Hereditary Angioedema Diagnosis and Therapeutic Interventions Alexander L




- Slides: 70
Hereditary Angioedema: Diagnosis and Therapeutic Interventions Alexander L. Ramirez, M. D. Chief, Otolaryngology Mc. Kay Dee Hospital
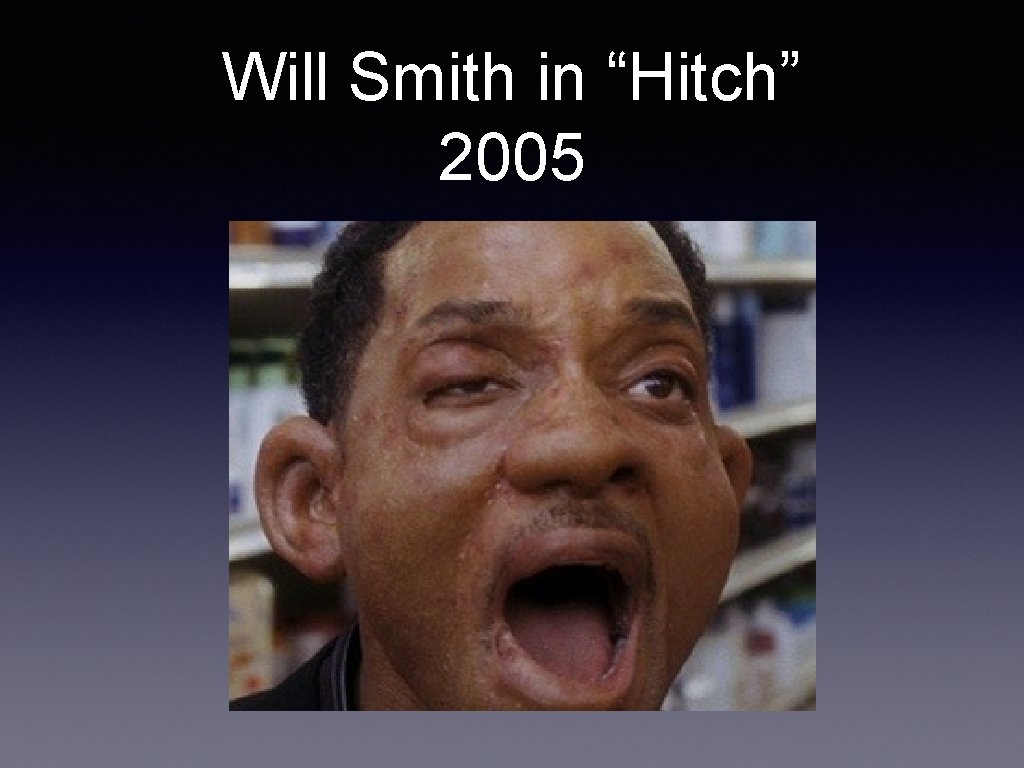
Will Smith in “Hitch” 2005
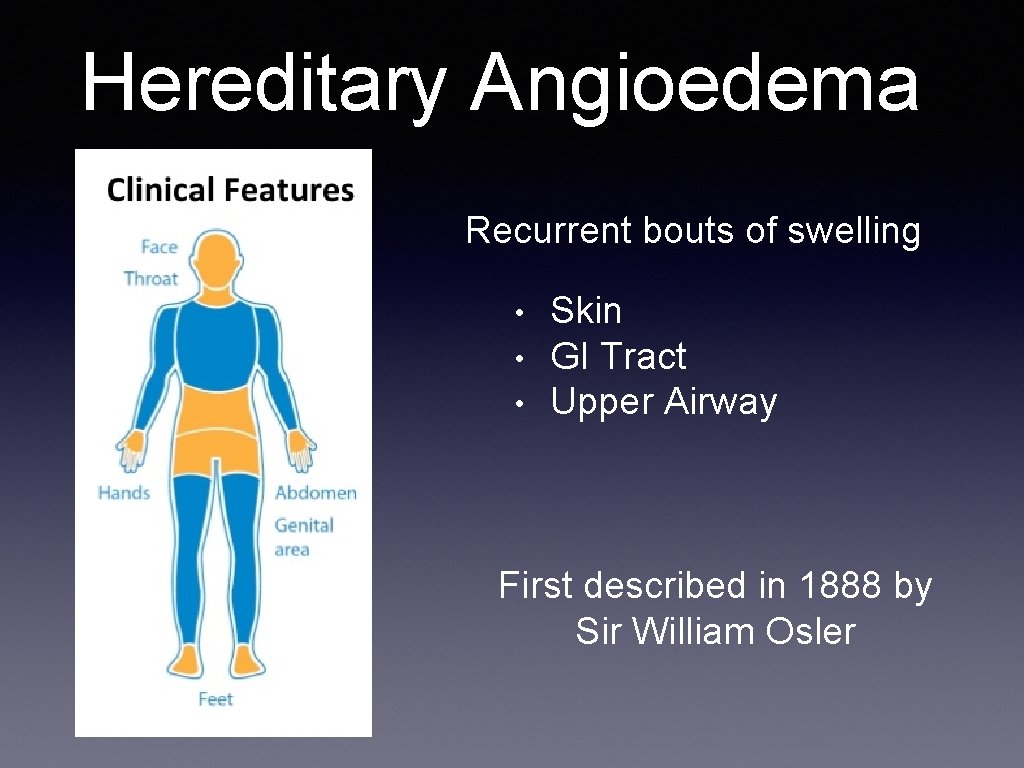
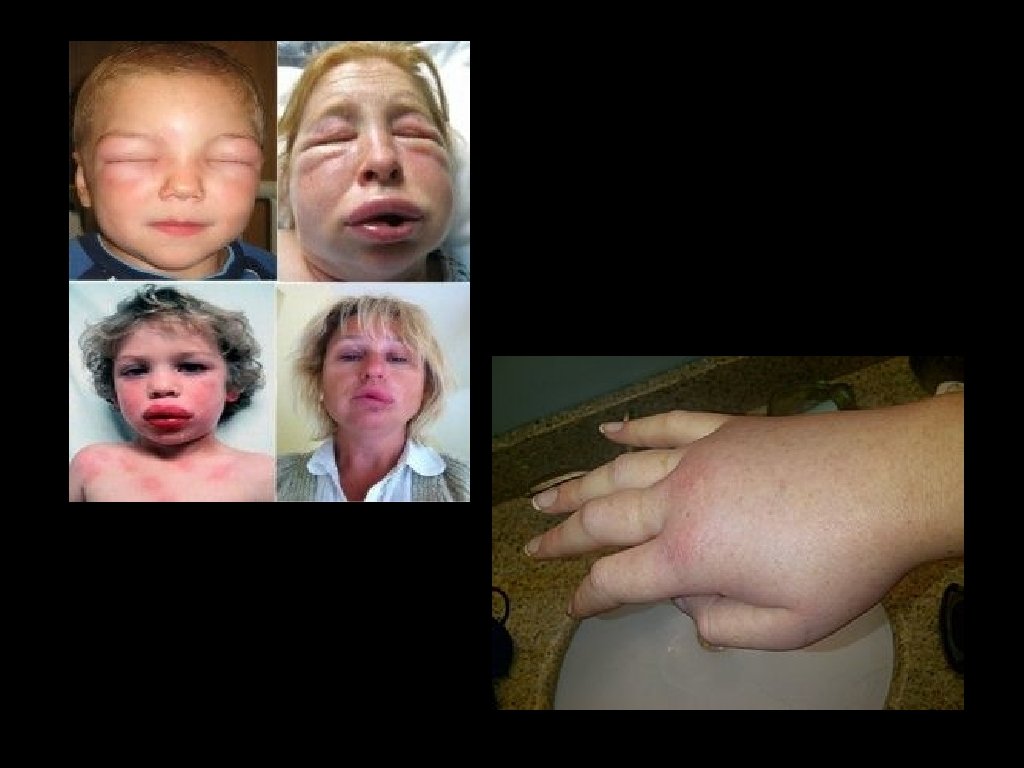
Introduction • Recurrent episodes of angioedema WITHOUT urticaria or pruritus • Skin or mucosal tissue (Upper airway or GI) • Self limited, but if larynx involved risk of fatal asphyxiation • Mortality was 30% prior to treatments available now
UFC Fight

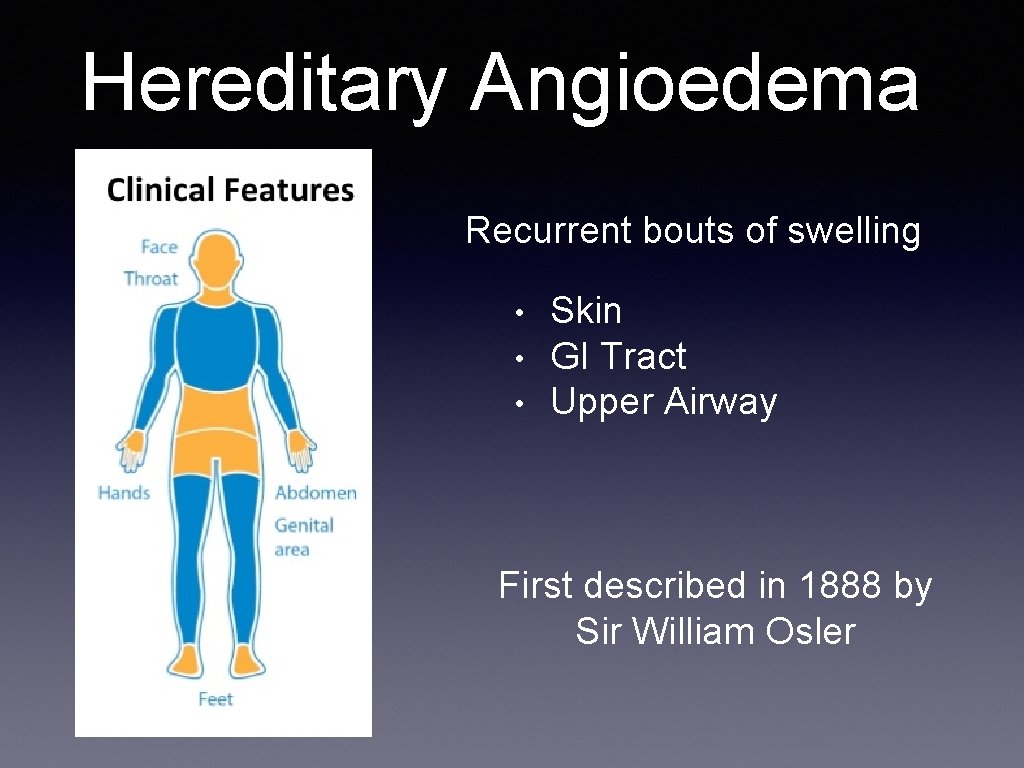
Hereditary Angioedema Recurrent bouts of swelling • • • Skin GI Tract Upper Airway First described in 1888 by Sir William Osler
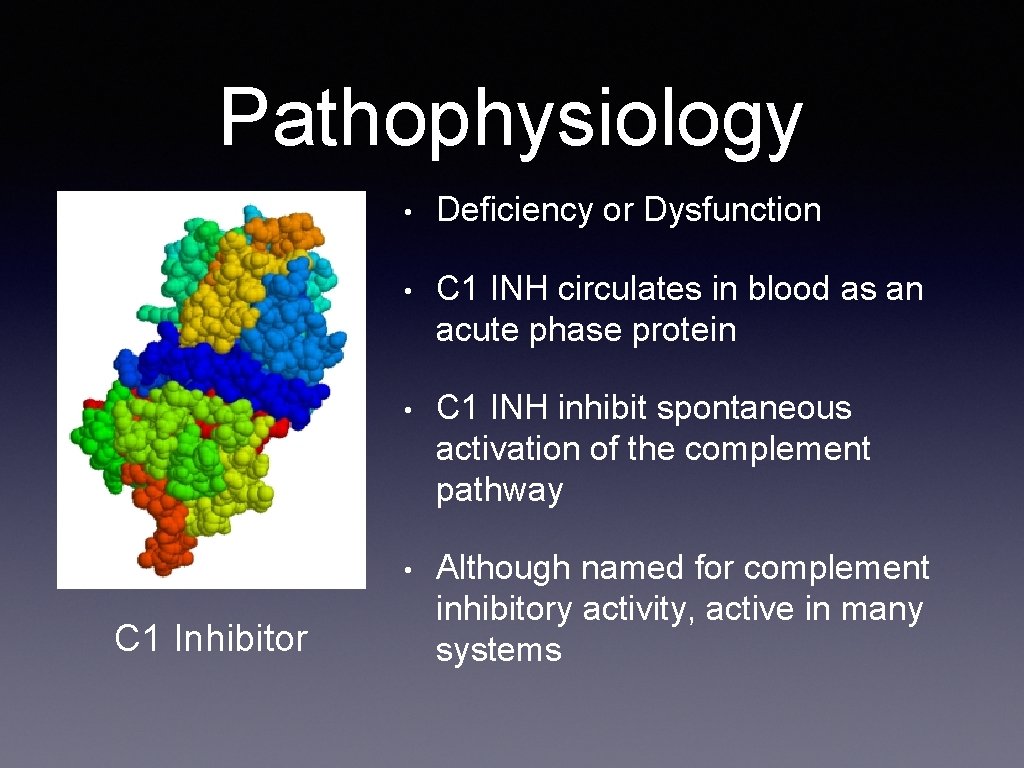
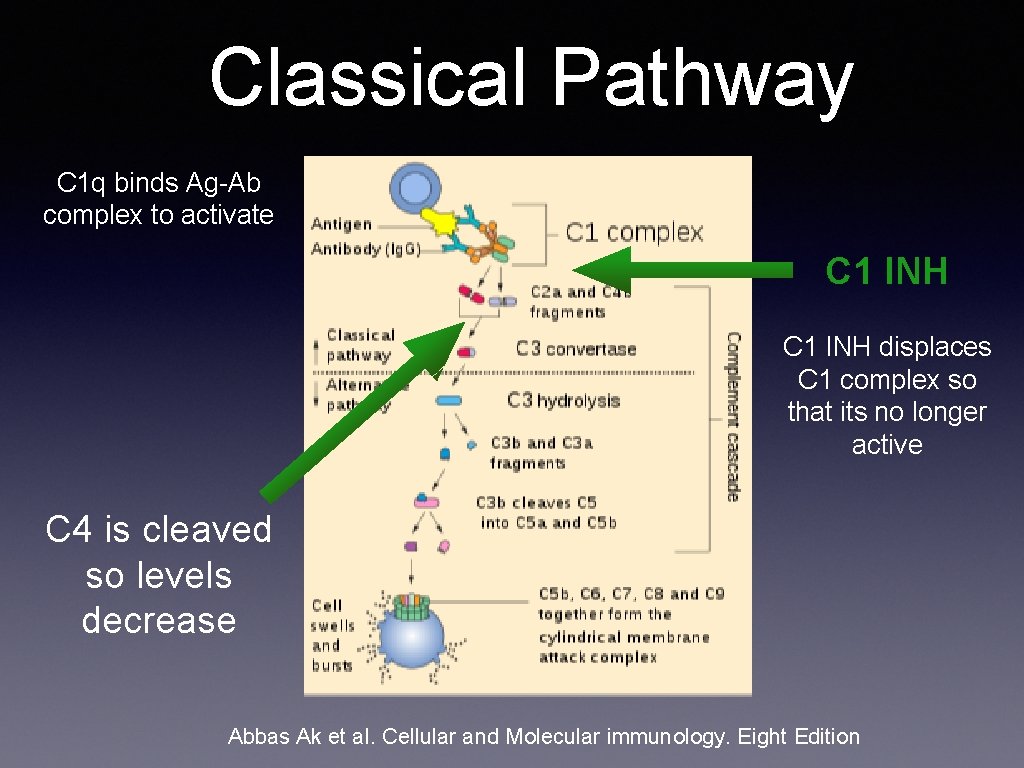
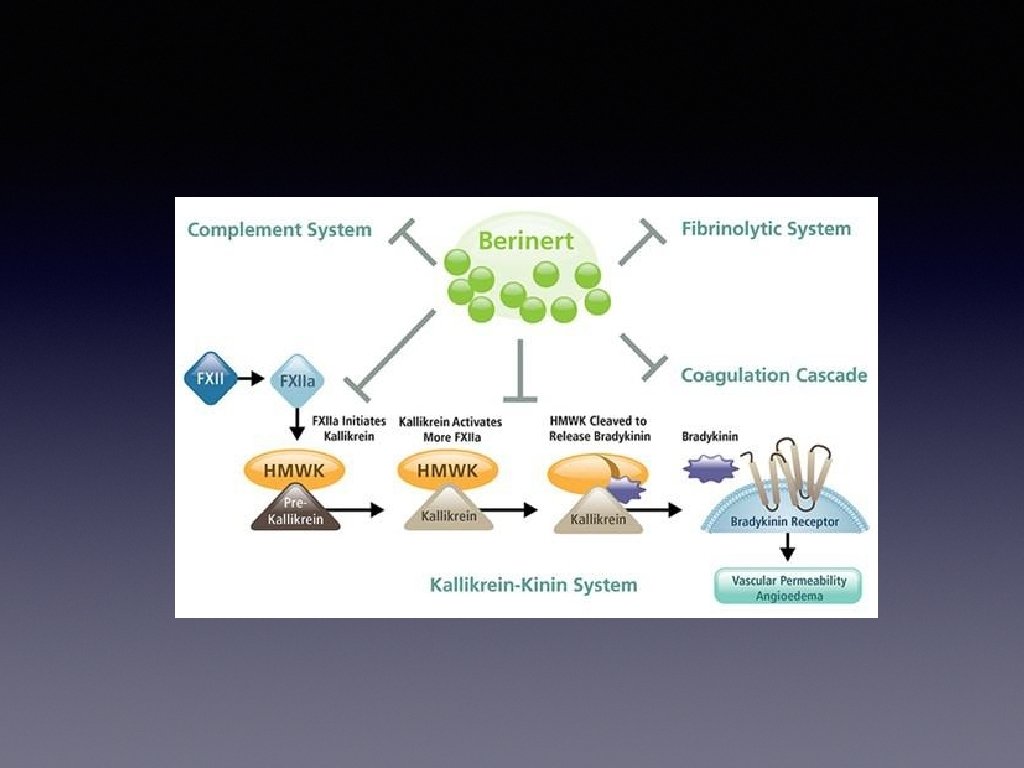
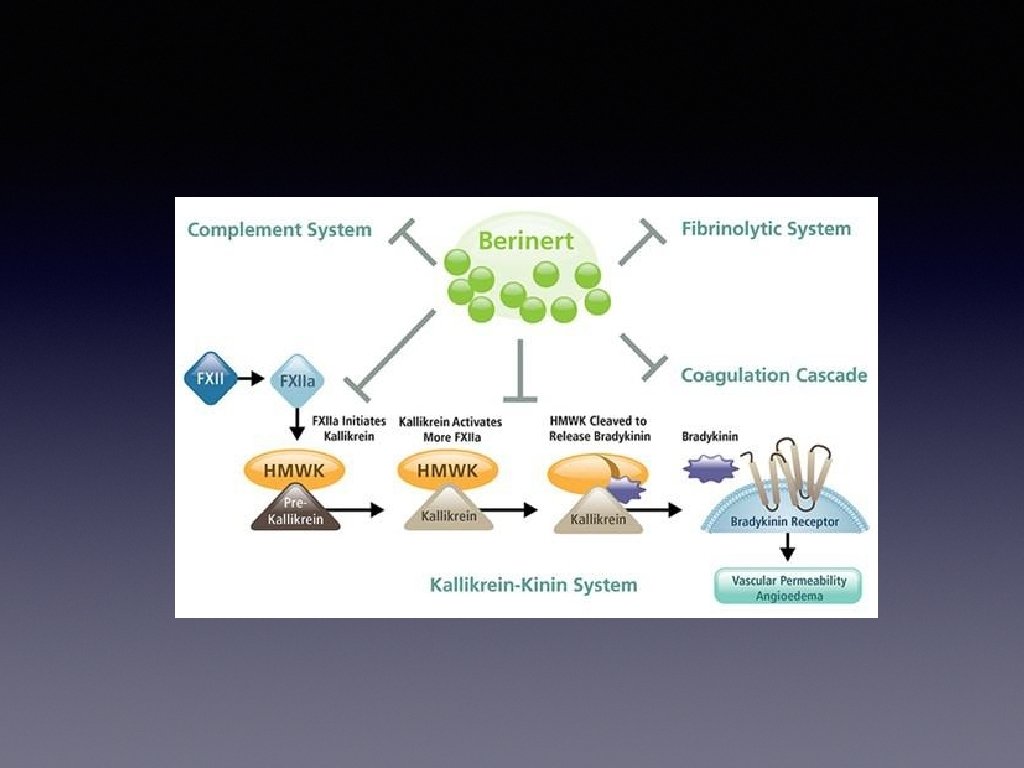
Pathophysiology C 1 Inhibitor • Deficiency or Dysfunction • C 1 INH circulates in blood as an acute phase protein • C 1 INH inhibit spontaneous activation of the complement pathway • Although named for complement inhibitory activity, active in many systems
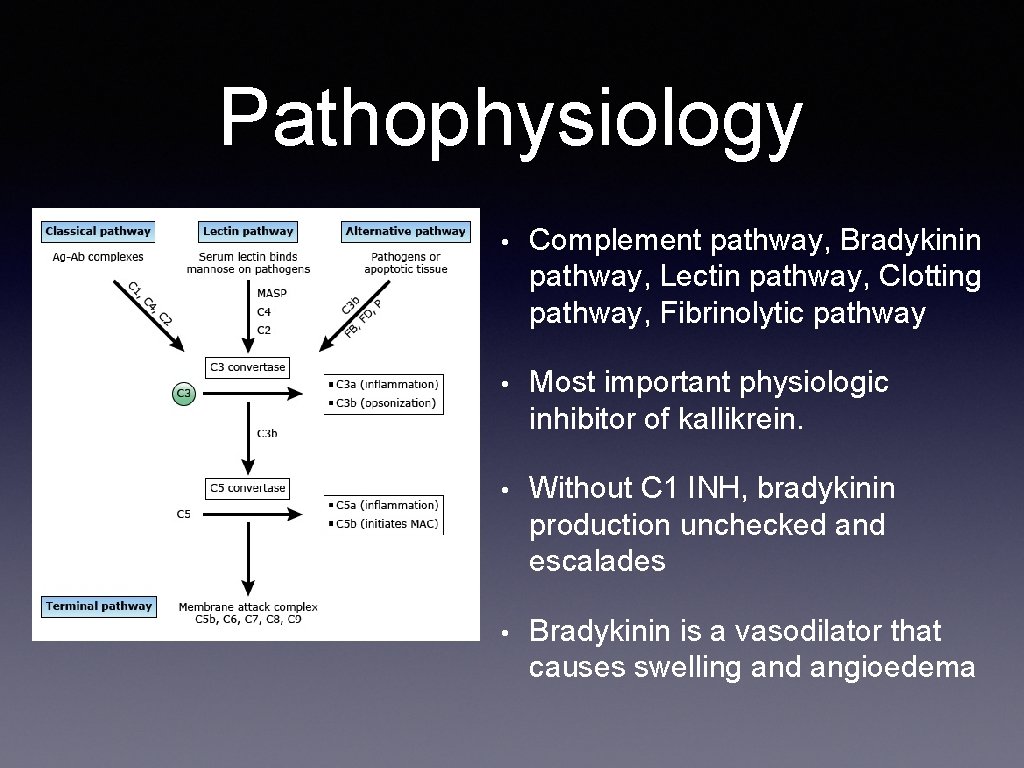
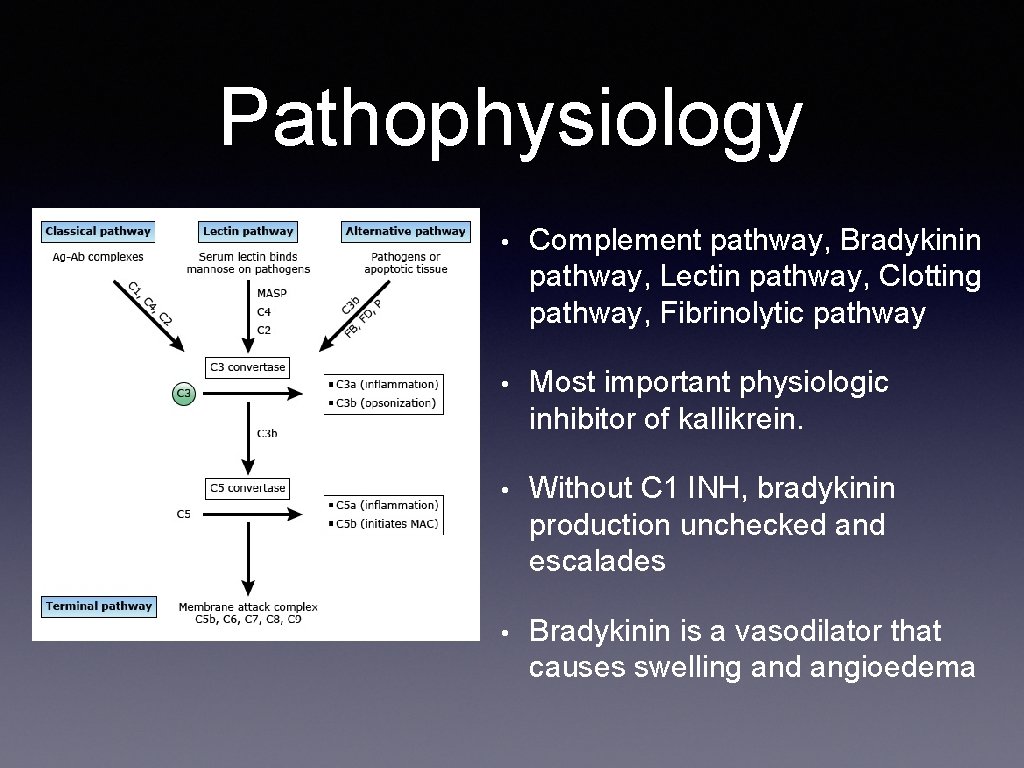
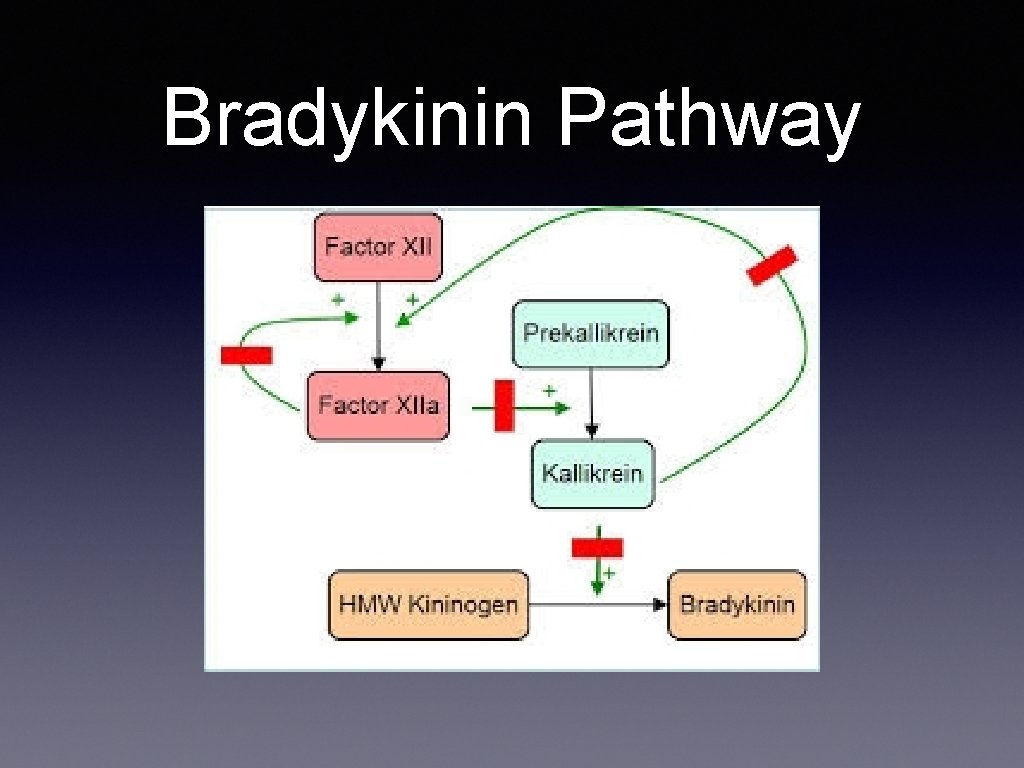
Pathophysiology • Complement pathway, Bradykinin pathway, Lectin pathway, Clotting pathway, Fibrinolytic pathway • Most important physiologic inhibitor of kallikrein. • Without C 1 INH, bradykinin production unchecked and escalades • Bradykinin is a vasodilator that causes swelling and angioedema
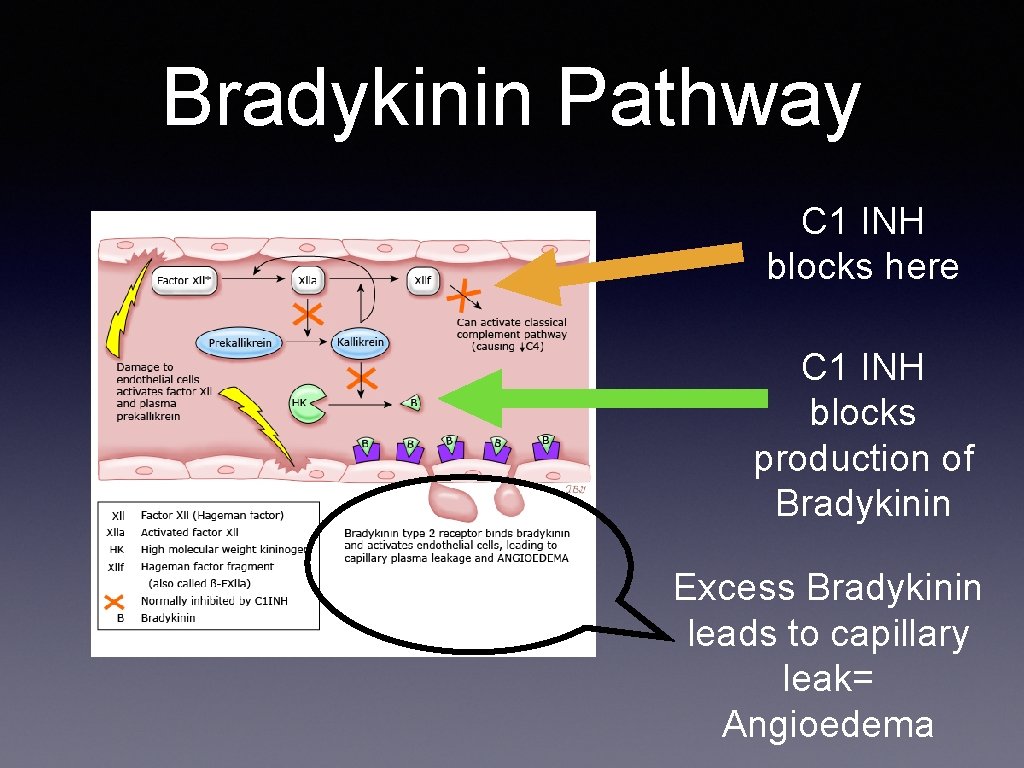
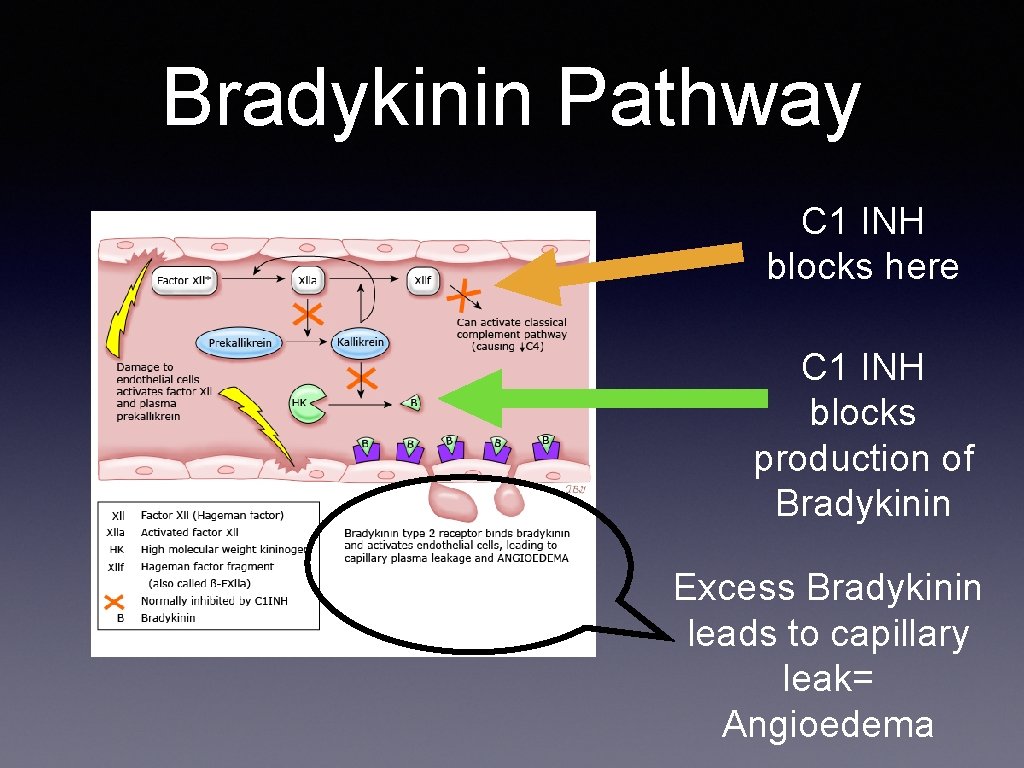
Bradykinin Pathway C 1 INH blocks here C 1 INH blocks production of Bradykinin Excess Bradykinin leads to capillary leak= Angioedema
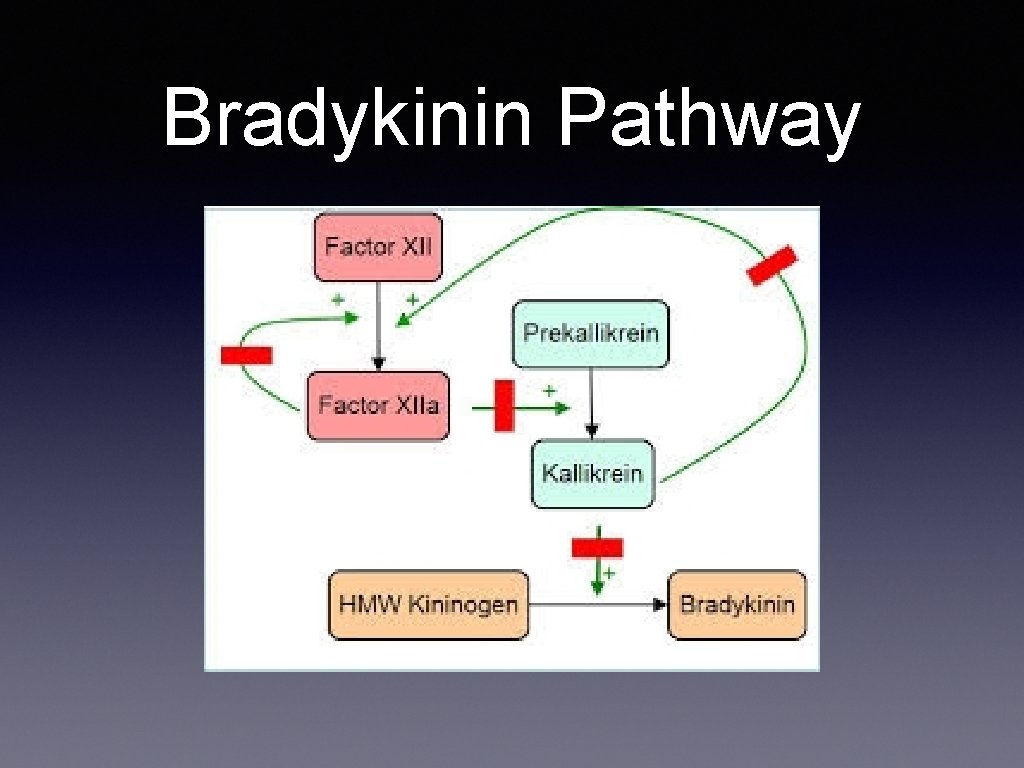
Bradykinin Pathway
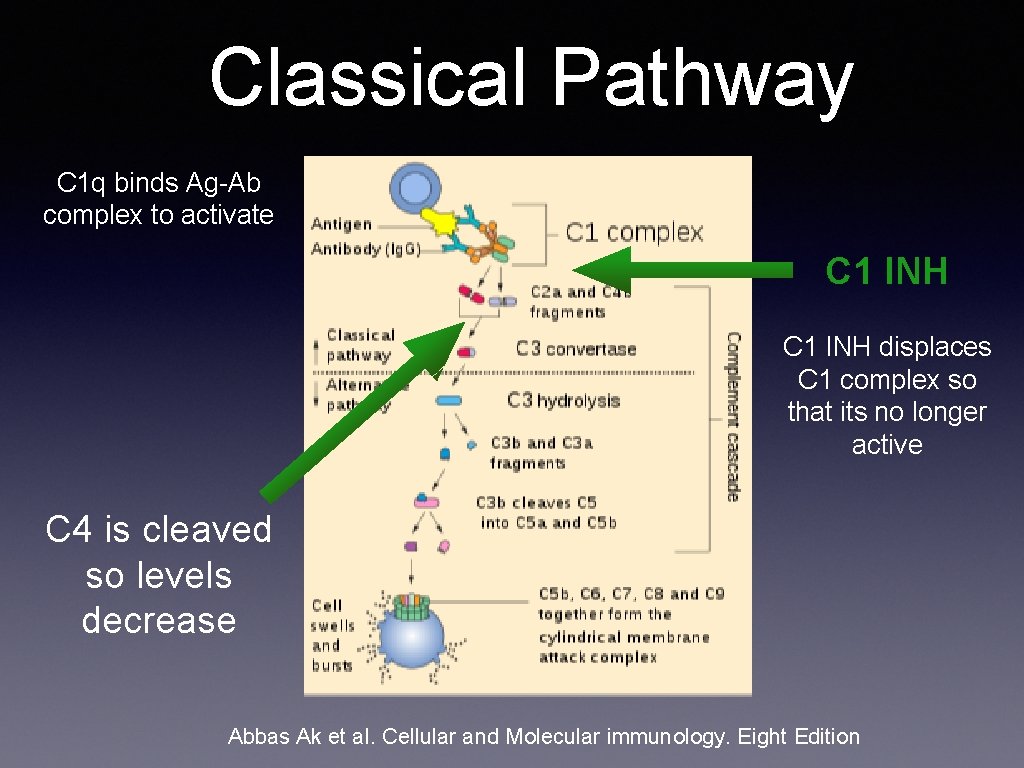
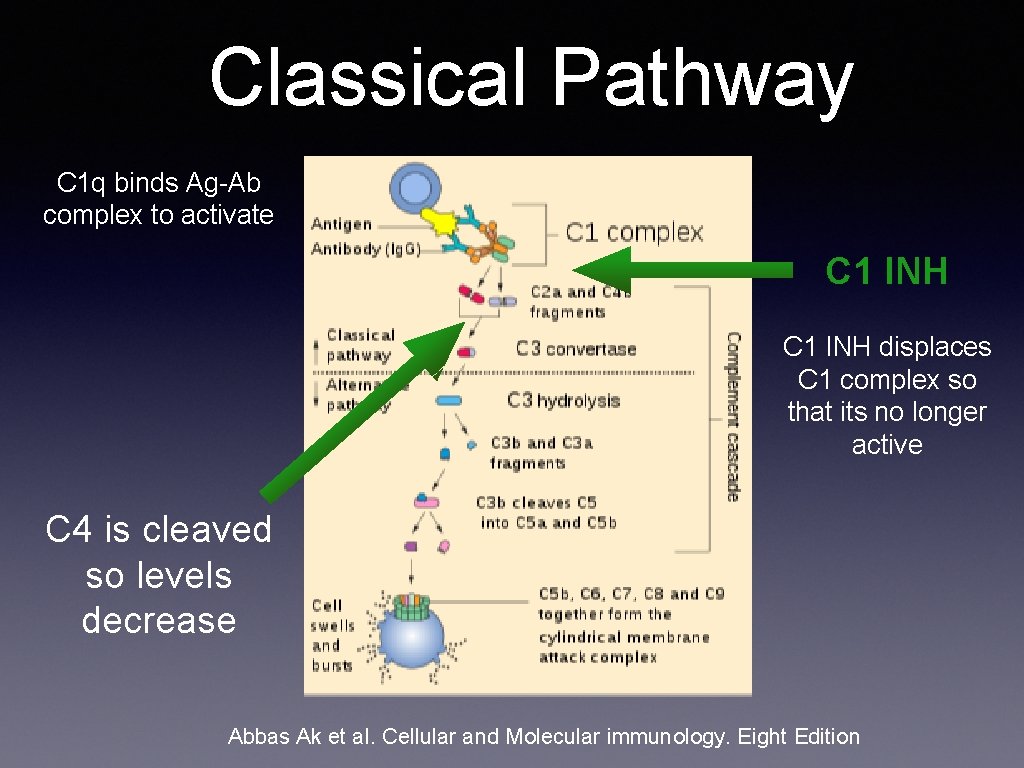
Classical Pathway C 1 q binds Ag-Ab complex to activate C 1 INH displaces C 1 complex so that its no longer active C 4 is cleaved so levels decrease Abbas Ak et al. Cellular and Molecular immunology. Eight Edition
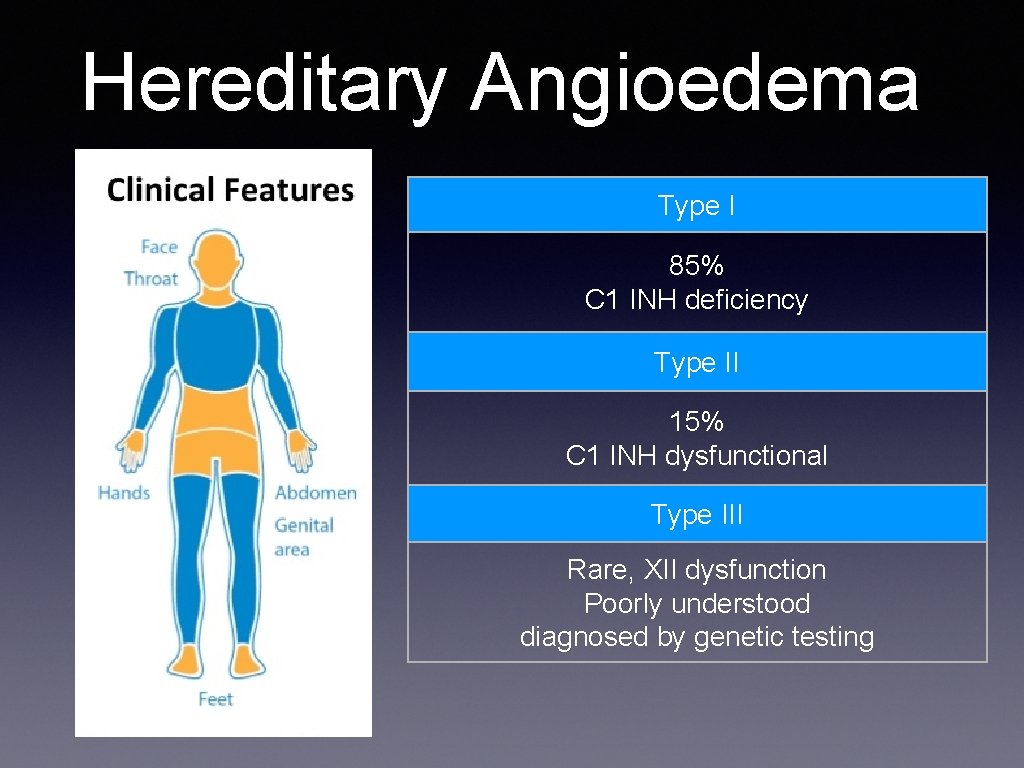
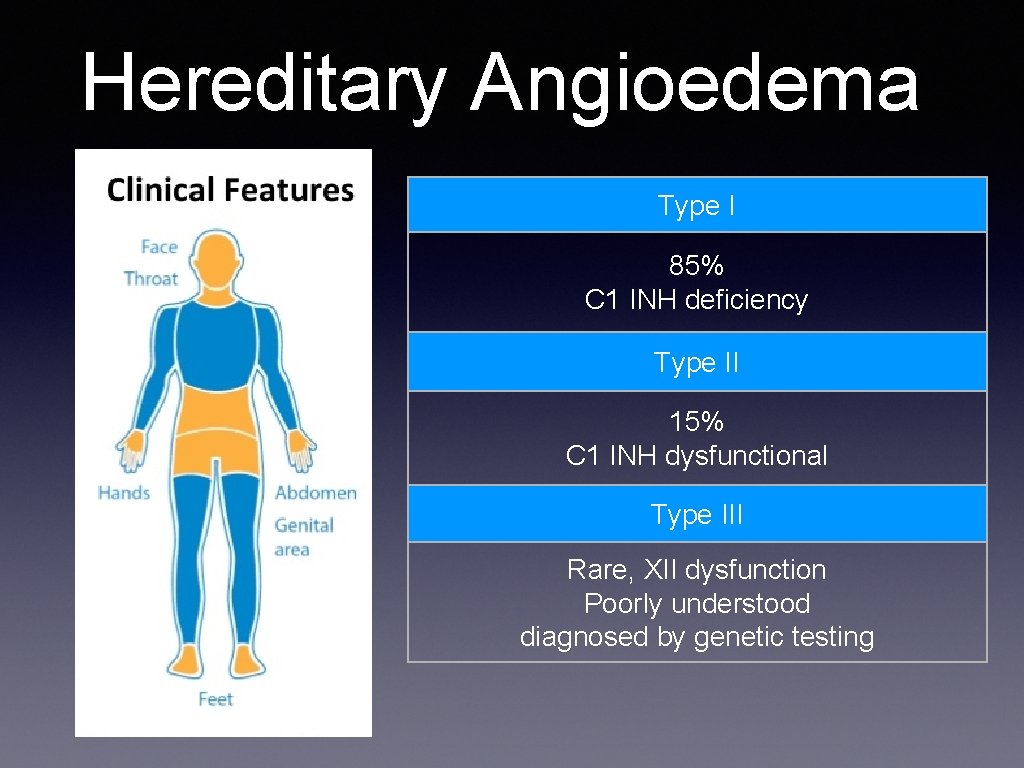
Hereditary Angioedema Type I 85% C 1 INH deficiency Type II 15% C 1 INH dysfunctional Type III Rare, XII dysfunction Poorly understood diagnosed by genetic testing
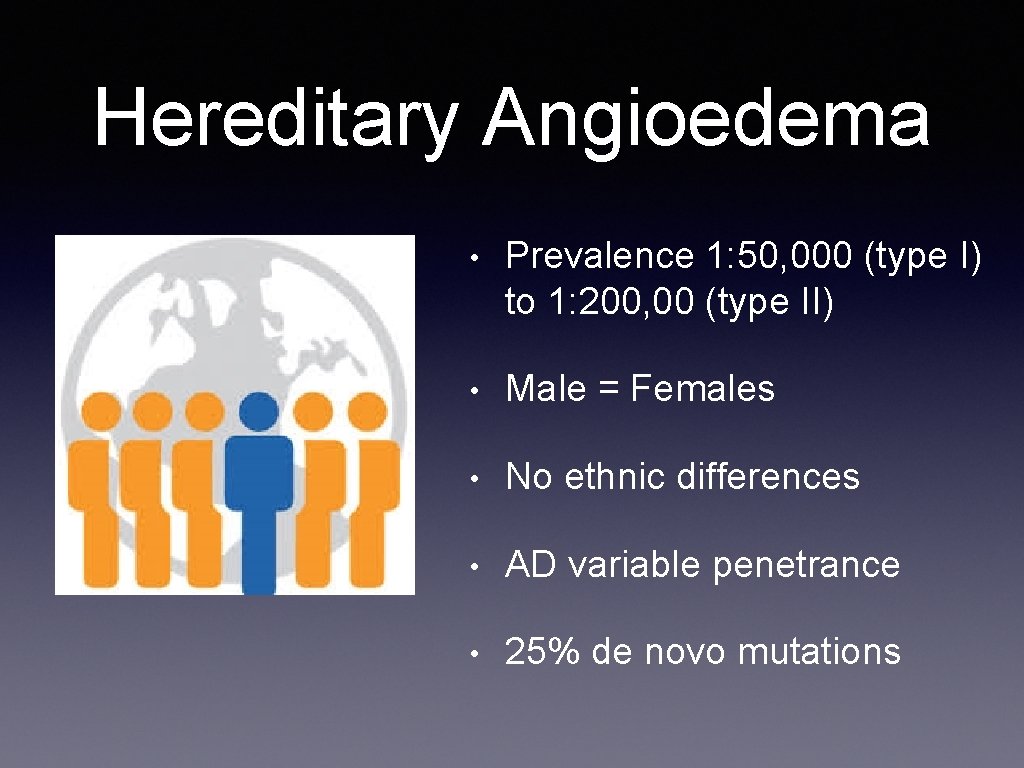
Hereditary Angioedema • Prevalence 1: 50, 000 (type I) to 1: 200, 00 (type II) • Male = Females • No ethnic differences • AD variable penetrance • 25% de novo mutations
• Age of onset usually in 20’s • 50% first attack before age 10 • 75% by age 15 • Symptoms worse around puberty
Other causes of Angioedema Often confused for Allergic Angioedema
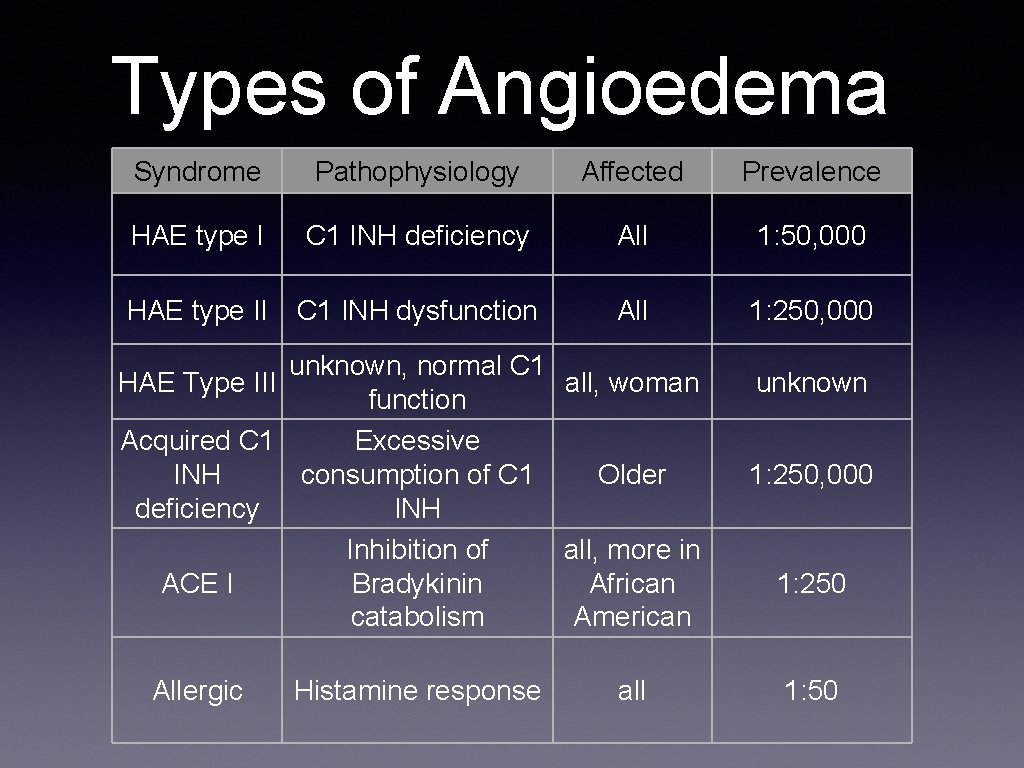
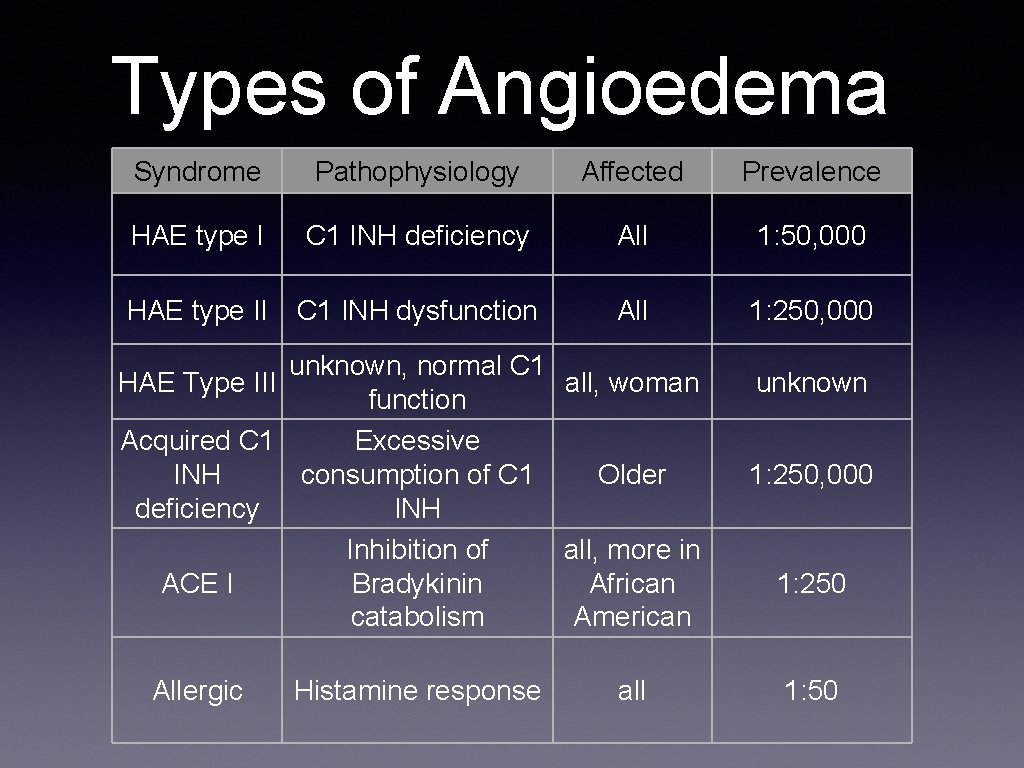
Types of Angioedema Syndrome Pathophysiology Affected Prevalence HAE type I C 1 INH deficiency All 1: 50, 000 HAE type II C 1 INH dysfunction All 1: 250, 000 unknown, normal C 1 HAE Type III all, woman function Acquired C 1 Excessive INH consumption of C 1 Older deficiency INH Inhibition of all, more in Bradykinin African ACE I catabolism American Allergic Histamine response all unknown 1: 250, 000 1: 250 1: 50
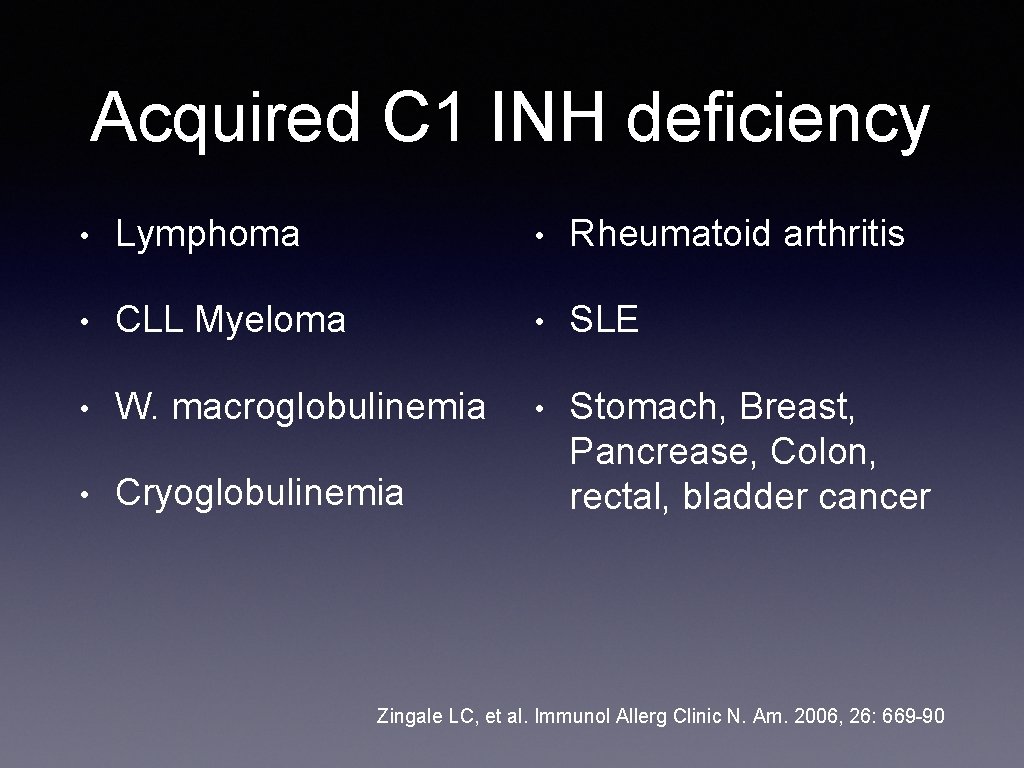
Acquired C 1 INH deficiency • Lymphoma • Rheumatoid arthritis • CLL Myeloma • SLE • W. macroglobulinemia • • Cryoglobulinemia Stomach, Breast, Pancrease, Colon, rectal, bladder cancer Zingale LC, et al. Immunol Allerg Clinic N. Am. 2006, 26: 669 -90

Triggers Physical Trauma • Dental work • intubation • tongue piercing • snoring • riding a bike
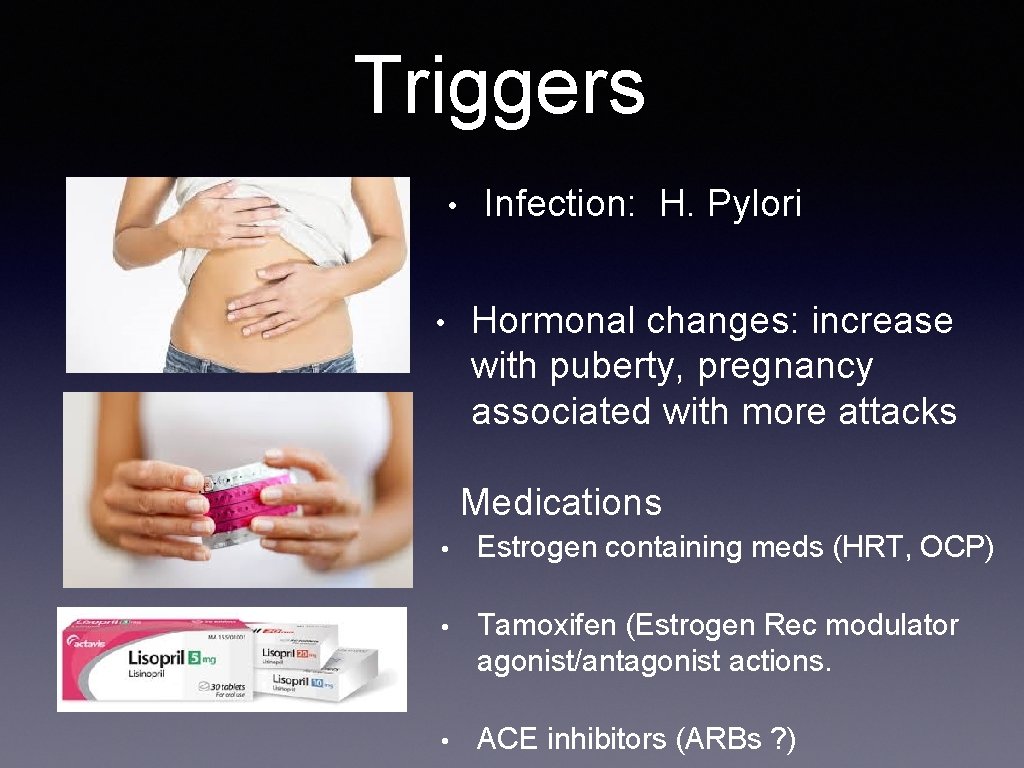
Triggers • • Infection: H. Pylori Hormonal changes: increase with puberty, pregnancy associated with more attacks Medications • Estrogen containing meds (HRT, OCP) • Tamoxifen (Estrogen Rec modulator agonist/antagonist actions. • ACE inhibitors (ARBs ? )
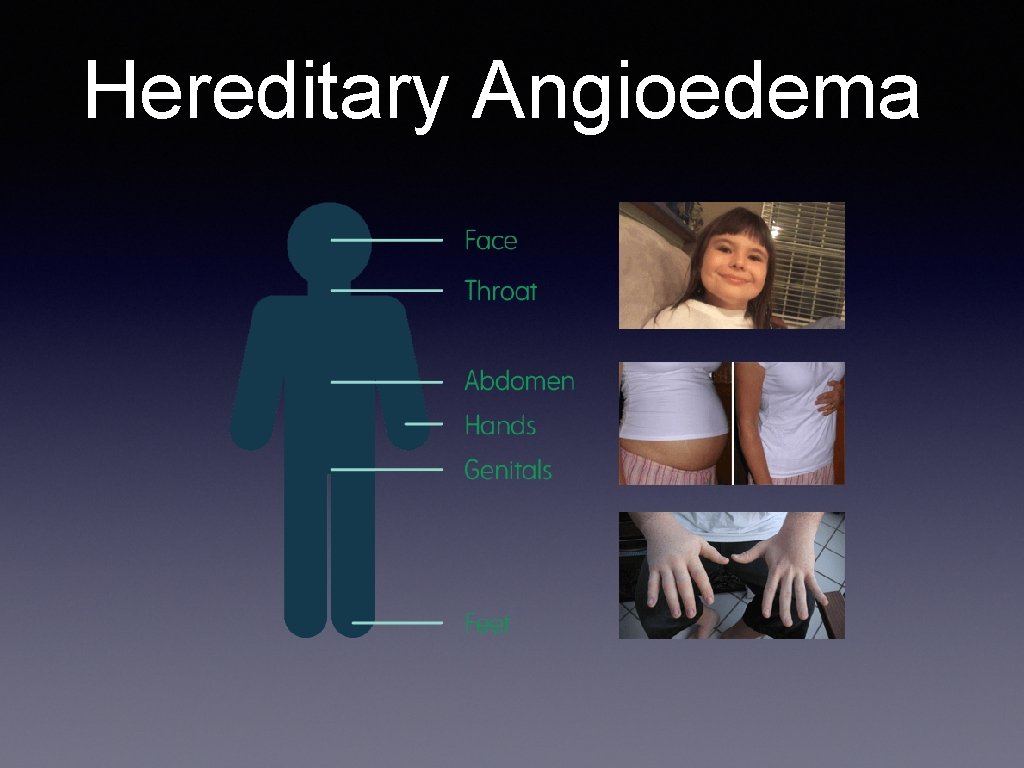
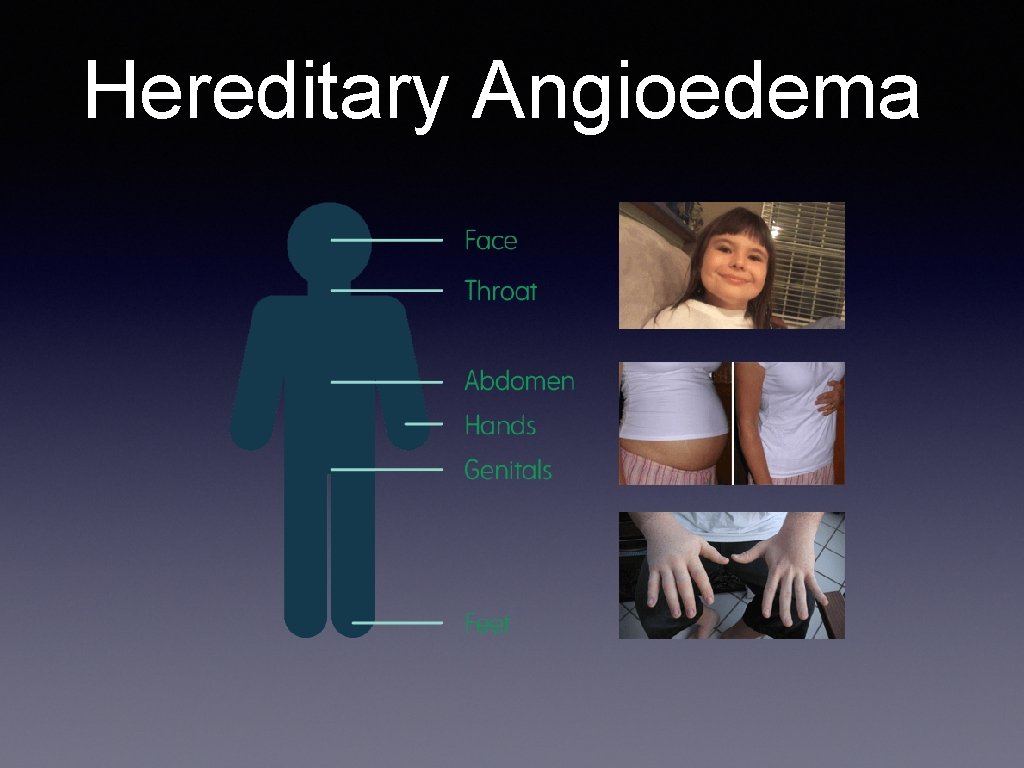
Hereditary Angioedema
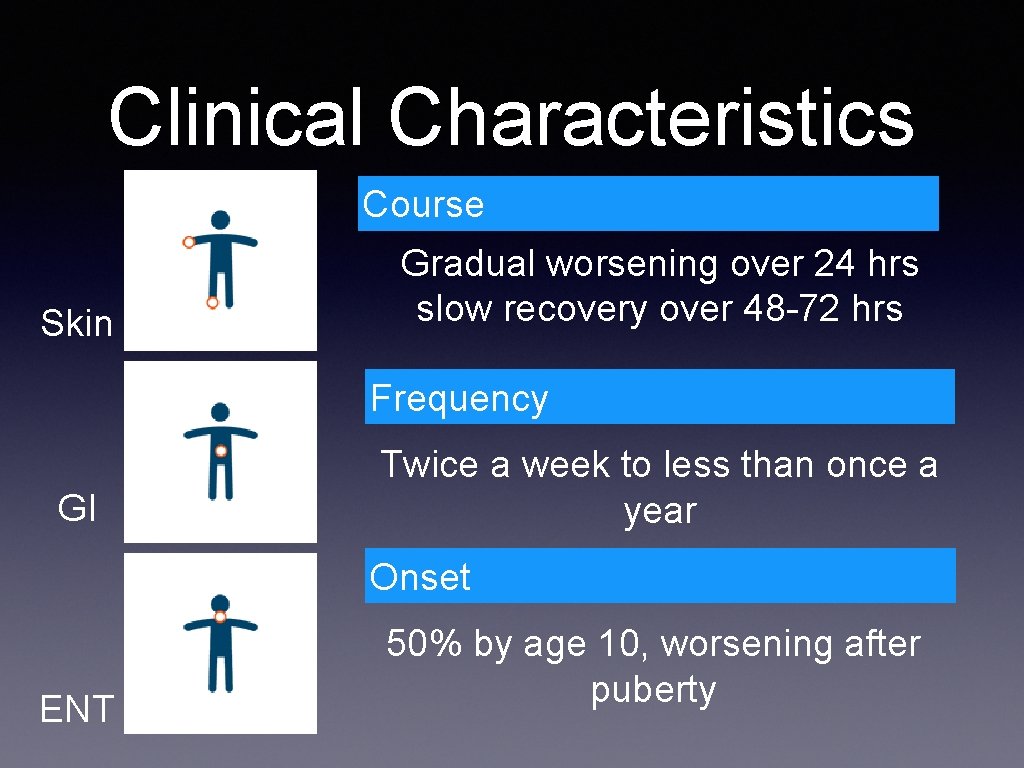
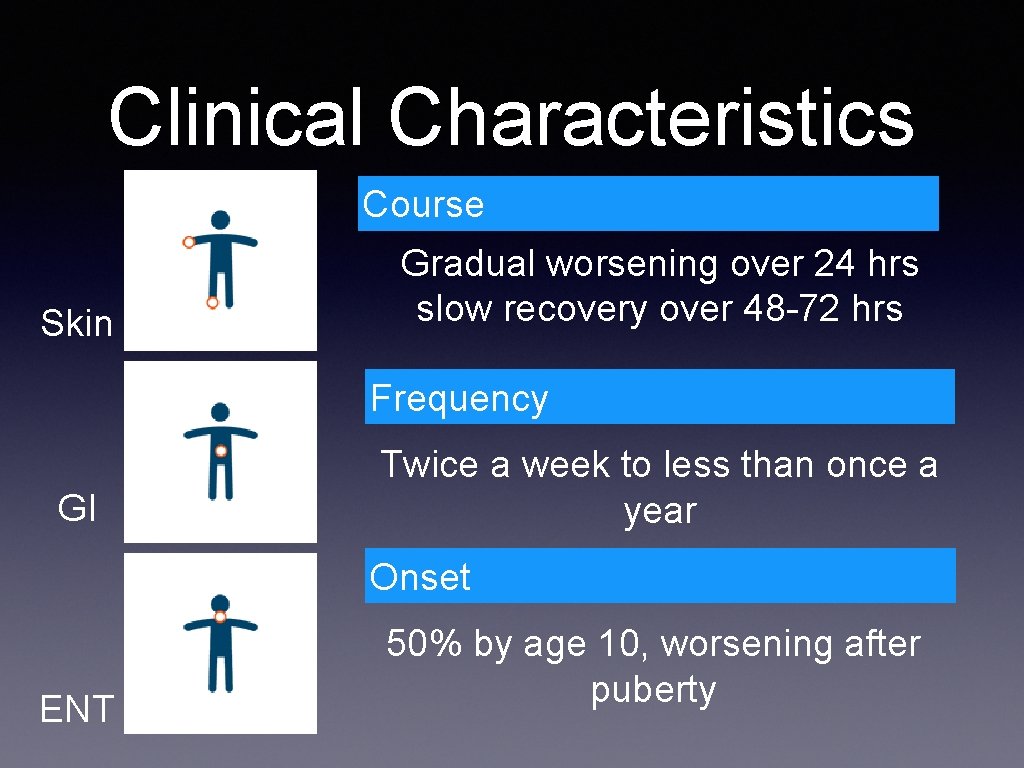
Clinical Characteristics Course Skin Gradual worsening over 24 hrs slow recovery over 48 -72 hrs Frequency GI Twice a week to less than once a year Onset ENT 50% by age 10, worsening after puberty
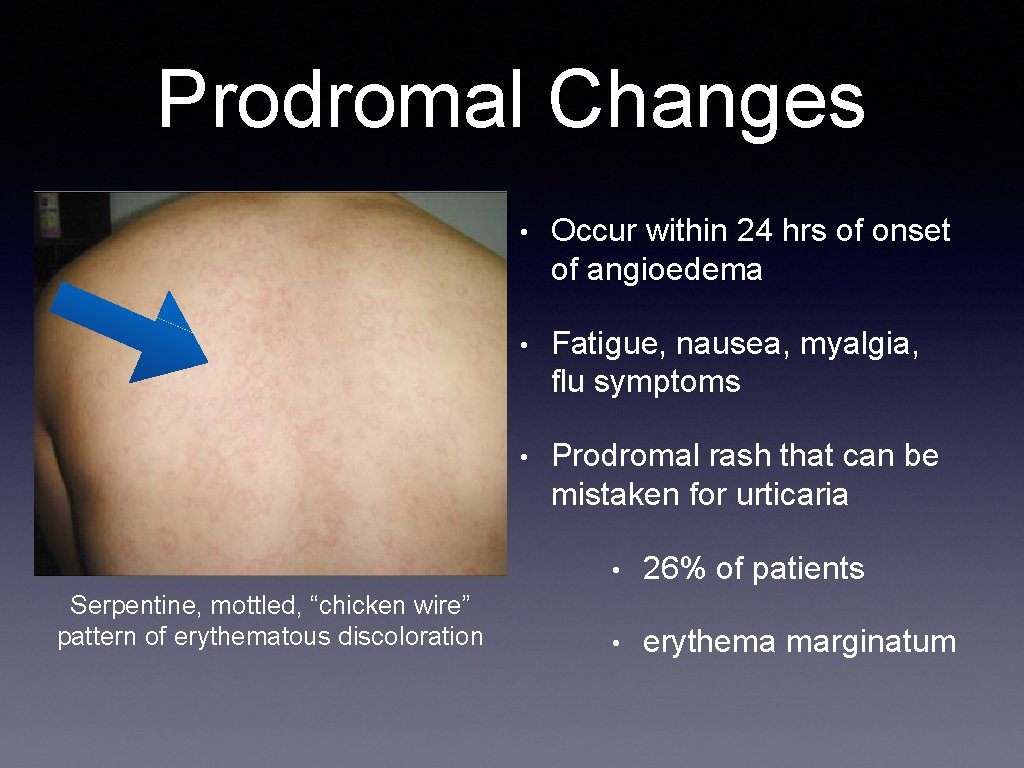
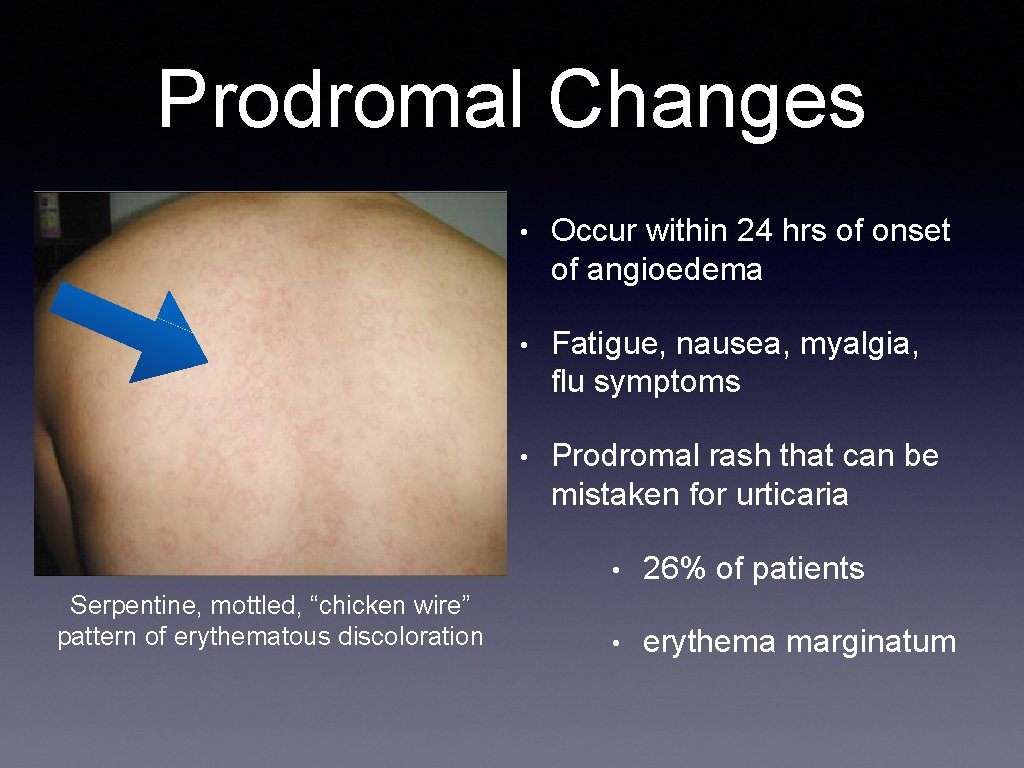
Prodromal Changes Serpentine, mottled, “chicken wire” pattern of erythematous discoloration • Occur within 24 hrs of onset of angioedema • Fatigue, nausea, myalgia, flu symptoms • Prodromal rash that can be mistaken for urticaria • 26% of patients • erythema marginatum
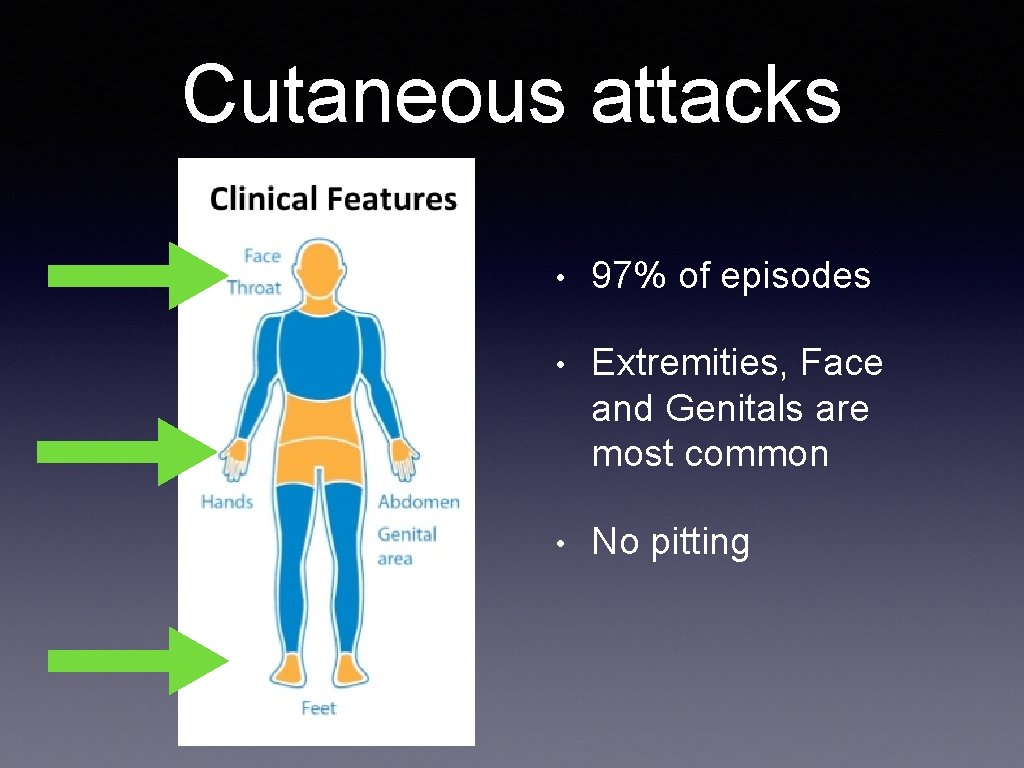
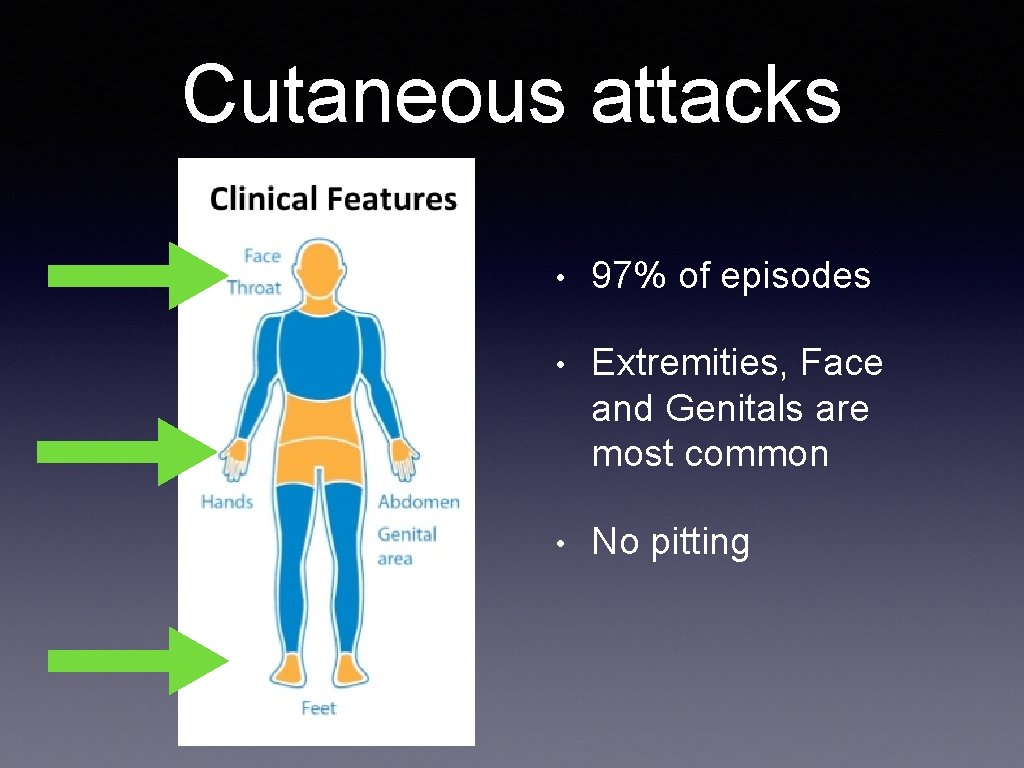
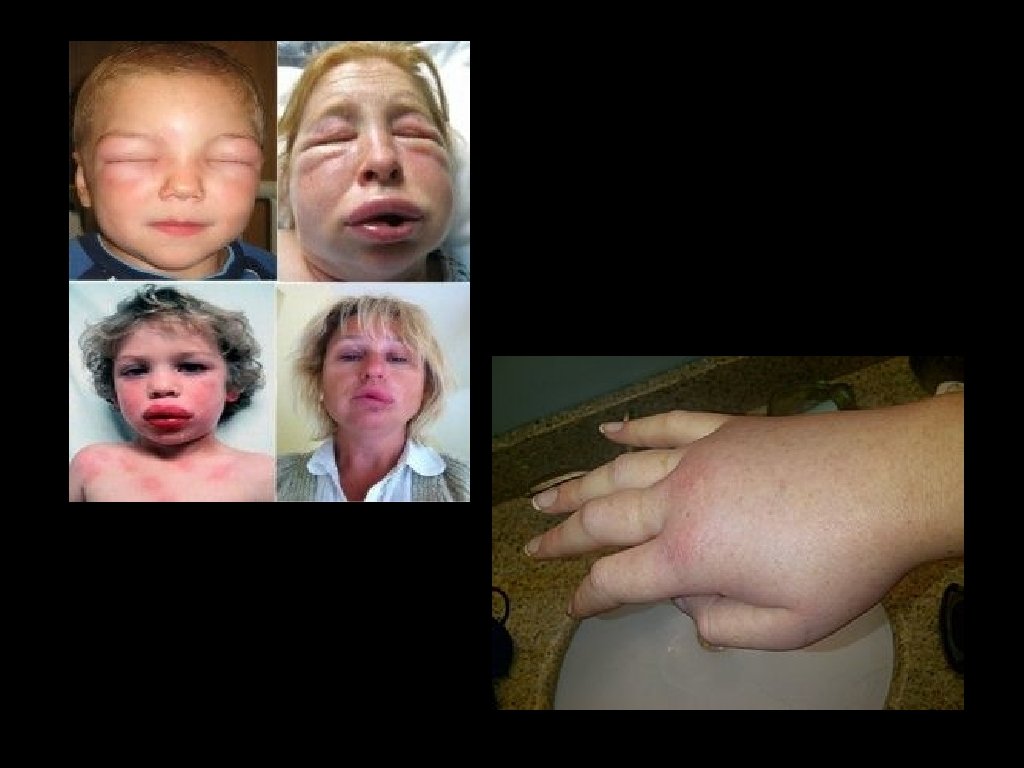
Cutaneous attacks • 97% of episodes • Extremities, Face and Genitals are most common • No pitting
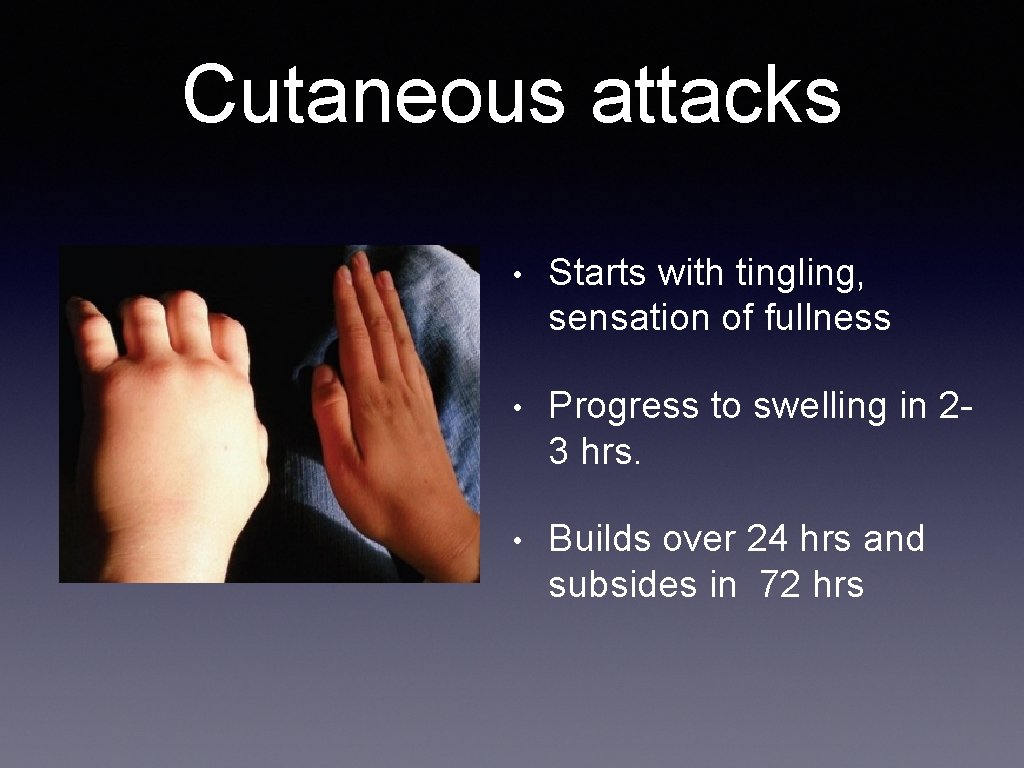
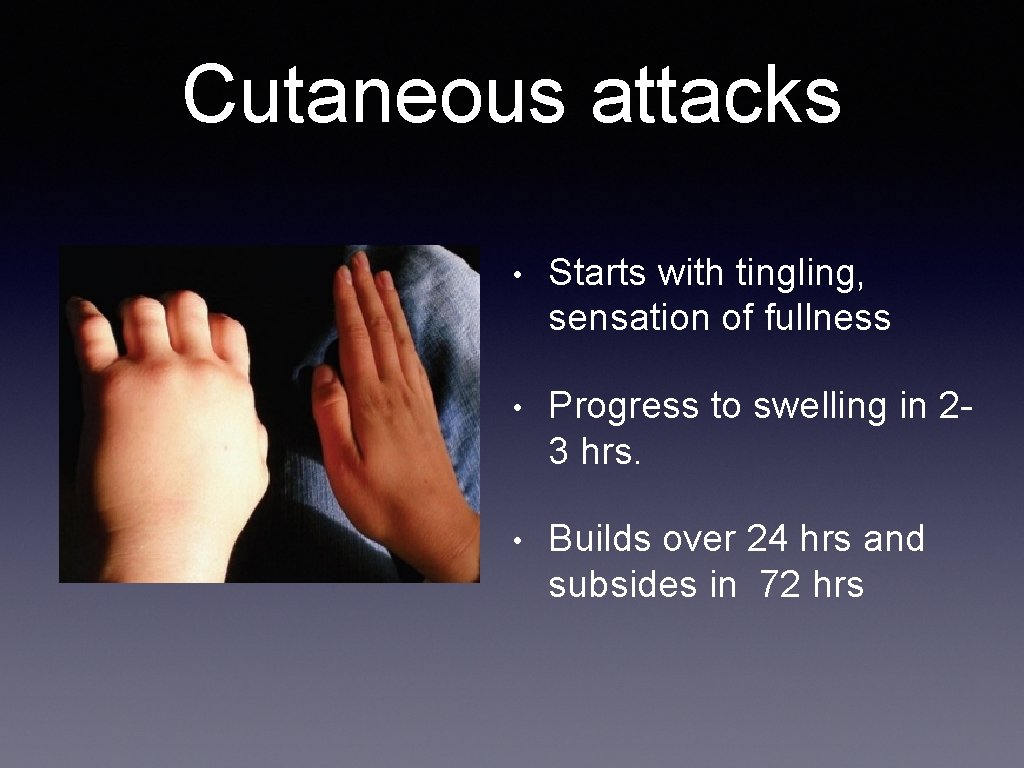
Cutaneous attacks • Starts with tingling, sensation of fullness • Progress to swelling in 23 hrs. • Builds over 24 hrs and subsides in 72 hrs
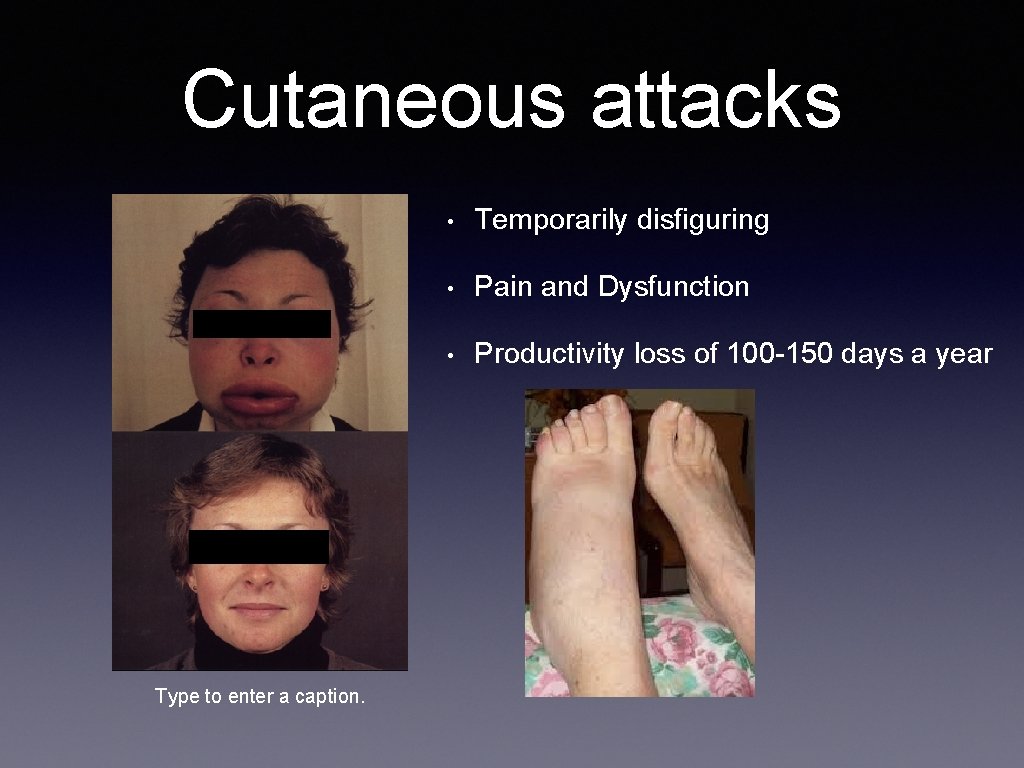
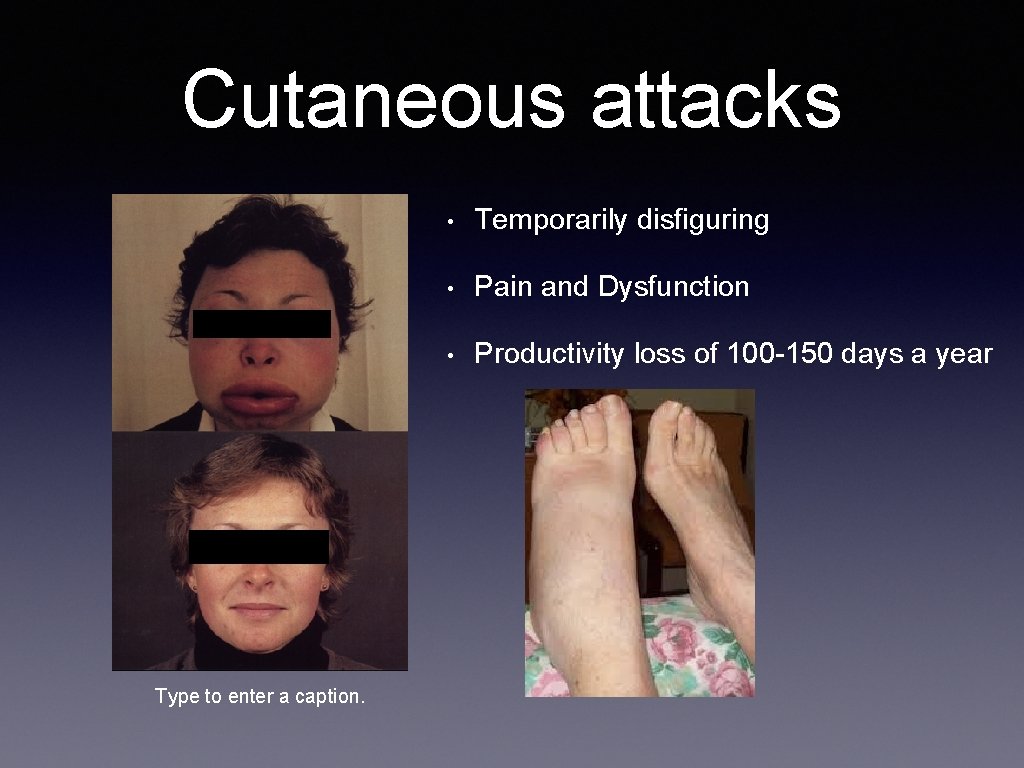
Cutaneous attacks Type to enter a caption. • Temporarily disfiguring • Pain and Dysfunction • Productivity loss of 100 -150 days a year
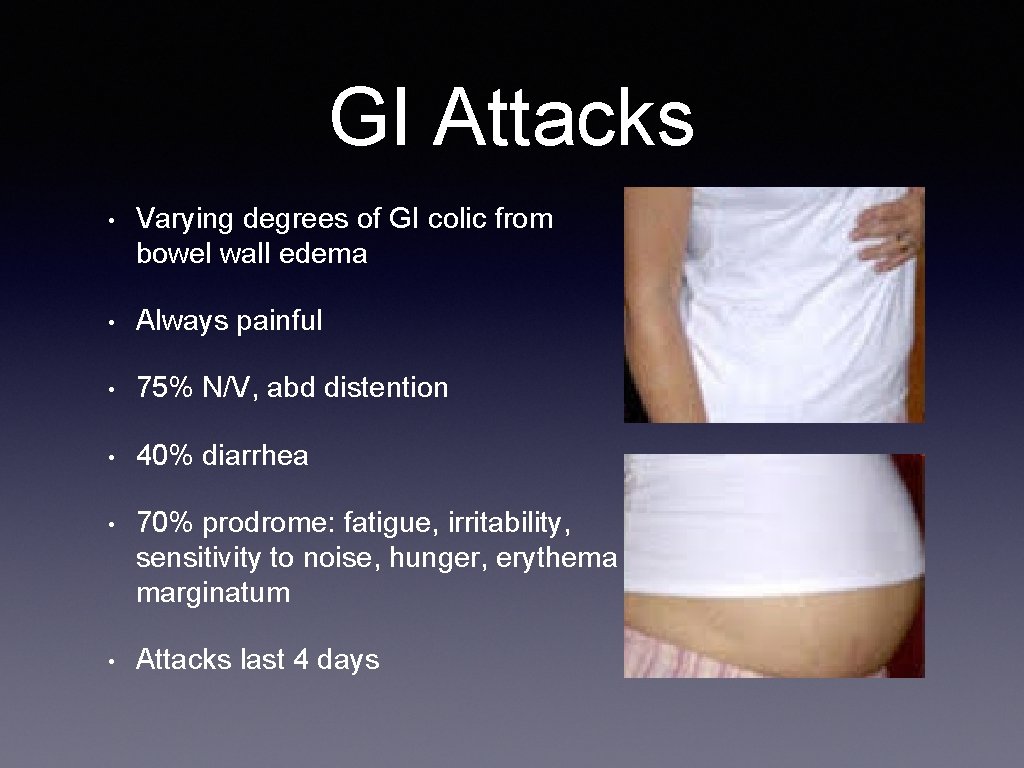
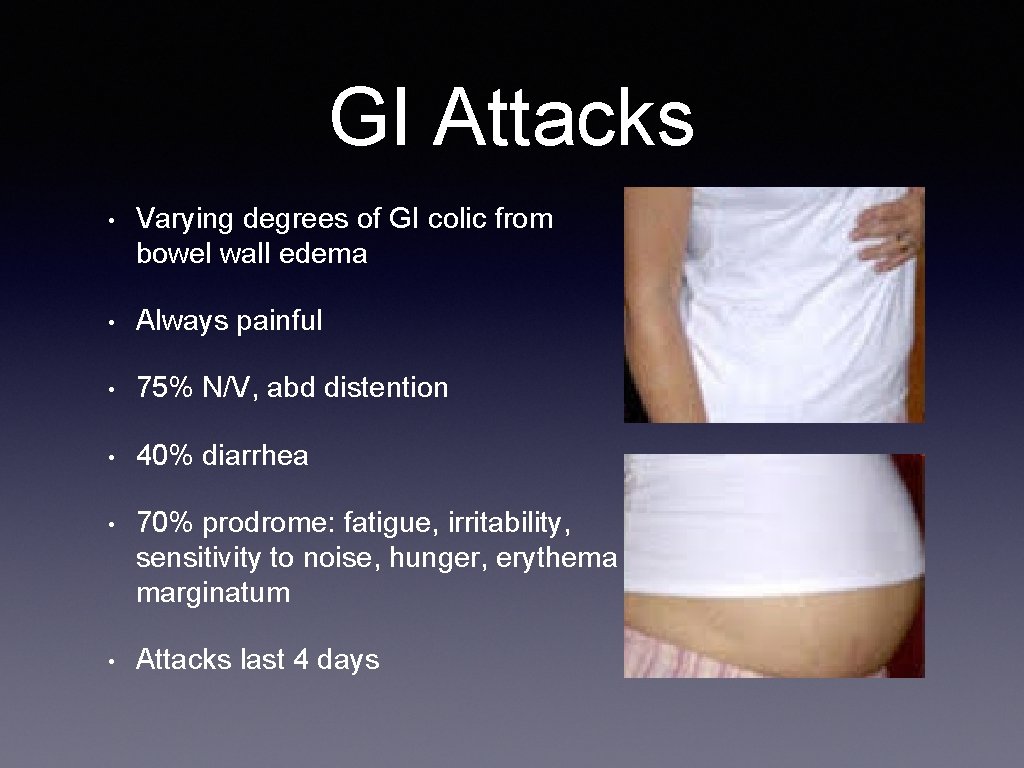
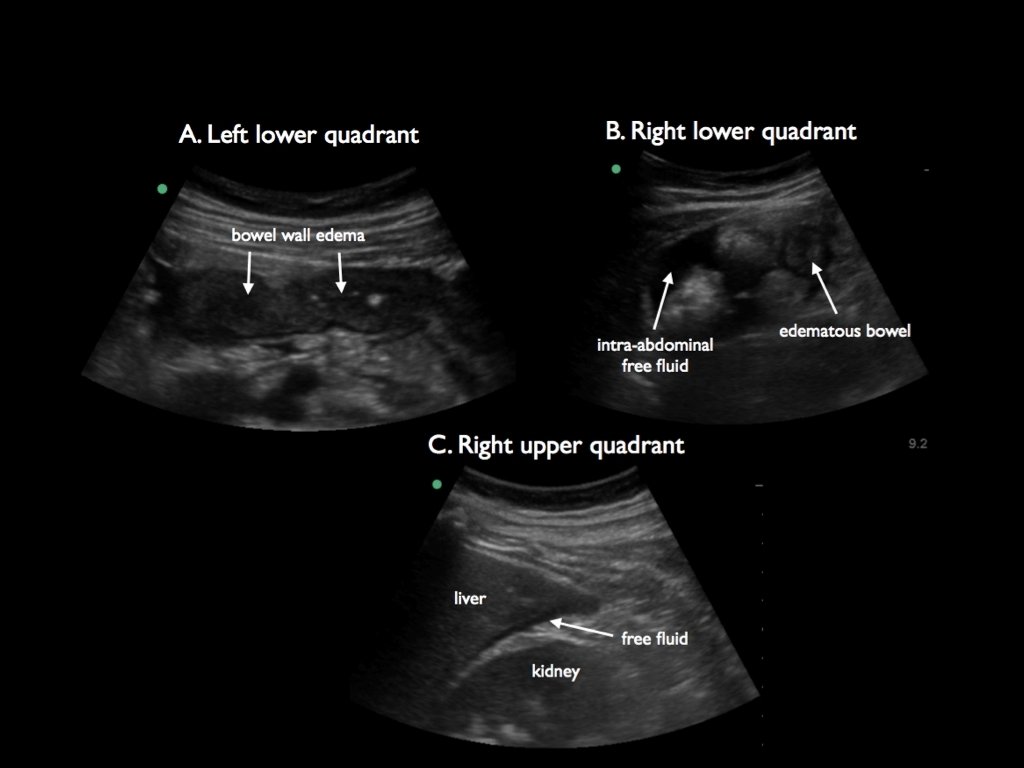
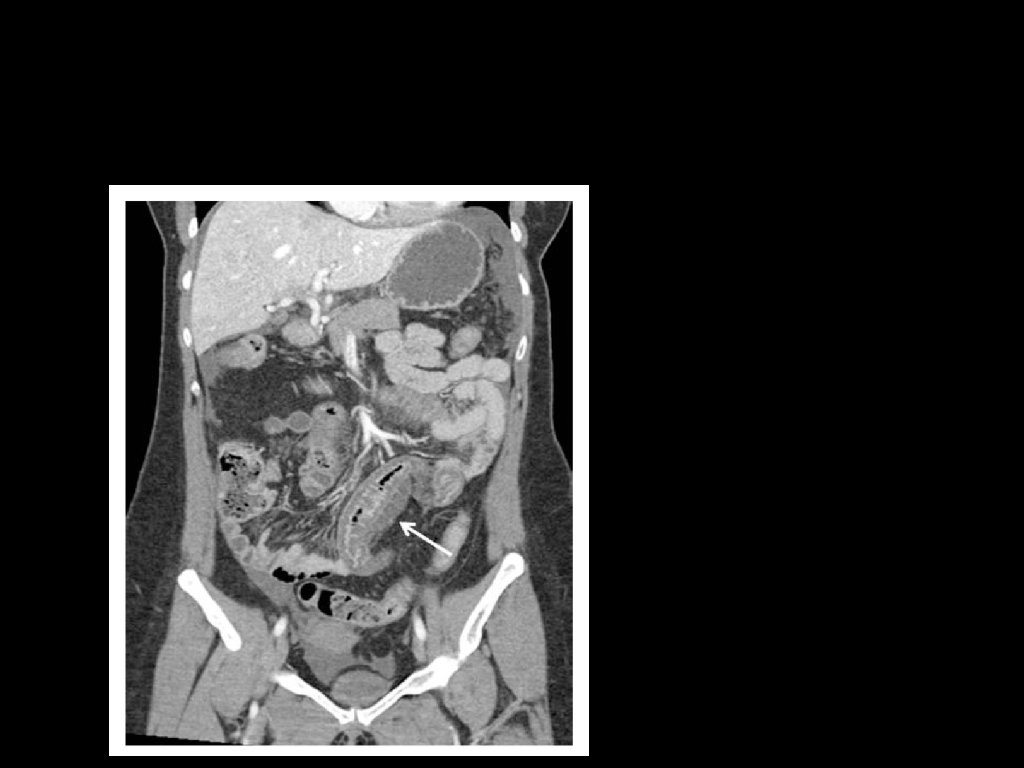
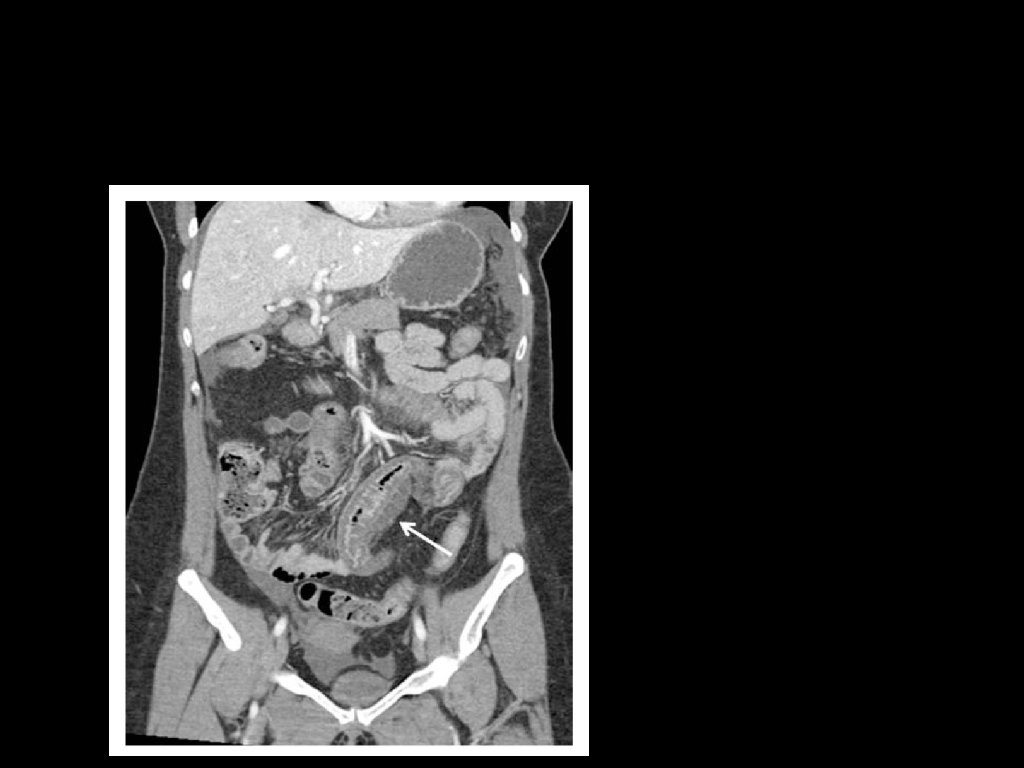
GI Attacks • Varying degrees of GI colic from bowel wall edema • Always painful • 75% N/V, abd distention • 40% diarrhea • 70% prodrome: fatigue, irritability, sensitivity to noise, hunger, erythema marginatum • Attacks last 4 days
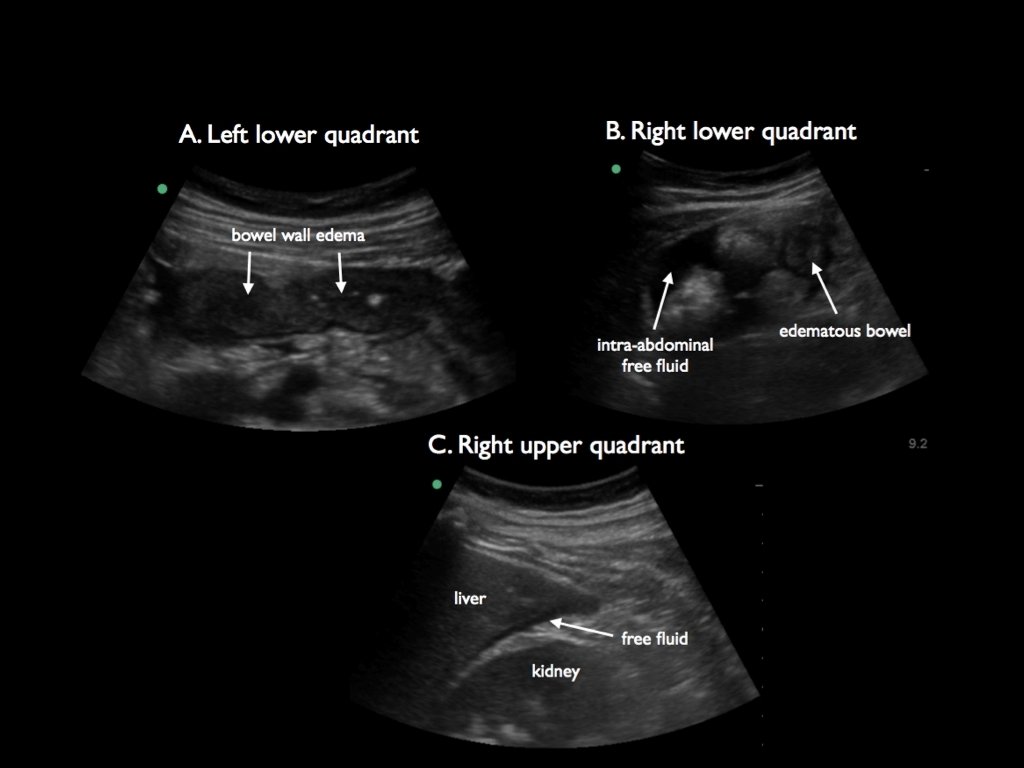
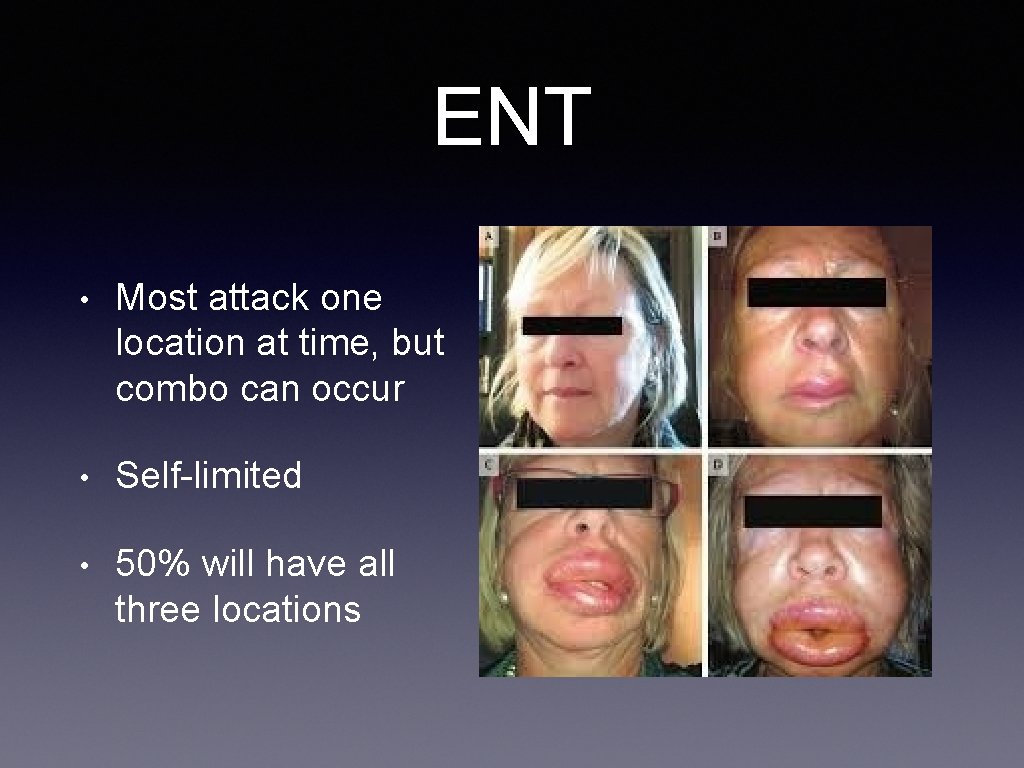
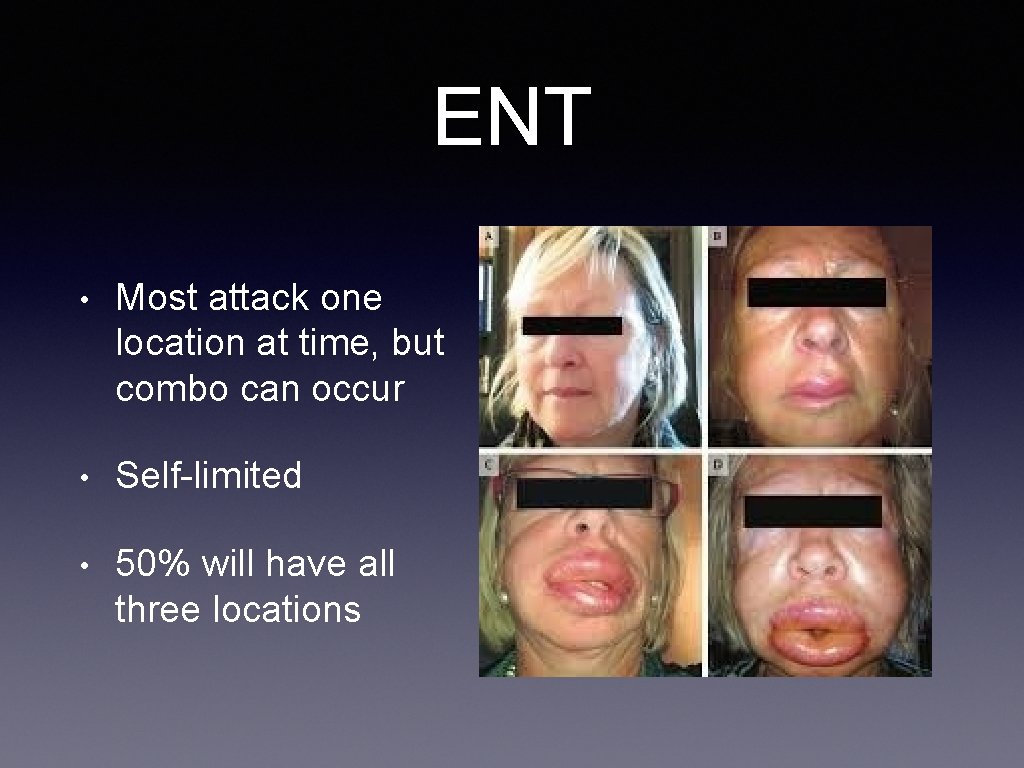
ENT • Most attack one location at time, but combo can occur • Self-limited • 50% will have all three locations
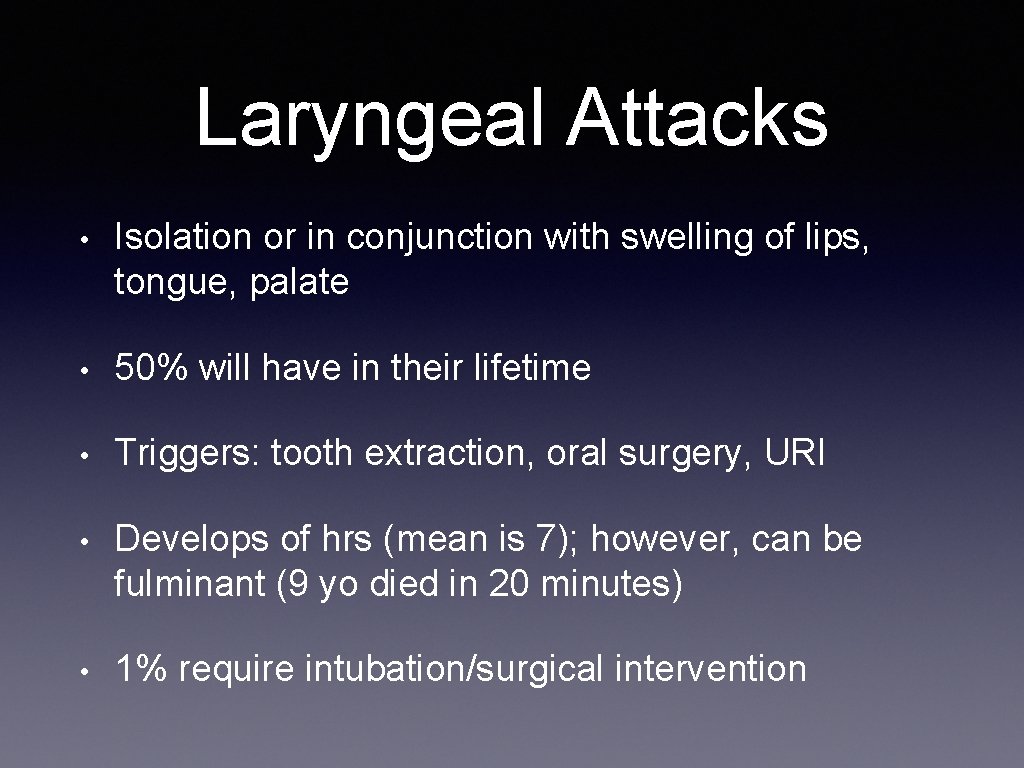
Laryngeal Attacks • Isolation or in conjunction with swelling of lips, tongue, palate • 50% will have in their lifetime • Triggers: tooth extraction, oral surgery, URI • Develops of hrs (mean is 7); however, can be fulminant (9 yo died in 20 minutes) • 1% require intubation/surgical intervention
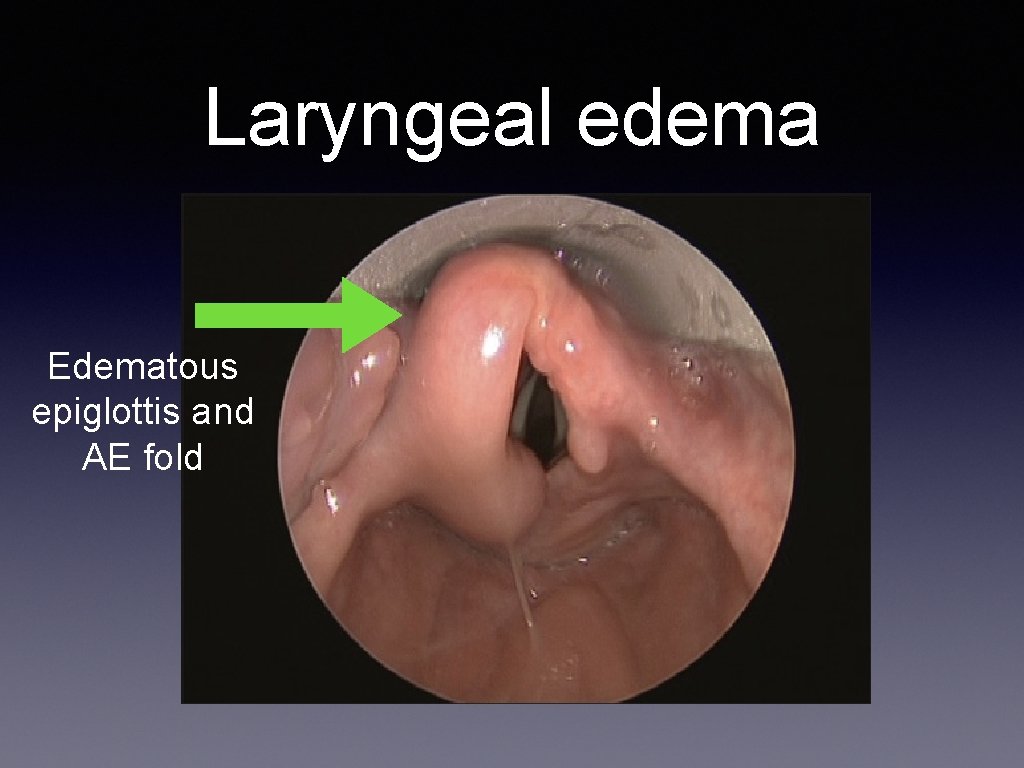
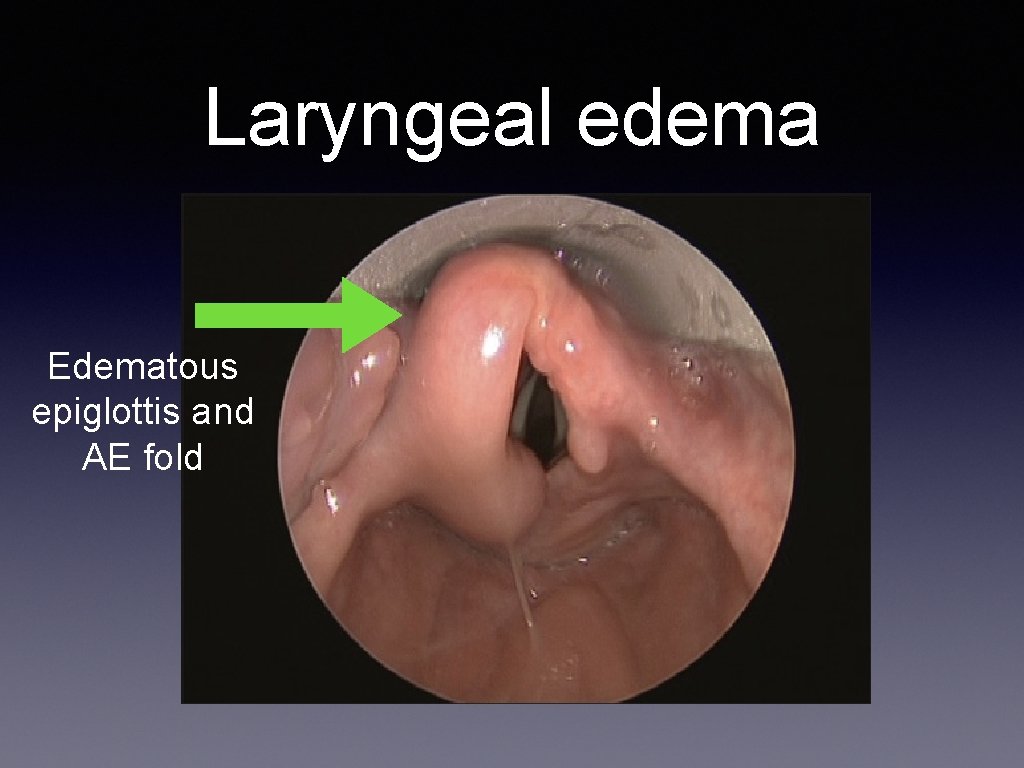
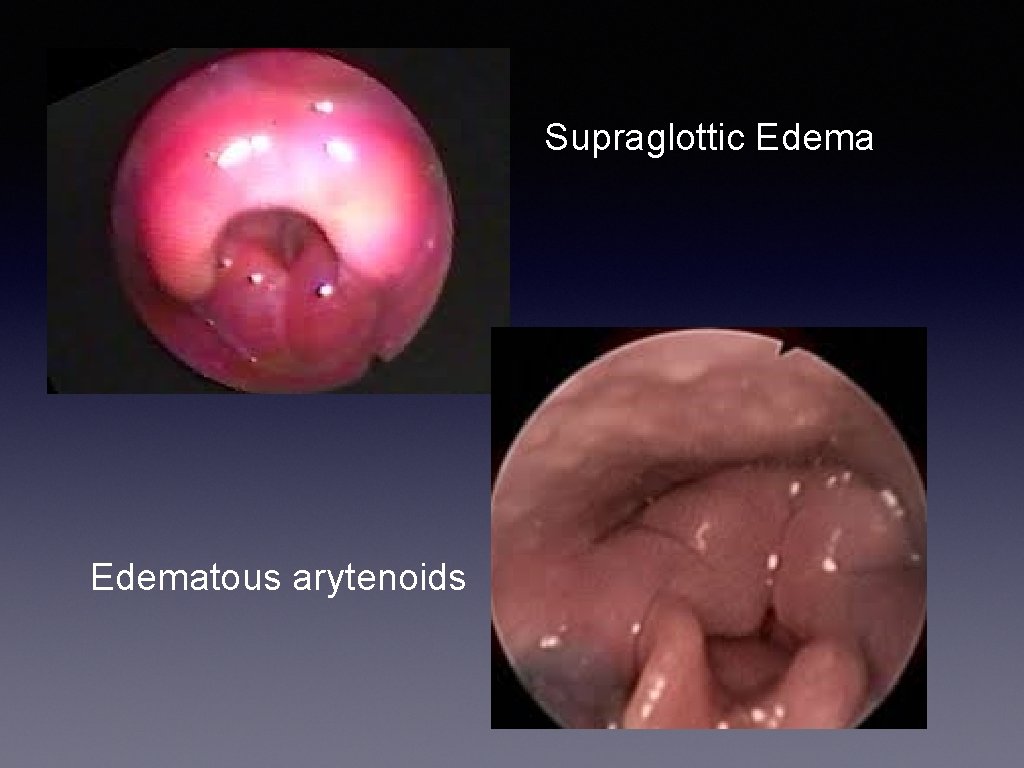
Laryngeal edema Edematous epiglottis and AE fold
3 phases • 1. Predyspnea (4 hrs): globus sensation • 2. Dyspnea (41 min): from onset of SOB to LOC • 3. Loss of consciousness (10 min): from LOC to death • Opportunity to intervene
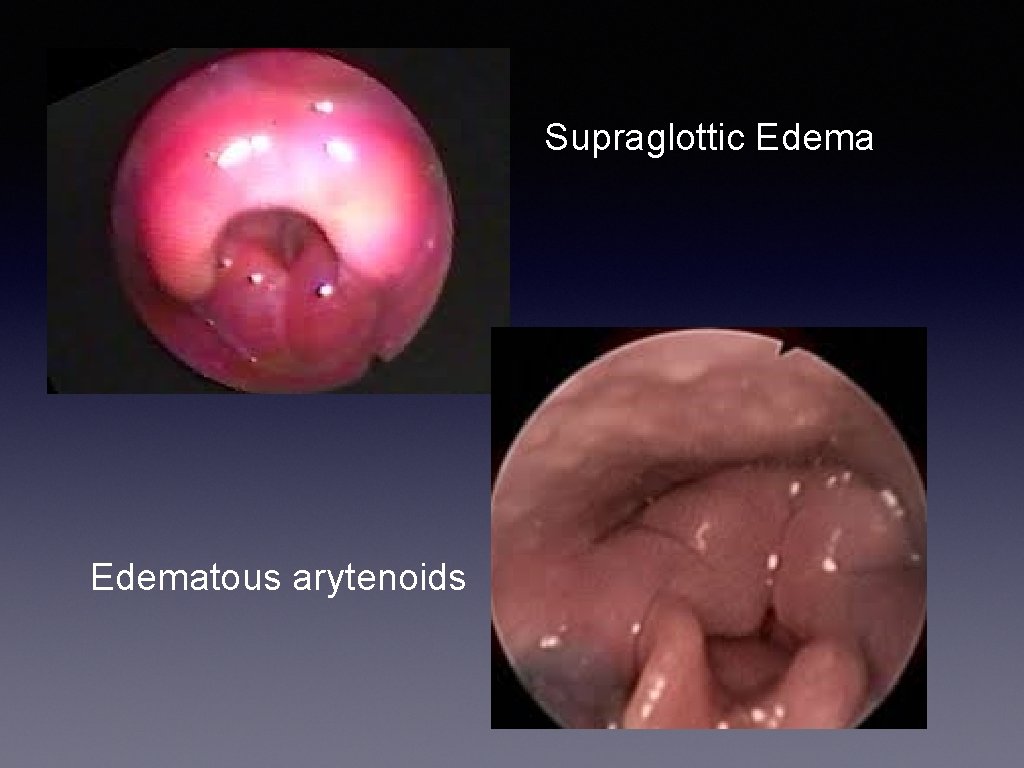
Supraglottic Edematous arytenoids
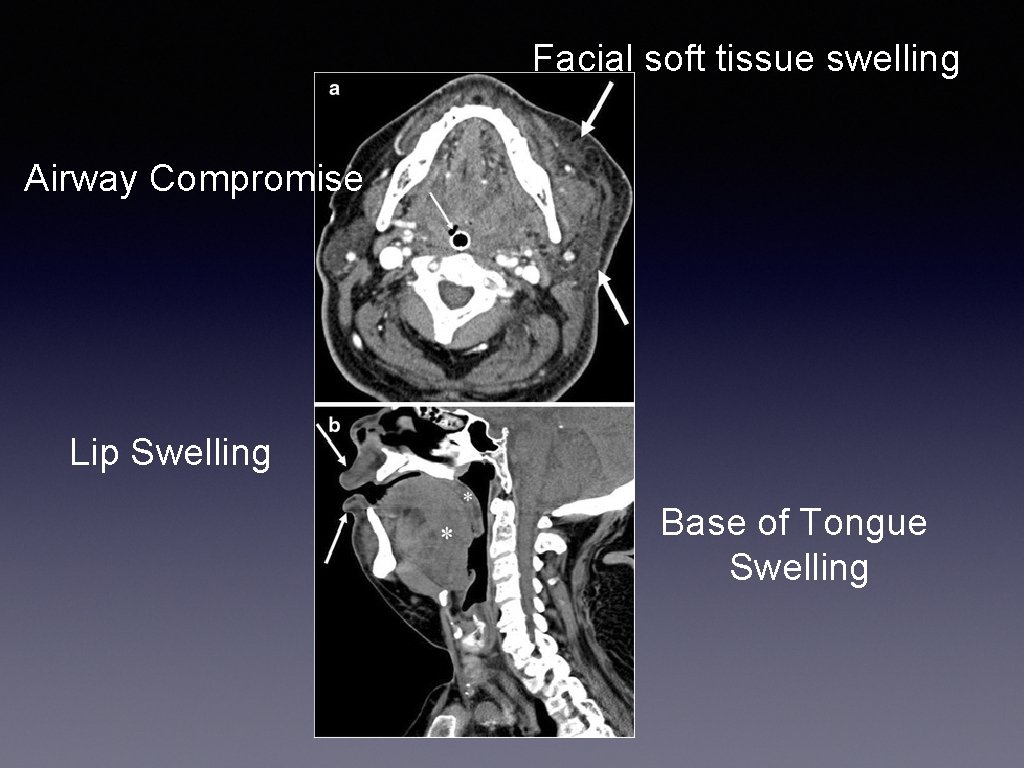
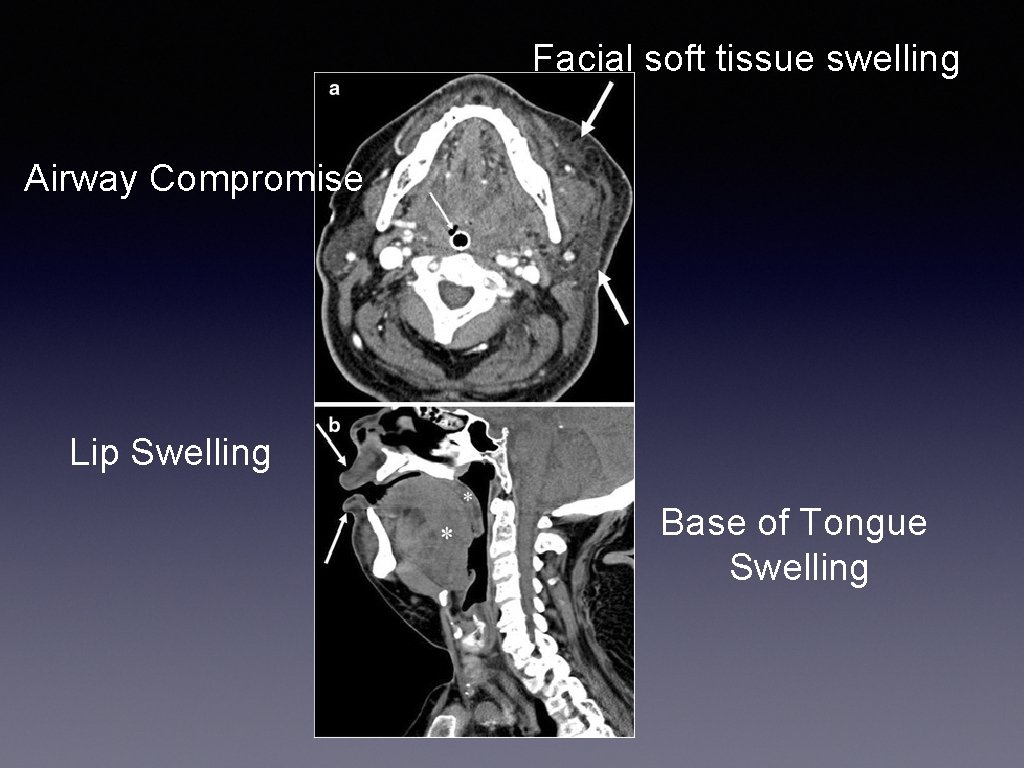
Facial soft tissue swelling Airway Compromise Lip Swelling Base of Tongue Swelling
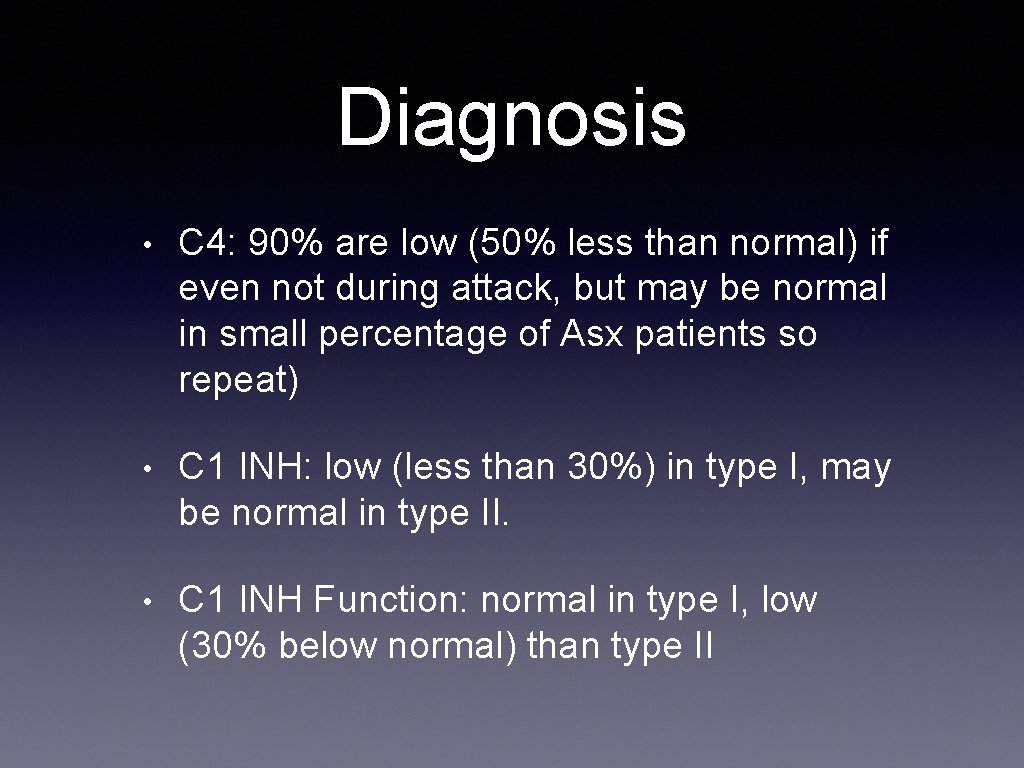
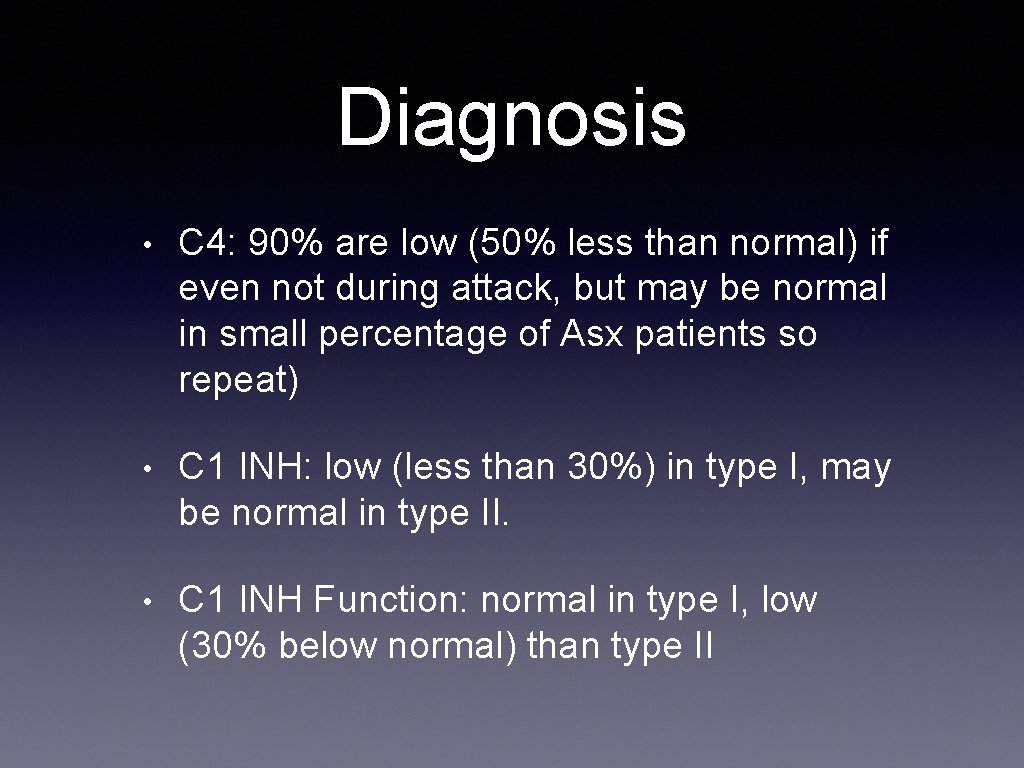
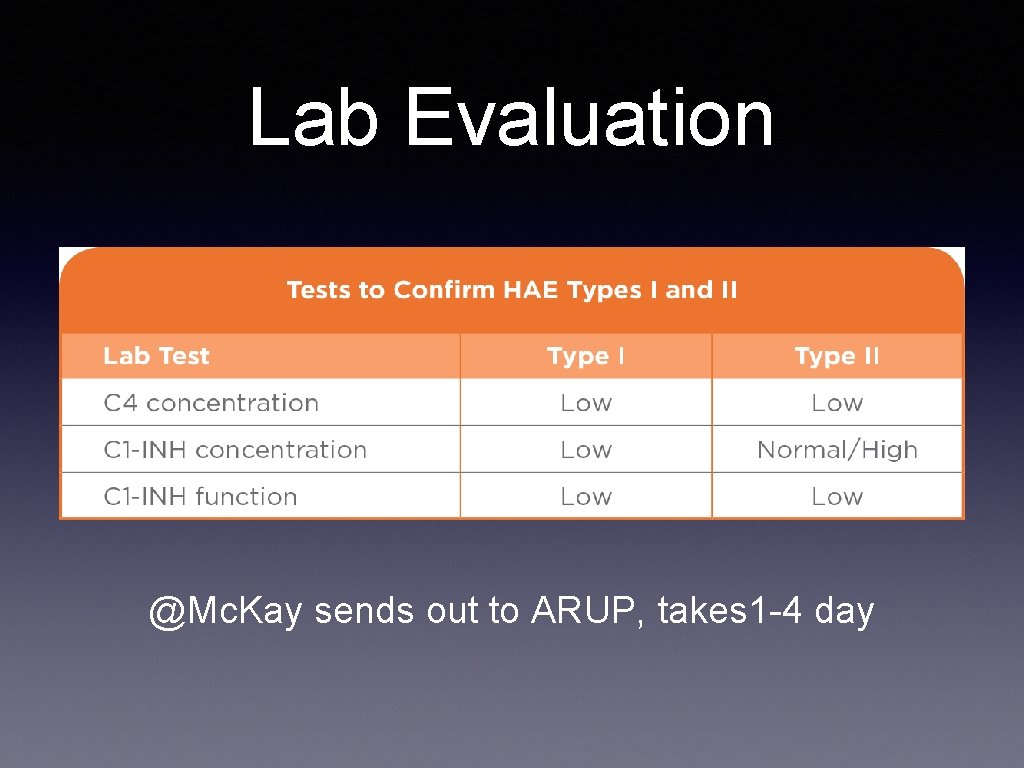
Diagnosis • C 4: 90% are low (50% less than normal) if even not during attack, but may be normal in small percentage of Asx patients so repeat) • C 1 INH: low (less than 30%) in type I, may be normal in type II. • C 1 INH Function: normal in type I, low (30% below normal) than type II
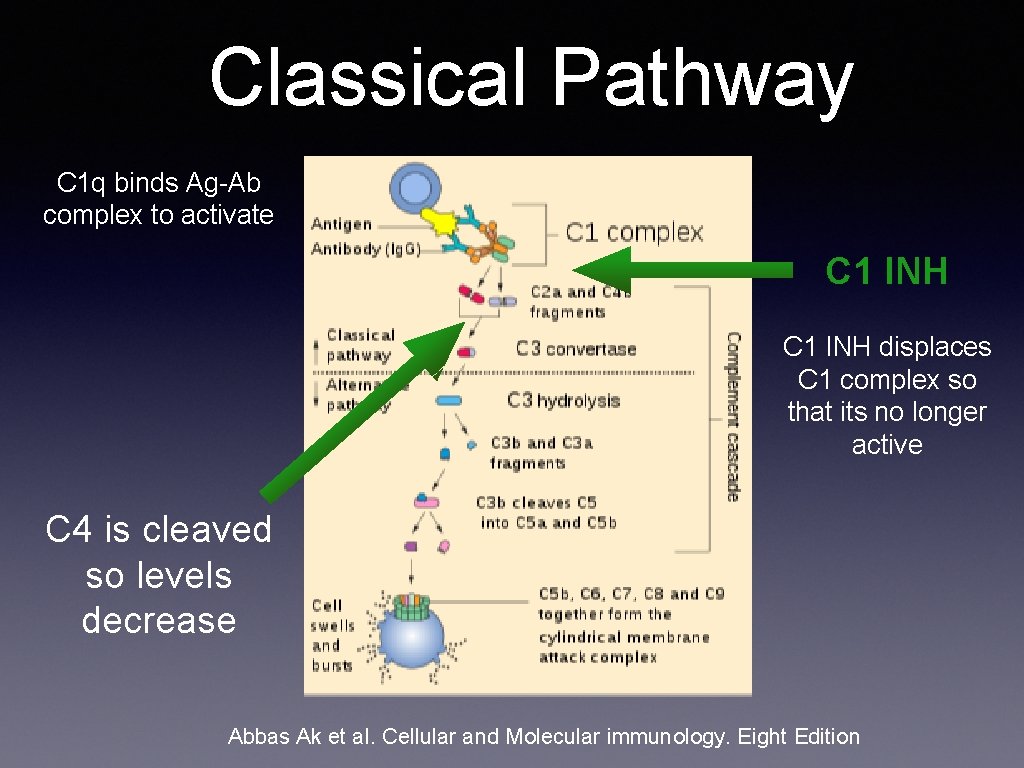
Classical Pathway C 1 q binds Ag-Ab complex to activate C 1 INH displaces C 1 complex so that its no longer active C 4 is cleaved so levels decrease Abbas Ak et al. Cellular and Molecular immunology. Eight Edition
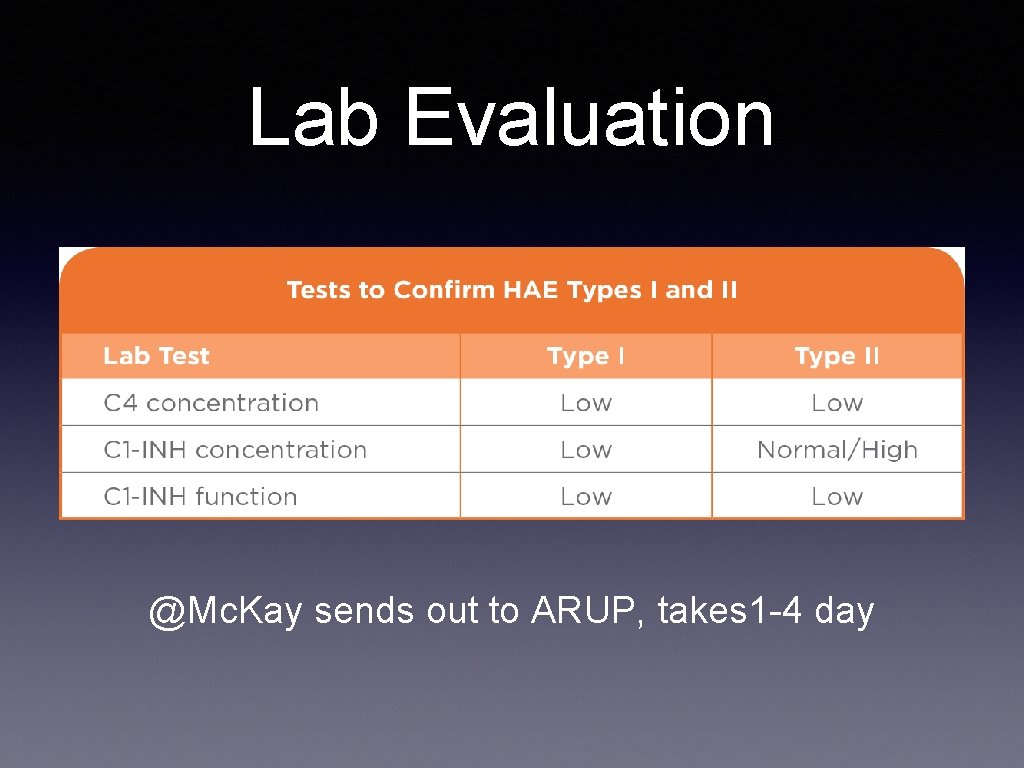
Lab Evaluation @Mc. Kay sends out to ARUP, takes 1 -4 day
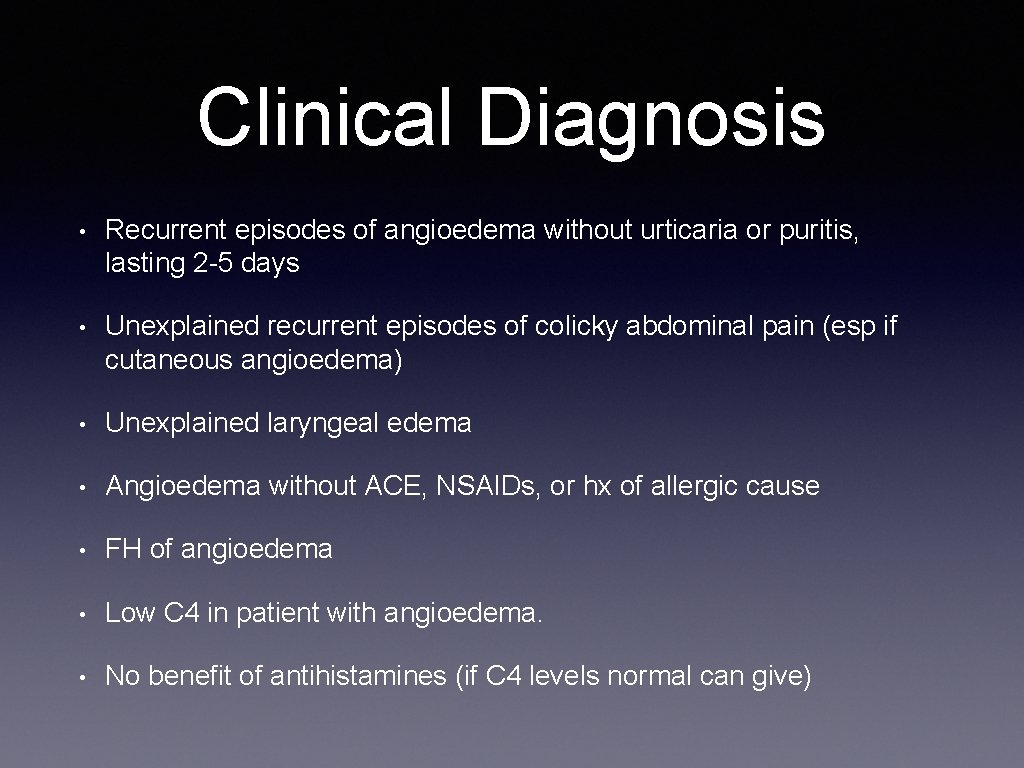
Clinical Diagnosis • Recurrent episodes of angioedema without urticaria or puritis, lasting 2 -5 days • Unexplained recurrent episodes of colicky abdominal pain (esp if cutaneous angioedema) • Unexplained laryngeal edema • Angioedema without ACE, NSAIDs, or hx of allergic cause • FH of angioedema • Low C 4 in patient with angioedema. • No benefit of antihistamines (if C 4 levels normal can give)
Treatment • prior to 2008, not many options • 30% mortality • Now several FDA approved options.
Treatment of Acute Attacks • Bradykinin mediated • Does NOT respond to epinephrine, antihistamines, glucocorticoids • Goal: replace C 1 INH or block production/function of bradykinin • Response within 2 hrs
First Line Therapies • C 1 INH plasm derived concentrates • Recombinant human C 1 INH • Icatibant (bradykinin receptor antagonist) • Ecallantide (recombinant Kallikrein Inhibitor) Cost: $5000 to $10000
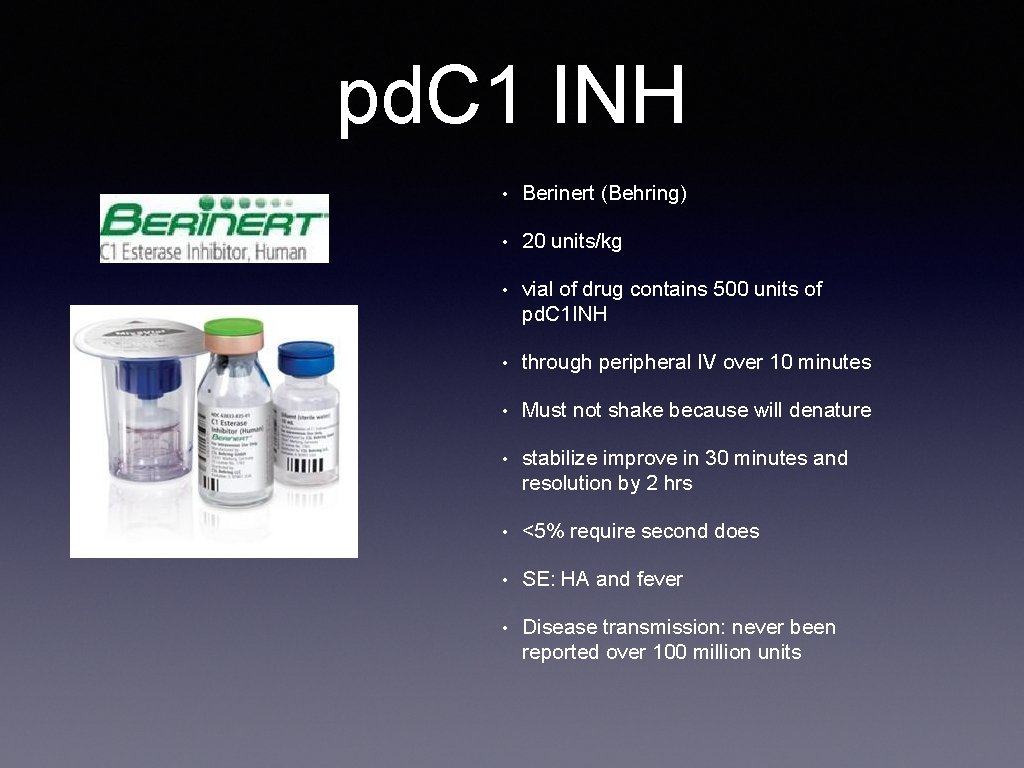
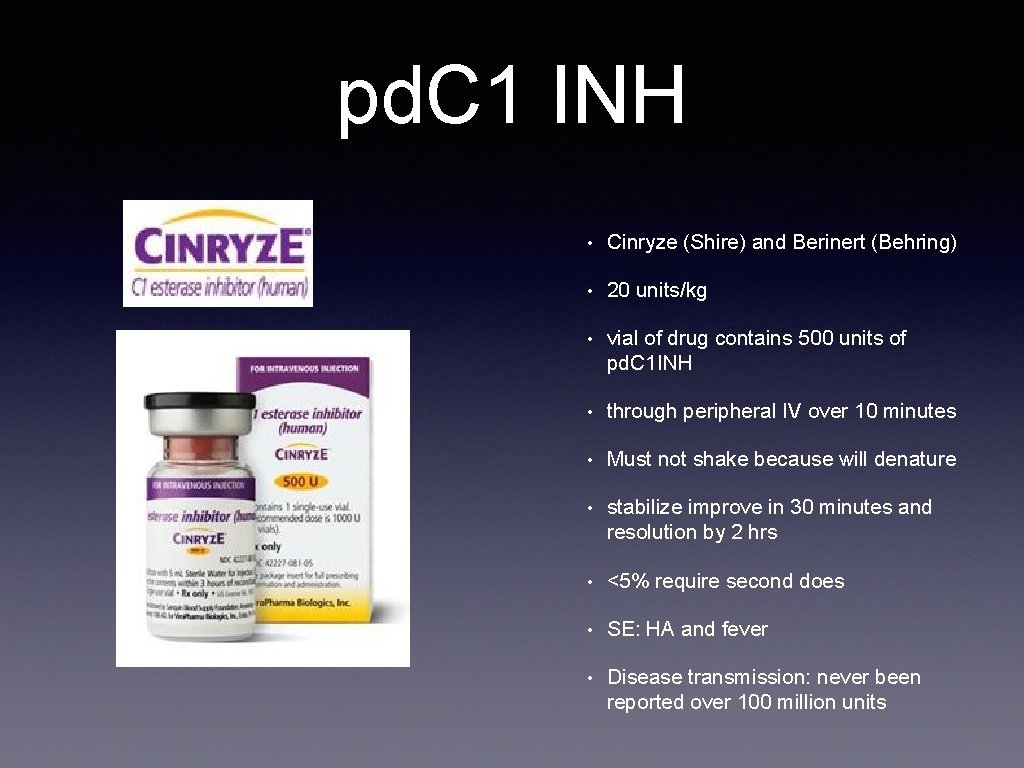
pd C 1 INH • plasma derived C 1 INH concentrate • pooled from human plasma • administer IV • best studied off all the C 1 INH • two types: Cinryze (Shire) and Berinert (Behring)

Plasma Derived C 1 INH
pd C 1 INH • routine prophylaxis against angioedema attacks in adolescent and ddults (cinryze) • treatment of acute abdominal facial or laryngeal attacked of HAE(Berinert)
Traditional place in practice • • Prophylaxis • Has been well established • Can be administered by HC provider in clinic/home or by the patient Treatment • for acute attack in the ED • Cinryze is FDA approvedment for treatment • Dosing 1000 units IV over 10 minutse. ay give second doses 60 mints later • 20 units /kg IV at rate of 4 ml/min
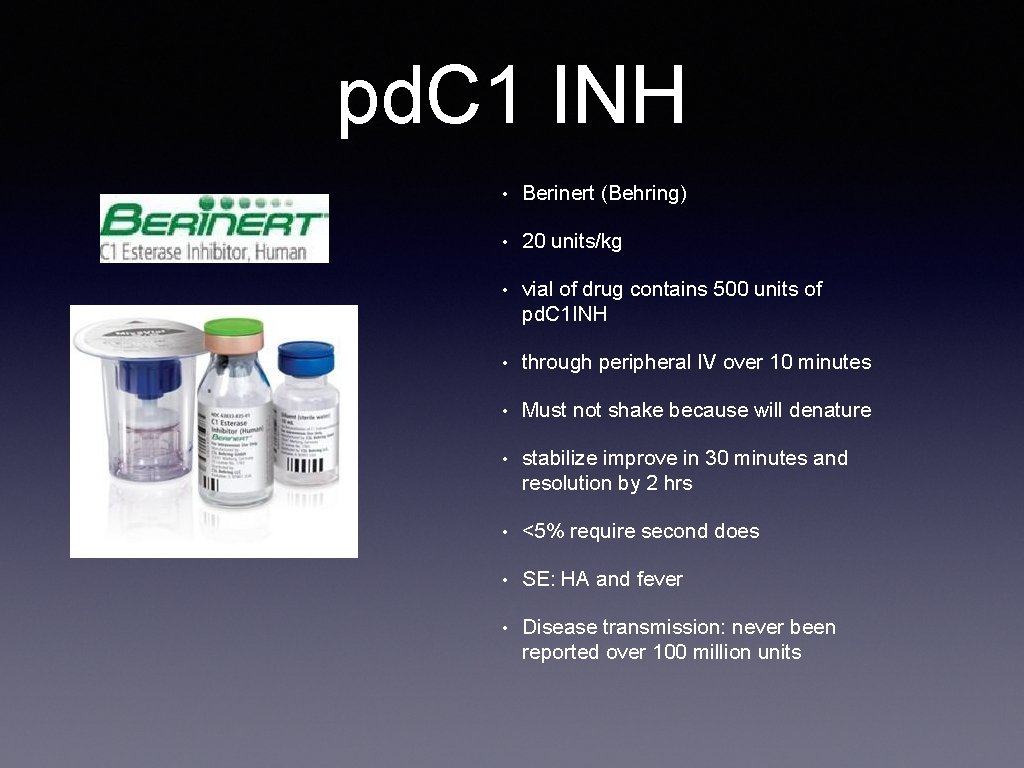
pd. C 1 INH • Berinert (Behring) • 20 units/kg • vial of drug contains 500 units of pd. C 1 INH • through peripheral IV over 10 minutes • Must not shake because will denature • stabilize improve in 30 minutes and resolution by 2 hrs • <5% require second does • SE: HA and fever • Disease transmission: never been reported over 100 million units
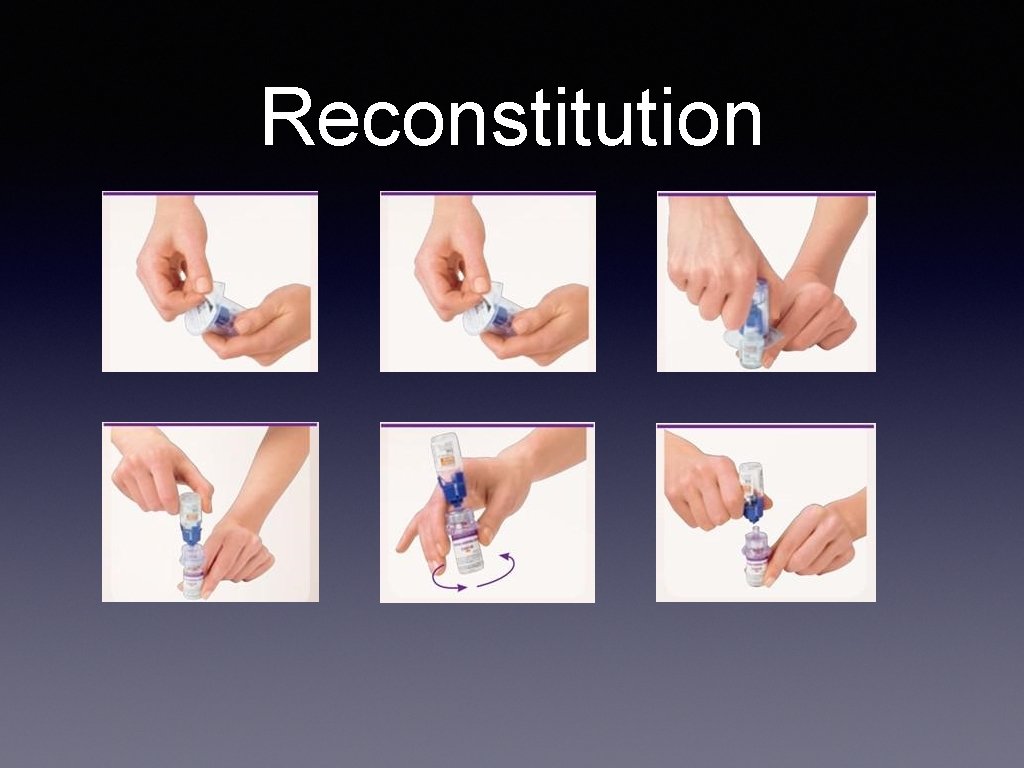
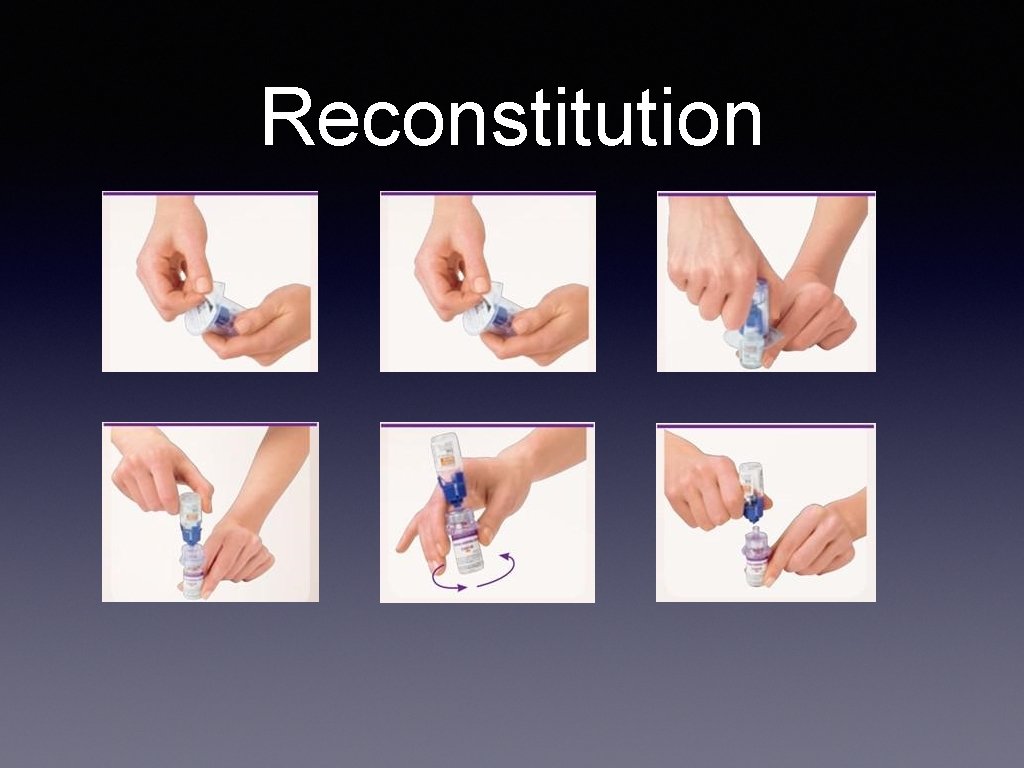
Reconstitution
pd. C 1 INH • Cinryze (Shire) and Berinert (Behring) • 20 units/kg • vial of drug contains 500 units of pd. C 1 INH • through peripheral IV over 10 minutes • Must not shake because will denature • stabilize improve in 30 minutes and resolution by 2 hrs • <5% require second does • SE: HA and fever • Disease transmission: never been reported over 100 million units
Dosing & Administration • For IV use only • Can be given IV push or IV drip over 10 min • administer within 3 hrs of reconstitution • Prophylaxis (Cinryze): 1000 units IV over 10 minutes Q 3 -4 days • Acute attack (Berinert): 20 units /kg IV at rate of 4 ml/min
Adverse Effects • Common • Headaches (7 -28%) • Nausea (1. 8% -18%) • Rash 3. 5% -10% • serious: hypersensitivity, DVT, MI, PE
Precautions • Hypersensitivity reactions can occur • Thrombotic events have been reports in high dose pd C 1 INH • Theoretical risk of transmission infectious agenst, e. g. HIV, HCV, CJD, etc
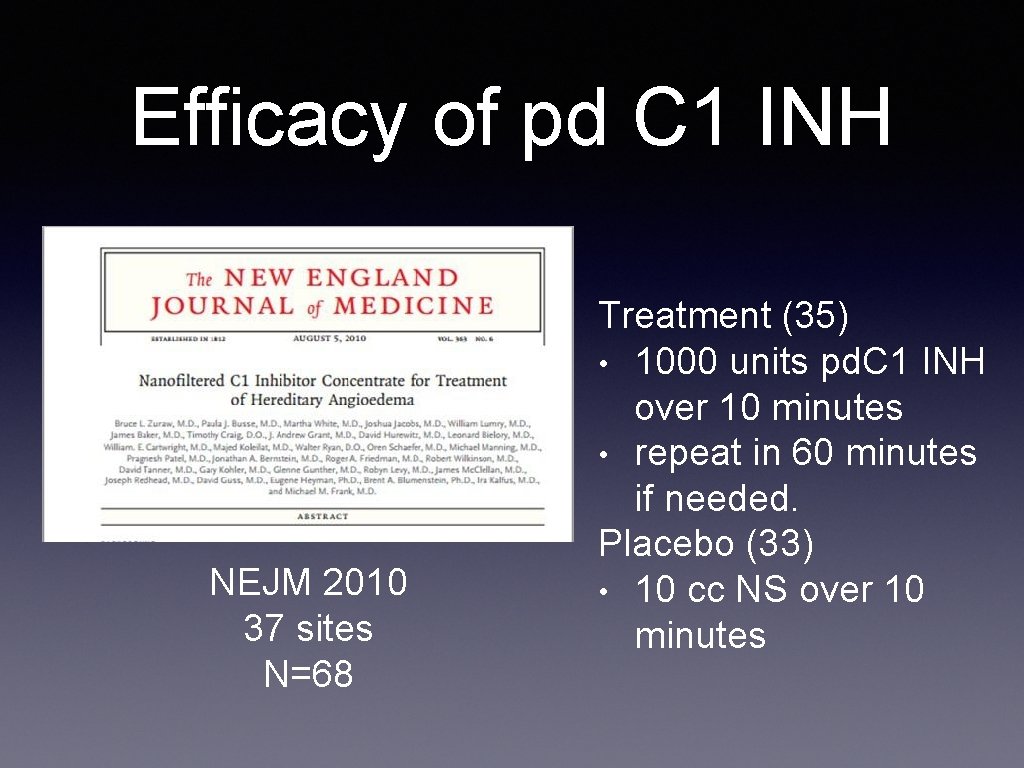
Efficacy of pd C 1 INH NEJM 2010 37 sites N=68 Treatment (35) • 1000 units pd. C 1 INH over 10 minutes • repeat in 60 minutes if needed. Placebo (33) • 10 cc NS over 10 minutes
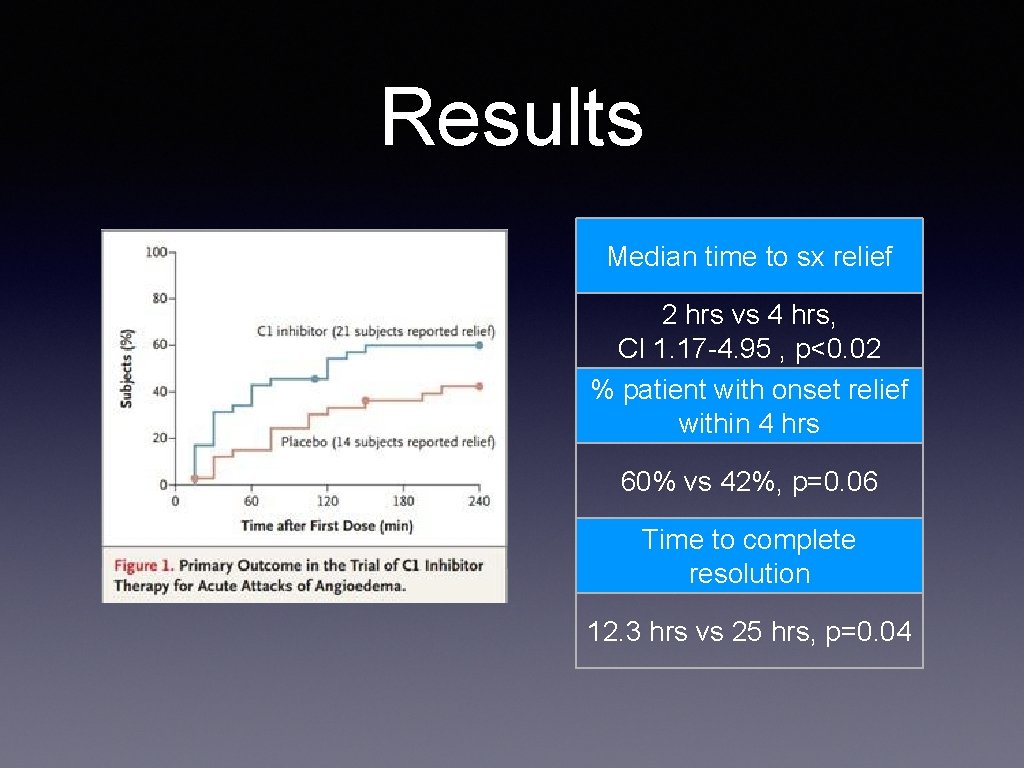
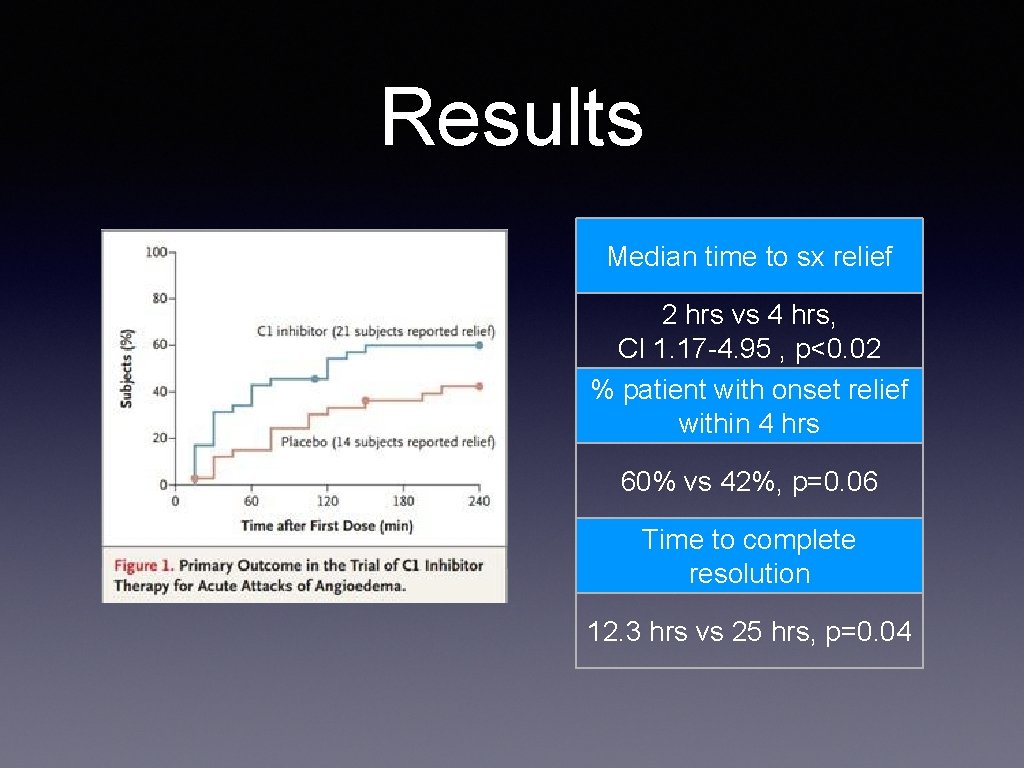
Results Median time to sx relief 2 hrs vs 4 hrs, CI 1. 17 -4. 95 , p<0. 02 % patient with onset relief within 4 hrs 60% vs 42%, p=0. 06 Time to complete resolution 12. 3 hrs vs 25 hrs, p=0. 04
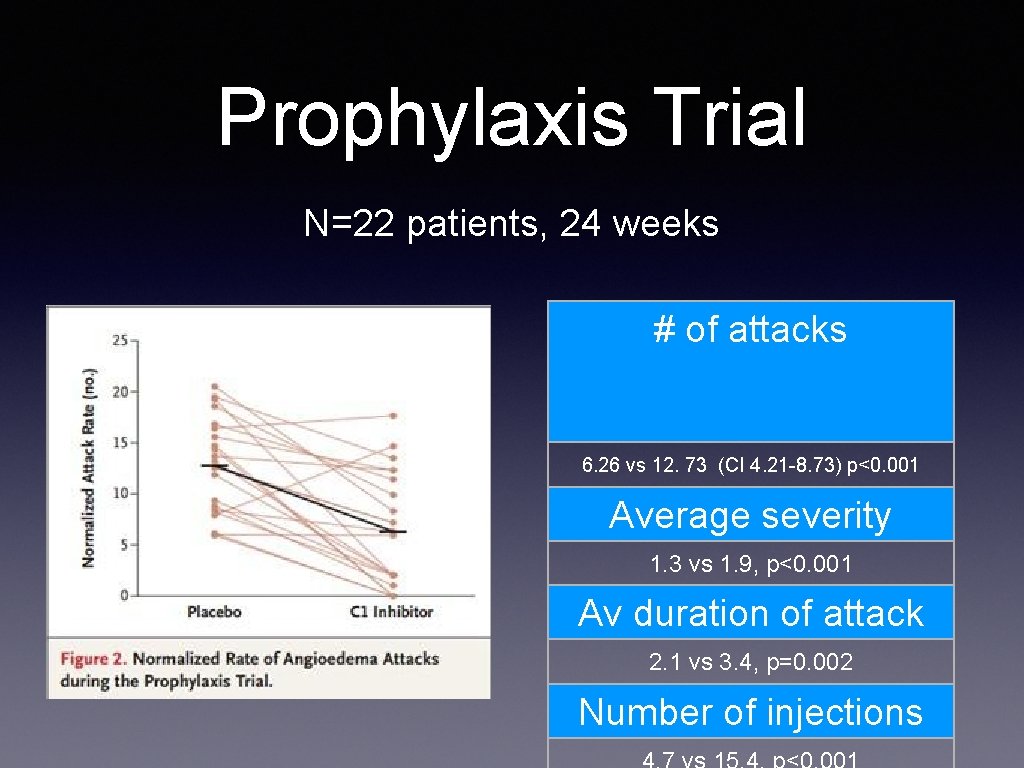
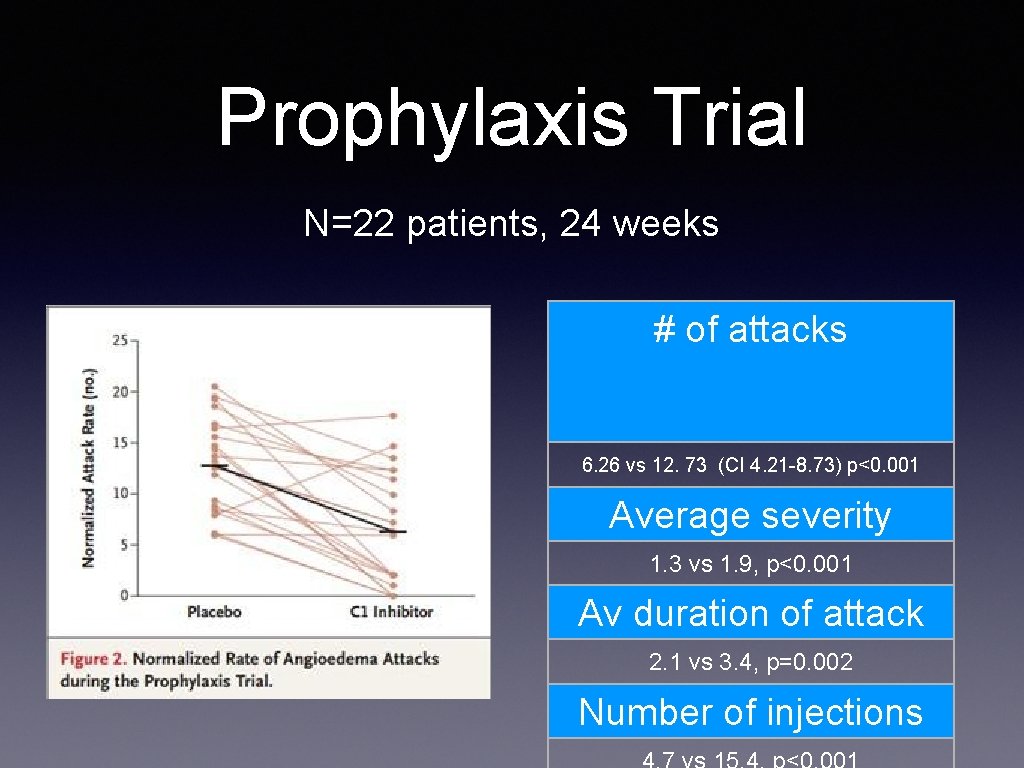
Prophylaxis Trial N=22 patients, 24 weeks # of attacks 6. 26 vs 12. 73 (CI 4. 21 -8. 73) p<0. 001 Average severity 1. 3 vs 1. 9, p<0. 001 Av duration of attack 2. 1 vs 3. 4, p=0. 002 Number of injections
Haegarda • pd C 1 INH SQ for prophylaxis by Behring • Home injections, FDA approved 2017 • pasteurized, lyophilized from pools of human plasma • N=90, 40 IU/kg or 60 IU/kg twice weekly • SE: injection site, hypersensitivity, nasopharngitis, dizziness
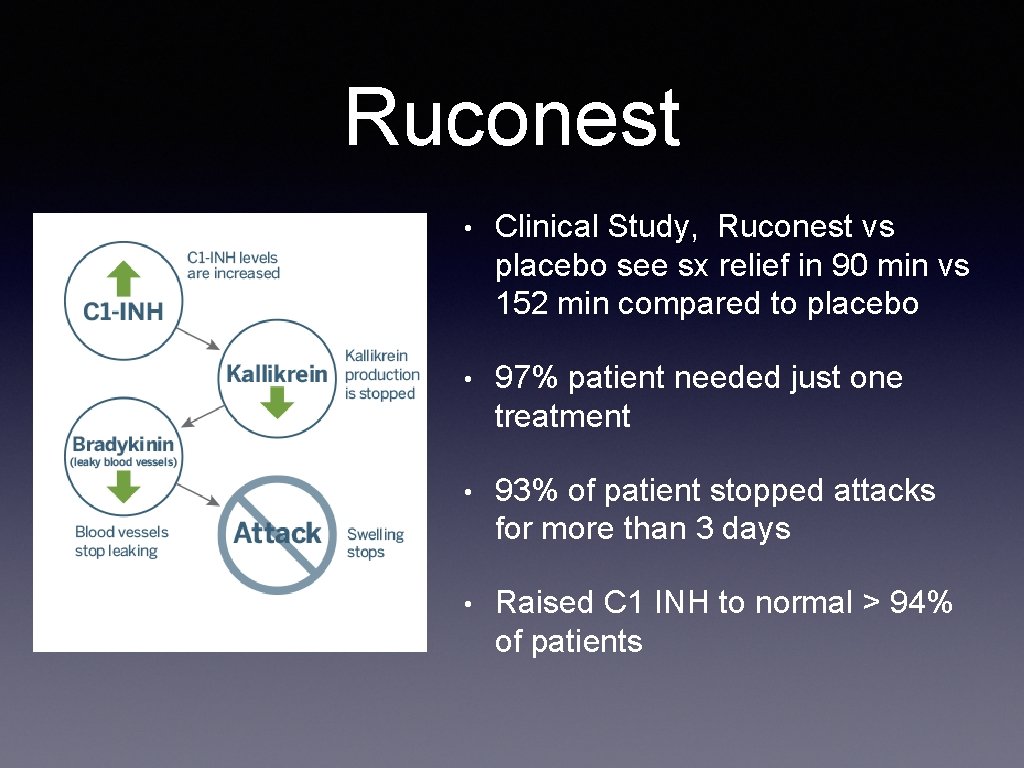
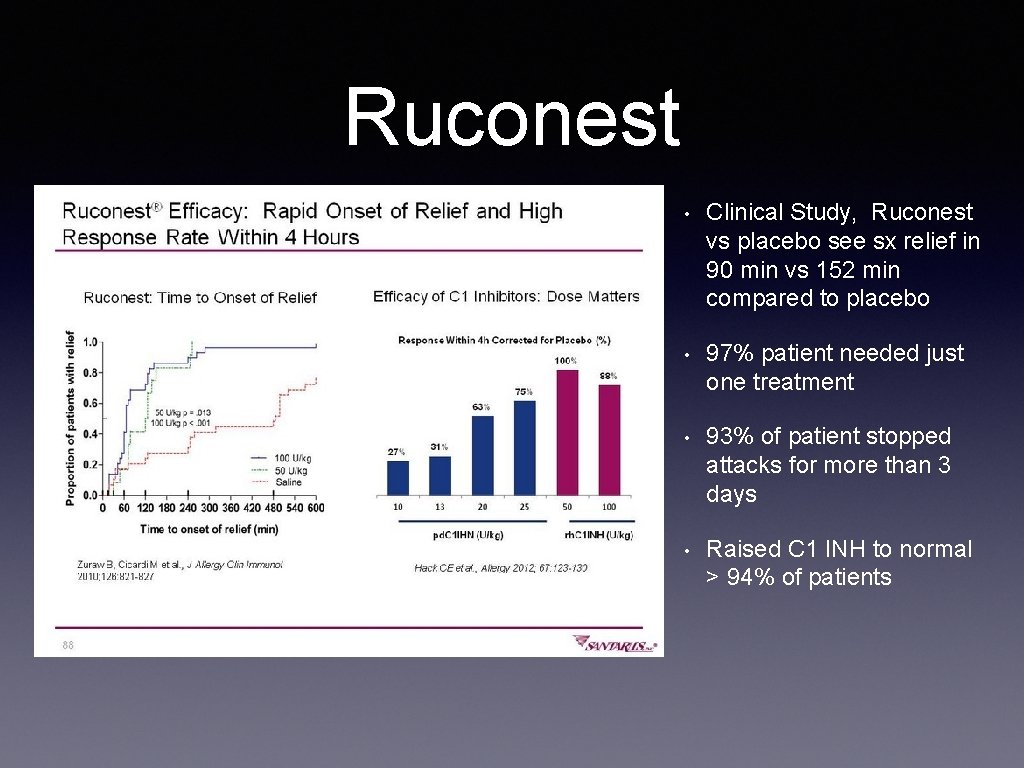
Recombinant C 1 INH • Ruconest became available in 2014 FDA approved for acute attacks in adolescents and adults (not for <13 years old) • milk of transgenic rabbits • plasma free so no risks of transmission of virus • Same activity but shorter half life • Dose: 50 units/kg (rounded up to the nearest vial ) IV • Vial: contains 2100 units • May repeat second dose, max dose is 4200 units • Reconstitute with sterile water, Inject in peripheral IV over 5 min • SE: HA, N, diarhea. Don’t given if Rabbit allergy • Never compared head to head with pd C 1 INH

Recombinant C 1 INH 60 min prior 4 hrs 60 min 2 hrs 8 hrs 24 hrs median time of onset 75 to 90 minutes
Ruconest • Clinical Study, Ruconest vs placebo see sx relief in 90 min vs 152 min compared to placebo • 97% patient needed just one treatment • 93% of patient stopped attacks for more than 3 days • Raised C 1 INH to normal > 94% of patients
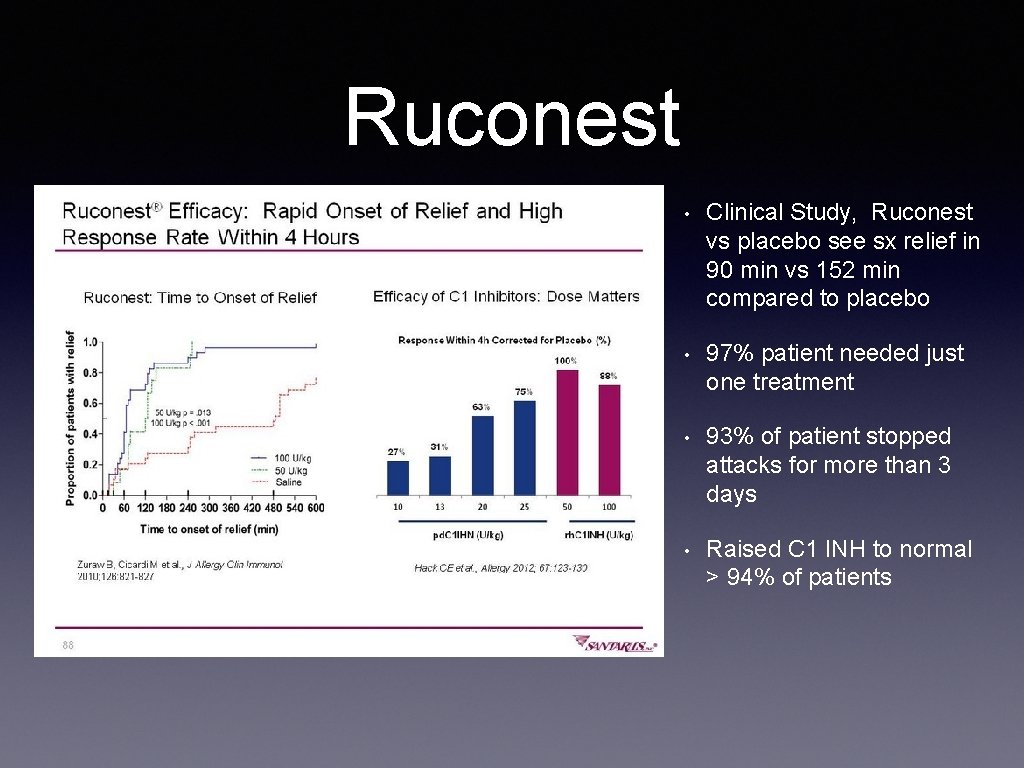
Ruconest • Clinical Study, Ruconest vs placebo see sx relief in 90 min vs 152 min compared to placebo • 97% patient needed just one treatment • 93% of patient stopped attacks for more than 3 days • Raised C 1 INH to normal > 94% of patients
Recombinant C 1 INH • SE: • headache 9% • Nausea 2% • Diarrhea 2% • may cause anaphylaxis, rabbit allergy • pregnancy category B
Icatibant • Bradykinin receptor antagonist by Firazyr, • Available in 2011 (patient >18 yo) • Dose: 30 mg, given SQ slowly in abdomen • can be self administered • A second injection may be given after 6 hrs, a third as well. Max 3 does in 24 hrs. • SE: pain at injection site, Nausea, GI colic, fever • Contraindication: unstable angina because reduce coronary blood flow in animal studies
Ecallantide • Kaliikrein inhibitor blocks the production of bradykinin by inhibiting kalidrein • Genetically engineered in yeast, Pichia Pastoris • FDA approved in 2008 (age >12) • 3 placebo controlled studies showed Ecallantide more than placebo in improving sx • anaphylaxis reported in 2 -3% in clinical trials • SQ injection Langhurt H. Lancet. 2012: 379, 474 -481
Ecallantide • Adult dose 30 mg, comes in 10 mg vials • SQ injection so more convienet: three injection separate areas: and, upper arm, and thigh • anatomic distant from the site of angioedema • A second dose may be given 1 hr to 24 hrs after the first • Not recommended outside a hospital given anaphylaxis
Second Line Therapy • Plasma • Two types: solvent/detergent treated plasma vs FFP • S/D plasma preferred because lower risk of viral transmission • Dose: 2 units of plasma, may repeat every 2 -4 hrs until improvement • comorbid condition: 10 -15 ml/kg because risk of fluid overload • No studies: effectiveness is suggested by case reports • Plasma could theoretically make things worse because has prekallikrein and HMW kininogen • risk: disease transmission S/D treatment inactivates enveloped viruses (HIV, HTLV, HBV, HCV, but not prions or nonenveloped viruses • FFP is pooled from single donor and they undergo testing
Treatment @ home • C 1 INH concentrate (plasma derived or recombinant) • given IV • Icatibant (bradykinin antagonist) SQ int • Ecallantide: three SQ injection by trained nurse at home
Testing Family • If the diagnosis is made, testing should be done of children, parents and siblings
“So if you don’t know, now you know” Notorious BIG via the Broadway Musical Hamilton