HEMORRHAGE Hemorrhage Hemorrhage Abnormal internal or external loss

HEMORRHAGE
Hemorrhage • Hemorrhage – Abnormal internal or external loss of blood
Causes Traumatic Injury • Abrasion - Also called a graze, this is caused by transverse action of a foreign object against the skin, and usually does not penetrate below the epidermis • Excoriation - In common with Abrasion, this is caused by mechanical destruction of the skin, although it usually has an underlying medical cause • Hematoma - Caused by damage to a blood vessel that in turn causes blood to collect under the skin. • Laceration - Irregular wound caused by blunt impact to soft tissue overlying hard tissue or tearing such as in childbirth. In some instances, this can also be used to describe an incision.
• Incision - A cut into a body tissue or organ, such as by a scalpel, made during surgery. • Puncture Wound - Caused by an object that penetrated the skin and underlying layers, such as a nail, needle or knife • Contusion - Also known as a bruise, this is a blunt trauma damaging tissue under the surface of the skin.
• Crushing Injuries - Caused by a great or extreme amount of force applied over a period of time. The extent of a crushing injury may not immediately present itself. • Ballistic Trauma - Caused by a projectile weapon such as a firearm. This may include two external wounds (entry and exit) and a contiguous wound between the two.

Hemorrhage Classification
External Hemorrhage • Results from soft tissue injury • The seriousness of the injury is dependent on: – Anatomical source of the hemorrhage (arterial, venous, capillary) – Degree of vascular disruption – Amount of blood loss that can be tolerated by the patient
Internal Hemorrhage • Can result from: – Blunt or penetrating trauma – Acute or chronic medical illnesses • Internal bleeding that can cause hemodynamic instability usually occurs in one of four body cavities: – Chest – Abdomen – Pelvis – Retroperitoneum
Internal Hemorrhage • Signs and symptoms : – Bright red blood from mouth, rectum, or other orifice – Coffee-ground appearance of vomitus – Melena (black, tarry stools) – Dizziness or syncope on sitting or standing – Orthostatic hypotension
Internal hemorrhage is associated with higher morbidity and mortality than external hemorrhage.
Revealed Hemorrhage • Revealed Hemorrhage is obvious external hemorrhage, result from 1 - Exsanguination from open arterial wound 2 - From massive haemetemesis 3 - From duodenal ulcer

Concealed Hemorrhage • Concealed hemorrhage is contained within the body cavity and must be suspected. Concealed hemorrhage may be 1 - Traumatic concealed hemorrhage 2 - Non – Traumatic concealed hemorrhage • In trauma hemorrhage may be concealed within the chest, abdominal cavity, pelvis, retroperitonium or in limbus may be associated with concealed vascular injury and log bone fracture. • Non – traumatic concealed hemorrhage include GIT bleeding & rupture aortic aneurysm
Primary Hemorrhage • Hemorrhage occurring immediately as result of an injury or surgery is recognized as “ primary hemorrhage”
Recreationary Hemorrhage • Recreationary hemorrhage is delayed hemorrhage within 24 hours and usually caused by the 1 - Dislodgement of clot by the resuscitation 2 - Normalization of blood pressure 3 - Vasodilatation (cessation of reflex vasospasm) 4 - Technical failure such as slippage of ligature
Secondary Hemorrhage • Secondary hemorrhage is caused by the sloughing of the wall of vessels • It usually occurs 7 – 14 days after the injury and precipitated by the factors such as 1 - Infection 2 - Pressure necrosis (result from drain) 3 - Malignancy
Surgical & Non-surgical hemorrhage • Surgical hemorrhage is the result of injury and amenable to surgical control, or from angioembolism • Non – surgical hemorrhage is general ooze from all raw surface due to coagulopathy, it can not be stopped by surgical mean, require correction coagulation abnormalities • Note: Packing can stop non-surgical hemorrhage
Degree of hemorrhage Class I Hemorrhage • involves up to 15% of blood volume. • There is typically no change in vital signs and fluid resuscitation is not usually necessary. Class II Hemorrhage • involves 15 -30% of total blood volume. • A patient is often tachycardic (rapid heart beat) with a narrowing of the difference between the systolic and diastolic blood pressures. • Skin may start to look pale and be cool to the touch. • Blood transfusion is not typically required.
Class III Hemorrhage • involves loss of 30 -40% of circulating blood volume. • The patient's blood pressure drops, the heart rate increases, peripheral hypoperfusion (shock), such as capillary refill worsens, and the mental status worsens. • Fluid resuscitation with crystalloid and blood transfusion are usually necessary. Class IV Hemorrhage • involves loss of >40% of circulating blood volume. • The limit of the body's compensation is reached and aggressive resuscitation is required to prevent death.
Basis Of Hemorrhagic Treatment • Treatment of the hemorrhage depend upon degree of the hypovolemic shock according to 1 - Vital Signs 2 - Preload assessment 3 - Base deficit 4 - Most important among these is dynamic response to fluid therapy. • In non-responder or transitient responder patients it is necessary to identify and control the site of the bleeding.
Hemorrhage Control • External Hemorrhage – Direct pressure and pressure dressing – General management • • • Direct pressure Elevation Ice Pressure points Constricting band Tourniquet – May use a BP cuff by inflating the cuff 20– 30 mm. Hg above the SBP – Release may send toxins to heart » Lactic acid and electrolytes

Tourniquets are ONLY used as a last resort!
Internal Hemorrhage Control • Hematoma – Pocket of blood between muscle and fascia • General Management – Immobilization, stabilization, elevation – Epistaxis: Nose Bleed • Causes: trauma, hypertension • Treatment: lean forward, pinch nostrils
Hemorrhage Assessment • Initial Assessment – General Impression • Obvious bleeding – Mental Status – ABC – Interventions – O 2 – Bleeding control – Shock
Hemorrhage Assessment • Ongoing Assessment – Reassess vitals and mental status: • Q 5 min: UNSTABLE patients • Q 15 min: STABLE patients – Reassess interventions: • • Oxygen ET IV Medication actions – Trending: improvement vs. deterioration • Pulse oximetry • End-tidal CO 2 levels
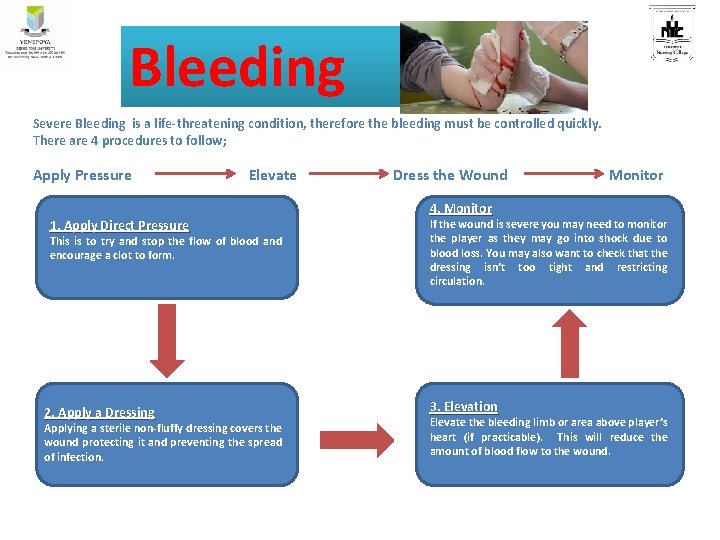
Bleeding Severe Bleeding is a life-threatening condition, therefore the bleeding must be controlled quickly. There are 4 procedures to follow; Apply Pressure Elevate 1. Apply Direct Pressure This is to try and stop the flow of blood and encourage a clot to form. 2. Apply a Dressing Applying a sterile non-fluffy dressing covers the wound protecting it and preventing the spread of infection. Dress the Wound Monitor 4. Monitor If the wound is severe you may need to monitor the player as they may go into shock due to blood loss. You may also want to check that the dressing isn’t too tight and restricting circulation. 3. Elevation Elevate the bleeding limb or area above player’s heart (if practicable). This will reduce the amount of blood flow to the wound.
Reference • Hockenberry, Wilson, Judie. Wong’s essentials of pediatric Nursing. South India Edition. Elsevier publication. • Dorothy R Marlow, Barbara A Redding, Raman Kalia. Marlow’s textbook of pediatric Nursing. Harcourt Brace & Company Asia Pte Ltd. • Parul Datta. Pediatric Nursing. 4 th edition. Jaypee Publishers. New Delhi.

Thank you
- Slides: 27