Heparin Lovenox Coumadin Charnelle Lee RN MSN Heparin
- Slides: 19
Heparin – Lovenox - Coumadin Charnelle Lee, RN, MSN
Heparin Anticoagulant Does not dissolve clots Interrupts the clotting process Helps the body stop the size of the clot from increasing • Takes 6 weeks for an existing clot to dissolve • Of course this is dependant on the size and patient condition • •
Heparin Antidote • Heparin® Antidote Protamine Sulfate • Protamine sulfate is a heparin antidote that works against the anti-coagulating effects of heparin by binding to the drug and making it ineffective. • Originally derived from the sperm of salmon, protamine sulfate can only effectively counteract heparin if 1 mg of protamine sulfate is administered for every 100 IU of active heparin received. • It's important to note that Vitamin K, which is effective at promoting blood clotting, is not an effective heparin antidote, as Vitamin K cannot stop heparin from working (like protamine sulfate does).
Protamine Sulfate • Unfortunately, using protamine sulfate to stop the effects of heparin can have its own complications, including: • constricting the lung's airways (bronchoconstriction) • dramatically increasing or decreasing blood pressure • severe allergic reaction, characterized by facial or tongue swelling, breathing difficulties and/or skin rash • promoting anti-coagulation (if large enough doses are administered)
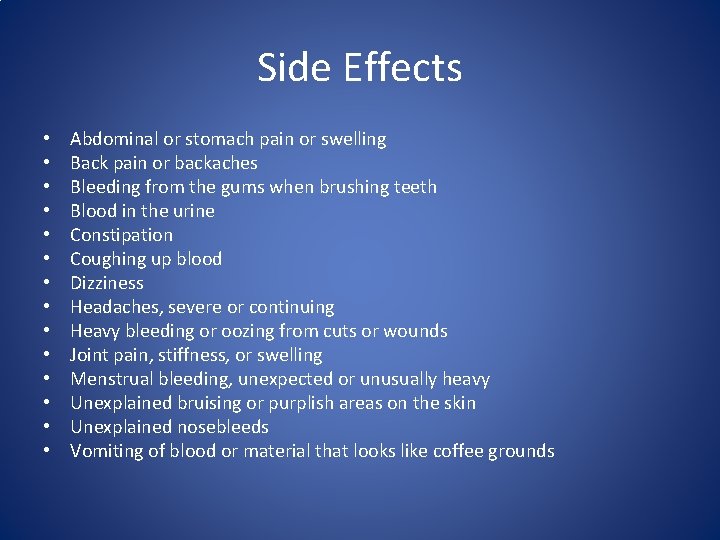
Side Effects • • • • Abdominal or stomach pain or swelling Back pain or backaches Bleeding from the gums when brushing teeth Blood in the urine Constipation Coughing up blood Dizziness Headaches, severe or continuing Heavy bleeding or oozing from cuts or wounds Joint pain, stiffness, or swelling Menstrual bleeding, unexpected or unusually heavy Unexplained bruising or purplish areas on the skin Unexplained nosebleeds Vomiting of blood or material that looks like coffee grounds
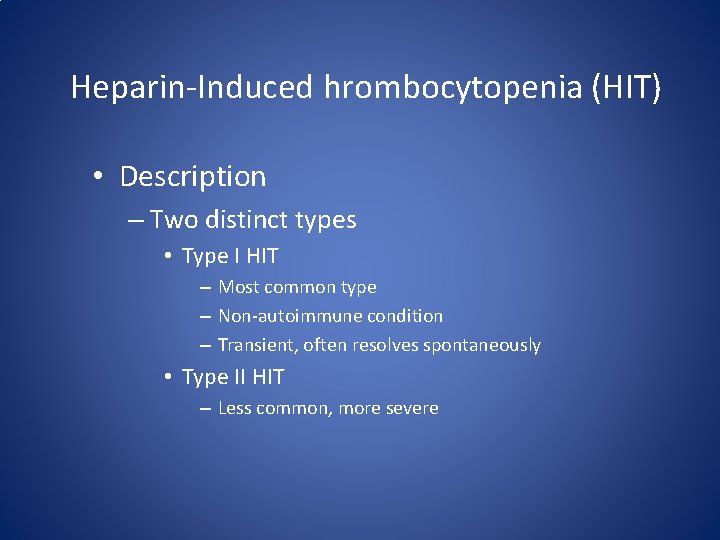
Heparin-Induced hrombocytopenia (HIT) • Description – Two distinct types • Type I HIT – Most common type – Non-autoimmune condition – Transient, often resolves spontaneously • Type II HIT – Less common, more severe
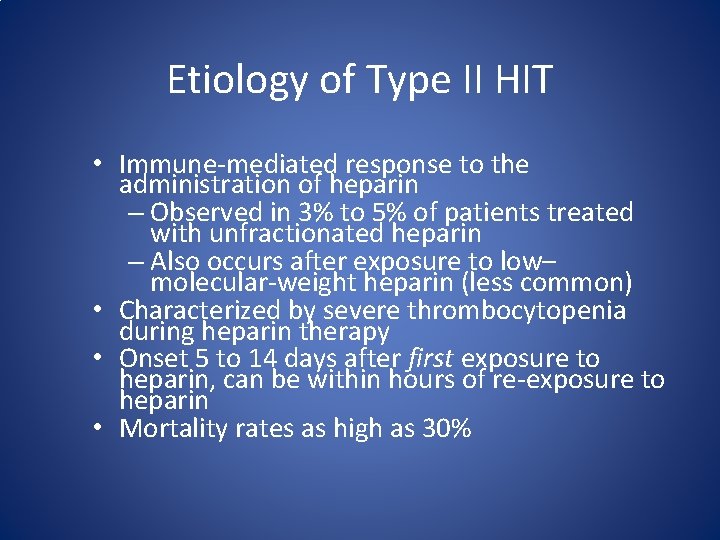
Etiology of Type II HIT • Immune-mediated response to the administration of heparin – Observed in 3% to 5% of patients treated with unfractionated heparin – Also occurs after exposure to low– molecular-weight heparin (less common) • Characterized by severe thrombocytopenia during heparin therapy • Onset 5 to 14 days after first exposure to heparin, can be within hours of re-exposure to heparin • Mortality rates as high as 30%
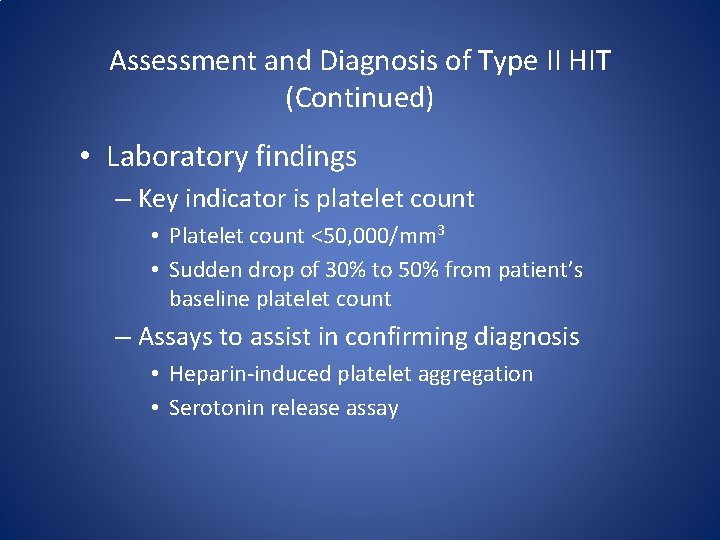
Assessment and Diagnosis of Type II HIT (Continued) • Laboratory findings – Key indicator is platelet count • Platelet count <50, 000/mm 3 • Sudden drop of 30% to 50% from patient’s baseline platelet count – Assays to assist in confirming diagnosis • Heparin-induced platelet aggregation • Serotonin release assay
Medical Management of Type II HIT • Early identification is critical to managing effects of Type II HIT • Focus of medical management revolves around: – Identification of Type II HIT – Discontinuation of heparin therapy – Alternative form of anticoagulation if needed
Nursing Management of Type II HIT • Nursing priorities in the management of the patient with HIT are focused toward: – Ensuring that all heparin is discontinued. – Maintaining surveillance for complications. – Providing comfort and emotional support.
Laboratory monitoring: platelet count • Check PLT count daily to detect heparin induced thrombocytopenia (HIT) • If count drops 30 -50%, consider HIT, withdraw heparin, start alternative anticoagulant, order confirmatory test for HIT • Overdose of UFH • Stop heparin and monitor PTT. Heparin half-life is approximately 30 minutes. If bleeding is severe, consider protamine sulfate (1 mg/100 units heparin) • FFP does not reverse heparin effect
Coumadin • • • Warfarin (Coumadin ) Indications for warfarin Treatment of arterial and venous thrombosis to prevent clot propagation Prevention of thromboembolic disease in thrombophilia, atrial fibrillation, mechanical heart valves, and high-risk surgery Mechanism of action for warfarin Prevents the vitamin K dependent gamma-carboxylation of factors II, VII, IX, and X, proteins C and S, slowing thrombin production Dosage of warfarin 5 -10 mg/day with no loading dose. Must be monitored due to unpredictable halflife. Affected by many drugs and dietary variation Requires 2 -7 days to reach therapeutic levels. To achieve immediate anticoagulation, begin with heparin
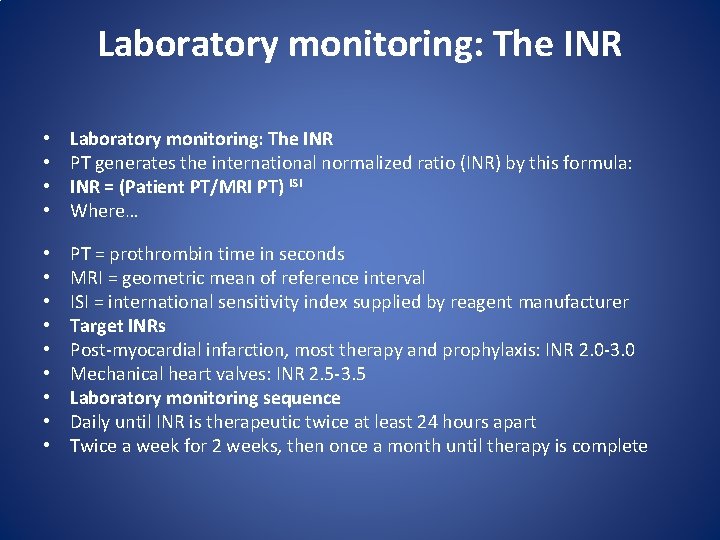
Laboratory monitoring: The INR • • Laboratory monitoring: The INR PT generates the international normalized ratio (INR) by this formula: INR = (Patient PT/MRI PT) ISI Where… • • • PT = prothrombin time in seconds MRI = geometric mean of reference interval ISI = international sensitivity index supplied by reagent manufacturer Target INRs Post-myocardial infarction, most therapy and prophylaxis: INR 2. 0 -3. 0 Mechanical heart valves: INR 2. 5 -3. 5 Laboratory monitoring sequence Daily until INR is therapeutic twice at least 24 hours apart Twice a week for 2 weeks, then once a month until therapy is complete
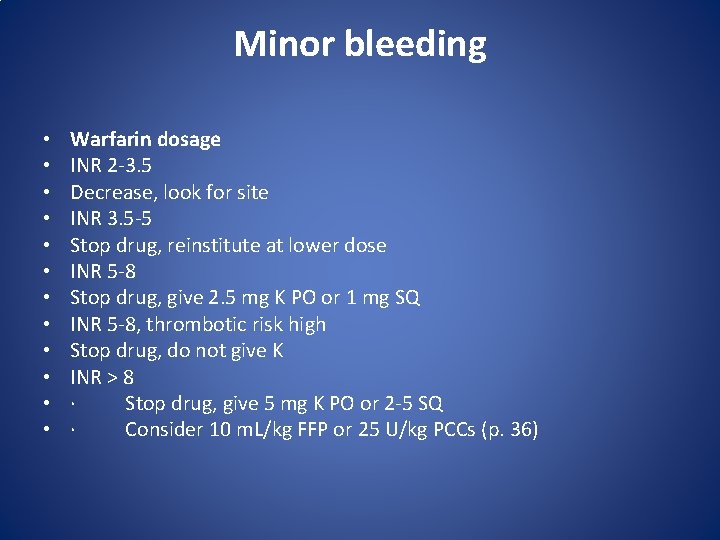
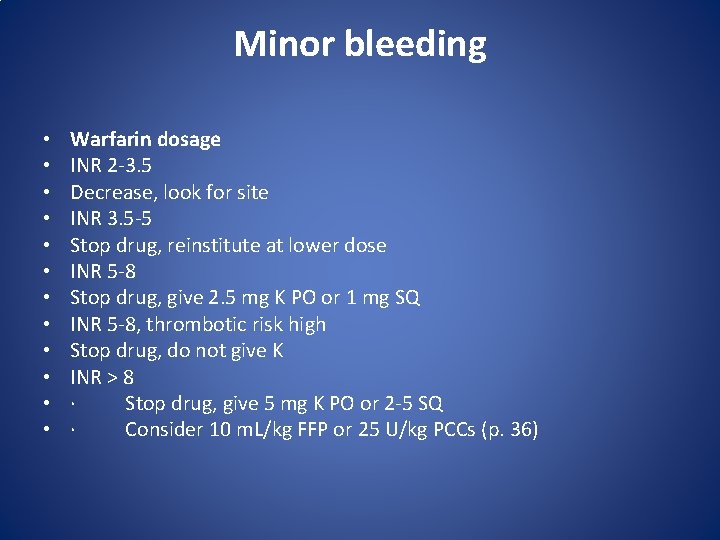
Minor bleeding • • • Warfarin dosage INR 2 -3. 5 Decrease, look for site INR 3. 5 -5 Stop drug, reinstitute at lower dose INR 5 -8 Stop drug, give 2. 5 mg K PO or 1 mg SQ INR 5 -8, thrombotic risk high Stop drug, do not give K INR > 8 · Stop drug, give 5 mg K PO or 2 -5 SQ · Consider 10 m. L/kg FFP or 25 U/kg PCCs (p. 36)
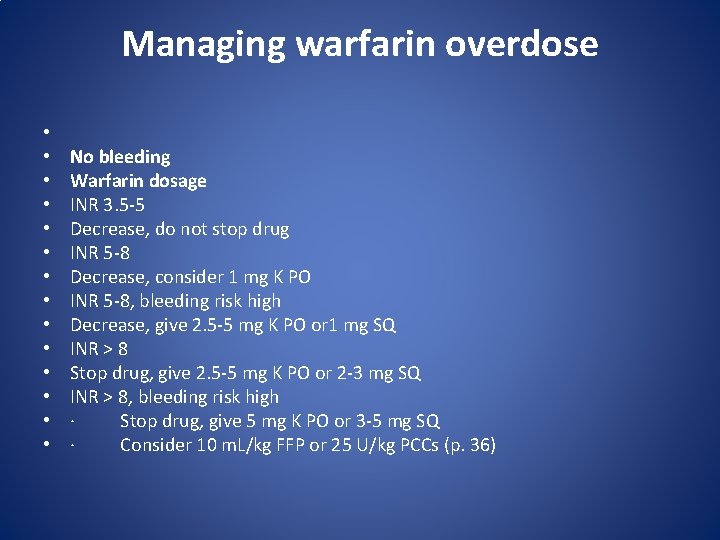
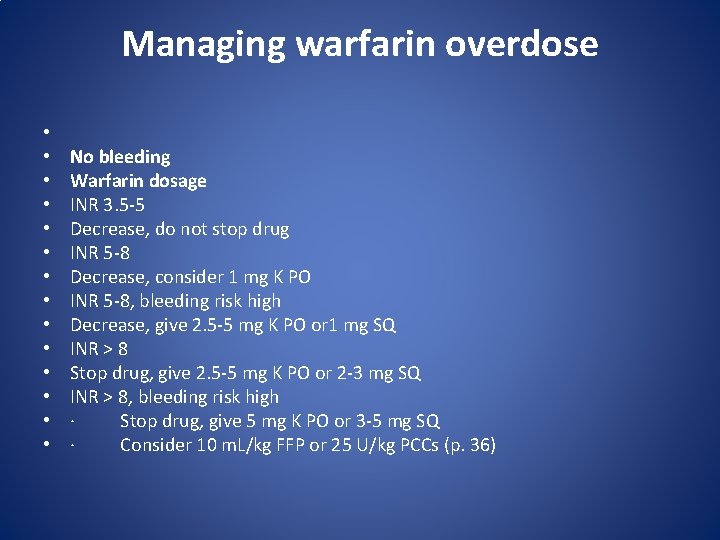
Managing warfarin overdose • • • • No bleeding Warfarin dosage INR 3. 5 -5 Decrease, do not stop drug INR 5 -8 Decrease, consider 1 mg K PO INR 5 -8, bleeding risk high Decrease, give 2. 5 -5 mg K PO or 1 mg SQ INR > 8 Stop drug, give 2. 5 -5 mg K PO or 2 -3 mg SQ INR > 8, bleeding risk high · Stop drug, give 5 mg K PO or 3 -5 mg SQ · Consider 10 m. L/kg FFP or 25 U/kg PCCs (p. 36)
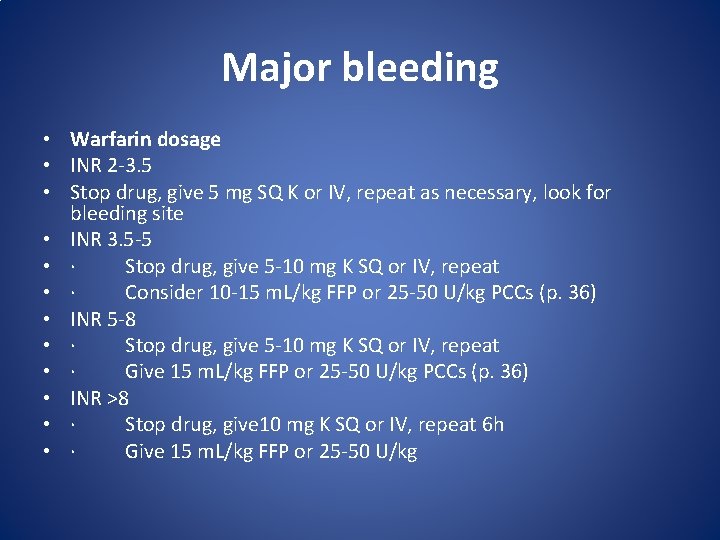
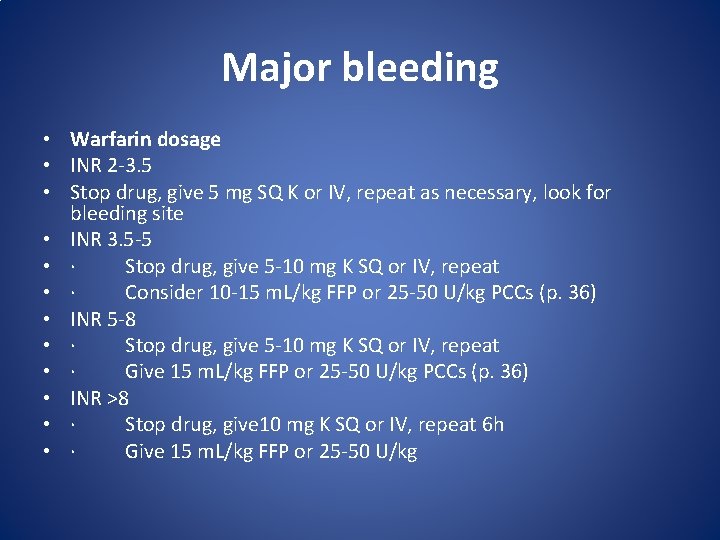
Major bleeding • Warfarin dosage • INR 2 -3. 5 • Stop drug, give 5 mg SQ K or IV, repeat as necessary, look for bleeding site • INR 3. 5 -5 • · Stop drug, give 5 -10 mg K SQ or IV, repeat • · Consider 10 -15 m. L/kg FFP or 25 -50 U/kg PCCs (p. 36) • INR 5 -8 • · Stop drug, give 5 -10 mg K SQ or IV, repeat • · Give 15 m. L/kg FFP or 25 -50 U/kg PCCs (p. 36) • INR >8 • · Stop drug, give 10 mg K SQ or IV, repeat 6 h • · Give 15 m. L/kg FFP or 25 -50 U/kg
Antidotes • Heparin – • Coumadin– 1 – 2
LMWH • What is Lovenox? • Lovenox is an anticoagulant (blood thinner) that prevents the formation of blood clots. • Lovenox is used to treat or prevent a type of blood clot called deep vein thrombosis (DVT), which can lead to blood clots in the lungs (pulmonary embolism). A DVT can occur after certain types of surgery, or in people who are bedridden due to a prolonged illness. • Lovenox is also used to prevent blood vessel complications in people with certain types of angina (chest pain) or heart attack. • Lovenox may also be used for other purposes not listed in this medication guide
Difference between Heparin and Lovenox • Lovenox is a brand name for the prescription medication enoxaparin, which, like heparin, is prescribed for the treatment of blood clots. Lovenox is actually derived from heparin and has molecules with a lighter weight than its parent drug. Read more at Suite 101: Lovenox vs. Heparin: Differences Between Anticoagulant Medications | Suite 101. com http: //www. suite 101. com/content/lovenox-vsheparin-a 193192#ixzz 1 Rom. Q 8 fcp