Highlights AUA 2017 Ca de Prstata Antonio Carlos


- Slides: 43
Highlights AUA 2017 - Ca de Próstata Antonio Carlos Lima Pompeo Prof. Titular - Disciplina de Urologia – FM-ABC Coordenador Depto Uro-Oncologia - SBU
Take Home Messages: Prostate Cancer Kirsten Greene, MD, MS, FACS Associate Professor and Vice Chair Department of Urology, UCSF
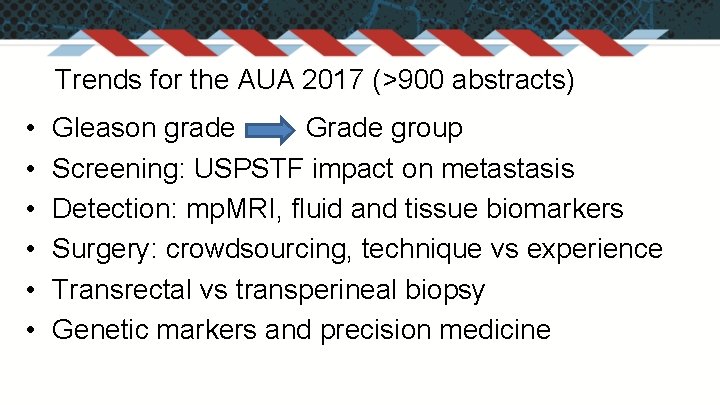
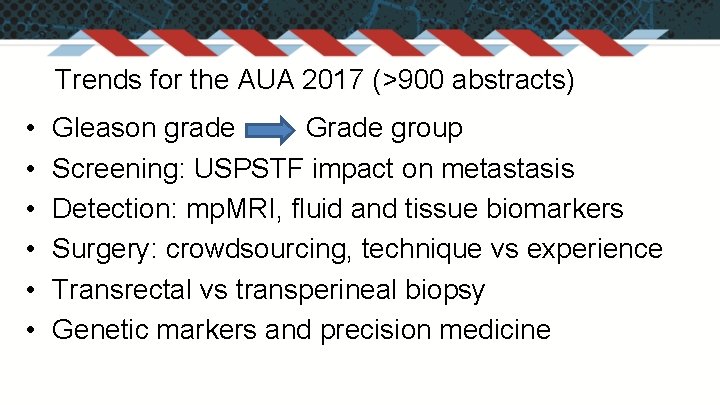
Trends for the AUA 2017 (>900 abstracts) • • • Gleason grade Grade group Screening: USPSTF impact on metastasis Detection: mp. MRI, fluid and tissue biomarkers Surgery: crowdsourcing, technique vs experience Transrectal vs transperineal biopsy Genetic markers and precision medicine
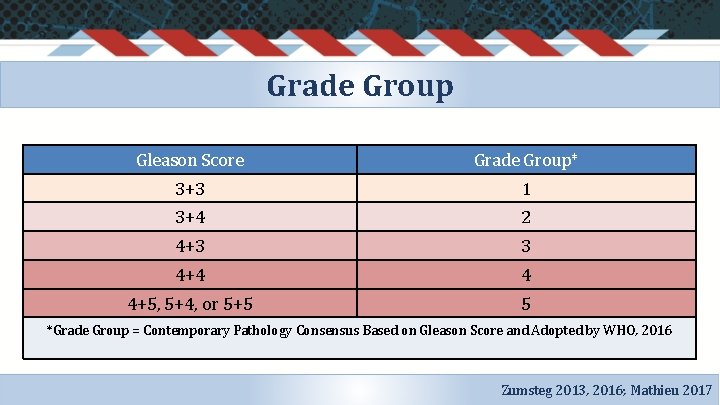
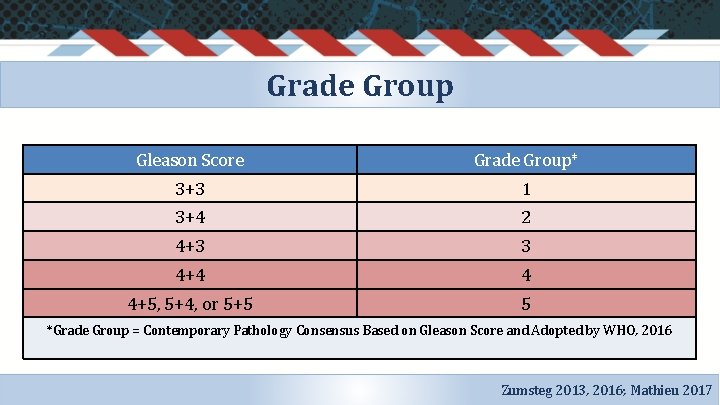
Grade Group Gleason Score Grade Group* 3+3 1 3+4 2 4+3 3 4+4 4 4+5, 5+4, or 5+5 5 *Grade Group = Contemporary Pathology Consensus Based on Gleason Score and Adopted by WHO, 2016 Zumsteg 2013, 2016; Mathieu 2017
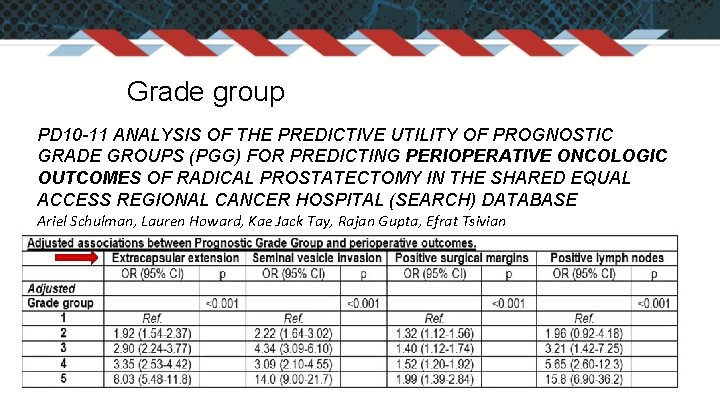
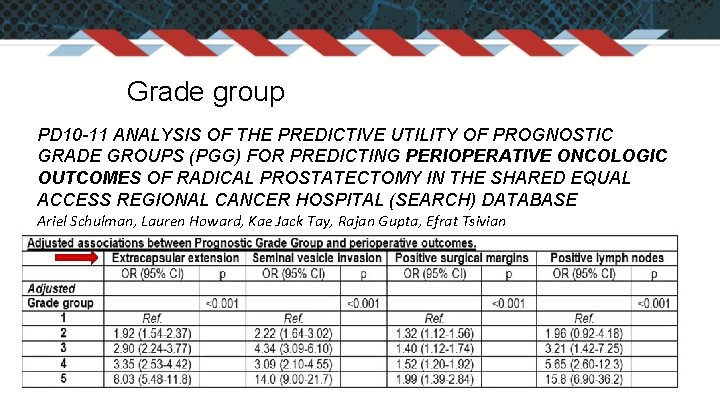
Grade group PD 10 -11 ANALYSIS OF THE PREDICTIVE UTILITY OF PROGNOSTIC GRADE GROUPS (PGG) FOR PREDICTING PERIOPERATIVE ONCOLOGIC OUTCOMES OF RADICAL PROSTATECTOMY IN THE SHARED EQUAL ACCESS REGIONAL CANCER HOSPITAL (SEARCH) DATABASE Ariel Schulman, Lauren Howard, Kae Jack Tay, Rajan Gupta, Efrat Tsivian
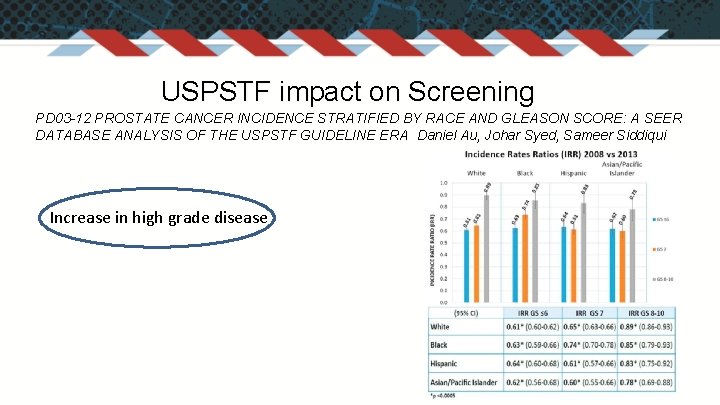
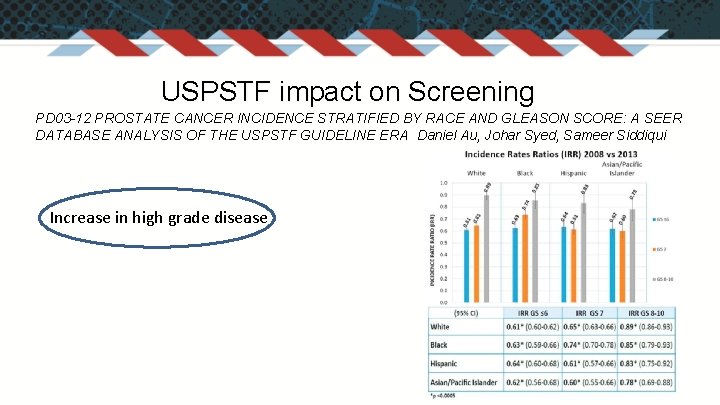
USPSTF impact on Screening PD 03 -12 PROSTATE CANCER INCIDENCE STRATIFIED BY RACE AND GLEASON SCORE: A SEER DATABASE ANALYSIS OF THE USPSTF GUIDELINE ERA Daniel Au, Johar Syed, Sameer Siddiqui Increase in high grade disease
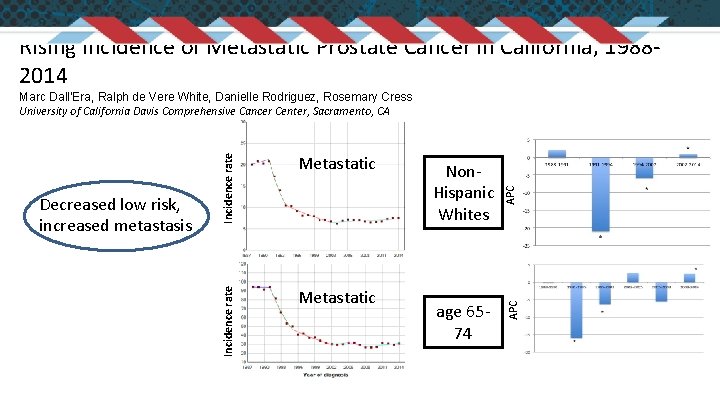
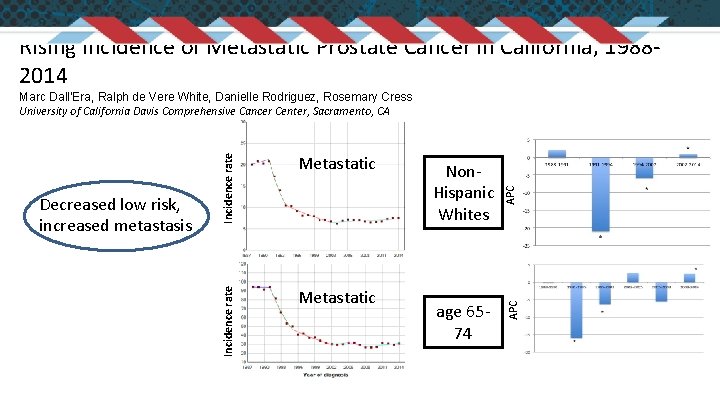
Rising Incidence of Metastatic Prostate Cancer in California, 19882014 age 6574 APC Metastatic Non. Hispanic Whites APC Incidence rate Decreased low risk, increased metastasis Metastatic Incidence rate Marc Dall’Era, Ralph de Vere White, Danielle Rodriguez, Rosemary Cress University of California Davis Comprehensive Cancer Center, Sacramento, CA
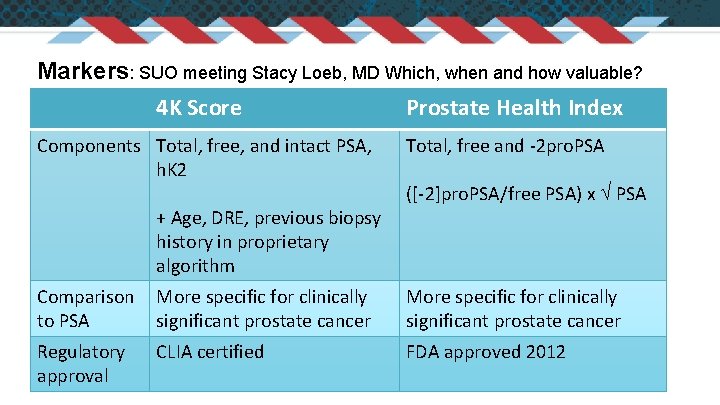
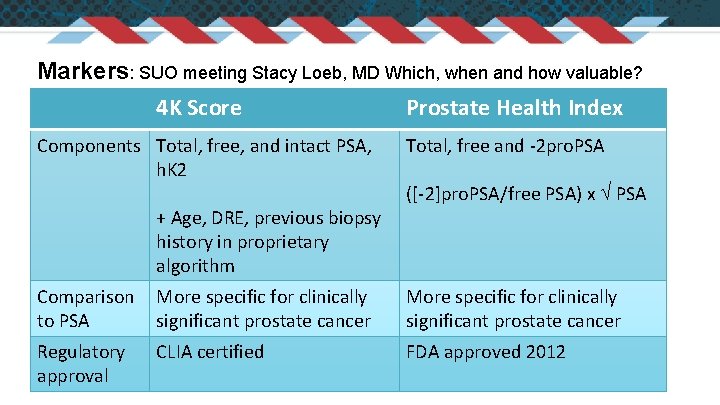
Detection: MRI, urine, serum, tissue markers Markers: SUO meeting Stacy Loeb, MD Which, when and how valuable? 4 K Score Prostate Health Index Components Total, free, and intact PSA, h. K 2 + Age, DRE, previous biopsy history in proprietary algorithm Total, free and -2 pro. PSA ([-2]pro. PSA/free PSA) x PSA Comparison More specific for clinically to PSA significant prostate cancer More specific for clinically significant prostate cancer Regulatory approval FDA approved 2012 CLIA certified
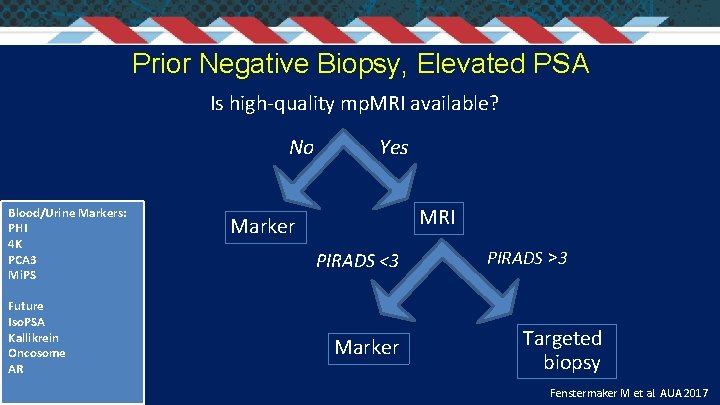
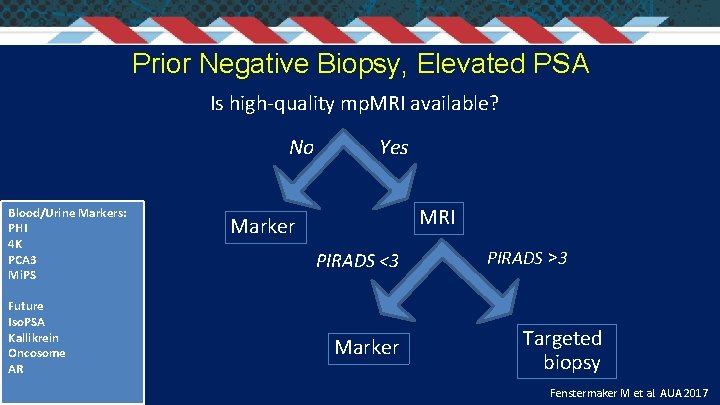
Prior Negative Biopsy, Elevated PSA Is high-quality mp. MRI available? No Blood/Urine Markers: PHI 4 K PCA 3 Mi. PS Future Iso. PSA Kallikrein Oncosome AR Yes MRI Marker PIRADS <3 Marker PIRADS >3 Targeted biopsy Fenstermaker M et al. AUA 2017
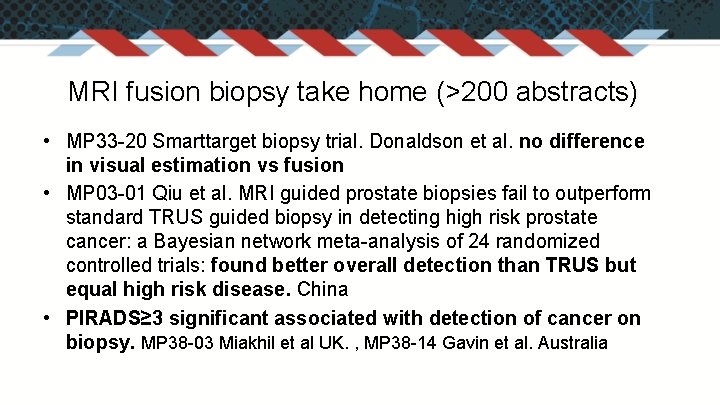
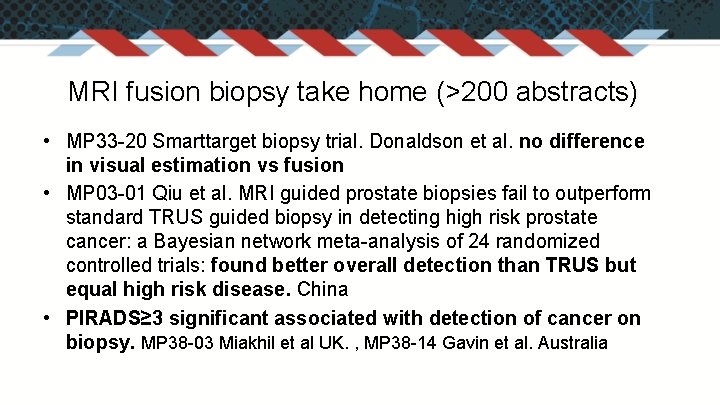
MRI fusion biopsy take home (>200 abstracts) • MP 33 -20 Smarttarget biopsy trial. Donaldson et al. no difference in visual estimation vs fusion • MP 03 -01 Qiu et al. MRI guided prostate biopsies fail to outperform standard TRUS guided biopsy in detecting high risk prostate cancer: a Bayesian network meta-analysis of 24 randomized controlled trials: found better overall detection than TRUS but equal high risk disease. China • PIRADS≥ 3 significant associated with detection of cancer on biopsy. MP 38 -03 Miakhil et al UK. , MP 38 -14 Gavin et al. Australia
Transperineal vs transrectal biopsy approach • Both with mp. MRI fusion or cognitive • Lower infection rates with transperineal biopsy • Anesthesia vs office based, costs
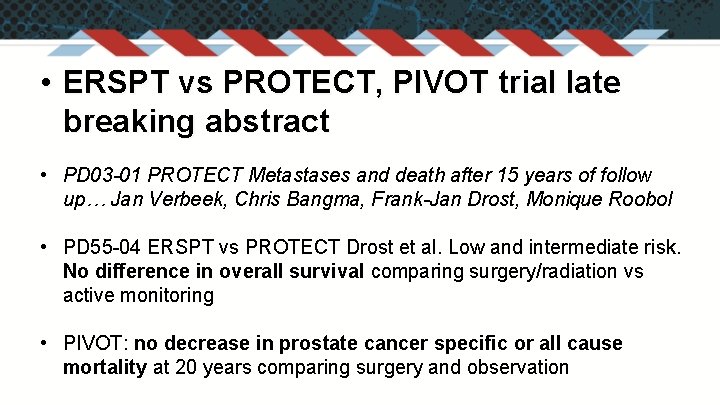
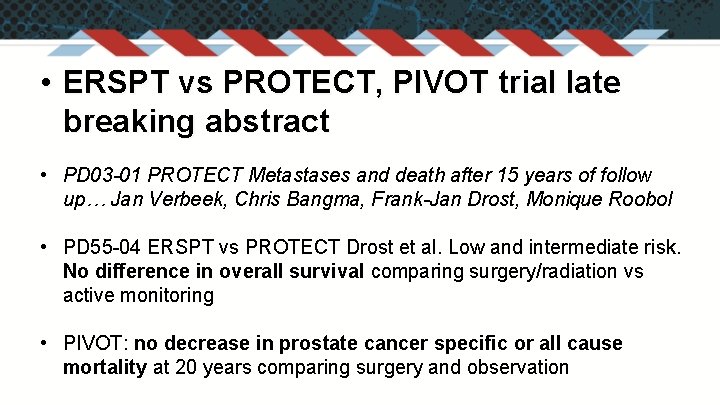
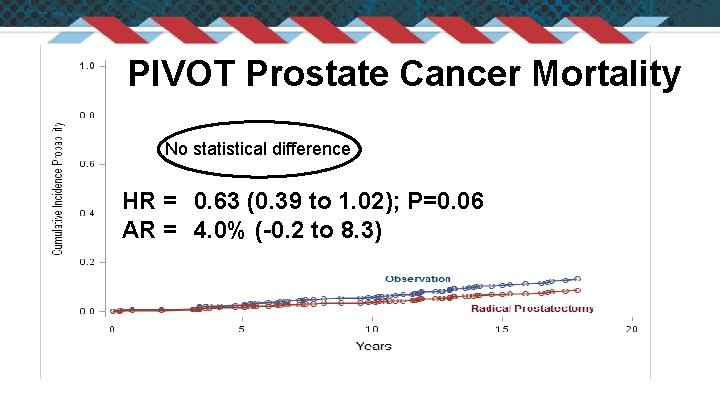
• ERSPT vs PROTECT, PIVOT trial late breaking abstract • PD 03 -01 PROTECT Metastases and death after 15 years of follow up… Jan Verbeek, Chris Bangma, Frank-Jan Drost, Monique Roobol • PD 55 -04 ERSPT vs PROTECT Drost et al. Low and intermediate risk. No difference in overall survival comparing surgery/radiation vs active monitoring • PIVOT: no decrease in prostate cancer specific or all cause mortality at 20 years comparing surgery and observation
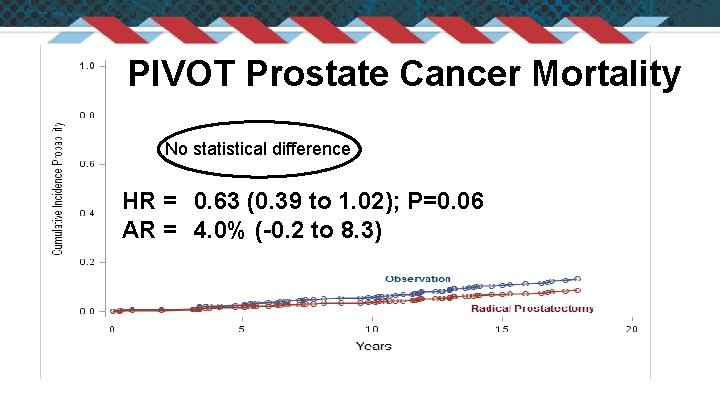
PIVOT Prostate Cancer Mortality No statistical difference HR = 0. 63 (0. 39 to 1. 02); P=0. 06 AR = 4. 0% (-0. 2 to 8. 3)
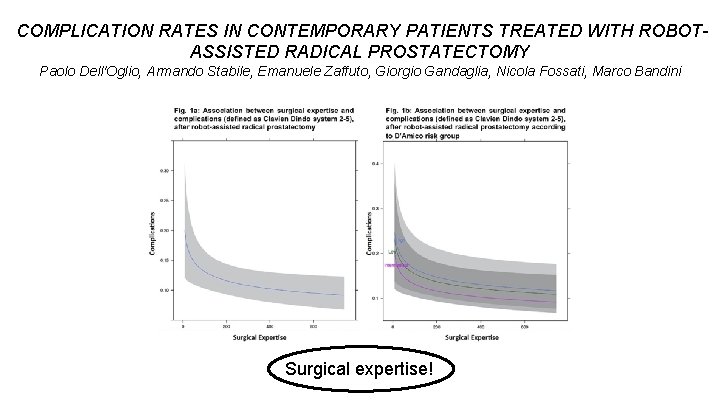
Surgery • Technique not as important as experience • Crowdsourcing can identify expertise • Open=robotic: outcomes and quality of life but better than laparoscopic • Fluorescent lymph node identification • Retzius sparing approach
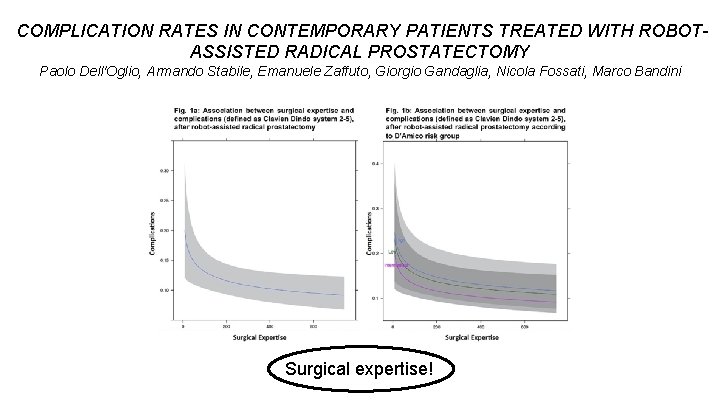
COMPLICATION RATES IN CONTEMPORARY PATIENTS TREATED WITH ROBOTASSISTED RADICAL PROSTATECTOMY Paolo Dell'Oglio, Armando Stabile, Emanuele Zaffuto, Giorgio Gandaglia, Nicola Fossati, Marco Bandini DOI: 10. 1016/j. juro. 2017. 02. 3292 Surgical expertise!

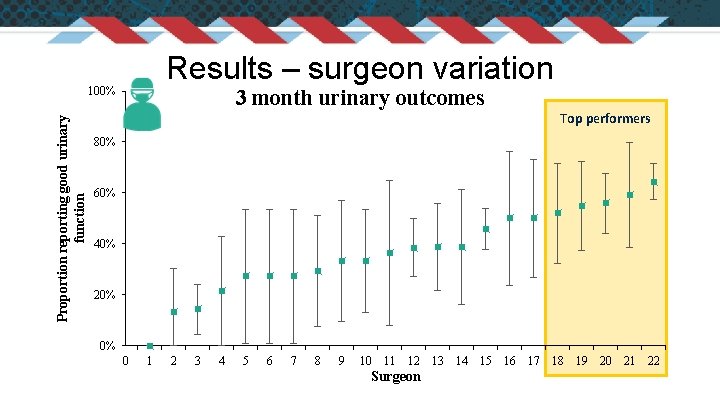
Measuring to improve: patient reported outcomes during the first year after prostatectomy in a statewide collaborative Gregory B. Auffenberg*, Ji Qi, Rodney L. Dunn, Tae Kim, James Peabody, Mani Menon, and David C. Miller for the Michigan Urological Surgery Improvement Collaborative
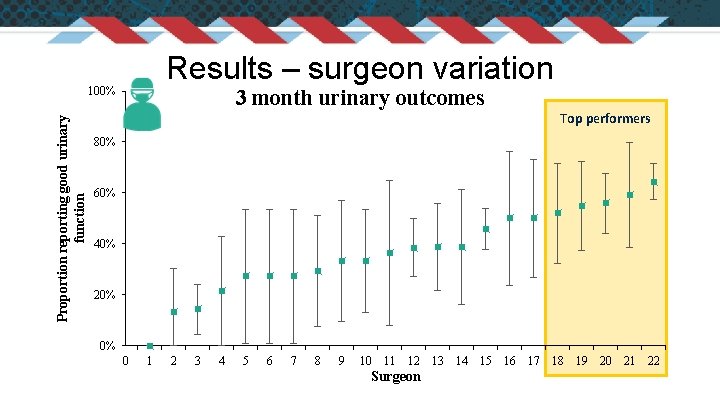
Results – surgeon variation Proportion reporting good urinary function 100% 3 month urinary outcomes Top performers 80% 60% 40% 20% 0% 0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 Surgeon
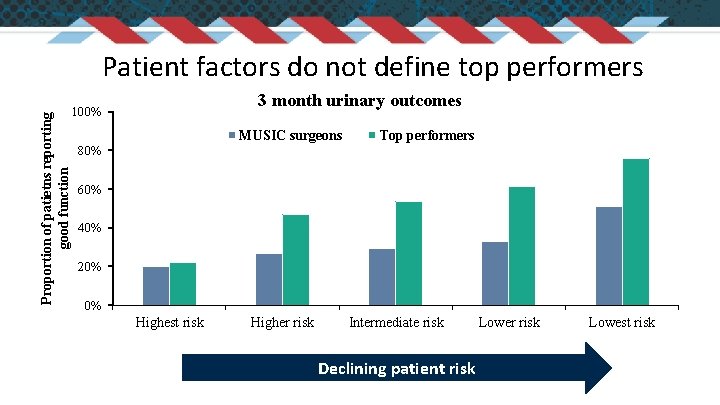
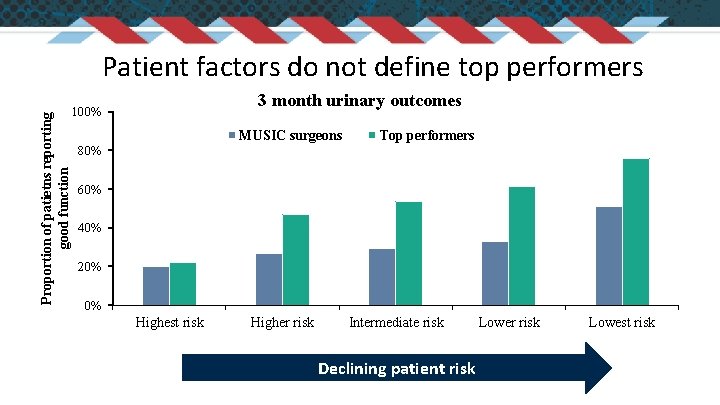
Proportion of patietns reporting good function Patient factors do not define top performers 3 month urinary outcomes 100% MUSIC surgeons Top performers 80% 60% 40% 20% 0% Highest risk Higher risk Intermediate risk Declining patient risk Lower risk Lowest risk
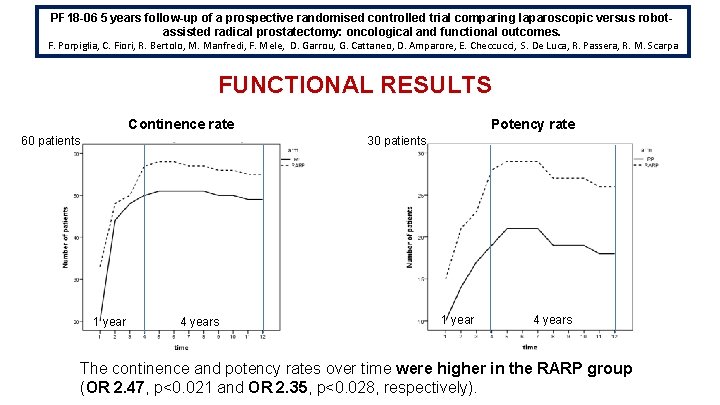
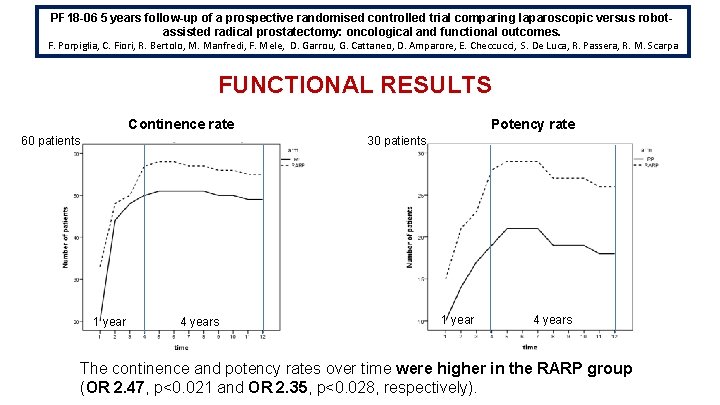
PF 18 -06 5 years follow-up of a prospective randomised controlled trial comparing laparoscopic versus robotassisted radical prostatectomy: oncological and functional outcomes. F. Porpiglia, C. Fiori, R. Bertolo, M. Manfredi, F. Mele, D. Garrou, G. Cattaneo, D. Amparore, E. Checcucci, S. De Luca, R. Passera, R. M. Scarpa FUNCTIONAL RESULTS Continence rate 60 patients Potency rate 30 patients 1 year 4 years The continence and potency rates over time were higher in the RARP group (ORb) 2. 47, p<0. 021 and OR 2. 35, p<0. 028, respectively).
Prospective Multicenter Comparison of Open and Robotic Radical Prostatectomy: The PROST-QA and PROST-QA/RP 2 Consortiums Peter Chang MD MPH, Andrew Wagner MD, Meredith Regan Sc. D, Dattatraya Patil MBBS MPH, Catrina Crociani MPH, Larry Hembroff Ph. D, Linda Stork, Kyle Davis, John Wei MD MS, David Wood MD, Chris Saigal MD MPH, Mark Litwin MD MPH, Jim Hu MD MPH, Eric Klein MD, Adam Kibel MD, Gerald Andriole MD, Matthew Cooperberg MD MPH, Peter Carroll MD MPH, Joseph Smith MD, Misop Han MD, Alan Partin MD Ph. D, Martin Sanda MD, and the PROST-QA and PROST-QA/RP 2 Consortiums
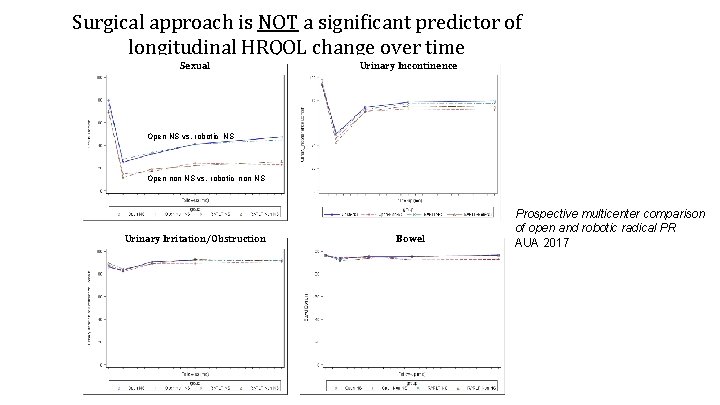
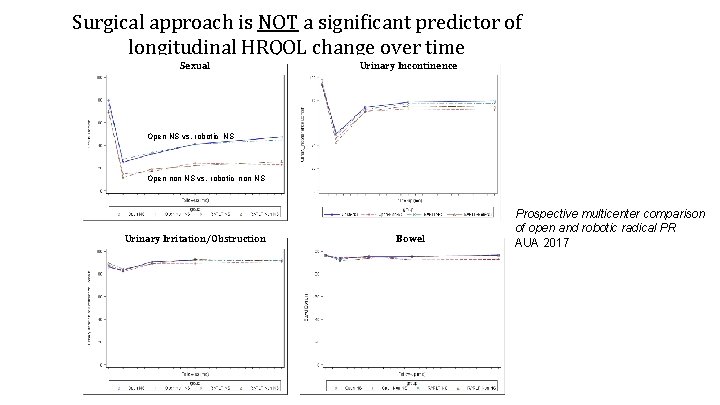
Surgical approach is NOT a significant predictor of longitudinal HRQOL change over time Sexual Urinary Incontinence Open NS vs. robotic NS Open non NS vs. robotic non NS Urinary Irritation/Obstruction Bowel Prospective multicenter comparison of open and robotic radical PR AUA 2017
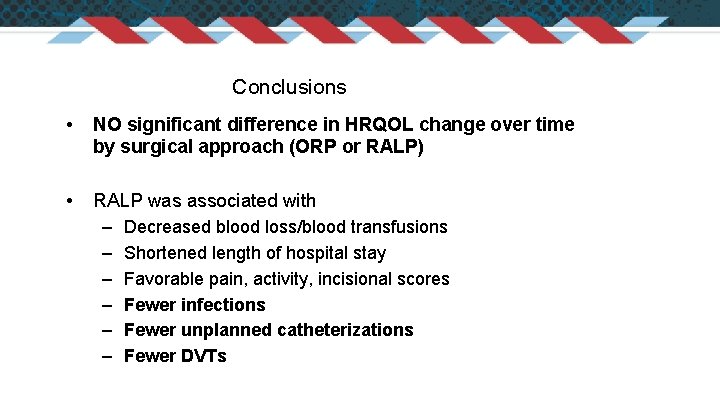
Conclusions • NO significant difference in HRQOL change over time by surgical approach (ORP or RALP) • RALP was associated with – Decreased blood loss/blood transfusions – Shortened length of hospital stay – Favorable pain, activity, incisional scores – Fewer infections – Fewer unplanned catheterizations – Fewer DVTs
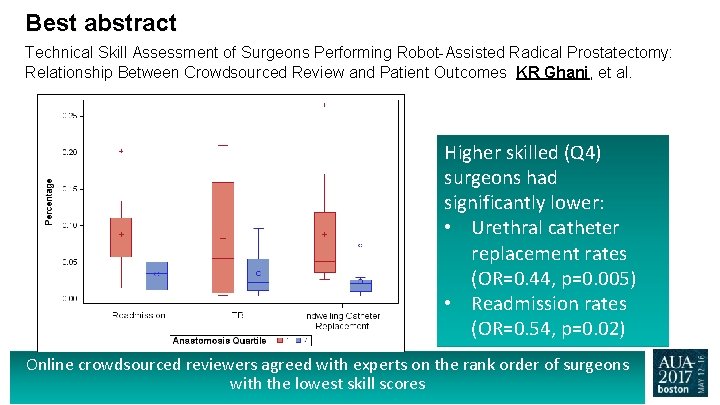
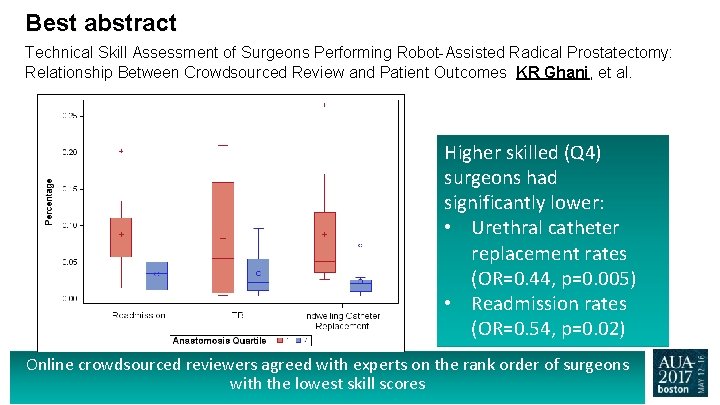
Best abstract Technical Skill Assessment of Surgeons Performing Robot-Assisted Radical Prostatectomy: Relationship Between Crowdsourced Review and Patient Outcomes KR Ghani, et al. Higher skilled (Q 4) surgeons had significantly lower: • Urethral catheter replacement rates (OR=0. 44, p=0. 005) • Readmission rates (OR=0. 54, p=0. 02) Online crowdsourced reviewers agreed with experts on the rank order of surgeons with the lowest skill scores
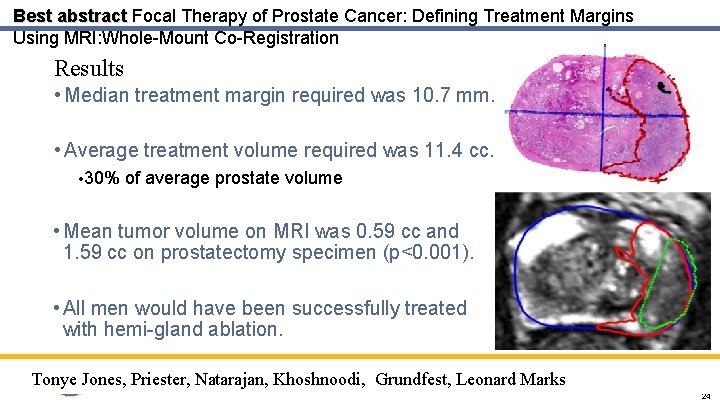
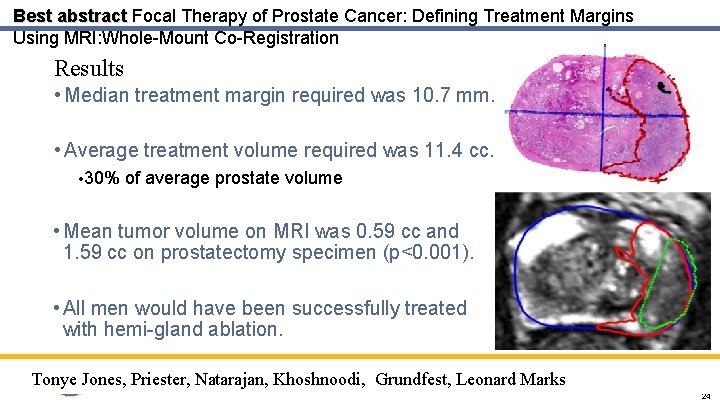
Best abstract Focal Therapy of Prostate Cancer: Defining Treatment Margins Using MRI: Whole-Mount Co-Registration Results • Median treatment margin required was 10. 7 mm. • Average treatment volume required was 11. 4 cc. • 30% of average prostate volume • Mean tumor volume on MRI was 0. 59 cc and 1. 59 cc on prostatectomy specimen (p<0. 001). • All men would have been successfully treated with hemi-gland ablation. Tonye Jones, Priester, Natarajan, Khoshnoodi, Grundfest, Leonard Marks 24
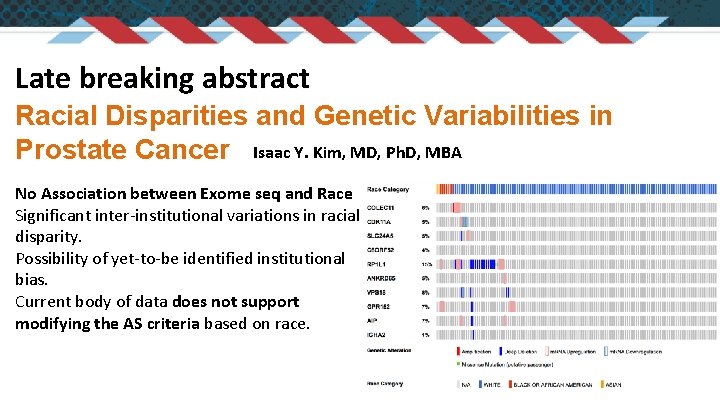
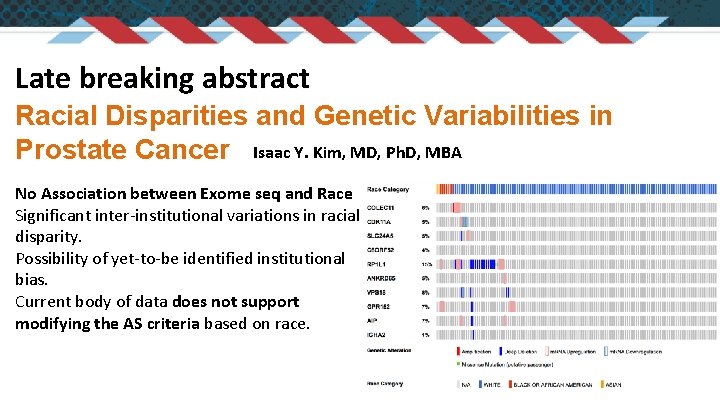
Late breaking abstract Racial Disparities and Genetic Variabilities in Prostate Cancer Isaac Y. Kim, MD, Ph. D, MBA No Association between Exome seq and Race Significant inter-institutional variations in racial disparity. Possibility of yet-to-be identified institutional bias. Current body of data does not support modifying the AS criteria based on race.
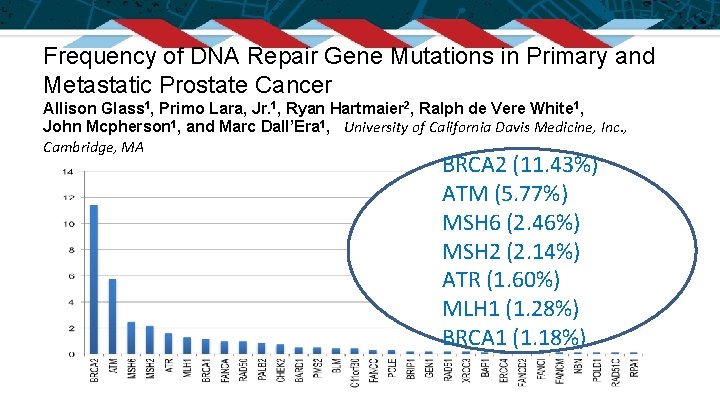
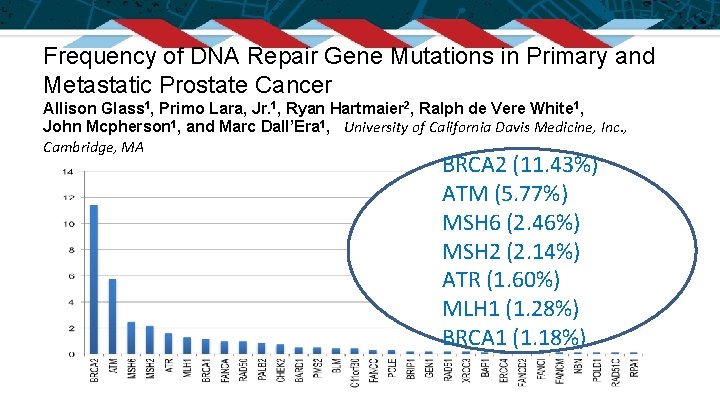
Frequency of DNA Repair Gene Mutations in Primary and Metastatic Prostate Cancer Allison Glass 1, Primo Lara, Jr. 1, Ryan Hartmaier 2, Ralph de Vere White 1, John Mcpherson 1, and Marc Dall’Era 1, University of California Davis Medicine, Inc. , Cambridge, MA BRCA 2 (11. 43%) ATM (5. 77%) MSH 6 (2. 46%) MSH 2 (2. 14%) ATR (1. 60%) MLH 1 (1. 28%) BRCA 1 (1. 18%)
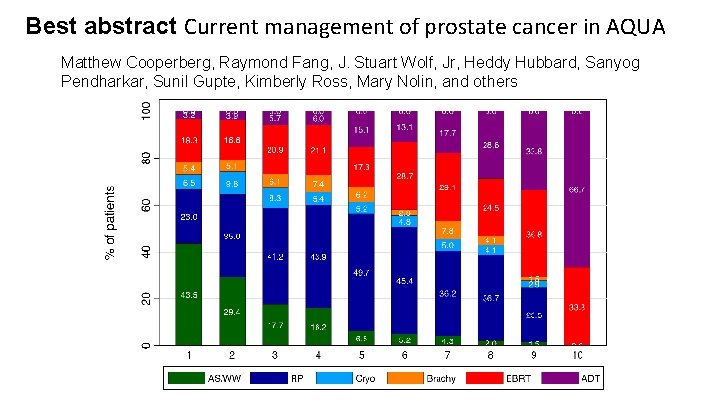
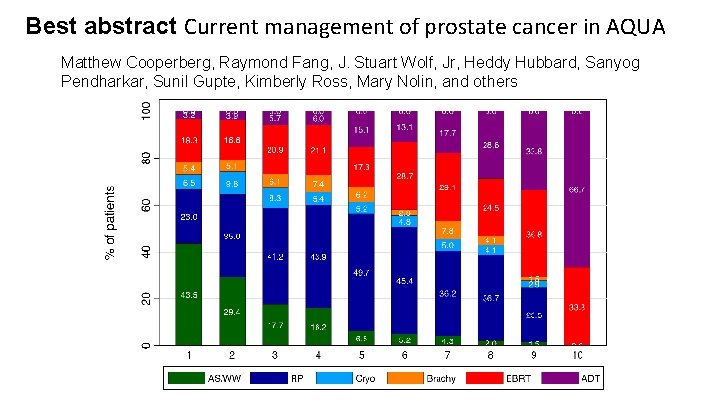
Best abstract Current management of prostate cancer in AQUA Matthew Cooperberg, Raymond Fang, J. Stuart Wolf, Jr, Heddy Hubbard, Sanyog Pendharkar, Sunil Gupte, Kimberly Ross, Mary Nolin, and others
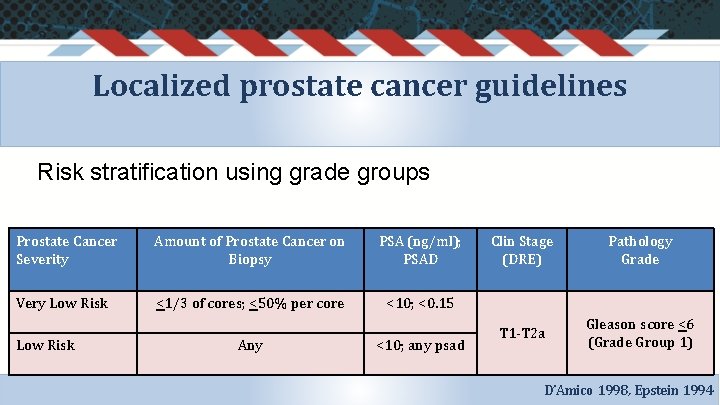
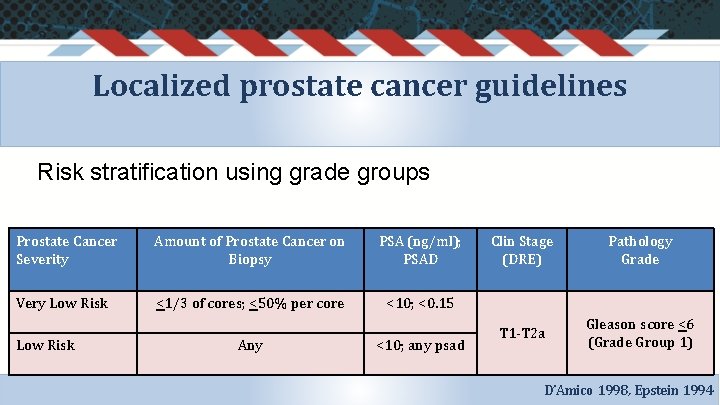
Localized prostate cancer guidelines Risk stratification using grade groups Prostate Cancer Severity Amount of Prostate Cancer on Biopsy PSA (ng/ml); PSAD Very Low Risk <1/3 of cores; <50% per core <10; <0. 15 Low Risk Any <10; any psad Clin Stage (DRE) Pathology Grade T 1 -T 2 a Gleason score <6 (Grade Group 1) D’Amico 1998, Epstein 1994
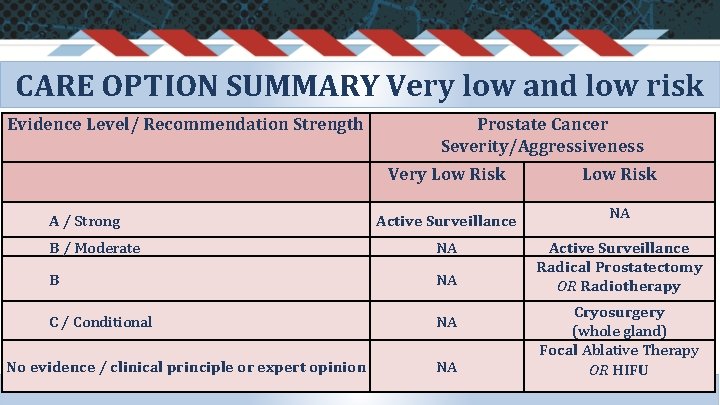
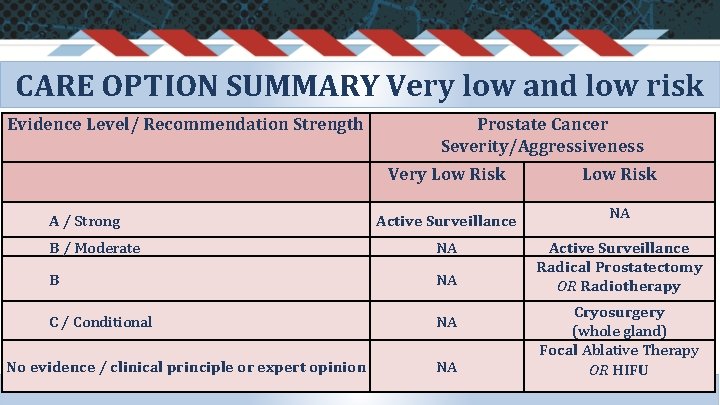
CARE OPTION SUMMARY Very low and low risk Evidence Level/ Recommendation Strength Prostate Cancer Severity/Aggressiveness Very Low Risk Active Surveillance NA B / Moderate NA B NA Active Surveillance Radical Prostatectomy OR Radiotherapy C / Conditional NA A / Strong No evidence / clinical principle or expert opinion NA Cryosurgery (whole gland) Focal Ablative Therapy OR HIFU
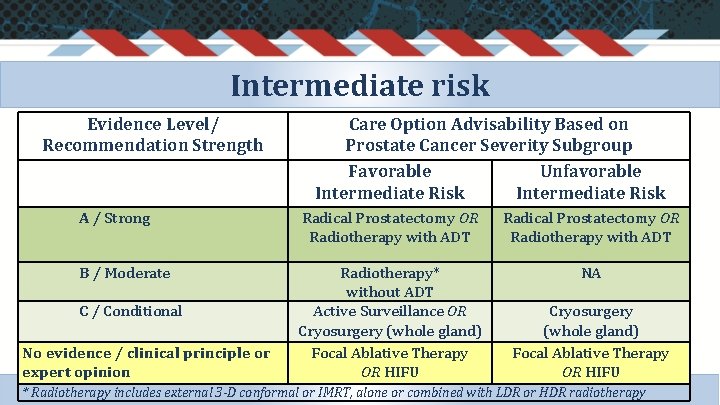
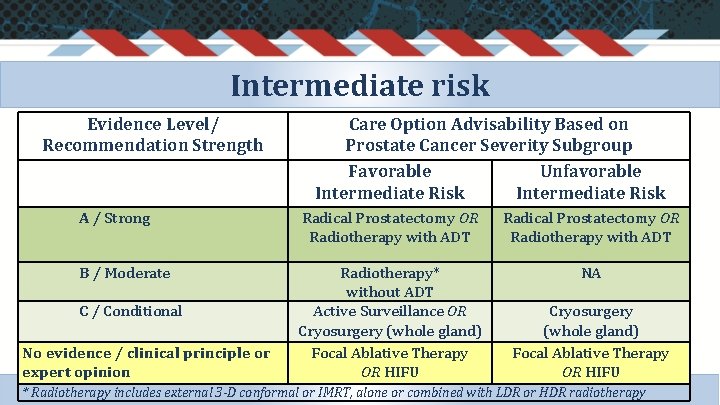
Intermediate risk Evidence Level/ Recommendation Strength Care Option Advisability Based on Prostate Cancer Severity Subgroup Favorable Unfavorable Intermediate Risk A / Strong Radical Prostatectomy OR Radiotherapy with ADT B / Moderate Radiotherapy* without ADT Active Surveillance OR Cryosurgery (whole gland) Focal Ablative Therapy OR HIFU NA C / Conditional No evidence / clinical principle or expert opinion Cryosurgery (whole gland) Focal Ablative Therapy OR HIFU * Radiotherapy includes external 3 -D conformal or IMRT, alone or combined with LDR or HDR radiotherapy
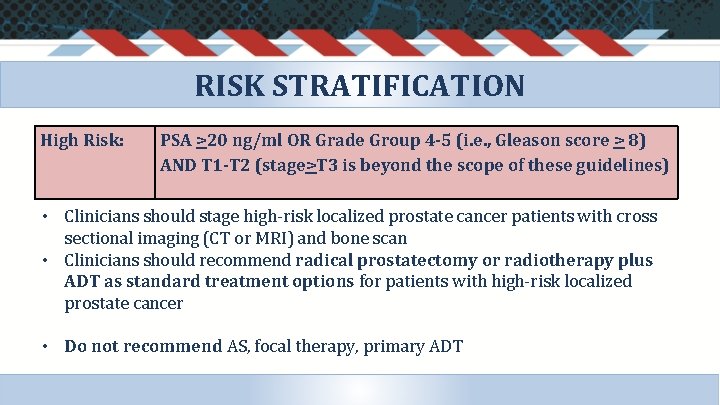
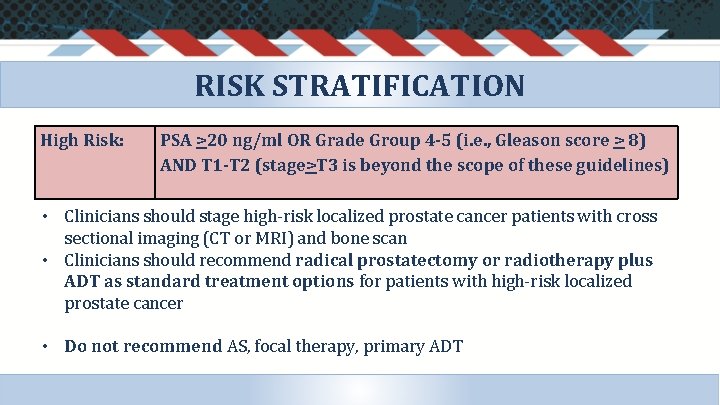
RISK STRATIFICATION High Risk: PSA >20 ng/ml OR Grade Group 4 -5 (i. e. , Gleason score > 8) AND T 1 -T 2 (stage>T 3 is beyond the scope of these guidelines) • Clinicians should stage high-risk localized prostate cancer patients with cross sectional imaging (CT or MRI) and bone scan • Clinicians should recommend radical prostatectomy or radiotherapy plus ADT as standard treatment options for patients with high-risk localized prostate cancer • Do not recommend AS, focal therapy, primary ADT
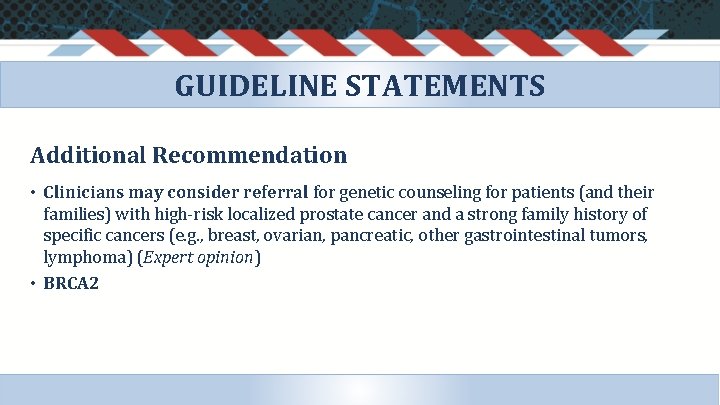
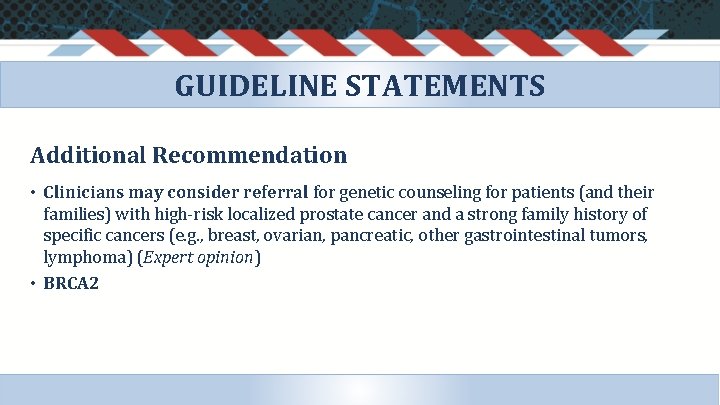
GUIDELINE STATEMENTS Additional Recommendation • Clinicians may consider referral for genetic counseling for patients (and their families) with high-risk localized prostate cancer and a strong family history of specific cancers (e. g. , breast, ovarian, pancreatic, other gastrointestinal tumors, lymphoma) (Expert opinion) • BRCA 2
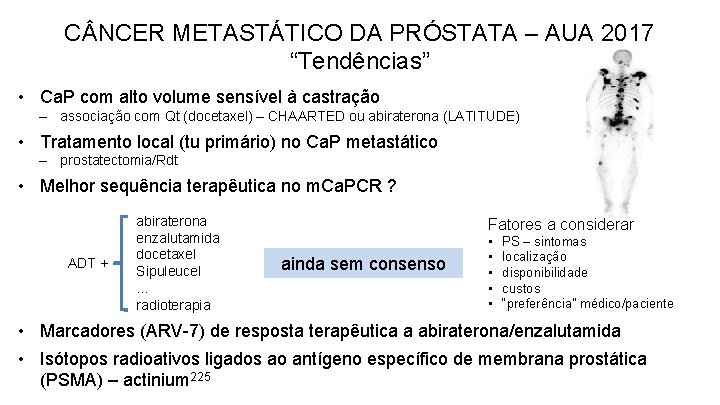
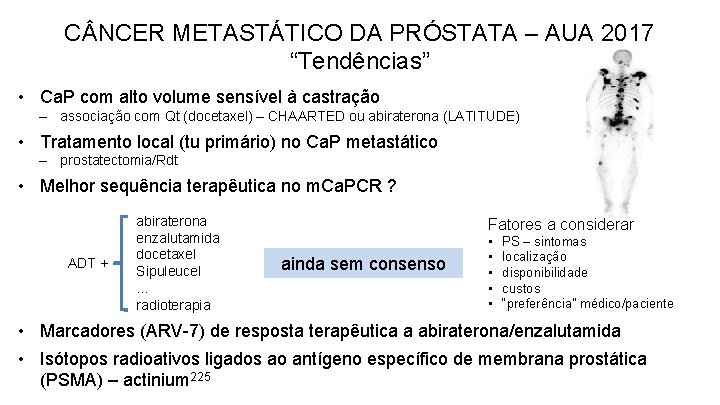
C NCER METASTÁTICO DA PRÓSTATA – AUA 2017 “Tendências” • Ca. P com alto volume sensível à castração – associação com Qt (docetaxel) – CHAARTED ou abiraterona (LATITUDE) • Tratamento local (tu primário) no Ca. P metastático – prostatectomia/Rdt • Melhor sequência terapêutica no m. Ca. PCR ? ADT + abiraterona enzalutamida docetaxel Sipuleucel. . . radioterapia Fatores a considerar ainda sem consenso • • • PS – sintomas localização disponibilidade custos “preferência” médico/paciente • Marcadores (ARV-7) de resposta terapêutica a abiraterona/enzalutamida • Isótopos radioativos ligados ao antígeno específico de membrana prostática (PSMA) – actinium 225
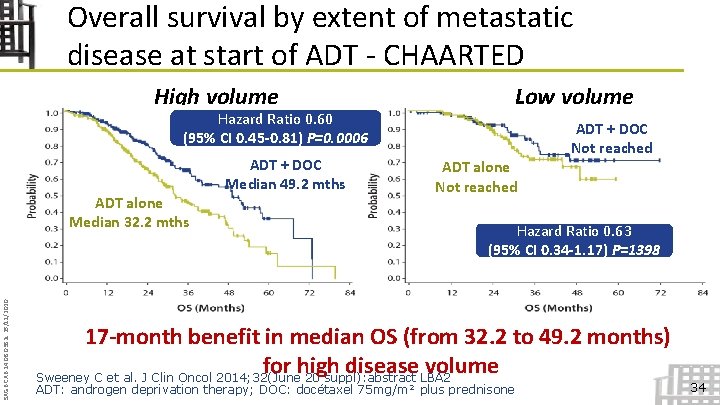
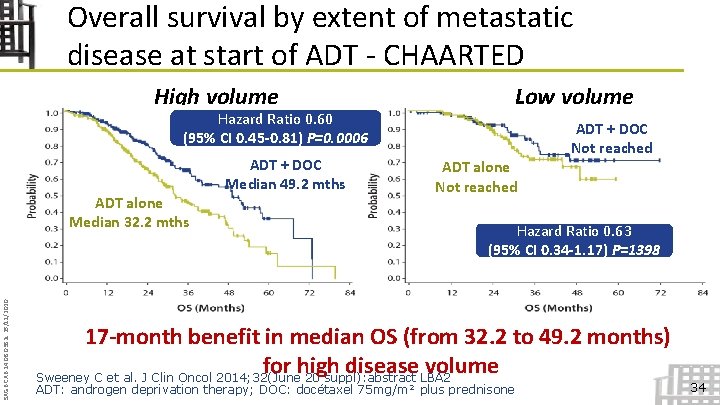
Overall survival by extent of metastatic disease at start of ADT - CHAARTED High volume Hazard Ratio 0. 60 (95% CI 0. 45 -0. 81) P=0. 0006 SAGB. CAB. 14. 08. 0382 c 25/11/2020 ADT alone Median 32. 2 mths ADT + DOC Median 49. 2 mths Low volume ADT + DOC Not reached ADT alone Not reached Hazard Ratio 0. 63 (95% CI 0. 34 -1. 17) P=1398 17 -month benefit in median OS (from 32. 2 to 49. 2 months) for high disease volume Sweeney C et al. J Clin Oncol 2014; 32(June 20 suppl): abstract LBA 2 ADT: androgen deprivation therapy; DOC: docétaxel 75 mg/m² plus prednisone 34
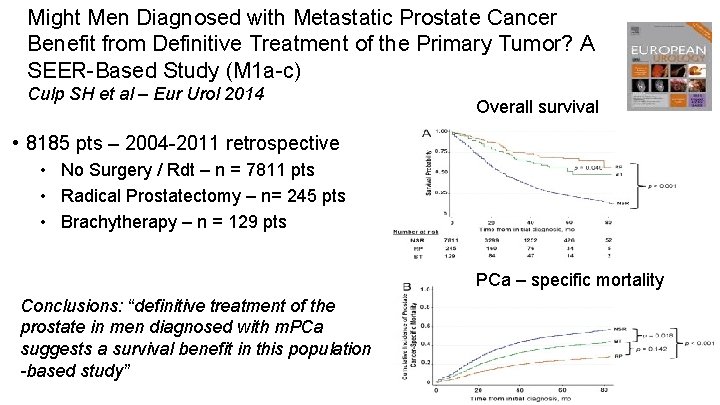
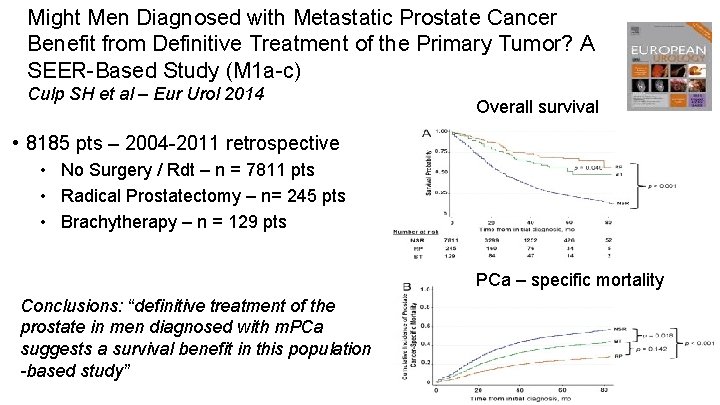
Might Men Diagnosed with Metastatic Prostate Cancer Benefit from Definitive Treatment of the Primary Tumor? A SEER-Based Study (M 1 a-c) Culp SH et al – Eur Urol 2014 Overall survival • 8185 pts – 2004 -2011 retrospective • No Surgery / Rdt – n = 7811 pts • Radical Prostatectomy – n= 245 pts • Brachytherapy – n = 129 pts PCa – specific mortality Conclusions: “definitive treatment of the prostate in men diagnosed with m. PCa suggests a survival benefit in this population -based study”
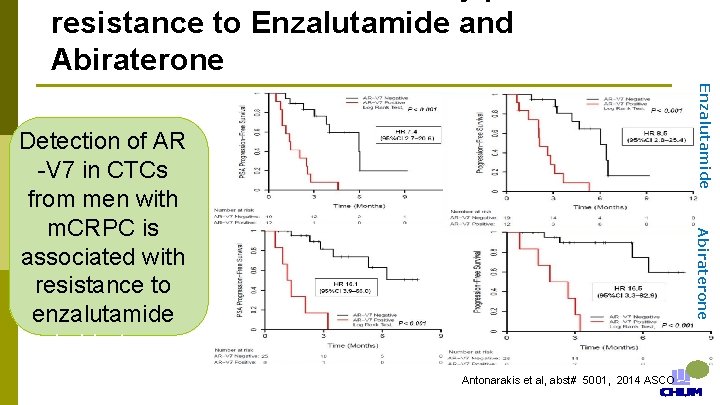
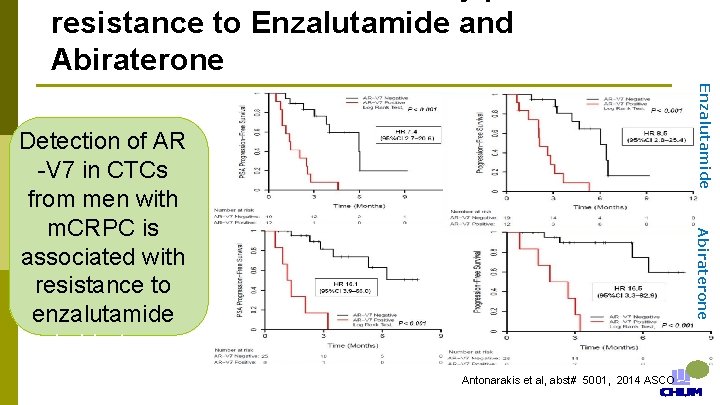
resistance to Enzalutamide and Abiraterone Enzalutamide Abiraterone Detection of AR -V 7 in CTCs from men with m. CRPC is associated with resistance to enzalutamide and abiraterone Antonarakis et al, abst# 5001, 2014 ASCO

AUA 2017 Ca. P: Tratamento futuro? Isótopo radioativo (actinium 225) ligado ao antígeno específico prostático de membrana PSMA Caso 1 Caso 2 RESULTADOS • respostas: completa do PSA e do tumor avaliado por PET • toxicidade hematológica insignificante, sem supressão medular, boca seca (xerostomia)
Thank you Obrigado!
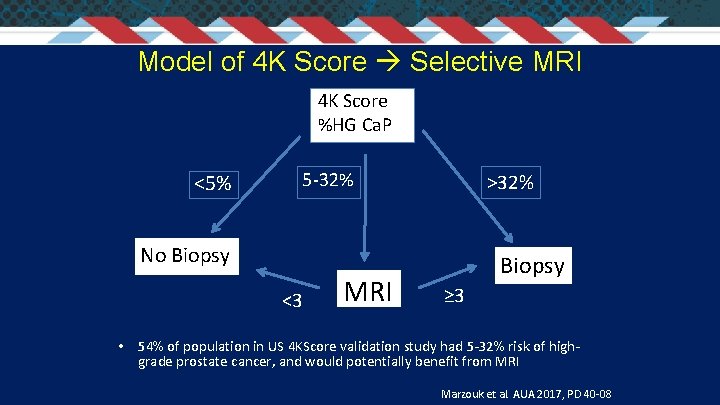
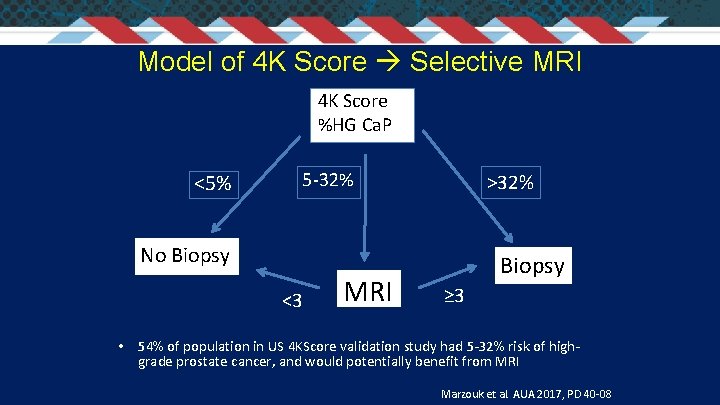
Model of 4 K Score Selective MRI 4 K Score %HG Ca. P <5% 5 -32% >32% No Biopsy <3 MRI Biopsy ≥ 3 • 54% of population in US 4 KScore validation study had 5 -32% risk of highgrade prostate cancer, and would potentially benefit from MRI Marzouk et al. AUA 2017, PD 40 -08
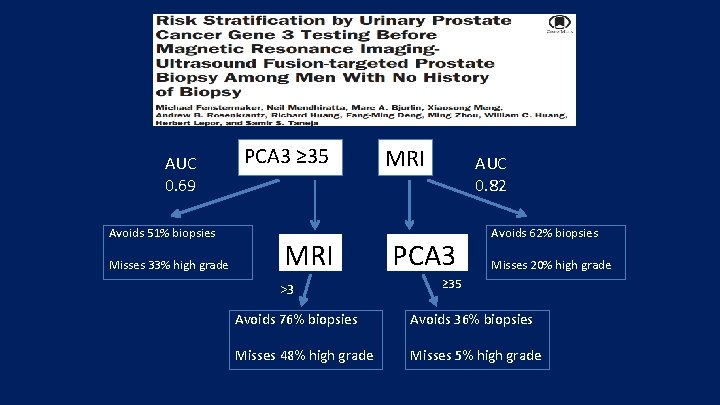
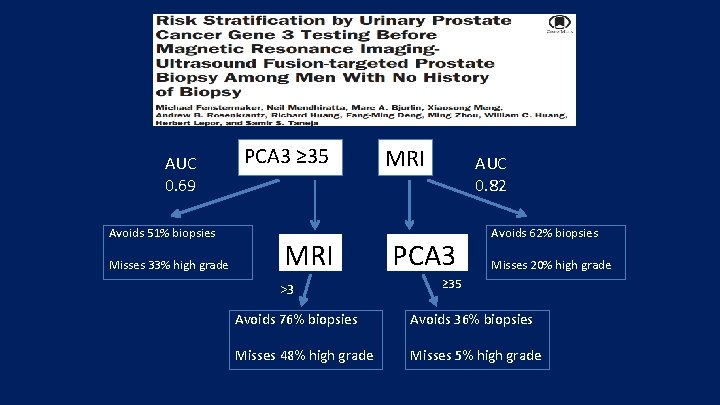
AUC 0. 69 Avoids 51% biopsies Misses 33% high grade PCA 3 ≥ 35 MRI >3 MRI AUC 0. 82 PCA 3 Avoids 62% biopsies Misses 20% high grade ≥ 35 Avoids 76% biopsies Avoids 36% biopsies Misses 48% high grade Misses 5% high grade
Breaking news, Best of, Guidelines • • PIVOT trial Best abstracts: prostate cancer genetics Late breaking abstracts Localized prostate cancer guidelines
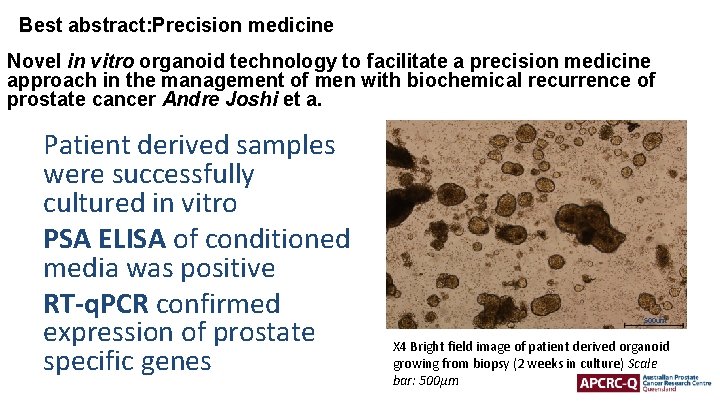
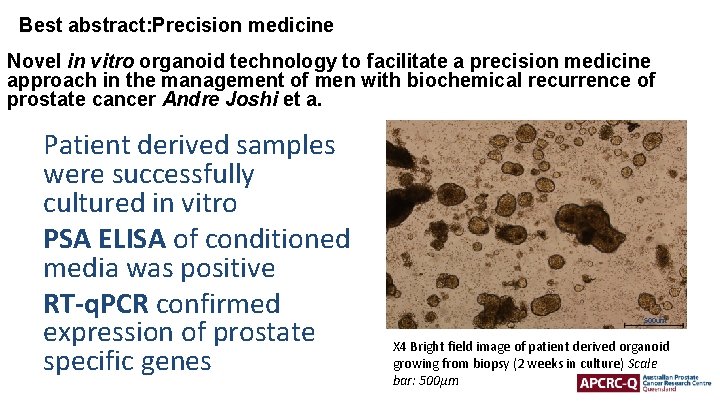
Best abstract: Precision medicine Novel in vitro organoid technology to facilitate a precision medicine approach in the management of men with biochemical recurrence of prostate cancer Andre Joshi et a. Patient derived samples were successfully cultured in vitro PSA ELISA of conditioned media was positive RT-q. PCR confirmed expression of prostate specific genes 500 um X 4 Bright field image of patient derived organoid growing from biopsy (2 weeks in culture) Scale bar: 500µm
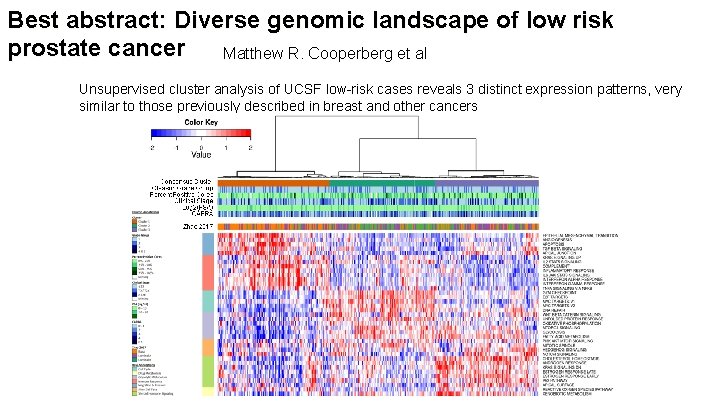
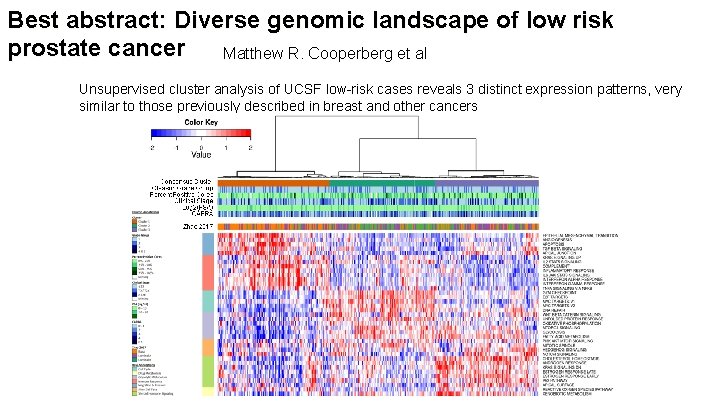
Best abstract: Diverse genomic landscape of low risk prostate cancer Matthew R. Cooperberg et al Unsupervised cluster analysis of UCSF low-risk cases reveals 3 distinct expression patterns, very similar to those previously described in breast and other cancers