High functioning clinical teams are extremely efficient How

- Slides: 36
High functioning clinical teams are extremely efficient: How to get one and achieve advanced access L. Gordon Moore MD Bertha Safford MD © 2004 Institute for Healthcare Improvement
Objectives t Explain what care teams are t Explain the attributes of a care team t Explain how care teams can reduce demand increase supply t Develop a care team © 2004 Institute for Healthcare Improvement
Definition t. A care team is the right mix of people coming together with the right tools to deliver the right care for a defined population of patients. © 2004 Institute for Healthcare Improvement
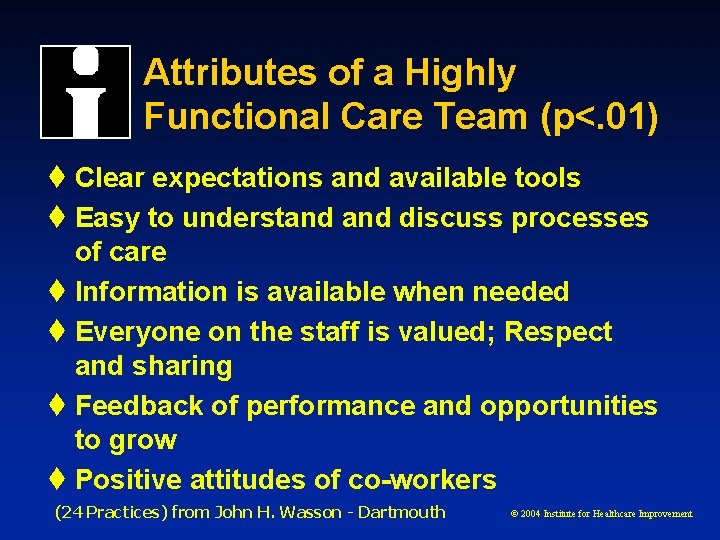
Attributes of a Highly Functional Care Team (p<. 01) t Clear expectations and available tools t Easy to understand discuss processes of care t Information is available when needed t Everyone on the staff is valued; Respect and sharing t Feedback of performance and opportunities to grow t Positive attitudes of co-workers (24 Practices) from John H. Wasson - Dartmouth © 2004 Institute for Healthcare Improvement
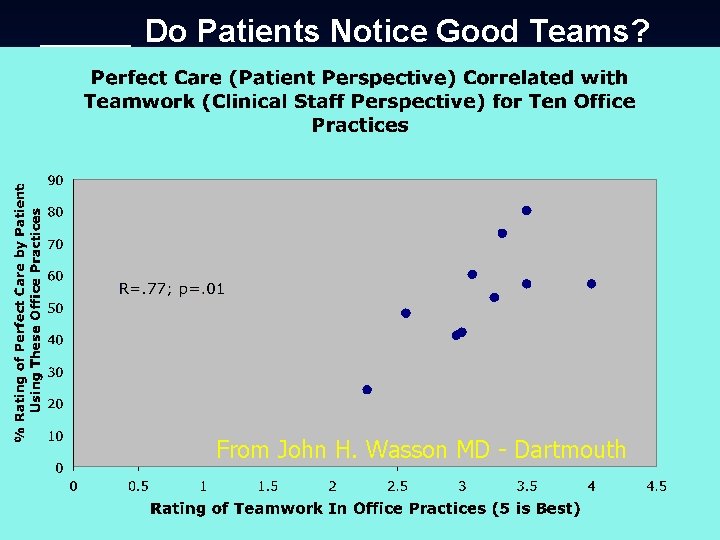
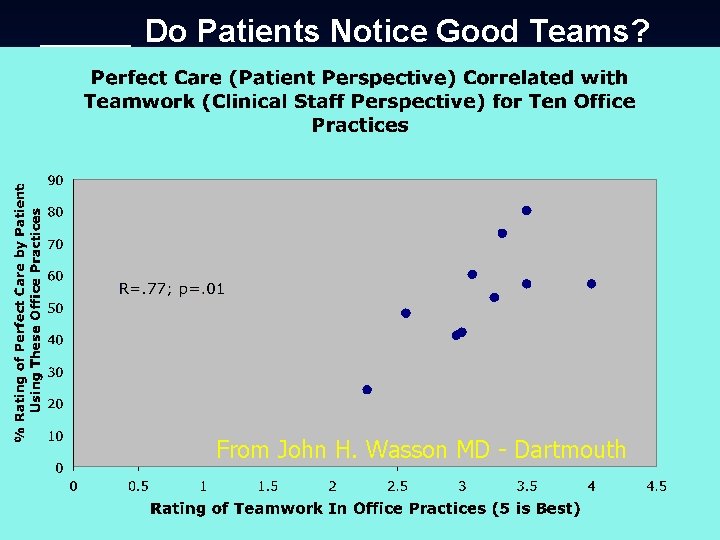
Do Patients Notice Good Teams? From John H. Wasson MD - Dartmouth © 2004 Institute for Healthcare Improvement
Does Patient Perception Matter? From John H. Wasson MD - Dartmouth © 2004 Institute for Healthcare Improvement
“Not perfect” in Patient Perception Looks Scary From John H. Wasson MD - Dartmouth © 2004 Institute for Healthcare Improvement
Why do this? t. Up to 40% of the work we do is rework: w Hand-offs w Repetitive patient calls & messages t. Staff salary & benefits makes up 70% of overhead © 2004 Institute for Healthcare Improvement
t. High functioning teams can accomplish more in less time w Better balance between work and life w Reduced overhead t. Advanced access is less work for us and serves our patients well © 2004 Institute for Healthcare Improvement
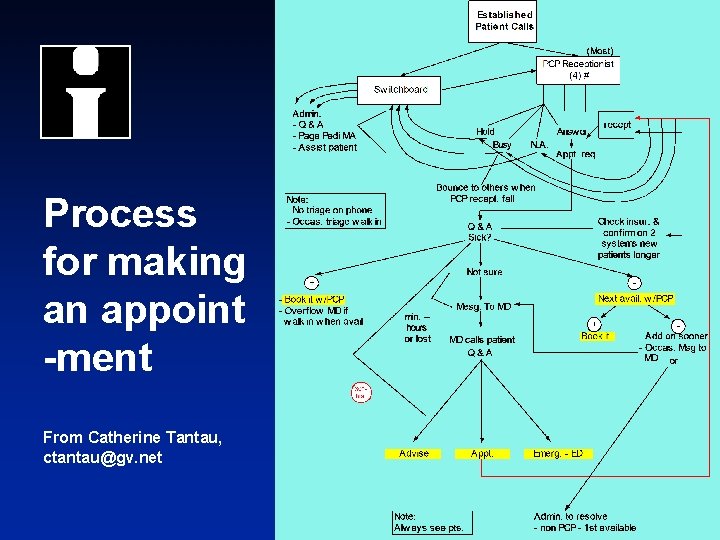
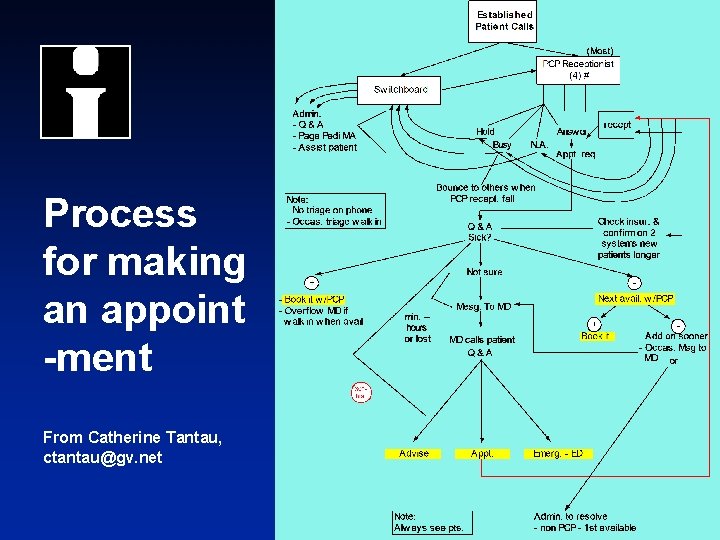
Process for making an appoint -ment From Catherine Tantau, ctantau@gv. net © 2004 Institute for Healthcare Improvement
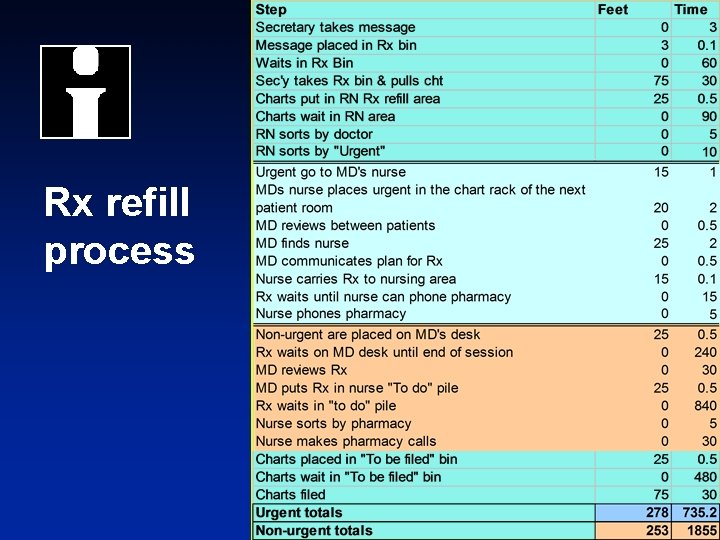
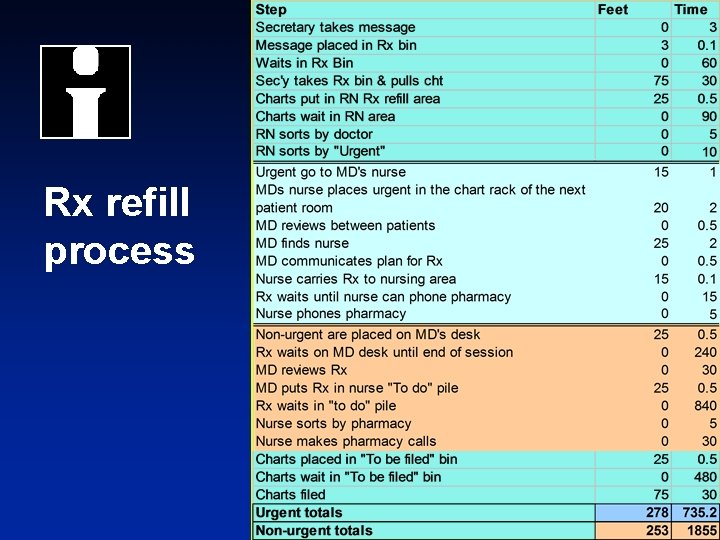
Rx refill process © 2004 Institute for Healthcare Improvement
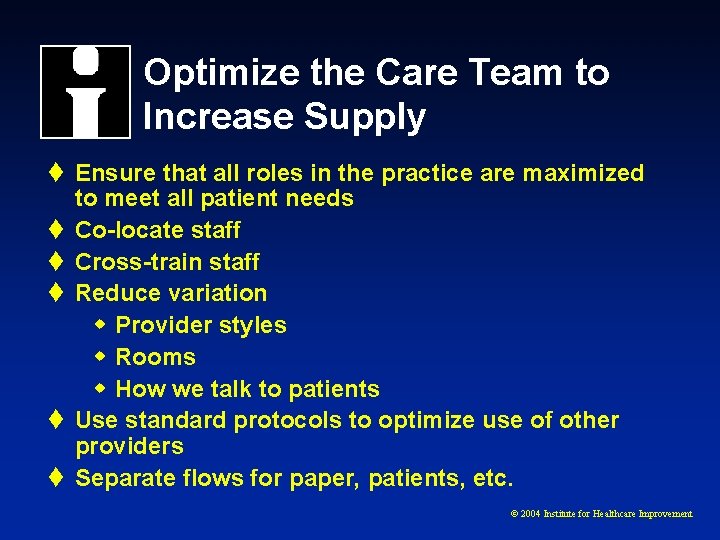
Optimize the Care Team to Increase Supply t Ensure that all roles in the practice are maximized to meet all patient needs t Co-locate staff t Cross-train staff t Reduce variation w Provider styles w Rooms w How we talk to patients t Use standard protocols to optimize use of other providers t Separate flows for paper, patients, etc. © 2004 Institute for Healthcare Improvement
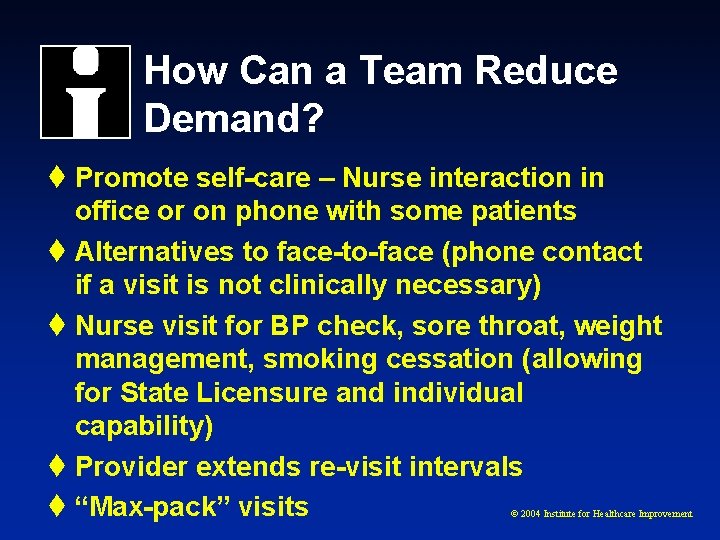
How Can a Team Reduce Demand? t Promote self-care – Nurse interaction in office or on phone with some patients t Alternatives to face-to-face (phone contact if a visit is not clinically necessary) t Nurse visit for BP check, sore throat, weight management, smoking cessation (allowing for State Licensure and individual capability) t Provider extends re-visit intervals t “Max-pack” visits © 2004 Institute for Healthcare Improvement
How do you Get There? t Ideally, start with resource planning t Then define the team necessary to meet the needs of your patients t All staff meet regularly t Get the data you need to inform you of your results w What is your team’s demand? w What is your team’s capacity? w Where is the constraint? © 2004 Institute for Healthcare Improvement

© 2004 Institute for Healthcare Improvement
Objectives § Apply the change concepts of Optimizing the Care Team from the Care Model § Use the “key changes” from the Care Model © 2004 Institute for Healthcare Improvement
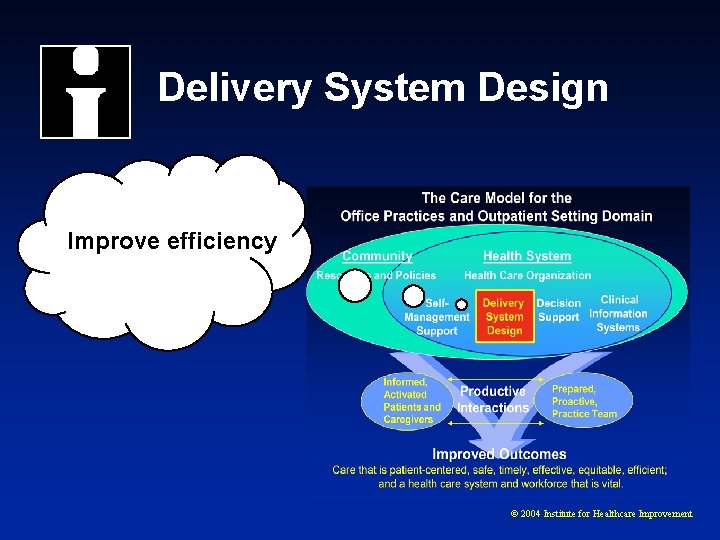
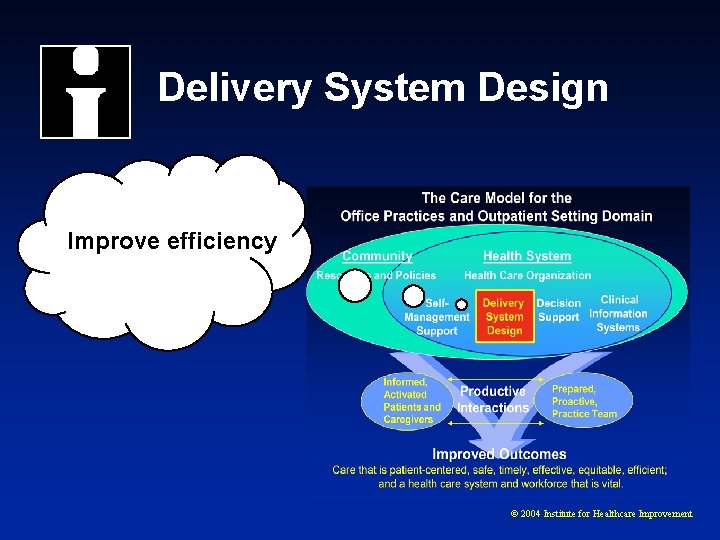
Delivery System Design Improve efficiency © 2004 Institute for Healthcare Improvement
Strategy: Improve Efficiency Change Concept § Optimize the Care Team and Staff © 2004 Institute for Healthcare Improvement
Change Concept: Optimizing Care Team and Staff Key Changes § Match the work to the individual’s licensure and capability § Cross train staff § Define and develop the team as unit © 2004 Institute for Healthcare Improvement
Content review: Traditional Roles in Clinical Office Practices § Roles held by tradition § Authority held by few § Function § Focus § Members of the team © 2004 Institute for Healthcare Improvement
Redesign Concepts for Care Teams § Co-location of people and resources § Cross-functioning and cross-training of staff § Self-organization & sharing of work § Weekly team meetings § “Visit planning” § Self-measurement for improvement § Care team huddles © 2004 Institute for Healthcare Improvement
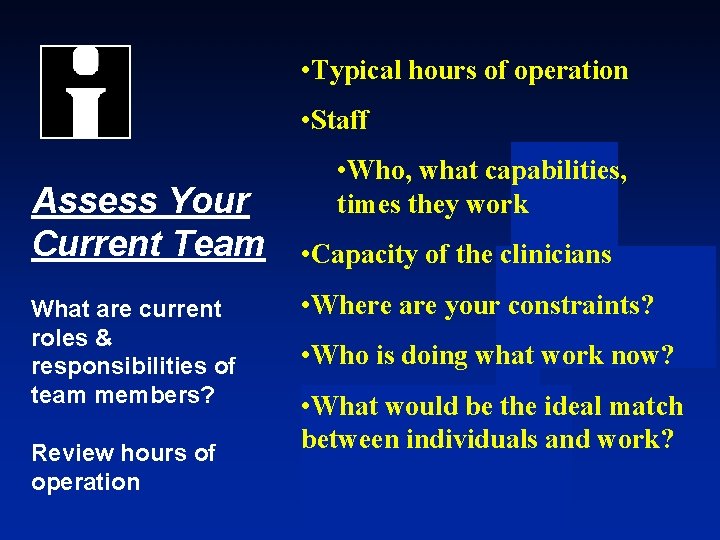
• Typical hours of operation • Staff Assess Your Current Team What are current roles & responsibilities of team members? Review hours of operation • Who, what capabilities, times they work • Capacity of the clinicians • Where are your constraints? • Who is doing what work now? • What would be the ideal match between individuals and work?
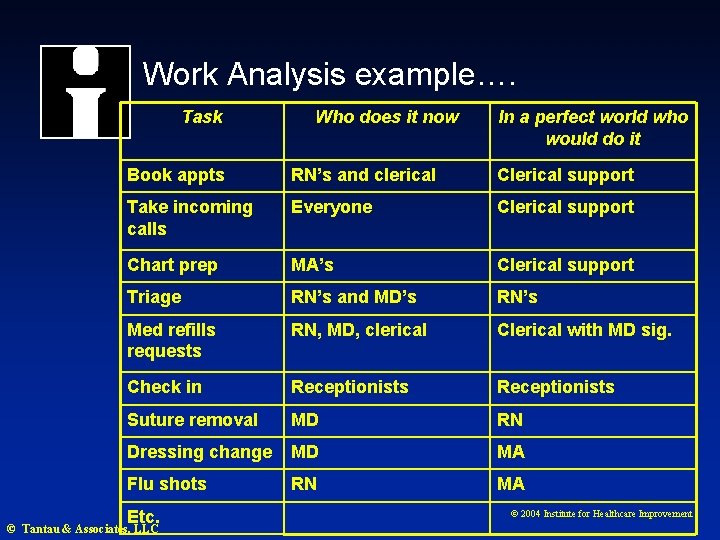
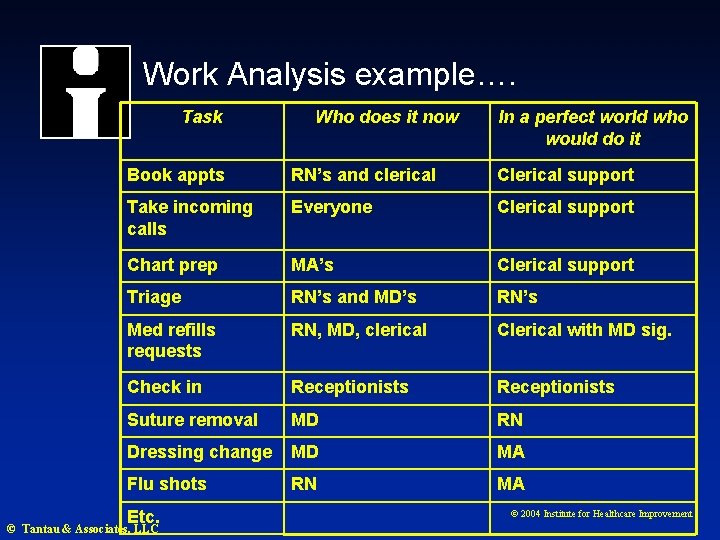
Work Analysis example…. Task Who does it now In a perfect world who would do it Book appts RN’s and clerical Clerical support Take incoming calls Everyone Clerical support Chart prep MA’s Clerical support Triage RN’s and MD’s RN’s Med refills requests RN, MD, clerical Clerical with MD sig. Check in Receptionists Suture removal MD RN Dressing change MD MA Flu shots RN MA Etc. © Tantau & Associates, LLC © 2004 Institute for Healthcare Improvement
Define the Activities: Visit and Non-Visit
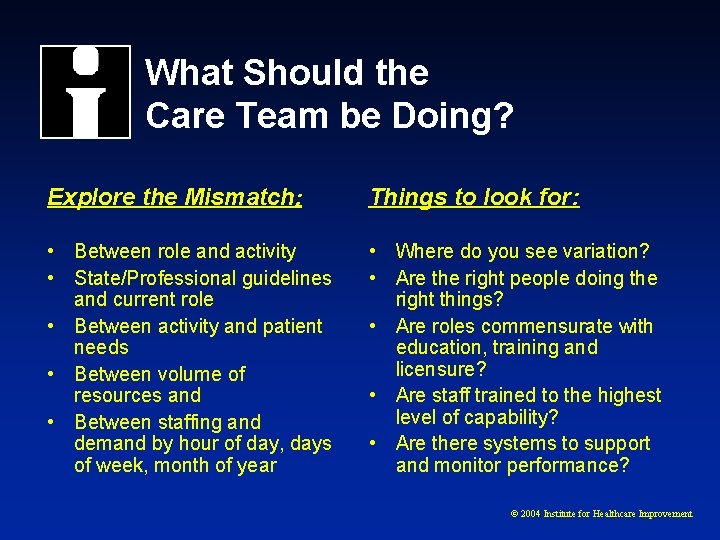
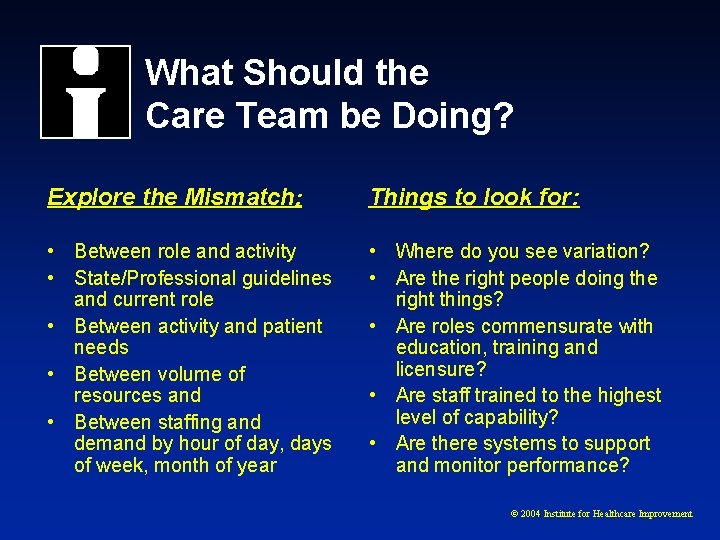
What Should the Care Team be Doing? Explore the Mismatch: Things to look for: • Between role and activity • State/Professional guidelines and current role • Between activity and patient needs • Between volume of resources and • Between staffing and demand by hour of day, days of week, month of year • Where do you see variation? • Are the right people doing the right things? • Are roles commensurate with education, training and licensure? • Are staff trained to the highest level of capability? • Are there systems to support and monitor performance? © 2004 Institute for Healthcare Improvement
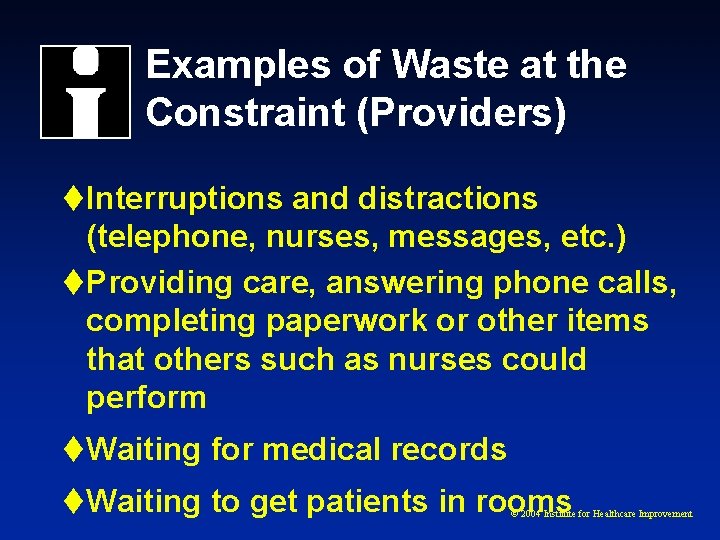
Examples of Waste at the Constraint (Providers) t Interruptions and distractions (telephone, nurses, messages, etc. ) t Providing care, answering phone calls, completing paperwork or other items that others such as nurses could perform t Waiting for medical records t Waiting to get patients in rooms © 2004 Institute for Healthcare Improvement
Examples of waste at constraint (Front office) t Multiple repeat patient phone calls due to w office policy of “we need five days notice for Rx refills” w Access delays • Provider schedule is not available • Sorting calls by “urgent” vs “routine” t Inaccurate PCP listed t Every patient signs waiver form at every visit © 2004 Institute for Healthcare Improvement
Building the “Right” Team “ A team is a small number of people with complimentary skills who are committed to a common purpose, set of performance goals, and an approach for which they hold themselves mutually accountable. ” Wisdom of Teams by Katzenbach © 2004 Institute for Healthcare Improvement
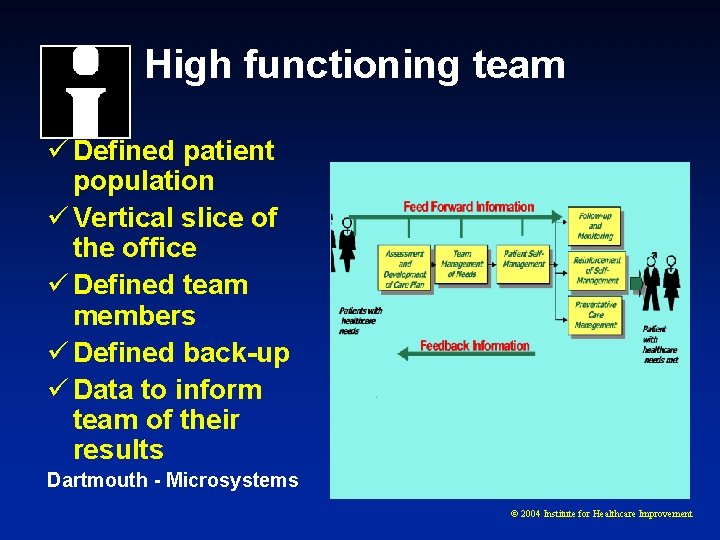
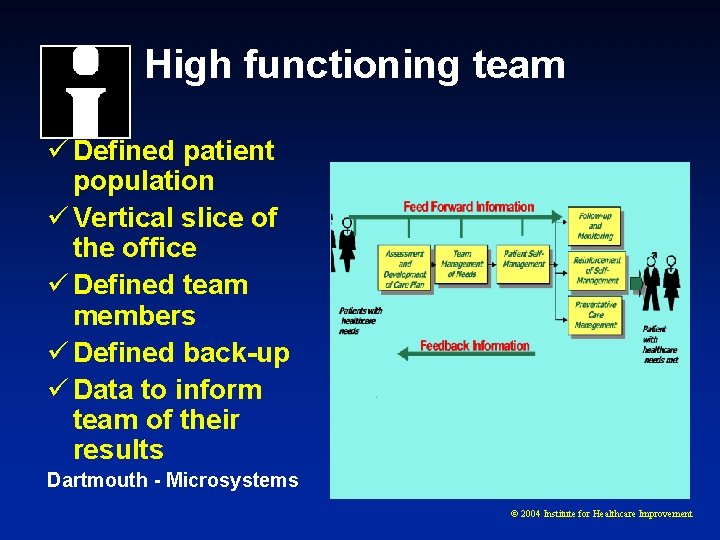
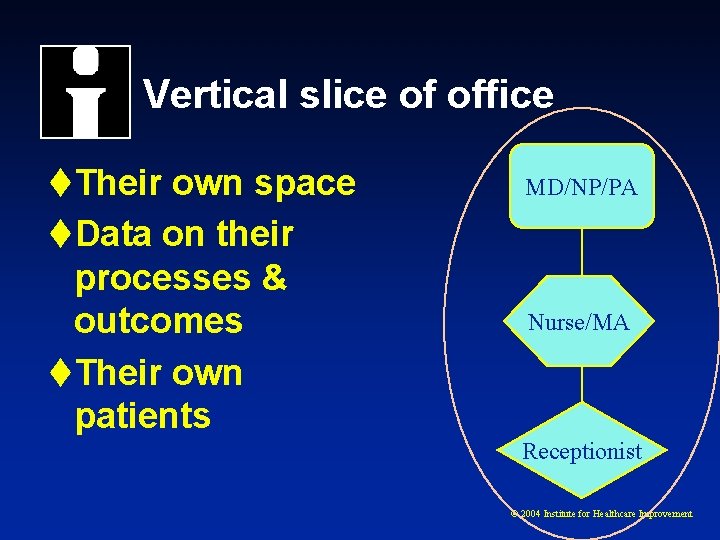
High functioning team ü Defined patient population ü Vertical slice of the office ü Defined team members ü Defined back-up ü Data to inform team of their results Dartmouth - Microsystems © 2004 Institute for Healthcare Improvement
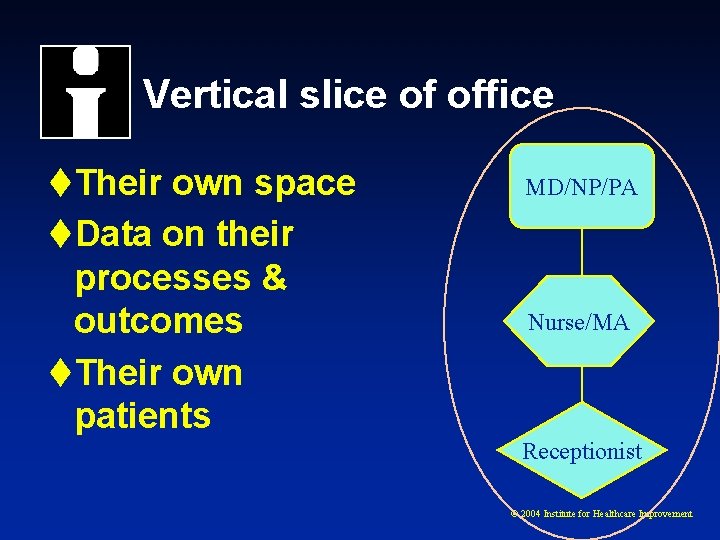
Vertical slice of office t. Their own space t. Data on their processes & outcomes t. Their own patients MD/NP/PA Nurse/MA Receptionist © 2004 Institute for Healthcare Improvement
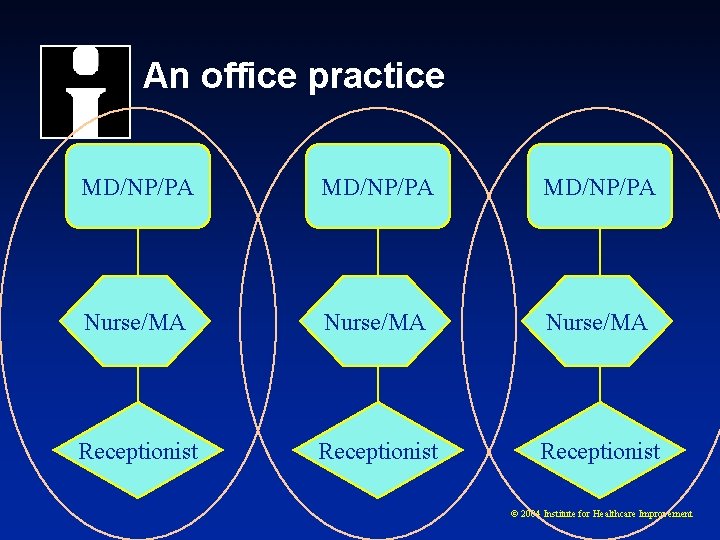
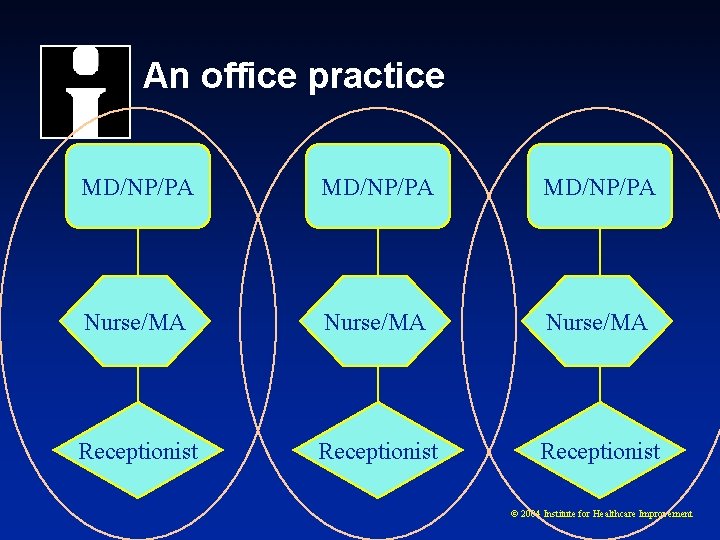
An office practice MD/NP/PA Nurse/MA Receptionist © 2004 Institute for Healthcare Improvement
Mutual Accountability § Know what’s expected § Capability § Feedback § Volunteer © 2004 Institute for Healthcare Improvement
Successful team behaviors t Daily: w Review day’s schedule • Is there anyone on the schedule who should not be/ • Anticipate equipment needs, visit length problems w Manage all patient demand within the team – e. g. see all visit demand that day t Weekly w Review future schedule for gaps in capacity • “I’m at a conference next Wednesday all day” w Review team data: access delays, cycle time, clinical process & outcomes w Define # of new patients (if any) team can accept © 2004 Institute for Healthcare Improvement
More team behaviors t Create and manage a contingency plan list w For the expected “unexpected” • 15 min visit for chest pain, rectal bleeding, three kids w Gaps between capacity and demand w Coordinating team activities across the practice • “We need to hold three appointments for Dr. Jones’s patients as she’s on the labor deck probably all day. ” © 2004 Institute for Healthcare Improvement
Successful practice behaviors t Correctly identify provider/team on patient charts and in “the system” t Separate work flow for various teams w Separate check in and check out window w Separate phone number w Teams wear color stickers • “We’re the Red team” t Triage becomes work flow backup for absent providers/teams © 2004 Institute for Healthcare Improvement
Resources § Clinical Microsystems Action Guide – www. clinicalmicrosystems. com § Advanced access: § www. ihi. org/IHI/Topics/Office. Practices/ Access § Senge P. M. 1994. The Fifth Discipline Fieldbook. Doubleday. § Presentation is on Gordon’s web site: www. idealhealthnetwork. com © 2004 Institute for Healthcare Improvement