High frequency oscillatory ventilation HFOV How does it
- Slides: 54
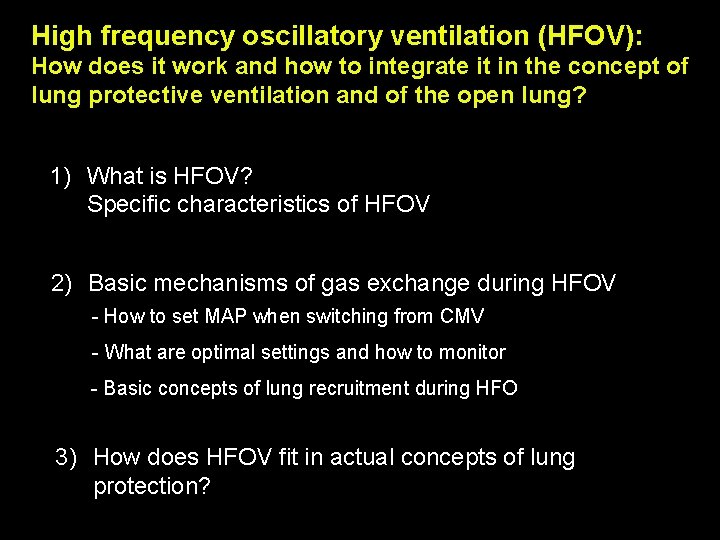
High frequency oscillatory ventilation (HFOV): How does it work and how to integrate it in the concept of lung protective ventilation and of the open lung? 1) What is HFOV? Specific characteristics of HFOV 2) Basic mechanisms of gas exchange during HFOV - How to set MAP when switching from CMV - What are optimal settings and how to monitor - Basic concepts of lung recruitment during HFO 3) How does HFOV fit in actual concepts of lung protection?
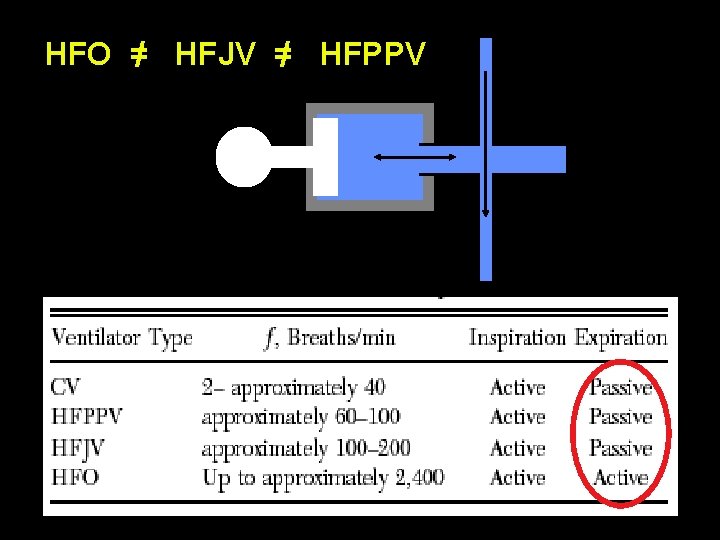
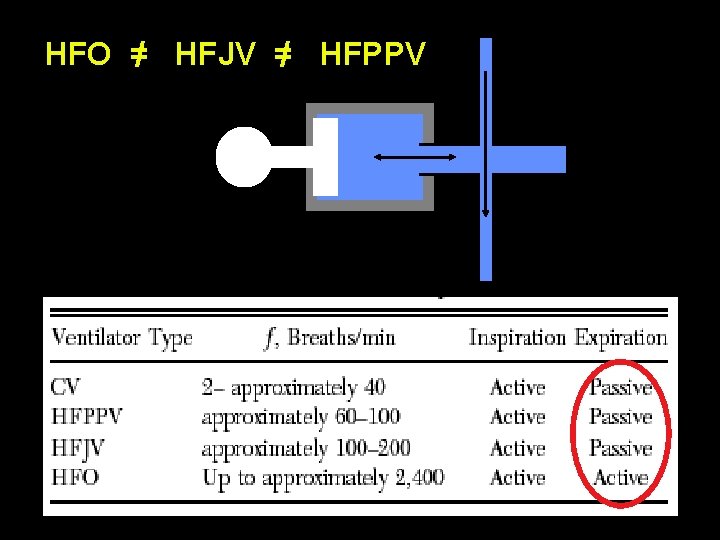
HFO =/ HFJV =/ HFPPV Humidifed Bias Flow Patient
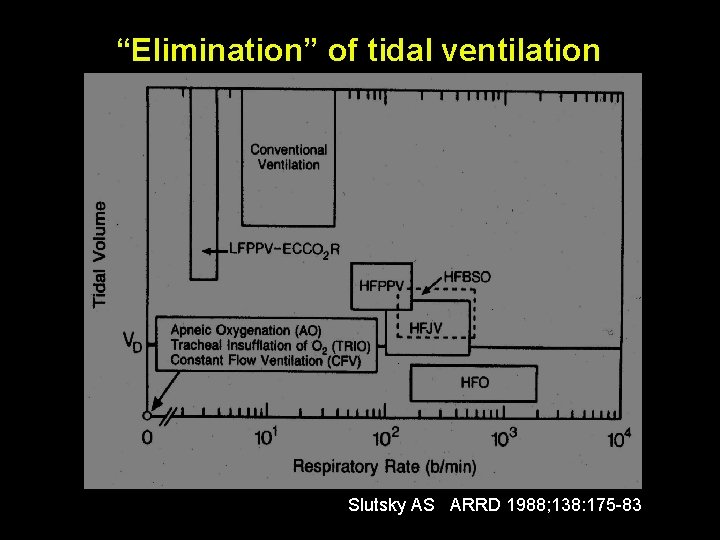
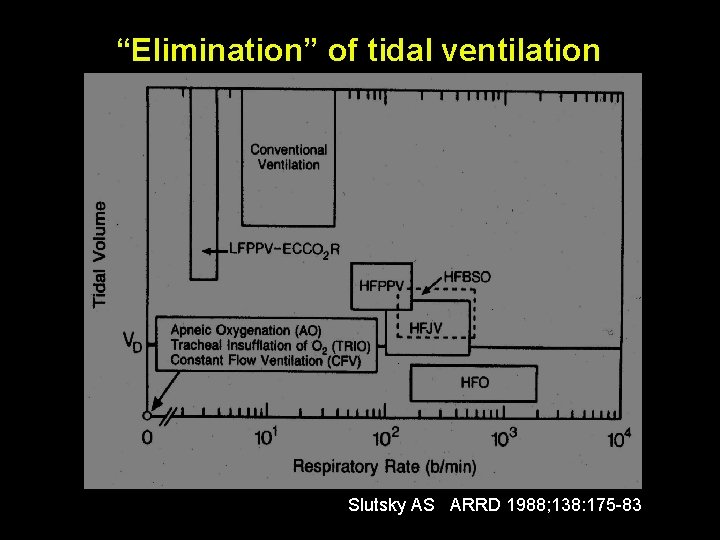
“Elimination” of tidal ventilation Slutsky AS ARRD 1988; 138: 175 -83
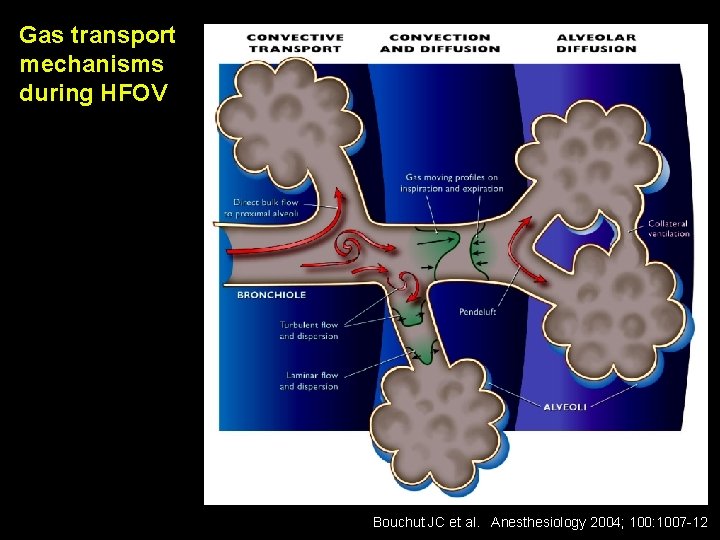
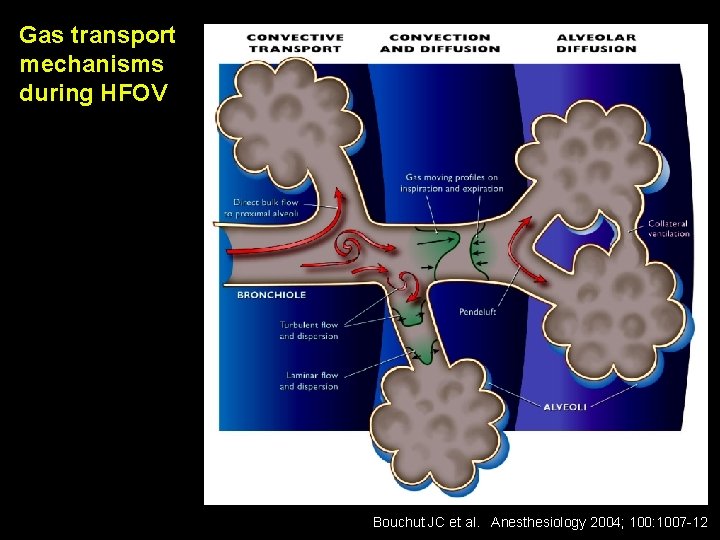
Gas transport mechanisms during HFOV Bouchut JC et al. Anesthesiology 2004; 100: 1007 -12
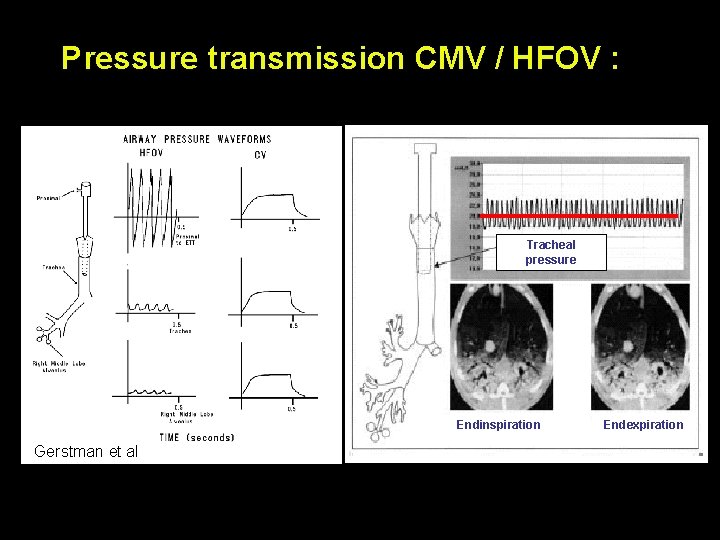
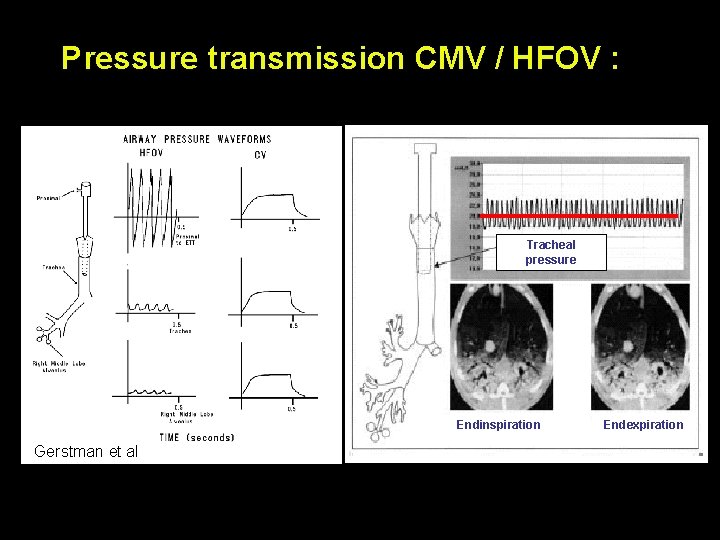
Pressure transmission CMV / HFOV : Tracheal pressure Endinspiration Gerstman et al Endexpiration
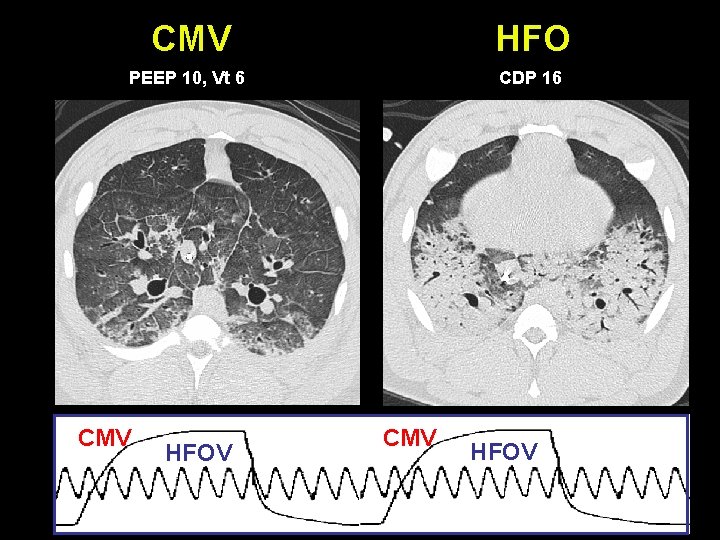
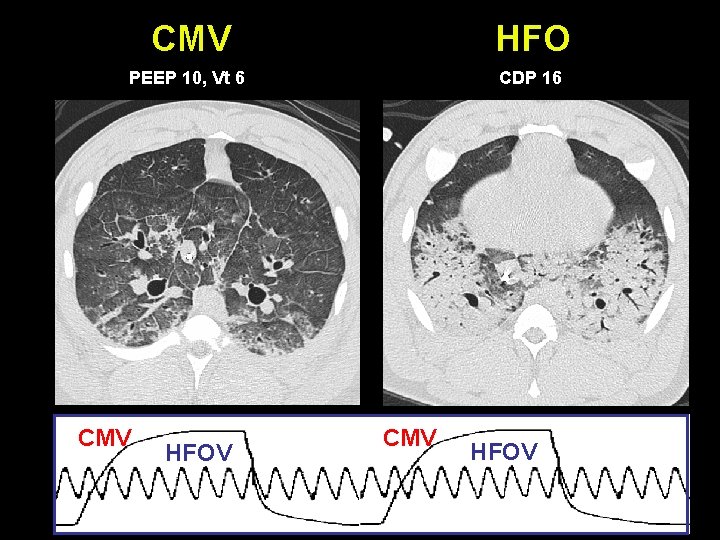
CMV HFO PEEP 10, Vt 6 CDP 16 CMV HFOV
HFO
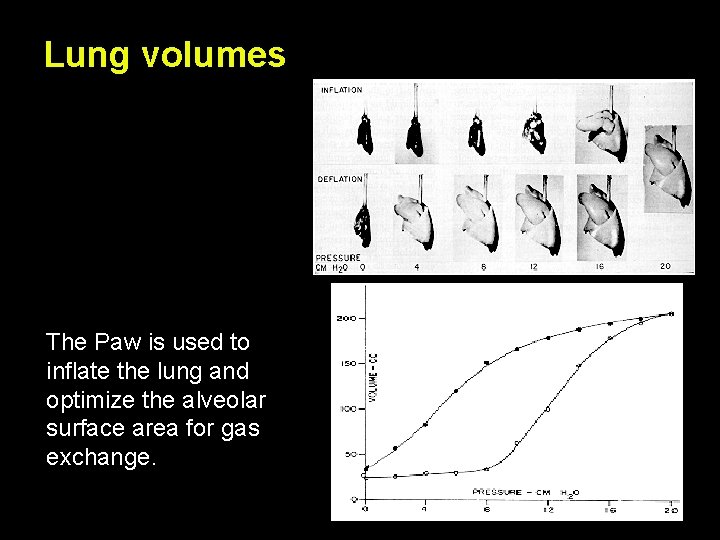
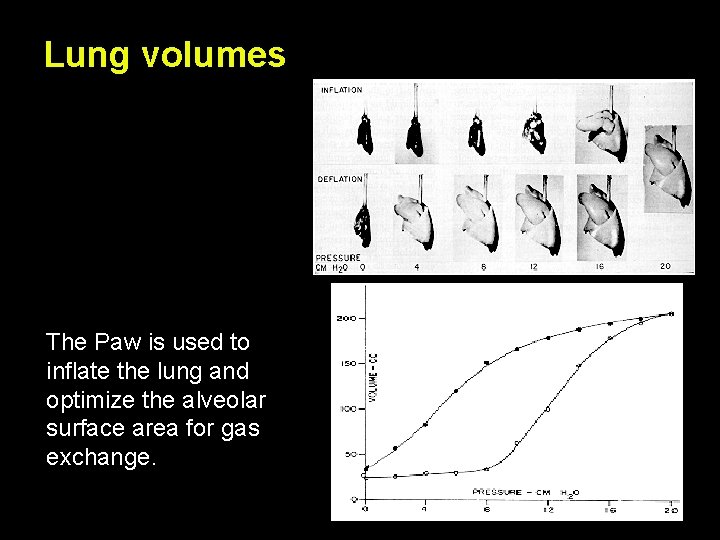
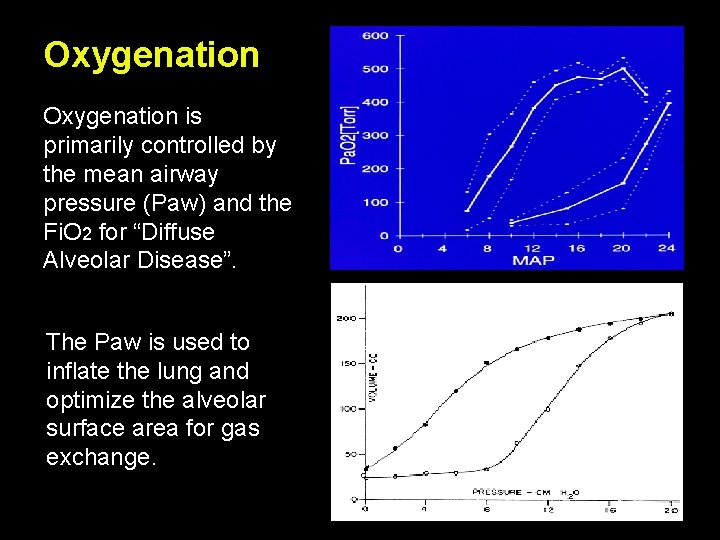
Lung volumes The Paw is used to inflate the lung and optimize the alveolar surface area for gas exchange. Paw = Lung Volume
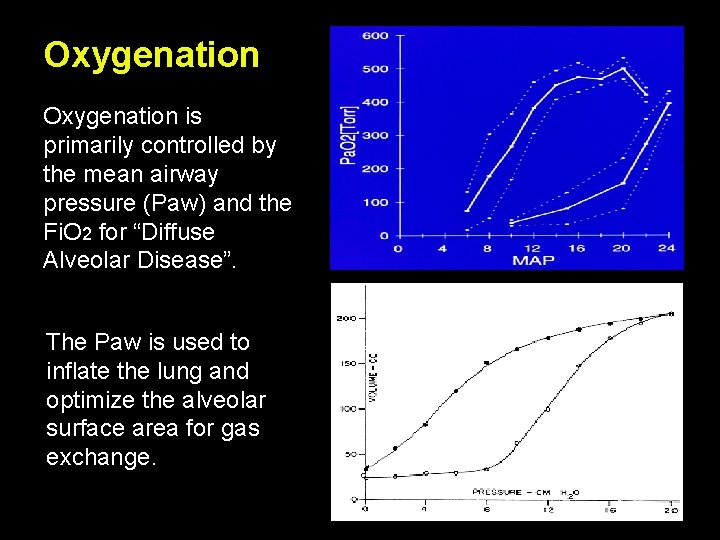
Oxygenation is primarily controlled by the mean airway pressure (Paw) and the Fi. O 2 for “Diffuse Alveolar Disease”. The Paw is used to inflate the lung and optimize the alveolar surface area for gas exchange. Paw = Lung Volume
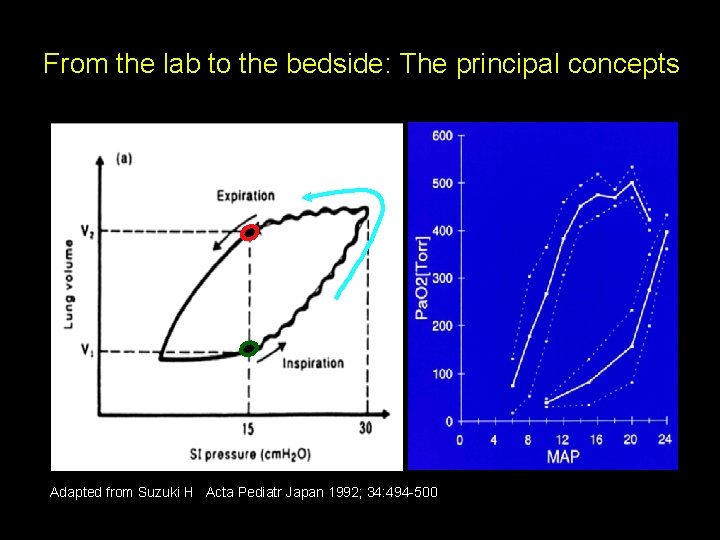
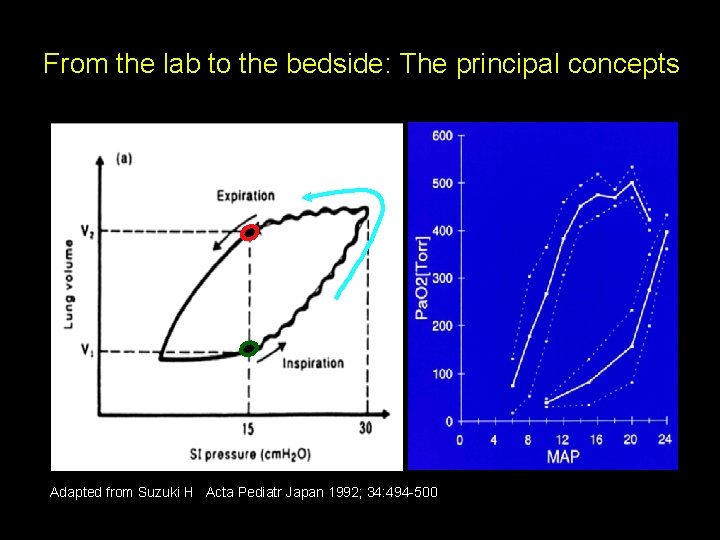
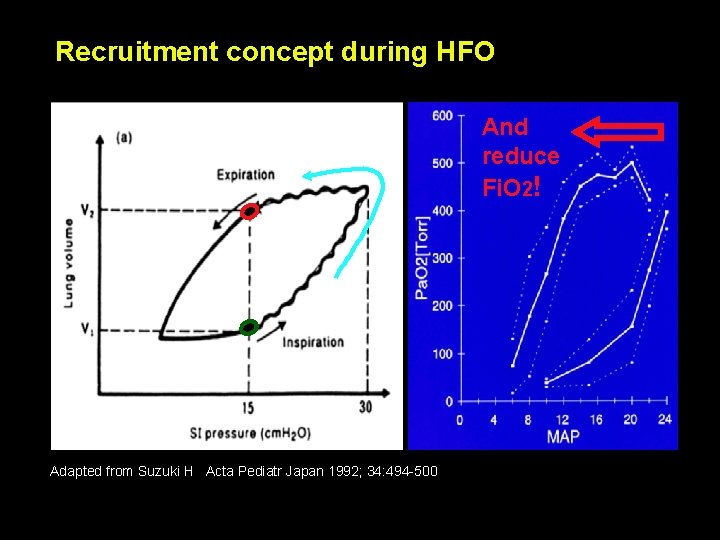
From the lab to the bedside: The principal concepts Adapted from Suzuki H Acta Pediatr Japan 1992; 34: 494 -500
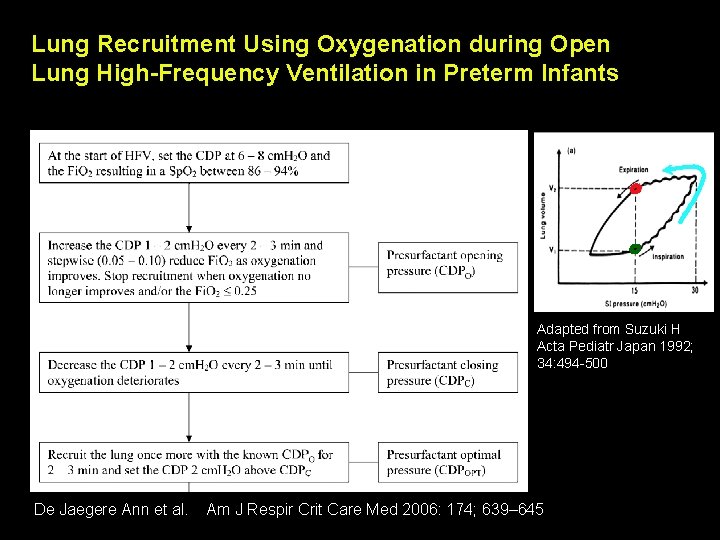
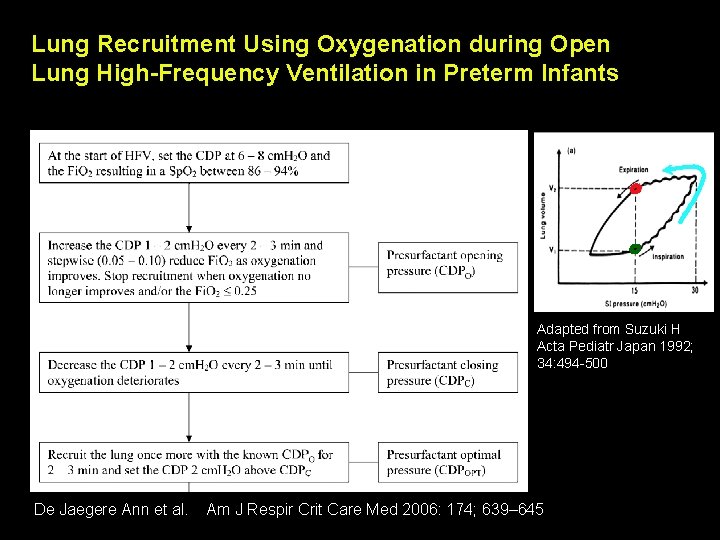
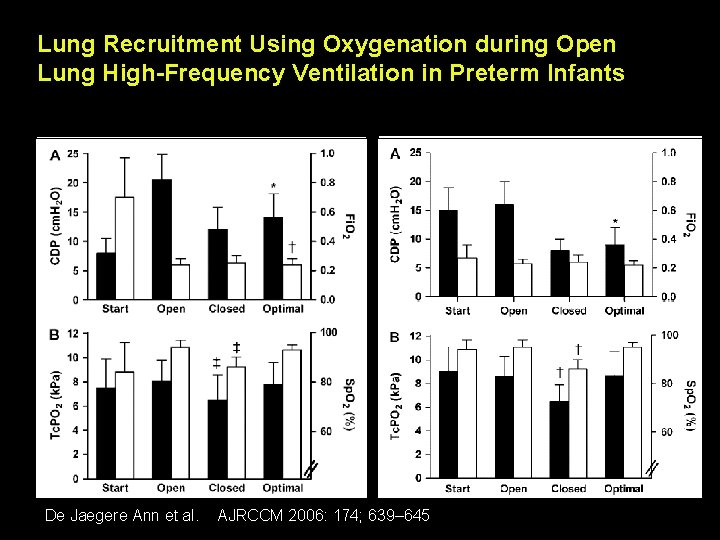
Lung Recruitment Using Oxygenation during Open Lung High-Frequency Ventilation in Preterm Infants Adapted from Suzuki H Acta Pediatr Japan 1992; 34: 494 -500 De Jaegere Ann et al. Am J Respir Crit Care Med 2006: 174; 639– 645
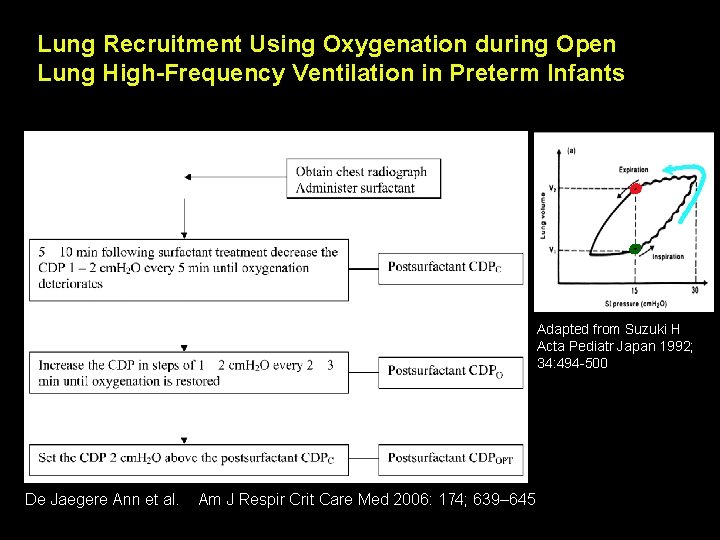
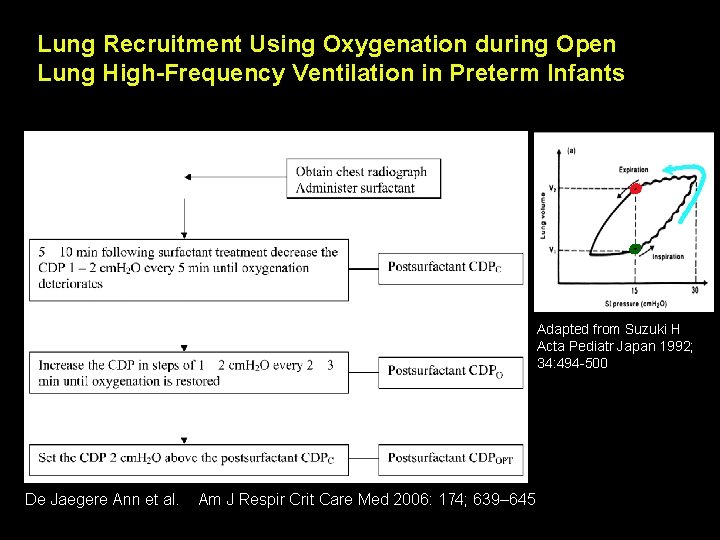
Lung Recruitment Using Oxygenation during Open Lung High-Frequency Ventilation in Preterm Infants Adapted from Suzuki H Acta Pediatr Japan 1992; 34: 494 -500 De Jaegere Ann et al. Am J Respir Crit Care Med 2006: 174; 639– 645
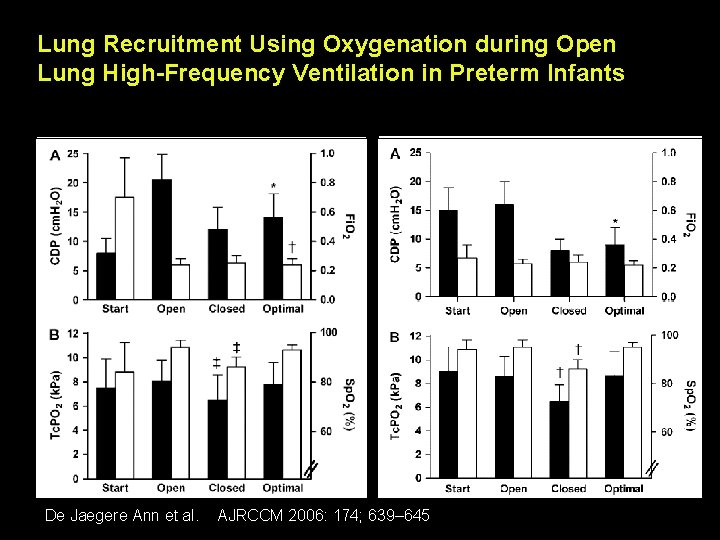
Lung Recruitment Using Oxygenation during Open Lung High-Frequency Ventilation in Preterm Infants before surfactant De Jaegere Ann et al. AJRCCM 2006: 174; 639– 645 after surfactant
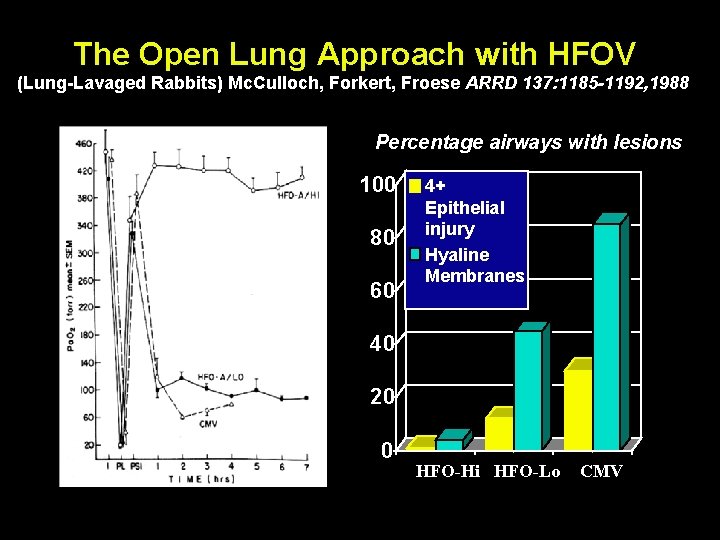
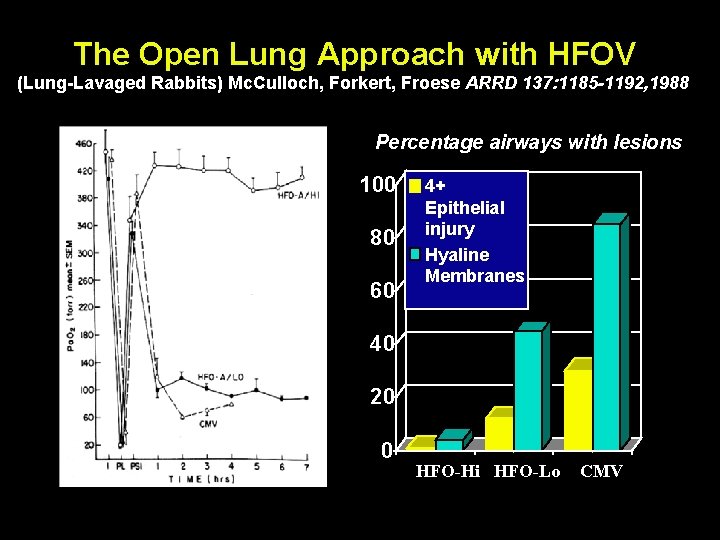
The Open Lung Approach with HFOV (Lung-Lavaged Rabbits) Mc. Culloch, Forkert, Froese ARRD 137: 1185 -1192, 1988 Percentage airways with lesions 100 80 60 4+ Epithelial injury Hyaline Membranes 40 20 0 HFO-Hi HFO-Lo CMV
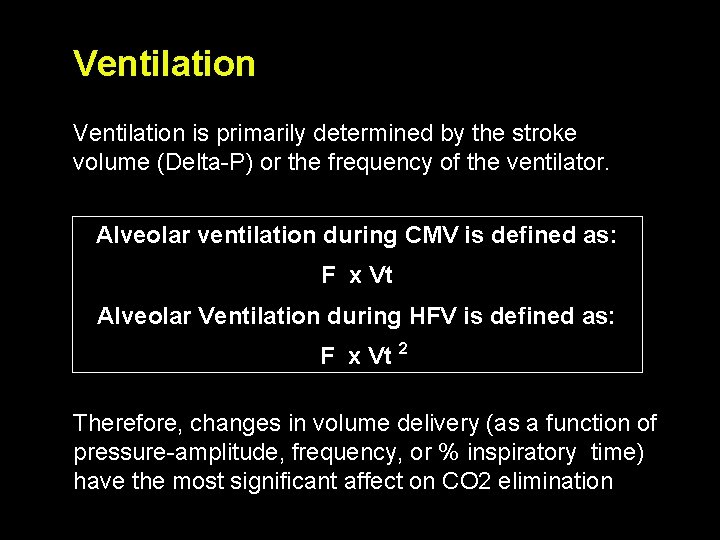
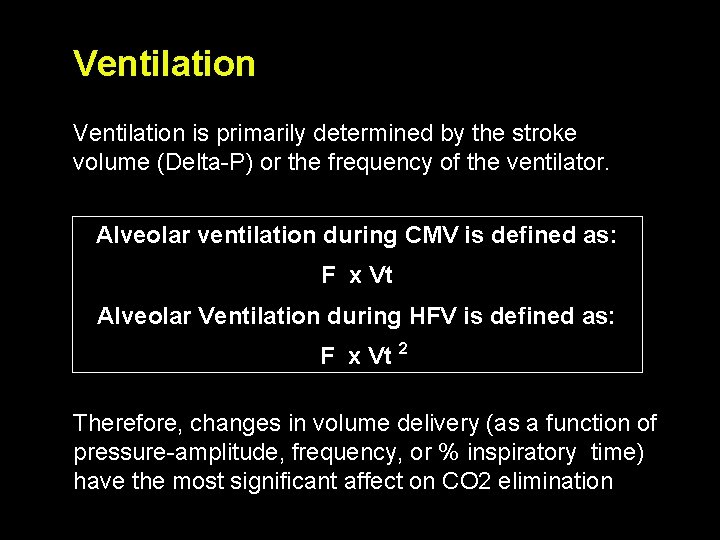
Ventilation is primarily determined by the stroke volume (Delta-P) or the frequency of the ventilator. Alveolar ventilation during CMV is defined as: F x Vt Alveolar Ventilation during HFV is defined as: F x Vt 2 Therefore, changes in volume delivery (as a function of pressure-amplitude, frequency, or % inspiratory time) have the most significant affect on CO 2 elimination
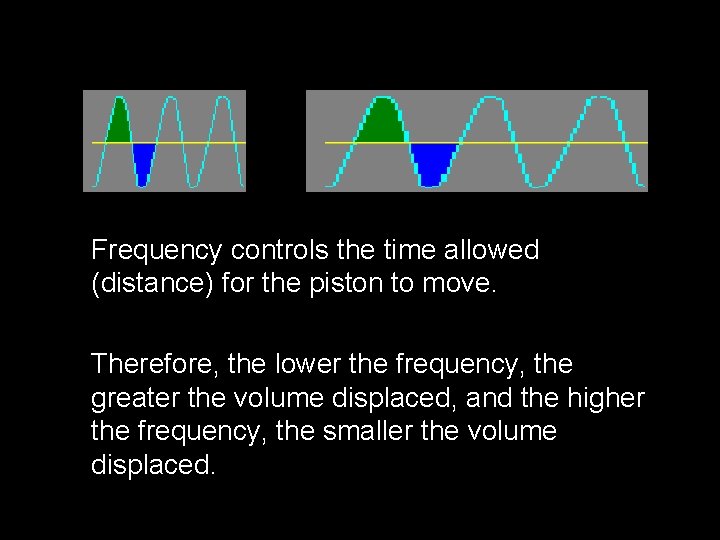
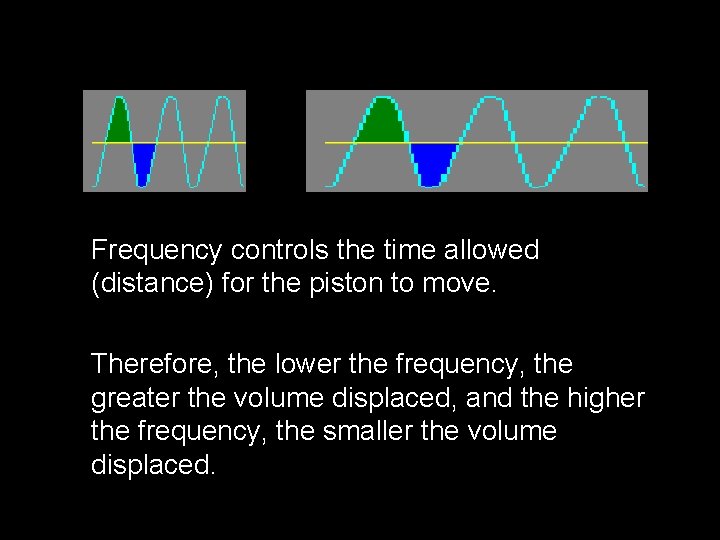
Frequency controls the time allowed (distance) for the piston to move. Therefore, the lower the frequency, the greater the volume displaced, and the higher the frequency, the smaller the volume displaced.
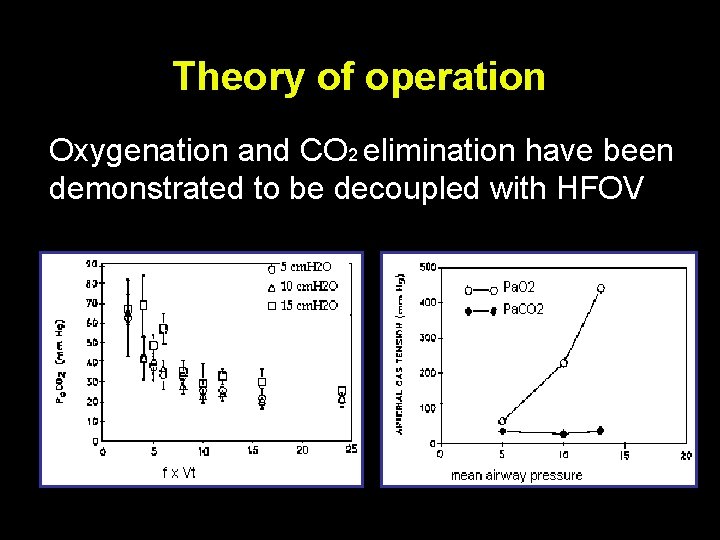
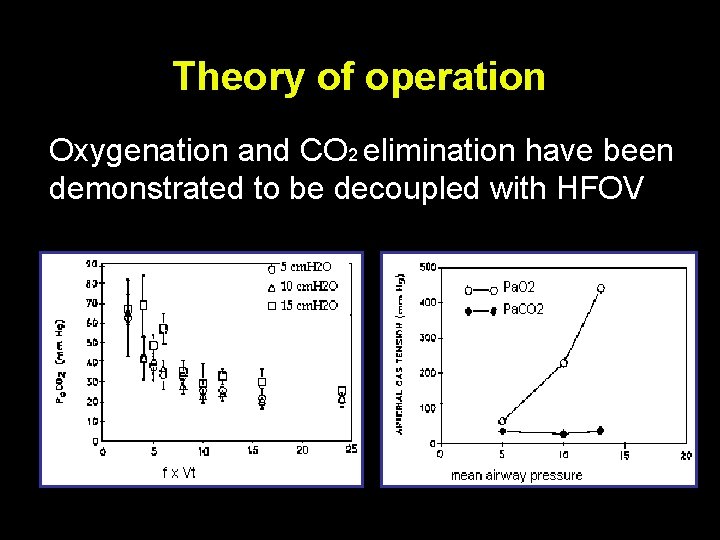
Theory of operation Oxygenation and CO 2 elimination have been demonstrated to be decoupled with HFOV
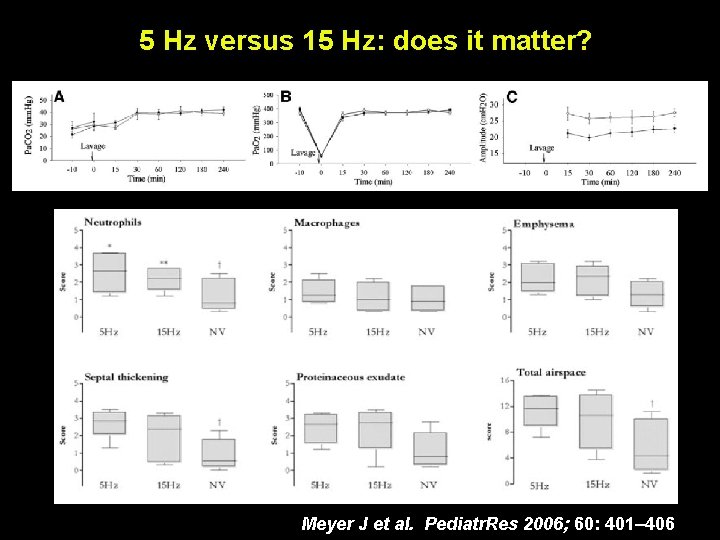
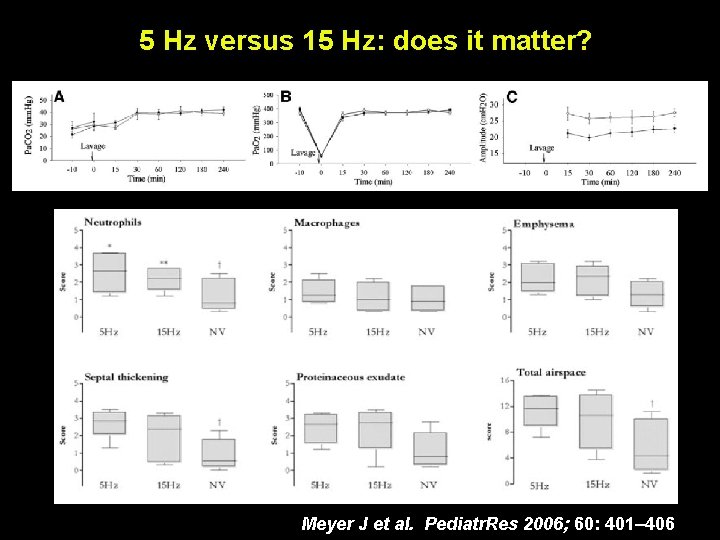
5 Hz versus 15 Hz: does it matter? Meyer J et al. Pediatr. Res 2006; 60: 401– 406
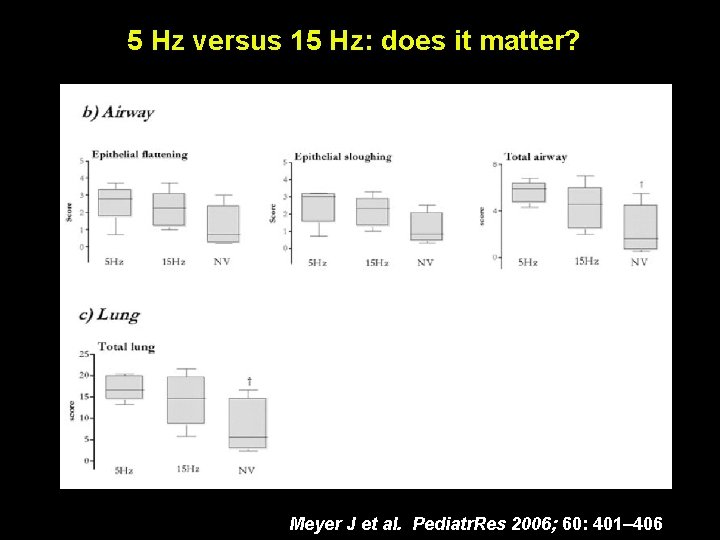
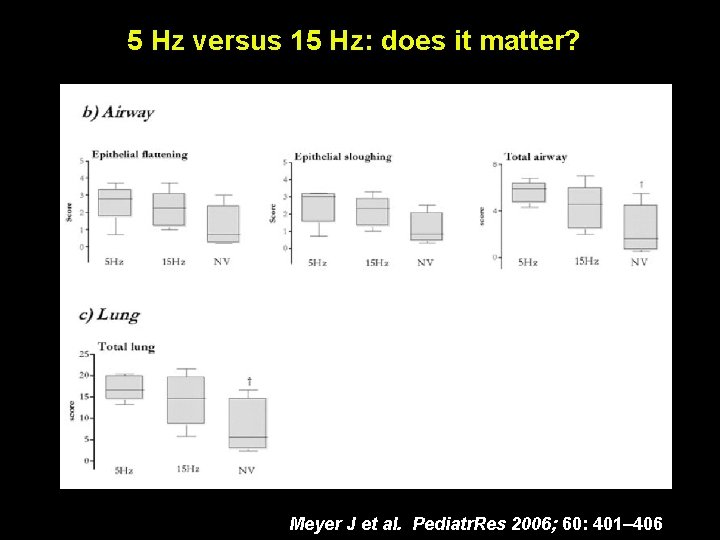
5 Hz versus 15 Hz: does it matter? Meyer J et al. Pediatr. Res 2006; 60: 401– 406
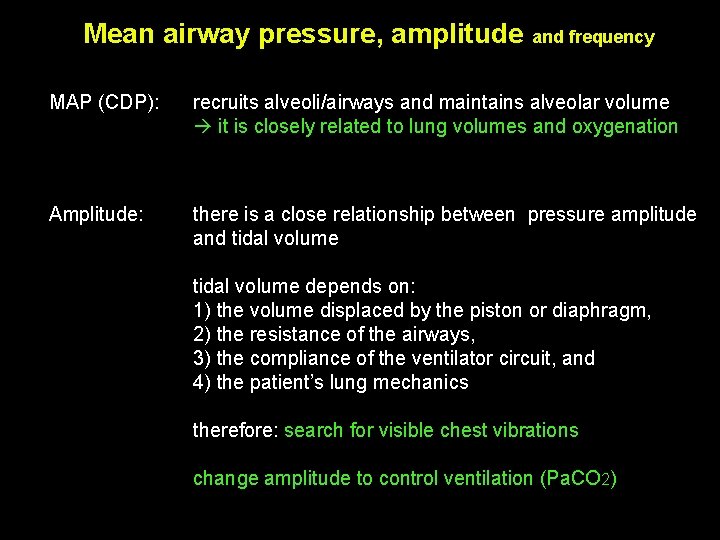
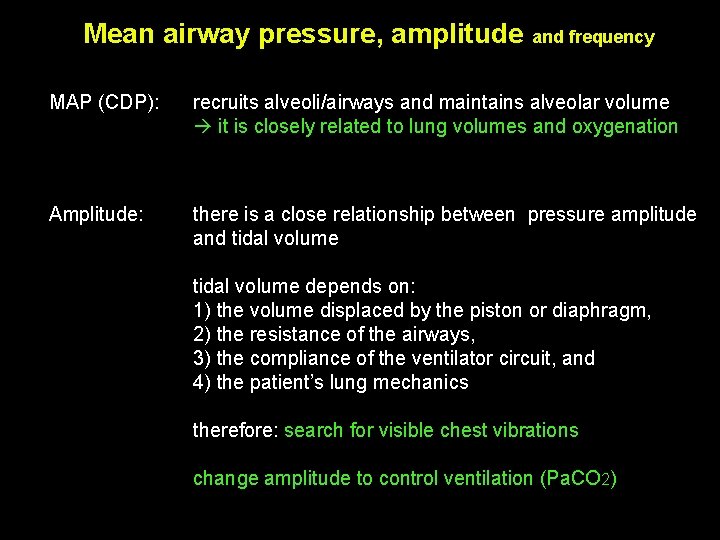
Mean airway pressure, amplitude and frequency MAP (CDP): recruits alveoli/airways and maintains alveolar volume it is closely related to lung volumes and oxygenation Amplitude: there is a close relationship between pressure amplitude and tidal volume depends on: 1) the volume displaced by the piston or diaphragm, 2) the resistance of the airways, 3) the compliance of the ventilator circuit, and 4) the patient’s lung mechanics therefore: search for visible chest vibrations change amplitude to control ventilation (Pa. CO 2)
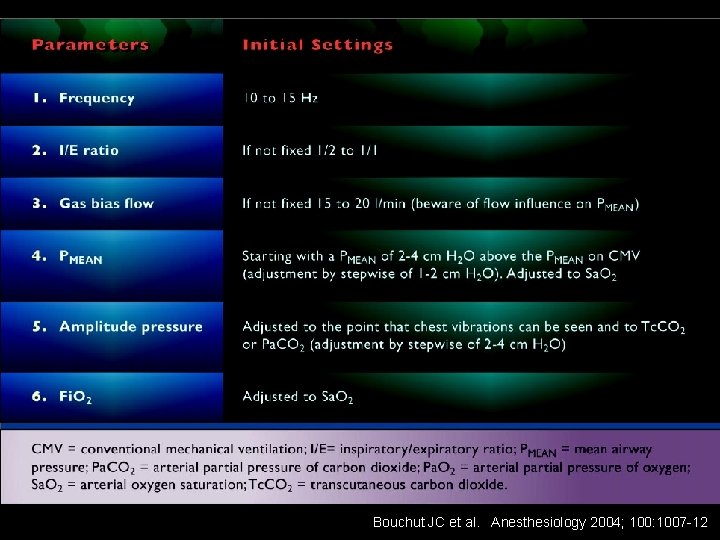
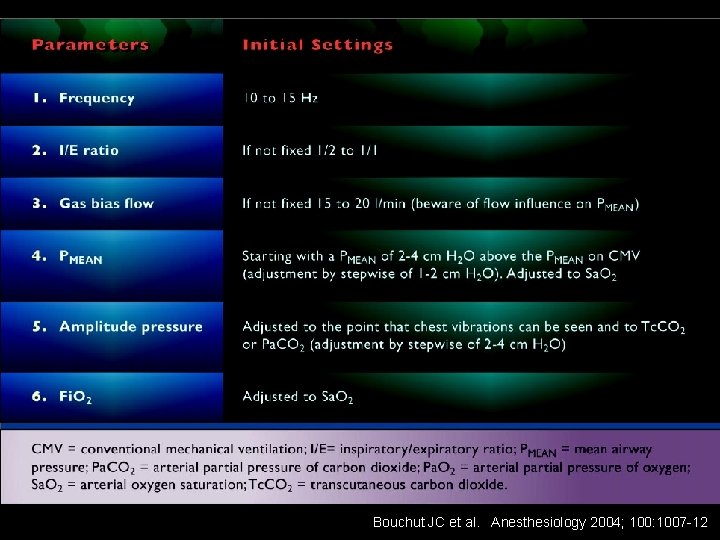
Bouchut JC et al. Anesthesiology 2004; 100: 1007 -12
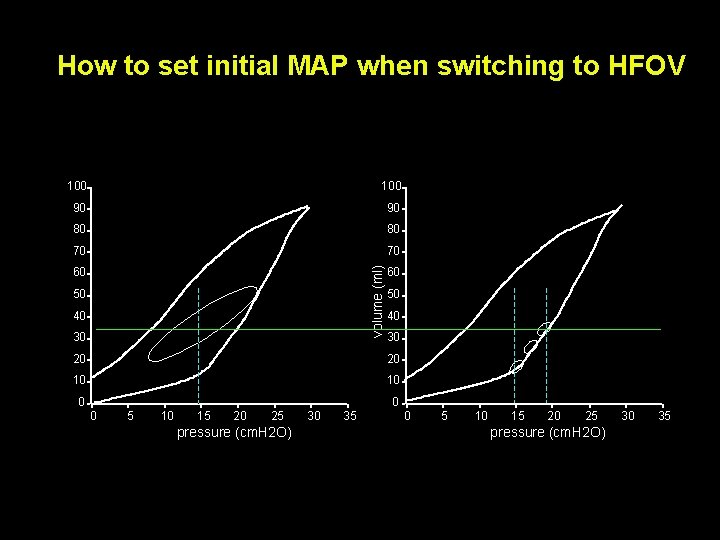
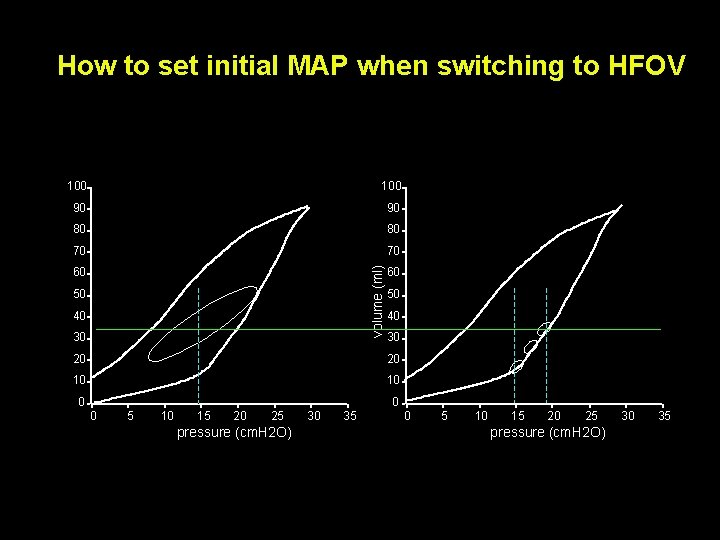
How to set initial MAP when switching to HFOV 100 90 90 80 80 70 70 volume (ml) 100 60 50 40 30 20 20 10 10 0 5 10 15 20 25 pressure (cm. H 2 O) 30 35
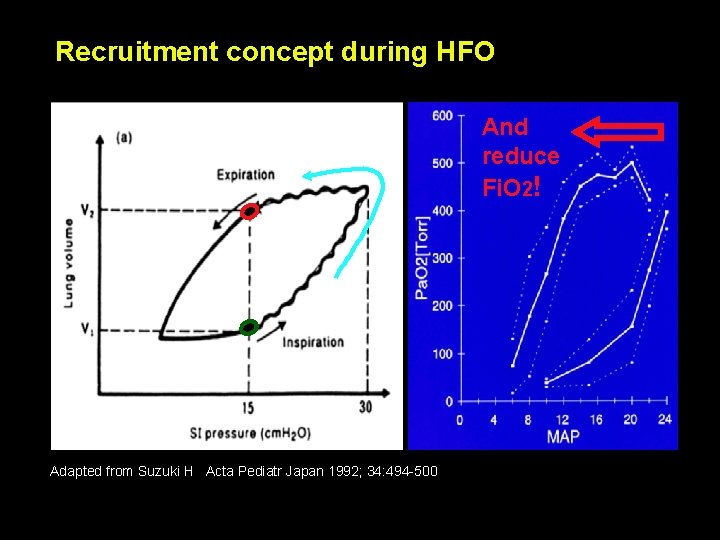
Recruitment concept during HFO And reduce Fi. O 2! Adapted from Suzuki H Acta Pediatr Japan 1992; 34: 494 -500
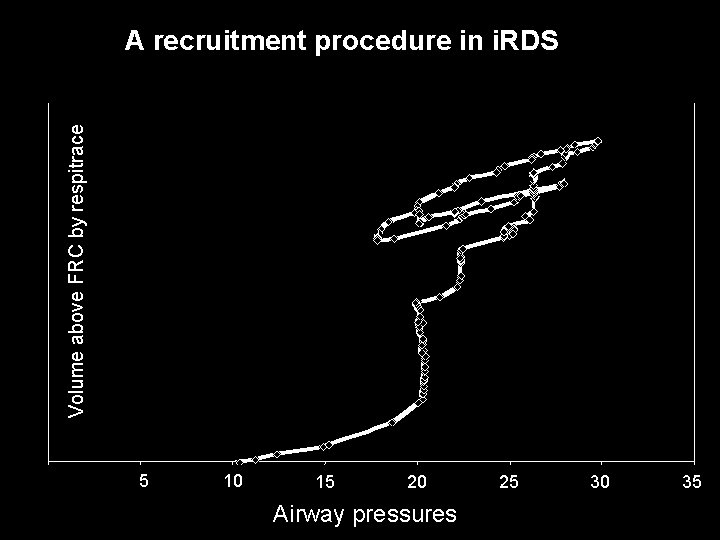
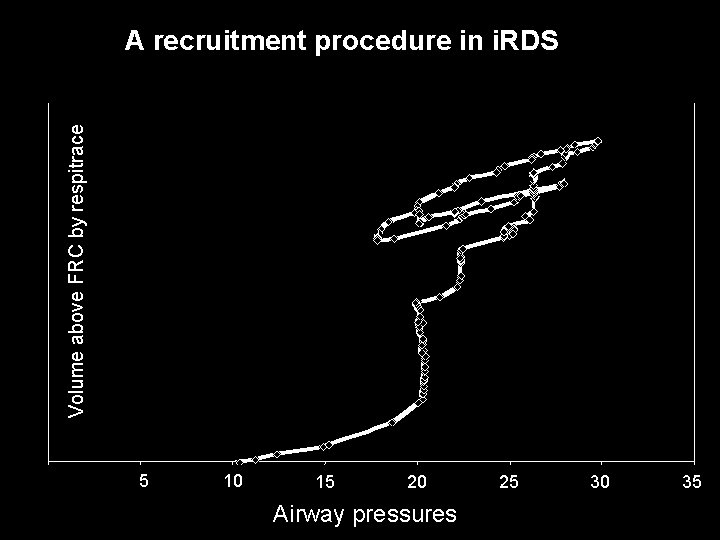
Volume above FRC by respitrace A recruitment procedure in i. RDS Drop in SO 2 5 10 10 15 20 Airway pressures 25 30 35
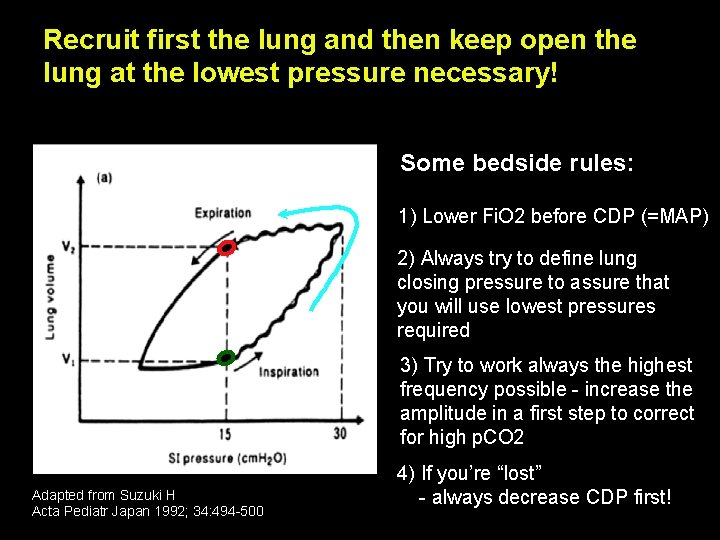
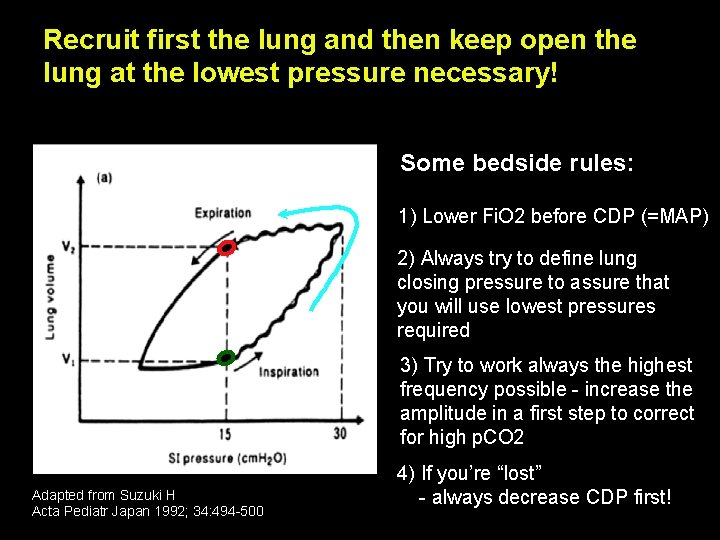
Recruit first the lung and then keep open the lung at the lowest pressure necessary! Some bedside rules: 1) Lower Fi. O 2 before CDP (=MAP) 2) Always try to define lung closing pressure to assure that you will use lowest pressures required 3) Try to work always the highest frequency possible - increase the amplitude in a first step to correct for high p. CO 2 Adapted from Suzuki H Acta Pediatr Japan 1992; 34: 494 -500 4) If you’re “lost” - always decrease CDP first!
The clinical experience: HFO vs CMV
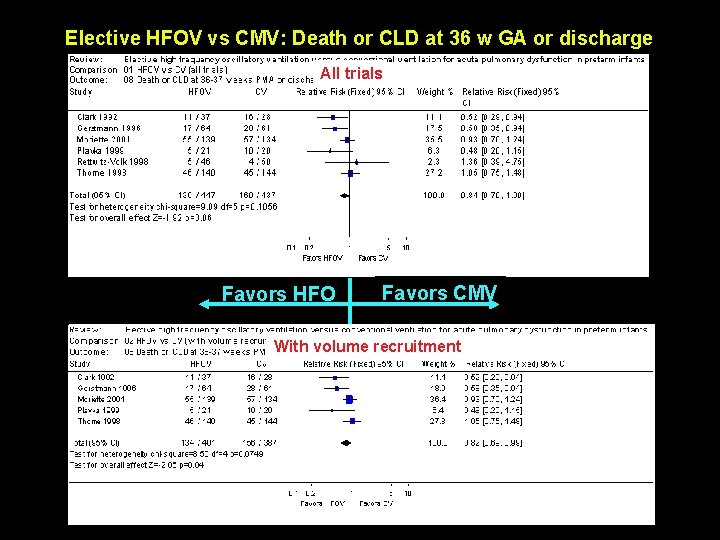
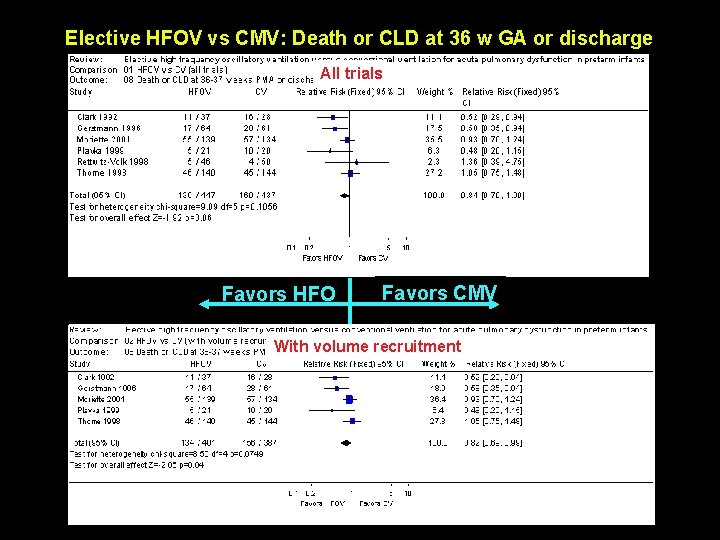
Elective HFOV vs CMV: Death or CLD at 36 w GA or discharge All trials Favors HFO Favors CMV With volume recruitment
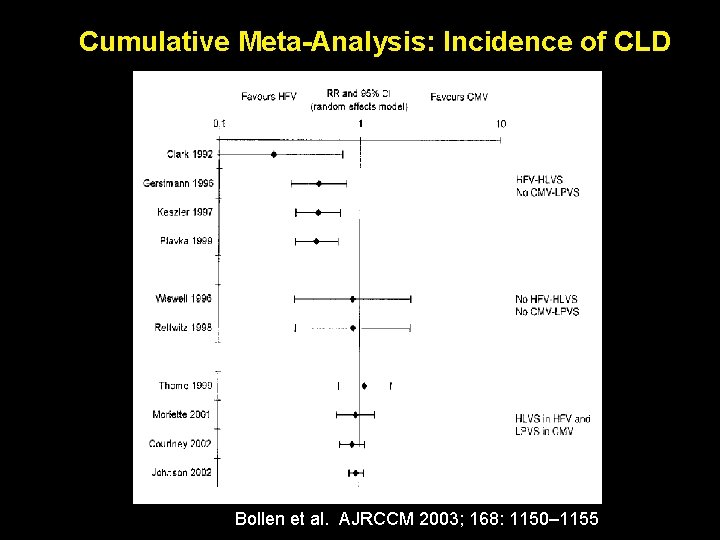
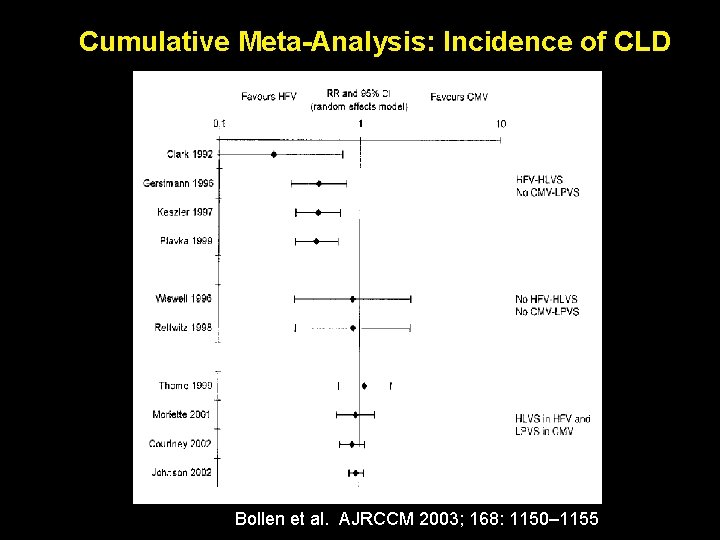
Cumulative Meta-Analysis: Incidence of CLD Bollen et al. AJRCCM 2003; 168: 1150– 1155
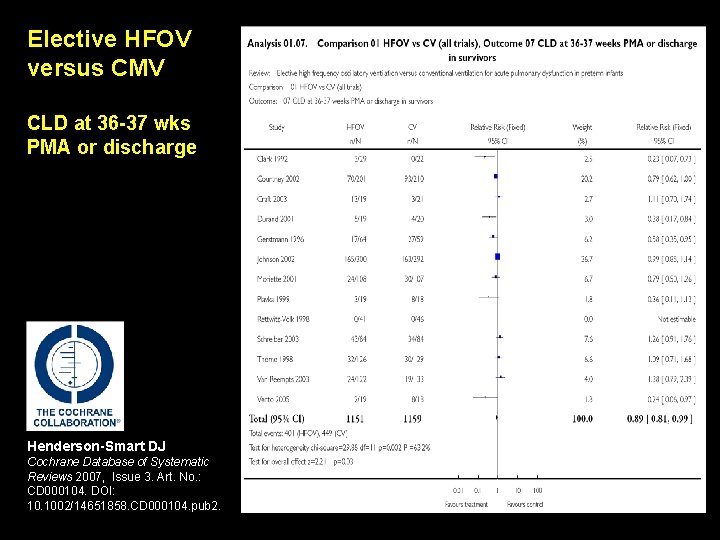
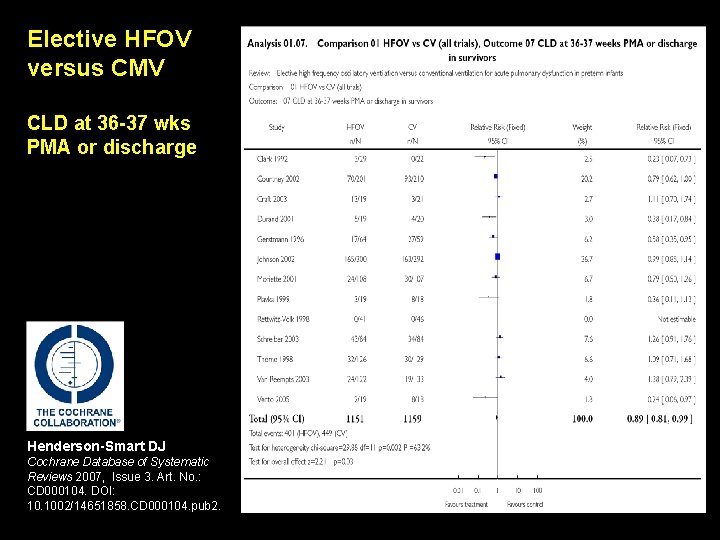
Elective HFOV versus CMV CLD at 36 -37 wks PMA or discharge Henderson-Smart DJ Cochrane Database of Systematic Reviews 2007, Issue 3. Art. No. : CD 000104. DOI: 10. 1002/14651858. CD 000104. pub 2.
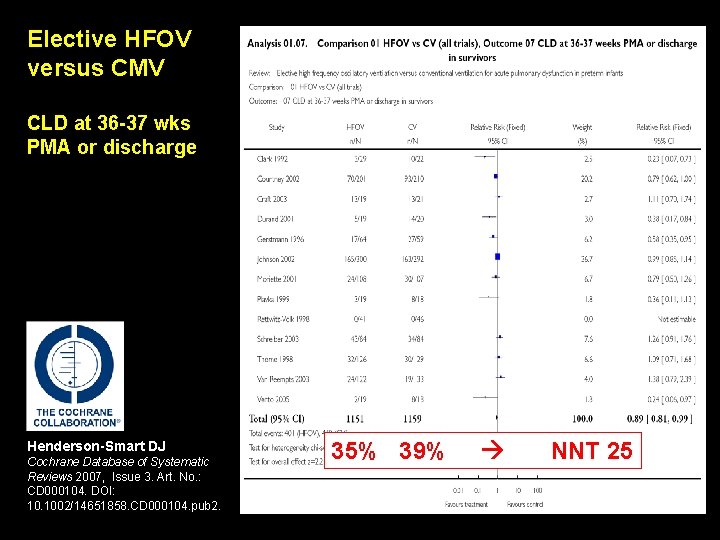
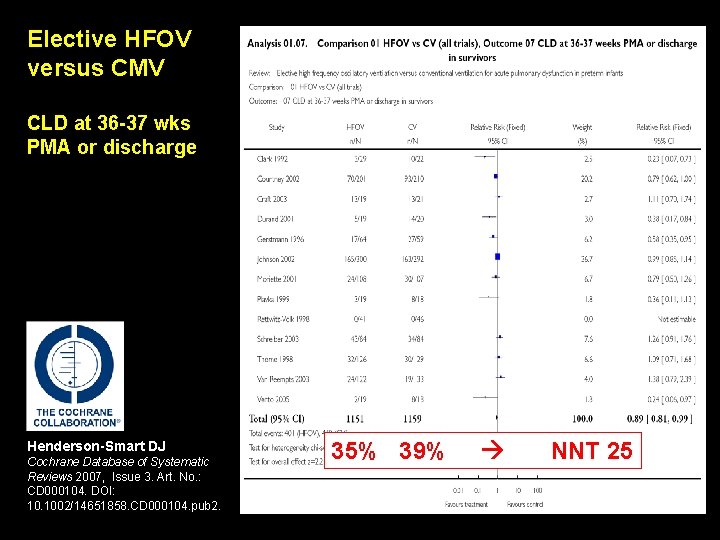
Elective HFOV versus CMV CLD at 36 -37 wks PMA or discharge Henderson-Smart DJ Cochrane Database of Systematic Reviews 2007, Issue 3. Art. No. : CD 000104. DOI: 10. 1002/14651858. CD 000104. pub 2. 35% 39% NNT 25
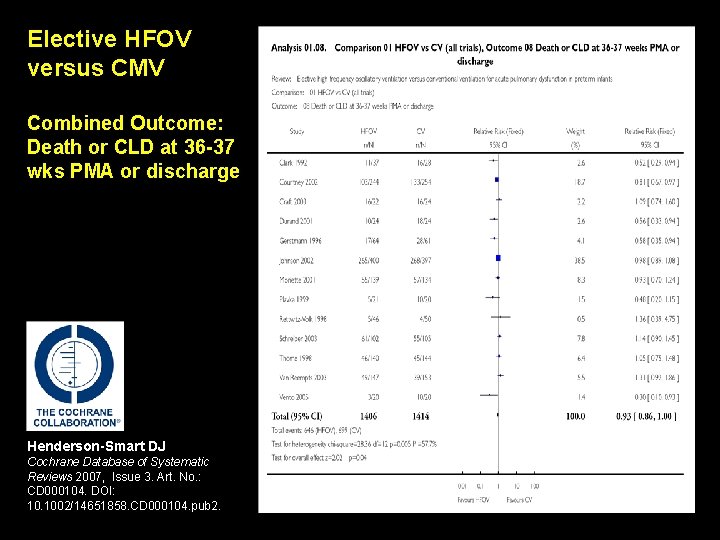
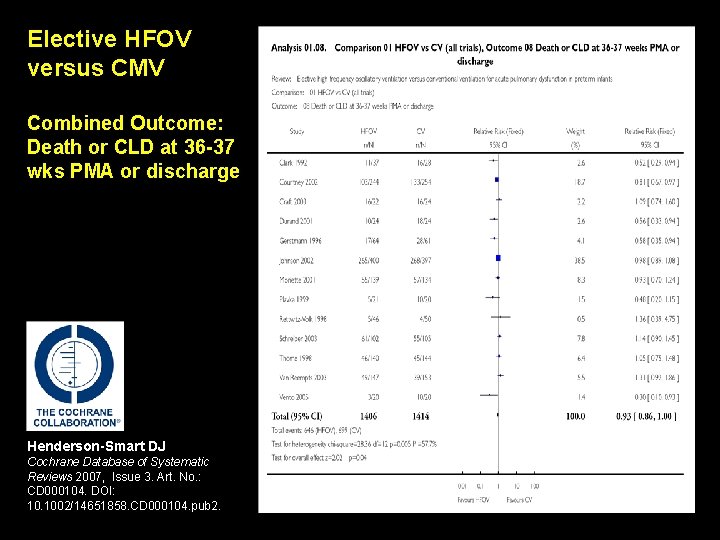
Elective HFOV versus CMV Combined Outcome: Death or CLD at 36 -37 wks PMA or discharge Henderson-Smart DJ Cochrane Database of Systematic Reviews 2007, Issue 3. Art. No. : CD 000104. DOI: 10. 1002/14651858. CD 000104. pub 2.
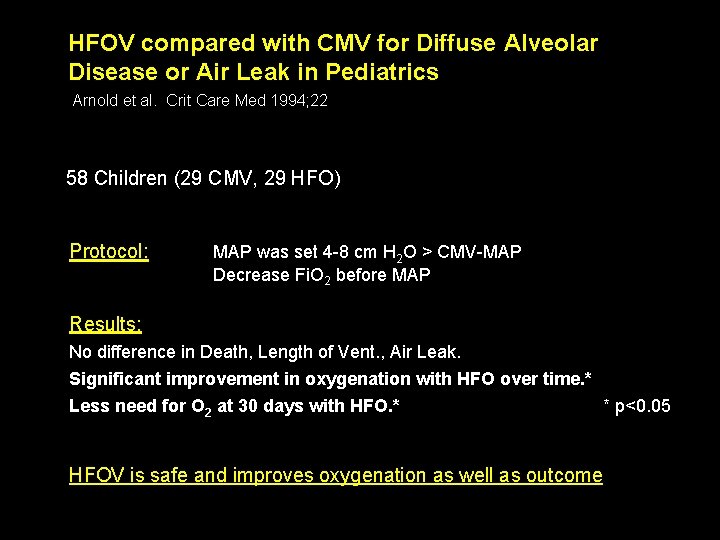
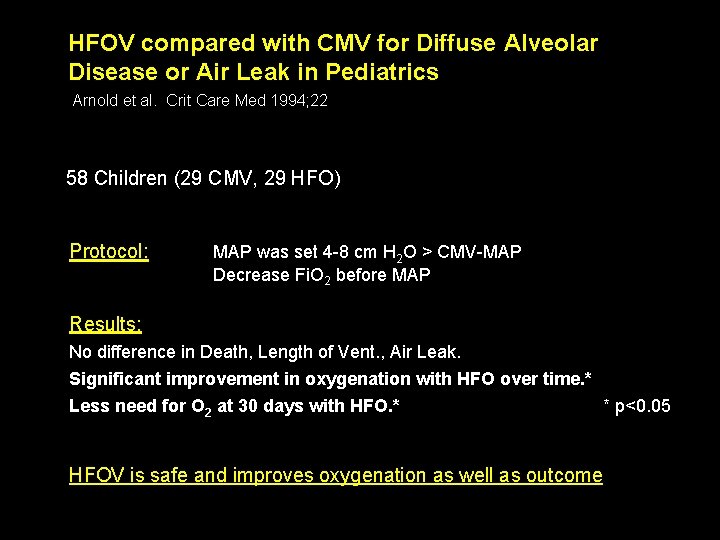
HFOV compared with CMV for Diffuse Alveolar Disease or Air Leak in Pediatrics Arnold et al. Crit Care Med 1994; 22 58 Children (29 CMV, 29 HFO) Protocol: MAP was set 4 -8 cm H 2 O > CMV-MAP Decrease Fi. O 2 before MAP Results: No difference in Death, Length of Vent. , Air Leak. Significant improvement in oxygenation with HFO over time. * Less need for O 2 at 30 days with HFO. * * p<0. 05 HFOV is safe and improves oxygenation as well as outcome
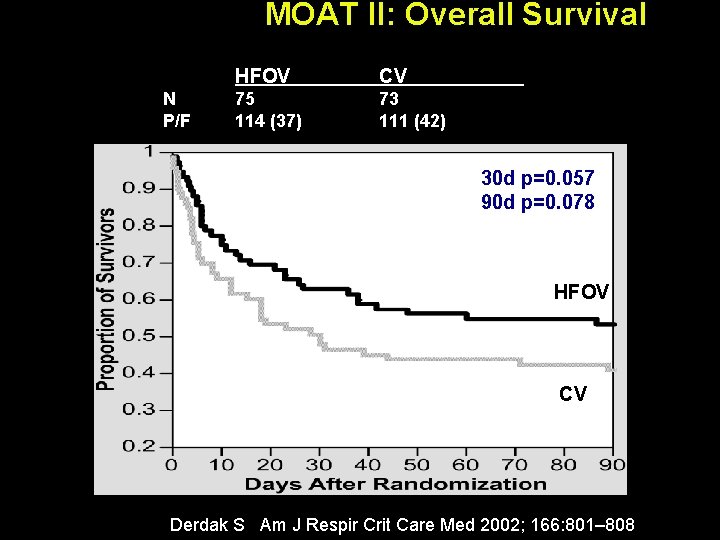
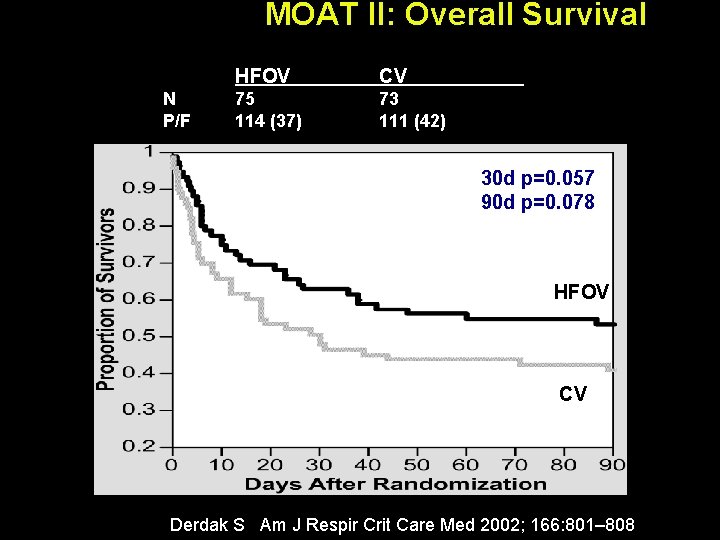
MOAT II: Overall Survival N P/F HFOV CV 75 114 (37) 73 111 (42) 30 d p=0. 057 90 d p=0. 078 HFOV CV Derdak S Am J Respir Crit Care Med 2002; 166: 801– 808
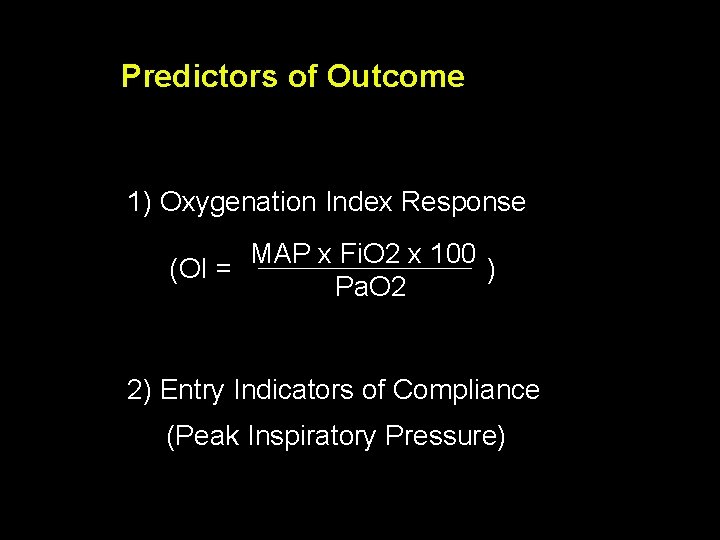
Predictors of Outcome 1) Oxygenation Index Response MAP x Fi. O 2 x 100 (OI = ) Pa. O 2 2) Entry Indicators of Compliance (Peak Inspiratory Pressure)
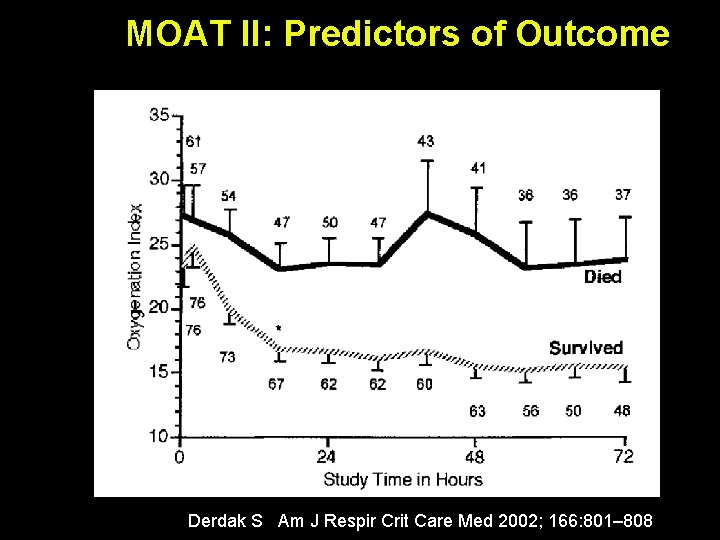
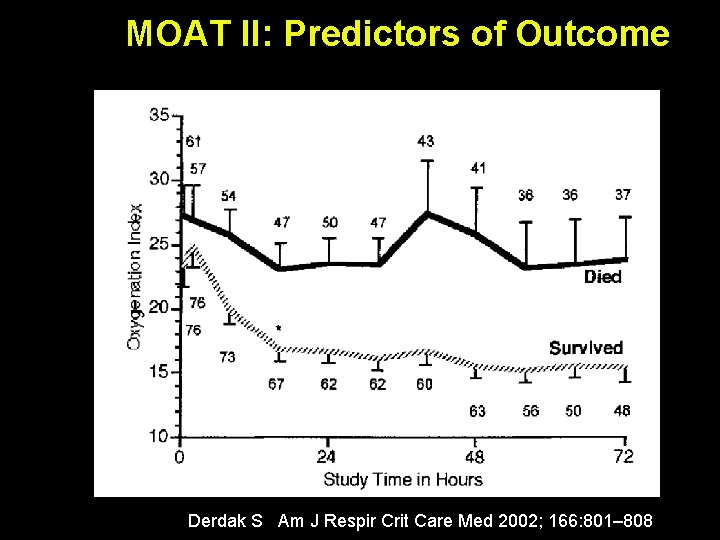
MOAT II: Predictors of Outcome Derdak S Am J Respir Crit Care Med 2002; 166: 801– 808
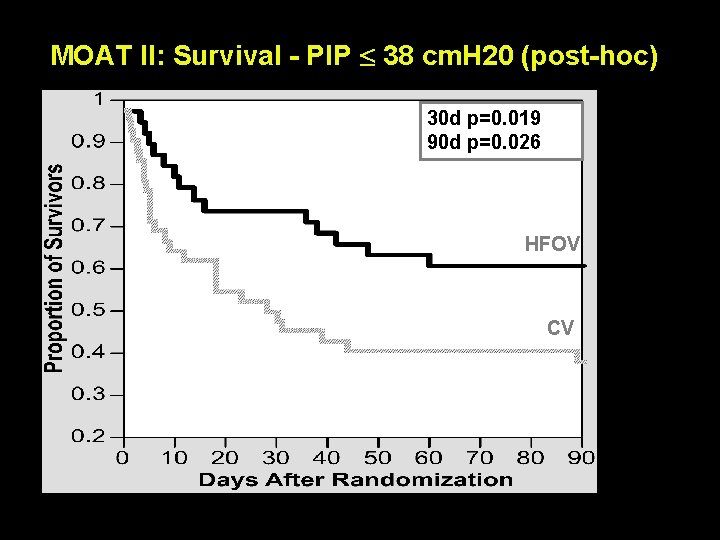
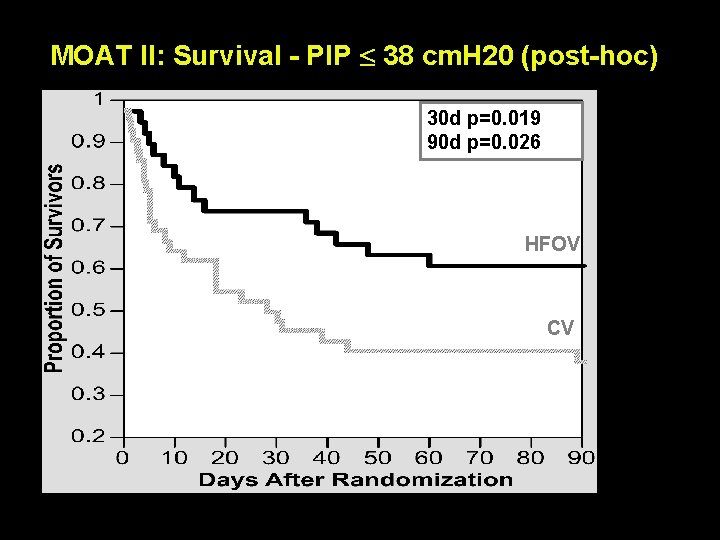
MOAT II: Survival - PIP 38 cm. H 20 (post-hoc) 30 d p=0. 019 90 d p=0. 026 HFOV CV HFV-Meeting 2001
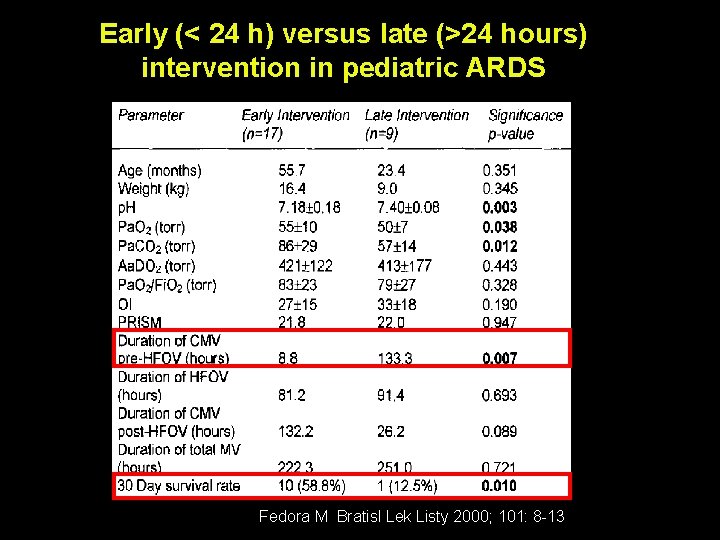
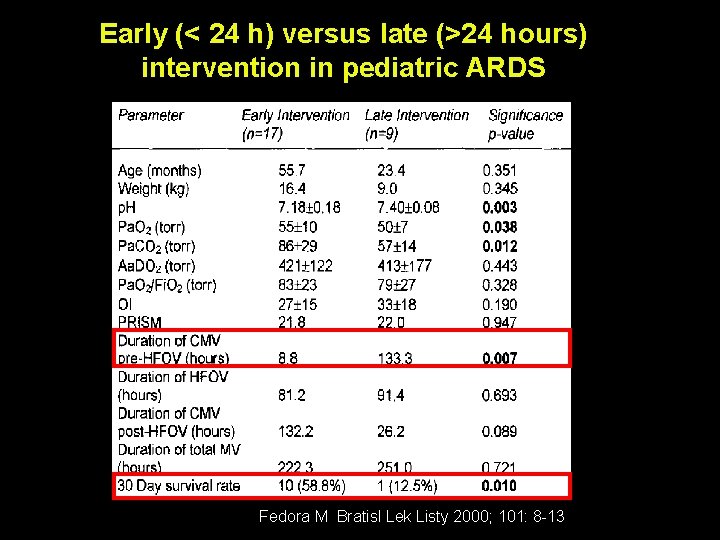
Early (< 24 h) versus late (>24 hours) intervention in pediatric ARDS Fedora M Bratisl Lek Listy 2000; 101: 8 -13
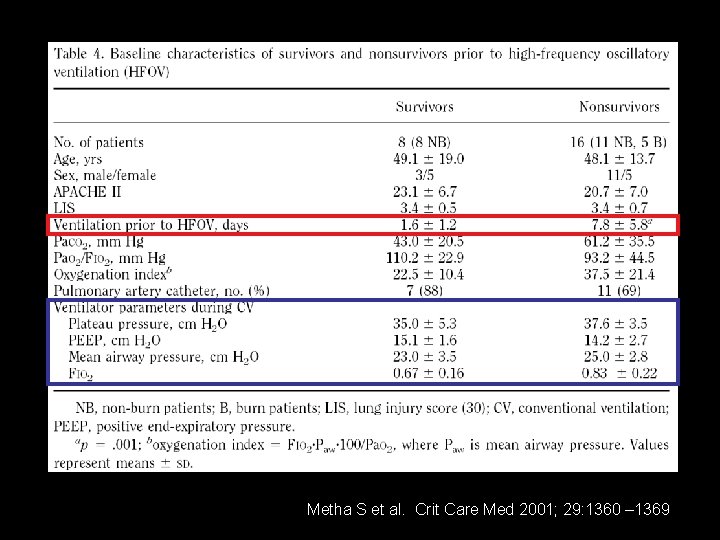
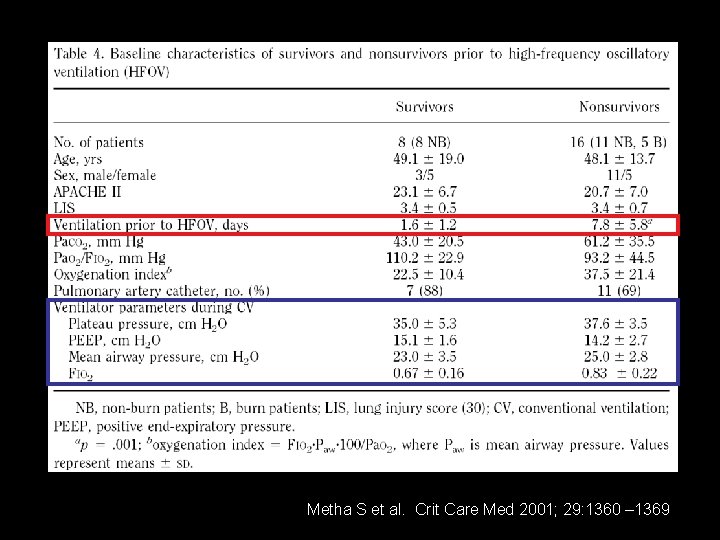
Metha S et al. Crit Care Med 2001; 29: 1360 – 1369
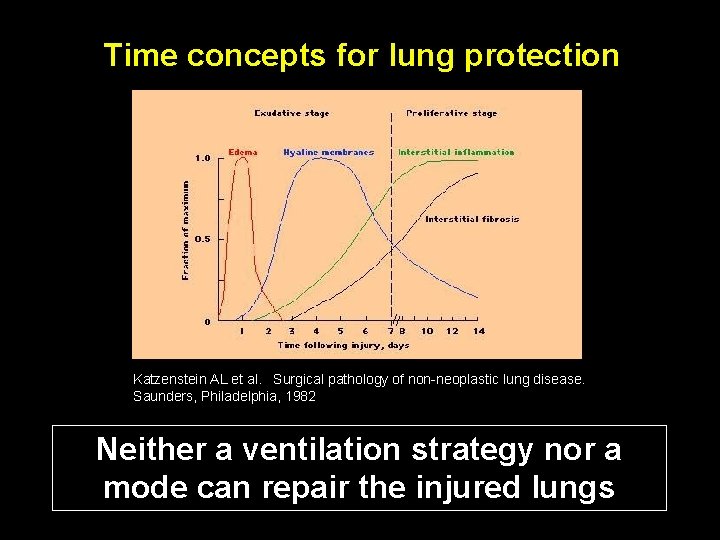
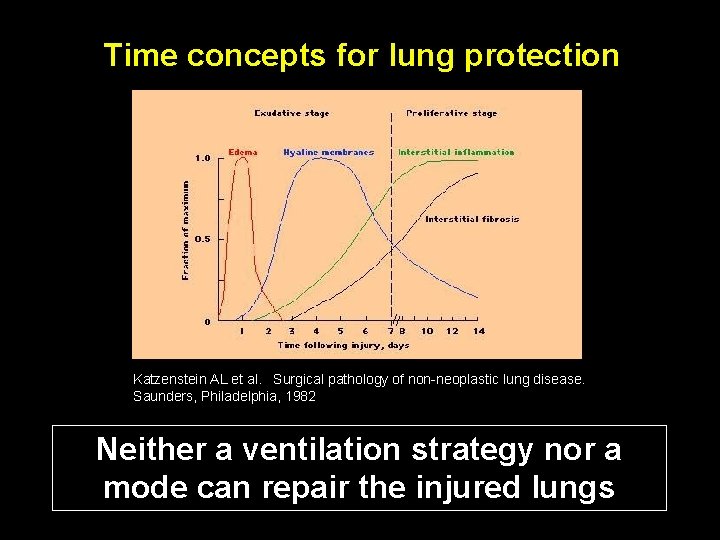
Time concepts for lung protection Katzenstein AL et al. Surgical pathology of non-neoplastic lung disease. Saunders, Philadelphia, 1982 Neither a ventilation strategy nor a mode can repair the injured lungs
First Intention HFO with early lung volume recruitment Rimensberger PC et al. Pediatrics 2000; 105: 1202 -1208
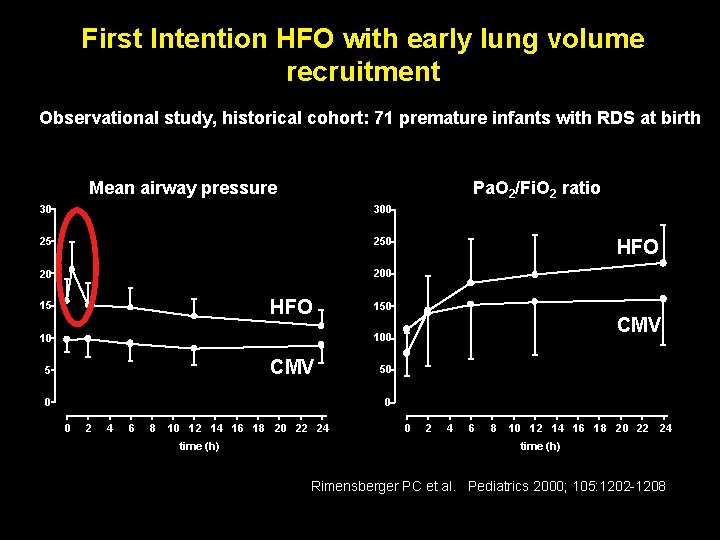
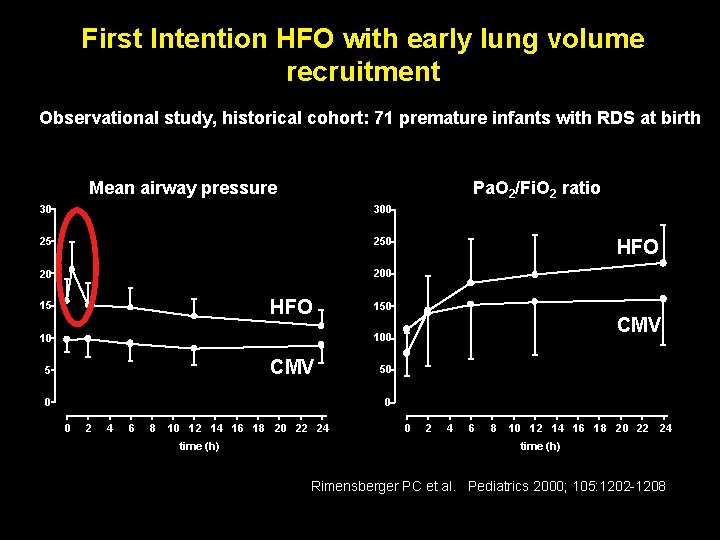
First Intention HFO with early lung volume recruitment Observational study, historical cohort: 71 premature infants with RDS at birth Mean airway pressure Pa. O 2/Fi. O 2 ratio 30 300 25 250 20 200 HFO 150 CMV 100 10 CMV 5 50 0 2 4 6 8 10 12 14 16 18 20 22 24 time (h) Rimensberger PC et al. Pediatrics 2000; 105: 1202 -1208
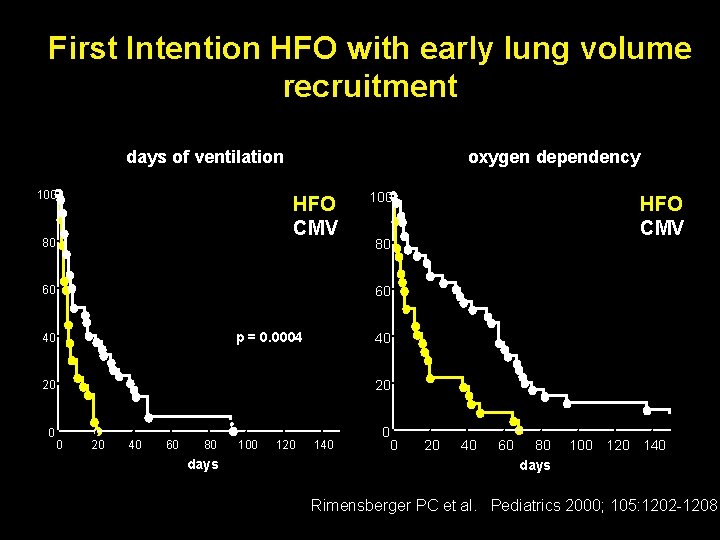
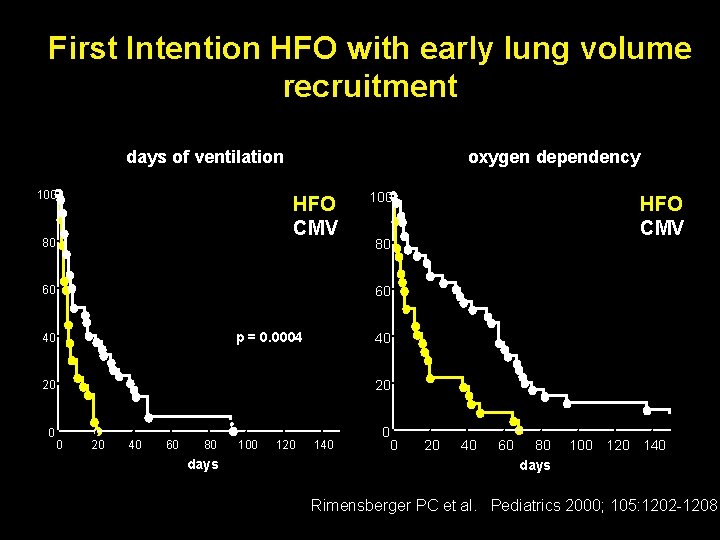
First Intention HFO with early lung volume recruitment days of ventilation 100 oxygen dependency • HFO • CMV 80 60 100 • HFO • CMV 80 60 p = 0. 0004 40 P < 0. 0001 40 20 20 n=3 0 0 20 40 60 80 days 100 120 140 Rimensberger PC et al. Pediatrics 2000; 105: 1202 -1208
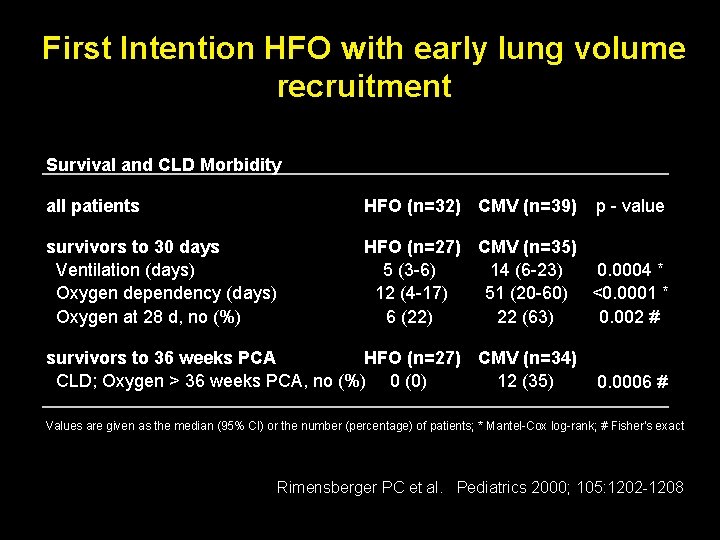
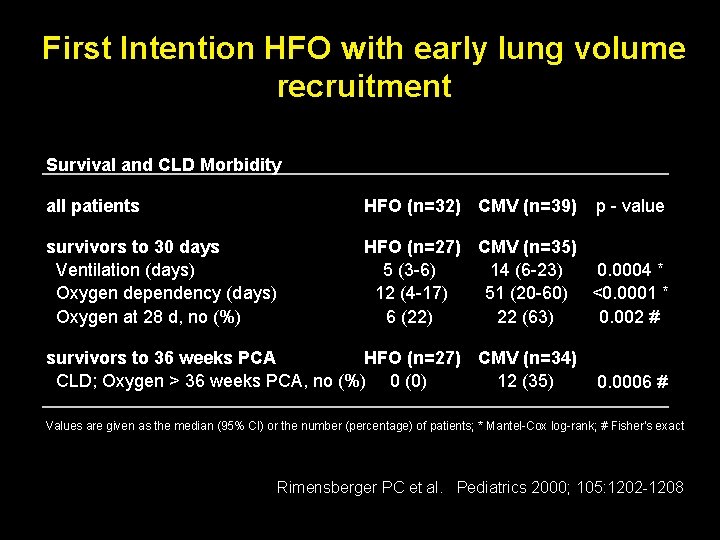
First Intention HFO with early lung volume recruitment Survival and CLD Morbidity all patients HFO (n=32) CMV (n=39) survivors to 30 days Ventilation (days) Oxygen dependency (days) Oxygen at 28 d, no (%) HFO (n=27) CMV (n=35) 5 (3 -6) 14 (6 -23) 0. 0004 * 12 (4 -17) 51 (20 -60) <0. 0001 * 6 (22) 22 (63) 0. 002 # survivors to 36 weeks PCA HFO (n=27) CMV (n=34) CLD; Oxygen > 36 weeks PCA, no (%) 0 (0) 12 (35) p - value 0. 0006 # Values are given as the median (95% CI) or the number (percentage) of patients; * Mantel-Cox log-rank; # Fisher's exact Rimensberger PC et al. Pediatrics 2000; 105: 1202 -1208
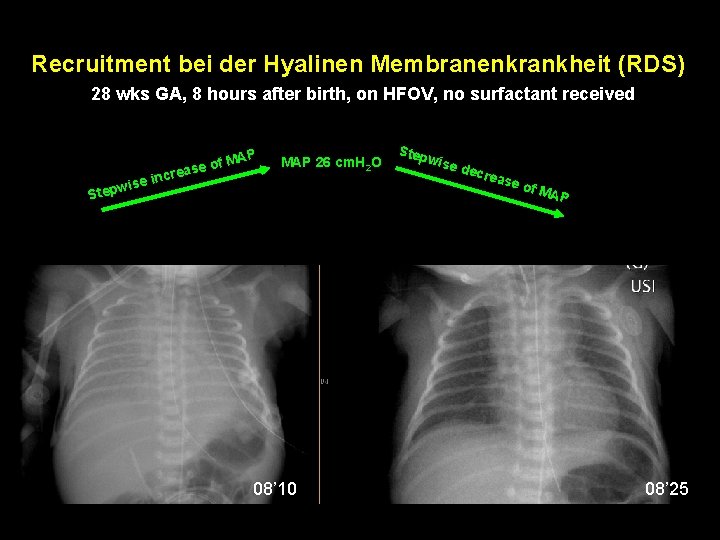
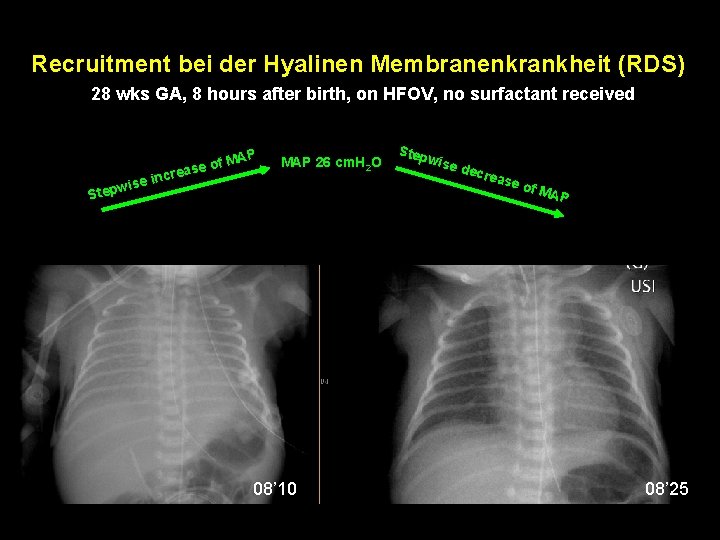
Recruitment bei der Hyalinen Membranenkrankheit (RDS) 28 wks GA, 8 hours after birth, on HFOV, no surfactant received se in i w p e P f MA o e s crea MAP 26 cm. H 2 O St MAP 12 cm. H 2 O, Amplitude 40, Fi. O 2 0. 8 08’ 10 Step wise decr e ase of M AP MAP 16 cm. H 2 O, Amplitude 28, Fi. O 2 0. 21 08’ 25
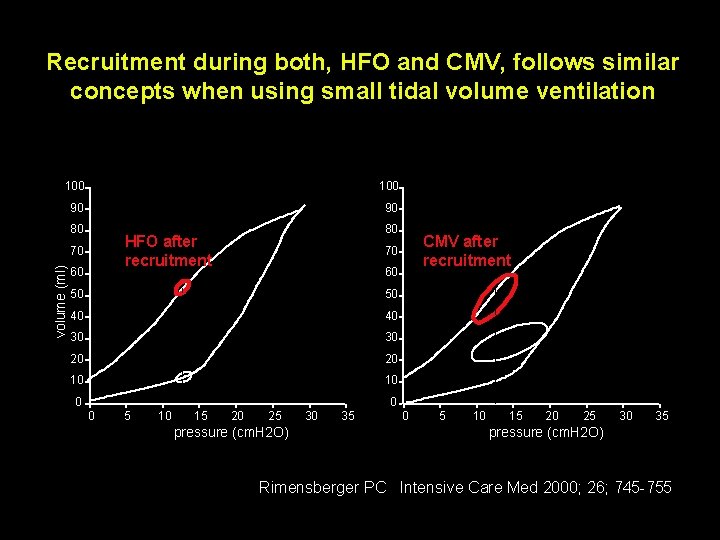
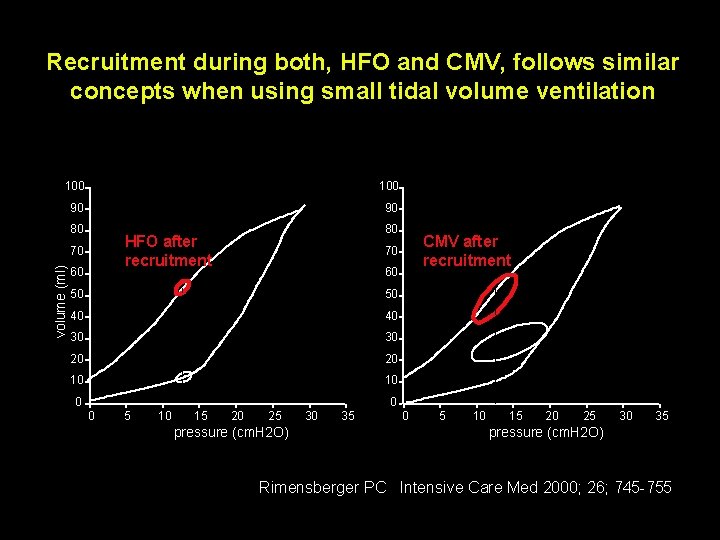
Recruitment during both, HFO and CMV, follows similar concepts when using small tidal volume ventilation 100 90 90 80 70 volume (ml) 80 HFO after recruitment 60 60 50 50 40 40 30 30 20 20 10 10 0 5 10 15 CMV after recruitment 70 20 25 pressure (cm. H 2 O) 30 35 0 5 10 15 20 25 30 35 pressure (cm. H 2 O) Rimensberger PC Intensive Care Med 2000; 26; 745 -755
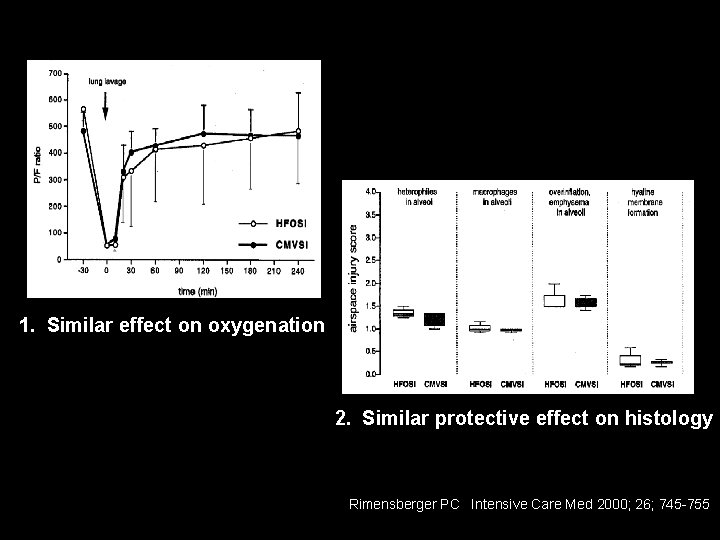
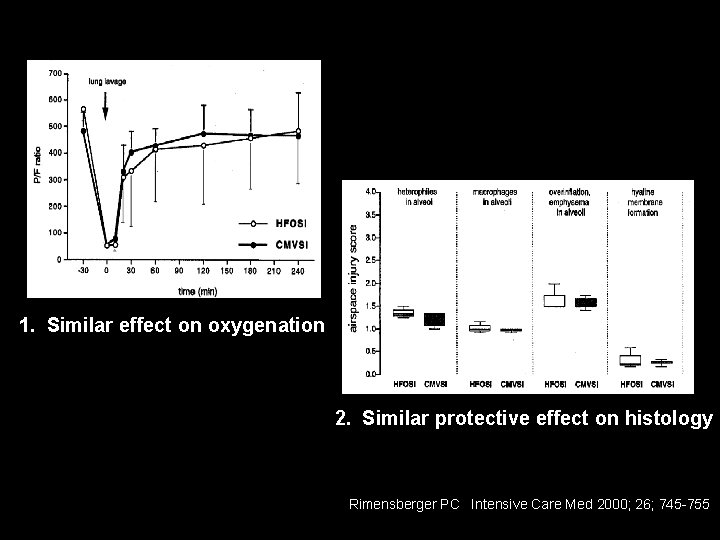
1. Similar effect on oxygenation 2. Similar protective effect on histology Rimensberger PC Intensive Care Med 2000; 26; 745 -755
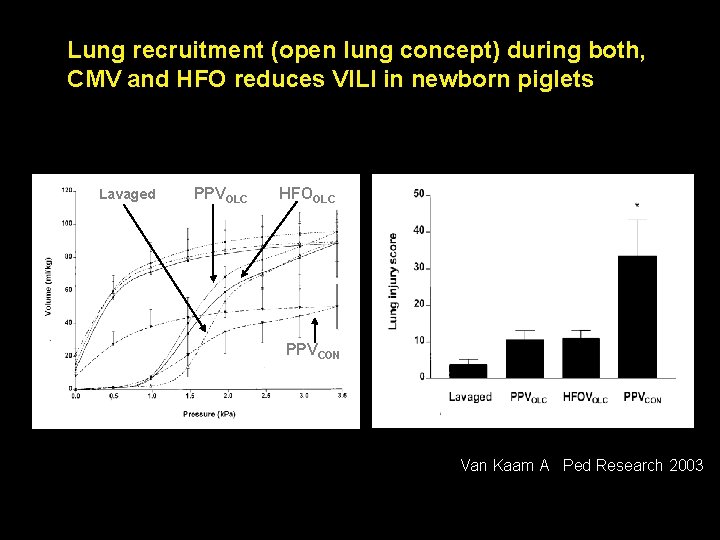
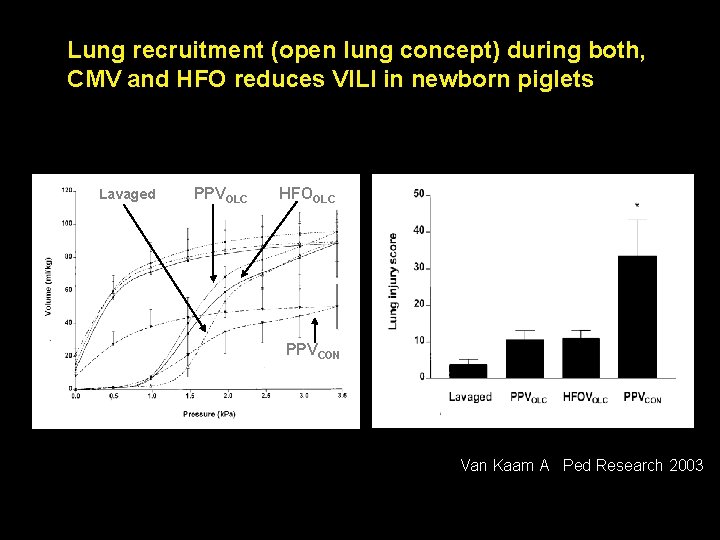
Lung recruitment (open lung concept) during both, CMV and HFO reduces VILI in newborn piglets Lavaged PPVOLC HFOOLC PPVCON Van Kaam A Ped Research 2003
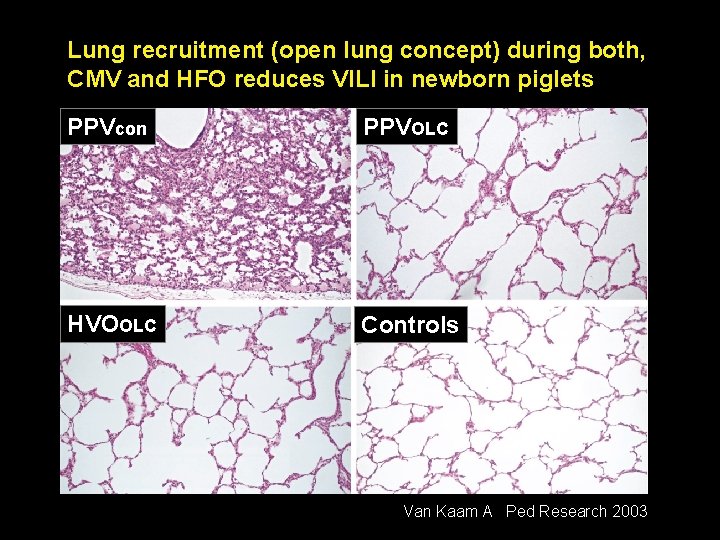
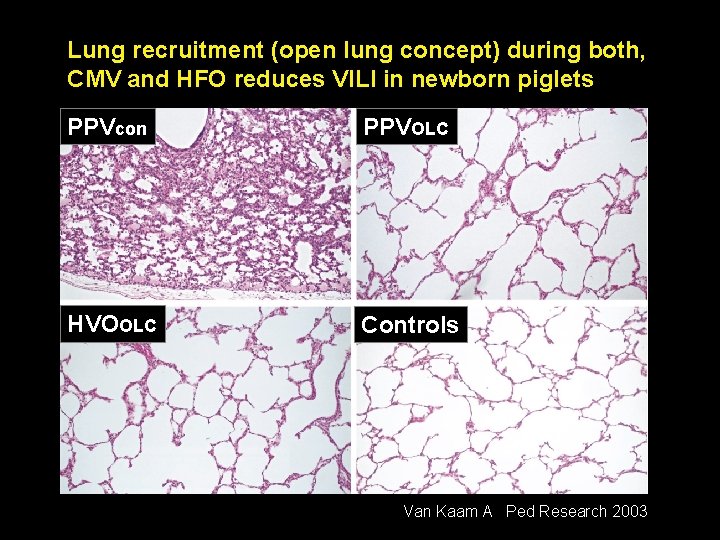
Lung recruitment (open lung concept) during both, CMV and HFO reduces VILI in newborn piglets PPVcon PPVOLC HVOOLC Controls Van Kaam A Ped Research 2003
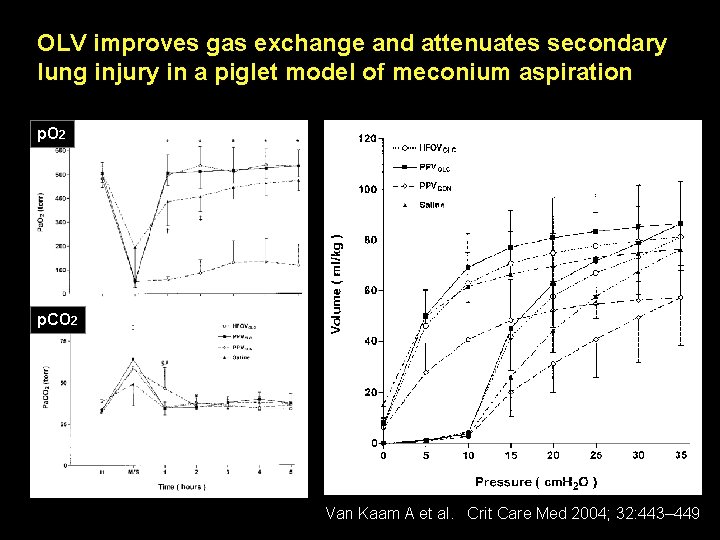
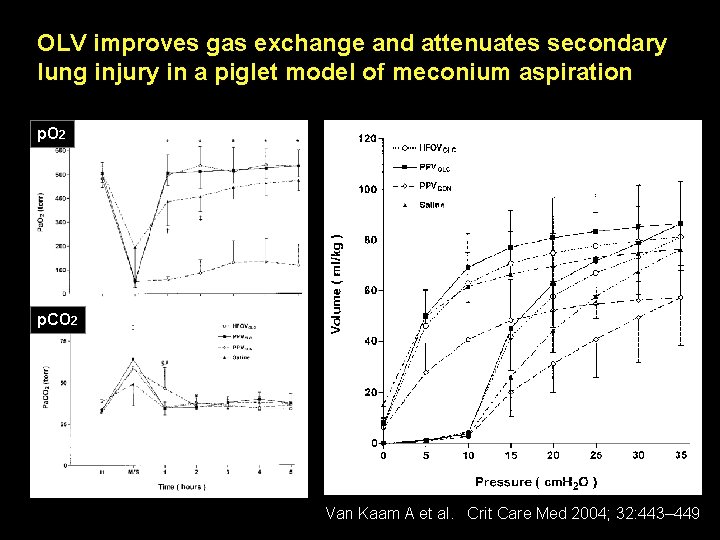
OLV improves gas exchange and attenuates secondary lung injury in a piglet model of meconium aspiration p. O 2 p. CO 2 Van Kaam A et al. Crit Care Med 2004; 32: 443– 449
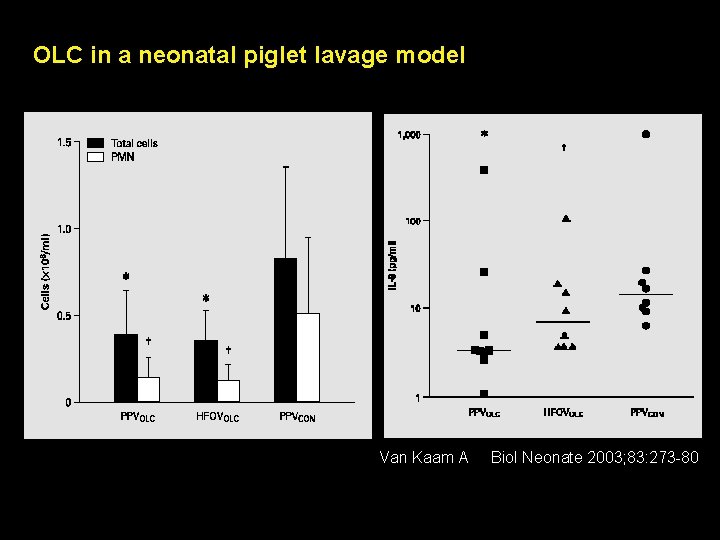
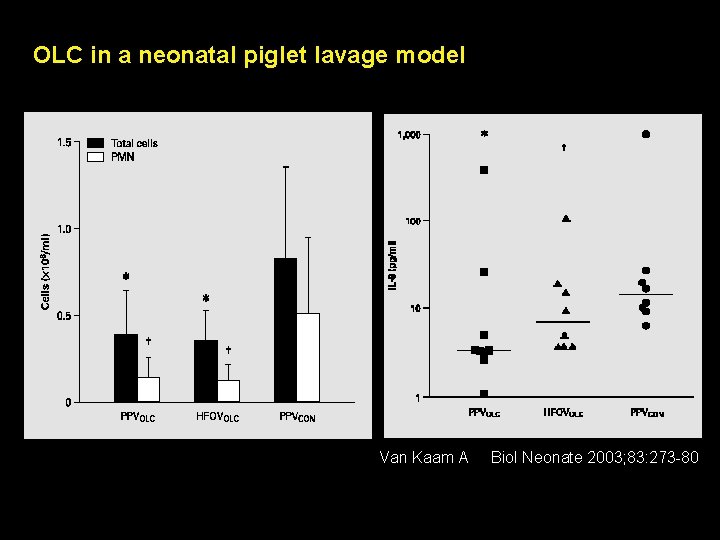
OLC in a neonatal piglet lavage model Van Kaam A Biol Neonate 2003; 83: 273 -80
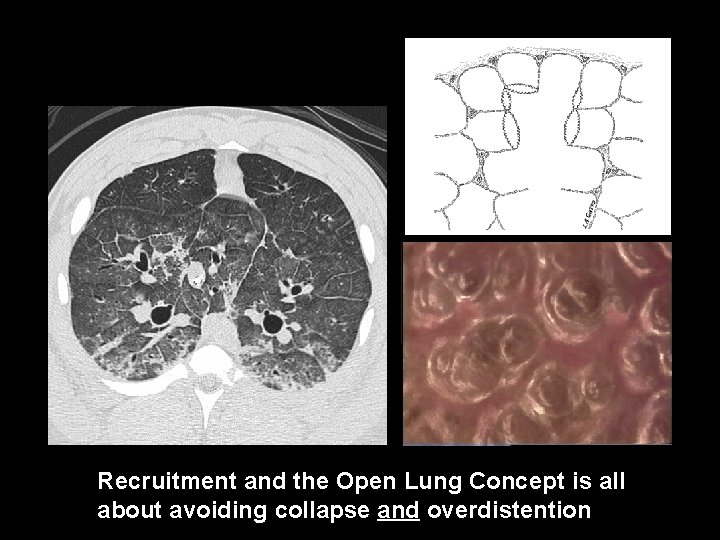
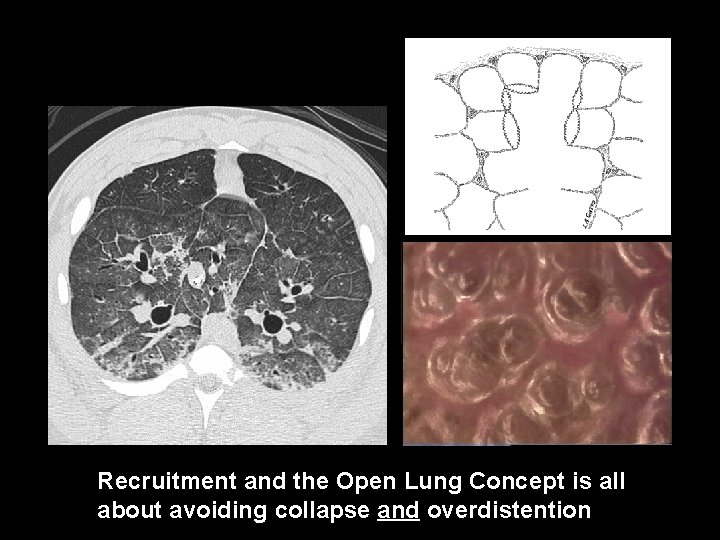
Recruitment and the Open Lung Concept is all about avoiding collapse and overdistention
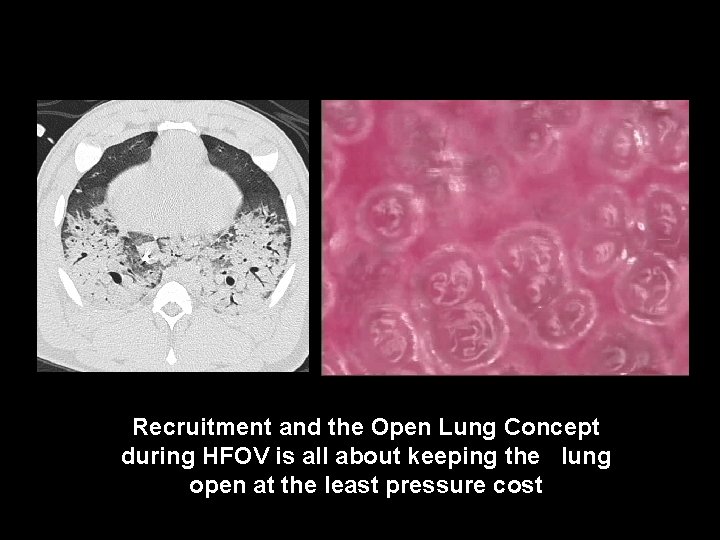
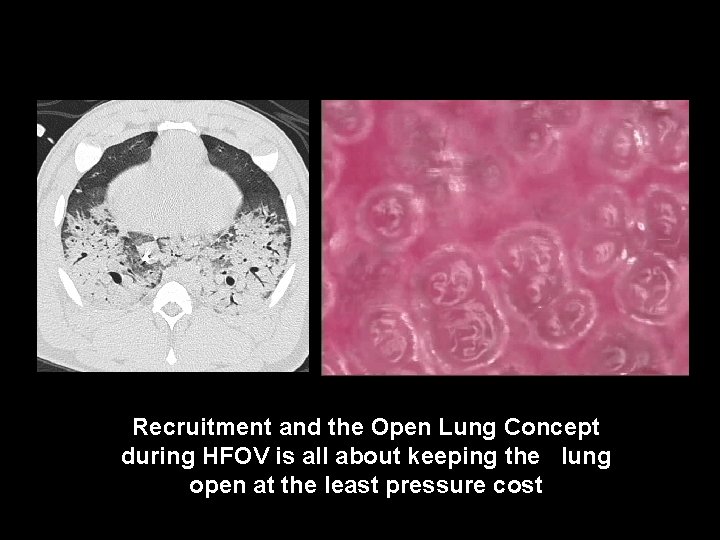
Recruitment and the Open Lung Concept during HFOV is all about keeping the lung open at the least pressure cost
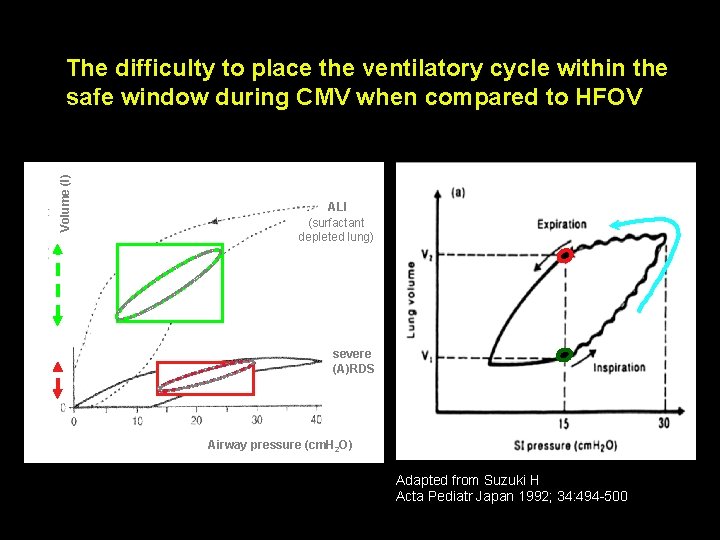
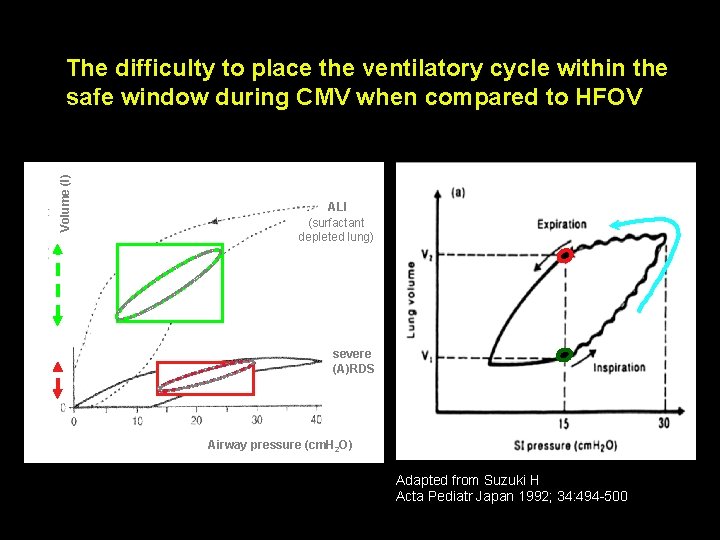
Volume (l) The difficulty to place the ventilatory cycle within the safe window during CMV when compared to HFOV ALI (surfactant depleted lung) severe (A)RDS Airway pressure (cm. H 2 O) Adapted from Suzuki H Acta Pediatr Japan 1992; 34: 494 -500
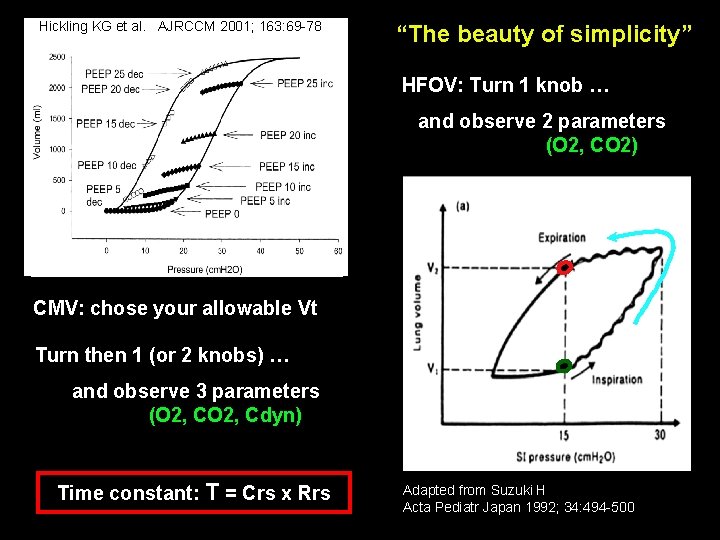
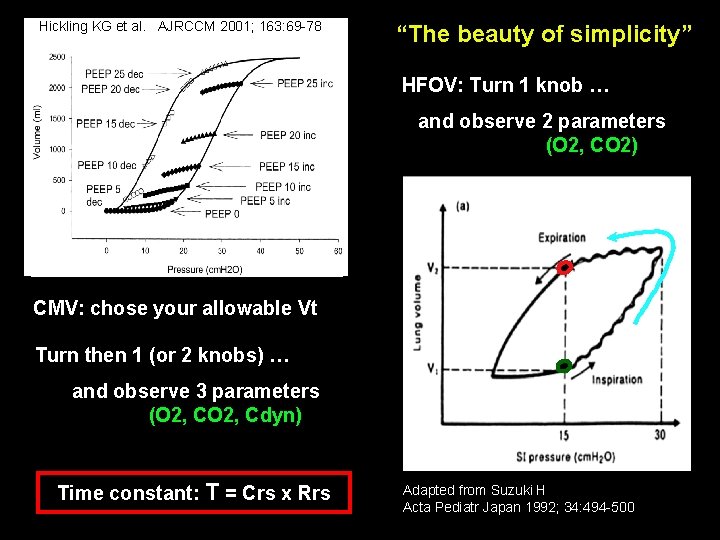
Hickling KG et al. AJRCCM 2001; 163: 69 -78 “The beauty of simplicity” HFOV: Turn 1 knob … and observe 2 parameters (O 2, CO 2) CMV: chose your allowable Vt Turn then 1 (or 2 knobs) … and observe 3 parameters (O 2, Cdyn) and remember to adapt Ti and Te Time constant: T = Crs x Rrs Adapted from Suzuki H Acta Pediatr Japan 1992; 34: 494 -500