Hertfordshire MultiAgency FGM Pathway and Assessment Tool Version
![References World Health Organisation: Female genital mutilation Fact sheet: [Updated February 2020] HM Government References World Health Organisation: Female genital mutilation Fact sheet: [Updated February 2020] HM Government](https://slidetodoc.com/presentation_image_h2/b48b09da1aa1ccd6d4556ed57b5bd98e/image-25.jpg)
- Slides: 26
Hertfordshire Multi-Agency FGM Pathway and Assessment Tool (Version 2) February 2021 This document is a step by step guide to identifying children and adults at risk of Female Genital Mutilation(FGM), or who have undergone FGM Please also refer to the accompanying HSCP FGM Procedure Document Within this document you will find: A Guide to FGM Risk Factors FGM Screening Tool Health Implications FGM Prevalence FGM Services Legal Framework FGM Pathways FGM Passport All referrals to Children's services and for Looked after Children Medicals must have a risk assessment (Screening tool) attached
THE WORLD HEALTH ORGANISATION The World Health Organisation (WHO) defines Female genital mutilation (FGM) as ‘all procedures that involve partial or total removal of the external female genitalia, or other injury to the female genital organs for non-medical reasons’
THE LEGAL FRAMEWORK **** Mandatory Reporting**** Under the Serious Crime Act 2015, there is a duty on regulated professionals such as teachers, social care, health care professionals to make a report to the police where they receive a disclosure of FGM or observe physical signs of FGM on a girl under 18. Criminal Law - In England, Wales and Northern Ireland, FGM is illegal under the Female Genital Mutilation Act 2003. It is an offence for a UK resident to perform / assist or carry out FGM on oneself or another person in the UK or abroad Offence under the Female Genital Mutilation Act 2003 carries maximum penalty of 14 years imprisonment and/or a fine. Failure to Protect The Serious Crime Act 2015 makes it an offence for a person with parental responsibility (and who has frequent contact with a child) such as mother, father, guardian to fail to protect a girl (under 16) from FGM. If 18 or over, the liable adult is one who assumes responsibility for the girl in the manner of a parent. Failure to protect a child carries maximum penalty of 7 years imprisonment and/or a fine FGM Protection Order This can be issued by courts to protect girls who are at risk of FGM or who have been subjected to FGM. Application can be submitted by: • The person who has had FGM or who is at risk of FGM. • A Local Authority. • Any other person with the permission of the court (for example, the police, a teacher, a charity or a family member). *It is an offence to publish any information that would likely lead to the identification of a person against whom an FGM offence is alleged to have been committed. Anonymity will commence once an allegation has been made and will last for the duration of the victim’s lifetime. Significant Harm In the case of B and G (Children) (No 2) January 2015, the President of the Family Division (Sir James Munby) concluded that all types of FGM (including Type 4) constitute “significant’’ harm
STATEMENT OPPOSING FEMALE GENITAL MUTILATION (FGM PASSPORT) • • • This Statement outlines what FGM is, the legislation and penalties involved and the help and support available. The statement is sometimes referred to as a ‘FGM/Health Passport’. The booklet is available in English but can also be obtained in the languages listed below via the following link : - Link to UK Government statement opposing female genital-mutilation This statement opposing female genital mutilation (FGM) can be taken abroad to explain the criminal status of FGM in the UK. If you know someone is in immediate danger and has been taken abroad, you should also contact the Foreign and Commonwealth Office on 020 7008 1500 or from overseas: +44 (0)20 7008 1500 17
FGM Prevalence – Who is at Risk
Summary of Factors that may increase the risk of FGM for children include: • History of FGM in family - Any girl who has a sister who has already undergone FGM must be considered to be at risk, as must other female children in the extended family. Any girl born to a woman who has been subjected to FGM may also be at risk. • Country of Prevalence (p. 6) - Pressures from community members, widespread support for FGM and high prevalence levels may increase risk to girls who are visiting their country of origin and may compromise the capacity of parents/carers to safeguard their children from FGM. Risk assessment should consider the views of the parents as well as the influence of extended family/community in the parent’s decisions concerning their children. • Cultural or religious requirement – Some families believe that FGM is integral to their child’s acceptance into their culture/community or that FGM is necessary to fulfil a religious obligation (i. e. make the child pure/clean). They may believe that if they do not perform FGM, this may result in negative consequences for the whole family (bad luck/spirit possession/ostracised). Girls born to such parents must be considered to be at risk. • Social isolation – Families from FGM practicing communities who are less integrated into UK society may be more likely to continue traditions such as FGM and have less understanding of the legal framework around FGM. It is important to note that in some countries FGM is legal and families may have the same expectation (if uninformed) of UK Law. • Education - Any girl withdrawn from Personal, Social and Health Education or Personal and Social Education may be at risk as a result of her parents wishing to keep her uninformed about her body and rights *Professionals should not assume that all women and girls from a particular community are supportive of, or at risk of FGM. See Risk Assessment - Part One (a & b) and Part Two
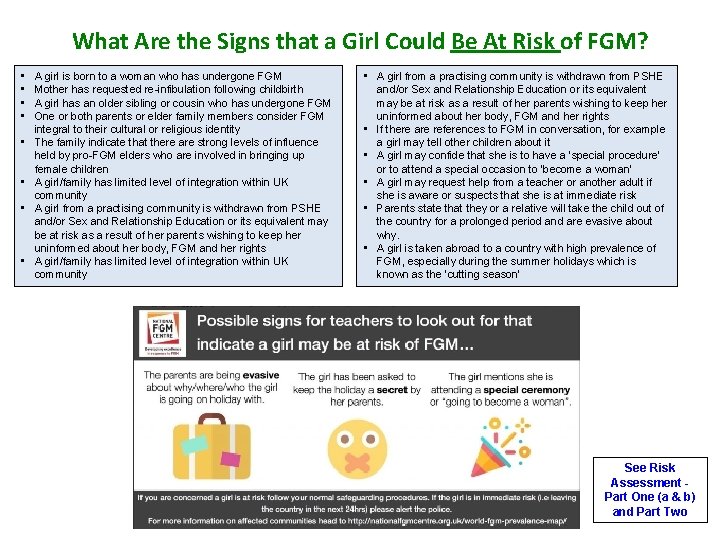
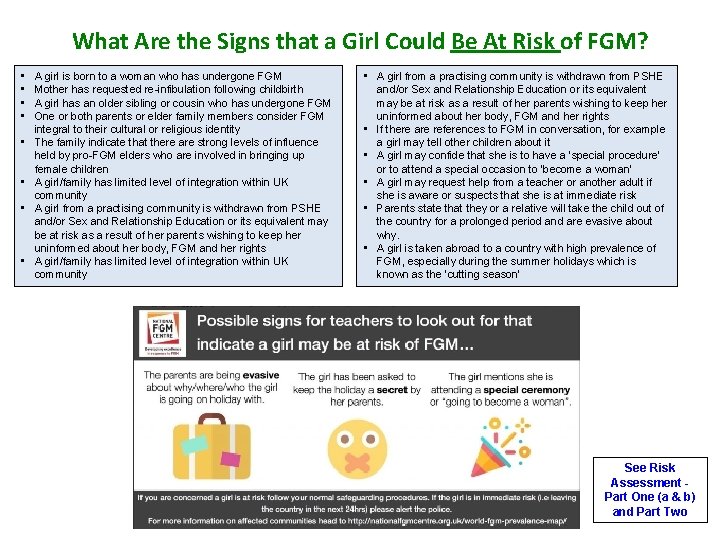
What Are the Signs that a Girl Could Be At Risk of FGM? • • A girl is born to a woman who has undergone FGM Mother has requested re-infibulation following childbirth A girl has an older sibling or cousin who has undergone FGM One or both parents or elder family members consider FGM integral to their cultural or religious identity The family indicate that there are strong levels of influence held by pro-FGM elders who are involved in bringing up female children A girl/family has limited level of integration within UK community A girl from a practising community is withdrawn from PSHE and/or Sex and Relationship Education or its equivalent may be at risk as a result of her parents wishing to keep her uninformed about her body, FGM and her rights A girl/family has limited level of integration within UK community • A girl from a practising community is withdrawn from PSHE and/or Sex and Relationship Education or its equivalent may be at risk as a result of her parents wishing to keep her uninformed about her body, FGM and her rights • If there are references to FGM in conversation, for example a girl may tell other children about it • A girl may confide that she is to have a ‘special procedure’ or to attend a special occasion to ‘become a woman’ • A girl may request help from a teacher or another adult if she is aware or suspects that she is at immediate risk • Parents state that they or a relative will take the child out of the country for a prolonged period and are evasive about why. • A girl is taken abroad to a country with high prevalence of FGM, especially during the summer holidays which is known as the ‘cutting season’ See Risk Assessment Part One (a & b) and Part Two
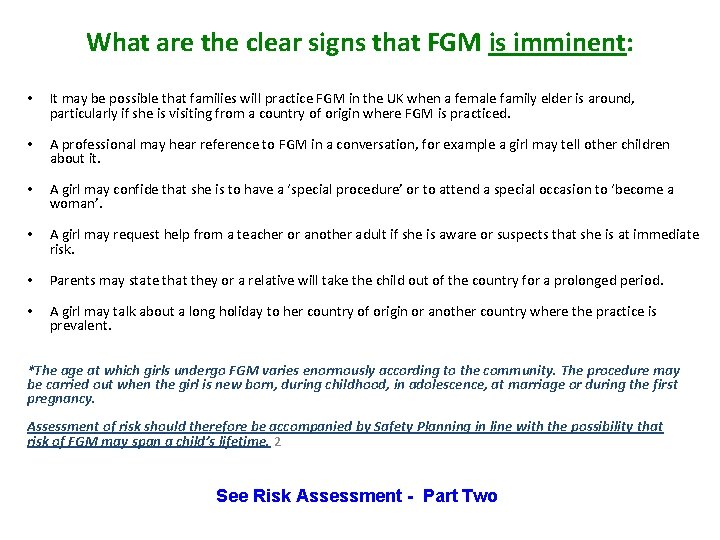
What are the clear signs that FGM is imminent: • It may be possible that families will practice FGM in the UK when a female family elder is around, particularly if she is visiting from a country of origin where FGM is practiced. • A professional may hear reference to FGM in a conversation, for example a girl may tell other children about it. • A girl may confide that she is to have a ‘special procedure’ or to attend a special occasion to ‘become a woman’. • A girl may request help from a teacher or another adult if she is aware or suspects that she is at immediate risk. • Parents may state that they or a relative will take the child out of the country for a prolonged period. • A girl may talk about a long holiday to her country of origin or another country where the practice is prevalent. *The age at which girls undergo FGM varies enormously according to the community. The procedure may be carried out when the girl is new born, during childhood, in adolescence, at marriage or during the first pregnancy. Assessment of risk should therefore be accompanied by Safety Planning in line with the possibility that risk of FGM may span a child’s lifetime. 2 See Risk Assessment - Part Two
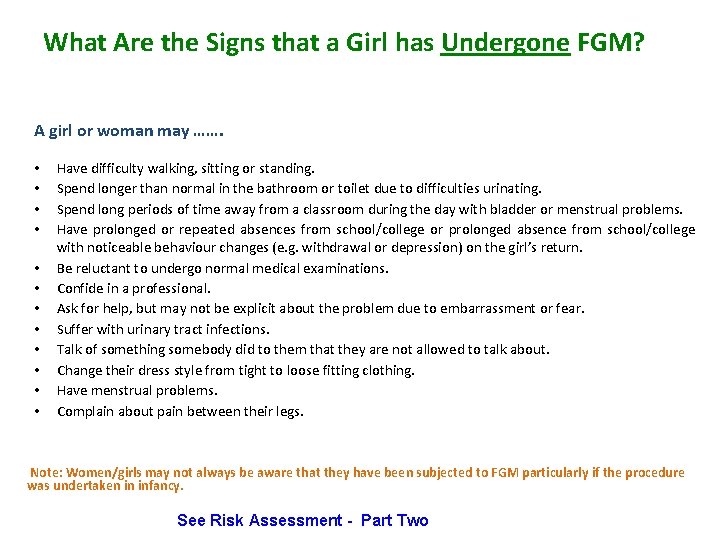
What Are the Signs that a Girl has Undergone FGM? A girl or woman may ……. • • • Have difficulty walking, sitting or standing. Spend longer than normal in the bathroom or toilet due to difficulties urinating. Spend long periods of time away from a classroom during the day with bladder or menstrual problems. Have prolonged or repeated absences from school/college or prolonged absence from school/college with noticeable behaviour changes (e. g. withdrawal or depression) on the girl’s return. Be reluctant to undergo normal medical examinations. Confide in a professional. Ask for help, but may not be explicit about the problem due to embarrassment or fear. Suffer with urinary tract infections. Talk of something somebody did to them that they are not allowed to talk about. Change their dress style from tight to loose fitting clothing. Have menstrual problems. Complain about pain between their legs. Note: Women/girls may not always be aware that they have been subjected to FGM particularly if the procedure was undertaken in infancy. See Risk Assessment - Part Two
Approaching conversations about FGM with adults and children Use language that the girl/woman understands such as genital ‘cutting’ , ‘Sunnah’, ‘Bondo’, ‘Excision’. ( Link to terminology used for FGM in other languages) Use an interpreter where required ü Ensure that you use a trained female interpreter, (preferably the same interpreter for every visit) who speaks the same language and dialect as the girl/ family. ü Do not use other family or community members to interpret. ü Inform the interpreter that you will be talking about FGM and ascertain her views on the subject to ensure she does not agree with the practice. (Be aware the interpreter may be a survivor of FGM as well. ) ü Agree on terminology used for FGM. Asking Questions: Link to examples of questions you may wish to use to guide your conversation: Complete a simple Genogram together as part of your assessment to help you understand the views of other members of the family and extended family (any assessment should always include the views of partners and fathers)
Recording Keeping You should always record clearly within your organisational records* • • • Any conversations you have and who with (verbatim record in speech marks) Any information given to you and by who Any non-verbal observations Any assessments undertaken such as FGM assessments (file any formal assessments you have undertaken in the records) Any referrals you make and to which service The outcome of any referrals Any actions you take Opinions that are within the remit of your role Any relevant pictures, drawings you make Any relevant audio or video you make anyone gives to you Anything else that you think is relevant for the child or adult *Refer to your Organisational Policy for Record Keeping.
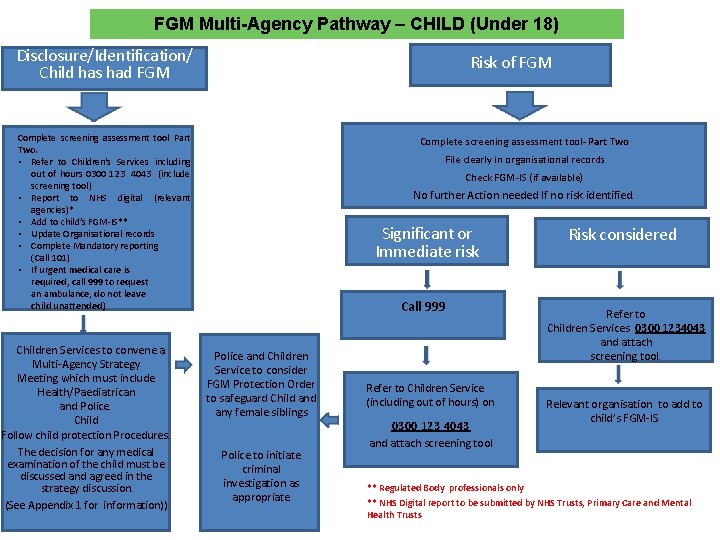
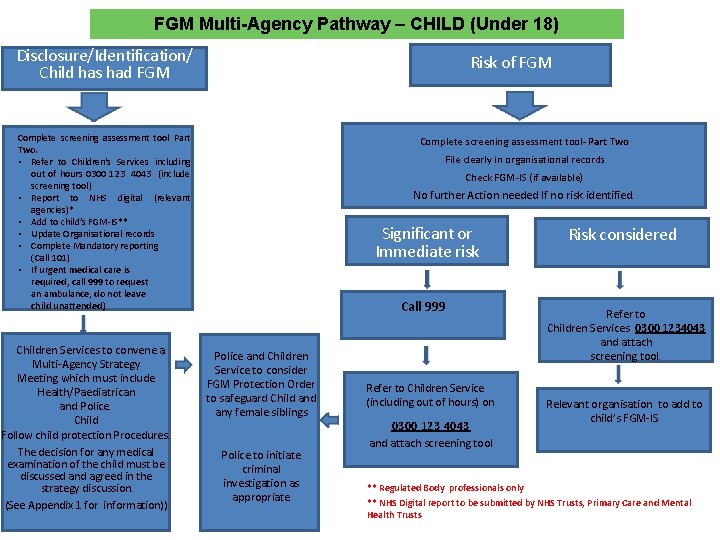
FGM Multi-Agency Pathway – CHILD (Under 18) Disclosure/Identification/ Child has had FGM Risk of FGM Complete screening assessment tool Part Two. • Refer to Children's Services including out of hours 0300 123 4043 (include screening tool) • Report to NHS digital (relevant agencies)* • Add to child’s FGM-IS** • Update Organisational records • Complete Mandatory reporting (Call 101) • If urgent medical care is required, call 999 to request an ambulance, do not leave child unattended) Children Services to convene a Multi-Agency Strategy Meeting which must include Health/Paediatrican and Police. Child Follow child protection Procedures. The decision for any medical examination of the child must be discussed and agreed in the strategy discussion. (See Appendix 1 for information)) Complete screening assessment tool- Part Two File clearly in organisational records Check FGM-IS (if available) No further Action needed If no risk identified. Significant or Immediate risk Call 999 Police and Children Service to consider FGM Protection Order to safeguard Child any female siblings Police to initiate criminal investigation as appropriate Refer to Children Service (including out of hours) on 0300 123 4043 and attach screening tool Risk considered Refer to Children Services 0300 1234043 and attach screening tool. Relevant organisation to add to child’s FGM-IS ** Regulated Body professionals only ** NHS Digital report to be submitted by NHS Trusts, Primary Care and Mental Health Trusts
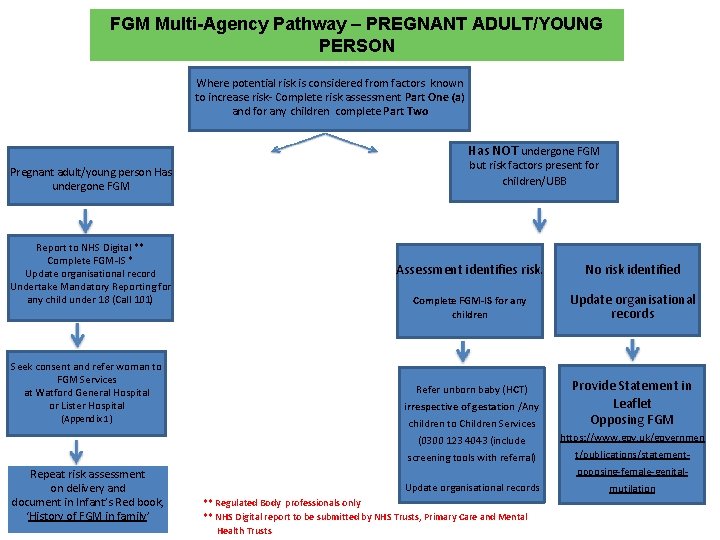
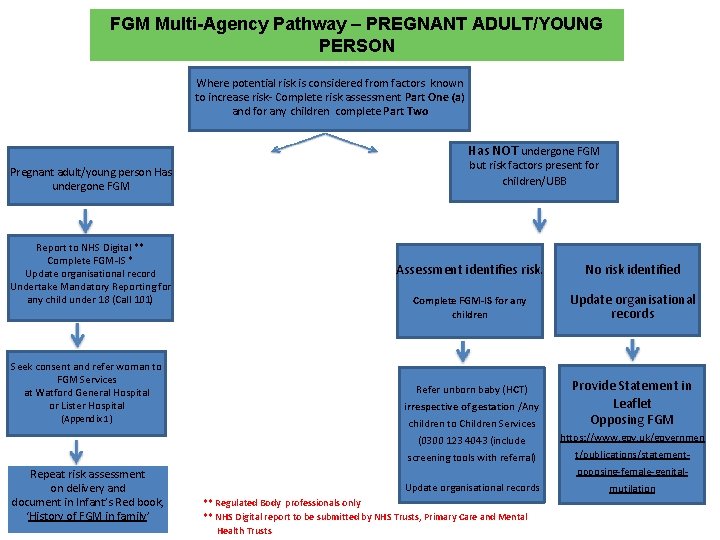
FGM Multi-Agency Pathway – PREGNANT ADULT/YOUNG PERSON Where potential risk is considered from factors known to increase risk- Complete risk assessment Part One (a) and for any children complete Part Two Has NOT undergone FGM Pregnant adult/young person Has undergone FGM Report to NHS Digital ** Complete FGM-IS * Update organisational record Undertake Mandatory Reporting for any child under 18 (Call 101) but risk factors present for children/UBB Assessment identifies risk. No risk identified Complete FGM-IS for any children Update organisational records Refer unborn baby (HCT) Seek consent and refer woman to FGM Services at Watford General Hospital or Lister Hospital irrespective of gestation /Any (Appendix 1) children to Children Services Provide Statement in Leaflet Opposing FGM (0300 123 4043 (include https: //www. gov. uk/governmen screening tools with referral) t/publications/statement- Repeat risk assessment on delivery and document in Infant’s Red book, ‘History of FGM in family’ opposing-female-genital. Update organisational records ** Regulated Body professionals only ** NHS Digital report to be submitted by NHS Trusts, Primary Care and Mental Health Trusts mutilation
FGM Multi-Agency Pathway – ADULT (NOT PREGNANT) Adult has undergone FGM Not a parent/No children
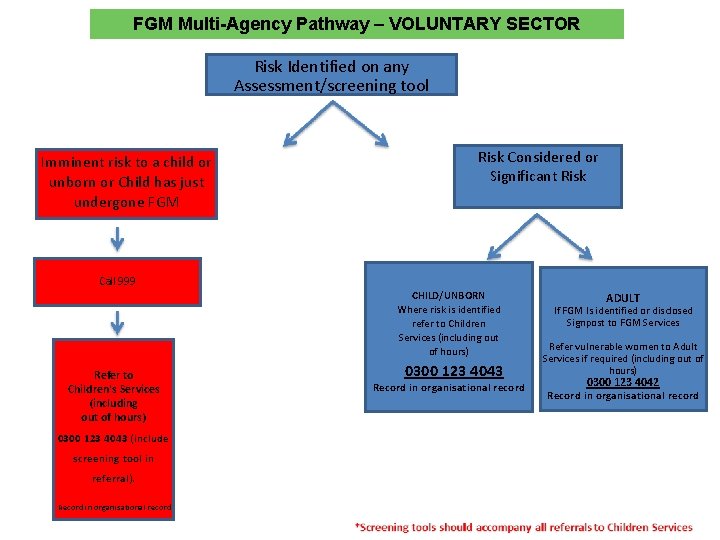
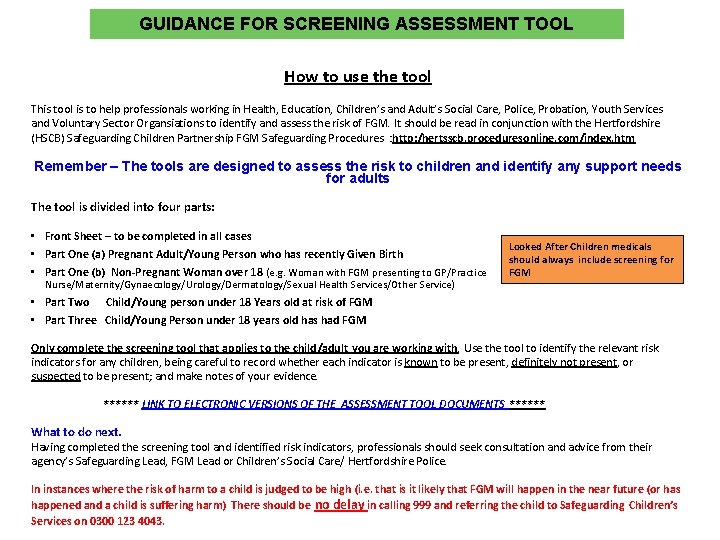
FGM Multi-Agency Pathway – VOLUNTARY SECTOR Risk Identified on any Assessment/screening tool Imminent risk to a child or unborn or Child has just undergone FGM Call 999 Refer to Children's Services (including out of hours) 0300 123 4043 (include screening tool in referral). Record in organisational record Risk Considered or Significant Risk CHILD/UNBORN Where risk is identified refer to Children Services (including out of hours) 0300 123 4043 Record in organisational record ADULT If FGM Is identified or disclosed Signpost to FGM Services Refer vulnerable women to Adult Services if required (including out of hours) 0300 123 4042 Record in organisational record
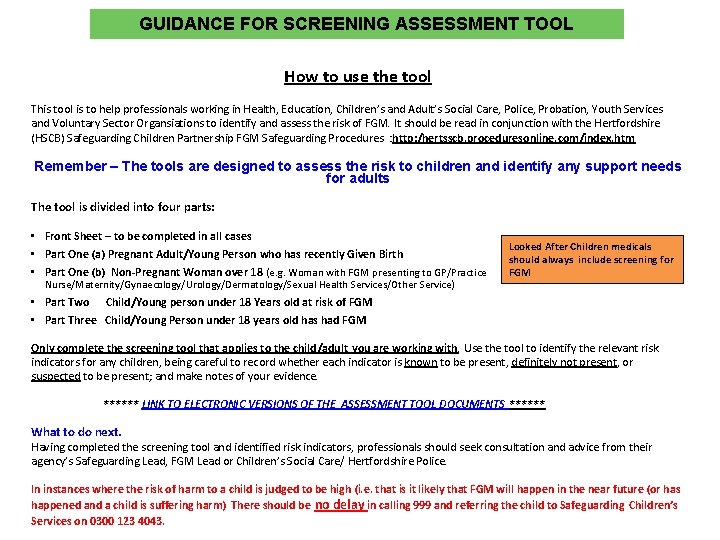
GUIDANCE FOR SCREENING ASSESSMENT TOOL How to use the tool This tool is to help professionals working in Health, Education, Children’s and Adult’s Social Care, Police, Probation, Youth Services and Voluntary Sector Organsiations to identify and assess the risk of FGM. It should be read in conjunction with the Hertfordshire (HSCB) Safeguarding Children Partnership FGM Safeguarding Procedures : http: /hertsscb. proceduresonline. com/index. htm Remember – The tools are designed to assess the risk to children and identify any support needs for adults The tool is divided into four parts: • Front Sheet – to be completed in all cases • Part One (a) Pregnant Adult/Young Person who has recently Given Birth • Part One (b) Non-Pregnant Woman over 18 (e. g. Woman with FGM presenting to GP/Practice Nurse/Maternity/Gynaecology/Urology/Dermatology/Sexual Health Services/Other Service) Looked After Children medicals should always include screening for FGM • Part Two Child/Young person under 18 Years old at risk of FGM • Part Three Child/Young Person under 18 years old has had FGM Only complete the screening tool that applies to the child/adult you are working with. Use the tool to identify the relevant risk indicators for any children, being careful to record whether each indicator is known to be present, definitely not present, or suspected to be present; and make notes of your evidence. ****** LINK TO ELECTRONIC VERSIONS OF THE ASSESSMENT TOOL DOCUMENTS ****** What to do next. Having completed the screening tool and identified risk indicators, professionals should seek consultation and advice from their agency’s Safeguarding Lead, FGM Lead or Children’s Social Care/ Hertfordshire Police. In instances where the risk of harm to a child is judged to be high (i. e. that is it likely that FGM will happen in the near future (or has happened and a child is suffering harm) There should be no delay in calling 999 and referring the child to Safeguarding Children’s Services on 0300 123 4043.
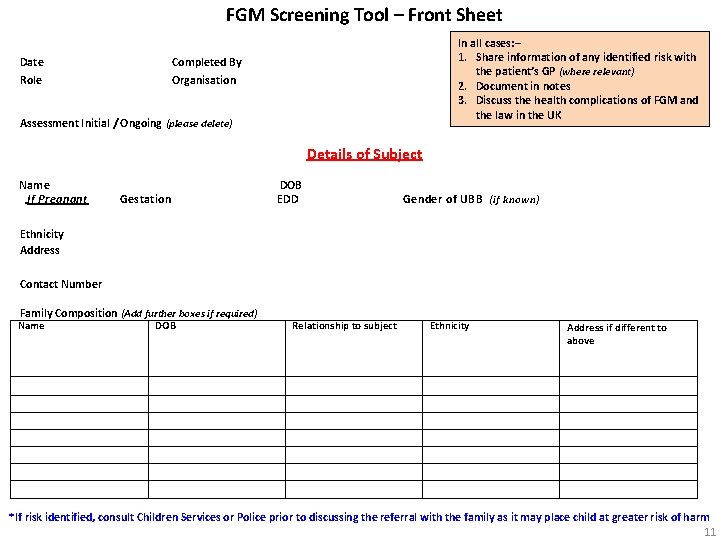
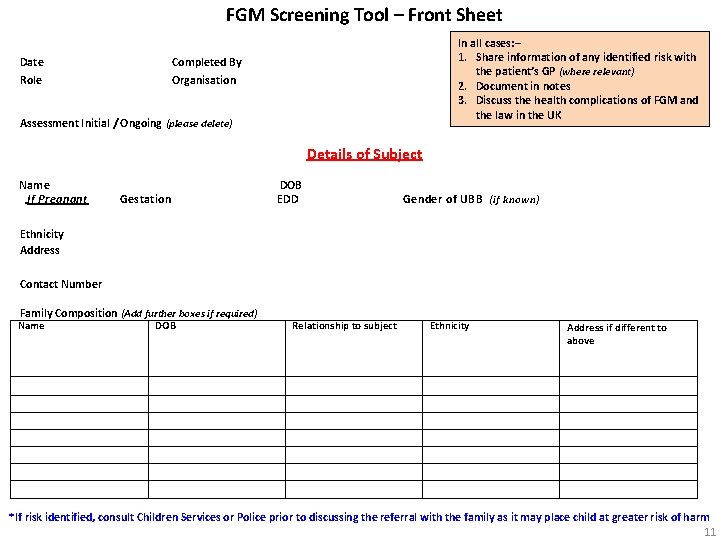
FGM Screening Tool – Front Sheet Date Role In all cases: – 1. Share information of any identified risk with the patient’s GP (where relevant) 2. Document in notes 3. Discuss the health complications of FGM and the law in the UK Completed By Organisation Assessment Initial / Ongoing (please delete) Details of Subject Name If Pregnant Gestation DOB EDD Gender of UBB (if known) Ethnicity Address Contact Number Family Composition (Add further boxes if required) Name DOB Relationship to subject Ethnicity Address if different to above *If risk identified, consult Children Services or Police prior to discussing the referral with the family as it may place child at greater risk of harm 11
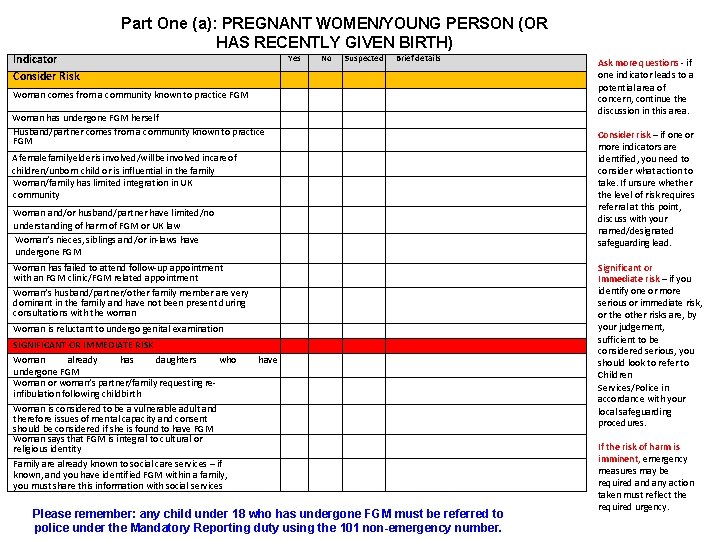
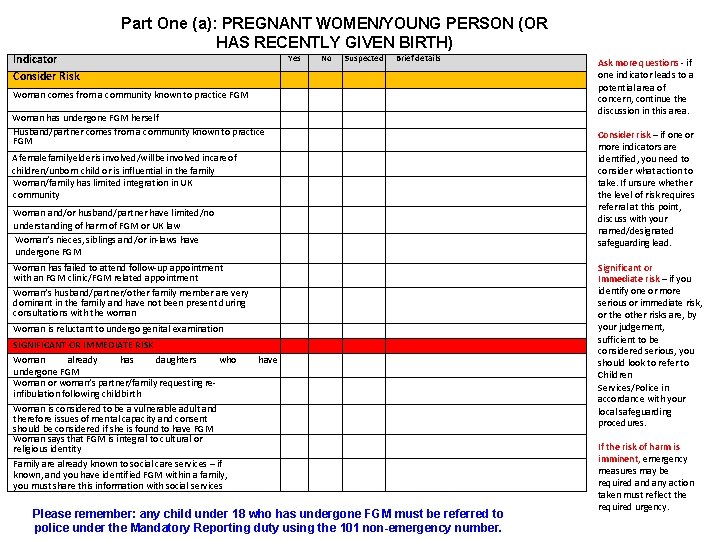
Part One (a): PREGNANT WOMEN/YOUNG PERSON (OR HAS RECENTLY GIVEN BIRTH) Indicator Consider Risk Yes No Suspected Brief details Woman comes from a community known to practice FGM Woman has undergone FGM herself Husband/partner comes from a community known to practice FGM A female family elder is involved/will be involved in care of children/unborn child or is influential in the family Woman/family has limited integration in UK community Woman and/or husband/partner have limited/no understanding of harm of FGM or UK law Woman’s nieces, siblings and/or in-laws have undergone FGM Woman has failed to attend follow-up appointment with an FGM clinic/FGM related appointment Woman’s husband/partner/other family member are very dominant in the family and have not been present during consultations with the woman Woman is reluctant to undergo genital examination SIGNIFICANT OR IMMEDIATE RISK Woman already has daughters who undergone FGM Woman or woman’s partner/family requesting reinfibulation following childbirth Woman is considered to be a vulnerable adult and therefore issues of mental capacity and consent should be considered if she is found to have FGM Woman says that FGM is integral to cultural or religious identity have Family are already known to social care services – if known, and you have identified FGM within a family, you must share this information with social services Please remember: any child under 18 who has undergone FGM must be referred to police under the Mandatory Reporting duty using the 101 non-emergency number. Ask more questions - if one indicator leads to a potential area of concern, continue the discussion in this area. Consider risk – if one or more indicators are identified, you need to consider what action to take. If unsure whether the level of risk requires referral at this point, discuss with your named/designated safeguarding lead. Significant or Immediate risk – if you identify one or more serious or immediate risk, or the other risks are, by your judgement, sufficient to be considered serious, you should look to refer to Children Services/Police in accordance with your local safeguarding procedures. If the risk of harm is imminent, emergency measures may be required any action taken must reflect the required urgency.
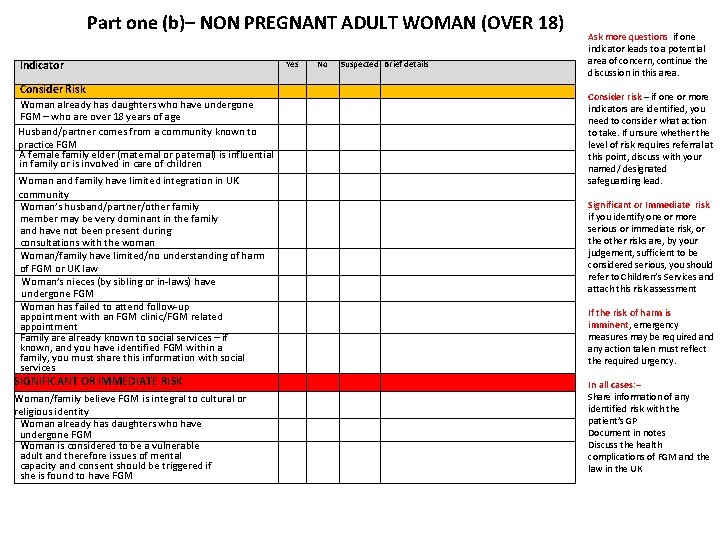
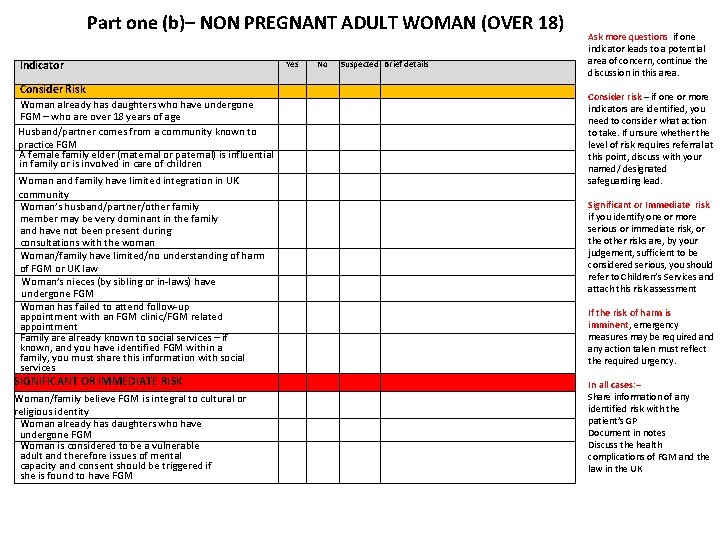
Part one (b)– NON PREGNANT ADULT WOMAN (OVER 18) Indicator Consider Risk Woman already has daughters who have undergone FGM – who are over 18 years of age Husband/partner comes from a community known to practice FGM A female family elder (maternal or paternal) is influential in family or is involved in care of children Woman and family have limited integration in UK community Woman’s husband/partner/other family member may be very dominant in the family and have not been present during consultations with the woman Woman/family have limited/no understanding of harm of FGM or UK law Woman’s nieces (by sibling or in-laws) have undergone FGM Woman has failed to attend follow-up appointment with an FGM clinic/FGM related appointment Family are already known to social services – if known, and you have identified FGM within a family, you must share this information with social services SIGNIFICANT OR IMMEDIATE RISK Woman/family believe FGM is integral to cultural or religious identity Woman already has daughters who have undergone FGM Woman is considered to be a vulnerable adult and therefore issues of mental capacity and consent should be triggered if she is found to have FGM Yes No Suspected Brief details Ask more questions if one indicator leads to a potential area of concern, continue the discussion in this area. Consider risk – if one or more indicators are identified, you need to consider what action to take. If unsure whether the level of risk requires referral at this point, discuss with your named/ designated safeguarding lead. Significant or Immediate risk if you identify one or more serious or immediate risk, or the other risks are, by your judgement, sufficient to be considered serious, you should refer to Children’s Services and attach this risk assessment If the risk of harm is imminent, emergency measures may be required any action taken must reflect the required urgency. In all cases: – Share information of any identified risk with the patient’s GP Document in notes Discuss the health complications of FGM and the law in the UK
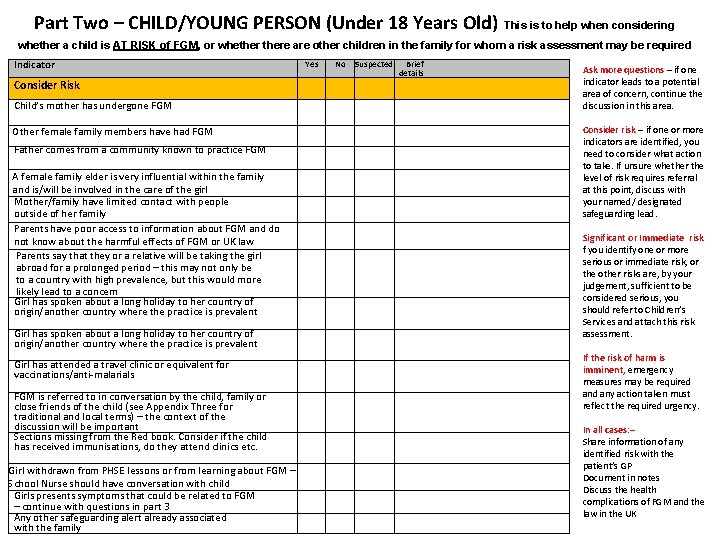
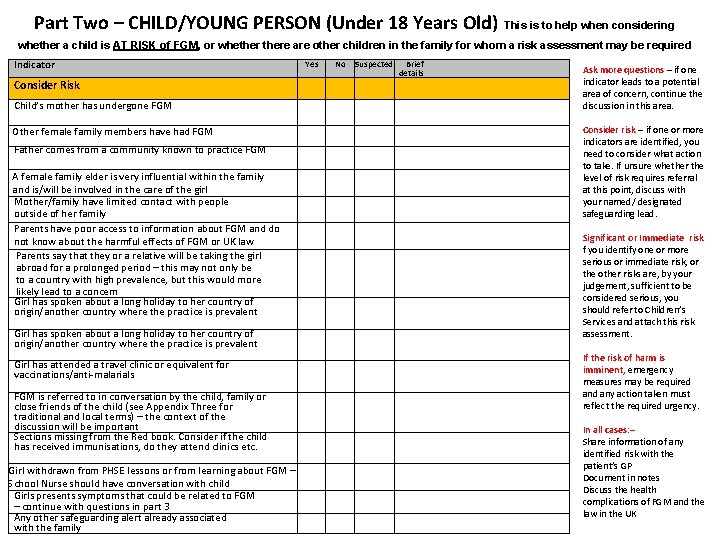
Part Two – CHILD/YOUNG PERSON (Under 18 Years Old) This is to help when considering whether a child is AT RISK of FGM, or whethere are other children in the family for whom a risk assessment may be required Indicator Consider Risk Child’s mother has undergone FGM Other female family members have had FGM Father comes from a community known to practice FGM A female family elder is very influential within the family and is/will be involved in the care of the girl Mother/family have limited contact with people outside of her family Parents have poor access to information about FGM and do not know about the harmful effects of FGM or UK law Parents say that they or a relative will be taking the girl abroad for a prolonged period – this may not only be to a country with high prevalence, but this would more likely lead to a concern Girl has spoken about a long holiday to her country of origin/another country where the practice is prevalent Girl has attended a travel clinic or equivalent for vaccinations/anti-malarials FGM is referred to in conversation by the child, family or close friends of the child (see Appendix Three for traditional and local terms) – the context of the discussion will be important Sections missing from the Red book. Consider if the child has received immunisations, do they attend clinics etc. Girl withdrawn from PHSE lessons or from learning about FGM – School Nurse should have conversation with child Girls presents symptoms that could be related to FGM – continue with questions in part 3 Any other safeguarding alert already associated with the family Yes No Suspected Brief details Ask more questions – if one indicator leads to a potential area of concern, continue the discussion in this area. Consider risk – if one or more indicators are identified, you need to consider what action to take. If unsure whether the level of risk requires referral at this point, discuss with your named/ designated safeguarding lead. Significant or Immediate risk f you identify one or more serious or immediate risk, or the other risks are, by your judgement, sufficient to be considered serious, you should refer to Children’s Services and attach this risk assessment. If the risk of harm is imminent, emergency measures may be required any action taken must reflect the required urgency. In all cases: – Share information of any identified risk with the patient’s GP Document in notes Discuss the health complications of FGM and the law in the UK
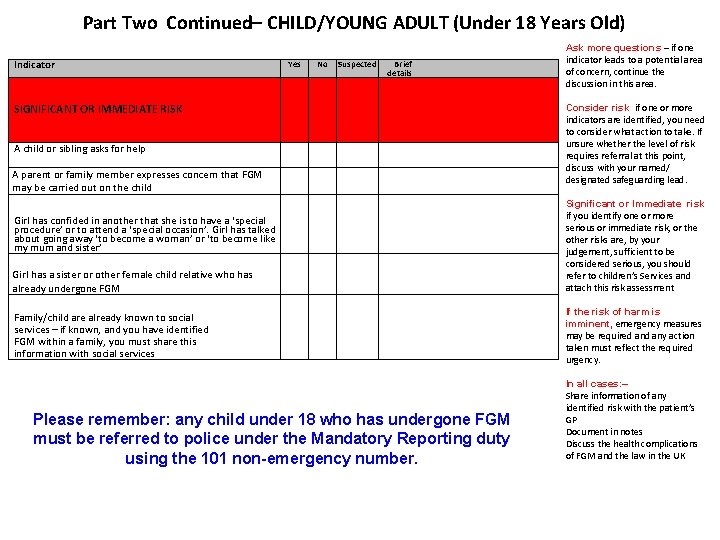
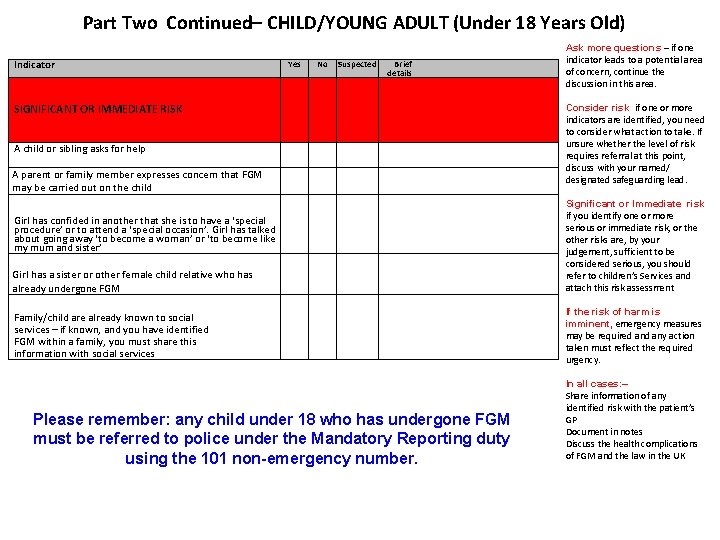
Part Two Continued– CHILD/YOUNG ADULT (Under 18 Years Old) Indicator Yes No Suspected Brief details SIGNIFICANT OR IMMEDIATE RISK A child or sibling asks for help A parent or family member expresses concern that FGM may be carried out on the child Girl has confided in another that she is to have a ‘special procedure’ or to attend a ‘special occasion’. Girl has talked about going away ‘to become a woman’ or ‘to become like my mum and sister’ Girl has a sister or other female child relative who has already undergone FGM Family/child are already known to social services – if known, and you have identified FGM within a family, you must share this information with social services Please remember: any child under 18 who has undergone FGM must be referred to police under the Mandatory Reporting duty using the 101 non-emergency number. Ask more questions – if one indicator leads to a potential area of concern, continue the discussion in this area. Consider risk if one or more indicators are identified, you need to consider what action to take. If unsure whether the level of risk requires referral at this point, discuss with your named/ designated safeguarding lead. Significant or Immediate risk if you identify one or more serious or immediate risk, or the other risks are, by your judgement, sufficient to be considered serious, you should refer to children’s Services and attach this risk assessment If the risk of harm is imminent, emergency measures may be required any action taken must reflect the required urgency. In all cases: – Share information of any identified risk with the patient’s GP Document in notes Discuss the health complications of FGM and the law in the UK
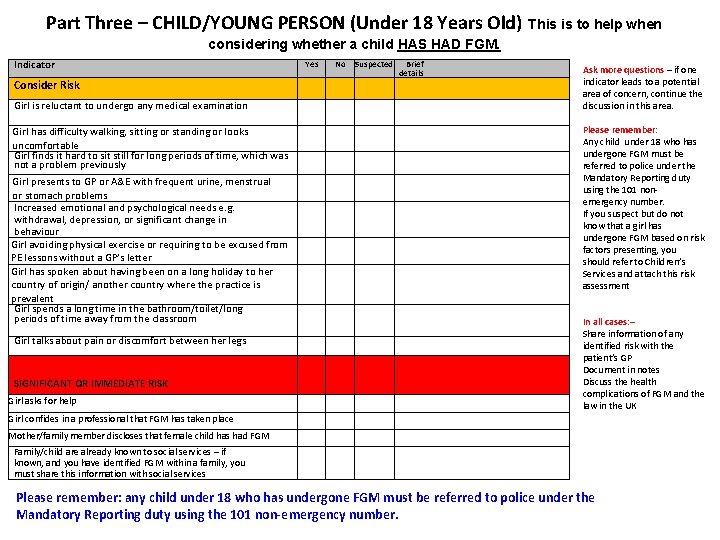
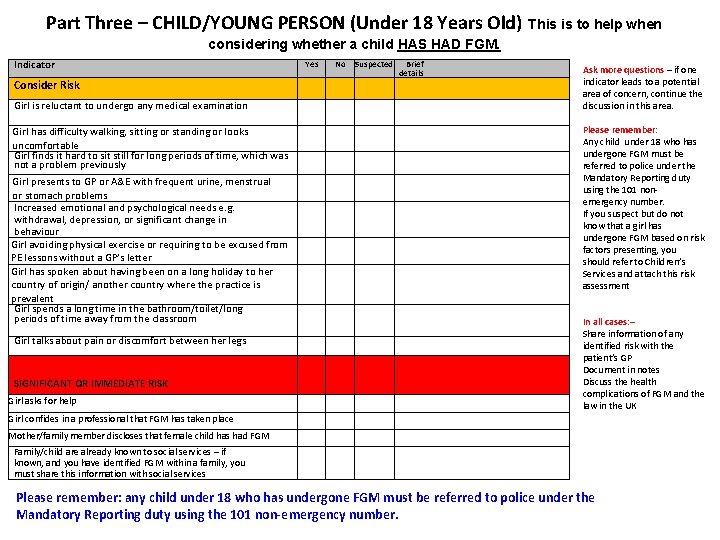
Part Three – CHILD/YOUNG PERSON (Under 18 Years Old) This is to help when considering whether a child HAS HAD FGM. Indicator Consider Risk Girl is reluctant to undergo any medical examination Girl has difficulty walking, sitting or standing or looks uncomfortable Girl finds it hard to sit still for long periods of time, which was not a problem previously Girl presents to GP or A&E with frequent urine, menstrual or stomach problems Increased emotional and psychological needs e. g. withdrawal, depression, or significant change in behaviour Girl avoiding physical exercise or requiring to be excused from PE lessons without a GP’s letter Girl has spoken about having been on a long holiday to her country of origin/ another country where the practice is prevalent Girl spends a long time in the bathroom/toilet/long periods of time away from the classroom Girl talks about pain or discomfort between her legs SIGNIFICANT OR IMMEDIATE RISK Girl asks for help Yes No Suspected Brief details Ask more questions – if one indicator leads to a potential area of concern, continue the discussion in this area. Please remember: Any child under 18 who has undergone FGM must be referred to police under the Mandatory Reporting duty using the 101 nonemergency number. If you suspect but do not know that a girl has undergone FGM based on risk factors presenting, you should refer to Children’s Services and attach this risk assessment In all cases: – Share information of any identified risk with the patient’s GP Document in notes Discuss the health complications of FGM and the law in the UK Girl confides in a professional that FGM has taken place Mother/family member discloses that female child has had FGM Family/child are already known to social services – if known, and you have identified FGM within a family, you must share this information with social services Please remember: any child under 18 who has undergone FGM must be referred to police under the Mandatory Reporting duty using the 101 non-emergency number.
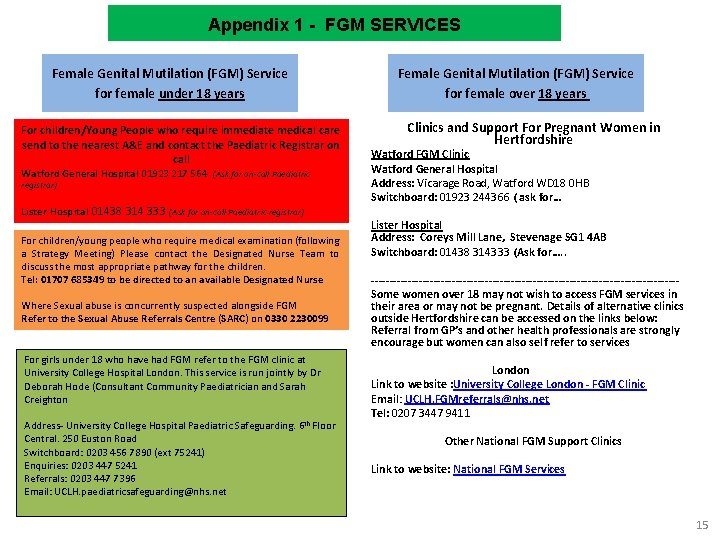
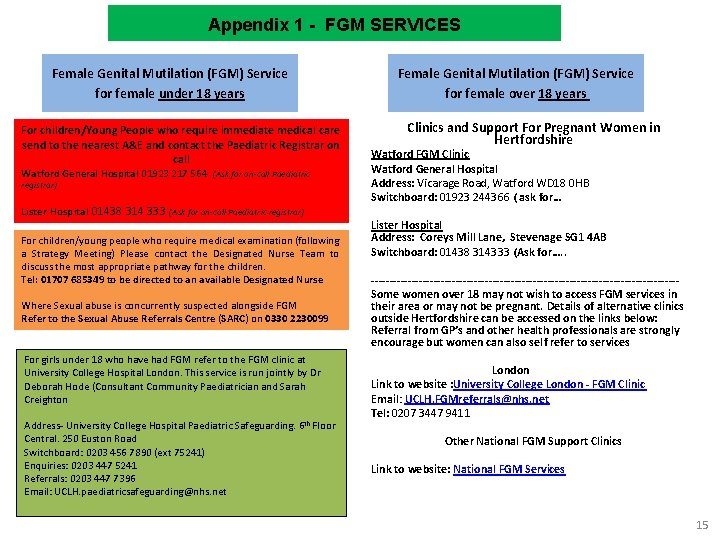
Appendix 1 4 - -FGM FGMSERVICES Services Appendix Female Genital Mutilation (FGM) Service for female under 18 years For children/Young People who require immediate medical care send to the nearest A&E and contact the Paediatric Registrar on call Watford General Hospital 01923 217 564 (Ask for on-call Paediatric registrar) Female Genital Mutilation (FGM) Service for female over 18 years Clinics and Support For Pregnant Women in Hertfordshire Watford FGM Clinic Watford General Hospital Address: Vicarage Road, Watford WD 18 0 HB Switchboard: 01923 244366 ( ask for… (ask Lister Hospital 01438 314 333 (Ask for on-call Paediatric registrar) For children/young people who require medical examination (following a Strategy Meeting) Please contact the Designated Nurse Team to discuss the most appropriate pathway for the children. Tel: 01707 685349 to be directed to an available Designated Nurse Where Sexual abuse is concurrently suspected alongside FGM Refer to the Sexual Abuse Referrals Centre (SARC) on 0330 2230099 For girls under 18 who have had FGM refer to the FGM clinic at University College Hospital London. This service is run jointly by Dr Deborah Hode (Consultant Community Paediatrician and Sarah Creighton Address- University College Hospital Paediatric Safeguarding. 6 th Floor Central. 250 Euston Road Switchboard: 0203 456 7890 (ext 75241) Enquiries: 0203 447 5241 Referrals: 0203 447 7396 Email: UCLH. paediatricsafeguarding@nhs. net Lister Hospital Address: Coreys Mill Lane, Stevenage SG 1 4 AB Switchboard: 01438 314333 (Ask for…. . ------------------------------------------Some women over 18 may not wish to access FGM services in their area or may not be pregnant. Details of alternative clinics outside Hertfordshire can be accessed on the links below: Referral from GP’s and other health professionals are strongly encourage but women can also self refer to services London Link to website : University College London - FGM Clinic Email: UCLH. FGMreferrals@nhs. net Tel: 0207 3447 9411 Other National FGM Support Clinics Link to website: National FGM Services 15
![References World Health Organisation Female genital mutilation Fact sheet Updated February 2020 HM Government References World Health Organisation: Female genital mutilation Fact sheet: [Updated February 2020] HM Government](https://slidetodoc.com/presentation_image_h2/b48b09da1aa1ccd6d4556ed57b5bd98e/image-25.jpg)
References World Health Organisation: Female genital mutilation Fact sheet: [Updated February 2020] HM Government (2020): Multi Agency Statutory Guidance on Female Genital Mutilation. Department of Health and Social Care (2017) Female Genital Mutilation risk and safeguarding: Guidance for professionals Department of Health and Social Care (2017) FGM safeguarding and Risk Assessment: Guidance for Health professionals Department of Health: FGM Risk assessment Templates Ministry of Justice/Home Office (March 2015) Serious Crime Act 2015 Factsheet – Female Genital Mutilation Department for Education/Home Office: Mandatory reporting of female genital mutilation [Updated 22. Jan 2020] SIR JAMES MUNBY PRESIDENT OF THE FAMILY DIVISION: In the matter of B and G (Children) (No 2) 14 th January 2015 Case No: LJ 13 C 00295 HM Government (2016) Statement Opposing Female Genital Mutilation 18
Authors: Amanda Merrett-Jones (Herts Valleys & East and North Hertfordshire Clinical Commissioning Groups) Treena Beard (Herts Valley & East and North Hertfordshire Commission Groups) Tawanda Bvumburai (West Herts Hospitals Trust) Contributions: Emma Bell (Named Midwife. East and North Herts Trust) Nicky Cottier (Named Nurse. Central London Healthcare Trust) Jane Domogal (Safeguarding Nurse Specialist. Hertfordshire Community NSH Trust) Teresa Drakes (Named Midwife. East and North Herts Trust) Keiley Perry (Named Midwife West Herts Hospitals Trust) Nicky Velacott (Named Nurse Central London health Care Trust) Hertfordshire Safeguarding Children's’ Services Partners Acknowledgments: National Centre for FGM http: //nationalfgmcentre. org. uk/ Hertfordshire Multi-Agency Partnership working Group. Version 1 (2016) 19