HEPATITIS Dr FERDA ZKAN Objectives and Aim To
HEPATITIS Dr. FERDA ÖZKAN
Objectives and Aim To learn the types of inflammatory diseases of liver n To learn the inflammatory changes in liver n
Inflammatory diseases n n n Viral Hepatitis Autoimmune Hepatitis Fulminant Hepatitis Postnecrotic Cirrhosis Liver Abscesses. Secondary infections: ¨ miliary tuberculosis, ¨ malaria, ¨ staphylococcal bacteremia, ¨ the salmonellosis, ¨ candida, n ¨ amebiasis.
Viral Hepatitis n Viral Hepatitis: ¨ Specific – Hepatitis A, B, C, D, E, & others ¨ Systemic - CMV, EBV, yellow fever.
n Infection of the liver caused by a small group of viruses having a particular affinity for the liver. n However, the anatomic pathology is generally similar. n Systemic viral infections ¨ (1) Infectious mononucleosis (Epstein-Barr virus), which may cause a mild hepatitis during the acute phase; ¨ (2) Cytomegalovirus, particularly in the newborn or immunosuppressed patient; ¨ (3) Yellow fever, which has been a major and serious cause of hepatitis in tropical countries.
Patterns of Viral Hepatitis Carrier state / Asymptomatic phase n Acute hepatitis n Chronic Hepatitis n ¨ Chronic Persistent Hepatitis (CPH) ¨ Chronic Active Hepatitis (CAH) Fulminant hepatitis n Cirrhosis n
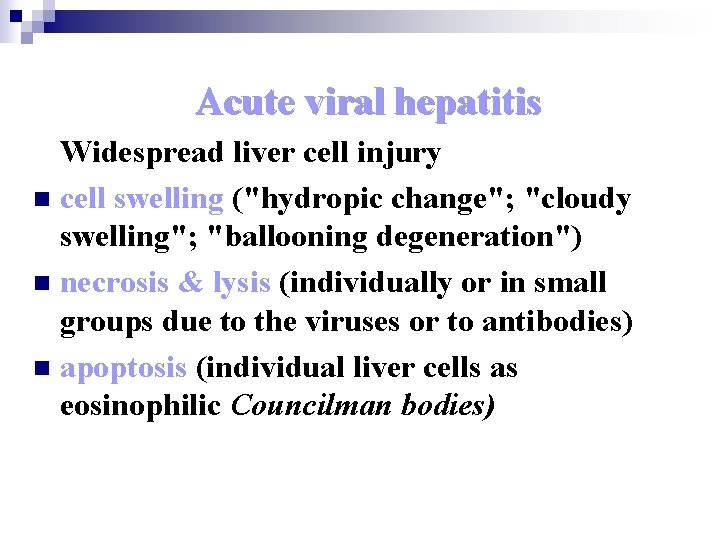
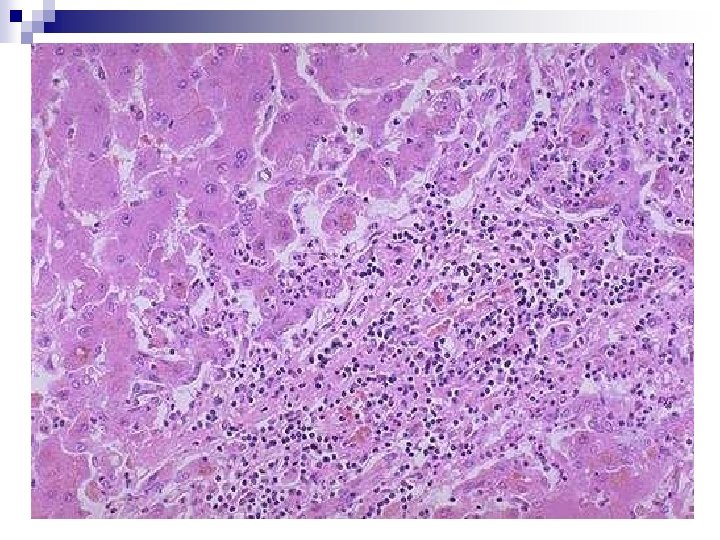
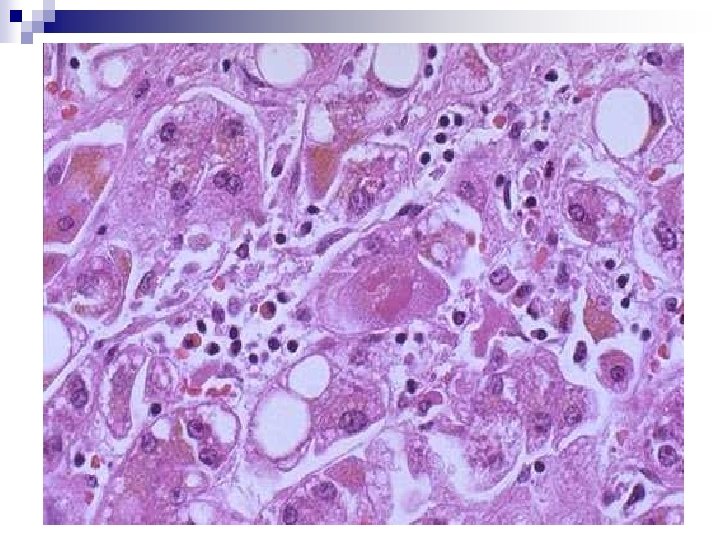
Acute viral hepatitis Widespread liver cell injury n cell swelling ("hydropic change"; "cloudy swelling"; "ballooning degeneration") n necrosis & lysis (individually or in small groups due to the viruses or to antibodies) n apoptosis (individual liver cells as eosinophilic Councilman bodies)
hypertrophy/hyperplasia of Kupffer cells n inflammatory cells (mostly lymphocytes, macrophages) in the portal areas, and some among the hepatocytes, n portal inflammation and cholestasis n hepatocyte regeneration (purple cells with big nuclei; during the recovery phase). n
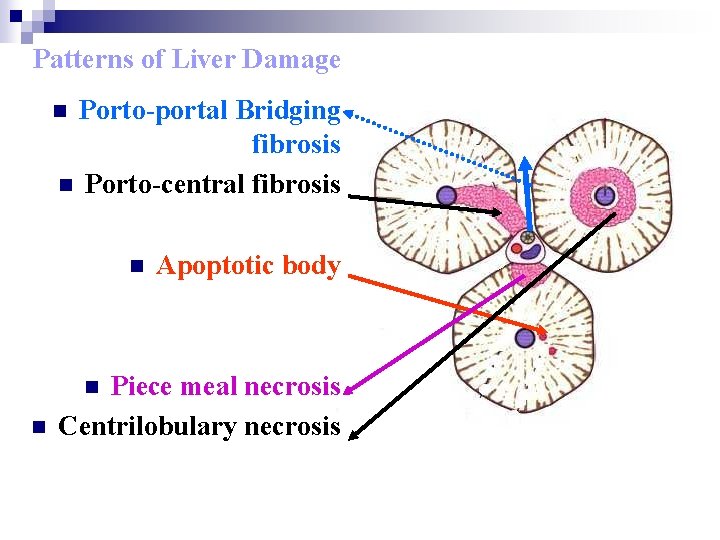
Patterns of Liver Damage Porto-portal Bridging fibrosis n Porto-central fibrosis n n Piece meal necrosis Centrilobulary necrosis n n Apoptotic body
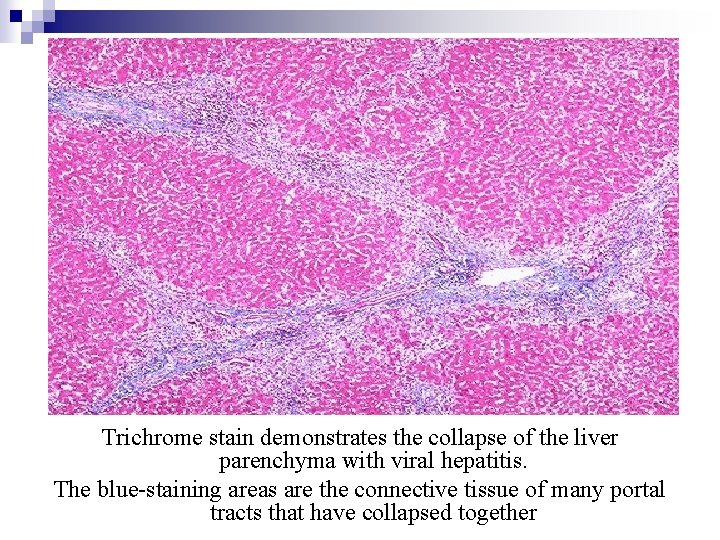
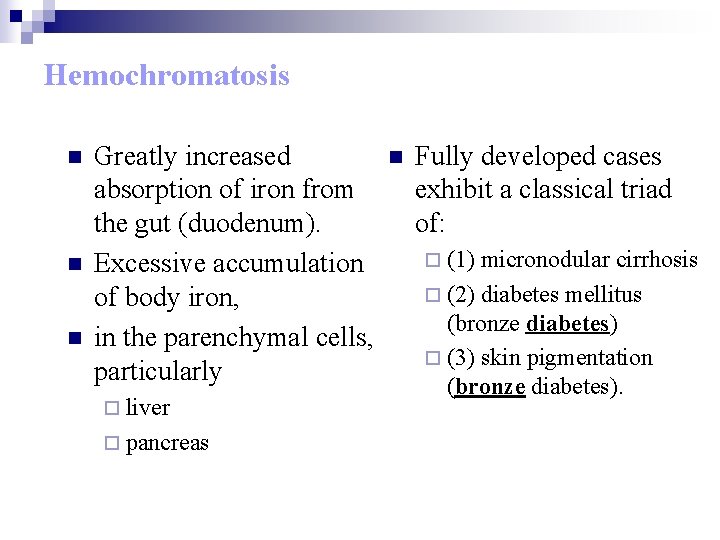
Trichrome stain demonstrates the collapse of the liver parenchyma with viral hepatitis. The blue-staining areas are the connective tissue of many portal tracts that have collapsed together
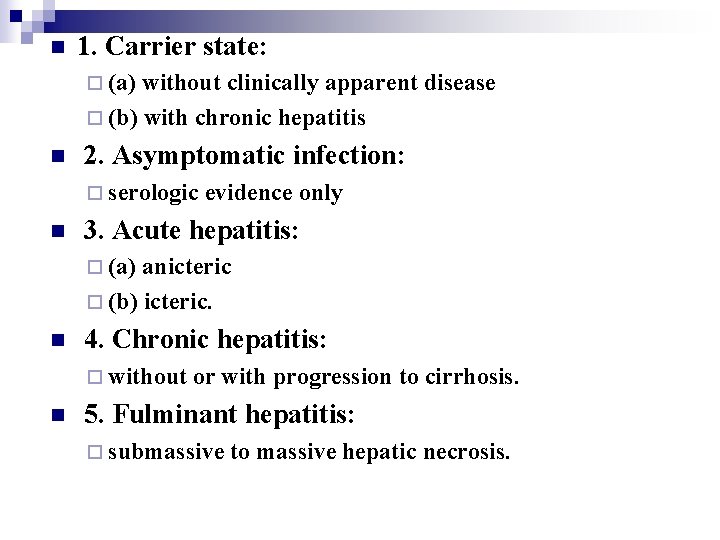
n 1. Carrier state: ¨ (a) without clinically apparent disease ¨ (b) with chronic hepatitis n 2. Asymptomatic infection: ¨ serologic n evidence only 3. Acute hepatitis: ¨ (a) anicteric ¨ (b) icteric. n 4. Chronic hepatitis: ¨ without n or with progression to cirrhosis. 5. Fulminant hepatitis: ¨ submassive to massive hepatic necrosis.
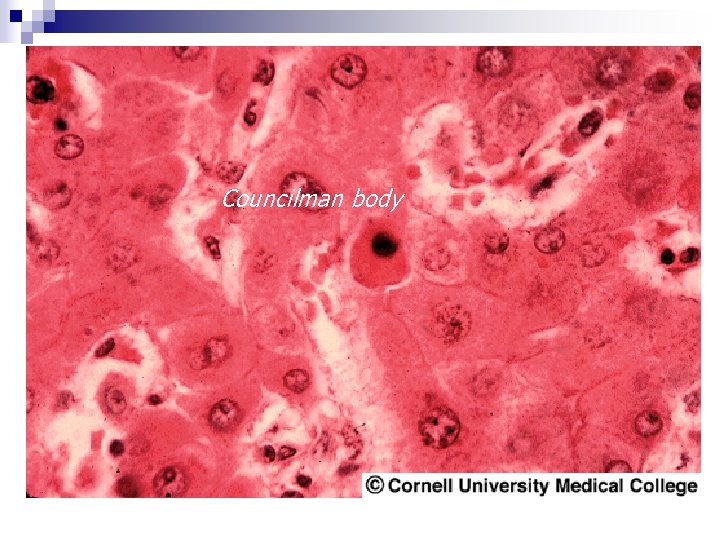
Councilman body
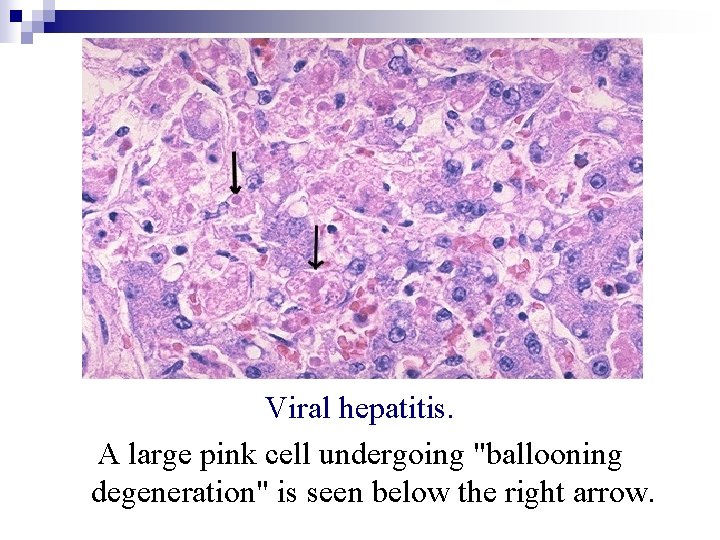
Viral hepatitis. A large pink cell undergoing "ballooning degeneration" is seen below the right arrow.
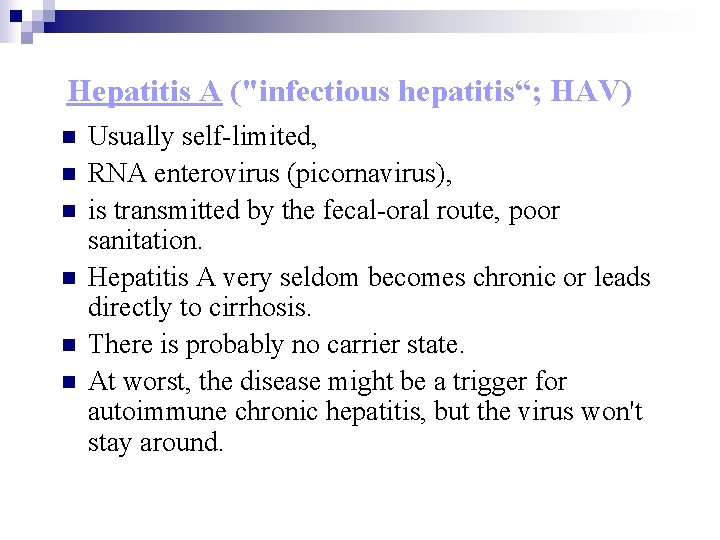
Hepatitis A ("infectious hepatitis“; HAV) n n n Usually self-limited, RNA enterovirus (picornavirus), is transmitted by the fecal-oral route, poor sanitation. Hepatitis A very seldom becomes chronic or leads directly to cirrhosis. There is probably no carrier state. At worst, the disease might be a trigger for autoimmune chronic hepatitis, but the virus won't stay around.
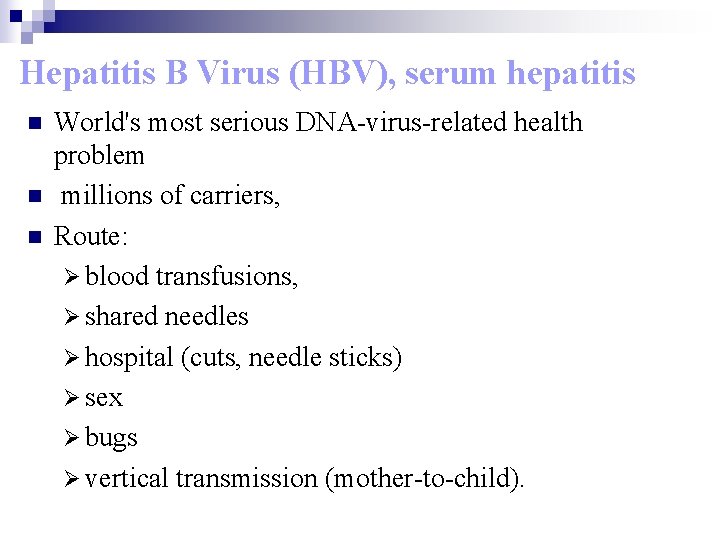
Hepatitis B Virus (HBV), serum hepatitis n n n World's most serious DNA-virus-related health problem millions of carriers, Route: Ø blood transfusions, Ø shared needles Ø hospital (cuts, needle sticks) Ø sex Ø bugs Ø vertical transmission (mother-to-child).
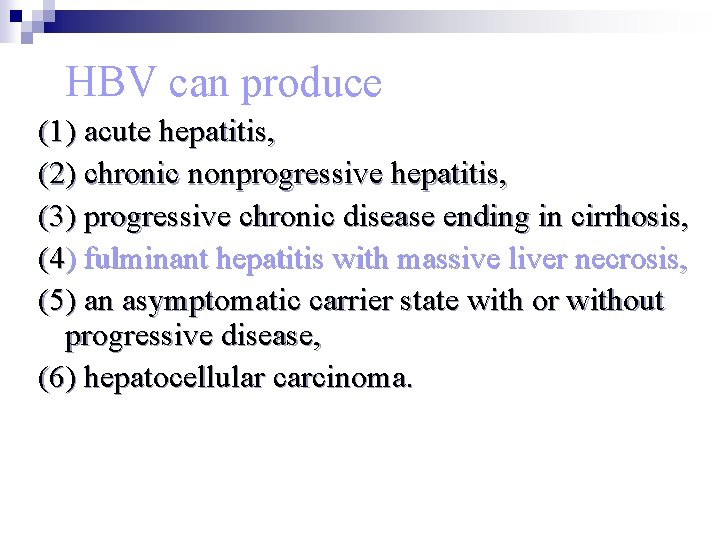
HBV can produce (1) acute hepatitis, (2) chronic nonprogressive hepatitis, (3) progressive chronic disease ending in cirrhosis, (4) fulminant hepatitis with massive liver necrosis, (5) an asymptomatic carrier state with or without progressive disease, (6) hepatocellular carcinoma.
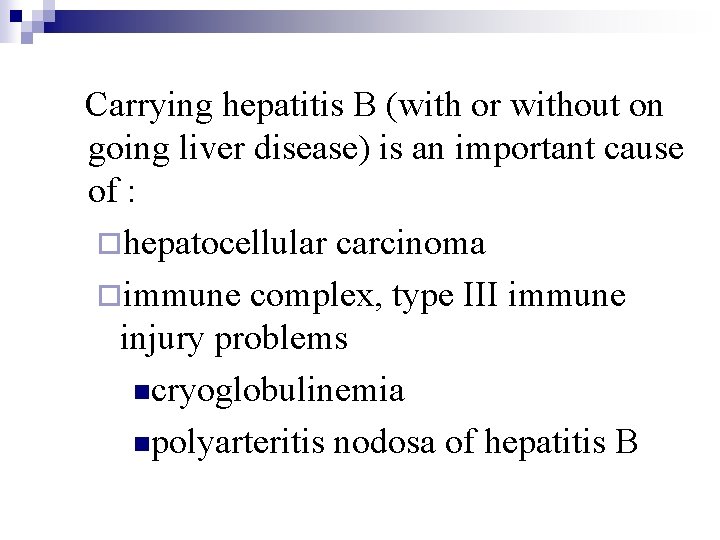
Carrying hepatitis B (with or without on going liver disease) is an important cause of : ¨hepatocellular carcinoma ¨immune complex, type III immune injury problems ncryoglobulinemia npolyarteritis nodosa of hepatitis B
Symptoms begin when T-cells are activated with HBs. Ag and HBc n start killing the hepatocytes n Histopathologists find T-cytotoxic cells where the hepatocytes are dying. n The only surviving liver cells are the ones that won't continue making viruses, and these replenish the liver. n
Hepatitis C Virus (non-A, non-B hepatitis) n n n Route: ¨ intravenous drug abusers (50 to 90%) ¨ blood transfusion (55 to 85%) ¨ hemodialysis (8 to 24%) ¨ Hospitals & dental clinics (cuts, needle sticks) ¨ vertical transmission (mother-to-child) Patients with unexplained cirrhosis and hepatocellular carcinoma have anti-HCV prevalence rates exceeding 50% In contrast to HBV, HCV has a high rate of progression to chronic disease and eventual cirrhosis, exceeding 70%
n Hallmarks: ¨persistent infection, ¨chronic hepatitis, ¨cirrhosis.
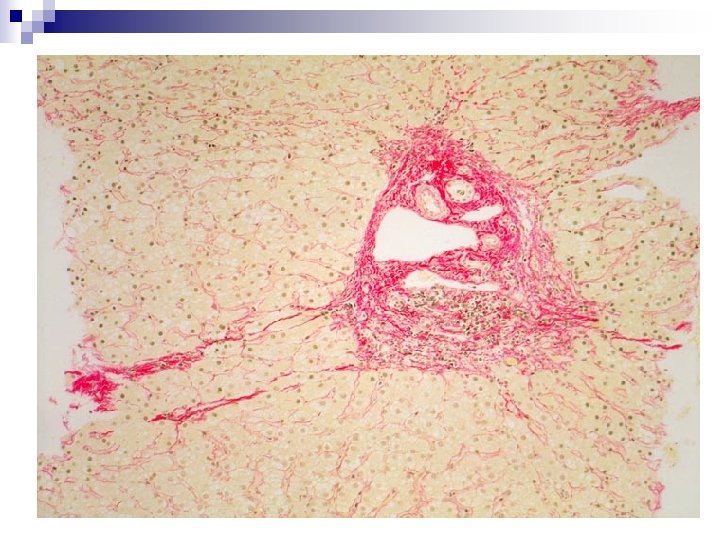
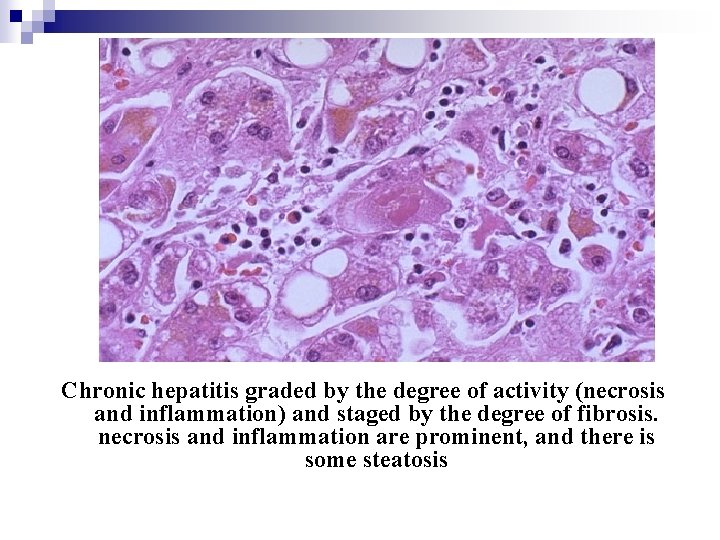
Chronic hepatitis graded by the degree of activity (necrosis and inflammation) and staged by the degree of fibrosis. necrosis and inflammation are prominent, and there is some steatosis
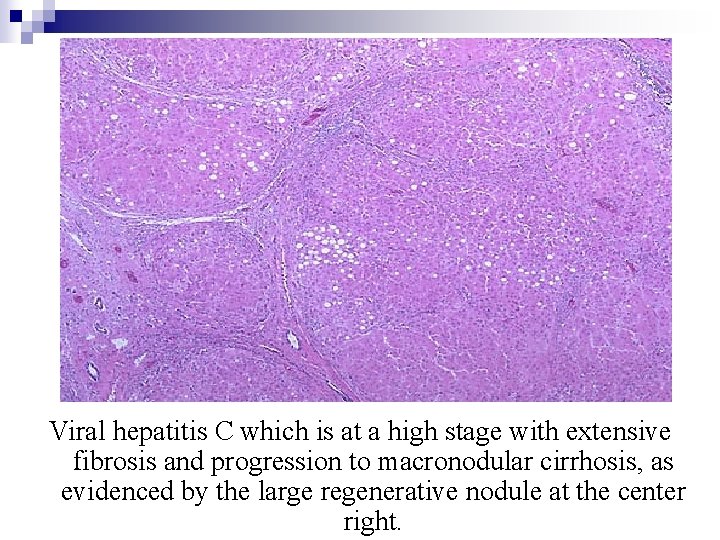
Viral hepatitis C which is at a high stage with extensive fibrosis and progression to macronodular cirrhosis, as evidenced by the large regenerative nodule at the center right.
Hepatitis D (HDV; hepatitis delta virus) Common in homosexual men and iv drugabusers. n 1. Acute coinfection: occurs following exposure to serum containing both HDV and HBV. n 2. Superinfection of a chronic carrier: HBV with a new inoculum of HDV. n ¨ The carrier may have been previously “healthy” or may have had underlying chronic hepatitis.
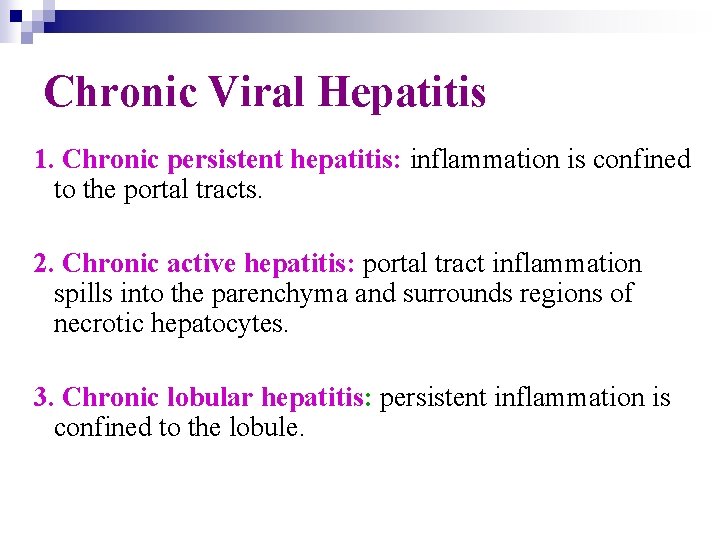
Chronic Viral Hepatitis 1. Chronic persistent hepatitis: inflammation is confined to the portal tracts. 2. Chronic active hepatitis: portal tract inflammation spills into the parenchyma and surrounds regions of necrotic hepatocytes. 3. Chronic lobular hepatitis: persistent inflammation is confined to the lobule.
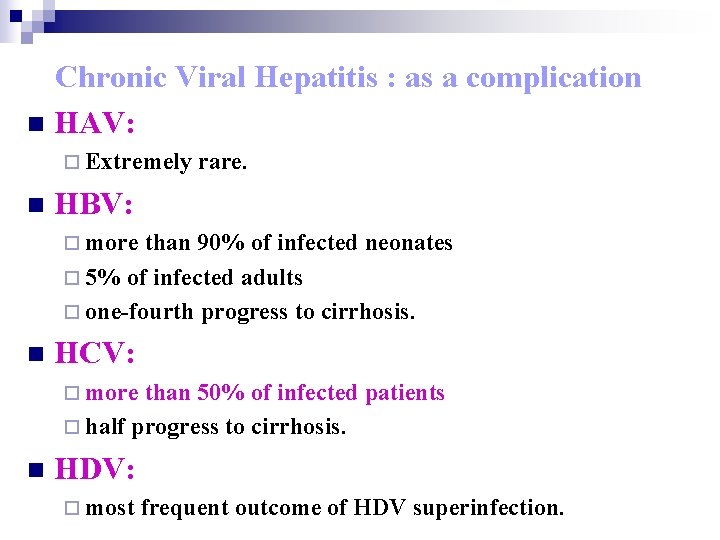
Chronic Viral Hepatitis : as a complication n HAV: ¨ Extremely n rare. HBV: ¨ more than 90% of infected neonates ¨ 5% of infected adults ¨ one-fourth progress to cirrhosis. n HCV: ¨ more than 50% of infected patients ¨ half progress to cirrhosis. n HDV: ¨ most frequent outcome of HDV superinfection.
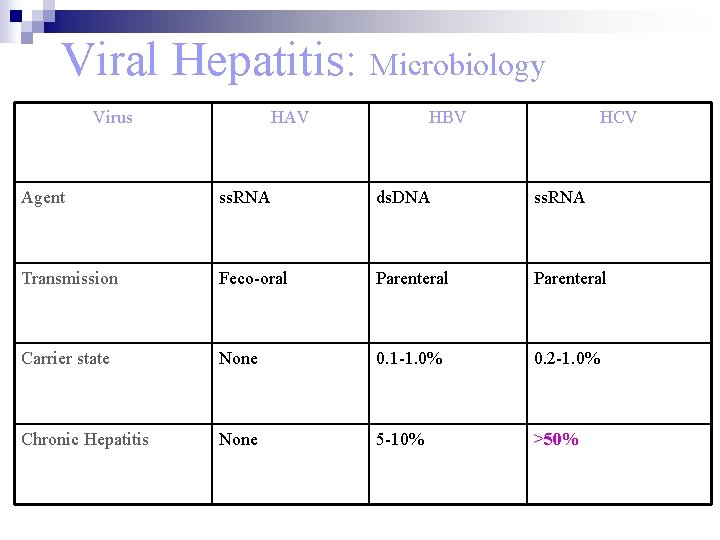
Viral Hepatitis: Microbiology Virus HAV HBV HCV Agent ss. RNA ds. DNA ss. RNA Transmission Feco-oral Parenteral Carrier state None 0. 1 -1. 0% 0. 2 -1. 0% Chronic Hepatitis None 5 -10% >50%
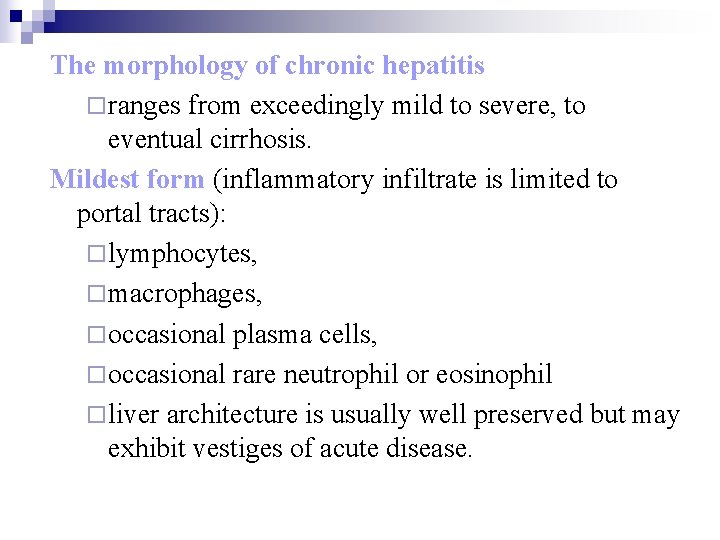
The morphology of chronic hepatitis ¨ ranges from exceedingly mild to severe, to eventual cirrhosis. Mildest form (inflammatory infiltrate is limited to portal tracts): ¨ lymphocytes, ¨ macrophages, ¨ occasional plasma cells, ¨ occasional rare neutrophil or eosinophil ¨ liver architecture is usually well preserved but may exhibit vestiges of acute disease.
Progressive form ¨ Piecemeal necrosis, ¨ the chronic inflammatory infiltrate spills out from portal tracts into adjacent parenchyma, ¨ necrosis of hepatocytes ¨ lobular inflammation with focal necrosis of hepatocytes. n Continued loss of hepatocytes results in ¨ fibrous septum formation, ¨ accompanied by hepatocyte regeneration, ¨ cirrhosis.
Autoimmune (lupoid) Hepatitis without chronic virus infection but with evidence of immune injury n chronic hepatitis cirrhosis n most common autoantibodies against smooth muscle. n Usually features a lot more plasma cells than does viral chronic hepatitis. n
Female predominance (70%), particularly young and perimenopausal women. n The absence of viral serologic markers. n Elevated serum Ig. G levels. n High serum titers of autoantibodies in 80% of cases: n ¨ anti-smooth muscle (SMA), ¨ antinuclear (ANA), ¨ antimitochondrial (AMA), ¨ anti-liver and kidney microsome (LKM) antibodies.
Fulminant Hepatitis n n Hepatic insufficiency progresses from onset of symptoms to hepatic encephalopathy (within 2 to 3 weeks), Drug or chemical toxicity (25 to 30%): ¨ acetaminophen (in suicidal doses), ¨ isoniazid, ¨ antidepressants (particularly monoamine oxidase inhibitors), ¨ halothane, ¨ methyldopa, ¨ mycotoxins (Amanita phalloides).
Fulminant hepatic failure may present with n n n n n jaundice, encephalopathy, fetor hepaticus, coagulopathy and bleeding instability, cardiovascular instability, renal failure, adult respiratory distress syndrome, electrolyte and acid-base disturbances, sepsis.
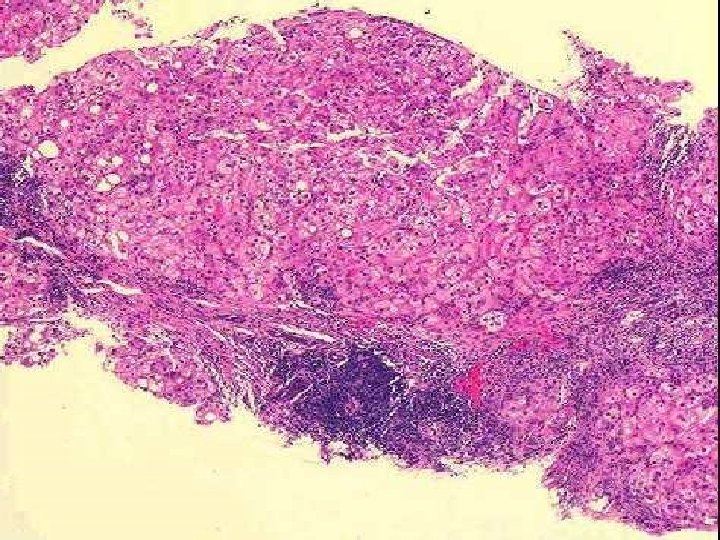
n n n n n Hepatic failure within 2 -3 weeks. Reactivation of chronic or acute hepatitis Massive necrosis, shrinkage, wrinkled Collapsed reticulin network Only portal tracts visible Little or massive inflammation – time More than a week – regenerative activity Cholestasis (blotchy green bile staining) Complete recovery – or - cirrhosis.
Histologically n Necrosis ¨ destroying the central and midzonal regions and sparing the periportal area of the lobule. Complete destruction of contiguous lobules n There may be surprisingly little inflammatory reaction n ¨ except possibly for an increase in lymphocytes, macrophages, ¨ occasional neutrophils within the portal tracts.
n Survivors: ¨ secondary regeneration of hepatocytes (primitive ductules) ¨ Kupffer cell proliferation (laden with lipofuscin and cellular debris) ¨ nodular masses of liver cells ¨ broad bands of scar tissue ¨ postnecrotic cirrhosis.
Postnecrotic Cirrhosis n n n Irregularly sized nodules (some several centimeters in diameter) separated by variable but mostly broad scars. Common causes: ¨ Previous viral infection ¨ Hepatotoxin: n n n phosphorus carbon tetrachloride mushroom poisoning ¨ Drugs: n acetaminophen, n oxyphenisatin, n alpha-methyldopa.
Liver Abscess The organisms reach the liver via n (1) the portal vein, n (2) arterial supply, n (3) ascending infection in the biliary tract (ascending cholangitis), n (4) direct invasion of the liver from a nearby source, n (5) a penetrating injury. n
n n Most abscesses are pyogenic, ¨ The majority of hepatic abscesses used to result from portal spread of intra-abdominal infections: n appendicitis, n diverticulitis, n colitis. Others: ¨ amebic, ¨ echinococcal, ¨ helminthic.
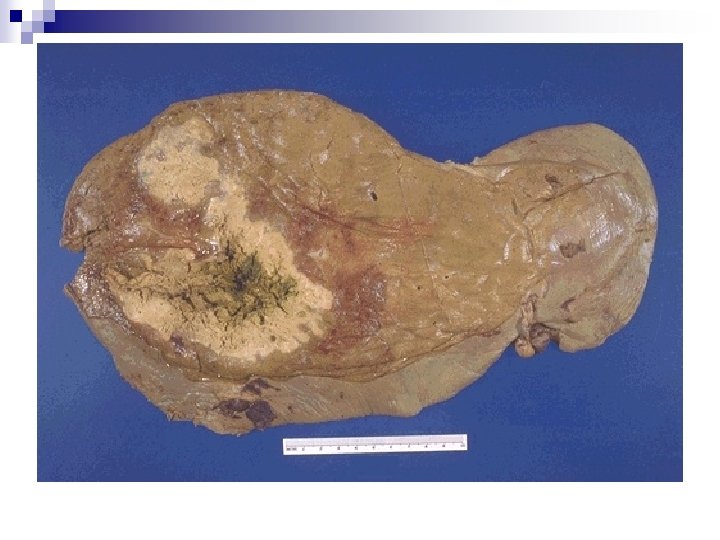
n Biliary abscesses: ¨ usually multiple, ¨ purulent material in adjacent bile ducts. n Pyogenic hepatic abscesses: ¨ Solitary or multiple lesions, n Solitary abscess: direct extension and trauma usually cause a solitary large abscess, n Multiple small abscesses: bacteremic spread through the arterial or portal system tends to produce from millimeters to massive lesions many centimeters in diameter.
Complications Sepsis & Pyemia n Rupture n ¨ Rupture thoracic cavity: empyema n lung abscess. n ¨ Rupture of subcapsular liver abscesses: peritonitis n localized peritoneal abscesses. n
Drug-Induced and Toxin-Induced Liver Disease n n Liver the major drug-metabolizing and drugdetoxifying organ subject to potential damage. Injury may result from ¨ (1) direct toxicity; ¨ (2) hepatic conversion of a xenobiotic to an active toxin; ¨ (3) via immune mechanisms, n usually when the drug or a metabolite acts as a hapten to convert a cellular protein into an immunogen.
n n The injury may be immediate or take weeks to months to develop, presenting only after severe liver damage has developed. The injury may take the form of hepatocyte necrosis, cholestasis, or insidious onset of liver dysfunction. Drug-induced chronic hepatitis is clinically and histologically indistinguishable from chronic viral hepatitis. Exposure to a toxin or therapeutic agent should be included in the differential diagnosis of any form of liver disease.
n Drugs: ¨ Acetaminophen n Chemicals: (paracetamol, ¨ Carbon tetrachloride "Tylenol") overdose ¨ Chloroform ¨ Acetaminophen + alcohol ¨ Phosphorus ¨ Stimulants: Cocaine, Ecstasy & Amphetamine n Nature: ¨ Isoniazid ¨ Mushrooms ¨ Methyldopa n Amanita phalloides (the death ¨ Arsenic (as for syphilis angel) therapy)

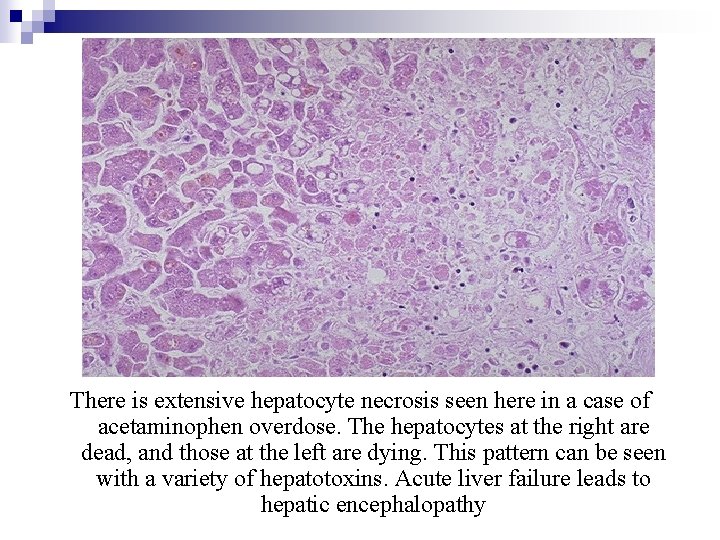
There is extensive hepatocyte necrosis seen here in a case of acetaminophen overdose. The hepatocytes at the right are dead, and those at the left are dying. This pattern can be seen with a variety of hepatotoxins. Acute liver failure leads to hepatic encephalopathy
Alcoholic Liver disease Ethyl alcohol : Common cause of acute/chronic liver disease n Alcoholic Liver disease - Patterns n ¨ Fatty change, ¨ Alcoholic hepatitis (Mallory hyaline bodies) ¨ Alcoholic Hepatic fibrosis ¨ Alcoholic Cirrhosis n All reversible except cirrhosis stage.
Alcoholic Liver Injury: Pathogenesis n n n Diversion of fat & carbohydrate metabolism to alcohol – fat storage. Acetaldehyde – metabolite – hepatotoxic Increased peripheral release of fatty acids. Alcohol stimulates collagen synthesis Inflammation, Portal bridging fibrosis Micronodular cirrhosis.
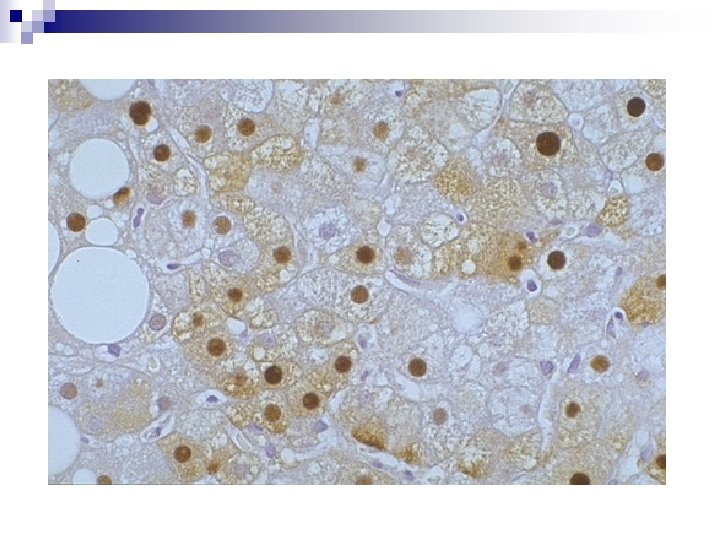
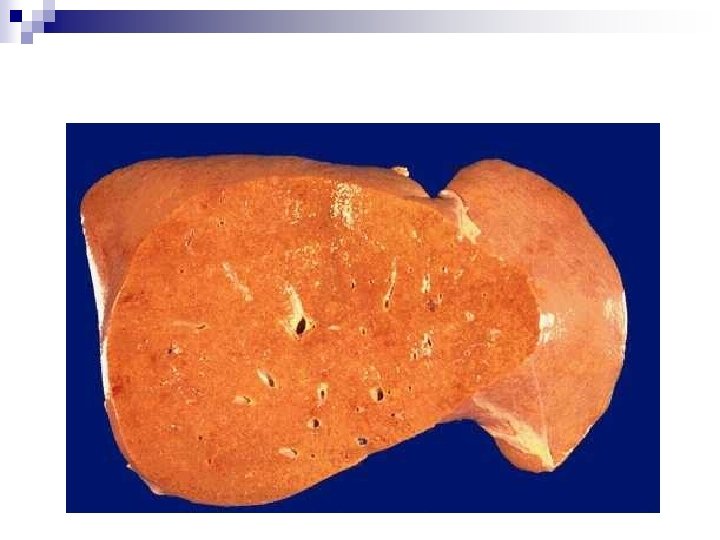
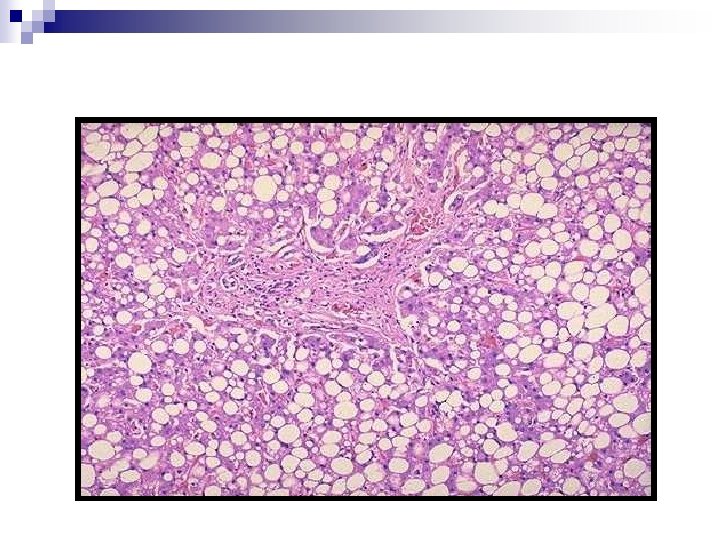
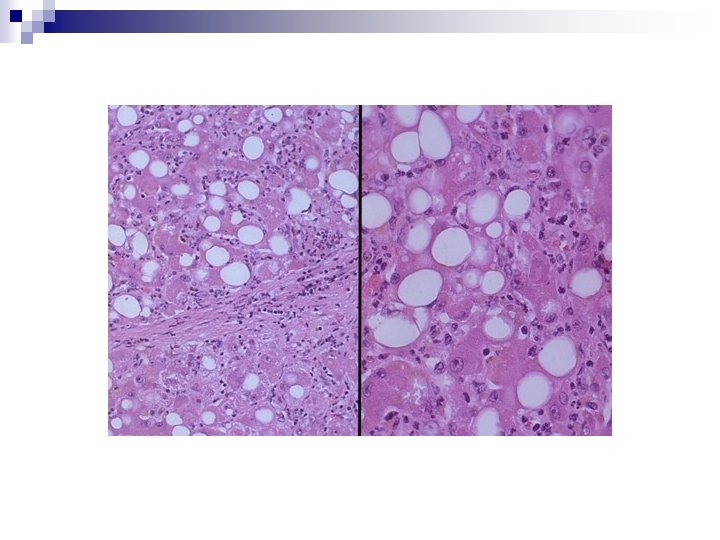
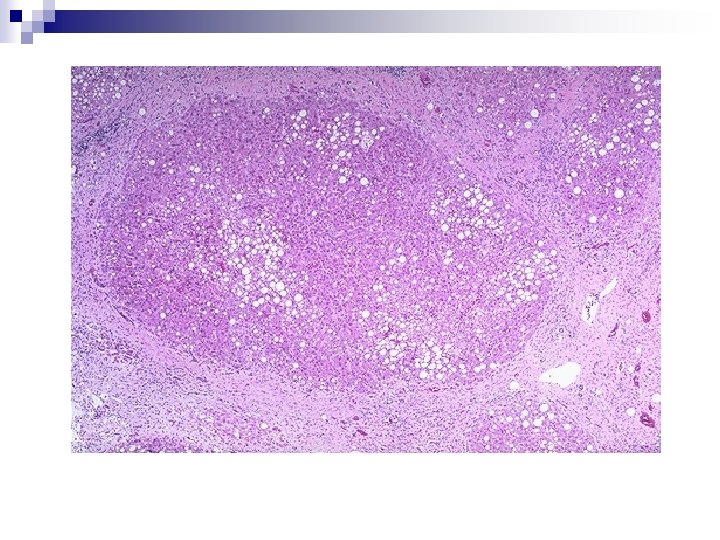
Alcoholic Liver Disease n Alcohol intake: n (1) hepatic steatosis n (2) alcoholic hepatitis and alcoholic hepatic fibrosis (3) cirrhosis small (microvesicular) lipid droplets in hepatocytes Chronic lipid accumulates large clear macrovesicular spaces compressing and displacing the nucleus to the periphery ¨ Moderate n This transformation is initially centrilobular, but in severe cases, it may involve the entire lobule.
Alcoholic steatosis (alcoholic fatty liver) n n n Alcohol hepatocytes make too much fatty acid make it into excess triglyceride instead of burning it can't complex the triglyceride to apolipoproteins can't export the lipoproteins Microvesicular steatosis. Reversible. Microvesicular steatosis (smaller vacuoles, usually several per cell): ¨ Alcoholic fatty liver, ¨ Reye's syndrome, ¨ Problem pregnancies, ¨ Mitochondrial problems ¨ Outdated-tetracycline poisoning.
n Early phase of abuse: ¨ Enlarged (up to 4 to 6 kg), soft, yellow-tan, greasy organ, ¨ little or no fibrosis.
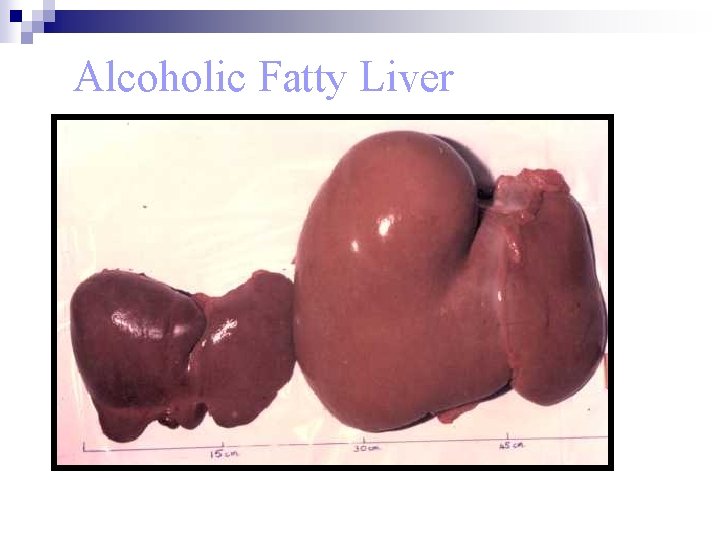
Alcoholic Fatty Liver
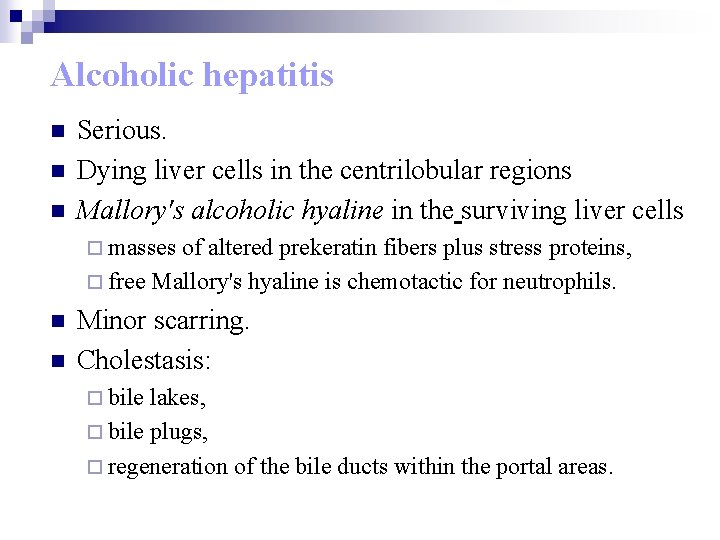
Alcoholic hepatitis n n n Serious. Dying liver cells in the centrilobular regions Mallory's alcoholic hyaline in the surviving liver cells ¨ masses of altered prekeratin fibers plus stress proteins, ¨ free Mallory's hyaline is chemotactic for neutrophils. n n Minor scarring. Cholestasis: ¨ bile lakes, ¨ bile plugs, ¨ regeneration of the bile ducts within the portal areas.
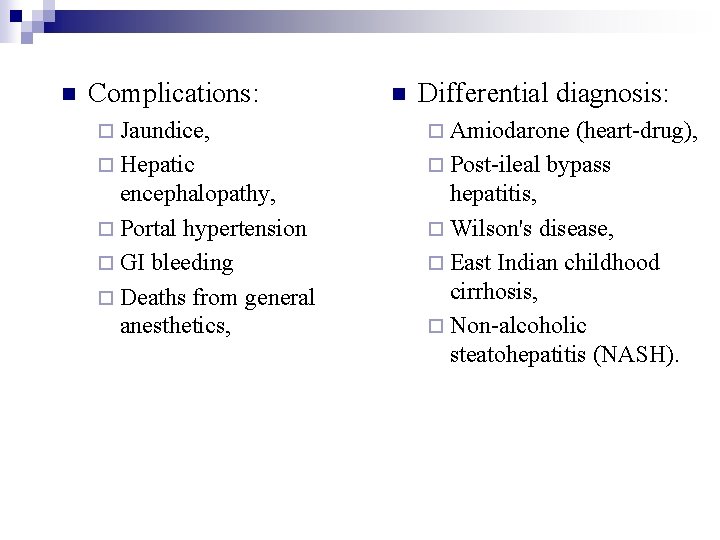
n Complications: ¨ Jaundice, ¨ Hepatic encephalopathy, ¨ Portal hypertension ¨ GI bleeding ¨ Deaths from general anesthetics, n Differential diagnosis: ¨ Amiodarone (heart-drug), ¨ Post-ileal bypass hepatitis, ¨ Wilson's disease, ¨ East Indian childhood cirrhosis, ¨ Non-alcoholic steatohepatitis (NASH).
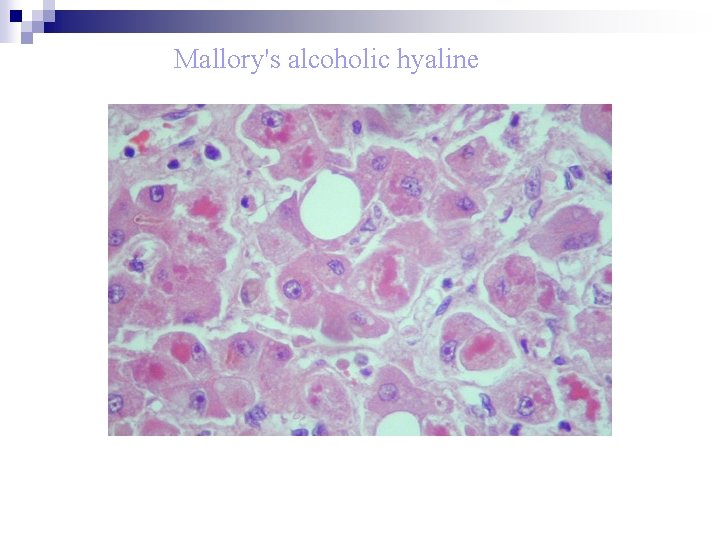
Mallory's alcoholic hyaline
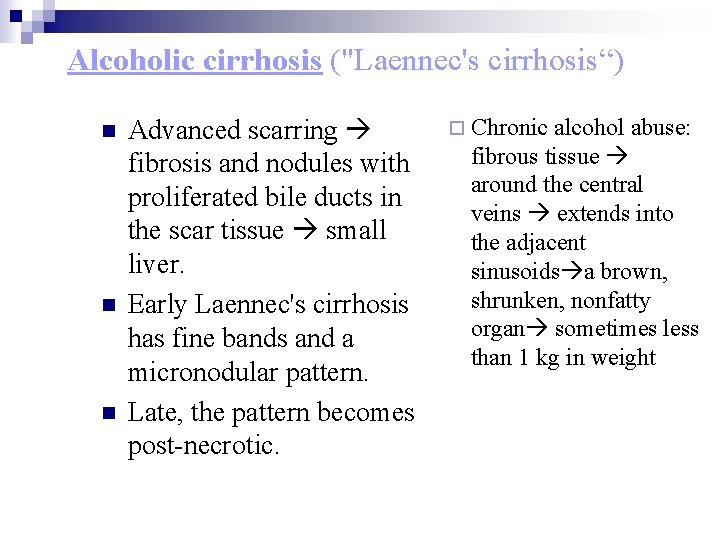
Alcoholic cirrhosis ("Laennec's cirrhosis“) n n n Advanced scarring fibrosis and nodules with proliferated bile ducts in the scar tissue small liver. Early Laennec's cirrhosis has fine bands and a micronodular pattern. Late, the pattern becomes post-necrotic. ¨ Chronic alcohol abuse: fibrous tissue around the central veins extends into the adjacent sinusoids a brown, shrunken, nonfatty organ sometimes less than 1 kg in weight
n n Regenerative activity of the entrapped parenchymal acini uniformly sized “micronodules. ” With time, the nodularity becomes more prominent scattered nodules become quite large occasionally nodules more than 2 cm in diameter may develop. n n Fibrous septae dissect and surround nodules the liver becomes more fibrotic loses fat shrinks. Parenchymal islands engulfed by bands of fibrous tissue mixed micronodular and macronodular patterns.
n n Ischemic necrosis and fibrous obliteration of nodules pale scar tissue leaving residual parenchymal nodules (protrude like “hobnails” from the surface of the liver) Laennec’s cirrhosis Microscopy: ¨ Scattered lymphocytes ¨ Reactive bile duct proliferation in the septae ¨ Bile stasis ¨ Mallory bodies (rarely at this stage) ¨ End-stage alcoholic cirrhosis (postnecrotic cirrhosis).

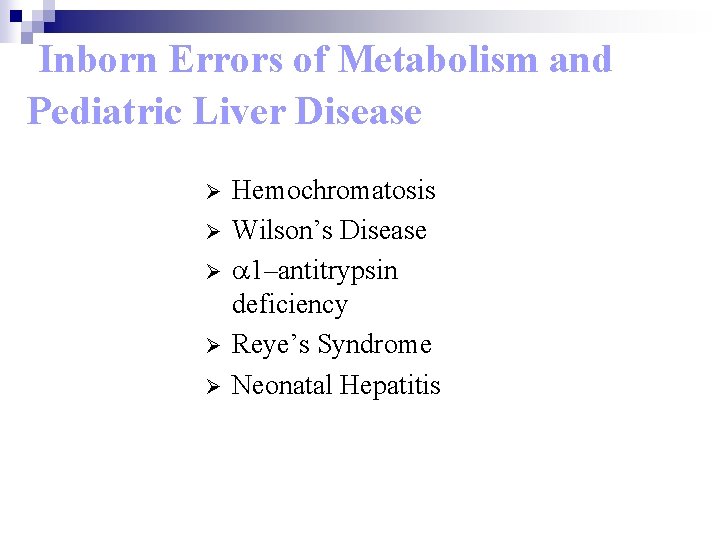
Inborn Errors of Metabolism and Pediatric Liver Disease Ø Ø Ø Hemochromatosis Wilson’s Disease a 1–antitrypsin deficiency Reye’s Syndrome Neonatal Hepatitis
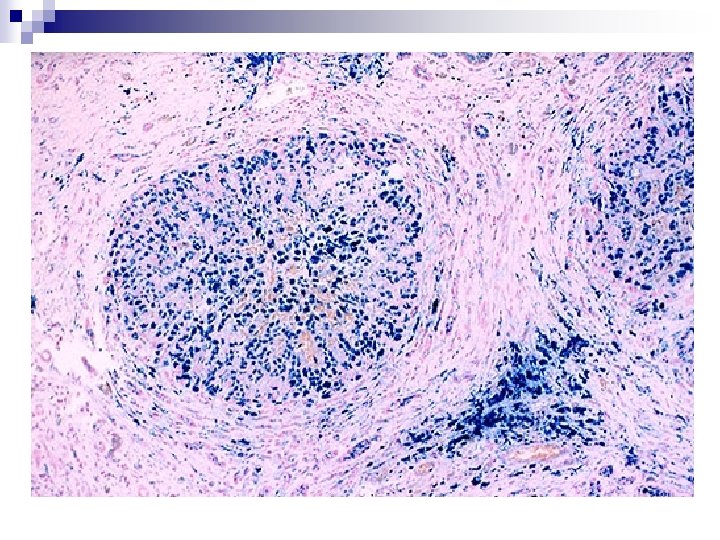
Hemochromatosis n n n Greatly increased absorption of iron from the gut (duodenum). Excessive accumulation of body iron, in the parenchymal cells, particularly ¨ liver ¨ pancreas n Fully developed cases exhibit a classical triad of: ¨ (1) micronodular cirrhosis ¨ (2) diabetes mellitus (bronze diabetes) ¨ (3) skin pigmentation (bronze diabetes).
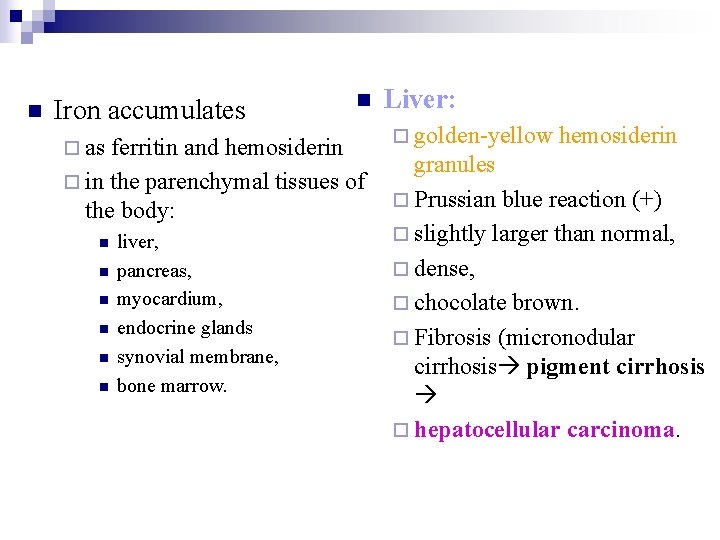
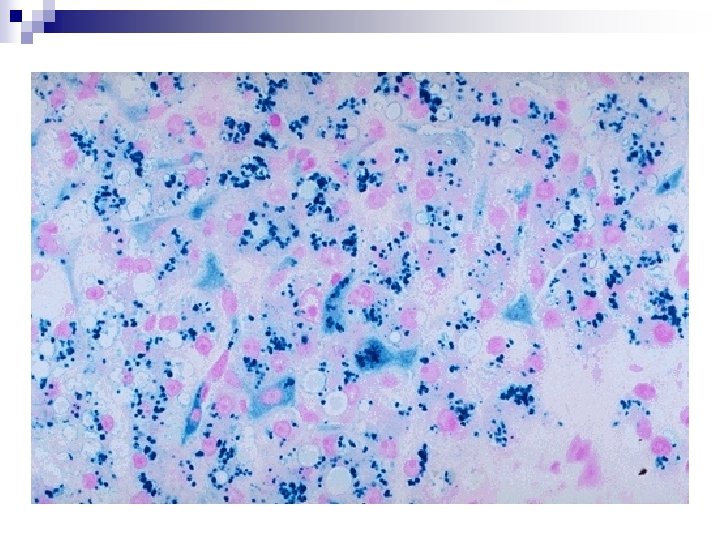
n Iron accumulates ¨ as n ferritin and hemosiderin ¨ in the parenchymal tissues of the body: n n n liver, pancreas, myocardium, endocrine glands synovial membrane, bone marrow. Liver: ¨ golden-yellow hemosiderin granules ¨ Prussian blue reaction (+) ¨ slightly larger than normal, ¨ dense, ¨ chocolate brown. ¨ Fibrosis (micronodular cirrhosis pigment cirrhosis ¨ hepatocellular carcinoma.
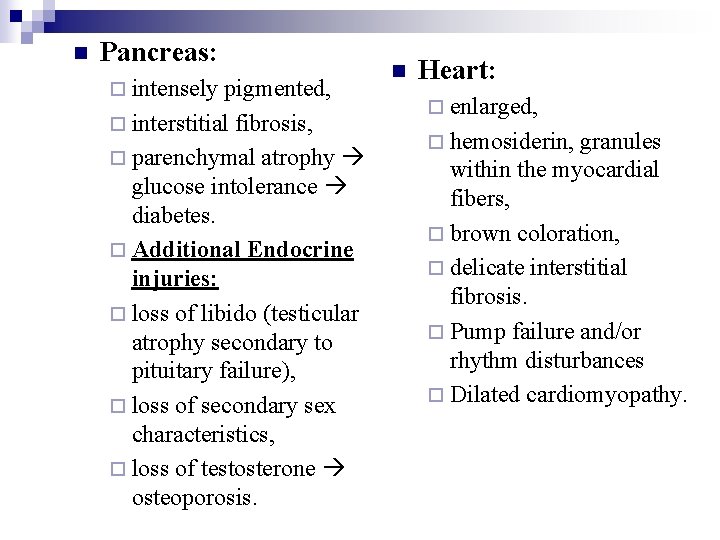
n Pancreas: ¨ intensely pigmented, ¨ interstitial fibrosis, ¨ parenchymal atrophy glucose intolerance diabetes. ¨ Additional Endocrine injuries: ¨ loss of libido (testicular atrophy secondary to pituitary failure), ¨ loss of secondary sex characteristics, ¨ loss of testosterone osteoporosis. n Heart: ¨ enlarged, ¨ hemosiderin, granules within the myocardial fibers, ¨ brown coloration, ¨ delicate interstitial fibrosis. ¨ Pump failure and/or rhythm disturbances ¨ Dilated cardiomyopathy.
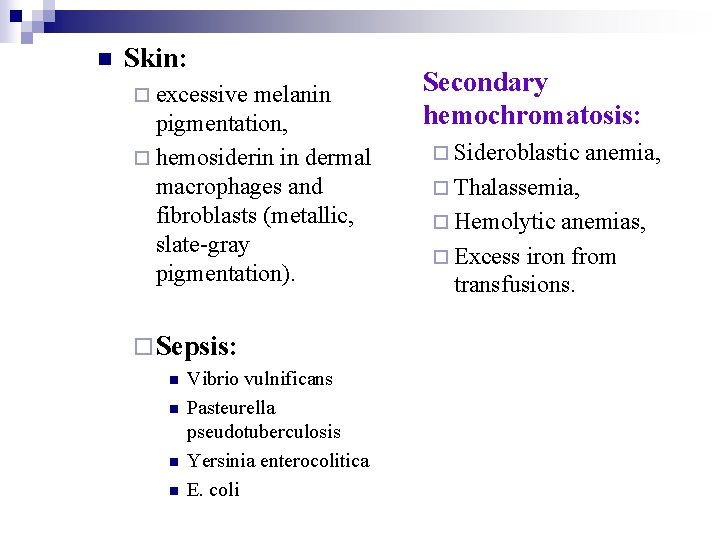
n Skin: ¨ excessive melanin pigmentation, ¨ hemosiderin in dermal macrophages and fibroblasts (metallic, slate-gray pigmentation). ¨ Sepsis: n n Vibrio vulnificans Pasteurella pseudotuberculosis Yersinia enterocolitica E. coli Secondary hemochromatosis: ¨ Sideroblastic anemia, ¨ Thalassemia, ¨ Hemolytic anemias, ¨ Excess iron from transfusions.
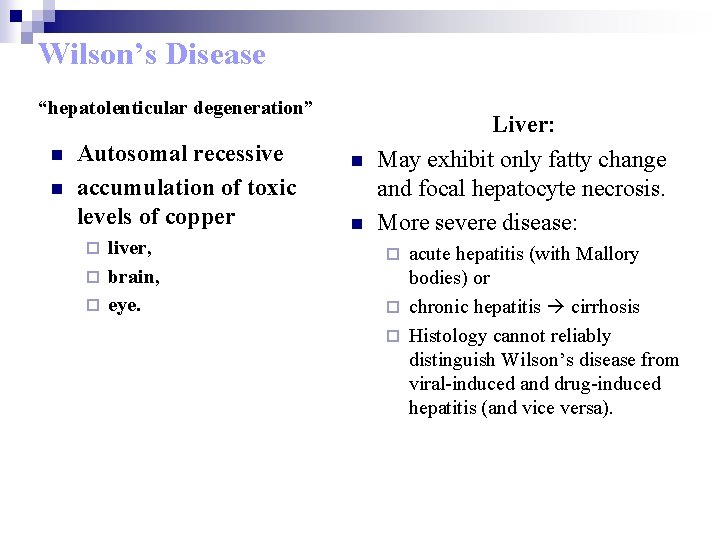
Wilson’s Disease “hepatolenticular degeneration” n n Autosomal recessive accumulation of toxic levels of copper liver, ¨ brain, ¨ eye. ¨ n n Liver: May exhibit only fatty change and focal hepatocyte necrosis. More severe disease: acute hepatitis (with Mallory bodies) or ¨ chronic hepatitis cirrhosis ¨ Histology cannot reliably distinguish Wilson’s disease from viral-induced and drug-induced hepatitis (and vice versa). ¨
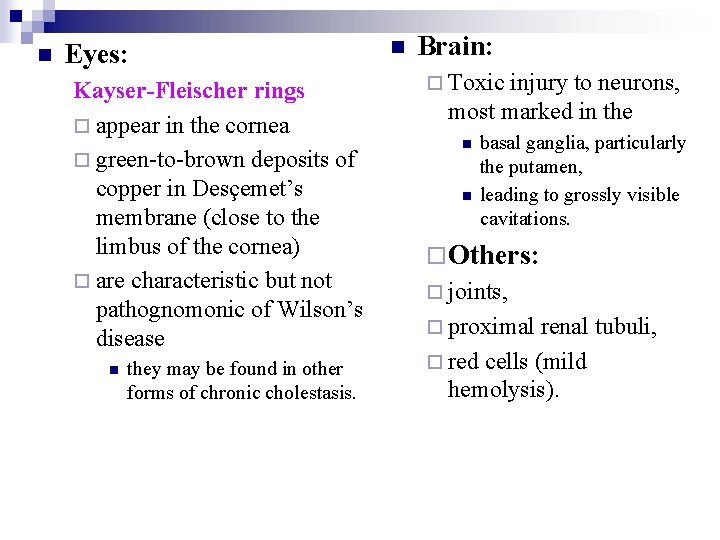
n Eyes: Kayser-Fleischer rings ¨ appear in the cornea ¨ green-to-brown deposits of copper in Desçemet’s membrane (close to the limbus of the cornea) ¨ are characteristic but not pathognomonic of Wilson’s disease n they may be found in other forms of chronic cholestasis. n Brain: ¨ Toxic injury to neurons, most marked in the n n basal ganglia, particularly the putamen, leading to grossly visible cavitations. ¨ Others: ¨ joints, ¨ proximal renal tubuli, ¨ red cells (mild hemolysis).
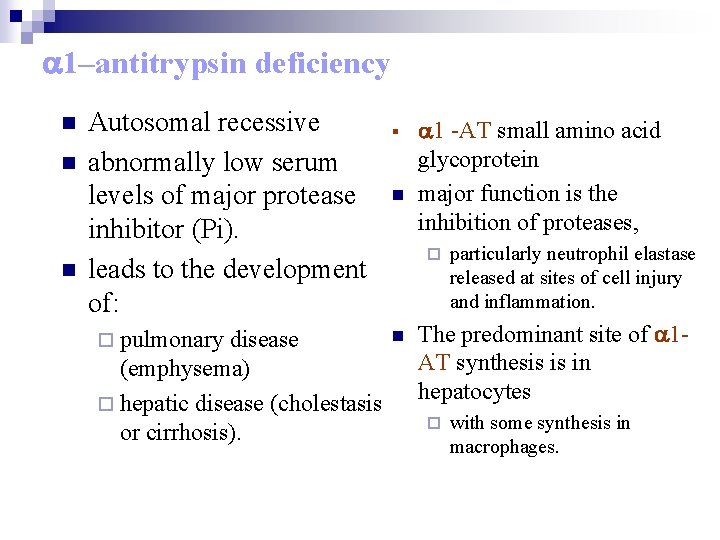
a 1–antitrypsin deficiency n n n Autosomal recessive abnormally low serum levels of major protease inhibitor (Pi). leads to the development of: ¨ pulmonary disease (emphysema) ¨ hepatic disease (cholestasis or cirrhosis). § n a 1 -AT small amino acid glycoprotein major function is the inhibition of proteases, ¨ n particularly neutrophil elastase released at sites of cell injury and inflammation. The predominant site of a 1 AT synthesis is in hepatocytes ¨ with some synthesis in macrophages.
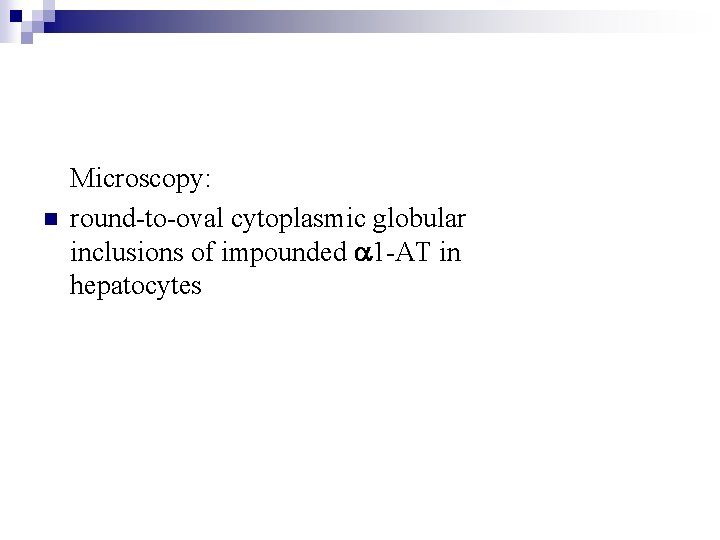
n Microscopy: round-to-oval cytoplasmic globular inclusions of impounded a 1 -AT in hepatocytes
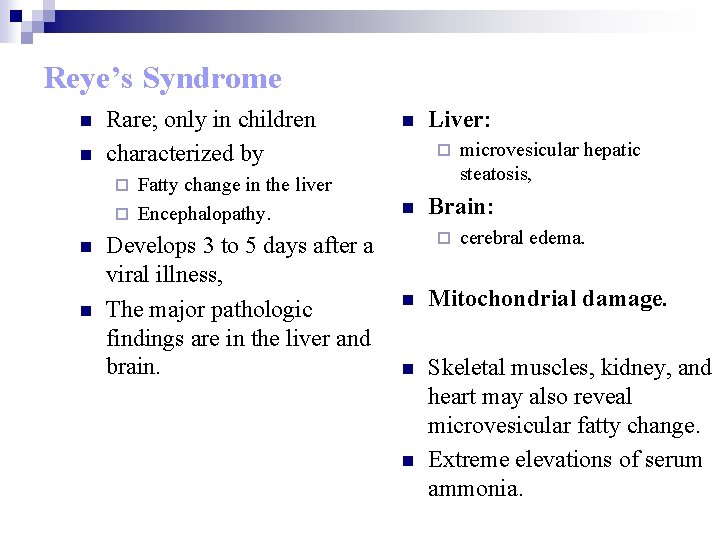
Reye’s Syndrome n n Rare; only in children characterized by Fatty change in the liver ¨ Encephalopathy. n ¨ ¨ n n Develops 3 to 5 days after a viral illness, The major pathologic findings are in the liver and brain. Liver: n microvesicular hepatic steatosis, Brain: ¨ cerebral edema. n Mitochondrial damage. n Skeletal muscles, kidney, and heart may also reveal microvesicular fatty change. Extreme elevations of serum ammonia. n
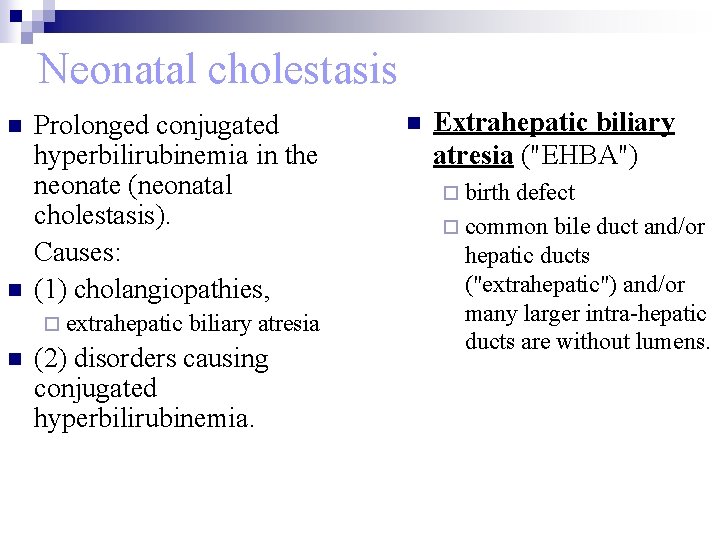
Neonatal cholestasis n n Prolonged conjugated hyperbilirubinemia in the neonate (neonatal cholestasis). Causes: (1) cholangiopathies, ¨ extrahepatic n biliary atresia (2) disorders causing conjugated hyperbilirubinemia. n Extrahepatic biliary atresia ("EHBA") ¨ birth defect ¨ common bile duct and/or hepatic ducts ("extrahepatic") and/or many larger intra-hepatic ducts are without lumens.
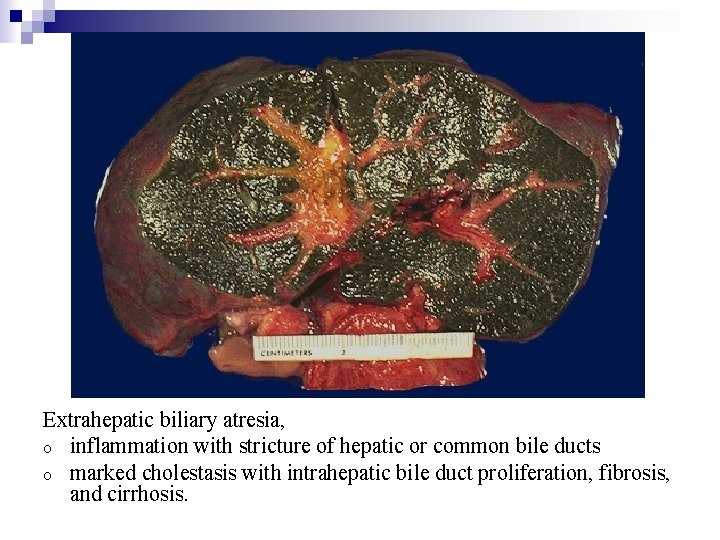
Extrahepatic biliary atresia, o inflammation with stricture of hepatic or common bile ducts o marked cholestasis with intrahepatic bile duct proliferation, fibrosis, and cirrhosis.
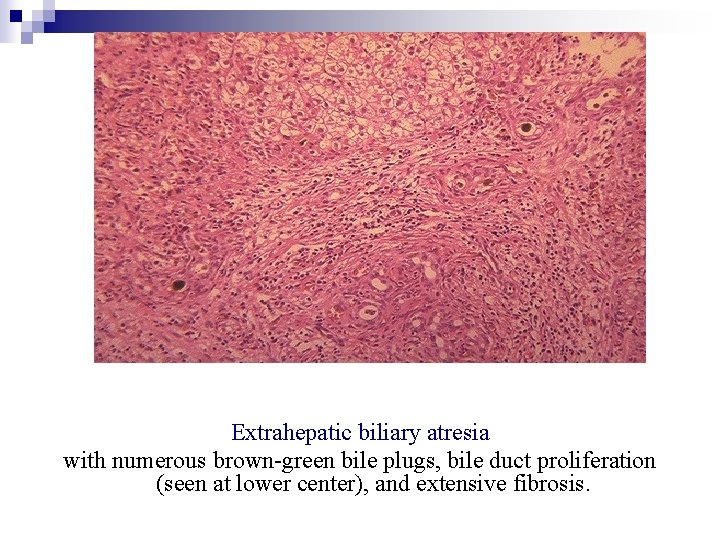
Extrahepatic biliary atresia with numerous brown-green bile plugs, bile duct proliferation (seen at lower center), and extensive fibrosis.
Neonatal hepatitis n n n n The morphologic features of neonatal hepatitis are as follows: 1. focal liver cell necrosis 2. giant cell transformation of hepatocytes 3. hepatocellular and canalicular cholestasis 4. mild mononuclear infiltration of the portal areas 5. reactive changes in the Kupffer cells 6. extramedullary hematopoiesis.
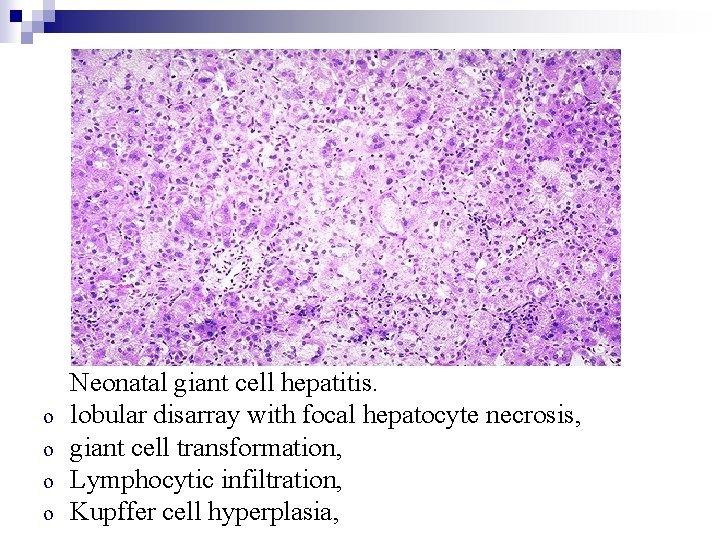
o o Neonatal giant cell hepatitis. lobular disarray with focal hepatocyte necrosis, giant cell transformation, Lymphocytic infiltration, Kupffer cell hyperplasia,
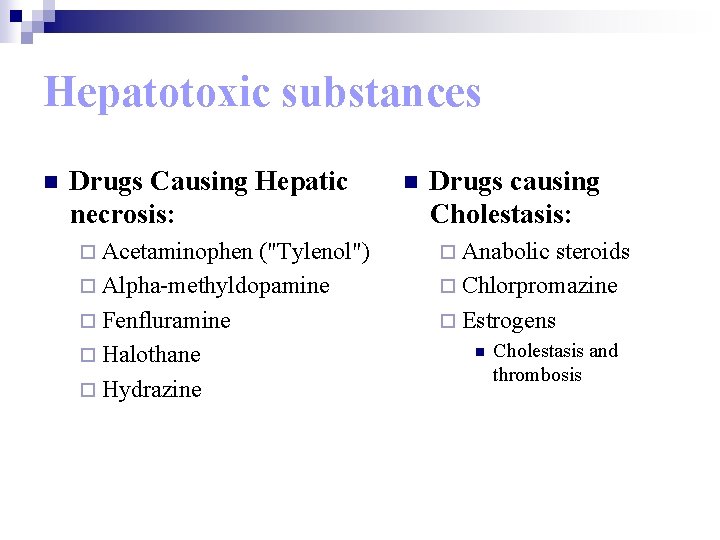
Hepatotoxic substances n Drugs Causing Hepatic necrosis: ¨ Acetaminophen ("Tylenol") ¨ Alpha-methyldopamine ¨ Fenfluramine ¨ Halothane ¨ Hydrazine n Drugs causing Cholestasis: ¨ Anabolic steroids ¨ Chlorpromazine ¨ Estrogens n Cholestasis and thrombosis
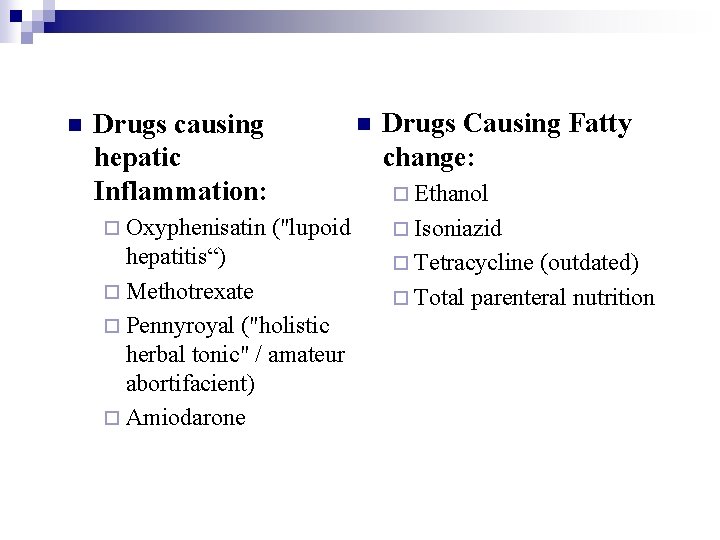
n Drugs causing hepatic Inflammation: ¨ Oxyphenisatin n Drugs Causing Fatty change: ¨ Ethanol ("lupoid hepatitis“) ¨ Methotrexate ¨ Pennyroyal ("holistic herbal tonic" / amateur abortifacient) ¨ Amiodarone ¨ Isoniazid ¨ Tetracycline (outdated) ¨ Total parenteral nutrition
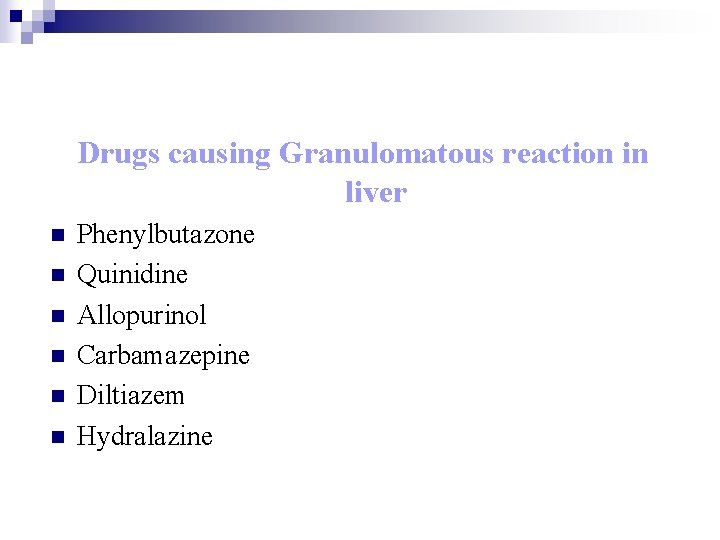
Drugs causing Granulomatous reaction in liver n n n Phenylbutazone Quinidine Allopurinol Carbamazepine Diltiazem Hydralazine
THANK YOU
- Slides: 90