High Frequency Oscillatory Ventilation Bradley Fuhrman MD Professor
High Frequency Oscillatory Ventilation Bradley Fuhrman, MD Professor and Chair, Department of Pediatrics brad. fuhrman@ttuhsc. edu COI – but will not discuss: Royalty Cook Catheter Equity Medical Conservation Devices 1

HFOV is a lung protective strategy. The natural history of acute respiratory failure is influenced by the way the lung is ventilated. The cardinal feature of Ventilator Induced Lung Injury (VILI) is pulmonary edema formation. 2

Effects of High Pressure Ventilation • Normal, 5 min @ 45 cm H 2 O, 20 min @ 45 cm H 2 O (Dreyfuss and Saumon) 3

Over-Distension Pulmonary Edema Is Protein Rich 4
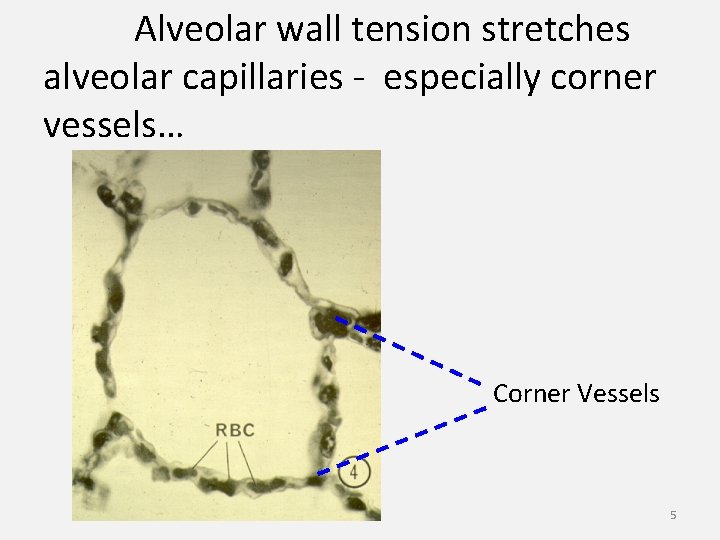
Alveolar wall tension stretches alveolar capillaries - especially corner vessels… Corner Vessels 5

Increased Wall Tension Raises Transmural Pressure Across Corner Vessels Alveolar Septum Interstitial Pressure Capillary Pressure Corner Vessel Alveolar Septum High lung volume and high surface tension promote transudation. 6

Traction on capillaries causes endothelial cell disruption. • allows PMNs to contact basement membrane • PMNs accumulate after several hours of VILI 7
Biotrauma • • • Neutrophil accumulation Neutrophil activation Cytokine elaboration Inflammation Increased capillary permeability to water, albumin and other proteins 8
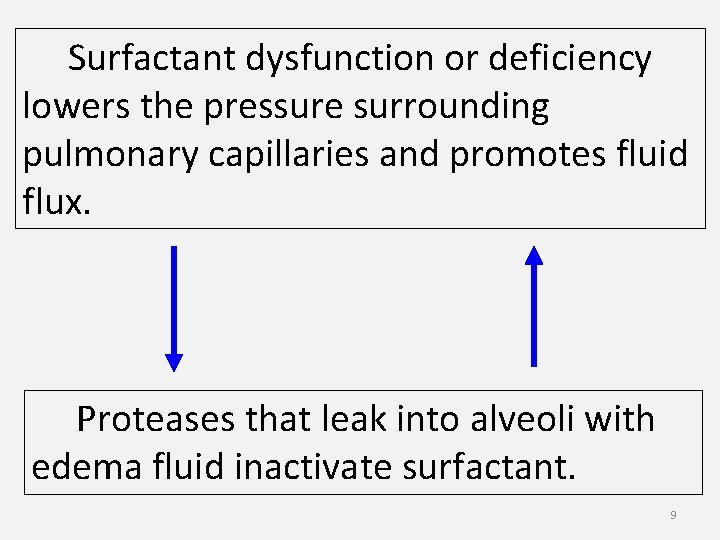
Surfactant dysfunction or deficiency lowers the pressure surrounding pulmonary capillaries and promotes fluid flux. Proteases that leak into alveoli with edema fluid inactivate surfactant. 9

Mechanisms of VILI • Increased vascular transmural pressure causes transudation of fluid • Surfactant dysfunction promotes capillary filtration • Direct trauma causes permeability edema • Biotrauma and inflammation promote capillary permeability and oxidative injury to cell membranes and other cell components 10

Mechanisms of VILI • Increased vascular transmural pressure causes transudation of fluid • Surfactant dysfunction promotes capillary filtration • Direct trauma causes permeability edema • Biotrauma and inflammation promote capillary permeability and oxidative injury to cell membranes and other cell components 11

Mechanisms of VILI • Increased vascular transmural pressure causes transudation of fluid • Surfactant dysfunction promotes capillary filtration • Direct trauma causes permeability edema • Biotrauma and inflammation promote capillary permeability and oxidative injury to cell membranes and other cell components 12
Mechanisms of VILI • Increased vascular transmural pressure causes transudation of fluid • Surfactant dysfunction promotes capillary filtration • Direct trauma causes permeability edema • Biotrauma and inflammation promote capillary permeability and oxidative injury to cell membranes and other cell components 13
Which clinical choices promote or avoid VILI ? 14

Volutrauma vs Barotrauma High Vt, High Paw Positive Pressure Vent High Vt, Paw=0 Negative Pressure Vent Thoracoabdominal. Strapped High Pressure Low Vt VILI can occur at high lung volume despite low airway pressure… 15
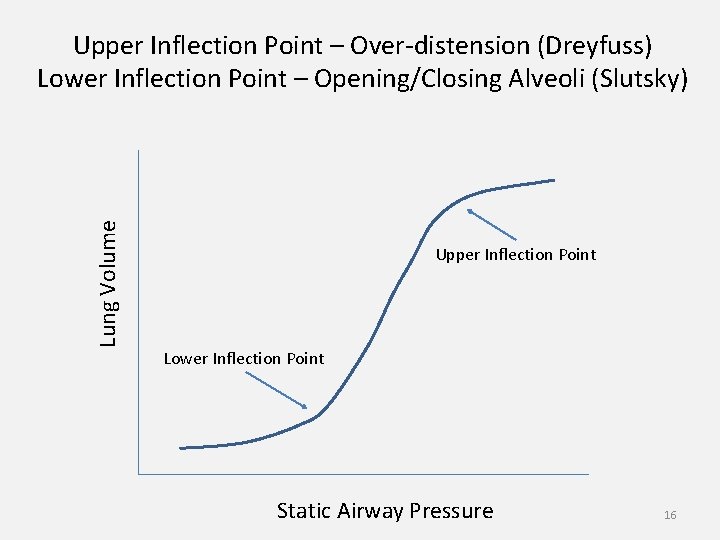
Lung Volume Upper Inflection Point – Over-distension (Dreyfuss) Lower Inflection Point – Opening/Closing Alveoli (Slutsky) Upper Inflection Point Lower Inflection Point Static Airway Pressure 16
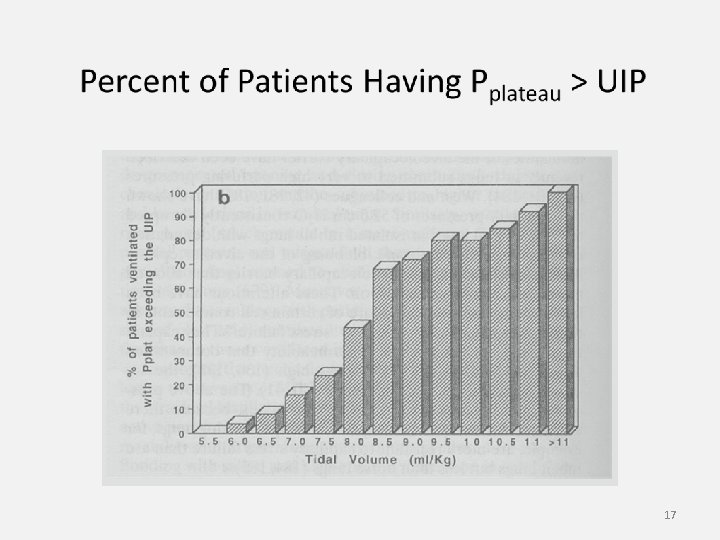
17
Open Lung Strategy to Avoid VILI PEEP > LIP Pplateau < UIP Amato et al (1995) 18
NIH ARDS Network Trial (PEEP not controlled) 6 ml/kg vs 12 ml/kg low TV 30% Mortality high TV 40% Mortality 19
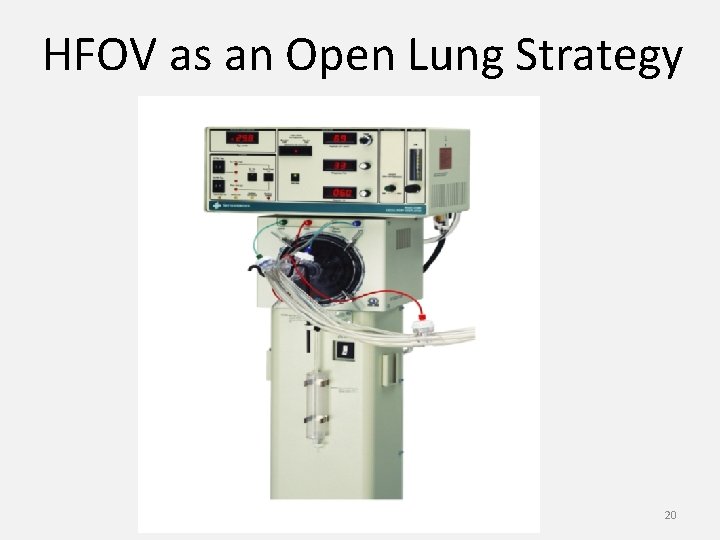
HFOV as an Open Lung Strategy 20
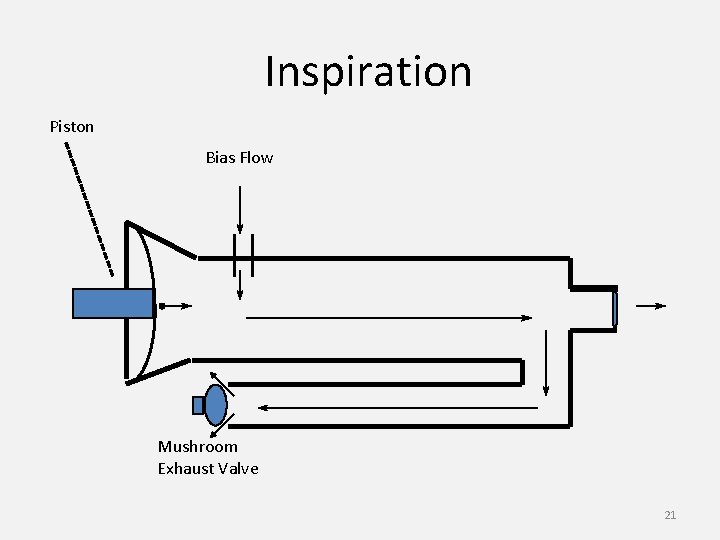
Inspiration Piston Bias Flow Mushroom Exhaust Valve 21

Expiration Piston Bias Flow Mushroom Exhaust Valve 22
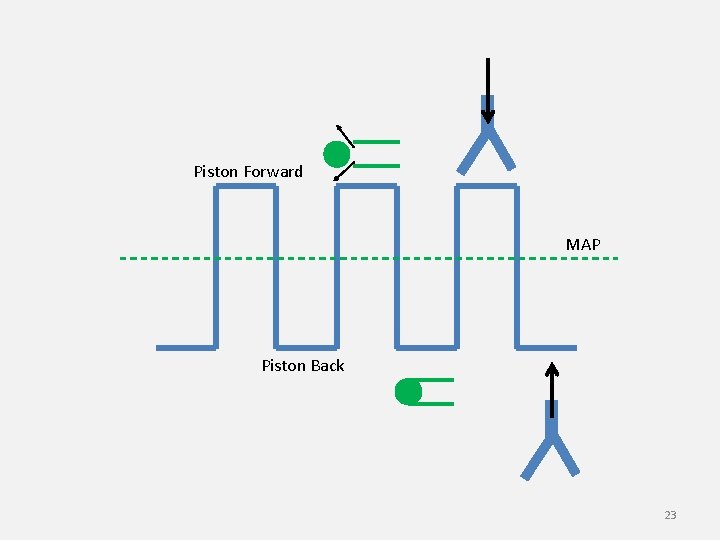
Piston Forward MAP Piston Back 23
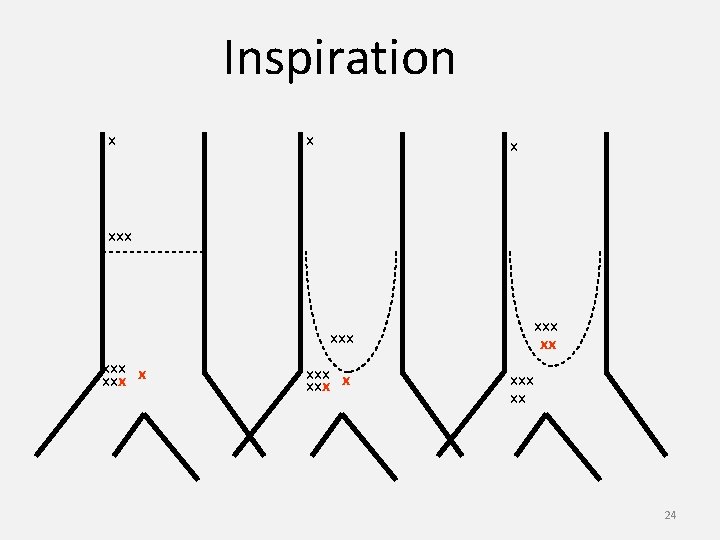
Inspiration x xxx xxx xxx xx 24
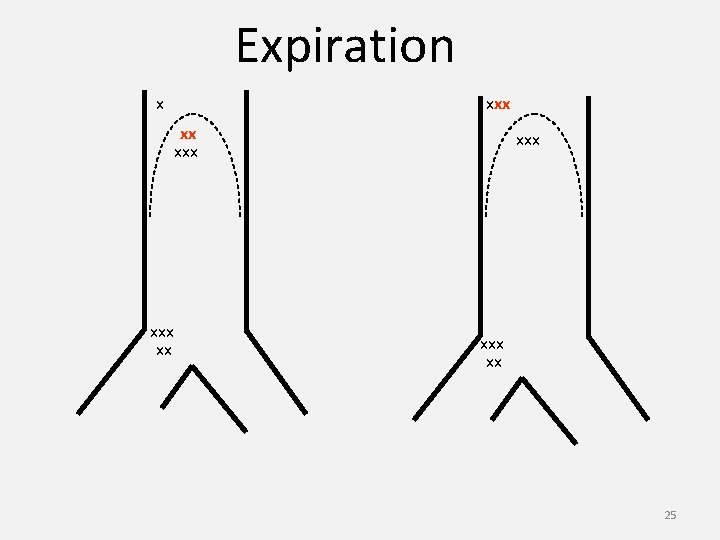
Expiration x xxx xx 25
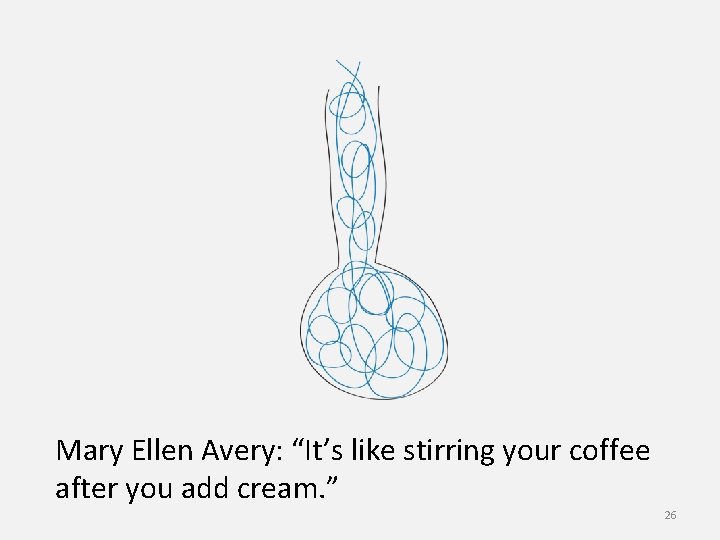
Mary Ellen Avery: “It’s like stirring your coffee after you add cream. ” 26
Indications for HFOV Open Lung Strategy – Lung Protective A Rescue Strategy ØExcessive Peak Pressure (Above UIP) ØAir Leak at High Peak Airway Pressure ØVery Low FRC Requiring High Airway Pressure to Maintain Oxygenation ØVery low Compliance Limiting TV - Causing Hypercarbia ØCardiac Output Impaired by High Peak Airway Pressure 27

How to Use HFOV in an Open Lung Strategy Set mean airway pressure between LIP and UIP Assure Oxygenation Increase amplitude until CO 2 clearance becomes adequate 28
Setting MAP Open Lung Strategy Ø Generally start 5 to 7 cm H 2 O above MAP on conventional mechanical ventilation Ø Increase as needed to achieve desired oxygenation Ø May be limited by effect on cardiac filling Ø MAP is set by adjusting pressure at which mushroom valve opens. 29
Setting Amplitude ØAmplitude impacts p. CO 2 ØTV proportional to amplitude ØAmplitude set by adjusting power (piston excursion) ØReading of amplitude is before endotracheal tube ØShould see jiggle at thighs 30

31
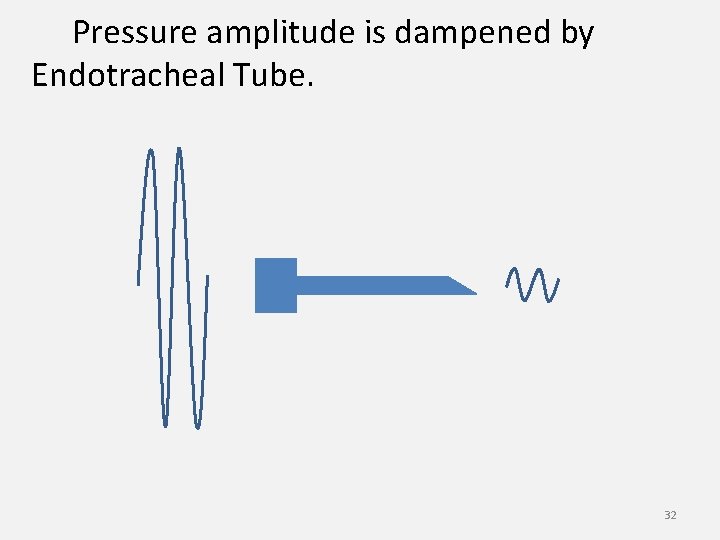
Pressure amplitude is dampened by Endotracheal Tube. 32
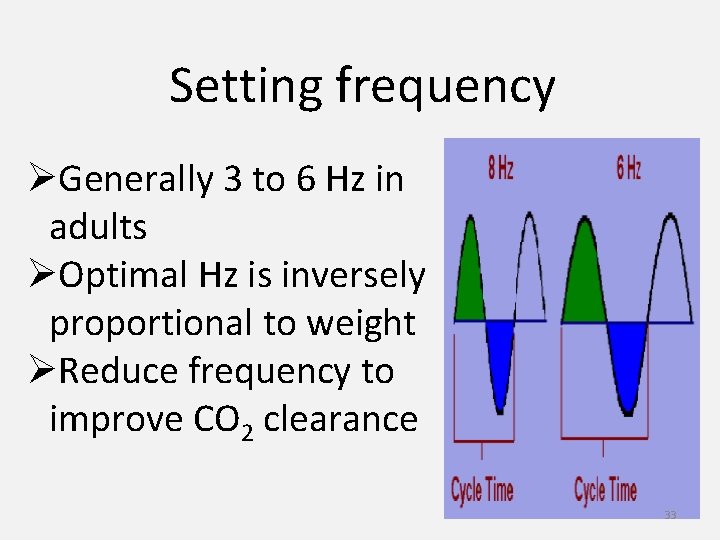
Setting frequency ØGenerally 3 to 6 Hz in adults ØOptimal Hz is inversely proportional to weight ØReduce frequency to improve CO 2 clearance 33

34
Optimal Tidal Volume ~ 2 ml/kg Not Measured 35
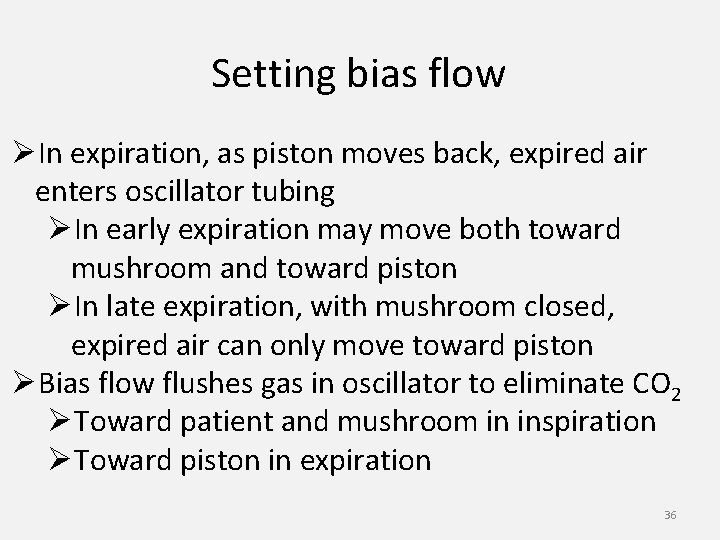
Setting bias flow ØIn expiration, as piston moves back, expired air enters oscillator tubing ØIn early expiration may move both toward mushroom and toward piston ØIn late expiration, with mushroom closed, expired air can only move toward piston ØBias flow flushes gas in oscillator to eliminate CO 2 ØToward patient and mushroom in inspiration ØToward piston in expiration 36
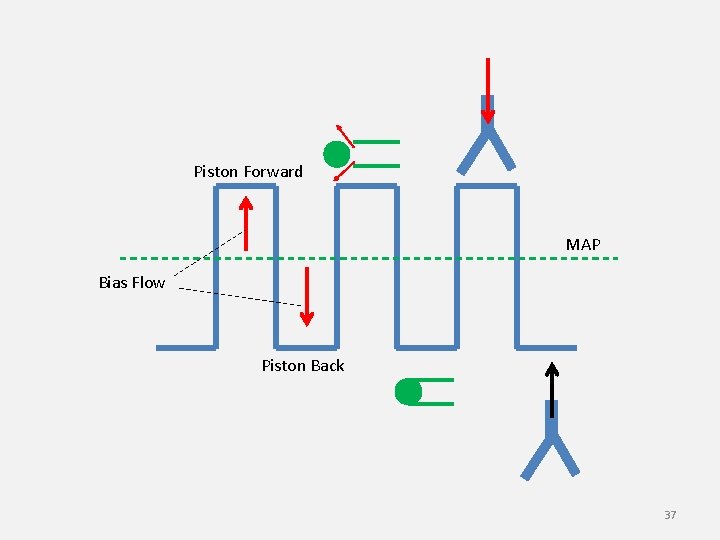
Piston Forward MAP Bias Flow Piston Back 37
Proof of Efficacy ØFDA approval based on avoidance of ECMO in MAS ØArnold et al 1994 – Better oxygenation, less barotrauma… ØBohn et al 1999 – Rev – No improvement in outcome… ØDerdak et al 2001 – RCT – Safe and effective in adults… ØRitacca et al 2003 – Rev – As good as CMV… 38

Thank you… 39
- Slides: 39