Hemodynamic Monitoring Part 2 PAC insertion measurements PAP
- Slides: 36
Hemodynamic Monitoring Part 2 PAC insertion & measurements: PAP, wedge, & cardiac output MICU Competencies 2006 - 2007 1
Pulmonary Artery Pressure Monitoring • Balloon tip, indwelling catheter with several lumens & thermistor placed in the PA • The PA (distal) & CVP (proximal) ports are connected to a hemodynamic monitoring system • Provides monitoring & measurement of the pulmonary artery wedge pressures (PAWP), cardiac outputs, & cardiopulmonary function 2
Indications for PA Monitoring • Alterations in cardiac output (CO) • Shock [cardiogenic, hypovolemic, septic] • Alteration in fluid volume [preload] • Alteration in tissue perfusion • Differentiate cardiac &/or pulmonary disease • Cardiac output measurements 3
Cardiac Output • Volume pumped by ventricles each minute; normal = 4 - 8 liters/minute • Cardiac Output = Heart Rate x Stroke Volume (CO = HR X SV) • SV = amount of blood ejected from each ventricle with each contraction; normal SV = 50 - 100 ml per contraction 4
Cardiac Index • Cardiac output (CO) adjusted to body size • Cardiac index (CI) = CO / body surface area • Normal CI range = 2. 5 to 4. 3 L/min/m 2 5
Low Cardiac Output • Inadequate ventricular filling dysrhythmias hypovolemia cardiac tamponade mitral or tricuspid stenosis constrictive pericarditis restrictive cardiomyopathy 6
Low Cardiac Output • Inadequate ventricular emptying mitral/tricuspid insufficiency myocardial infarction &/or disease increased afterload (hypertension) metabolic disorders (acidosis, hypoxia) negative inotropic drugs (beta-blockers, calcium channel blockers) 7
High Cardiac Output • Increased HR and/or contractility and/or decreased afterload – Sepsis – Anemia – Pregnancy – Hyperthyroid crisis 8
Determinants of Cardiac Output & Stroke Volume • Preload - Volume or pressure generated in the ventricles at end diastole • Afterload – Resistance to ejection of blood from the ventricles • Contractility – Force of ventricular ejection; difficult to measure clinically 9
Clinical Measurement of Preload • Left ventricular end diastolic pressure = LVEDP; measures preload in left ventricle – Pulmonary artery wedge pressure (PAWP) reflects LVEDP; normal = 8 - 12 mm. Hg – If unable to wedge PAC, use PA diastolic – PA diastolic (PAD); normal = 10 - 15 mm. Hg – PAD indirectly reflects left atrial pressure, which indirectly reflects LVEDP 10
Clinical Measurement of Preload • Central venous pressure = CVP; measures preload in the right ventricle – Normal CVP = 2 – 8 mm. Hg 11
Factors that Affect Preload • Anything that alters → – Circulating blood volume – Blood returning to the heart – Ventricular filling time 12
Factors that Decrease Preload Affect right & left ventricles (CVP & Wedge) • Hypovolemia • Patient position reducing venous return • Vasodilatation causing blood to pool • Reduced venous return due to mechanical ventilation - high PIP, high levels of PEEP • Tension pneumothorax Blood is not returning to the heart to fill the ventricles. 13
Factors that Increase Preload • Intravascular volume overload • Cardiac tamponade • Restrictive cardiomyopathies • Left ventricular dysfunction (↑ PCWP & CVP) • Right ventricular dysfunction (↑ CVP) 14
Afterload • Afterload is any resistance against which the ventricle must pump in order to eject its volume – Systemic Vascular Resistance (SVR) reflects LV afterload • Normal Range = 800 -1200 dynes/sec/cm-5 – Pulmonary Vascular Resistance (PVR) reflects RV afterload • Normal Range =100 -250 dynes/sec/cm-5 15
Factors that Affect Afterload • Volume & mass of blood ejected from the ventricle – Inverse relationship between afterload and CO (↑CO = ↓afterload; ↓CO = ↑afterload) • Compliance & diameter of the vessels into which the blood is ejected • Aortic impedance, peripheral vascular resistance, and blood viscosity 16
Decreased Afterload (↓ SVR) • Arterial dilatation from drugs such as nitroprusside, nitroglycerin, calcium channel blockers, beta blockers • Shock (septic, anaphylactic, neurogenic) • Hyperthermia (fever) 17
Increased Afterload (↑SVR) • Accomplished by vasoconstriction – Hypothermia – Hypertension – Alpha agonists (pressors) • Levophed, Dopamine, Phenylephrine, Epinephrine – Low CO with hypovolemic or cardiogenic shock • An effect of obstruction – Aortic/pulmonic stenosis 18
Increased Afterload (↑ PVR) • Conditions exhibiting increased PVR – Pulmonary hypertension – Hypoxia – End-stage COPD (Cor pulmonale) – Pulmonary emboli 19
Contractility = Inotropy • Inherent ability of cardiac muscle to contract • Reflected indirectly by stroke volume index (SVI) and the stroke work index for each ventricle (LVSWI & RVSWI) • Influenced by myocardial oxygenation & functionality; electrolyte balance; +/inotropes; amounts of preload and afterload 20
Factors/Meds Increasing Contractility Positive Inotropes • Sympathic stimulation – “fight or flight” • Dobutamine • Epinephrine (Adrenalin) • Norepinephrine (Levophed) • Amrinone (Inocor) • Dopamine (5 – 10 mcg/kg/min) • Calcium; glucagon; caffeine • Digoxin (only oral inotrope) 21
Factors Decreasing Contractility Negative inotropes • Acidemia • Hypoxia • Beta blockers • Anti-arrhythmics 22
PACs in the MICU In 2006, Dr. Wheeler presented the findings from the Fluid and Catheter Treatment Trial (FACTT) to nurses in our MICU. Data from this study indicates a preference for using the CVP to monitor fluid status and conservative fluid management of the patient. Therefore, we do not frequently see or manage patients with PAC’s in our MICU. 23
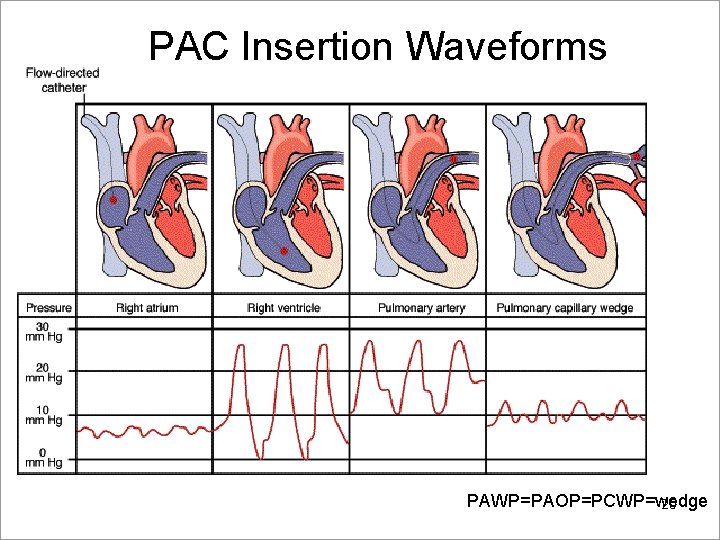
PA Catheter Insertion • Strict sterile technique; threaded through an introducer • Common sites are subclavian & jugular (occasionally femoral) • PA balloon is inflated & floated through the RA → tricuspid valve → RV → the pulmonic valve → PA → the wedged position • Record a continuous strip of the insertion hemodynamic waveforms at the bedside 24
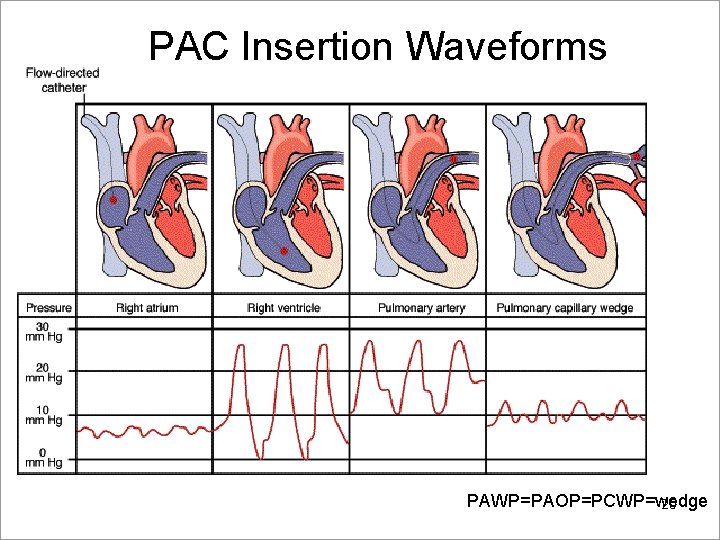
PAC Insertion Waveforms PAWP=PAOP=PCWP=wedge 25
Manual CVP Measurement • Zero/level CVP stopcock at the phlebostatic axis • Record duel channel strip with CVP and Ao waveforms • Measure all waveforms at end-expiration (See slides #30 & 31) 26
Manual PA/PCWP Measurement • Zero/level PA stopcock at phlebostatic axis • Record duel channel strip with PA and Ao • PA systolic = 20 -30; PA diastolic = 10 -15 • Slowly inflate balloon with 1. 0 – 1. 5 ml air • KEEP EYES ON MONITOR • Keep inflated 5 – 10 seconds • Passively deflate • Record the return of PA waveform 27
Cardiac Output Measurements • 10 ml syringe of room temperature D 5 W injected quickly & smoothly via the proximal port • Thermistor at the tip of the catheter senses the change in temperature • Rate of change in blood temperature generates a cardiac output value • Minimum of 3 measurements within 10% of each other averaged for a mean cardiac output • Confirm on the monitor 28
Maintenance, Care & Measurement • Sterile technique during tubing & dressing changes • Consistent leveling & measurement techniques • Measure CVP, PAP, and PCWP at end-expiration • Do not over-inflate balloon (only 1. 5 ml) • Allow balloon to deflate passively • Only MDs advance PAC when necessary (i. e. PAC 29 not wedging)
Using End-expiration Reference • Draw at least 2 vertical lines • First line = Ao tracing deviates from baseline • Back up 200 msec (one large box) to draw second vertical line • Draw a horizontal line to the left of the second line indicating – Systolic and diastolic values for PAP – Mean of the CVP; mean of the PAWP See next slide for example 30
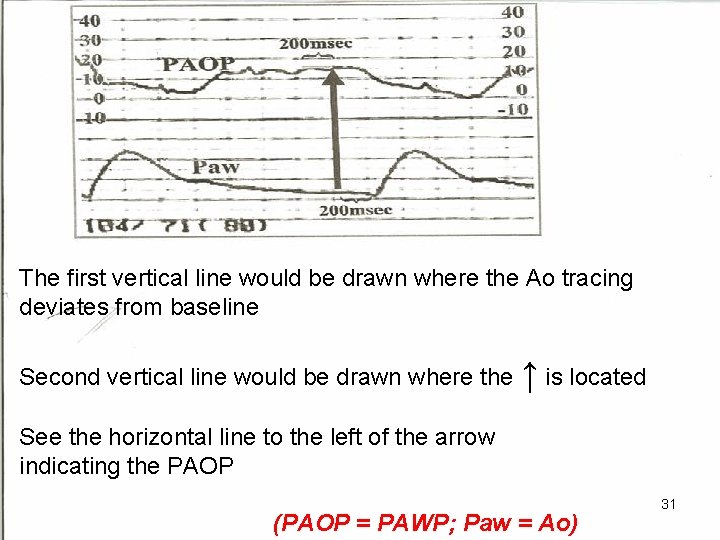
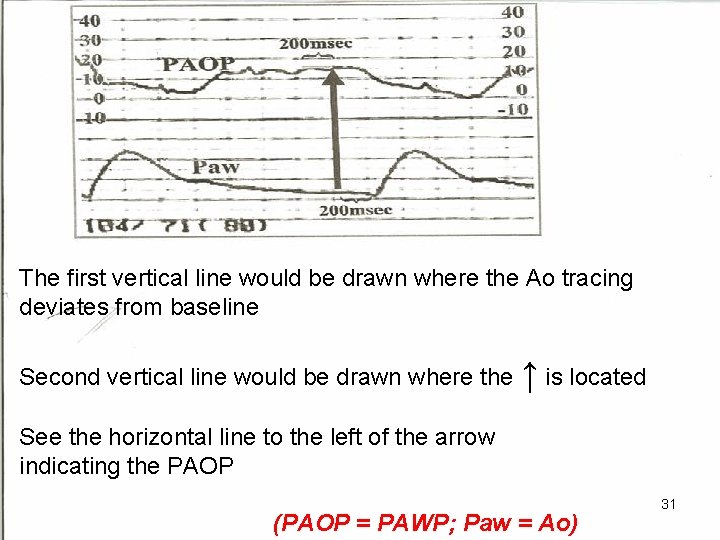
The first vertical line would be drawn where the Ao tracing deviates from baseline Second vertical line would be drawn where the ↑ is located See the horizontal line to the left of the arrow indicating the PAOP (PAOP = PAWP; Paw = Ao) 31
Keys to Excellent Measurements • Use only the Ao as a reference for endexpiration. The respiratory waveform is not accurate! • To help determine end-expiration for a non -ventilated patient, remember: – “Vent = valley” (lower portion of waveform) – “Patient = peak” (higher portion of waveform) • PA mean = PAS + 2(PAD)/3 32
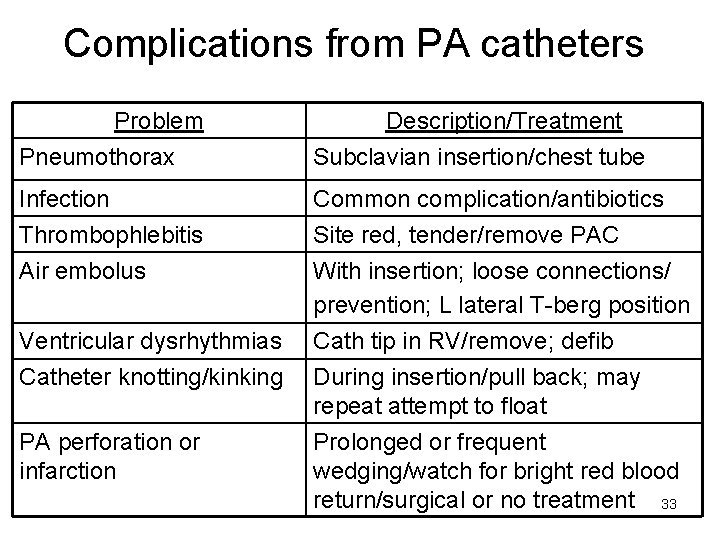
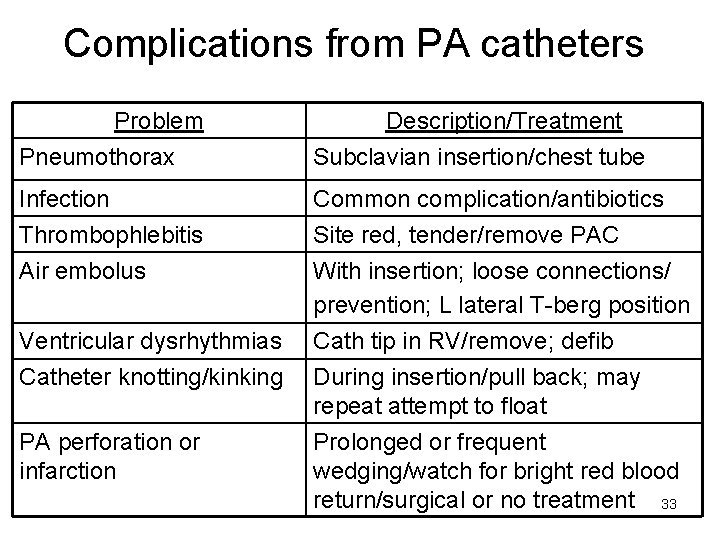
Complications from PA catheters Problem Pneumothorax Description/Treatment Subclavian insertion/chest tube Infection Thrombophlebitis Common complication/antibiotics Site red, tender/remove PAC Air embolus With insertion; loose connections/ prevention; L lateral T-berg position Cath tip in RV/remove; defib During insertion/pull back; may repeat attempt to float Prolonged or frequent wedging/watch for bright red blood return/surgical or no treatment 33 Ventricular dysrhythmias Catheter knotting/kinking PA perforation or infarction
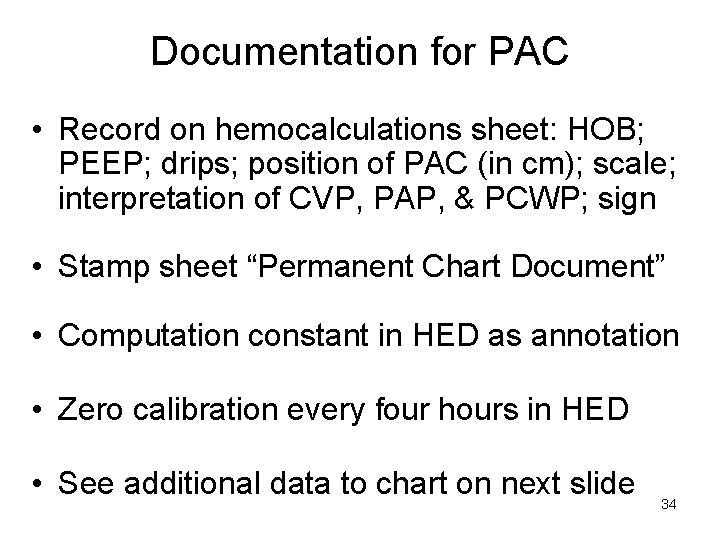
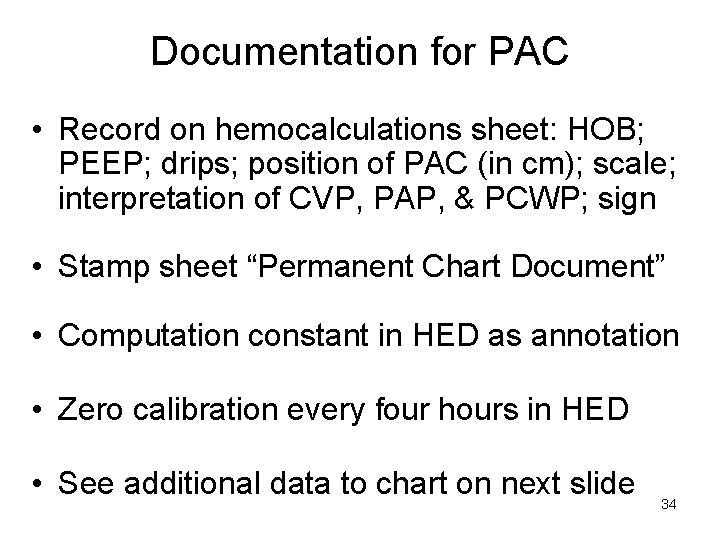
Documentation for PAC • Record on hemocalculations sheet: HOB; PEEP; drips; position of PAC (in cm); scale; interpretation of CVP, PAP, & PCWP; sign • Stamp sheet “Permanent Chart Document” • Computation constant in HED as annotation • Zero calibration every four hours in HED • See additional data to chart on next slide 34
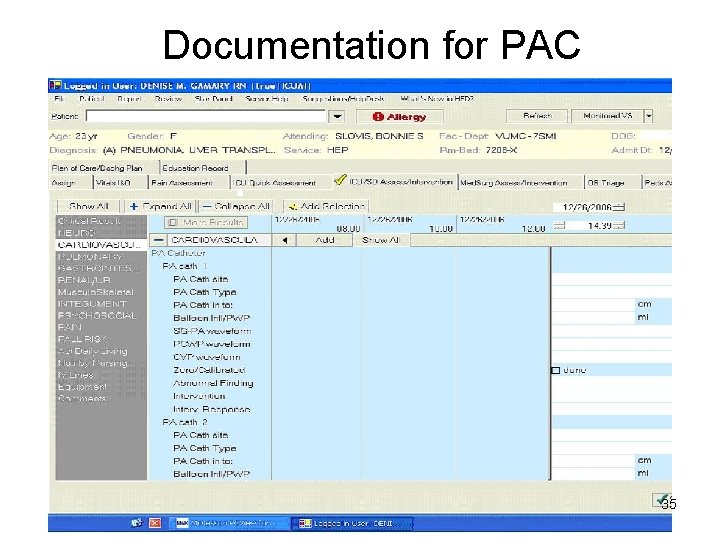
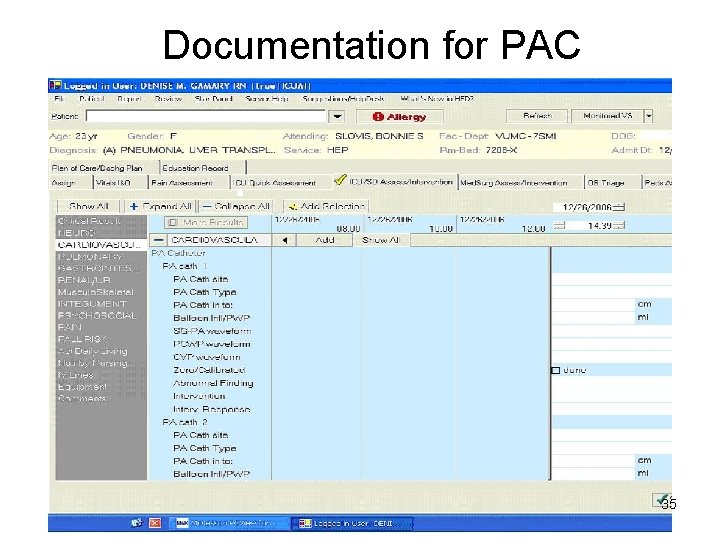
Documentation for PAC 35
References & Resources Burns, S. M. (2004). Continuous airway pressure monitoring. Critical Care Nurse, 24(6), 70 -74. Chulay, M. , & Burns, S. M. (2006). AACN Essentials of critical care. Mc. Graw-Hill: New York. Edwards. (2006). Pulmonary Artery Catheter Educational Project. http: //www. pacep. org Edwards Lifesciences. (n. d. ) Educational videos. www. edwards. com MICU Routine Practice Guidelines. www. vanderbiltmicu. com MICU Bedside Resource Books MICU Education Kits – Pulmonary Artery Catheter (Red cart in conference room) MICU Preceptors, Help All Nurses, & Charge Nurses VUMC policies. http: //vumcpolicies. mc. vanderbilt. edu 36