Hemodynamics Cellular Phases Types of Exudates Role of












- Slides: 62
Hemodynamics & Cellular Phases Types of Exudates (Role of Chemical mediators in inflammation)

Hemodynamics • Hemodynamics consist of maintenance of: I-Vessel wall integrity. • II-Intravascular pressure & osmalarity. • III-Blood as liquid.
Hemodynamic Changes • • These are; I-Disturbances in cellular phases. II-Disturbances in blood. III-Non clot formation.
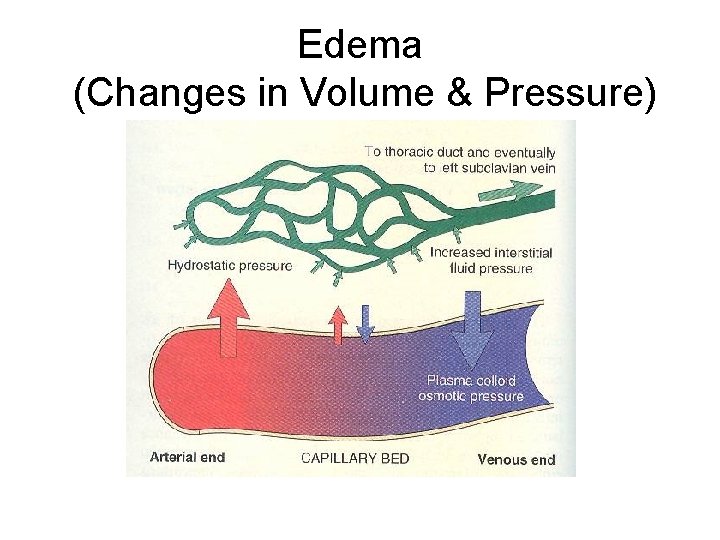
Hemodynamic Changes • Disturbances in Cellular Phases: Disturbances occur in blood & endothelium, like: • I-Changes in volume, pressure & proteins contents. • II-Alteration in epithelial function. • Both cause movements of water towards the vessel wall & out side the vessel in the interstitial tissue/spaces, called edema.
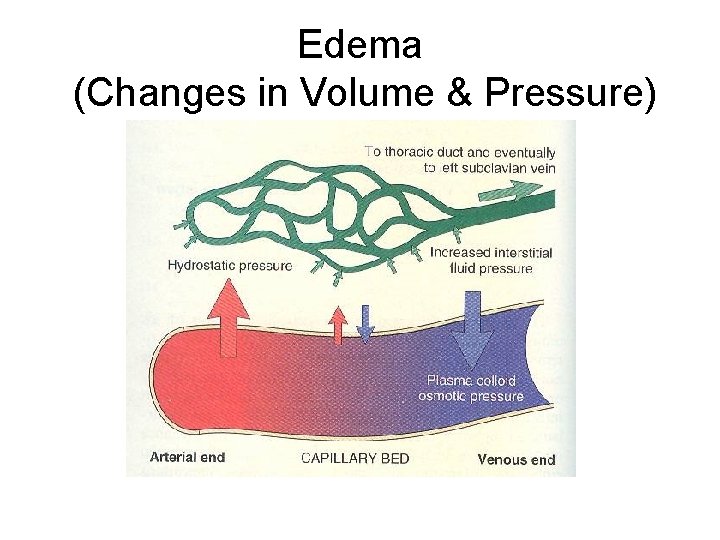
Edema (Changes in Volume & Pressure)
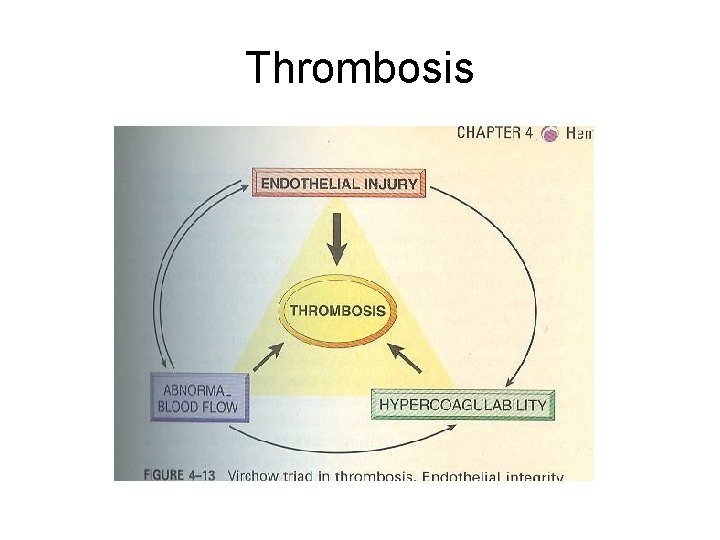
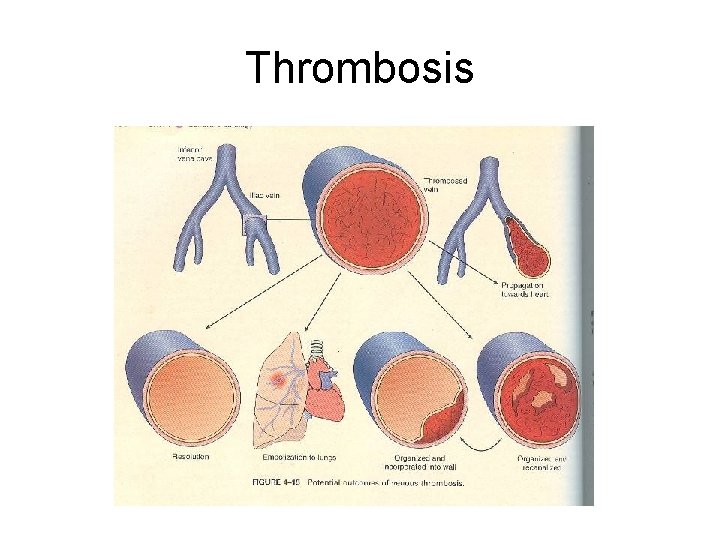
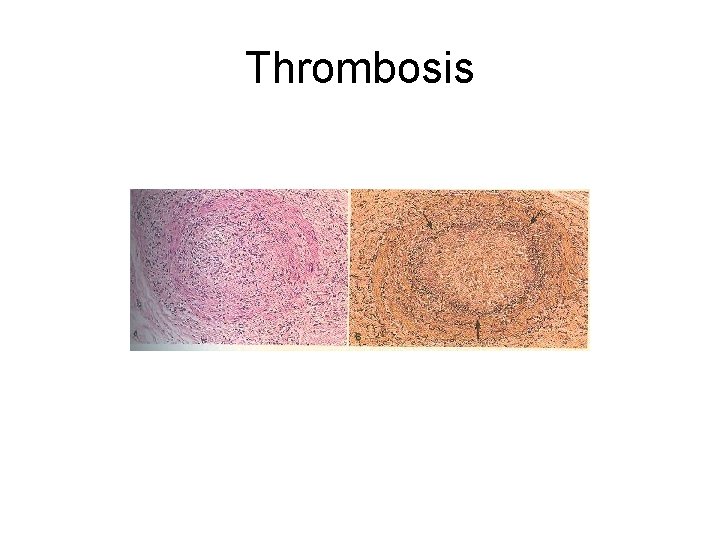
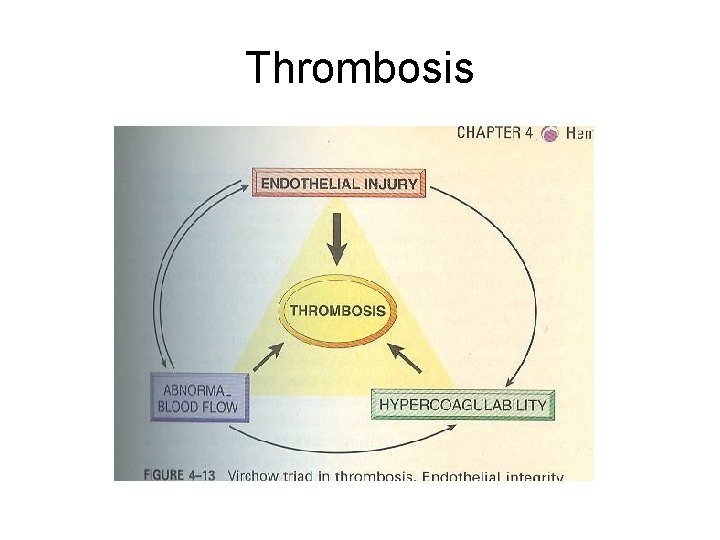
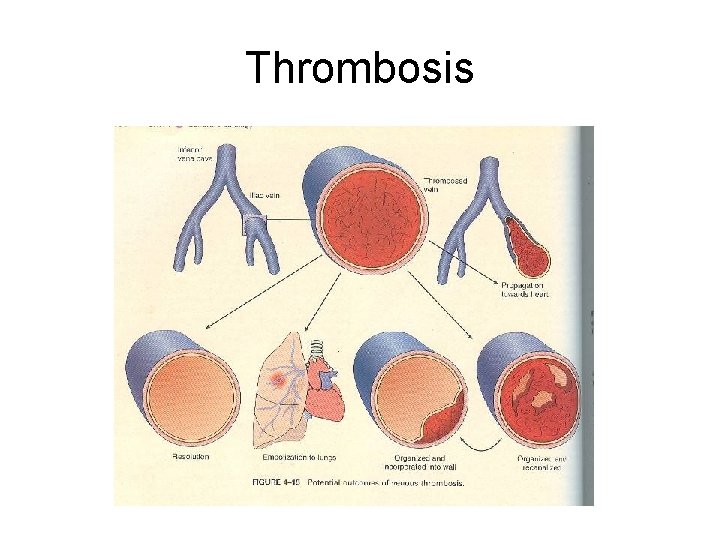
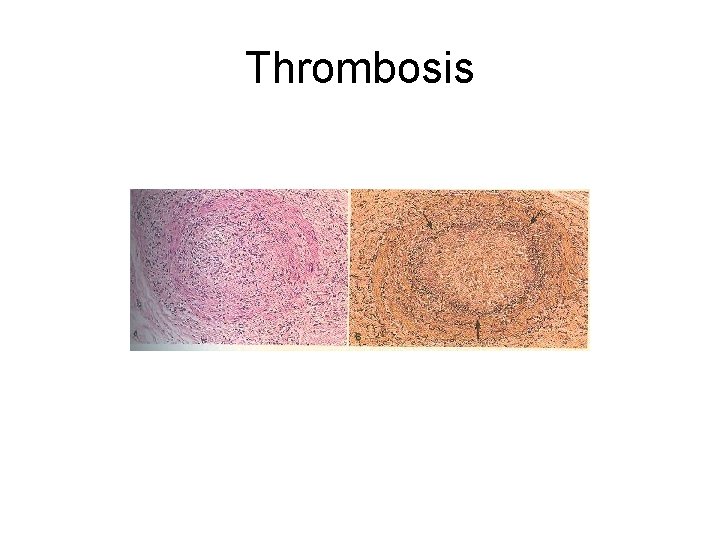
Hemodynamic Changes • II-Disturbances in blood: • Disturbance in fluidity of blood. • Blood not maintain as fluid with injury, causes clot formation. • Fixed clot formation in vessel wall lumen called Thrombosis.
Thrombosis
Thrombosis
Thrombosis
Thrombosis
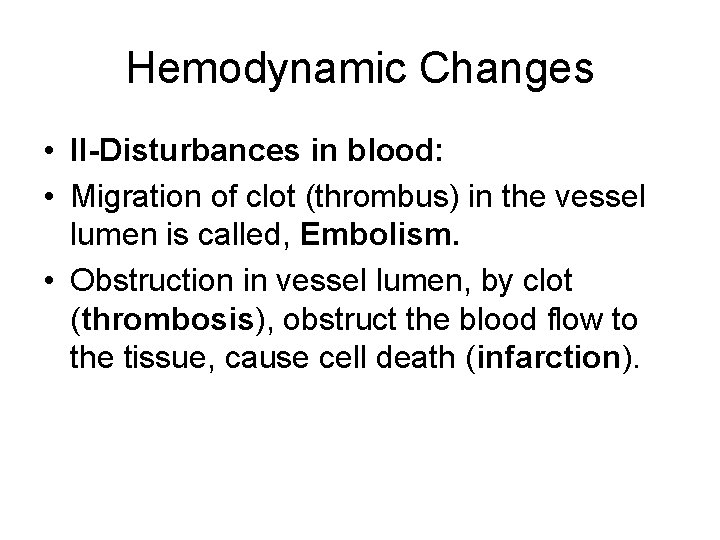
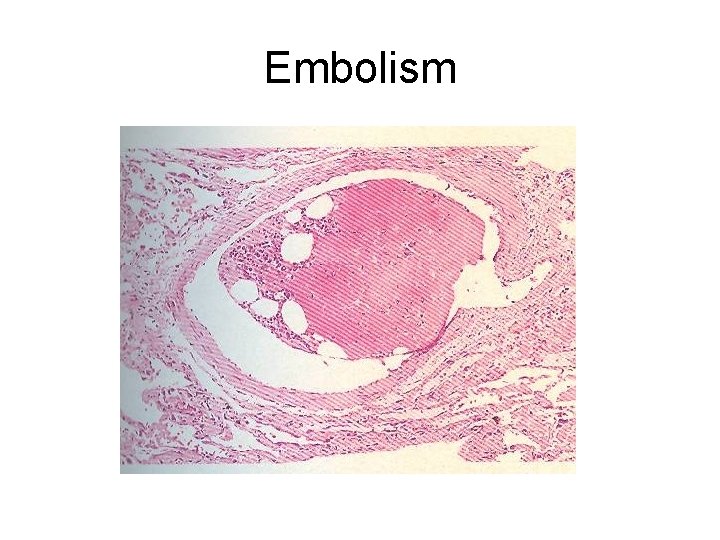
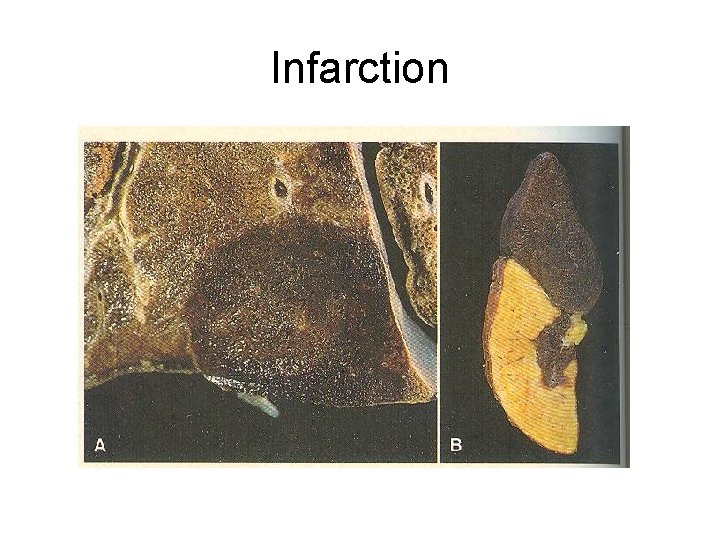
Hemodynamic Changes • II-Disturbances in blood: • Migration of clot (thrombus) in the vessel lumen is called, Embolism. • Obstruction in vessel lumen, by clot (thrombosis), obstruct the blood flow to the tissue, cause cell death (infarction).
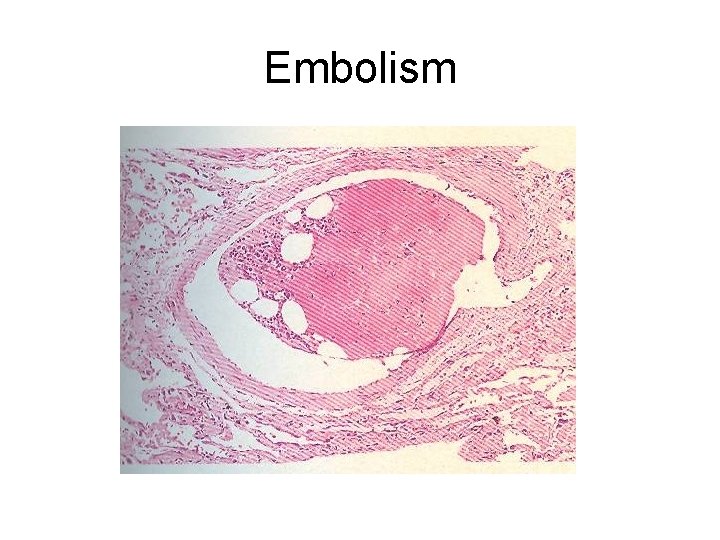
Embolism
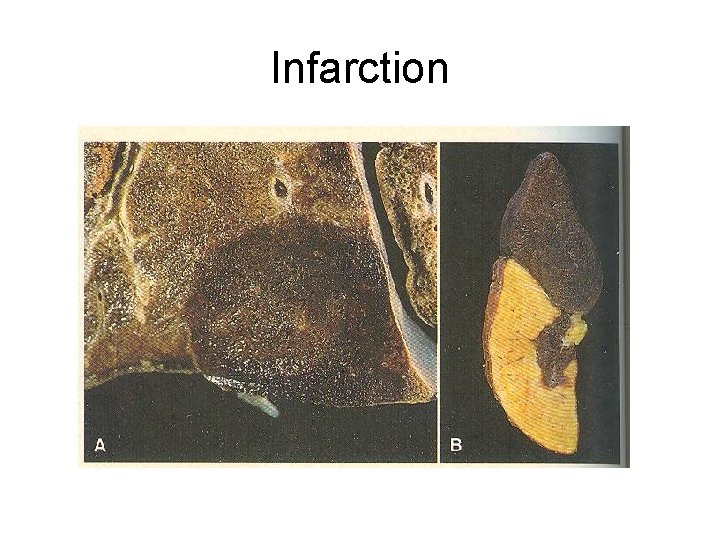
Infarction
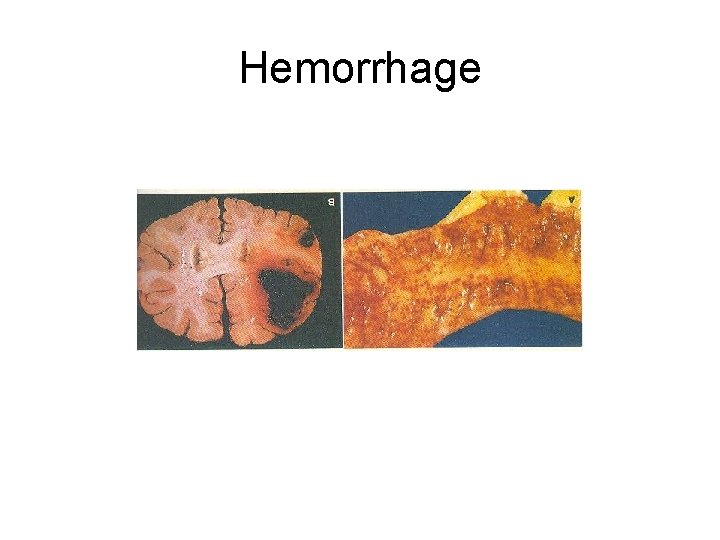
Hemodynamic Changes • III-Non clot formation: • Inability to clot after vascular injury results in hemorrhage. • Local bleeding cause, tissue perfusion. • Extensive hemorrhage results in hypotension (shock) & death.
Types of Edema • These are: • I-Fluid collection in interstitial tissue cause edema. • II-Inflammatory edema due to increase vascular permeability.

Types of Edema • I-Fluid collection in interstitial tissue cause edema: • There is sever or generalized edema with subcutaneous tissue swelling called Anasarca.
Types of Edema • II-Inflammatory edema due to increase vascular permeability: • i-Dependent edema. • ii-Fluid collection (edema fluid) in the body cavities.
Types of Edema • II-Inflammatory edema due to increse vascular permeability: • i-Dependent edema; • In feet. • In legs. • At sacral region.
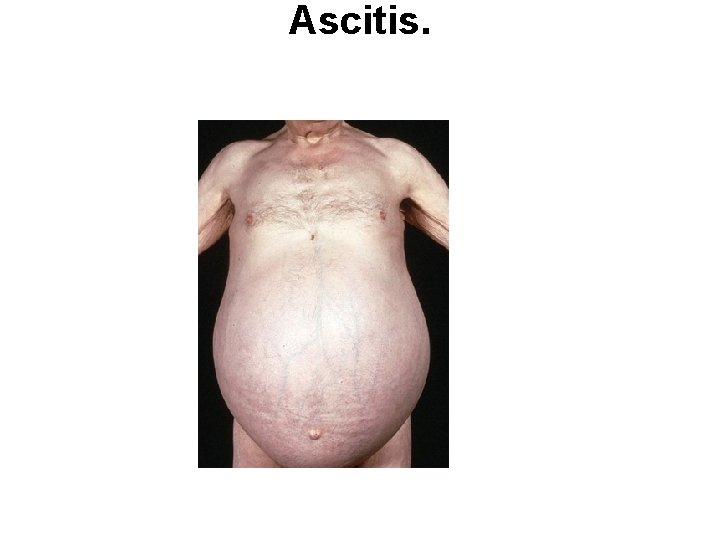
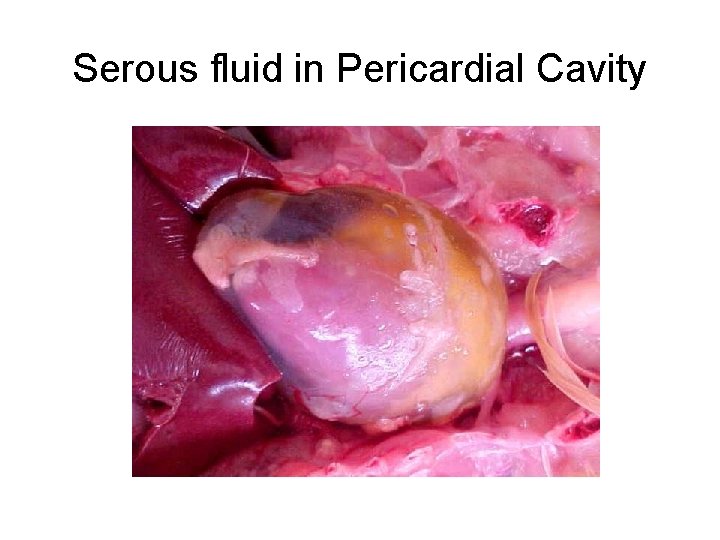
Types of Edema • II-Inflammatory edema due to increse vascular permeability: • ii-Fluid collection (edema fluid) in the body cavities: • Hydrothorax, (fluid in thoracic cavity). • Hydropericardium, (fluid in pericardial cavity). • Hydroperitoneum, (fluid in peritoneal cavity), also called Ascitis.
Hydrothorax

Hydropericardium
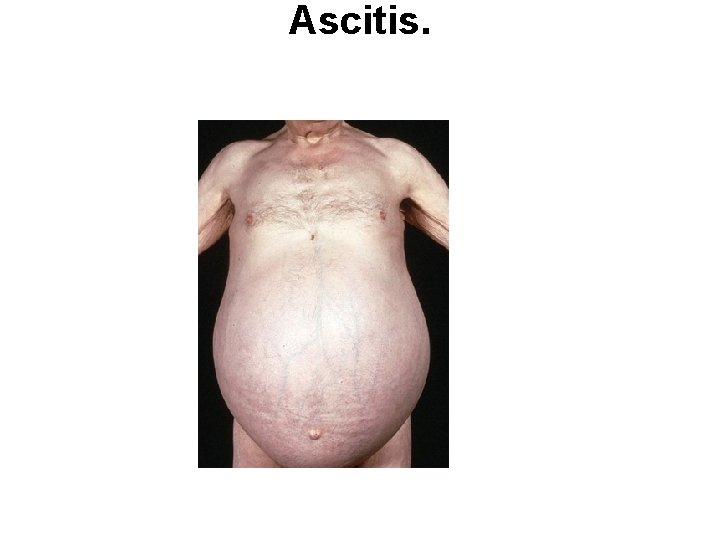
Ascitis.
Hyperermia & Congestion • Hyperemia is an active process, occurs due to arteriole dilation, cause engorgement of vessels with oxygeneted blood. • This occur as red area on body in; • Inflammation. • Skeletal muscle during exercise.
Hyperermia & Congestion • Congestion is a passive process resulting from impaired blood out flow from a tissue • Blue red color (cyanosis), can occur due to accumulation of deoxygeneted blood. • Congestion can occur: • Locally due to an isolated venous obstruction. • Systematically in cardiac failure.

Hyperemia
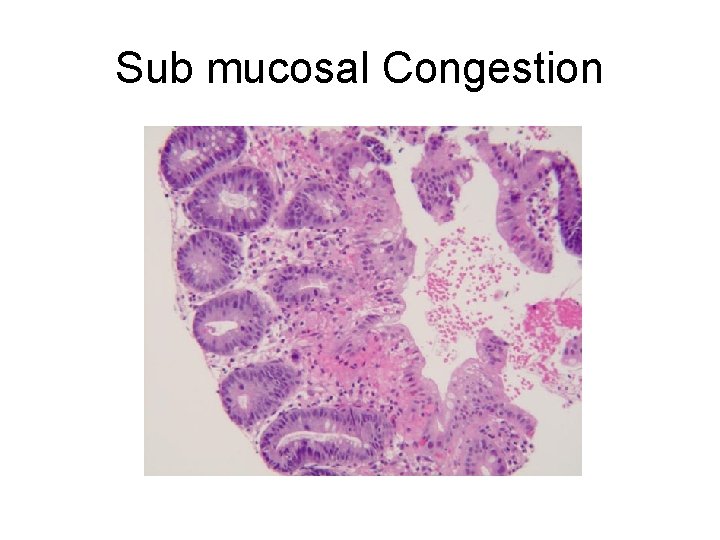
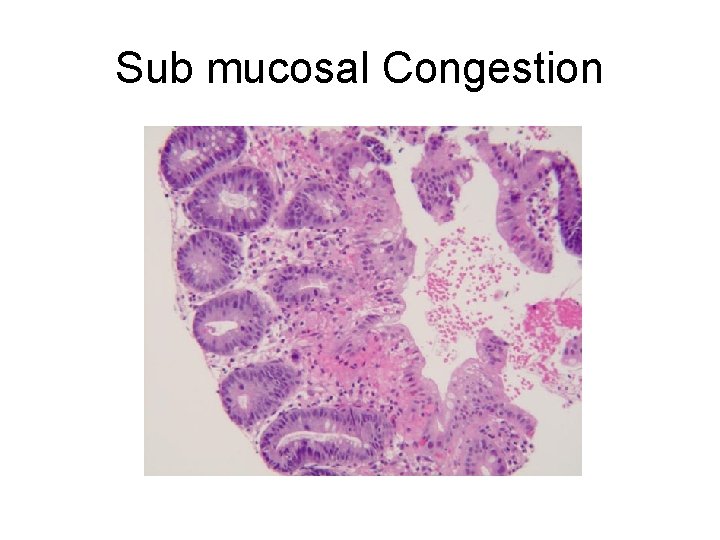
Sub mucosal Congestion
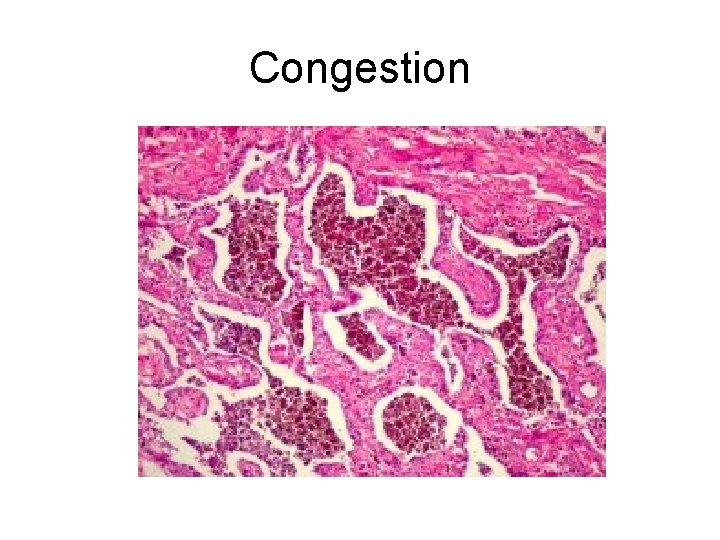
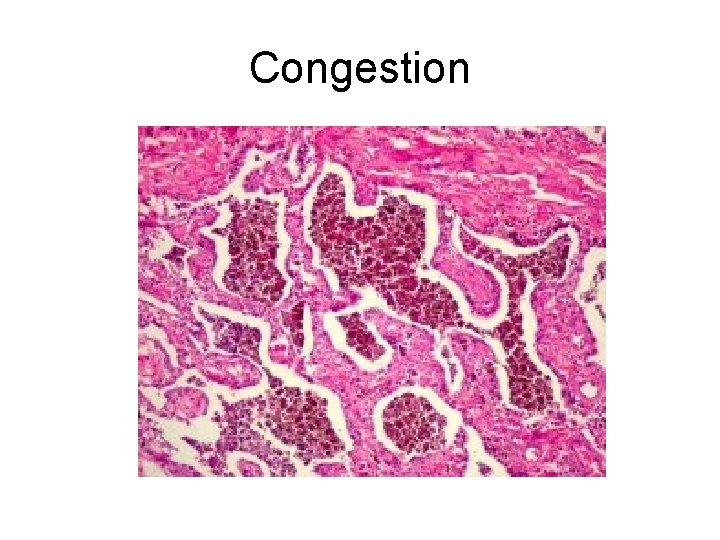
Congestion
Exudate Formation In Inflammation Vascular changes Cardinal signs RUBOR (Redness ) – Increased arterial blood flow CALOR (Rise in temperature) – Increased arterial blood flow DOLOR ( Pain ) – Physical / Chemical irritation of nerve TUMOR (Swelling ) – Collection of exudate
Exudate • Exudates it is an inflammatory extra vascular fluid that has a high protein concentration, cellular debris and an specific gravity above 1. 020. There is also disturbance in the normal permeability of small blood vessels in the area of injury.
Types of exudate • • • The types are: Serous. Fibrinous. Suppurative. Hemorrhegic. Ulceration.
Types of exudate • Serous / Catarrhal Resorption (No complication) • Watery, protein-poor effusion (e. g. , blister) • Fibrinous Fibrinolysed / Fibrosis (May or may not have complication) • Fibrin accumulation. Either entirely removed or becomes fibrotic
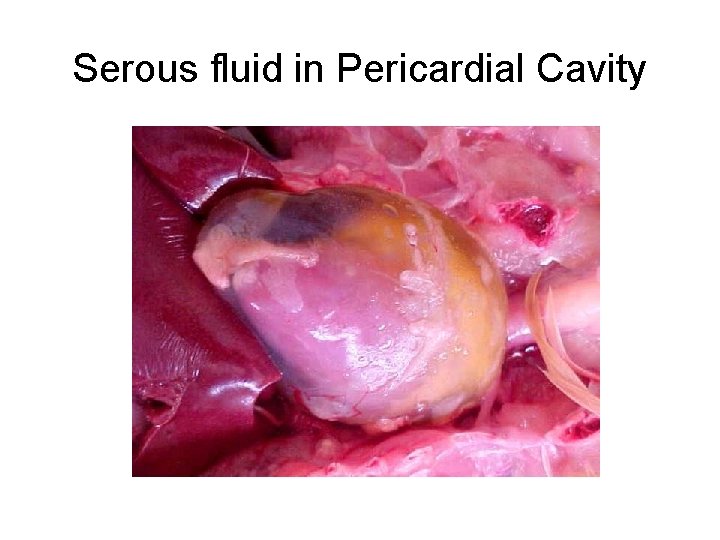
Serous fluid in Pericardial Cavity
Types of exudate Suppurative Presence of pus (pyogenic staphylococcal species). Often walled-off if persistent. Haemorrhagic Adherence (Complication)
Hemorrhage
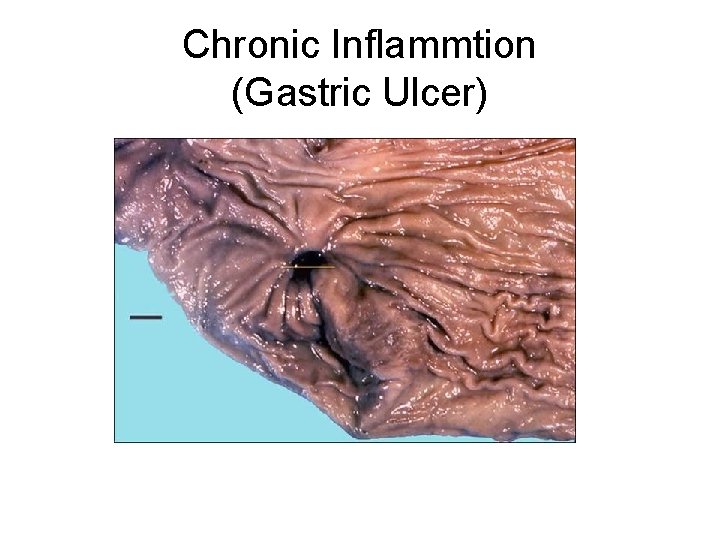
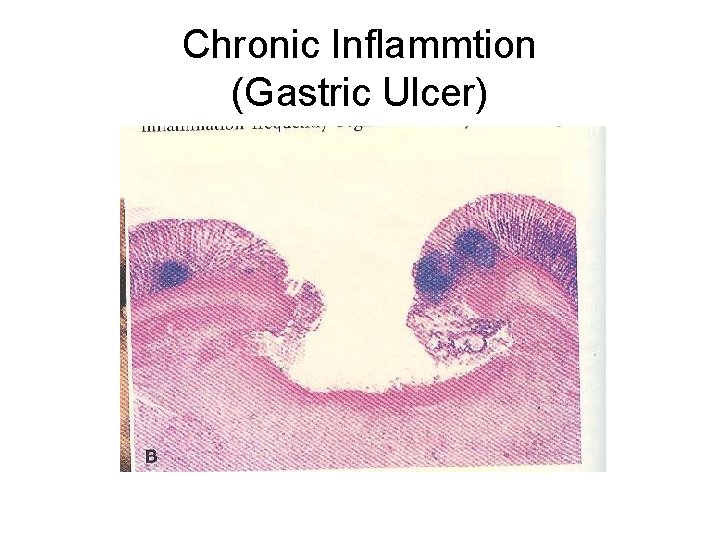
Types of exudate • Ulceration – Necrotic and eroded epithelial surface – Underlying acute and chronic inflammation – Trauma, toxins, vascular insufficiency
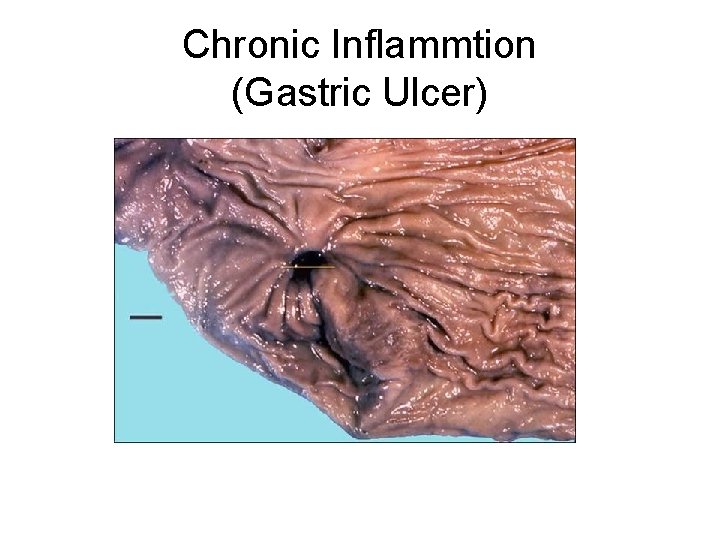
Chronic Inflammtion (Gastric Ulcer)
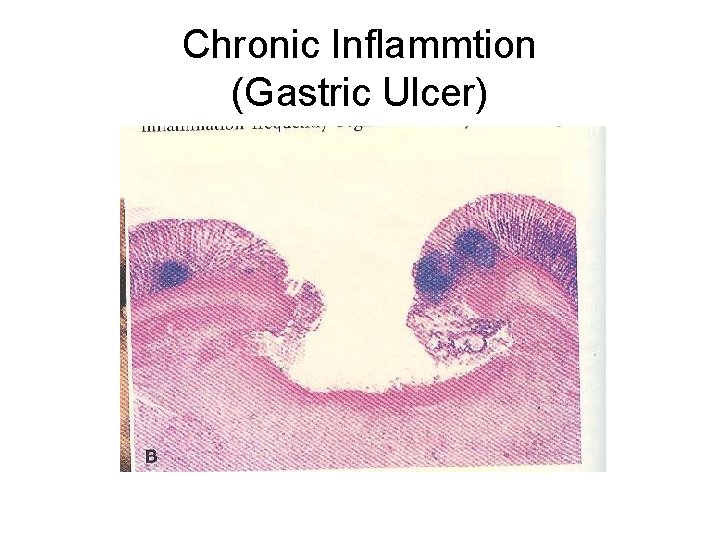
Chronic Inflammtion (Gastric Ulcer)
Chemical mediators • Chemical mediators are the chemical complexes induce inflammation. • They originate from: • Plasma, (plasma derived mediaters). • Cells, (cells derived mediaters). •
Chemical mediators • Plasma-derived: – Complement, kinins, proteins & coagulation factors present in plasma. – Many in “pro-form” requiring activation (enzymatic cleavage like proteolytic enzymes)
Chemical mediators • Cell-derived: – Preformed, sequestered and released (mast cell histamine, in intercellular granules of mast cells). – Synthesized as needed (prostaglandin & cytokines).
The cells which release mediators • • • These are; Platelets. Neutrophils. Monocytes. Macrophages. Mast cells.
Activation of Mediators • • Mediators are triggered by; Microbial products. Damaged tissue. By host proteins from; -Complement system. -Kinin system. -Clotting system.
Types of Chemical Mediaters • • Vasoactive amines: -Histamine. -Serotonin. Plasma proeases: -Complement system. -Kinin system. -Clotting system.

Types of Chemical Mediaters • • Arachidonic acid metabolies: -Prostaglandis. -Leukotriens. -Lipoxins. Platelet activating factors (PAF). Cytokines & Chemokines: -Tumor necrosis factors. -Inteleukin-1
Types of Chemical Mediaters • • • Lysosomal constituents of leukocytes. Oxygen derived free radicals. Neuropeptides. Other mediates: -Hypoxia induce factor-1. -Necrotic tissue.
Chemical mediators • Vasoactive amines: • Histamines & Serotonin-1 st mediaters released in inflammation. • Mast cells, Basophils, Platelets & connective tissue (around the blood vessels), released histamine. • Pre-formed histamine is present in mast cells granules.
Chemical mediators • Vasoactive amines: • Histamine is mainly released by mast cells granules in response of different stimuli: • Physical injury- trauma, cold or heat. • Immune reaction- binding of antibodies to mast cells.
Chemical mediators • Vasoactive amines, (histamin release): • Anaphylotoxins- C 3 a & C 5 a. • Histamine releasing proteins- from leukocytes. • Neuropeptides- substance P. • Cytokines- IL-1 & IL-2.
Chemical mediators • • Functions of Histamine: - Dilation of arterioles. - Increase permeability of venules. - Constriction of large arteries.

Chemical mediators • • • Serotonin: Pre-formed vasoactive mediater. Functions are same as Histamine. Activated by platelets aggregates. Serotonin & platelet aggregates are stimulated by platelet activating factor (PAF). • Serotonin cause increase permeability during immunologic reaction.

Chemical mediators • • Plasma proteins: -Complement system. -Kinin system. -Clotting system.
Chemical mediators • -Complement system: • Consists of 20 component proteins with cleavage products. • The system is consist of; • Innate immunity. • Adaptive immunity. • Both types immunity act against microbial agents.

Chemical mediators • • -Complement activation causes: - Increased vascular permeablity. - Chemtaxis. - Opsonization.

Chemical mediators • -Kinin system: • Kinin system form the vasoactive peptides. Kininogens from the plasma proteins. • Kinin system also release nonpeptide bradykinin- produce histamin like effect. • Hog man factor also release bradykinin.
Chemical mediators • • • -Kinin system: Function nonpeptide bradykinin: Increase vascular permeability. Dilation of blood vessels. Contraction of smooth muscles. Pain when injected in the skin.

Chemical mediators • • -Clotting system: It is divided into two; Intrinsic pathway. Extrinsic pathway.
Chemical mediators • -Clotting system: • Intrinsic pathway- is a series of plasma proteins, activated by Hogman factor (factor xii). • Hogman factor (inactive protein) synthesized in liver. • Hogman factor with negatively charged surfaces (collagen, platelets, basement membrane & in endothelial injury) form, factor XIIa & activate a verity of mediaters.

Chemical mediators • • Arachidonic acid metabolites: - Prostaglandins. - Leukotriens. - Lipoxins.

Chemical mediators • Arachidonic acid metabolites: • Arachidonic acid is a 20 -carbon polyunsaturated fatty acid (from diet or from essential fatty acids). • Present in cell membrane, as phospholipids. • It release from cell membrane by phospholipase (phospholipase A 2).
Chemical mediators • Arachidonic acid metabolites: • It release from cell membrane by phospholipase (phospholipase A 2). • The cellular phospholipase is activated by; • Mechanical stimuli. • Chemical stimuli. • Physical stimuli. • Mediaters like C 5 a.
Thank You
 Causes of cotton wool spots
Causes of cotton wool spots Shock prof
Shock prof Neurogenic shock symptoms
Neurogenic shock symptoms Hemodynamics made incredibly visual
Hemodynamics made incredibly visual Types of capillaries
Types of capillaries Arterioles function
Arterioles function Hemodynamics
Hemodynamics Role of cellular respiration
Role of cellular respiration Azure web role vs worker role
Azure web role vs worker role Interaktionistisches rollenmodell
Interaktionistisches rollenmodell Statuses and their related roles determine the structure
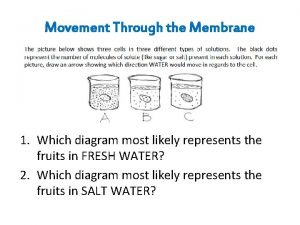
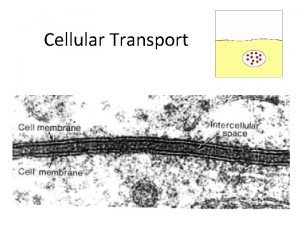
Statuses and their related roles determine the structure Practice types of cellular transport
Practice types of cellular transport Types of active transport
Types of active transport Types of cellular transport
Types of cellular transport Meaning
Meaning Functions of industrial estate
Functions of industrial estate Molecular level vs cellular level
Molecular level vs cellular level Cellular respiration redox
Cellular respiration redox The gray-brown haze often found over large cities is called
The gray-brown haze often found over large cities is called Chemiosmosis steps
Chemiosmosis steps Where is aerobic respiration located
Where is aerobic respiration located Fermentieren
Fermentieren Why is cellular respiration important
Why is cellular respiration important Cellular organization in porifera
Cellular organization in porifera The process of photosynthesis and cellular respiration
The process of photosynthesis and cellular respiration Cellular respiration chemical equation
Cellular respiration chemical equation Cellular respiration reactants
Cellular respiration reactants Cellular respiration equation
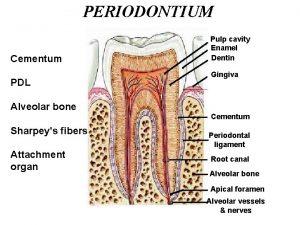
Cellular respiration equation Dentin
Dentin Photosynthesis recipe card
Photosynthesis recipe card Cellular network range
Cellular network range Electron carriers in cellular respiration
Electron carriers in cellular respiration Overview of cellular respiration
Overview of cellular respiration Respiration overview
Respiration overview Cellular respiration
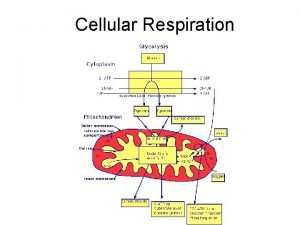
Cellular respiration Overview of cellular respiration
Overview of cellular respiration Cellular basis of learning and memory
Cellular basis of learning and memory Lab bench cellular respiration
Lab bench cellular respiration Cellular system
Cellular system Protists unicellular or multicellular
Protists unicellular or multicellular What is the word equation for cellular respiration
What is the word equation for cellular respiration Cellular events of acute inflammation
Cellular events of acute inflammation Differences between acute and chronic inflammation
Differences between acute and chronic inflammation Higher human biology cellular respiration
Higher human biology cellular respiration Controlean cellular weight loss
Controlean cellular weight loss What is the equation for cellular respiration
What is the equation for cellular respiration Function of cellular respiration
Function of cellular respiration Cellular respiration releases
Cellular respiration releases Chapter 9 section 1 cellular growth
Chapter 9 section 1 cellular growth Starting materials for cellular respiration
Starting materials for cellular respiration Chapter 8 section 3 cellular respiration continued
Chapter 8 section 3 cellular respiration continued Cellular energy section 2 photosynthesis answer key
Cellular energy section 2 photosynthesis answer key Redox reaction in cellular respiration
Redox reaction in cellular respiration Section 7-1 life is cellular
Section 7-1 life is cellular System design fundamentals
System design fundamentals Organelle
Organelle Cellular vs plasmodial slime molds
Cellular vs plasmodial slime molds Cellular respiration formula
Cellular respiration formula Cellular respiration releases
Cellular respiration releases Cellular respiration redox
Cellular respiration redox Crash course glycolysis
Crash course glycolysis Aerobic cellular respiration equation
Aerobic cellular respiration equation Process of cellular respiration
Process of cellular respiration