Hendarsyah Suryadinata dr Sp PD TempatTanggal Lahir Bandung
Hendarsyah Suryadinata, dr. , Sp. PD Tempat/Tanggal Lahir : Bandung, 24 November 1977 Email : hendarsyahsuryadinata@gmail. com Pekerjaan : Departemen Ilmu Penyakit Dalam Divisi Respirologi dan Respirasi Kritis Jabatan : Staff Departemen Ilmu Penyakit Dalam RSHS Bandung Integrated Respiratory Care IV | 16– 18 September 2016

LOGO Management of Dyspnea Hendarsyah Suryadinata Divisi Repirologi dan Kritis Respirasi Departemen/SMF Ilmu Penyakit Dalam FK Unpad/RSUP Dr Hasan Sadikin Bandung
Dyspnea q. Dyspnea on Effort (DOE) q. Exertion-induced SOB q. Orthopnea q. Recumbent-induced SOB q. Paroxysmal nocturnal dyspnea (PND) q. Sudden SOB after recumbent q. Sever breathness at night relieved when patient sits up
Dyspnea Rapid Assessment q. ABC’s q. Mental status q. Presence of cyanosis
Dyspnea Initial Interventions q. IV assess q. Pulse oximetry; supplemental O 2 q. Cardiac monitor
What Are the Indications for Airway Management? q. Secure & maintain patency q. Protection q. Oxygenation q. Ventilation q. Treatment – Suction, medications
Dyspnea : History q Prolonged questioning can be counterproductive q Yes/No questions if significantly dyspneic q Unlike pain, severity of dyspnea = severity of disease q What does patient mean by SOB? q How long has SOB been present? q Is it sudden or gradual q Does anything make it better or worse?
Dyspnea : History q. Has there been similar episodes? q. Are there associated symptoms? q. What is the past medical Hx? q. Smoking Hx? q. Medications?
Cause : Acute q. Bronchial asthma q. Pneumonitis q. Pneumonia q. Pneumothorax q. Thromboembolic disease q. Cardiac q. Pulmonary Edema q. Non Cardiac Pulmonary Edema q. Psychogenic
Cause : Chronic Pulmonary Cause q. COPD q. Bronchial Asthma q. Emphysema Chronic Bronchitis q. Restrictive Lung Disease q. Sarcoidosis q. Rheumatoid lung qfibrosing alveolitis q. Pneumoconosis
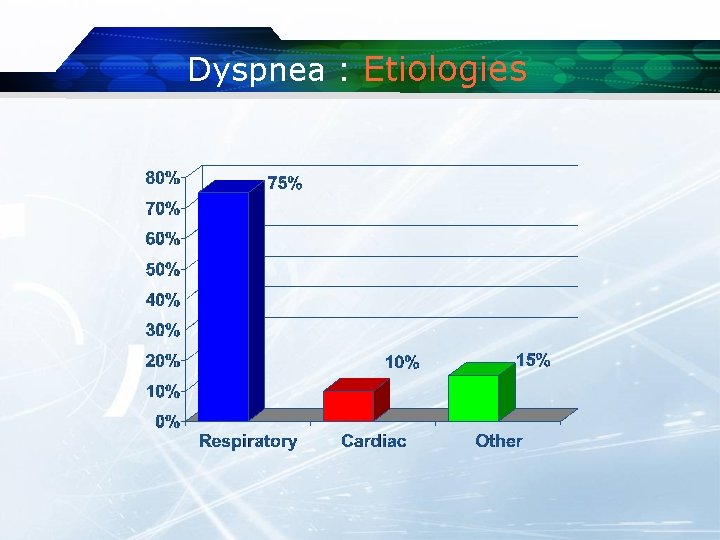
Dyspnea : Etiologies
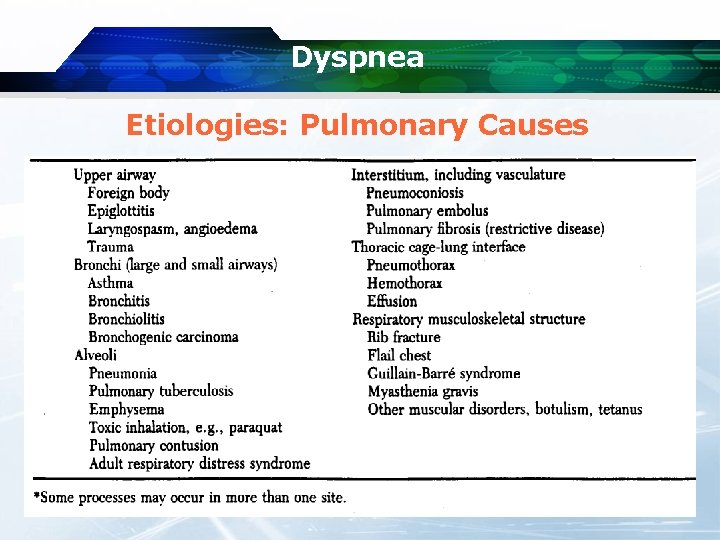
Dyspnea Etiologies: Pulmonary Causes
Dyspnea Common Pulmonary Causes q. Obstructive lung disease q. Asthma/COPD q. Pneumonia q. Pulmonary embolism q. Pneumothorax
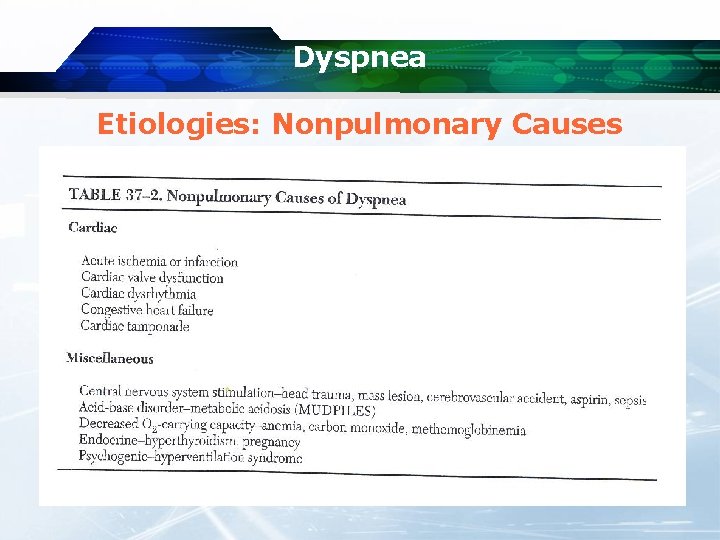
Dyspnea Etiologies: Nonpulmonary Causes
Dyspnea Common Cardiac Causes q. Acute coronary syndromes q. CHF q. Dysrhythmias q. Valvular heart disease
Dyspnea Common Miscellaneous Causes v. Metabolic acidemias v. Severe Anemia v. Pregnancy v. Hyperventilation Syndrome
Pulmonary Diseases & Disorders q Pulmonary Disease & Conditions may result from: q. Infectious causes q. Non-Infectious causes q Adversely affect one or more of the following q. Ventilation q. Diffusion q. Perfusion
Pulmonary Diseases & Disorders q The Respiratory Emergency may stem from dysfunction or disease of (examples only): q. Control System q. Hyperventilation q. Central Respiratory Depression q. CVA q. Thoracic Bellows q. Chest/Diaphragm Trauma q. Pickwickian Syndrome q. Guillian-Barre Syndrome q. Myasthenia Gravis q. COPD
Pulmonary Diseases & Disorders v The Respiratory Emergency may affect the upper or lower airways v Upper Airway Obstruction § § § Tongue Foreign Body Aspiration Angioneurotic Edema Maxillofacial, Larnygotracheal Trauma Croup Epiglottitis
Pulmonary Diseases & Disorders v Lower Airway Obstruction § § Emphysema Chronic Bronchitis Asthma Cystic Fibrosis
Pulmonary Diseases & Disorders v The Respiratory Emergency may stem from Gas Exchange Surface Abnormalities § § § Cardiogenic Pulmonary Edema Non-cardiogenic Pulmonary Edema Pneumonia Toxic Gas Inhalation Pulmonary Embolism Drowning
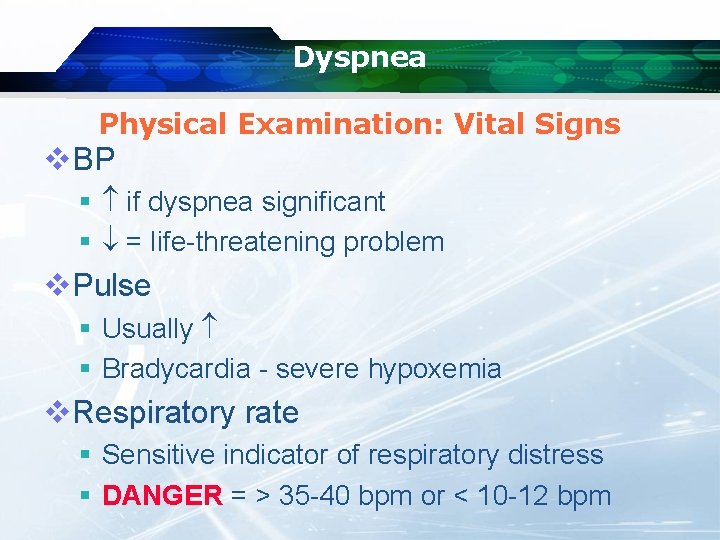
Dyspnea Physical Examination: Vital Signs v. BP § if dyspnea significant § = life-threatening problem v. Pulse § Usually § Bradycardia - severe hypoxemia v. Respiratory rate § Sensitive indicator of respiratory distress § DANGER = > 35 -40 bpm or < 10 -12 bpm
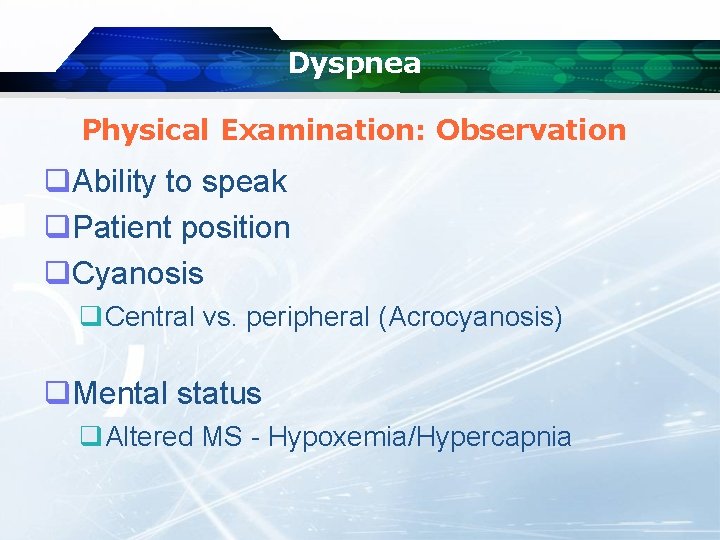
Dyspnea Physical Examination: Observation q. Ability to speak q. Patient position q. Cyanosis q. Central vs. peripheral (Acrocyanosis) q. Mental status q. Altered MS - Hypoxemia/Hypercapnia
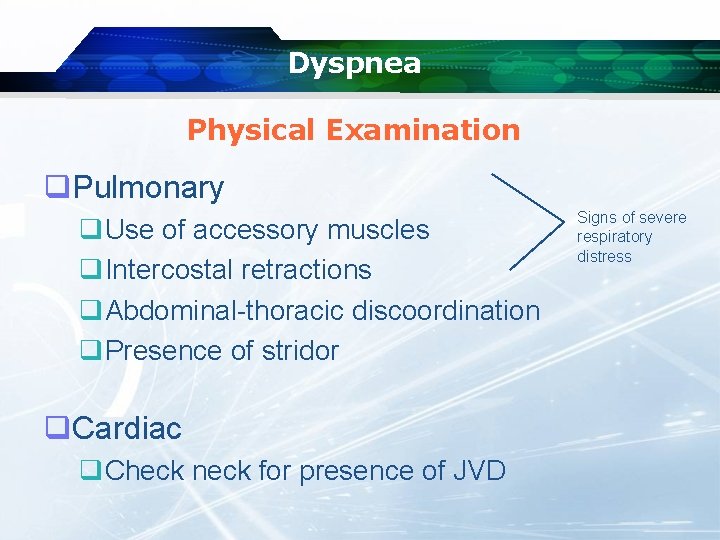
Dyspnea Physical Examination q. Pulmonary q. Use of accessory muscles q. Intercostal retractions q. Abdominal-thoracic discoordination q. Presence of stridor q. Cardiac q. Check neck for presence of JVD Signs of severe respiratory distress
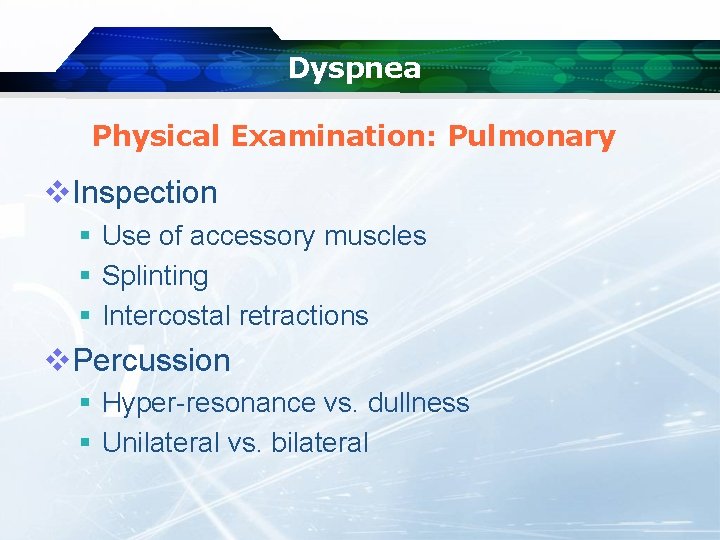
Dyspnea Physical Examination: Pulmonary v. Inspection § Use of accessory muscles § Splinting § Intercostal retractions v. Percussion § Hyper-resonance vs. dullness § Unilateral vs. bilateral
Dyspnea Physical Examination: Pulmonary q. Auscultation q. Air Entry q. Stridor = Upper Airway Obstruction q. Breath sounds q. Normal q. Abnormal q. Wheezing, Rales, Rhonchi, etc. q. Unilateral vs Bilateral
Dyspnea Physical Examination: Cardiac q. Neck q. JVP ? q. Auscultation q. Abnormal S 2 splitting q. Present of S 3 and/or S 4 q. Rubs q. Murmurs
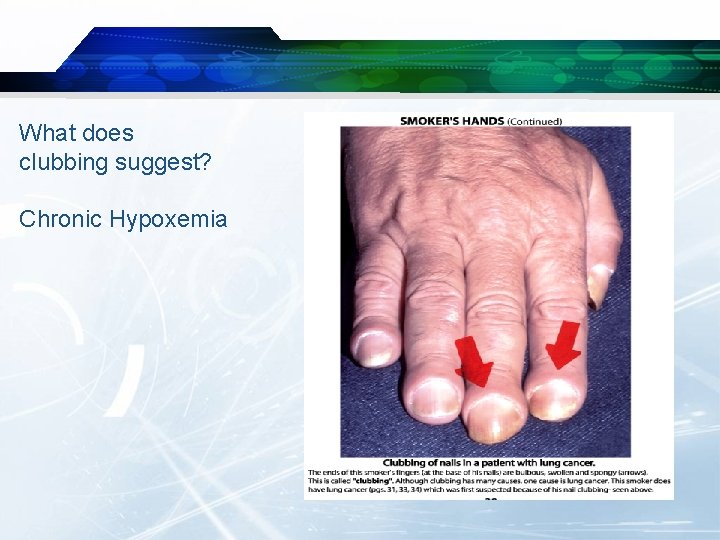
What does clubbing suggest? Chronic Hypoxemia
Pneumonia 1. 2. 3. 4. 5. 6. 7. 8. 9. Fever with Chill Pleuratic Chest Pain Purulent Sputum History of Upper Respiratory Symptoms Signs of Consolidation CXR CBC Blood Culture BGA
Pneumonia q Inflammation of the bronchioles and alveoli q. Products of inflammation (secretions, pus) add to respiration difficulty q Gas exchange is impaired q Work of breathing increases q May lead to q. Atelectasis q. Sepsis q. V/Q Mismatch q. Hypoxemia
Pneumonia: Etiology q Viral q Bacterial q Fungi q Protozoa (pneumocystis) q Aspiration
Management of Pneumonia q Treatment mostly based upon symptoms § § § Oxygen Rarely is intubation required IV Access & Rehydration B 2 agonists may be useful Antibiotics Antipyretics

Pneumonia: Management q MD follow-up for labs, cultures & Rx q Transport considerations § § Elderly have significant co-morbidity Young have difficulty with oral medications ED vs PMD office/clinic Transport in position of comfort
Acute Bronchial Asthma 1. 2. 3. 4. 5. 6. 7. Age Start in Young Age Family History H/O Allergic Rhinitis Physical Examination Barrel Shape CXR BGA
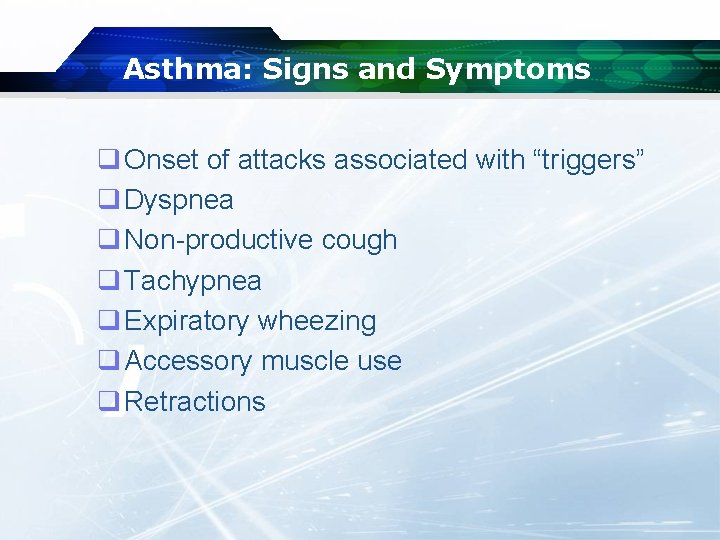
Asthma: Signs and Symptoms q Onset of attacks associated with “triggers” q Dyspnea q Non-productive cough q Tachypnea q Expiratory wheezing q Accessory muscle use q Retractions
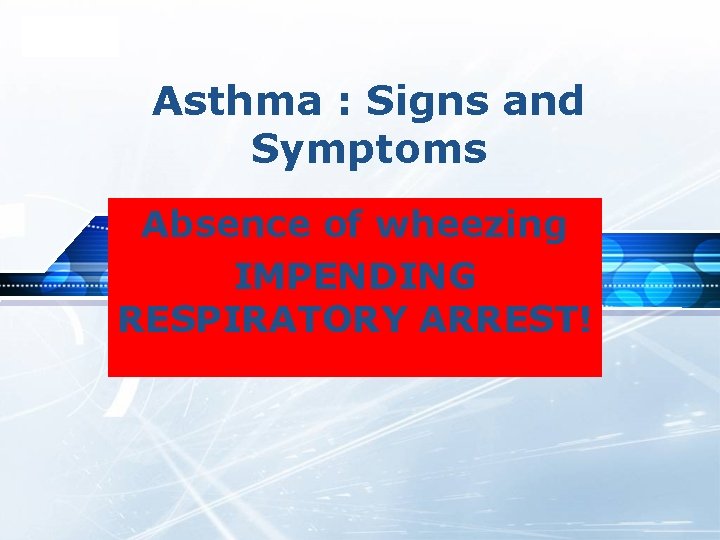
LOGO Asthma : Signs and Symptoms Absence of wheezing IMPENDING RESPIRATORY ARREST!
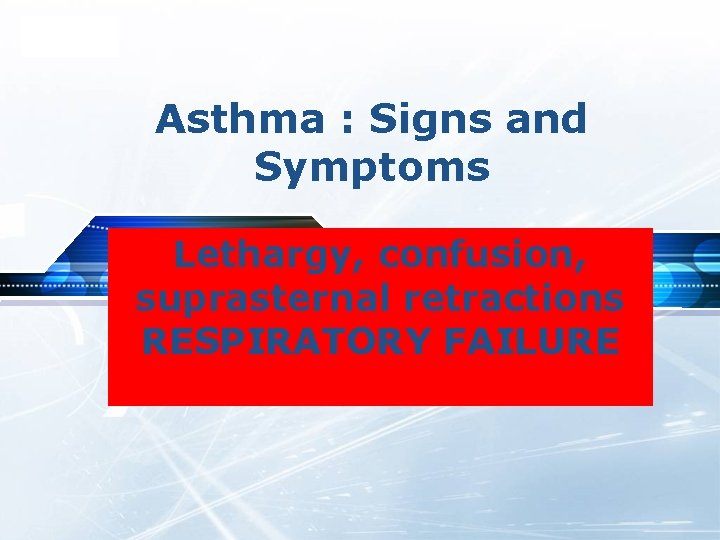
LOGO Asthma : Signs and Symptoms Lethargy, confusion, suprasternal retractions RESPIRATORY FAILURE
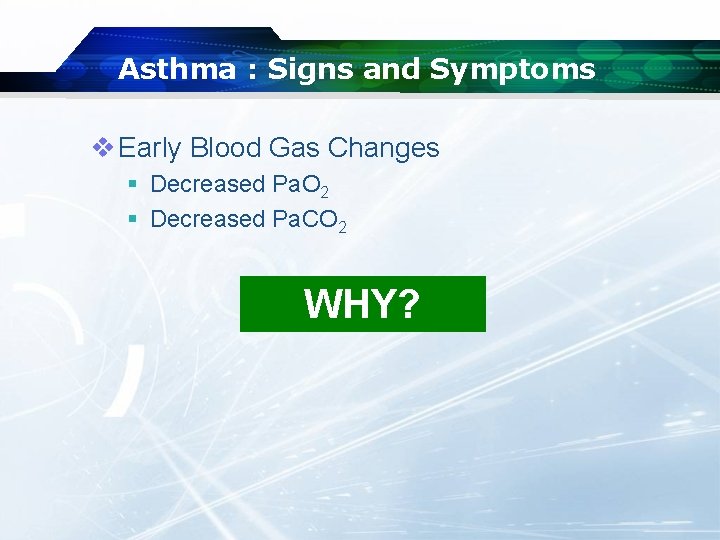
Asthma : Signs and Symptoms v Early Blood Gas Changes § Decreased Pa. O 2 § Decreased Pa. CO 2 WHY?
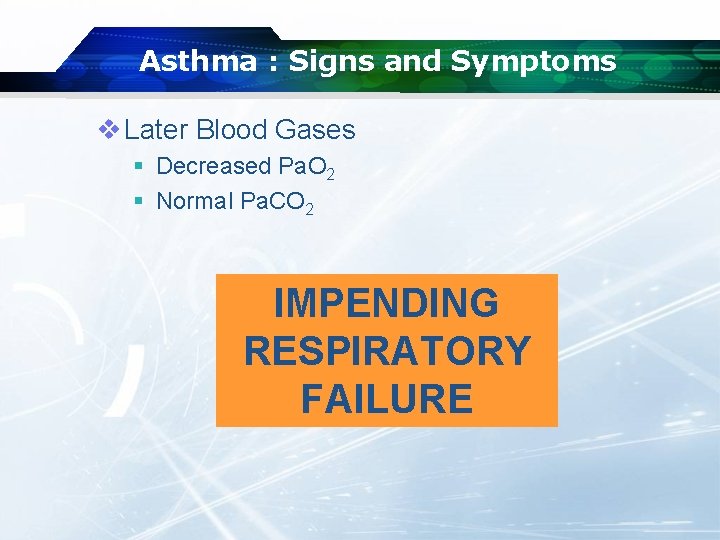
Asthma : Signs and Symptoms v Later Blood Gases § Decreased Pa. O 2 § Normal Pa. CO 2 IMPENDING RESPIRATORY FAILURE
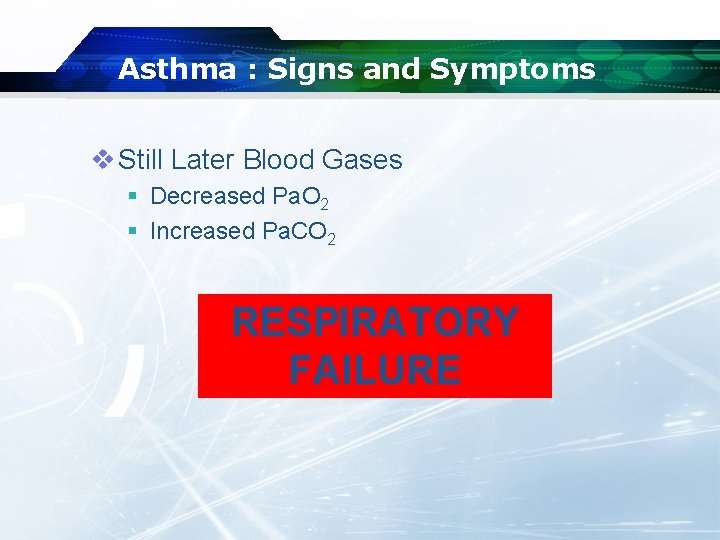
Asthma : Signs and Symptoms v Still Later Blood Gases § Decreased Pa. O 2 § Increased Pa. CO 2 RESPIRATORY FAILURE
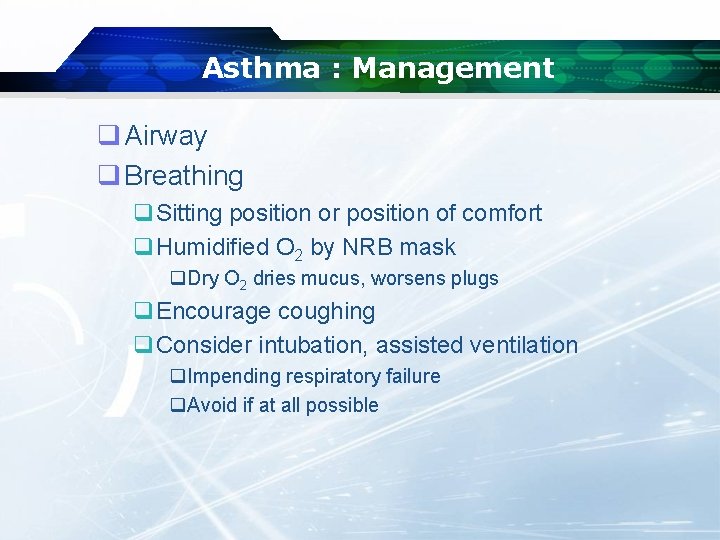
Asthma : Management q Airway q Breathing q. Sitting position or position of comfort q. Humidified O 2 by NRB mask q. Dry O 2 dries mucus, worsens plugs q. Encourage coughing q. Consider intubation, assisted ventilation q. Impending respiratory failure q. Avoid if at all possible
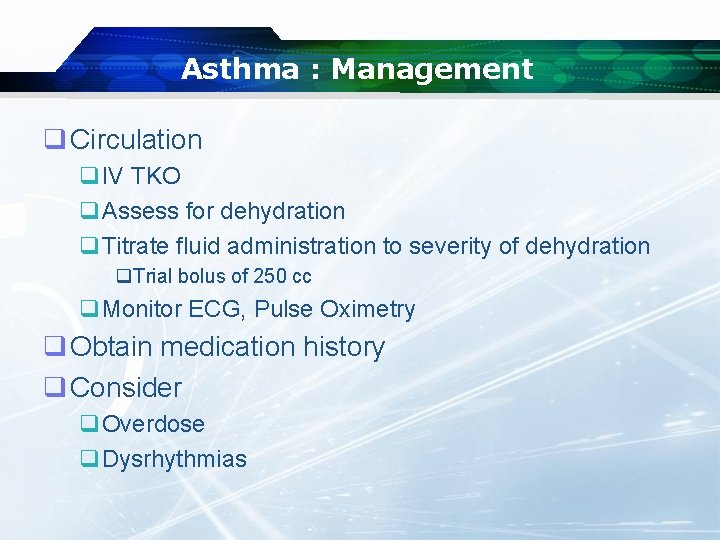
Asthma : Management q Circulation q. IV TKO q. Assess for dehydration q. Titrate fluid administration to severity of dehydration q. Trial bolus of 250 cc q. Monitor ECG, Pulse Oximetry q Obtain medication history q Consider q. Overdose q. Dysrhythmias
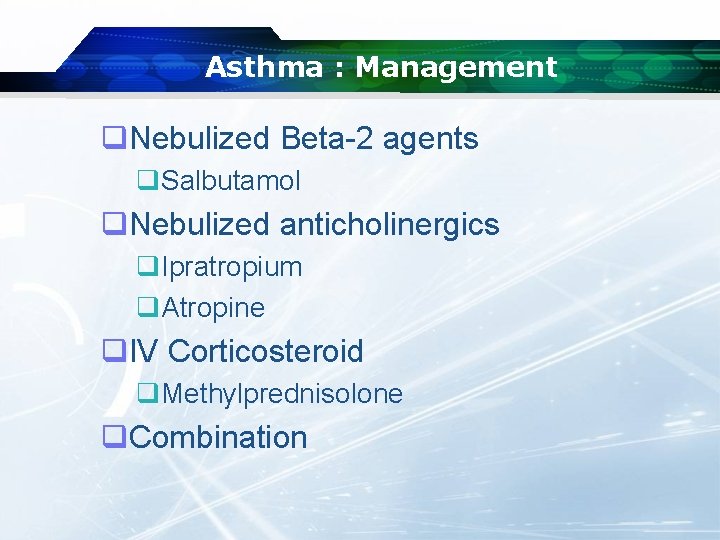
Asthma : Management q. Nebulized Beta-2 agents q. Salbutamol q. Nebulized anticholinergics q. Ipratropium q. Atropine q. IV Corticosteroid q. Methylprednisolone q. Combination
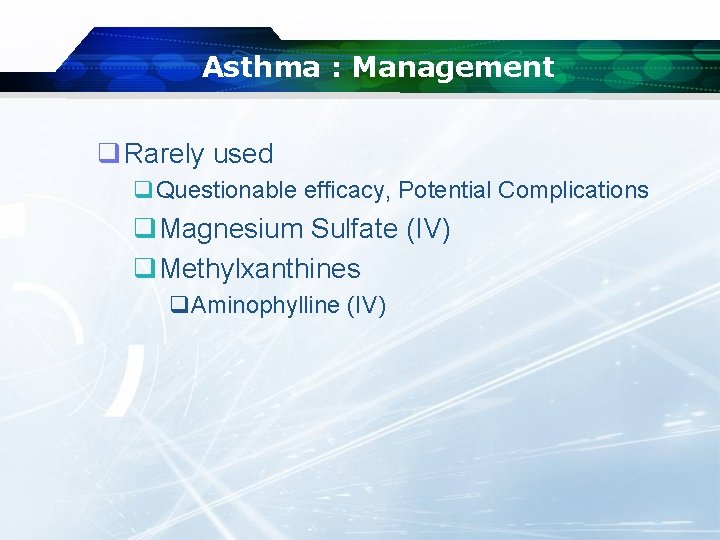
Asthma : Management q Rarely used q. Questionable efficacy, Potential Complications q. Magnesium Sulfate (IV) q. Methylxanthines q. Aminophylline (IV)
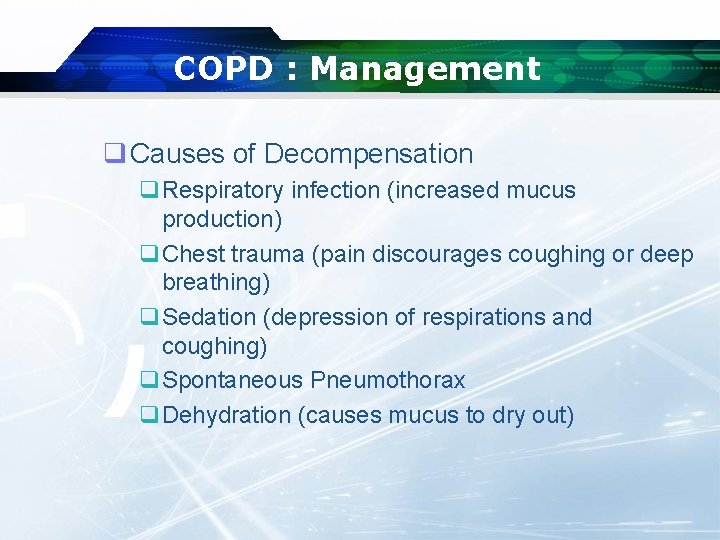
COPD : Management q Causes of Decompensation q. Respiratory infection (increased mucus production) q. Chest trauma (pain discourages coughing or deep breathing) q. Sedation (depression of respirations and coughing) q. Spontaneous Pneumothorax q. Dehydration (causes mucus to dry out)
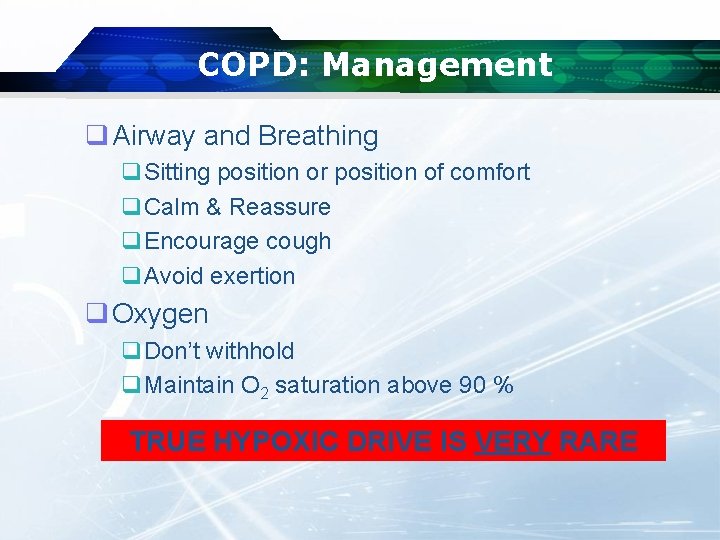
COPD: Management q Airway and Breathing q. Sitting position or position of comfort q. Calm & Reassure q. Encourage cough q. Avoid exertion q Oxygen q. Don’t withhold q. Maintain O 2 saturation above 90 % TRUE HYPOXIC DRIVE IS VERY RARE
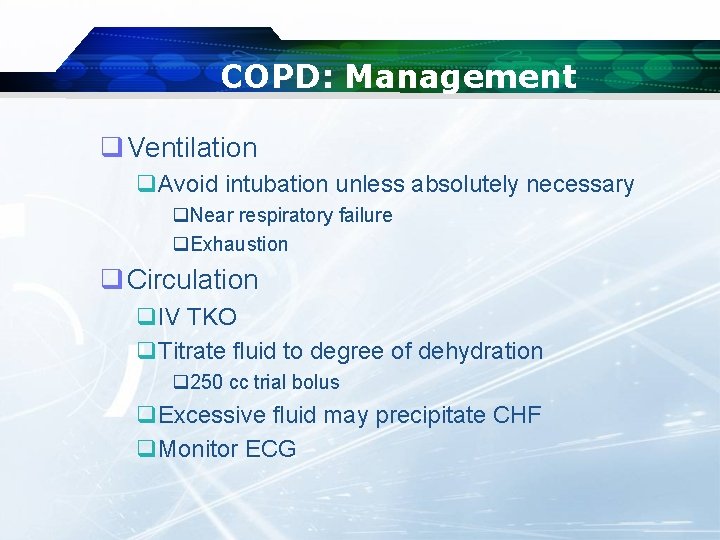
COPD: Management q Ventilation q. Avoid intubation unless absolutely necessary q. Near respiratory failure q. Exhaustion q Circulation q. IV TKO q. Titrate fluid to degree of dehydration q 250 cc trial bolus q. Excessive fluid may precipitate CHF q. Monitor ECG
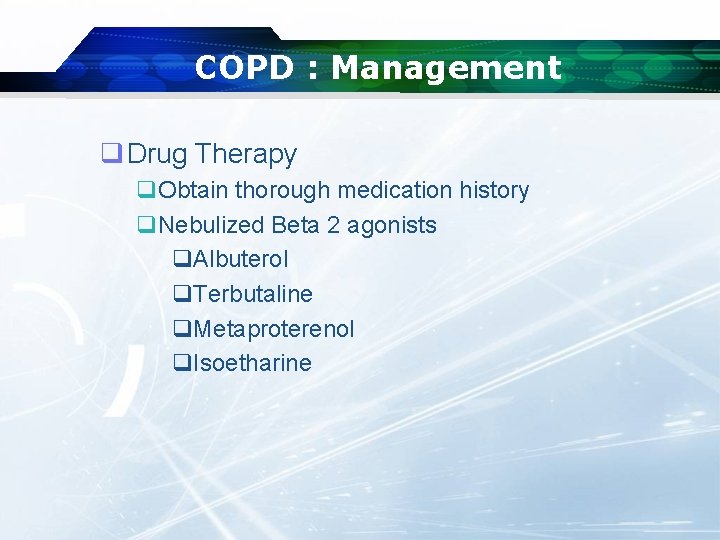
COPD : Management q Drug Therapy q. Obtain thorough medication history q. Nebulized Beta 2 agonists q. Albuterol q. Terbutaline q. Metaproterenol q. Isoetharine
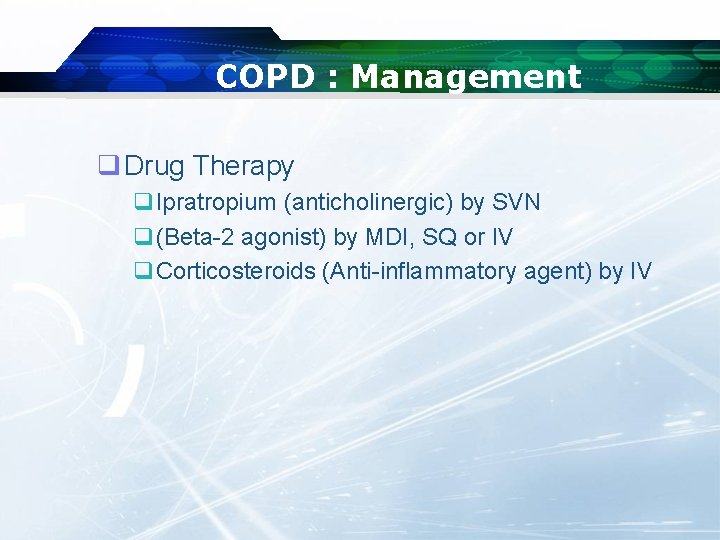
COPD : Management q Drug Therapy q. Ipratropium (anticholinergic) by SVN q(Beta-2 agonist) by MDI, SQ or IV q. Corticosteroids (Anti-inflammatory agent) by IV
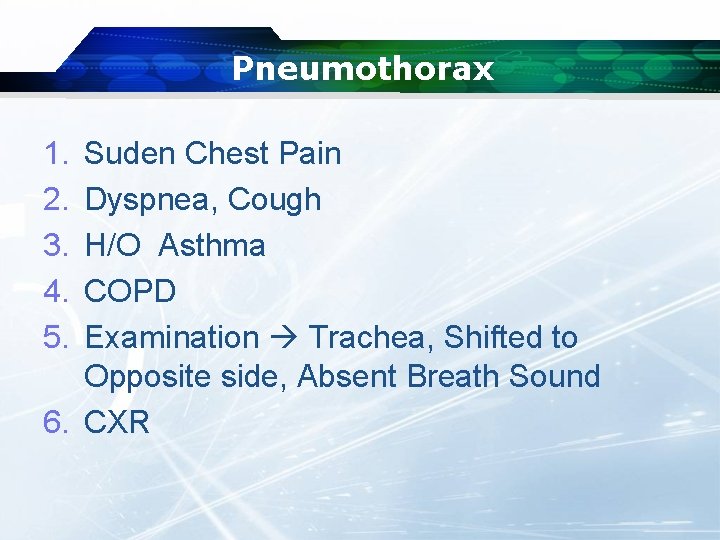
Pneumothorax 1. 2. 3. 4. 5. Suden Chest Pain Dyspnea, Cough H/O Asthma COPD Examination Trachea, Shifted to Opposite side, Absent Breath Sound 6. CXR
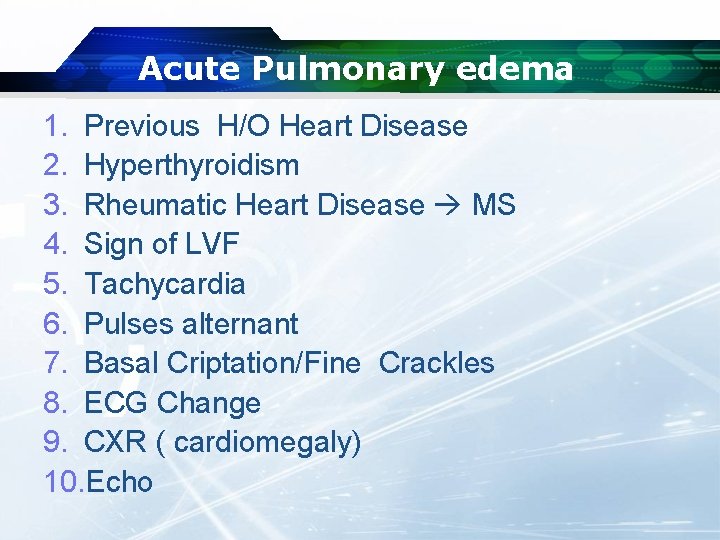
Acute Pulmonary edema 1. Previous H/O Heart Disease 2. Hyperthyroidism 3. Rheumatic Heart Disease MS 4. Sign of LVF 5. Tachycardia 6. Pulses alternant 7. Basal Criptation/Fine Crackles 8. ECG Change 9. CXR ( cardiomegaly) 10. Echo
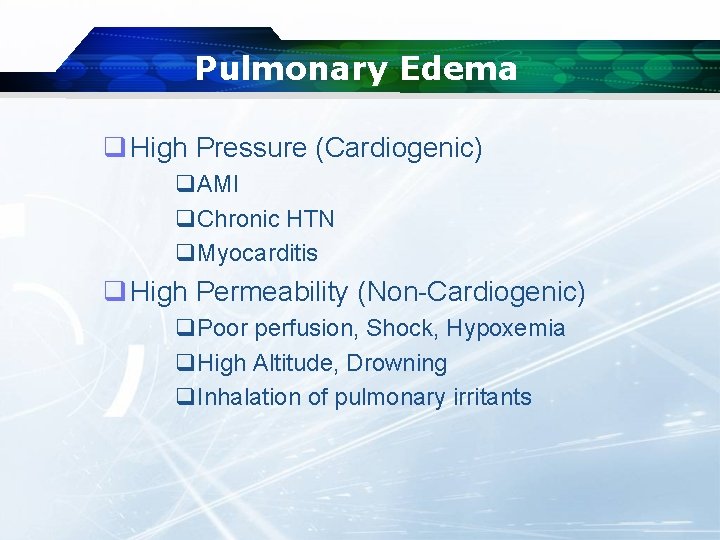
Pulmonary Edema q High Pressure (Cardiogenic) q. AMI q. Chronic HTN q. Myocarditis q High Permeability (Non-Cardiogenic) q. Poor perfusion, Shock, Hypoxemia q. High Altitude, Drowning q. Inhalation of pulmonary irritants

Cardiogenic Pulmonary Edema: Etiology q Left ventricular failure q Valvular heart disease q. Stenosis q. Insufficiency q Hypertensive crisis (high afterload) q Volume overload Increased Pressure in Pulmonary Vascular Bed
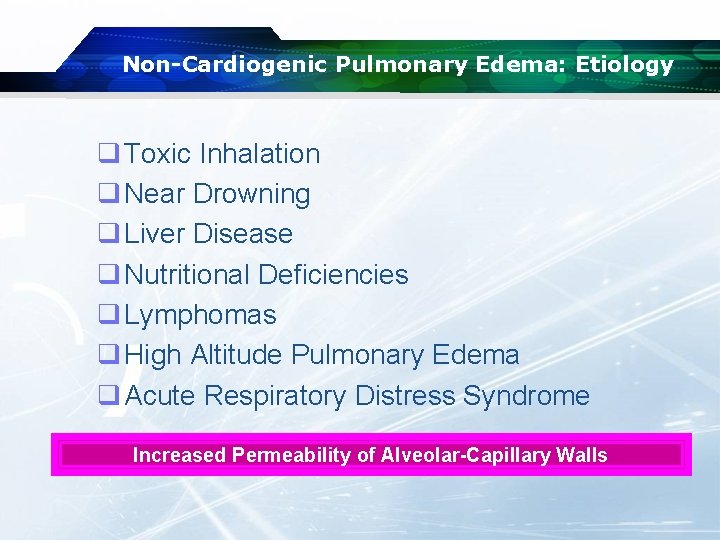
Non-Cardiogenic Pulmonary Edema: Etiology q Toxic Inhalation q Near Drowning q Liver Disease q Nutritional Deficiencies q Lymphomas q High Altitude Pulmonary Edema q Acute Respiratory Distress Syndrome Increased Permeability of Alveolar-Capillary Walls
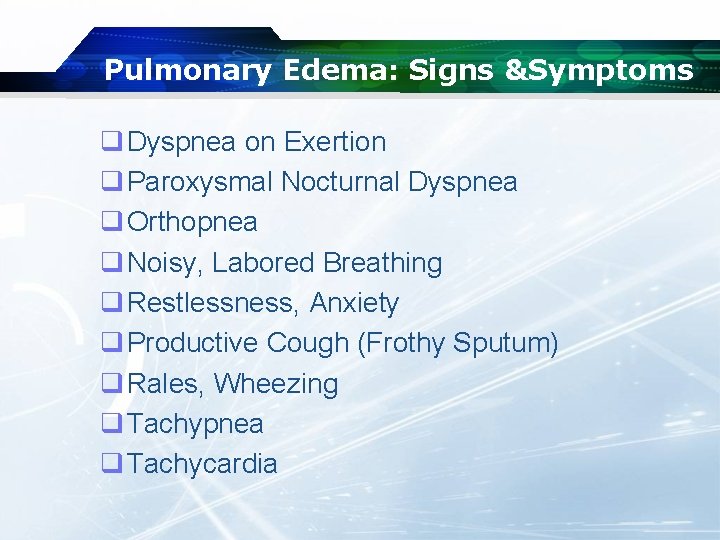
Pulmonary Edema: Signs &Symptoms q Dyspnea on Exertion q Paroxysmal Nocturnal Dyspnea q Orthopnea q Noisy, Labored Breathing q Restlessness, Anxiety q Productive Cough (Frothy Sputum) q Rales, Wheezing q Tachypnea q Tachycardia
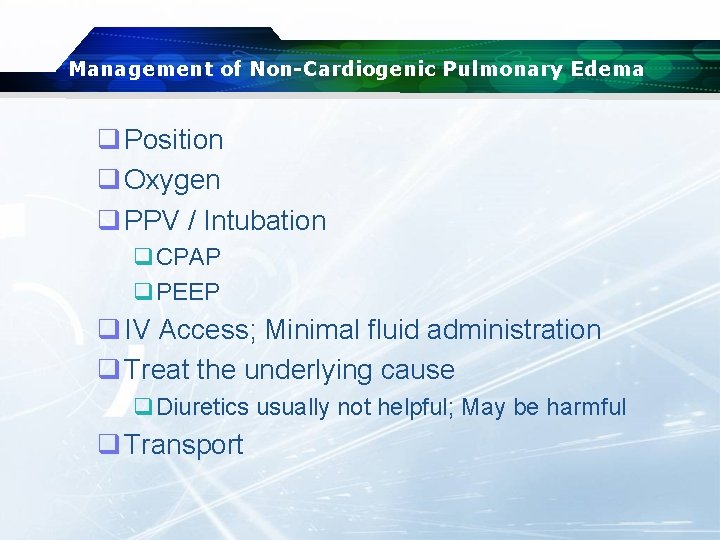
Management of Non-Cardiogenic Pulmonary Edema q Position q Oxygen q PPV / Intubation q. CPAP q. PEEP q IV Access; Minimal fluid administration q Treat the underlying cause q. Diuretics usually not helpful; May be harmful q Transport
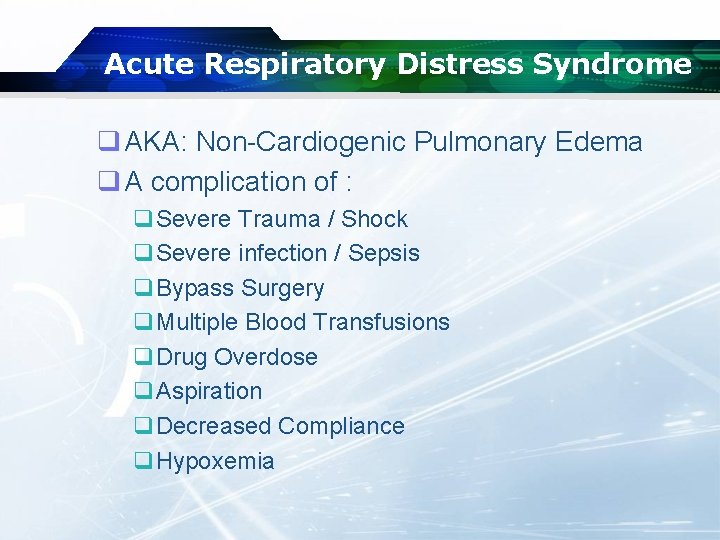
Acute Respiratory Distress Syndrome q AKA: Non-Cardiogenic Pulmonary Edema q A complication of : q. Severe Trauma / Shock q. Severe infection / Sepsis q. Bypass Surgery q. Multiple Blood Transfusions q. Drug Overdose q. Aspiration q. Decreased Compliance q. Hypoxemia
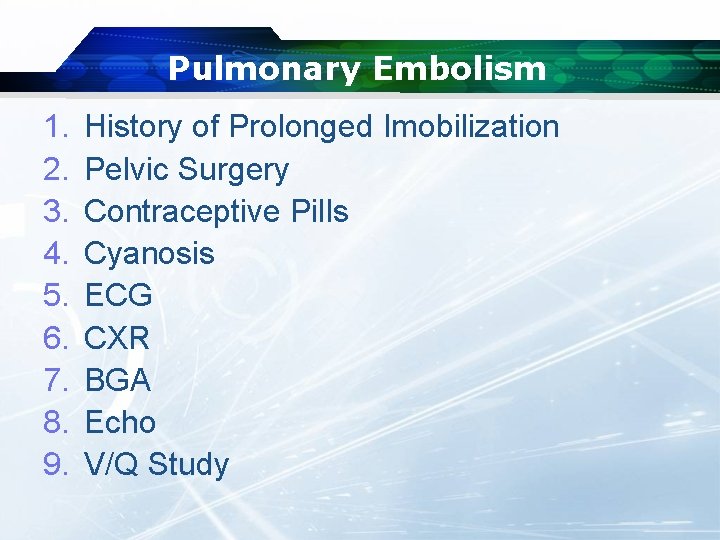
Pulmonary Embolism 1. 2. 3. 4. 5. 6. 7. 8. 9. History of Prolonged Imobilization Pelvic Surgery Contraceptive Pills Cyanosis ECG CXR BGA Echo V/Q Study
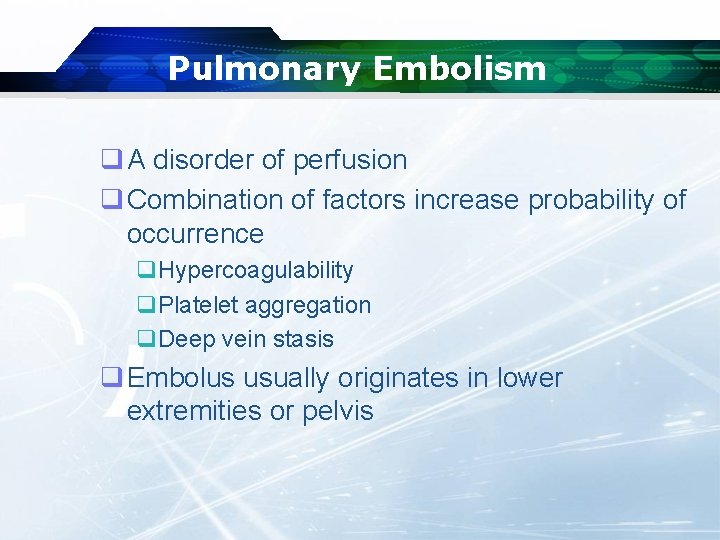
Pulmonary Embolism q A disorder of perfusion q Combination of factors increase probability of occurrence q. Hypercoagulability q. Platelet aggregation q. Deep vein stasis q Embolus usually originates in lower extremities or pelvis
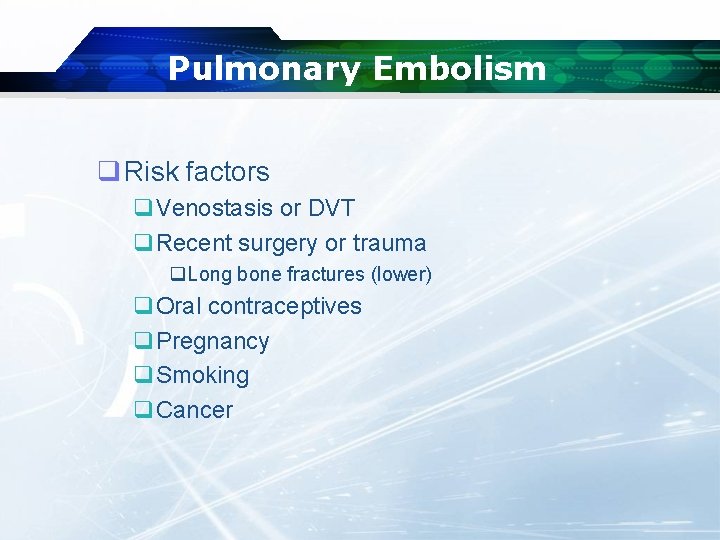
Pulmonary Embolism q Risk factors q. Venostasis or DVT q. Recent surgery or trauma q. Long bone fractures (lower) q. Oral contraceptives q. Pregnancy q. Smoking q. Cancer
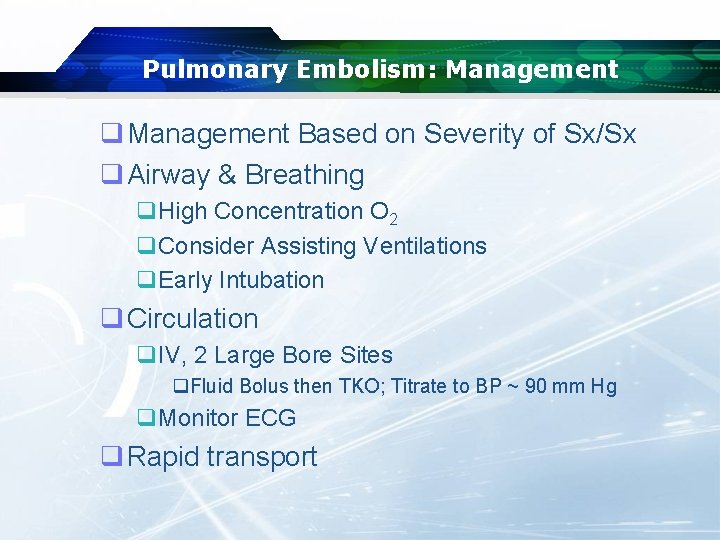
Pulmonary Embolism: Management q Management Based on Severity of Sx/Sx q Airway & Breathing q. High Concentration O 2 q. Consider Assisting Ventilations q. Early Intubation q Circulation q. IV, 2 Large Bore Sites q. Fluid Bolus then TKO; Titrate to BP ~ 90 mm Hg q. Monitor ECG q Rapid transport
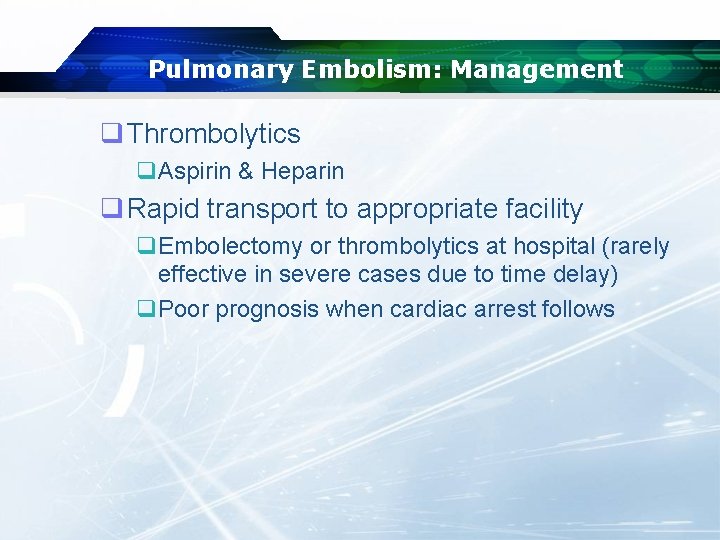
Pulmonary Embolism: Management q Thrombolytics q. Aspirin & Heparin q Rapid transport to appropriate facility q. Embolectomy or thrombolytics at hospital (rarely effective in severe cases due to time delay) q. Poor prognosis when cardiac arrest follows
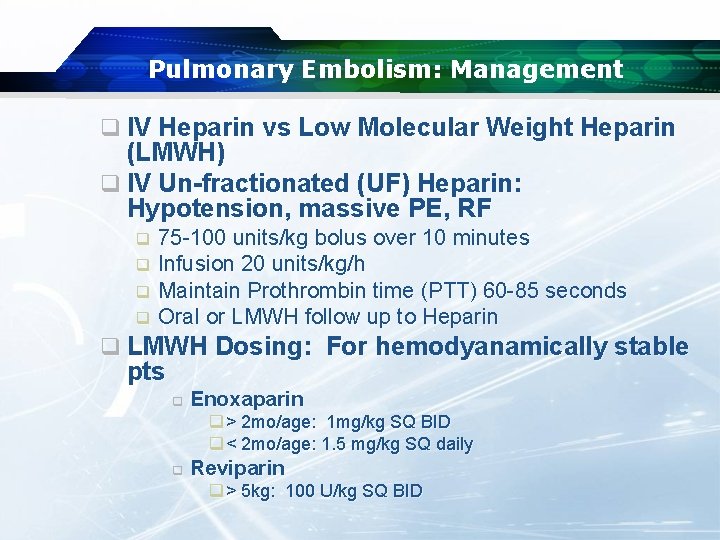
Pulmonary Embolism: Management q IV Heparin vs Low Molecular Weight Heparin (LMWH) q IV Un-fractionated (UF) Heparin: Hypotension, massive PE, RF q q 75 -100 units/kg bolus over 10 minutes Infusion 20 units/kg/h Maintain Prothrombin time (PTT) 60 -85 seconds Oral or LMWH follow up to Heparin q LMWH Dosing: For hemodyanamically stable pts q Enoxaparin q > 2 mo/age: 1 mg/kg SQ BID q < 2 mo/age: 1. 5 mg/kg SQ daily q Reviparin q > 5 kg: 100 U/kg SQ BID
Pleurisy q Inflammation of pleura caused by a friction rub q. Layers of pleura rubbing together q Commonly associated with other respiratory disease
Presentation of Pleurisy q Sharp, sudden and intermittent chest pain with related dyspnea q. Possibly referred to shoulder q. May or with respiration q Pleural “friction rub” may be audible” q May have effusion or be dry
Pleurisy q. Management q. Based upon severity of presentation q. Mostly supportive
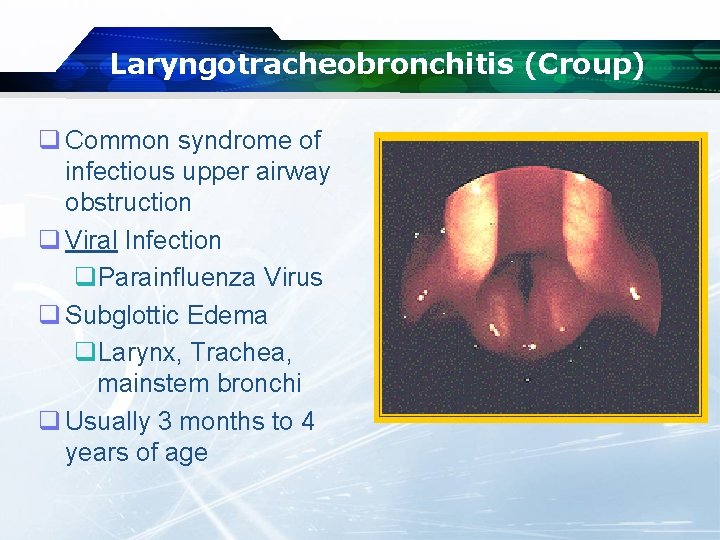
Laryngotracheobronchitis (Croup) q Common syndrome of infectious upper airway obstruction q Viral Infection q. Parainfluenza Virus q Subglottic Edema q. Larynx, Trachea, mainstem bronchi q Usually 3 months to 4 years of age
Croup: Management q Usually requires little out of home treatment q Calm & Prevent agitation q Moist cool air - mist q Humidified O 2 by mask or blowby q Do Not Examine Upper Airways
Croup: Management q If in respiratory distress: q. Racemic epinephrine via nebulizer q. Decreases subglottic edema (temporarily) q. Necessitates transport for observation for rebound q. IV TKO - ONLY if severe respiratory distress q. Transport
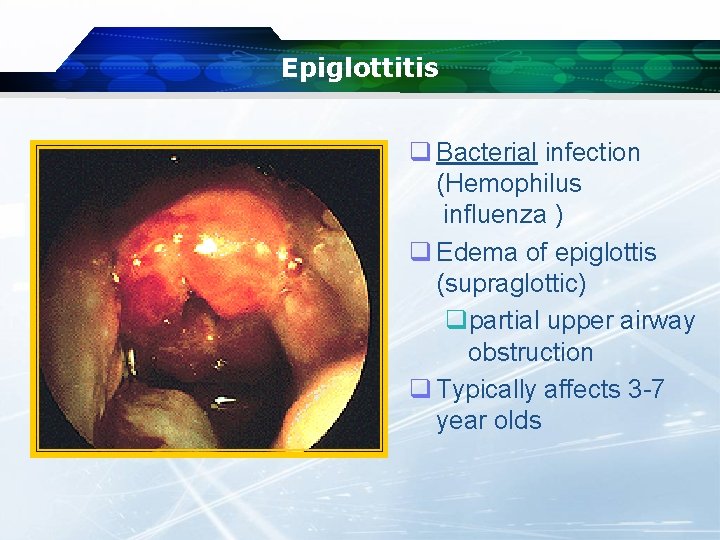
Epiglottitis q Bacterial infection (Hemophilus influenza ) q Edema of epiglottis (supraglottic) qpartial upper airway obstruction q Typically affects 3 -7 year olds
Epiglottitis: Management Immediate life threat (8 -12% die from airway obstruction) v Do NOT attempt to visualize airway v Allow child to assume position of comfort § AVOID agitation of the child § AVOID anxiety of the healthcare providers v O 2 by high concentration mask
Epiglottitis: Management q If respiratory failure is eminent: q. IV TKO ONLY if eminent or respiratory arrest q. Be prepared to take control of airway q. Intubation equipment with smaller sized tubes q. Needle cricothyrotomy & jet ventilation equipment q Rapid but calm transport q. Appropriate facility
Upper Respiratory Infection q Common illness q Rarely life-threatening q Often exacerbates underlying pulmonary conditions q May become more significant in some patients q. Immunosuppressed q. Elderly q. Chronic pulmonary disease
Management of URI q Usually requires no intervention q Oxygen if underlying condition has been exacerbated q Rarely, pharmacologic interventions are required q. Bronchodilators q. Corticosteroid
LOGO Hyperventilation Syndrome
Hyperventilation Syndrome q A diagnosis of EXCLUSION!!! q An increased ventilatory rate that q. DOES NOT have a pathologic origin q. Results from anxiety q Remains a real problem for the patient
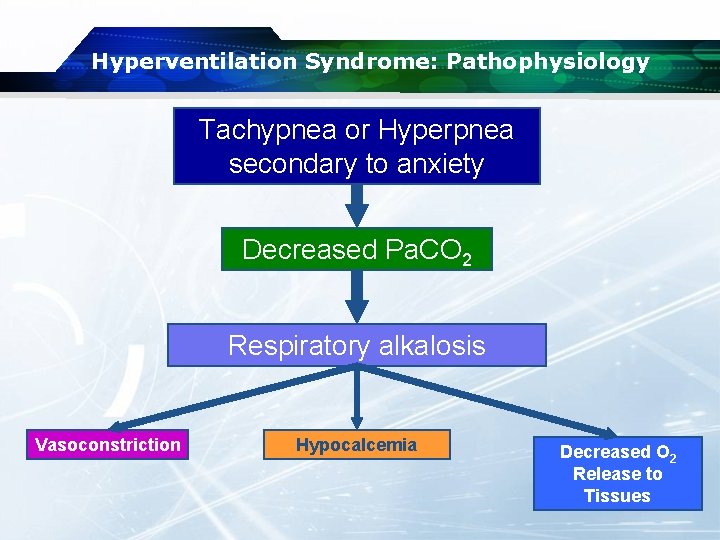
Hyperventilation Syndrome: Pathophysiology Tachypnea or Hyperpnea secondary to anxiety Decreased Pa. CO 2 Respiratory alkalosis Vasoconstriction Hypocalcemia Decreased O 2 Release to Tissues
Hyperventilation Syndrome : Signs & Symptoms q. Light-headedness, giddiness, anxiety q. Numbness, paresthesias of: q. Hands q. Feet q. Circumoral area q. Cold hands, feet q. Carpopedal spasms q. Dyspnea q. Chest pain
Hyperventilation Syndrome : Signs & Symptoms q Signs q. Rapid breathing q. Cool & possibly pale skin q. Carpopedal spasm q. Dysrhythmias q. Sinus Tachycardia q. SVT q. Sinus arrhythmia q. Loss of consciousness and seizures (late & rare)
Hyperventilation Syndrome : Management q Educate patient & family q. Consider possible psychopathology especially in “repeat customers” q Transport occasionally required q. If loss of consciousness, carpopedal spasm, muscle twitching, or seizures occur: q. Monitor EKG q. IV TKO q. Transport
LOGO Hyperventilation Syndrome Serious diseases can mimic hyperventilation Hyperventilation itself can be serious
LOGO Central Respiratory Depression
Respiratory Depression : Causes q Head trauma q CVA q Depressant drug toxicity q. Narcotics q. Barbiturates q. Benzodiazepines q. ETOH
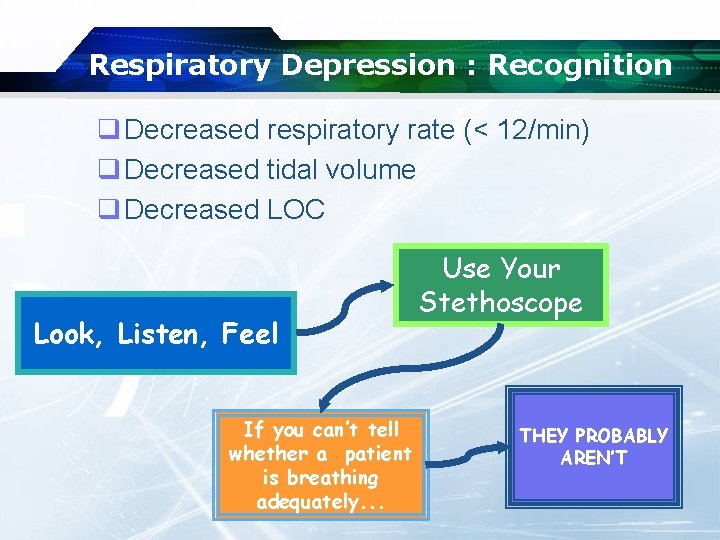
Respiratory Depression : Recognition q Decreased respiratory rate (< 12/min) q Decreased tidal volume q Decreased LOC Look, Listen, Feel If you can’t tell whether a patient is breathing adequately. . . Use Your Stethoscope THEY PROBABLY AREN’T
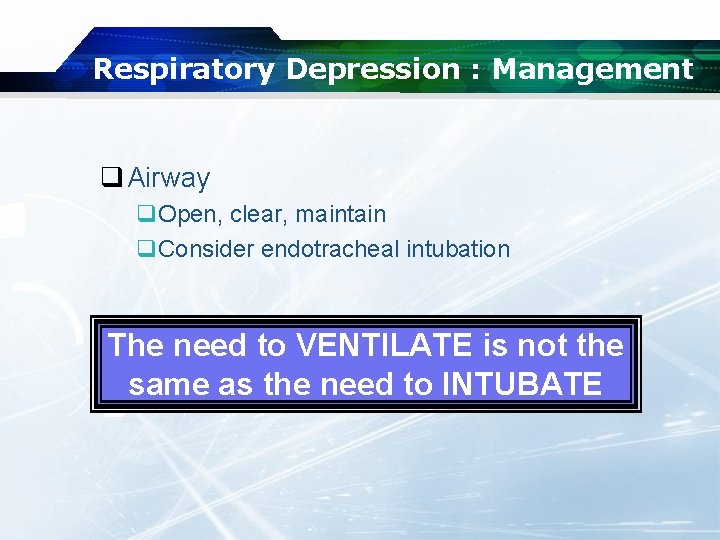
Respiratory Depression : Management q Airway q. Open, clear, maintain q. Consider endotracheal intubation The need to VENTILATE is not the same as the need to INTUBATE
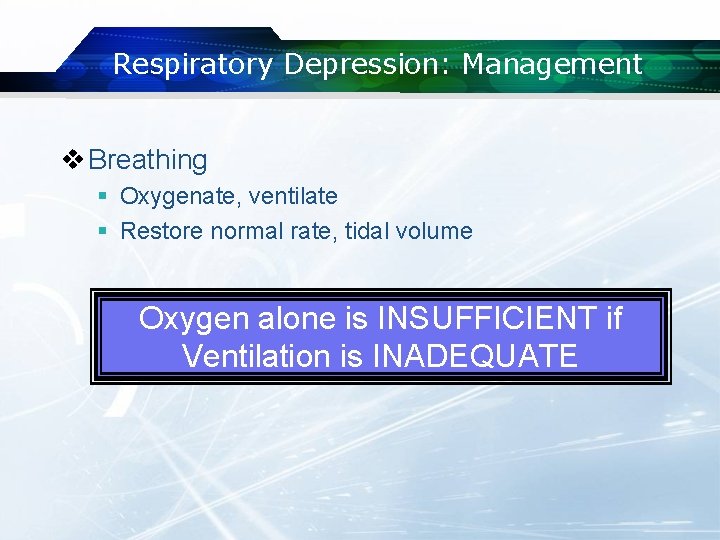
Respiratory Depression: Management v Breathing § Oxygenate, ventilate § Restore normal rate, tidal volume Oxygen alone is INSUFFICIENT if Ventilation is INADEQUATE
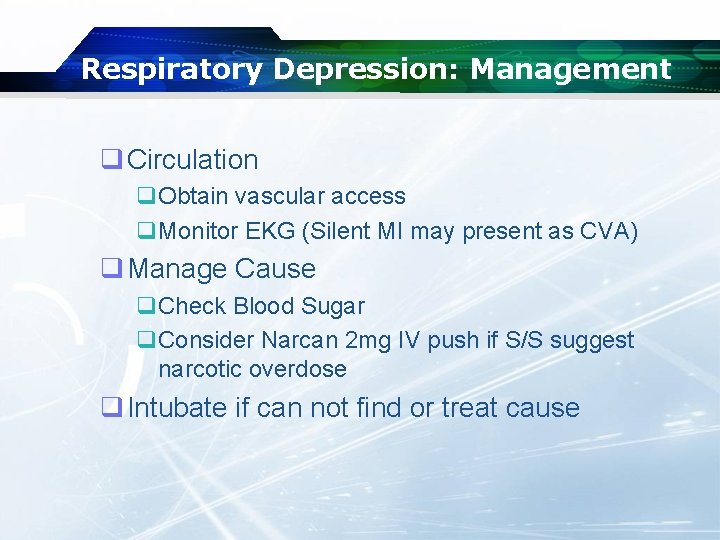
Respiratory Depression: Management q Circulation q. Obtain vascular access q. Monitor EKG (Silent MI may present as CVA) q Manage Cause q. Check Blood Sugar q. Consider Narcan 2 mg IV push if S/S suggest narcotic overdose q Intubate if can not find or treat cause
Guillian-Barre´ Syndrome q Autoimmune disease q. Leads to inflammation and degeneration of sensory and motor nerve roots (demyelination) q Progressive ascending paralysis q. Progressive tingling and weakness q. Moves from extremities then proximally q. May lead to respiratory paralysis (25%)
Guillian-Barre´ Syndrome Management q Treatment based on severity of symptoms q. Control airway q. Support ventilation q. Oxygen q. Transport in cases of respiratory depression, distress or arrest
Myasthenia Gravis q Autoimmune disease q Causes loss of ACh receptors at neuromuscular junction q. Attacks the ACh transport mechanism at the NMJ q Episodes of extreme skeletal muscle weakness q Can cause loss of control of airway, respiratory paralysis
Myasthenia Gravis Presentation q Gradual onset of muscle weakness q. Face and throat q. Extreme muscle weakness q Respiratory weakness -> paralysis q Inability to process mucus
Myasthenia Gravis Management q Treat symptomatically q Watch for aspiration q May require assisted ventilations q Assess for Pulmonary infection q Transport based upon severity of presentation q Plasmapharesis

LOGO
- Slides: 93