imidazole derivative It is widely distributed in skin, GIT mucosa, lungs, brain, cerebro spinal fluid and bone marrow v It is also a component of some venoms and sting secretions
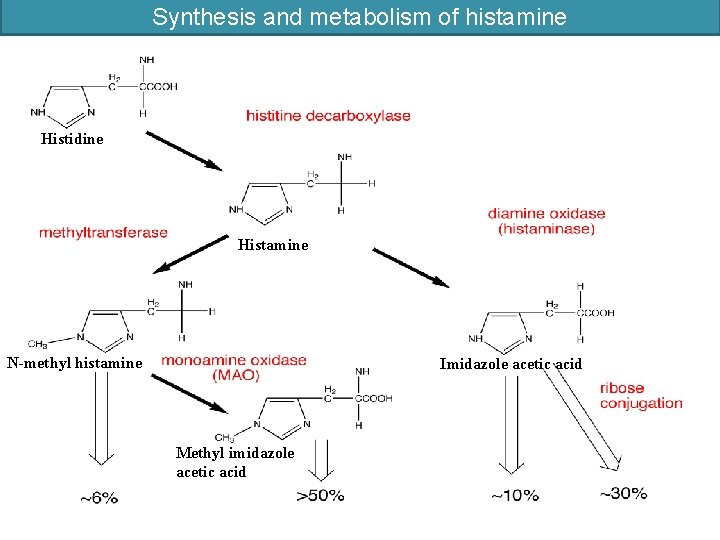
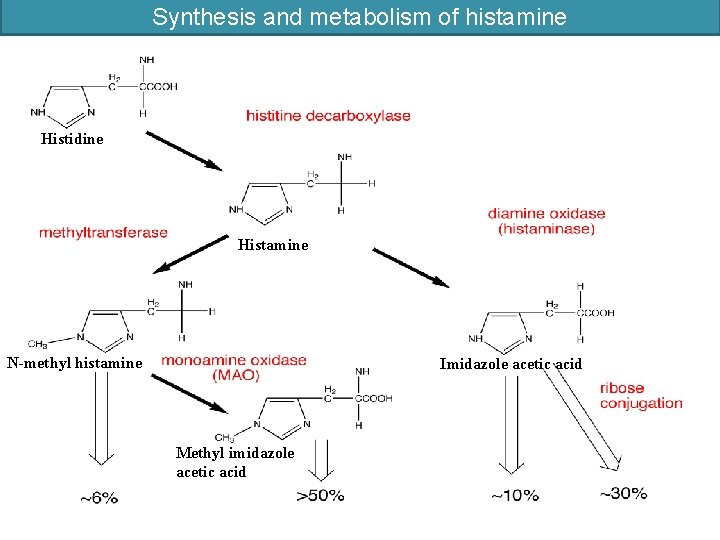
Synthesis and metabolism of histamine Histidine Histamine N-methyl histamine Imidazole acetic acid Methyl imidazole acetic acid
Histamine: Storage and Release Immunologic Release: � The most important mechanism for histamine release is in response to an immunological stimulus. � In mast cells, if sensitized by surface Ig. E antibodies, degranulate when exposed specific antigen. � Degranulation means liberation of the contents of the mast cell granules, including histamine. � Degranulation is involved in the immediate (type I) allergic reaction.
Mechanical /Chemical Release: �A second type of release occurs following chemical or mechanical injury to mast cells. Ø In these injuries caused degranulation Ø drugs like morphine, succinyl choline, d-tubocurarine , hydralazine, dextran, poly vinyl pyridone (PVP) will liberate the histamine
Drugs that inhibit histamine release � β 2 -agonists like adrenaline, ephidrine, isoproterenol � Mast cell membrane stabilisers: disodiumcromoglycate and ketotifen
Receptors & Effects � Two receptors for histamine, H 1 and H 2, mediate most of the well-defined actions; 1. H 1 receptor: important in smooth muscle effects, especially those caused by Ig. E-mediated responses. ① IP 3 and DAG are released. ② Bronchoconstriction and vasodilation. ③ Vasodilation by release of endothelium-derived relaxing factor (EDRF), are typical responses of smooth muscle. ④ Capillary endothelium, in addition to releasing EDRF, also contracts, opening gaps in the permeability barrier and resulting in the formation of local edema.
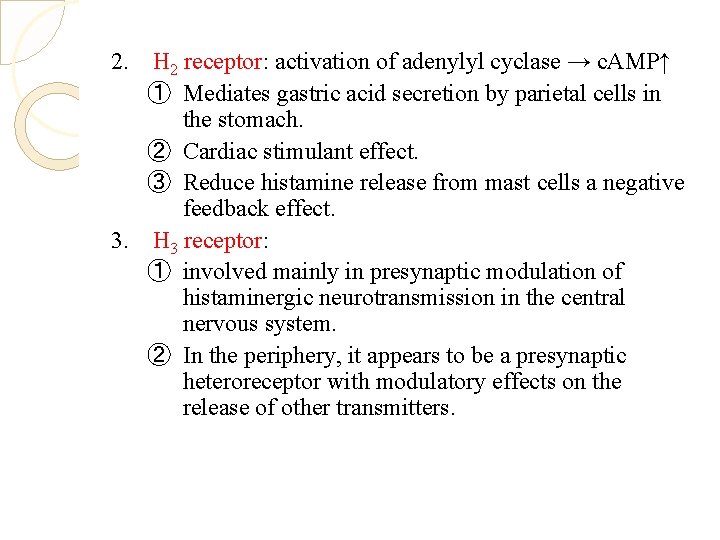
2. H 2 receptor: activation of adenylyl cyclase → c. AMP↑ ① Mediates gastric acid secretion by parietal cells in the stomach. ② Cardiac stimulant effect. ③ Reduce histamine release from mast cells a negative feedback effect. 3. H 3 receptor: ① involved mainly in presynaptic modulation of histaminergic neurotransmission in the central nervous system. ② In the periphery, it appears to be a presynaptic heteroreceptor with modulatory effects on the release of other transmitters.
Tissues and Organ System Effects of Histamine � Exerts powerful effects on smooth and cardiac muscle, on certain endothelial and nerve cells, and on the secretory cells of the stomach. � Sensitivity to histamine varies greatly among species - Humans, guinea pigs, dogs, and cats are quite sensitive, while mice and rats are much less so.
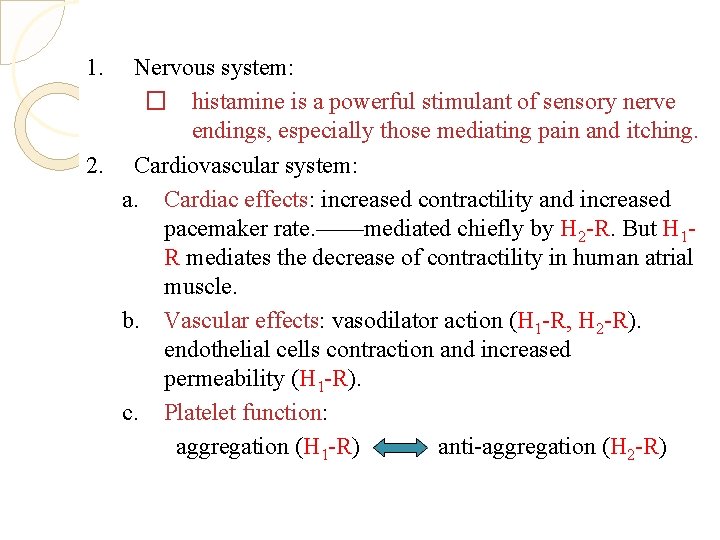
1. Nervous system: � histamine is a powerful stimulant of sensory nerve endings, especially those mediating pain and itching. 2. Cardiovascular system: a. Cardiac effects: increased contractility and increased pacemaker rate. ——mediated chiefly by H 2 -R. But H 1 R mediates the decrease of contractility in human atrial muscle. b. Vascular effects: vasodilator action (H 1 -R, H 2 -R). endothelial cells contraction and increased permeability (H 1 -R). c. Platelet function: aggregation (H 1 -R) anti-aggregation (H 2 -R)

3. 4. Smooth muscle: contraction (H 1 -R) → bronchoconstriction, abort. Histamine - induced contraction of guinea pig ileum is a standard bioassay for this amine. Secretory tissues: stimulant of gastric acid secretion and, to a lesser extent, of gastric pepsin and intrinsic factor production. (H 2 -R)
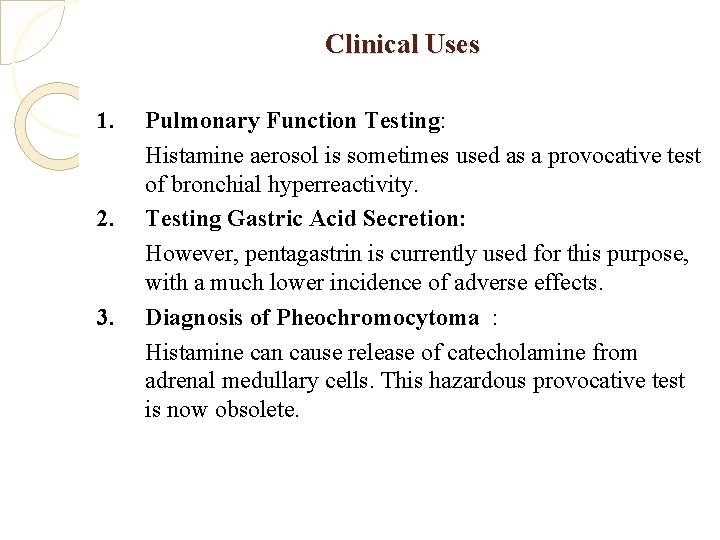
Clinical Uses 1. 2. 3. Pulmonary Function Testing: Histamine aerosol is sometimes used as a provocative test of bronchial hyperreactivity. Testing Gastric Acid Secretion: However, pentagastrin is currently used for this purpose, with a much lower incidence of adverse effects. Diagnosis of Pheochromocytoma : Histamine can cause release of catecholamine from adrenal medullary cells. This hazardous provocative test is now obsolete.
Clinical uses, toxicity and contraindications of histamine � Main clinical use of histamine is as a positive control injection for skin allergy testing's ADR’S: � Flushing � Hypotension � Headache � Wheal formation � Bronchoconstriction � Gastric acidity
Other Histamine Agonists � Betahistine : � Impromidine : � α-methylhistamine : H 1 -R agonist H 2 -R agonists H 3 -R agonists Histamine antagonists Receptor antagonists: � Selective types) blockade of histamine receptors (H 1, H 2, H 3

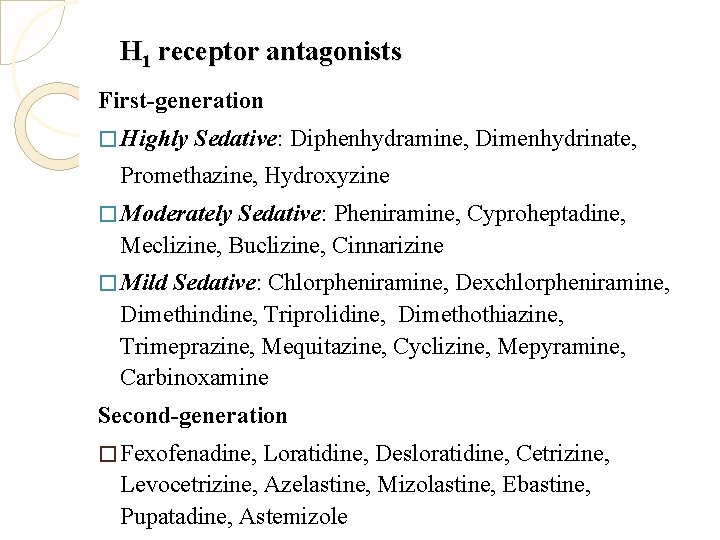
H 1 receptor antagonists First-generation � Highly Sedative: Diphenhydramine, Dimenhydrinate, Promethazine, Hydroxyzine � Moderately Sedative: Pheniramine, Cyproheptadine, Meclizine, Buclizine, Cinnarizine � Mild Sedative: Chlorpheniramine, Dexchlorpheniramine, Dimethindine, Triprolidine, Dimethothiazine, Trimeprazine, Mequitazine, Cyclizine, Mepyramine, Carbinoxamine Second-generation � Fexofenadine, Loratidine, Desloratidine, Cetrizine, Levocetrizine, Azelastine, Mizolastine, Ebastine, Pupatadine, Astemizole
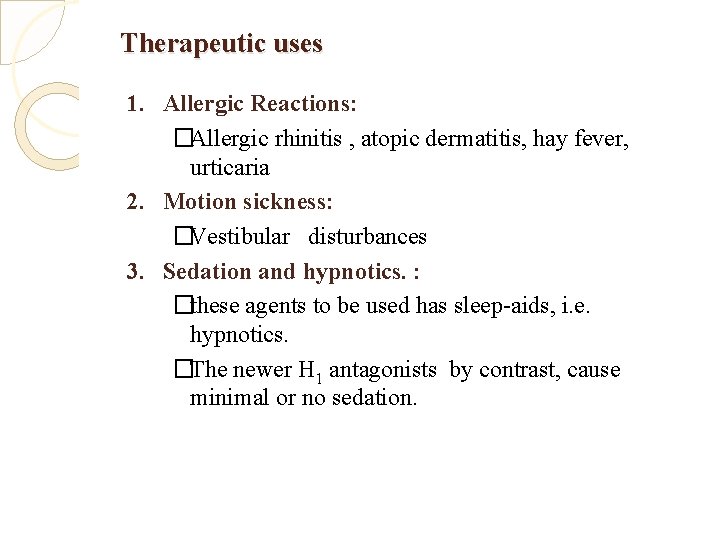
Therapeutic uses 1. Allergic Reactions: �Allergic rhinitis , atopic dermatitis, hay fever, urticaria 2. Motion sickness: �Vestibular disturbances 3. Sedation and hypnotics. : �these agents to be used has sleep-aids, i. e. hypnotics. �The newer H 1 antagonists by contrast, cause minimal or no sedation.

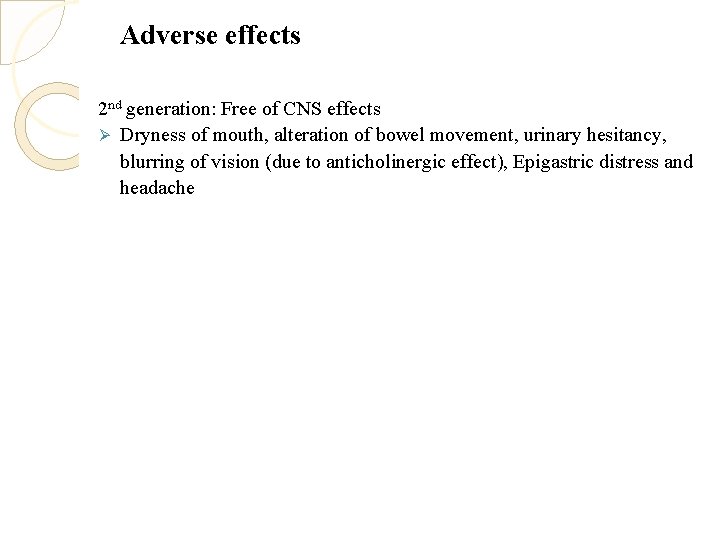
Adverse effects 2 nd generation: Free of CNS effects Ø Dryness of mouth, alteration of bowel movement, urinary hesitancy, blurring of vision (due to anticholinergic effect), Epigastric distress and headache
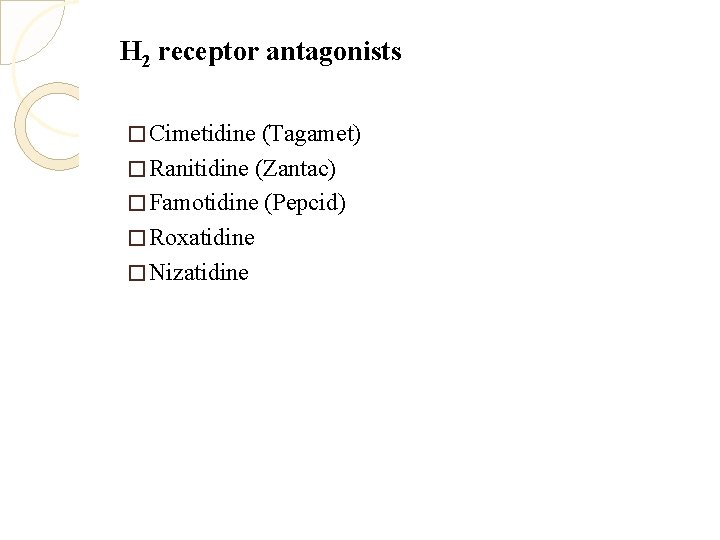
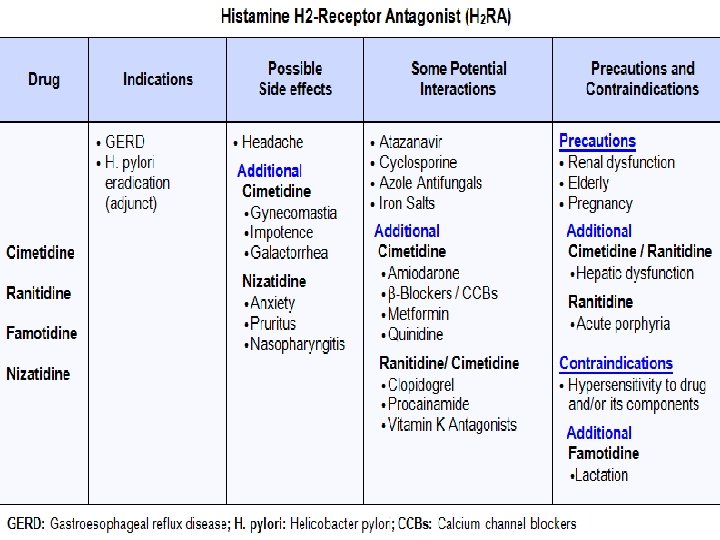
H 2 receptor antagonists � Cimetidine (Tagamet) � Ranitidine (Zantac) � Famotidine (Pepcid) � Roxatidine � Nizatidine
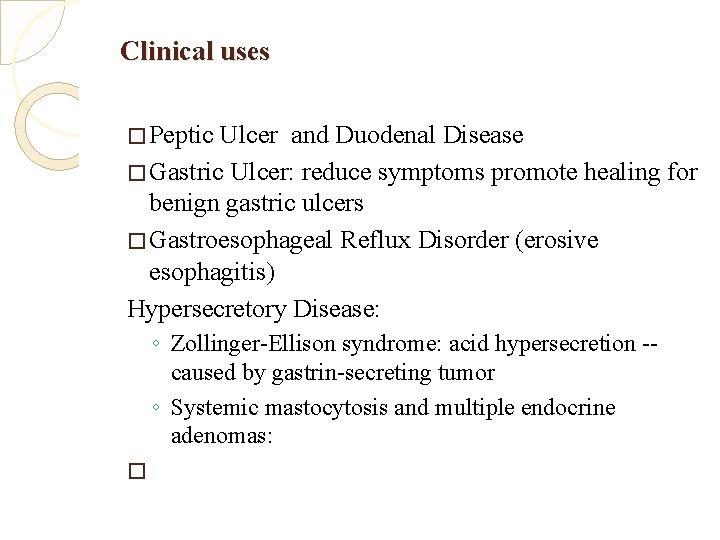
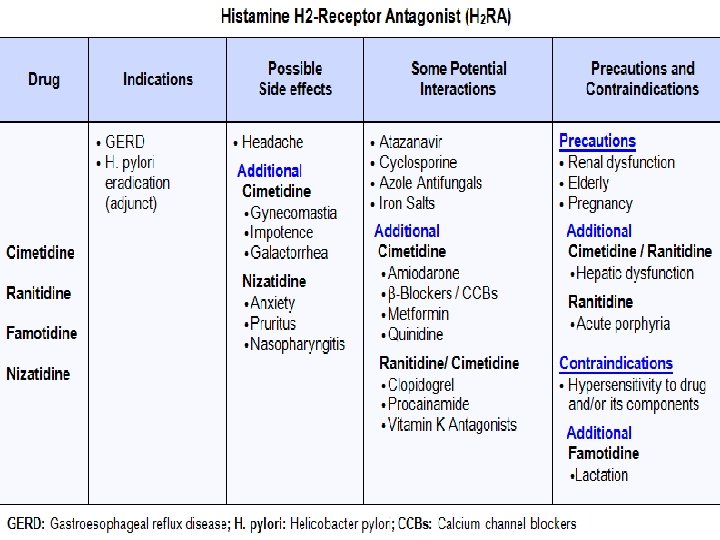
Clinical uses � Peptic Ulcer and Duodenal Disease � Gastric Ulcer: reduce symptoms promote healing for benign gastric ulcers � Gastroesophageal Reflux Disorder (erosive esophagitis) Hypersecretory Disease: ◦ Zollinger-Ellison syndrome: acid hypersecretion -caused by gastrin-secreting tumor ◦ Systemic mastocytosis and multiple endocrine adenomas: �
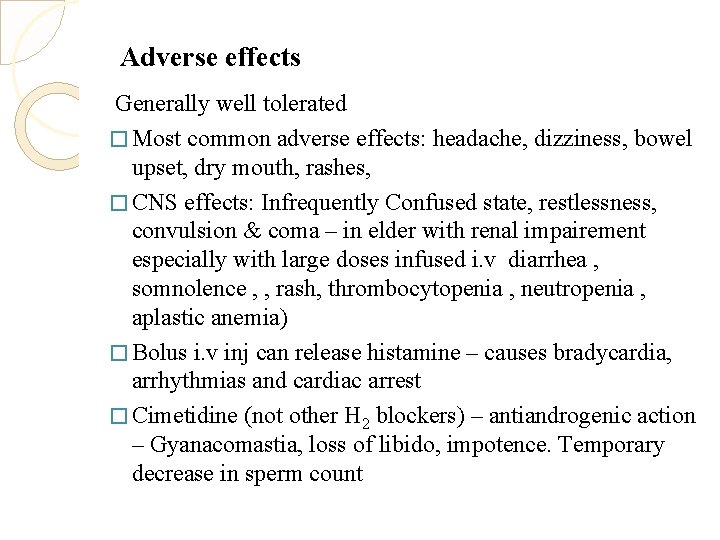
Adverse effects Generally well tolerated � Most common adverse effects: headache, dizziness, bowel upset, dry mouth, rashes, � CNS effects: Infrequently Confused state, restlessness, convulsion & coma – in elder with renal impairement especially with large doses infused i. v diarrhea , somnolence , , rash, thrombocytopenia , neutropenia , aplastic anemia) � Bolus i. v inj can release histamine – causes bradycardia, arrhythmias and cardiac arrest � Cimetidine (not other H 2 blockers) – antiandrogenic action – Gyanacomastia, loss of libido, impotence. Temporary decrease in sperm count
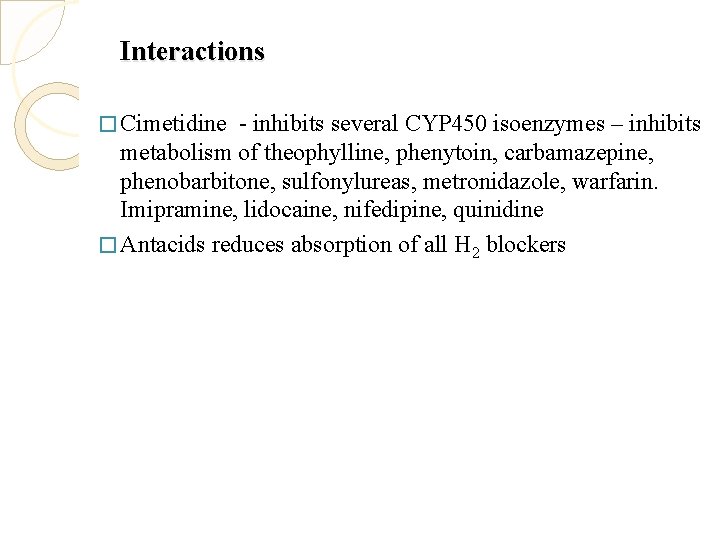
Interactions � Cimetidine - inhibits several CYP 450 isoenzymes – inhibits metabolism of theophylline, phenytoin, carbamazepine, phenobarbitone, sulfonylureas, metronidazole, warfarin. Imipramine, lidocaine, nifedipine, quinidine � Antacids reduces absorption of all H 2 blockers

 Diaminooxydase
Diaminooxydase N chalapathi
N chalapathi Tidal percussion
Tidal percussion Pharmacology of drugs acting on respiratory system
Pharmacology of drugs acting on respiratory system Adrenal drugs pharmacology
Adrenal drugs pharmacology Triple response of histamine
Triple response of histamine Bronchodilator drugs
Bronchodilator drugs Histamine
Histamine Histamine
Histamine Histamine test brachial plexus
Histamine test brachial plexus Autacoids classification
Autacoids classification Medical education and drugs department
Medical education and drugs department Venipuncture for radiologic technologists
Venipuncture for radiologic technologists Chapter 15 diagnostic procedures and pharmacology
Chapter 15 diagnostic procedures and pharmacology Toxicology and applied pharmacology
Toxicology and applied pharmacology Annual review of pharmacology and toxicology
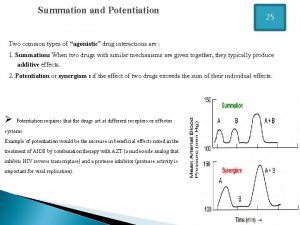
Annual review of pharmacology and toxicology Potentiation example
Potentiation example Creatinine clearance formula
Creatinine clearance formula What is ion trapping in pharmacology
What is ion trapping in pharmacology Drug metabolism definition
Drug metabolism definition Chapter 30 principles of pharmacology
Chapter 30 principles of pharmacology Ion trapping
Ion trapping What is pharmacology
What is pharmacology Summary of drug administration
Summary of drug administration First pass effect
First pass effect Mechanism of drug action
Mechanism of drug action First pass metabolism definition pharmacology
First pass metabolism definition pharmacology Alpha 1 vs alpha 2 receptors
Alpha 1 vs alpha 2 receptors