HEMOLYTIC ANEMIA Dr M A Sofi MD FRCP


- Slides: 19

HEMOLYTIC ANEMIA Dr. M. A Sofi MD; FRCP (London); FRCEdin; FRCSEdin
HEMOLYTIC ANEMIA Hemolytic anemia is a form of anemia due to hemolysis, the abnormal breakdown of red blood cells (RBCs), either in the blood vessels (intravascular) or elsewhere in the human body (extravascular). • It has numerous possible causes, ranging from relatively harmless to life-threatening. • The general classification of hemolytic anemia is either inherited or acquired. • Treatment depends on the cause and nature of the breakdown.
HEMOLYTIC ANEMIA: Hemolysis is the premature destruction of erythrocytes • A hemolytic anemia • Mild hemolysis can be will develop if bone asymptomatic while marrow activity cannot the anemia in severe compensate for the hemolysis can be life erythrocyte loss. threatening and cause angina and • The severity of the cardiopulmonary deanemia depends on compensation. whether the onset of hemolysis is gradual or abrupt and on the extent of erythrocyte destruction.
Classification: Acquired haemolytic anaemia: immune Immune (direct antiglobulin test often positive): • Warm antibody autoimmune haemolytic anaemia: antibody (usually Ig. G) binds most avidly at core body temperature. • Associated with underlying diseases such as: • SLE • Lymphoma • Chronic lymphocytic leukaemia. 3 • Cold antibody autoimmune haemolytic anaemia: antibody binds RBC at temperature below body temperature. (often Ig. M, but may be Ig. G). Can be idiopathic, or associated with infection or malignancy. • Drug-induced immune haemolytic anaemia. • Alloimmune haemolytic anaemia: haemolytic disease of the newborn or transfusion reaction.
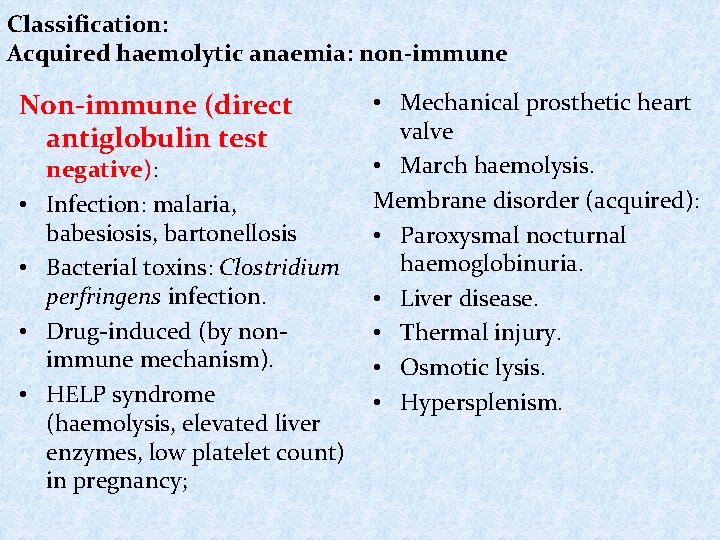
Classification: Acquired haemolytic anaemia: non-immune Non-immune (direct antiglobulin test • • negative): Infection: malaria, babesiosis, bartonellosis Bacterial toxins: Clostridium perfringens infection. Drug-induced (by nonimmune mechanism). HELP syndrome (haemolysis, elevated liver enzymes, low platelet count) in pregnancy; • Mechanical prosthetic heart valve • March haemolysis. Membrane disorder (acquired): • Paroxysmal nocturnal haemoglobinuria. • Liver disease. • Thermal injury. • Osmotic lysis. • Hypersplenism.
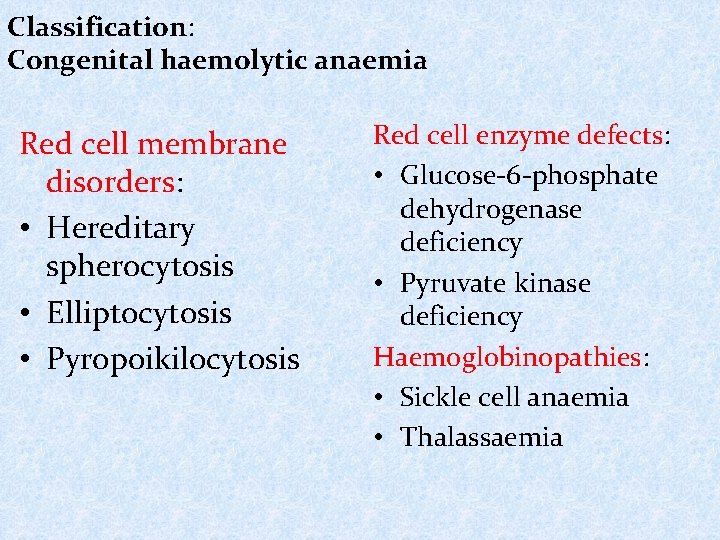
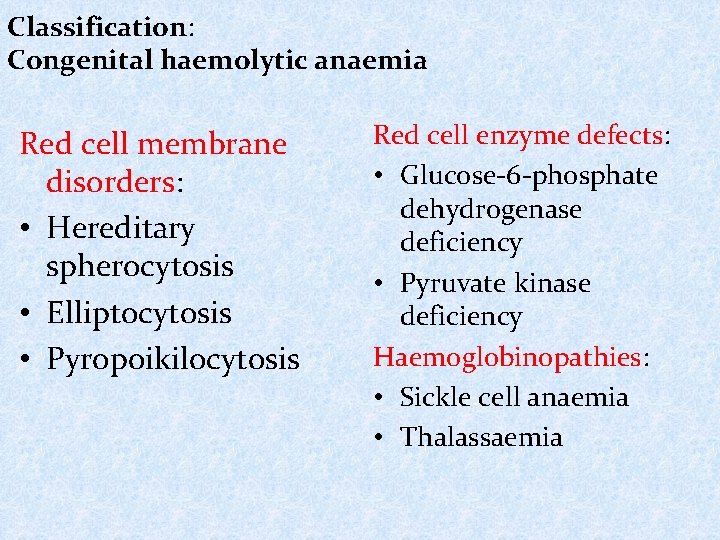
Classification: Congenital haemolytic anaemia Red cell membrane disorders: • Hereditary spherocytosis • Elliptocytosis • Pyropoikilocytosis Red cell enzyme defects: • Glucose-6 -phosphate dehydrogenase deficiency • Pyruvate kinase deficiency Haemoglobinopathies: • Sickle cell anaemia • Thalassaemia

HEMOLYTIC ANEMIA Hemolytic anemia involves: • Abnormal and accelerated destruction of red cells. • Increased breakdown of hemoglobin, which may result in: • Increased bilirubin level (mainly indirect-reacting) with jaundice • Increased fecal and urinary urobilinogen • Hemoglobinemia, Methemalbuminemia, Hemoglobinuria and Hemosiderinuria • Bone marrow compensatory reaction: • Erythroid hyperplasia with accelerated production of red cells, reticulocytosis, and slight macrocytosis. • Expansion of bone marrow in infants and children with severe chronic hemolysis - changes in bone visible on X -ray • The balance between red cell destruction and marrow compensation determines the severity of anemias.
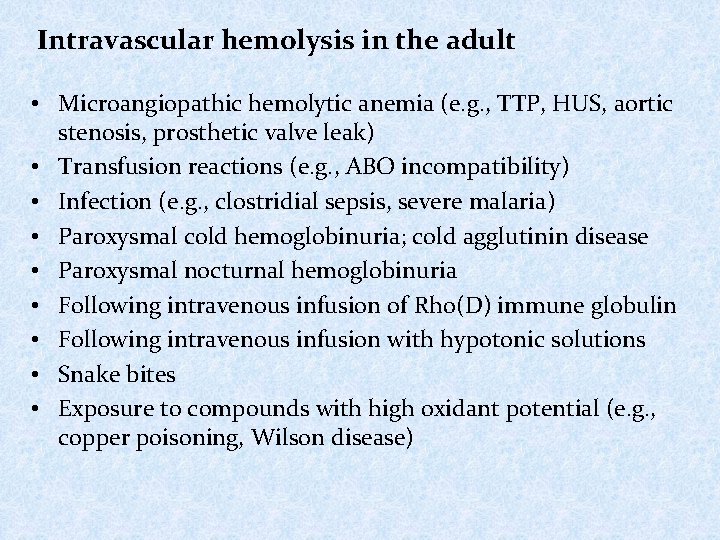
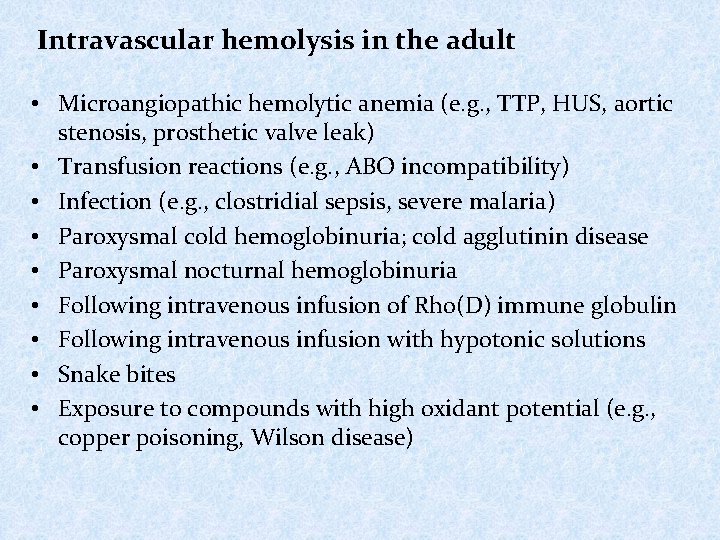
Intravascular hemolysis in the adult • Microangiopathic hemolytic anemia (e. g. , TTP, HUS, aortic stenosis, prosthetic valve leak) • Transfusion reactions (e. g. , ABO incompatibility) • Infection (e. g. , clostridial sepsis, severe malaria) • Paroxysmal cold hemoglobinuria; cold agglutinin disease • Paroxysmal nocturnal hemoglobinuria • Following intravenous infusion of Rho(D) immune globulin • Following intravenous infusion with hypotonic solutions • Snake bites • Exposure to compounds with high oxidant potential (e. g. , copper poisoning, Wilson disease)
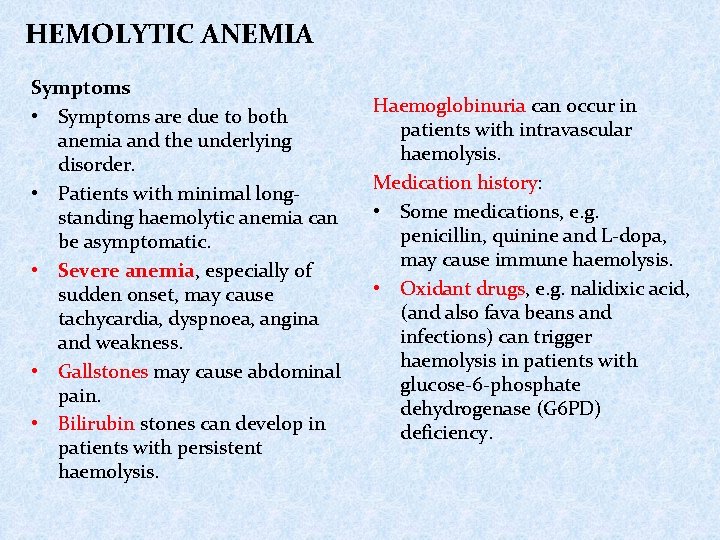
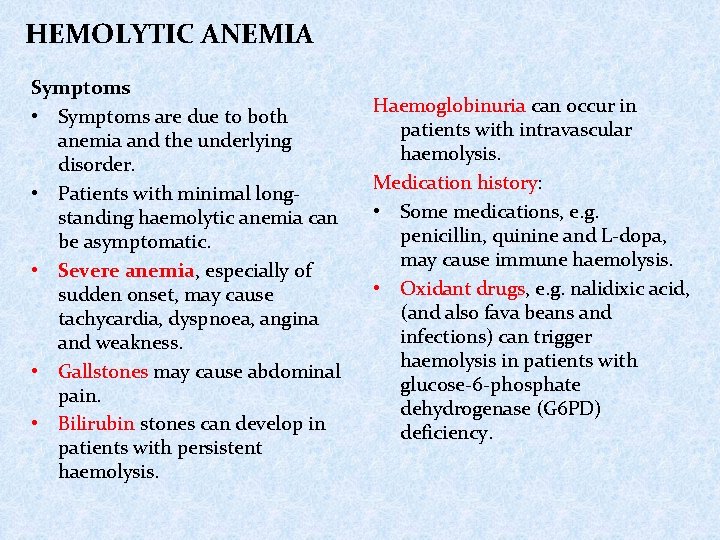
HEMOLYTIC ANEMIA Symptoms • Symptoms are due to both anemia and the underlying disorder. • Patients with minimal longstanding haemolytic anemia can be asymptomatic. • Severe anemia, especially of sudden onset, may cause tachycardia, dyspnoea, angina and weakness. • Gallstones may cause abdominal pain. • Bilirubin stones can develop in patients with persistent haemolysis. Haemoglobinuria can occur in patients with intravascular haemolysis. Medication history: • Some medications, e. g. penicillin, quinine and L-dopa, may cause immune haemolysis. • Oxidant drugs, e. g. nalidixic acid, (and also fava beans and infections) can trigger haemolysis in patients with glucose-6 -phosphate dehydrogenase (G 6 PD) deficiency.
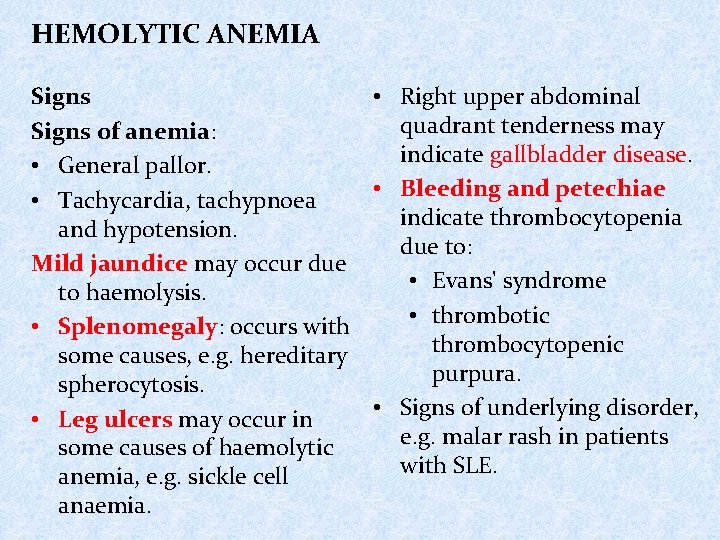
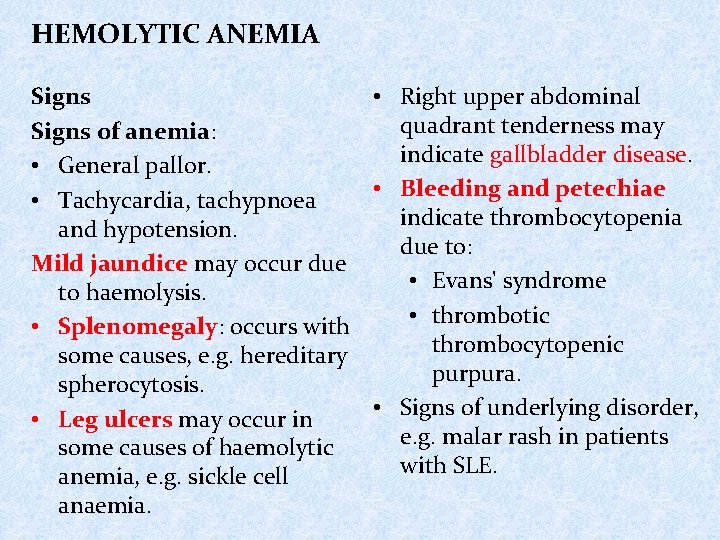
HEMOLYTIC ANEMIA Signs • Right upper abdominal quadrant tenderness may Signs of anemia: indicate gallbladder disease. • General pallor. • Bleeding and petechiae • Tachycardia, tachypnoea indicate thrombocytopenia and hypotension. due to: Mild jaundice may occur due • Evans' syndrome to haemolysis. • thrombotic • Splenomegaly: occurs with thrombocytopenic some causes, e. g. hereditary purpura. spherocytosis. • Signs of underlying disorder, • Leg ulcers may occur in e. g. malar rash in patients some causes of haemolytic with SLE. anemia, e. g. sickle cell anaemia.
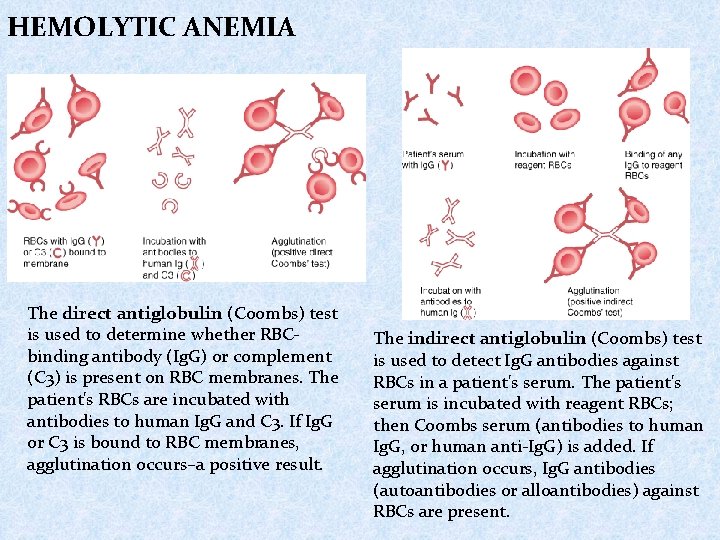
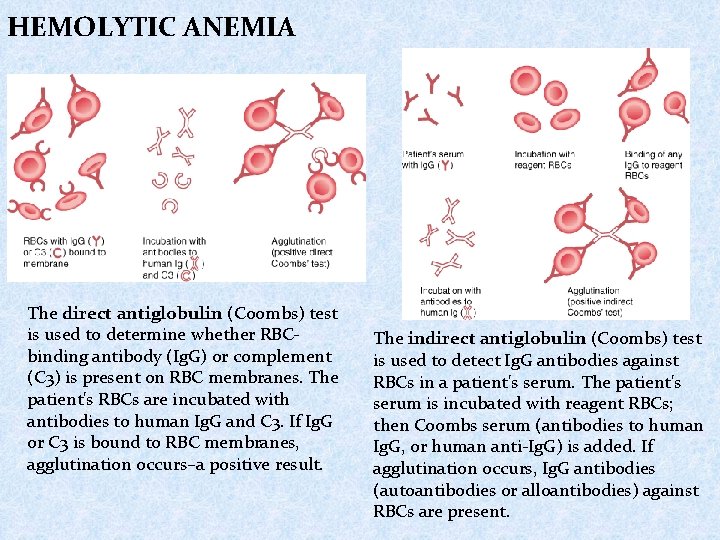
HEMOLYTIC ANEMIA The direct antiglobulin (Coombs) test is used to determine whether RBCbinding antibody (Ig. G) or complement (C 3) is present on RBC membranes. The patient's RBCs are incubated with antibodies to human Ig. G and C 3. If Ig. G or C 3 is bound to RBC membranes, agglutination occurs–a positive result. The indirect antiglobulin (Coombs) test is used to detect Ig. G antibodies against RBCs in a patient's serum. The patient's serum is incubated with reagent RBCs; then Coombs serum (antibodies to human Ig. G, or human anti-Ig. G) is added. If agglutination occurs, Ig. G antibodies (autoantibodies or alloantibodies) against RBCs are present.
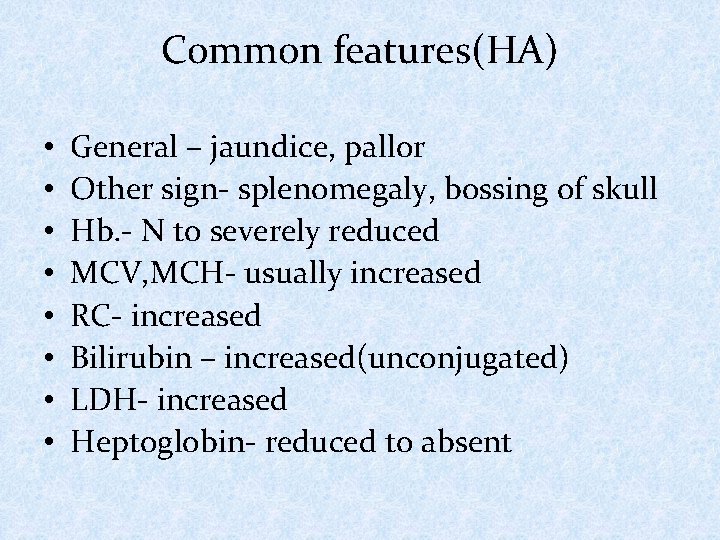
Common features(HA) • • General – jaundice, pallor Other sign- splenomegaly, bossing of skull Hb. - N to severely reduced MCV, MCH- usually increased RC- increased Bilirubin – increased(unconjugated) LDH- increased Heptoglobin- reduced to absent
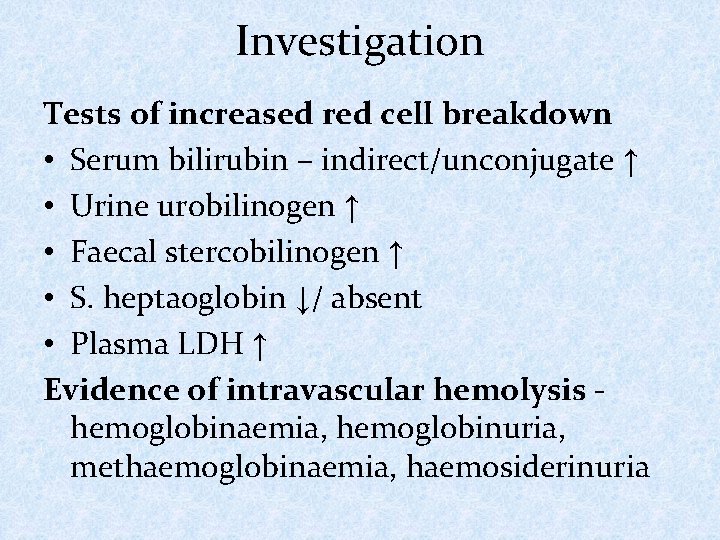
Investigation Tests of increased red cell breakdown • Serum bilirubin – indirect/unconjugate ↑ • Urine urobilinogen ↑ • Faecal stercobilinogen ↑ • S. heptaoglobin ↓/ absent • Plasma LDH ↑ Evidence of intravascular hemolysis - hemoglobinaemia, hemoglobinuria, methaemoglobinaemia, haemosiderinuria
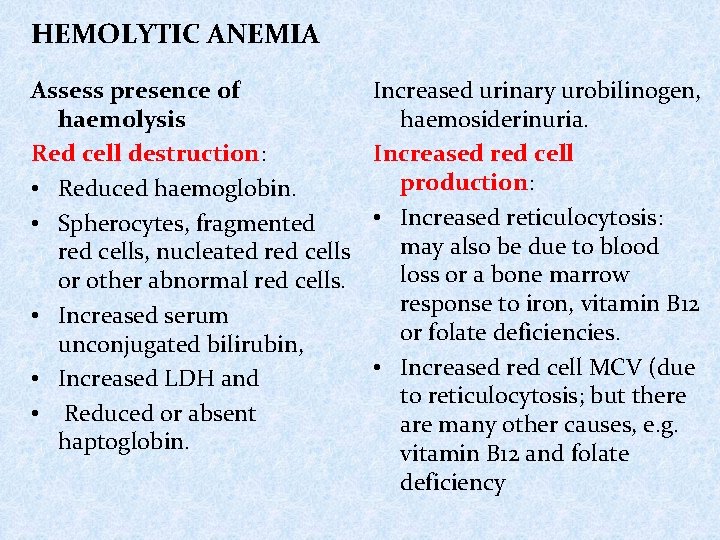
HEMOLYTIC ANEMIA Assess presence of haemolysis Red cell destruction: • Reduced haemoglobin. • Spherocytes, fragmented red cells, nucleated red cells or other abnormal red cells. • Increased serum unconjugated bilirubin, • Increased LDH and • Reduced or absent haptoglobin. Increased urinary urobilinogen, haemosiderinuria. Increased red cell production: • Increased reticulocytosis: may also be due to blood loss or a bone marrow response to iron, vitamin B 12 or folate deficiencies. • Increased red cell MCV (due to reticulocytosis; but there are many other causes, e. g. vitamin B 12 and folate deficiency
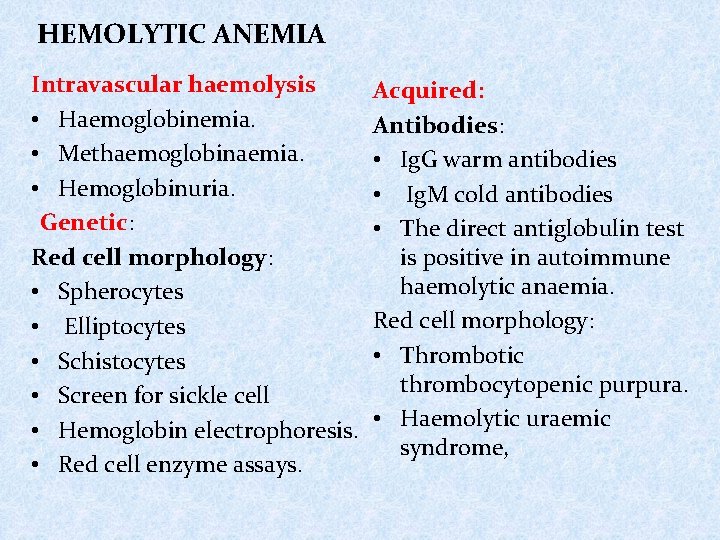
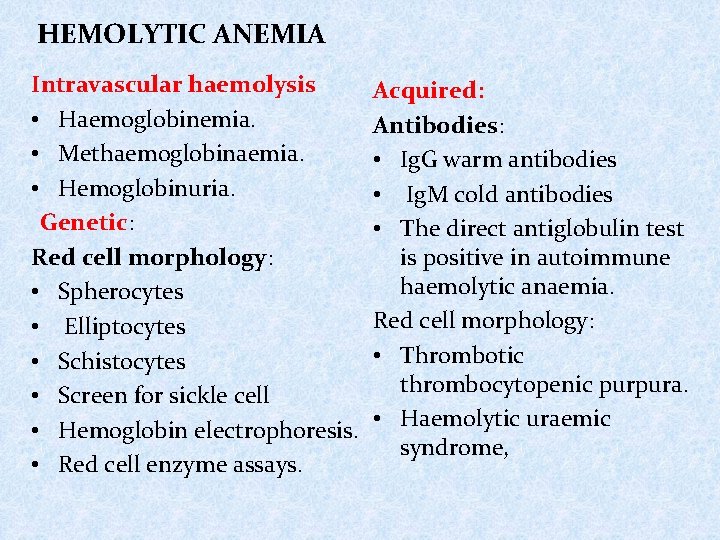
HEMOLYTIC ANEMIA Intravascular haemolysis • Haemoglobinemia. • Methaemoglobinaemia. • Hemoglobinuria. Genetic: Red cell morphology: • Spherocytes • Elliptocytes • Schistocytes • Screen for sickle cell • Hemoglobin electrophoresis. • Red cell enzyme assays. Acquired: Antibodies: • Ig. G warm antibodies • Ig. M cold antibodies • The direct antiglobulin test is positive in autoimmune haemolytic anaemia. Red cell morphology: • Thrombotic thrombocytopenic purpura. • Haemolytic uraemic syndrome,
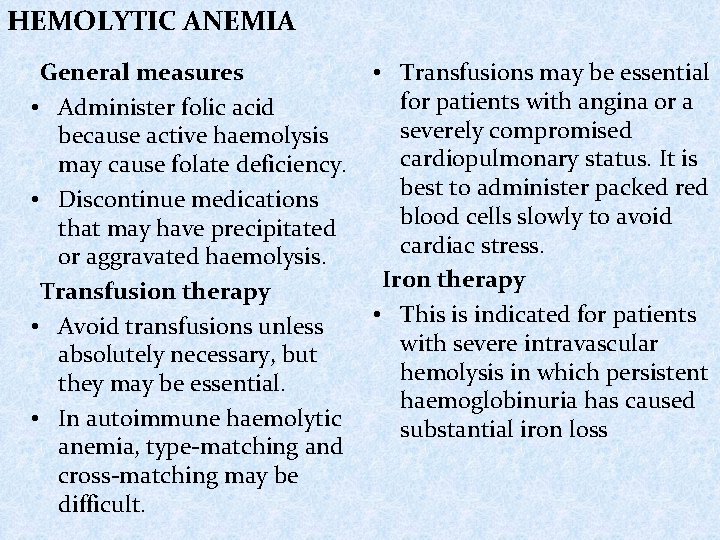
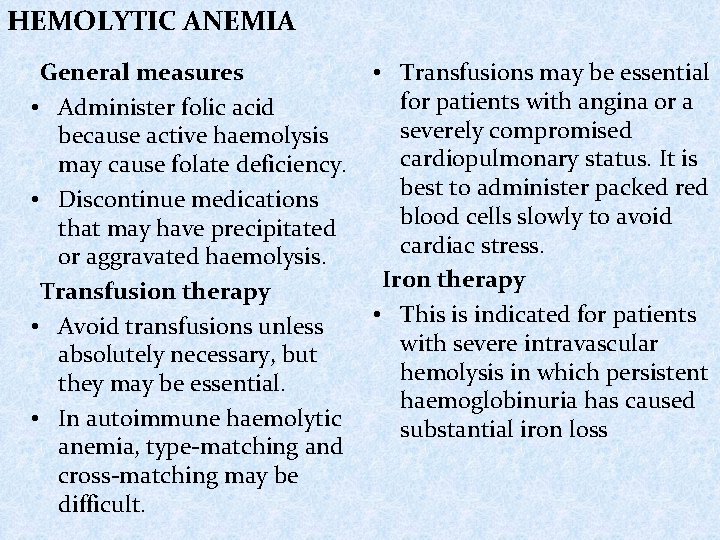
HEMOLYTIC ANEMIA General measures • Transfusions may be essential for patients with angina or a • Administer folic acid severely compromised because active haemolysis cardiopulmonary status. It is may cause folate deficiency. best to administer packed red • Discontinue medications blood cells slowly to avoid that may have precipitated cardiac stress. or aggravated haemolysis. Iron therapy Transfusion therapy • This is indicated for patients • Avoid transfusions unless with severe intravascular absolutely necessary, but hemolysis in which persistent they may be essential. haemoglobinuria has caused • In autoimmune haemolytic substantial iron loss anemia, type-matching and cross-matching may be difficult.
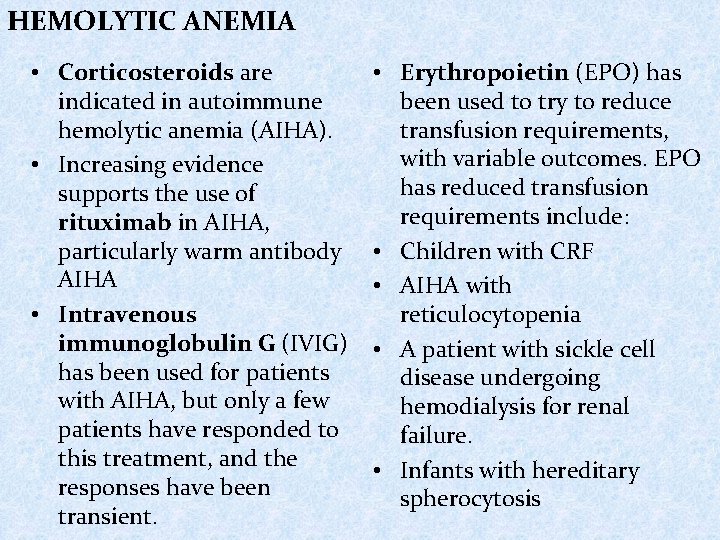
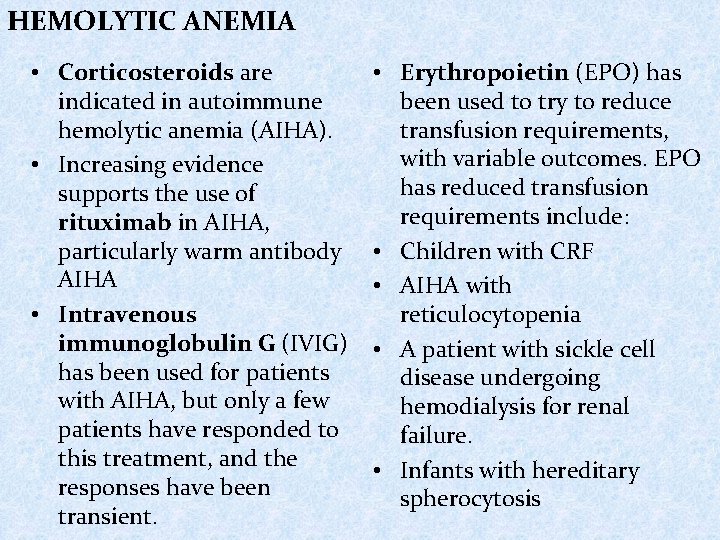
HEMOLYTIC ANEMIA • Corticosteroids are indicated in autoimmune hemolytic anemia (AIHA). • Increasing evidence supports the use of rituximab in AIHA, particularly warm antibody AIHA • Intravenous immunoglobulin G (IVIG) has been used for patients with AIHA, but only a few patients have responded to this treatment, and the responses have been transient. • Erythropoietin (EPO) has been used to try to reduce transfusion requirements, with variable outcomes. EPO has reduced transfusion requirements include: • Children with CRF • AIHA with reticulocytopenia • A patient with sickle cell disease undergoing hemodialysis for renal failure. • Infants with hereditary spherocytosis
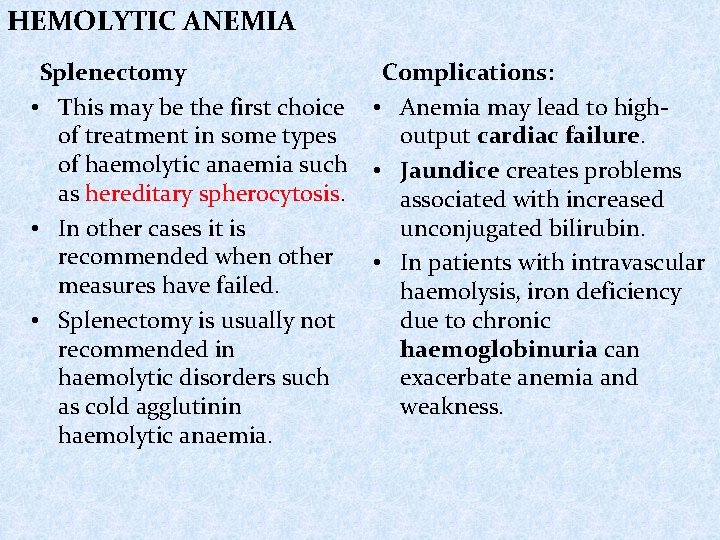
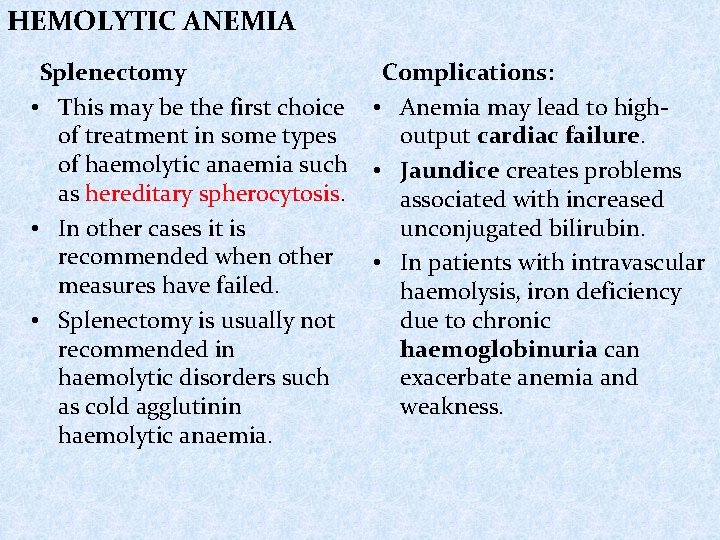
HEMOLYTIC ANEMIA Splenectomy Complications: • This may be the first choice • Anemia may lead to highof treatment in some types output cardiac failure. of haemolytic anaemia such • Jaundice creates problems as hereditary spherocytosis. associated with increased • In other cases it is unconjugated bilirubin. recommended when other • In patients with intravascular measures have failed. haemolysis, iron deficiency • Splenectomy is usually not due to chronic recommended in haemoglobinuria can haemolytic disorders such exacerbate anemia and as cold agglutinin weakness. haemolytic anaemia.
THANK YOU FOR YOUR ATTENTION