Hemostatic System general information Normal hemostatic system vessel
- Slides: 12
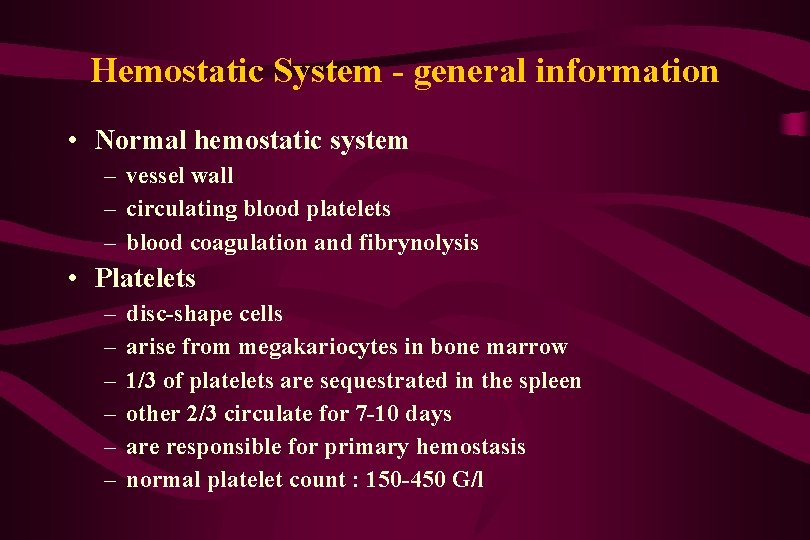
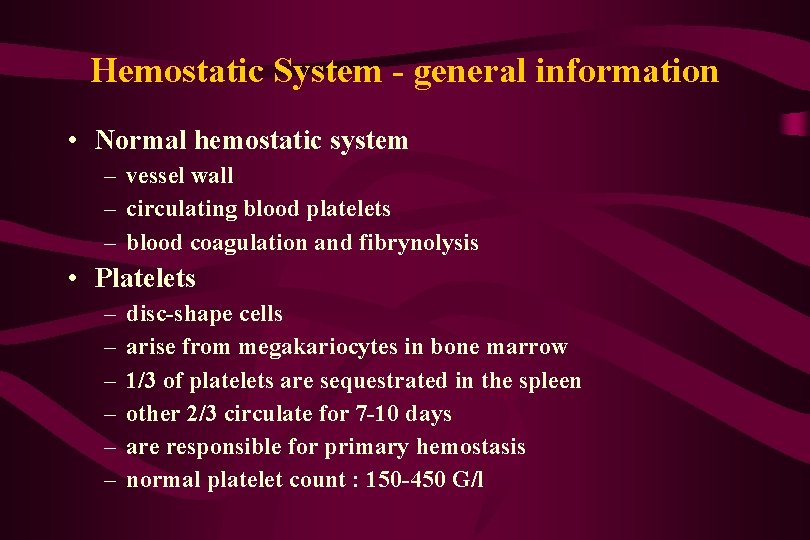
Hemostatic System - general information • Normal hemostatic system – vessel wall – circulating blood platelets – blood coagulation and fibrynolysis • Platelets – – – disc-shape cells arise from megakariocytes in bone marrow 1/3 of platelets are sequestrated in the spleen other 2/3 circulate for 7 -10 days are responsible for primary hemostasis normal platelet count : 150 -450 G/l
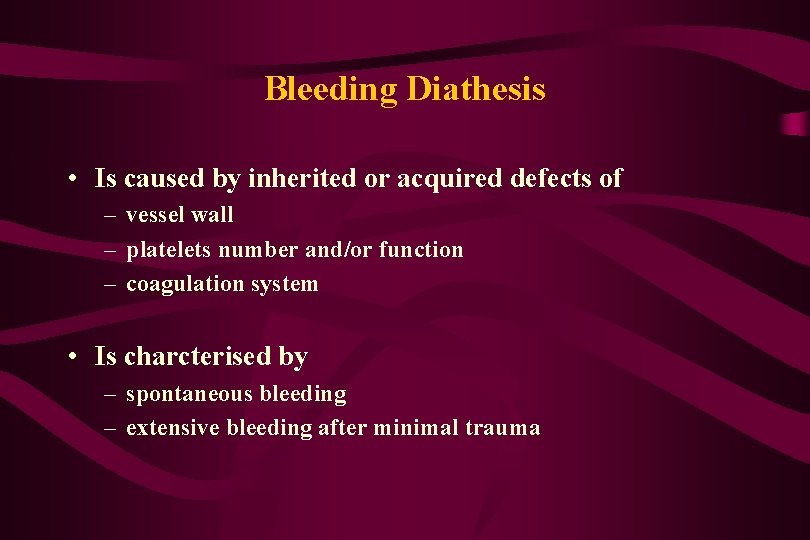
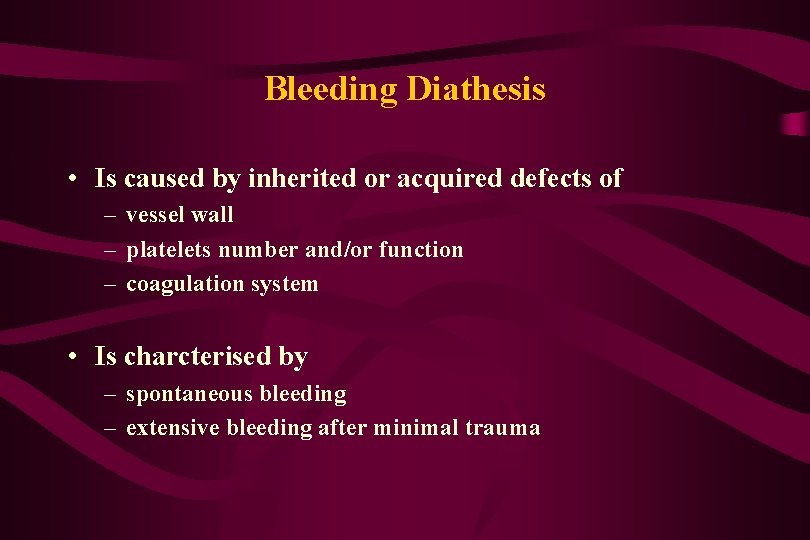
Bleeding Diathesis • Is caused by inherited or acquired defects of – vessel wall – platelets number and/or function – coagulation system • Is charcterised by – spontaneous bleeding – extensive bleeding after minimal trauma
Platelets Disorder • Disorder of platelet number – thrombocytopenia – thrombocytosis • Disorder of platelet function
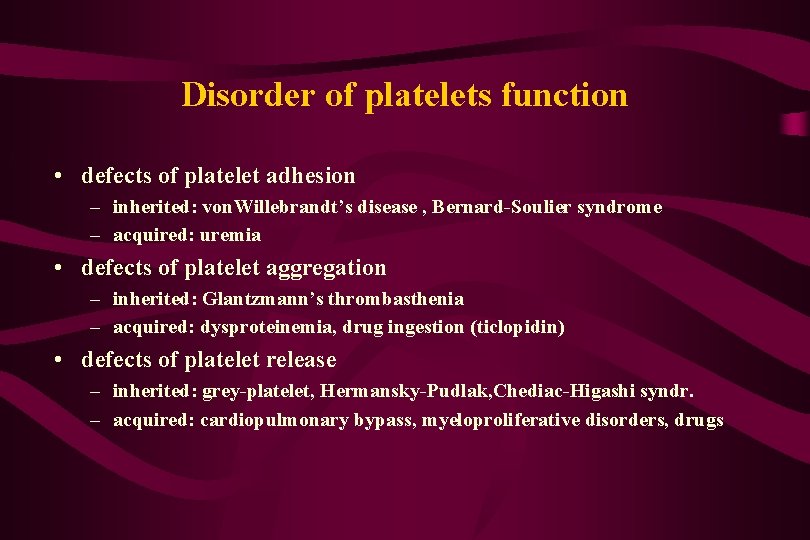
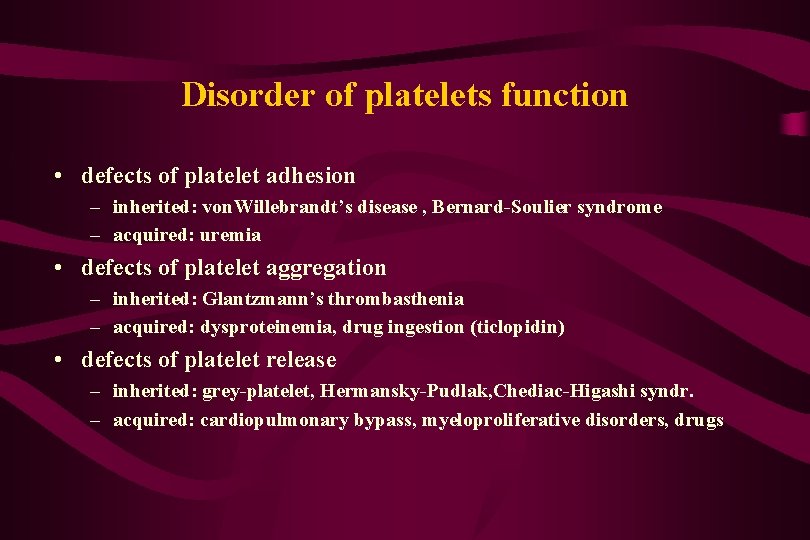
Disorder of platelets function • defects of platelet adhesion – inherited: von. Willebrandt’s disease , Bernard-Soulier syndrome – acquired: uremia • defects of platelet aggregation – inherited: Glantzmann’s thrombasthenia – acquired: dysproteinemia, drug ingestion (ticlopidin) • defects of platelet release – inherited: grey-platelet, Hermansky-Pudlak, Chediac-Higashi syndr. – acquired: cardiopulmonary bypass, myeloproliferative disorders, drugs
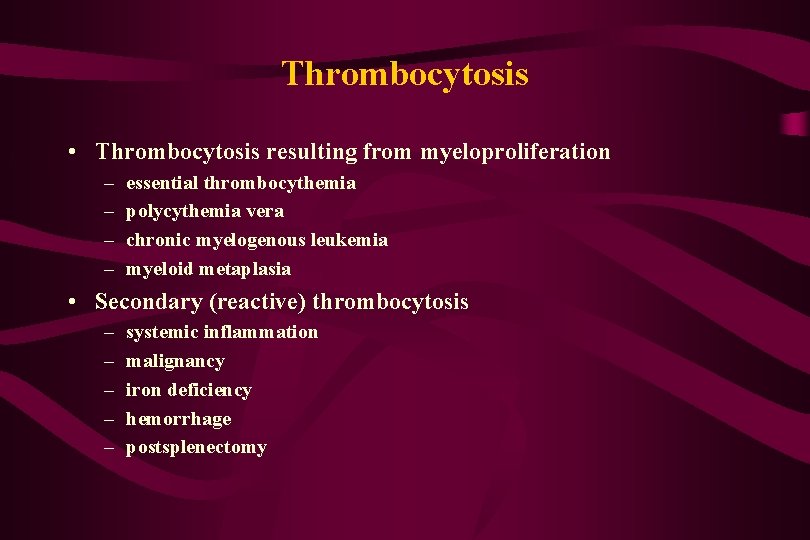
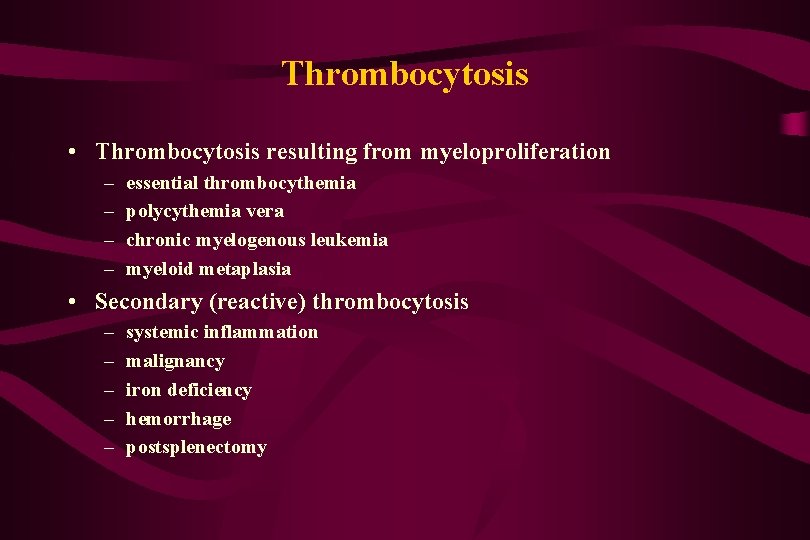
Thrombocytosis • Thrombocytosis resulting from myeloproliferation – – essential thrombocythemia polycythemia vera chronic myelogenous leukemia myeloid metaplasia • Secondary (reactive) thrombocytosis – – – systemic inflammation malignancy iron deficiency hemorrhage postsplenectomy
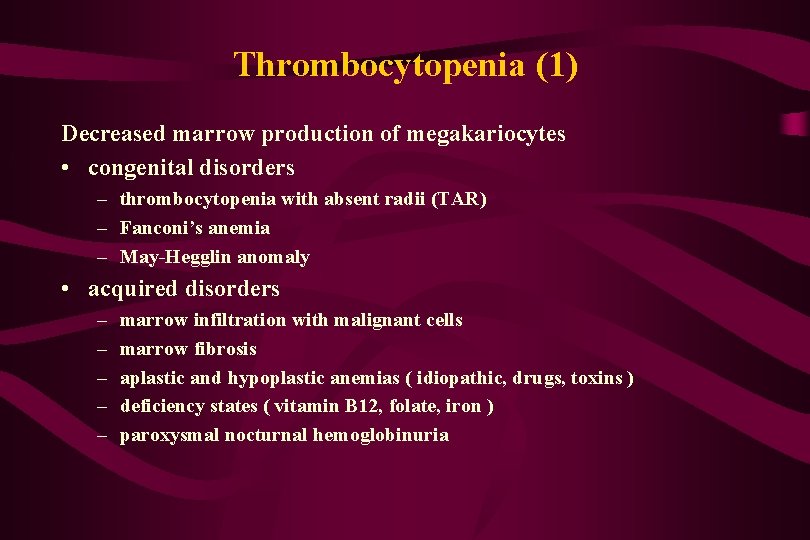
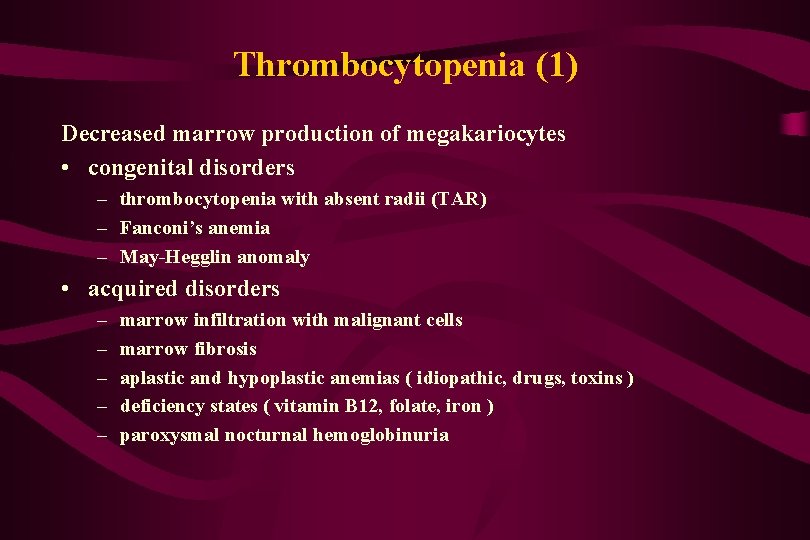
Thrombocytopenia (1) Decreased marrow production of megakariocytes • congenital disorders – thrombocytopenia with absent radii (TAR) – Fanconi’s anemia – May-Hegglin anomaly • acquired disorders – – – marrow infiltration with malignant cells marrow fibrosis aplastic and hypoplastic anemias ( idiopathic, drugs, toxins ) deficiency states ( vitamin B 12, folate, iron ) paroxysmal nocturnal hemoglobinuria
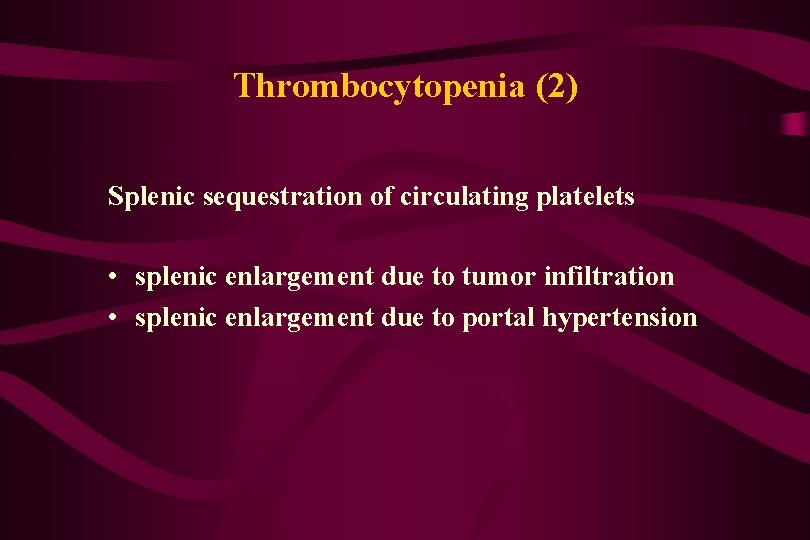
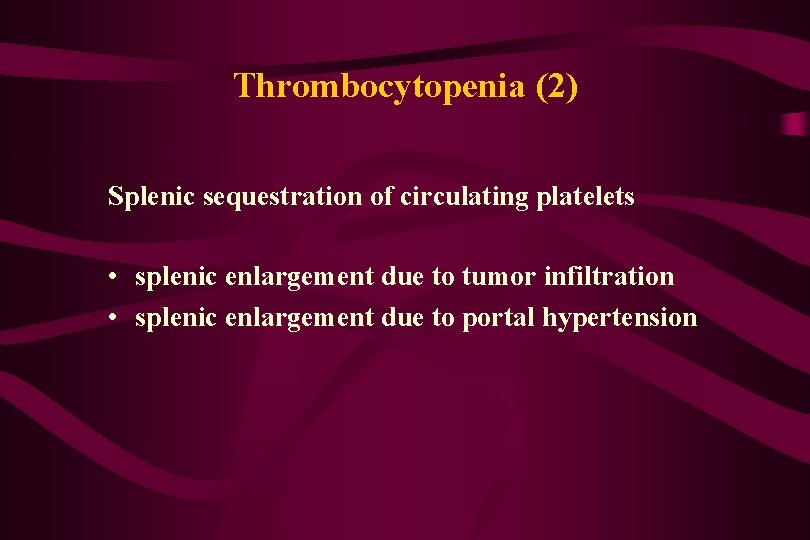
Thrombocytopenia (2) Splenic sequestration of circulating platelets • splenic enlargement due to tumor infiltration • splenic enlargement due to portal hypertension
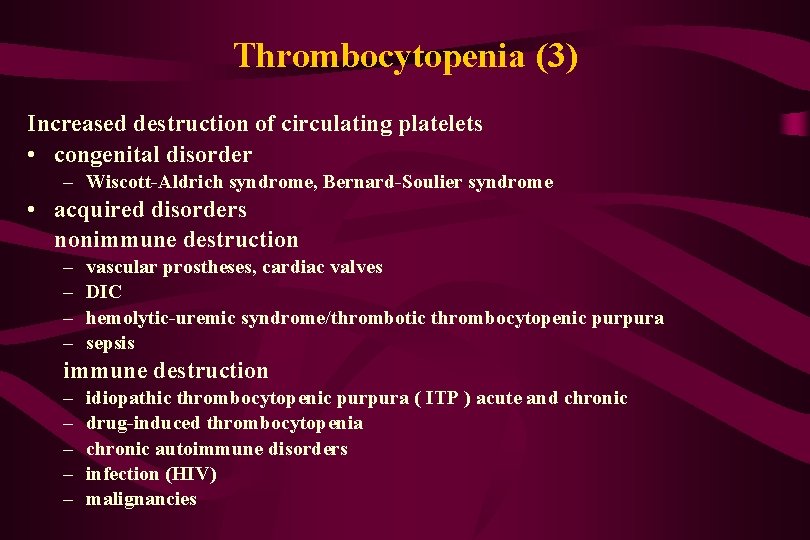
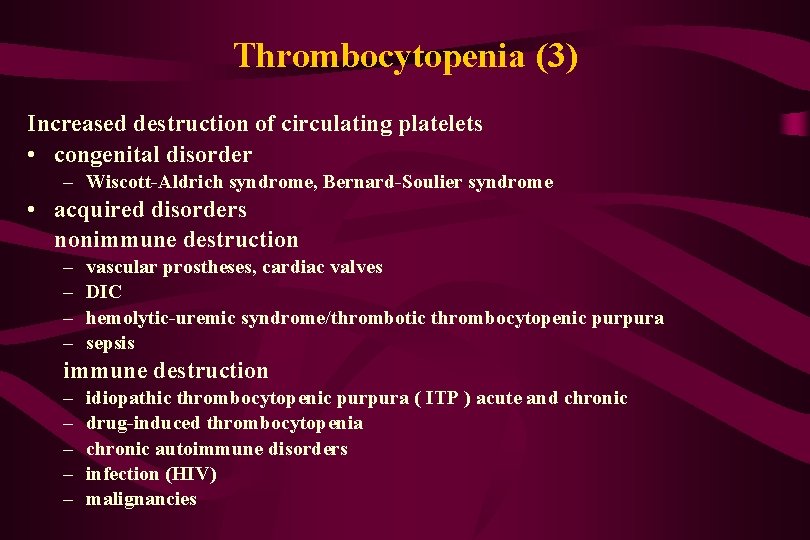
Thrombocytopenia (3) Increased destruction of circulating platelets • congenital disorder – Wiscott-Aldrich syndrome, Bernard-Soulier syndrome • acquired disorders nonimmune destruction – – vascular prostheses, cardiac valves DIC hemolytic-uremic syndrome/thrombotic thrombocytopenic purpura sepsis immune destruction – – – idiopathic thrombocytopenic purpura ( ITP ) acute and chronic drug-induced thrombocytopenia chronic autoimmune disorders infection (HIV) malignancies
Platelets Disorder - signs and symptoms • asymptomatic if platelets count > 50 G/l • onset of bleeding after trauma - immediate • site of bleeding - superficial: skin, mucous membranes, nose, genitourinary tract • physical finding - petechiae, ecchymoses
Idiopathic Thrombocytopenic Purpura (1) • the most common cause of isolated thrombocytopenia • autoimmune disease with antiplatelet antibodies and shortened platelets life span • forms of ITP acute ITP – children (90% of pediatric case of immune thrombocytopenia) – preceded by viral infection – spontaneous recovery within 4 -6 weeks in 60% of patients chronic ITP – 20 -40 years – women predominance F: M=3: 1
Idiopathic Thrombocytopenic Purpura (2) • Clinical features – – – petechiae ecchymoses mucose membranes bleeding menorrhagia rare internal, intracranial bleeding • Diagnosis – – platelet count <100 G/l bleeding time - usually normal peripheral blood smear - large platelets bone marrow examination - normal or increased number of megakariocytes – antibodies against Gp IIb/IIIa – shortened platelet survival
Treatment of ITP • not necessary unless platelets count > 20 G/l or there is extensive bleeding • corticosteroids permanent responses - 30% – prednisone 1 mg/kg for 4 -6 weeks • • splenectomy permanent responses - 60% immunosuppresive drugs intravenous immunoglobulins other - danazol, anti. Rh. D