HEMODYNAMIC DISORDERS THROMBOEMBOLIC DISEASE AND SHOCK What is
ﺑﻪ ﻧﺎﻡ ﺧﺪﺍ HEMODYNAMIC DISORDERS, THROMBOEMBOLIC DISEASE, AND SHOCK
What is the edema ? ﺧﻴﺰ

EDEMA
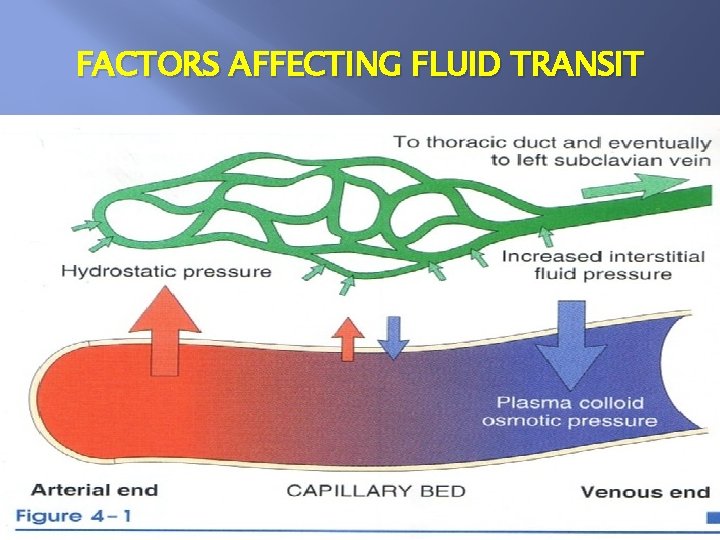
FACTORS AFFECTING FLUID TRANSIT
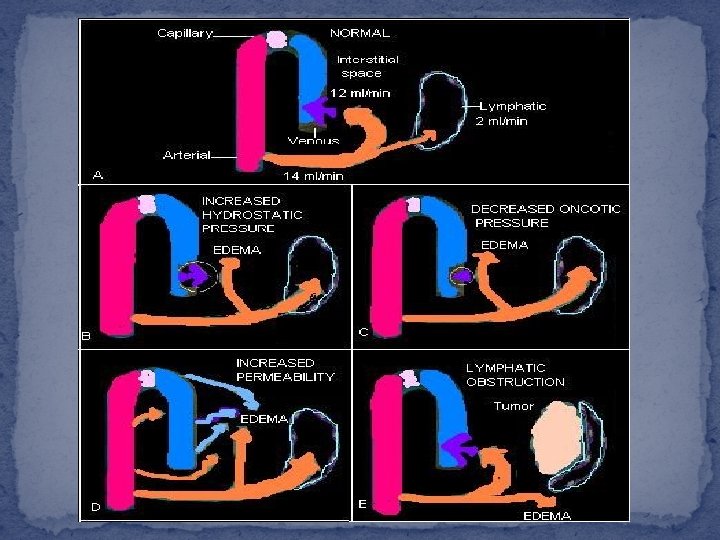

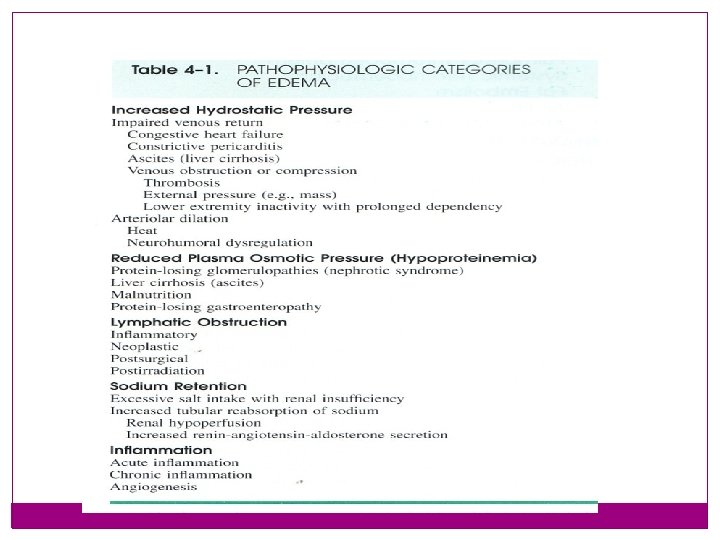
PATHOPHYSIOLOGIC CATEGORIES OF EDEMA INCREASED HYDROSTATIC PRESURE REDUCED PLASMA OSMOTIC SODIUM AND WATER RETENTION LYMPHATIC OBSTRACTION INFLAMMATION
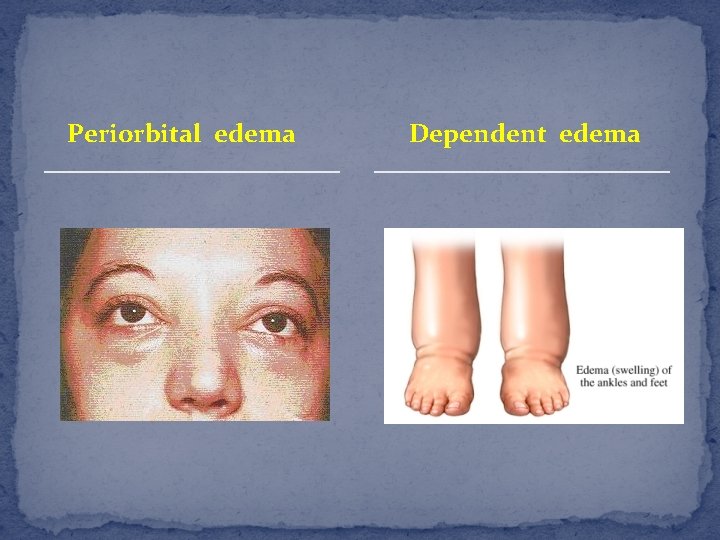
Periorbital edema Dependent edema
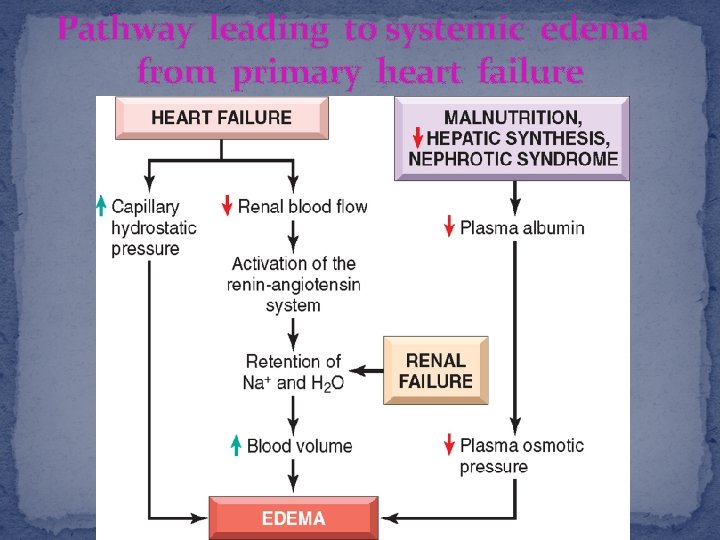
Pathway leading to systemic edema from primary heart failure
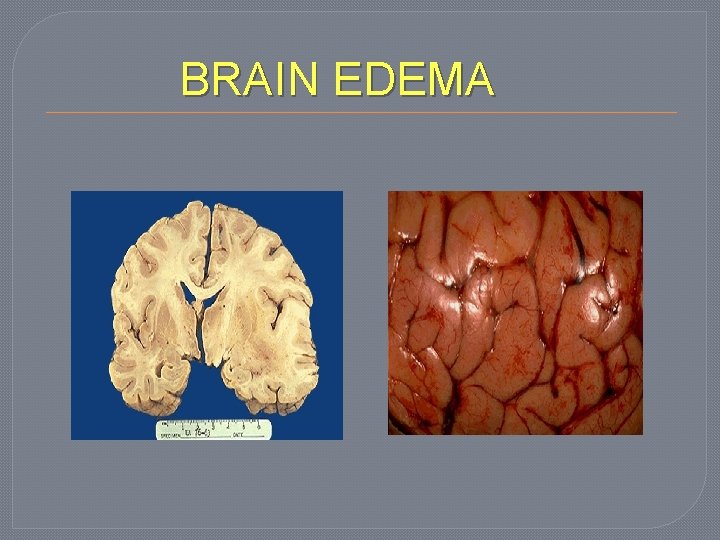
BRAIN EDEMA
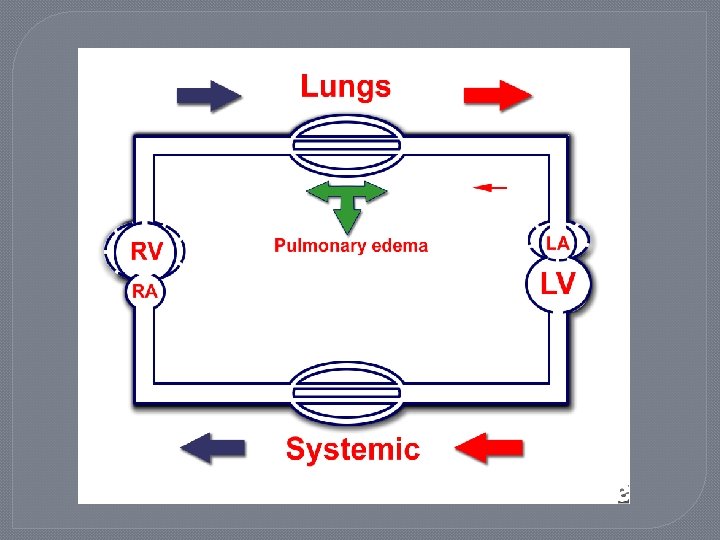

Pulmonary edema
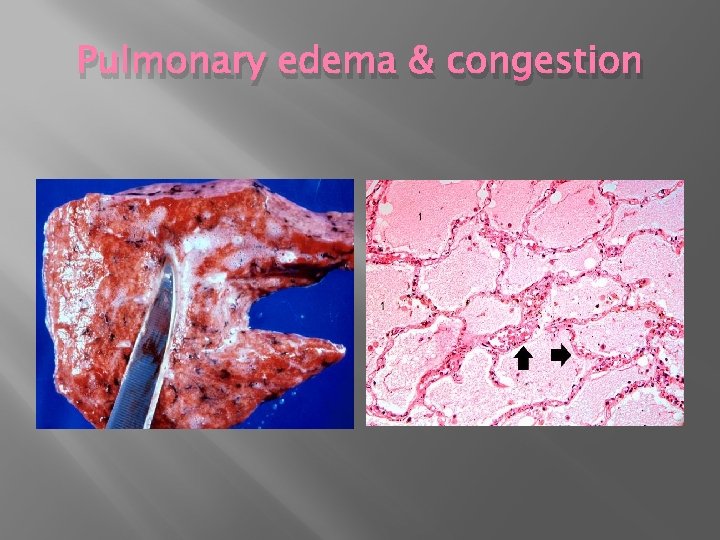
Pulmonary edema & congestion
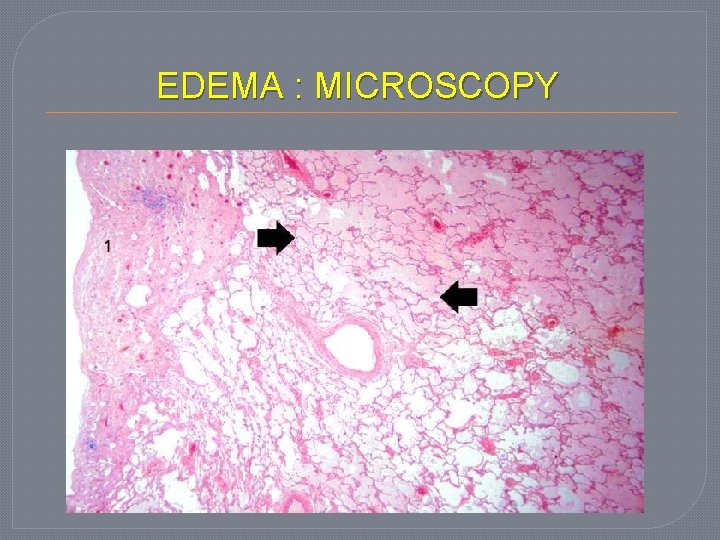
EDEMA : MICROSCOPY
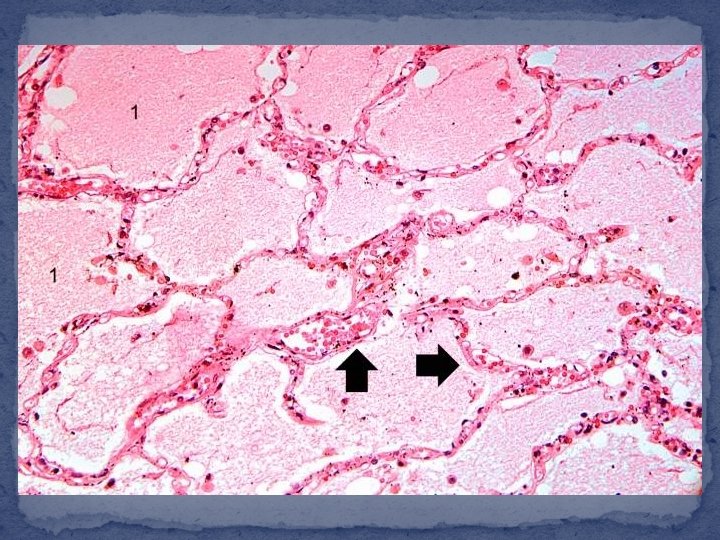

Chronic Pulmonary congestion cardiac cell
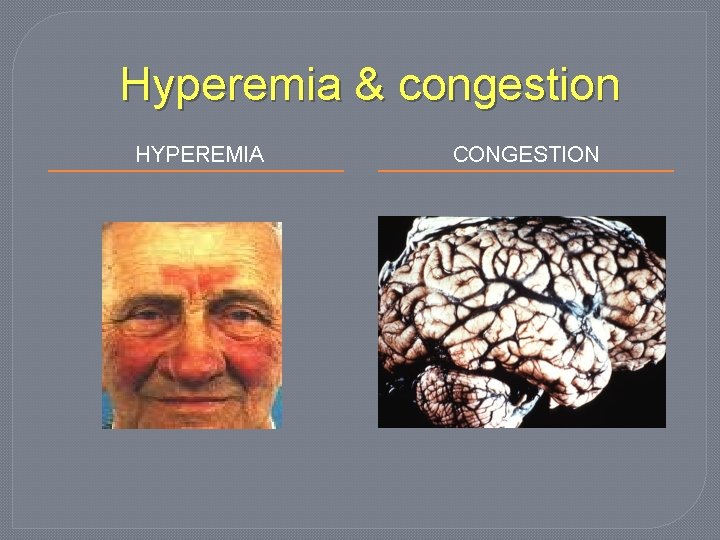
Hyperemia & congestion HYPEREMIA CONGESTION
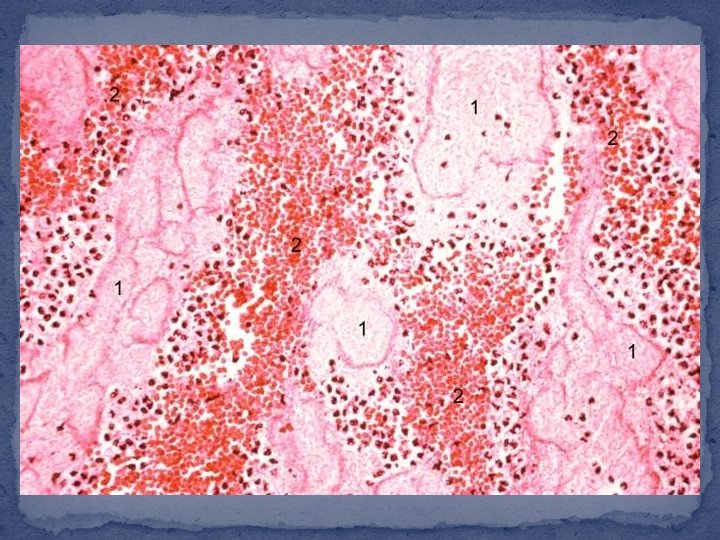

Conjestion
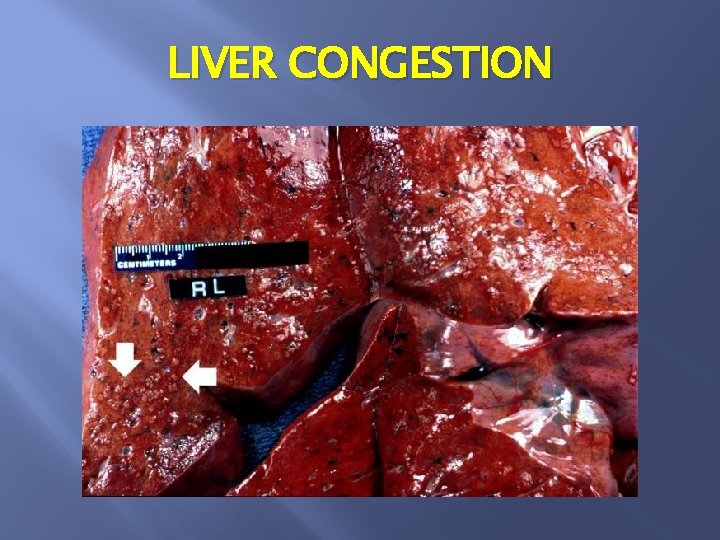
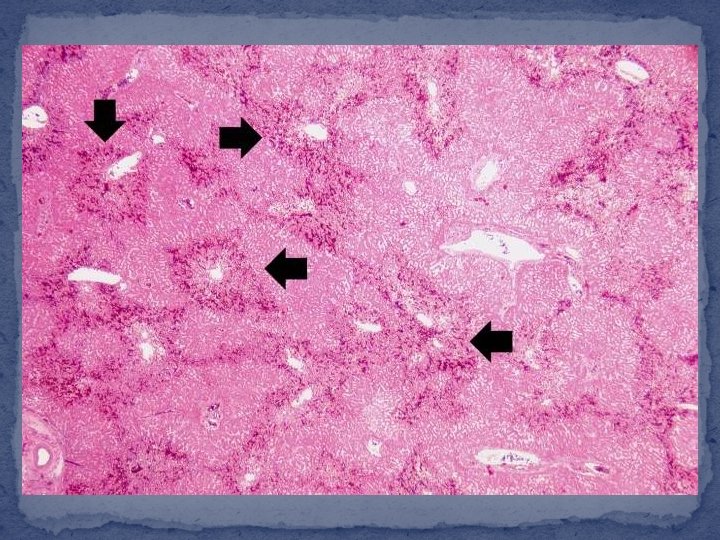
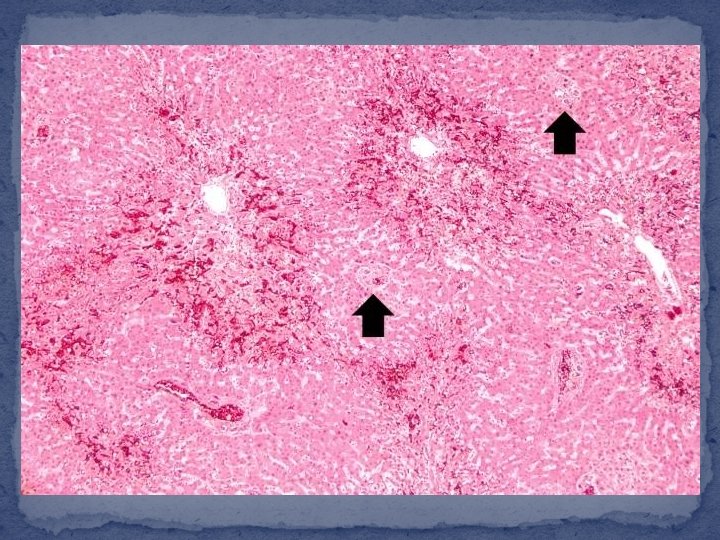
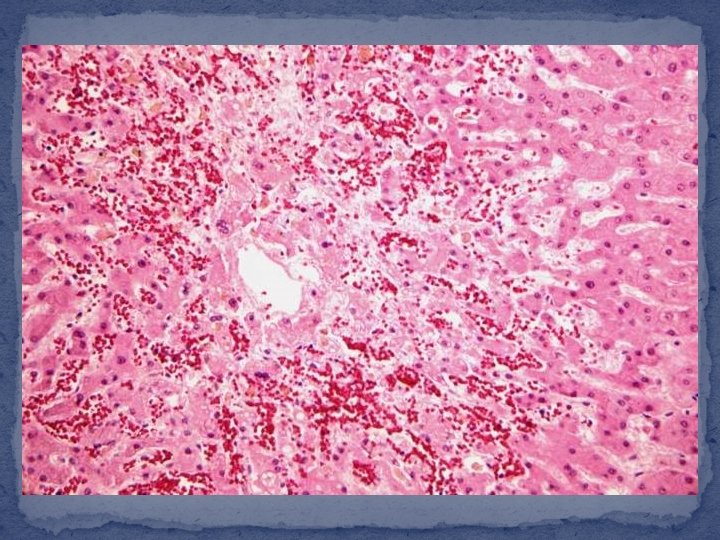
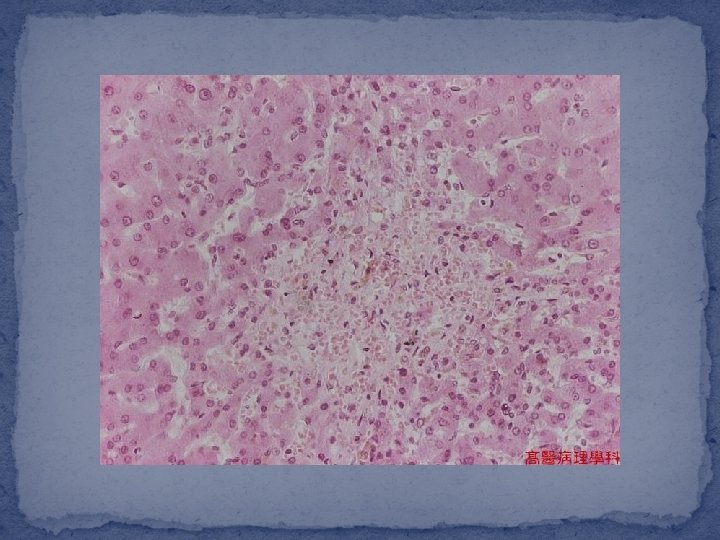
LIVER CONGESTION
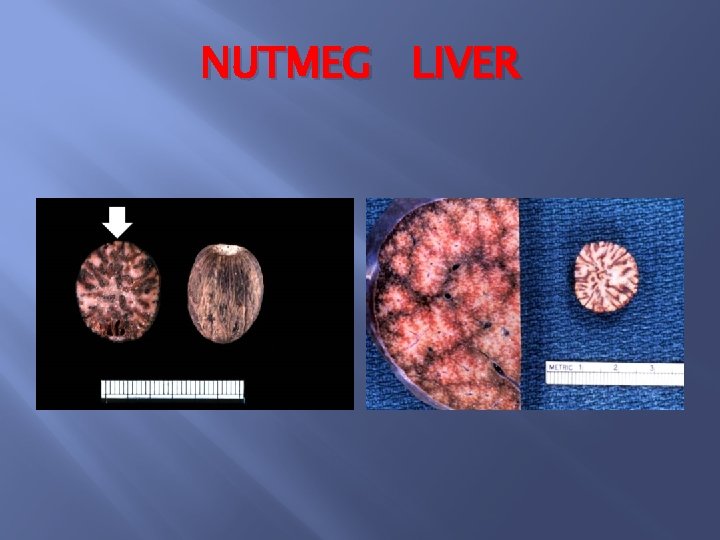
NUTMEG LIVER
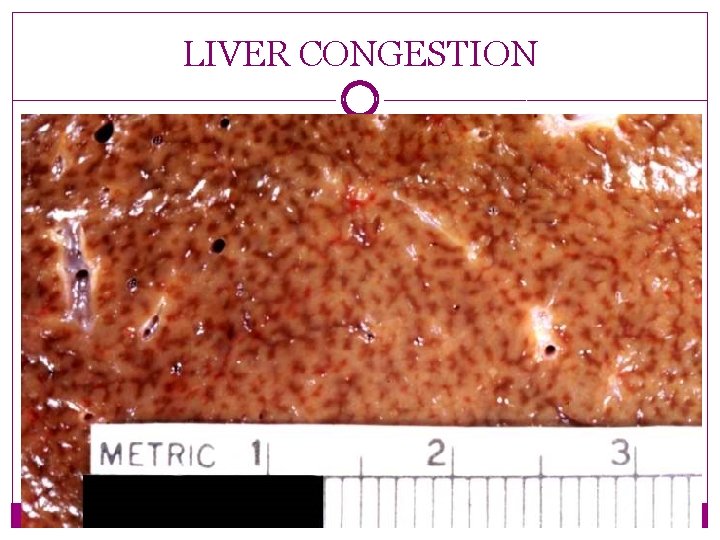
LIVER CONGESTION
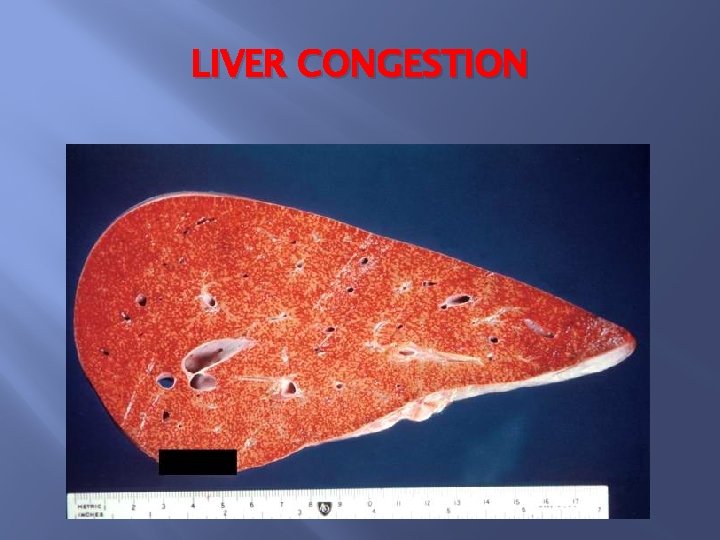
LIVER CONGESTION
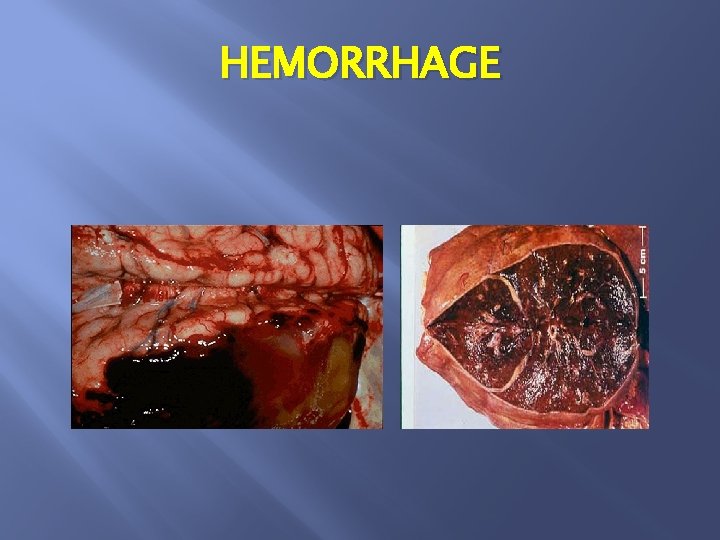
HEMORRHAGE
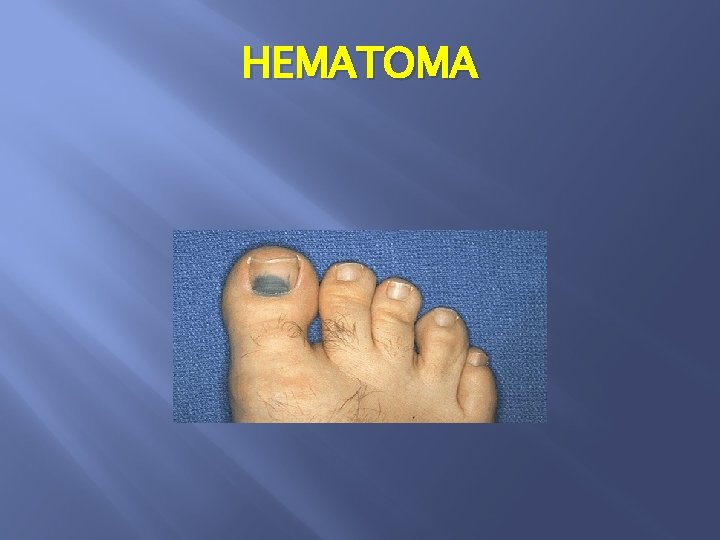
HEMATOMA
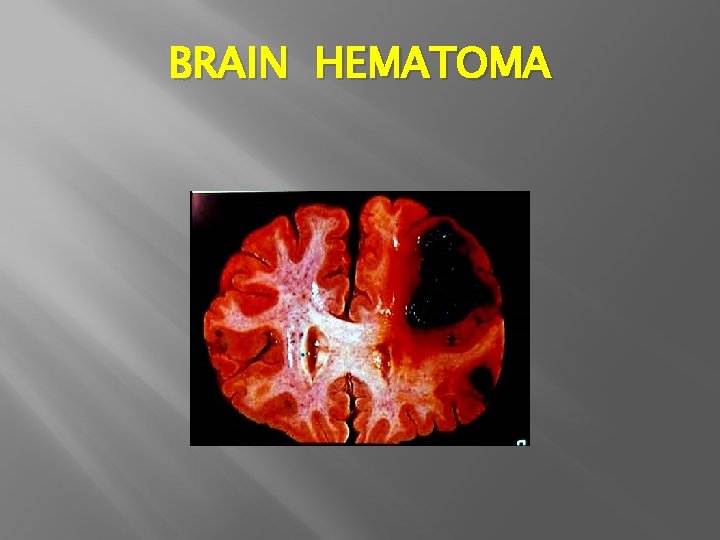
BRAIN HEMATOMA
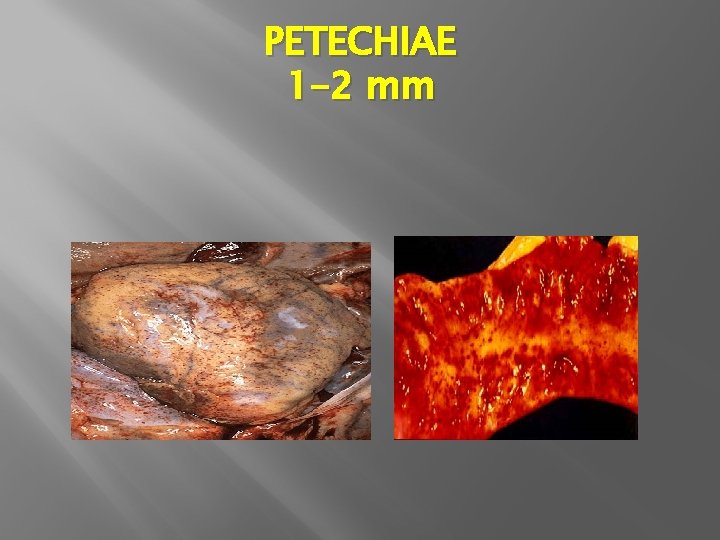
PETECHIAE 1 -2 mm

PURPURAS = or > 3 mm

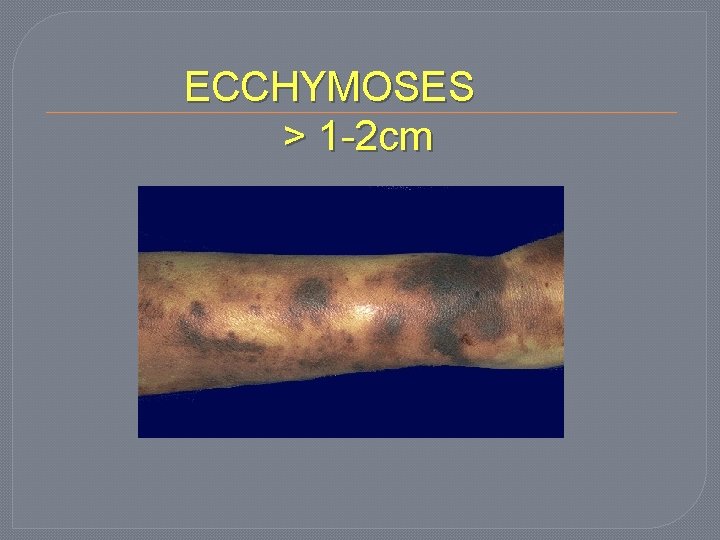
ECCHYMOSES > 1 -2 cm
ACCUMULATION OF BLOOD IN BODY CAVITY HEMOTHORAX HEMOPERICARDIUM HEMOPERITONEUM EMARTHROSIS
HEMOSTASIS AND THROMBOSIS
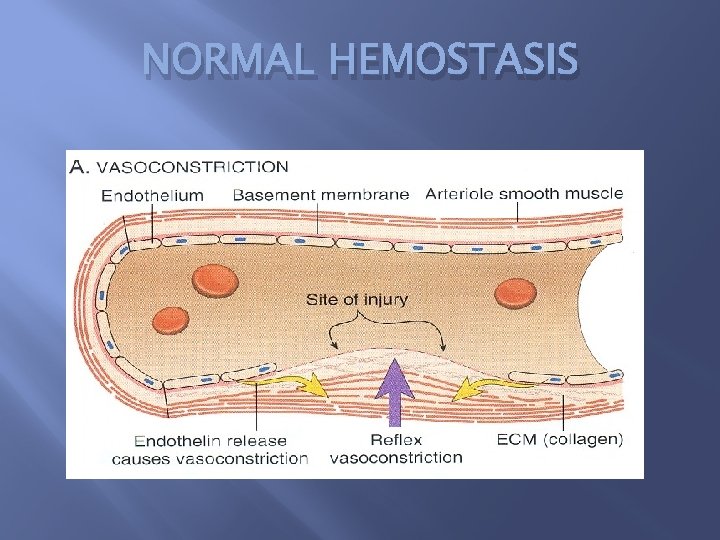
NORMAL HEMOSTASIS
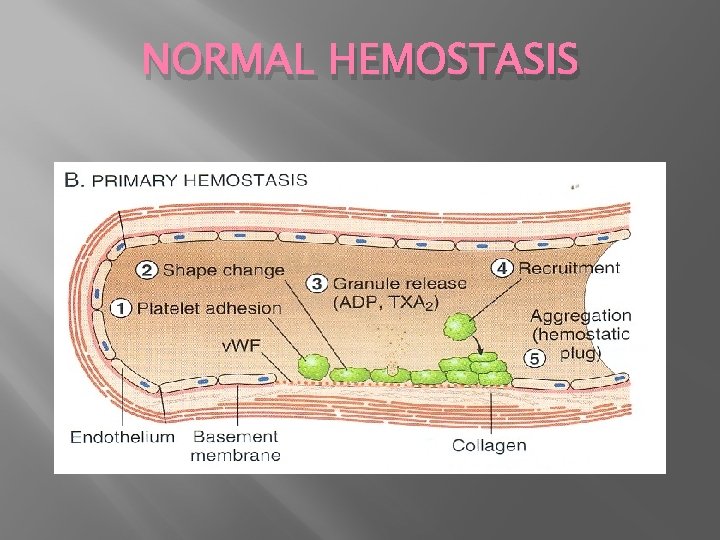
NORMAL HEMOSTASIS
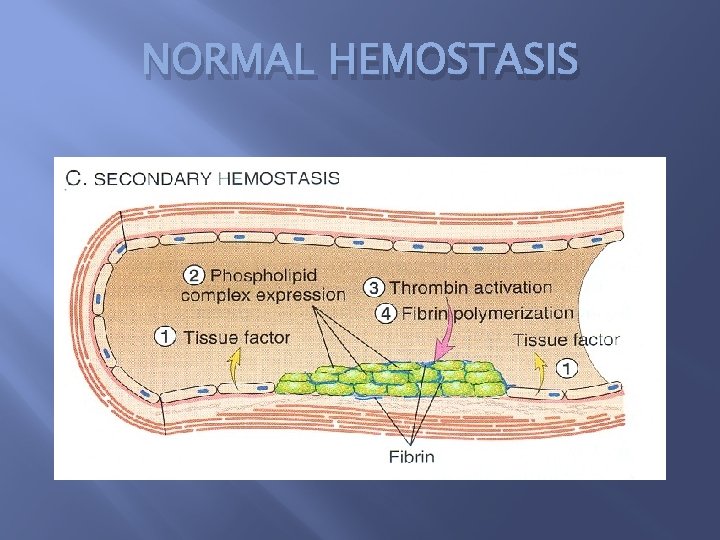
NORMAL HEMOSTASIS
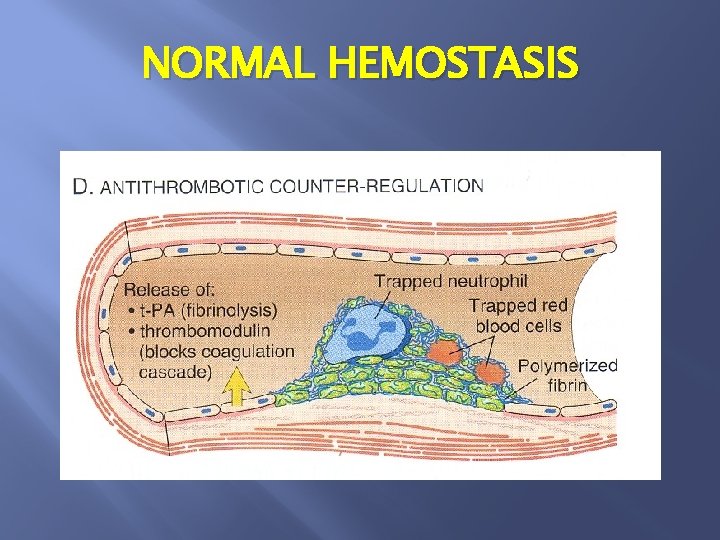
NORMAL HEMOSTASIS
NORMAL HEMOSTASIS ENDOTHELIUM � � PLATELET � � COAGULATION CASCADE �
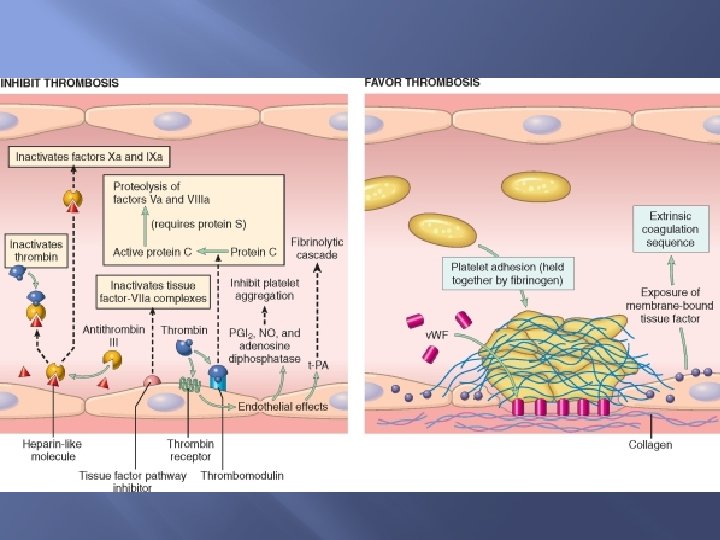
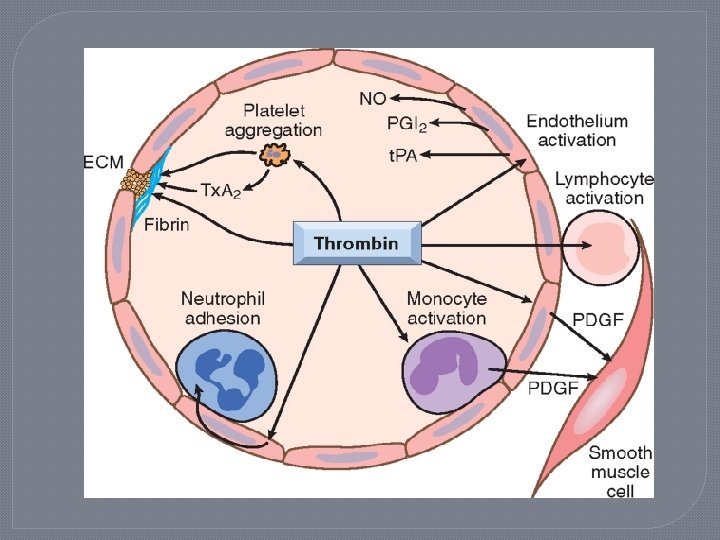
ANTITHROMBOTIC PROPERTIES ATELET EFFECTS � ICUAGULANT PROPERTIES FIBRRINOLYTIC PROPERTIES � � PROTHROMBOTIC PROPERTIES �
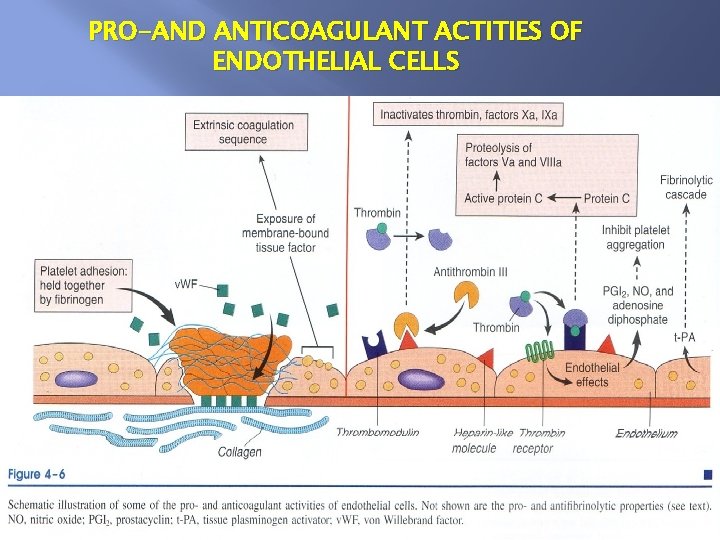
PRO-AND ANTICOAGULANT ACTITIES OF ENDOTHELIAL CELLS
ANTIPLATELET EFFECTS OF ENDOTHELIUM PG I 2 NO ADPase
Anticoagulant effects of endothelium � Heparin-like molecule � Thrombomodulin � Pro S
Fibrinolytic effects of endothelium t-PA
PROTHROMBOTIC PROPERTIES Platelet effects ( v. WF ) Procoagulant effects ( tissue factor ) Antifibrinolytic effects ( PAIs )
PLATELETS � ADHESION � SECRETION � AGGREGATION

PLATELET ADHESION ECM v. WF GP 1 b
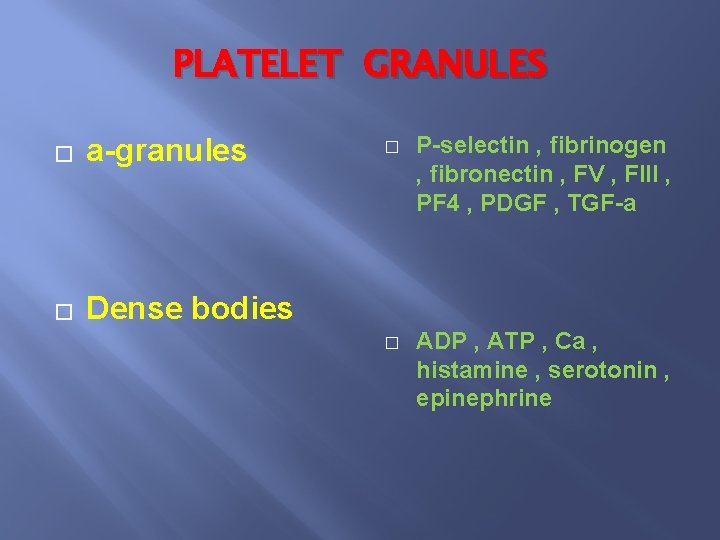
PLATELET GRANULES � a-granules � Dense bodies � P-selectin , fibrinogen , fibronectin , FV , FIII , PF 4 , PDGF , TGF-a � ADP , ATP , Ca , histamine , serotonin , epinephrine
PLATELET AGGREGATION ADP TXA 2 THROMBIN FIBRINOGEN
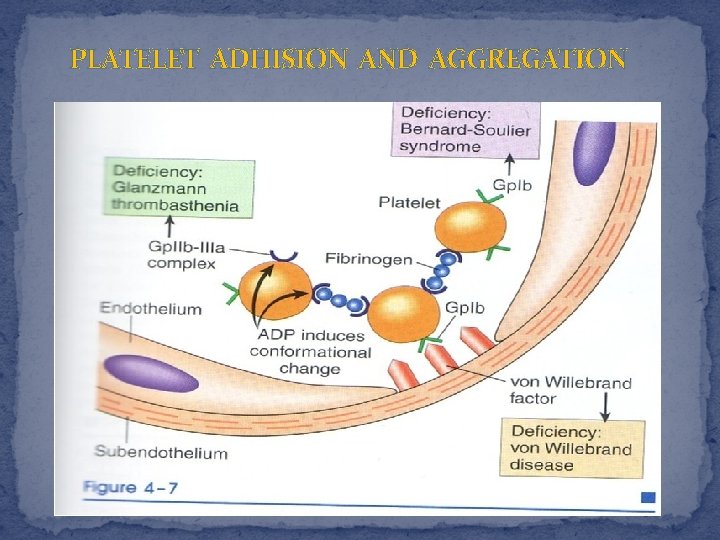
PLATELET ADHISION AND AGGREGATION
COAGULATION CASCADE
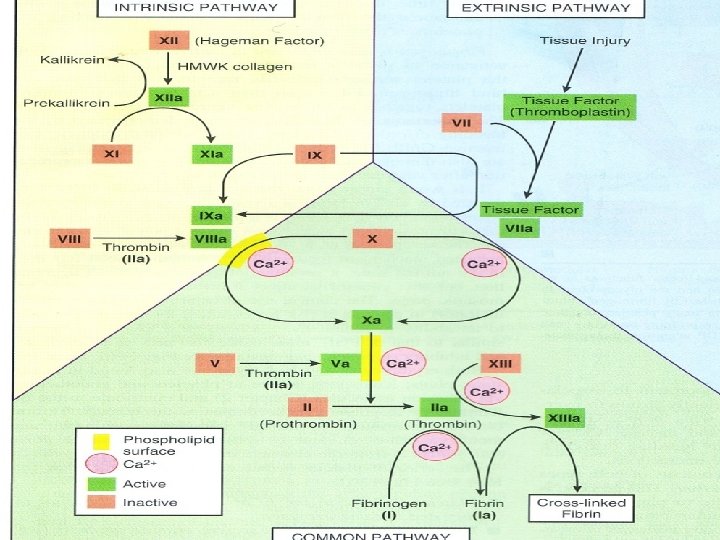
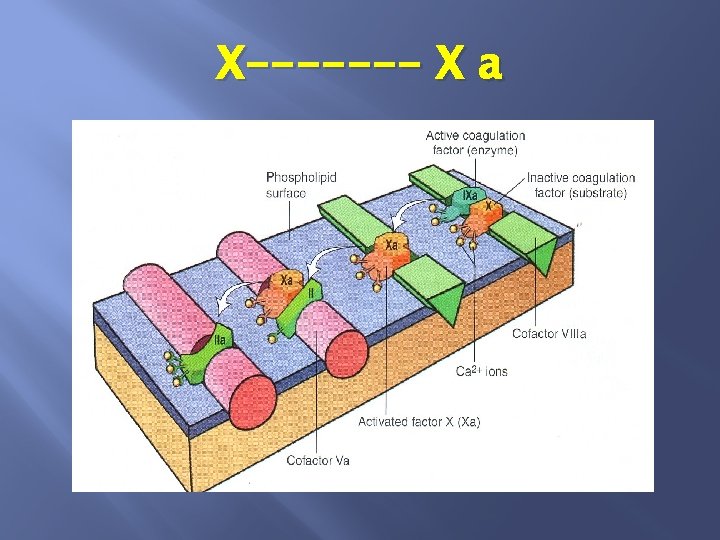
INHIBITION OF CLOTTING AN TITHROMBINS (antithrombin III ) Inactivate: thrombin-IXa-Xa-XIIa
INHIBITION OF CLOTTING PROTEIN C & S INACTIVATE: Va-VIIIa
INHIBITION OF CLOTTING FIBRINOLYTIC CASCADE: plsminogen-plasmin
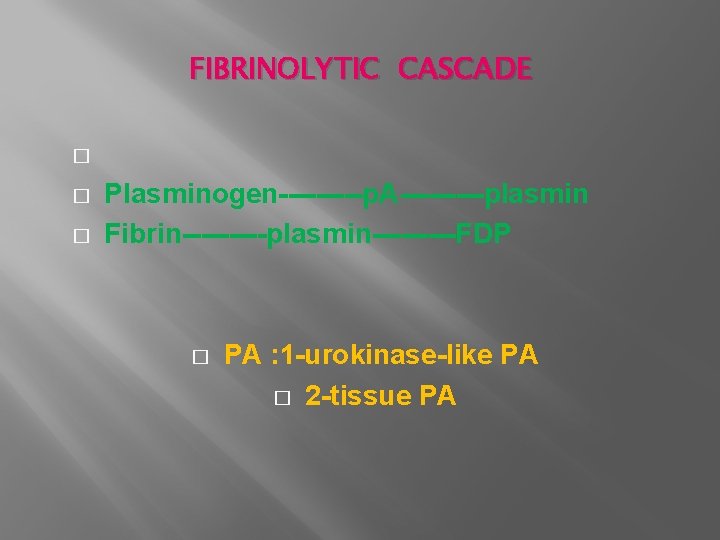
FIBRINOLYTIC CASCADE � � � Plasminogen-----p. A-----plasmin Fibrin-----plasmin-----FDP � PA : 1 -urokinase-like PA � 2 -tissue PA
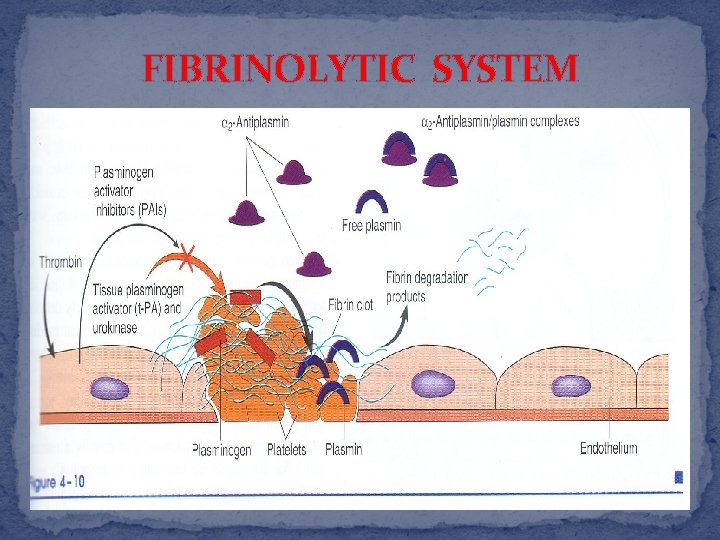
FIBRINOLYTIC SYSTEM

THROMBOSIS
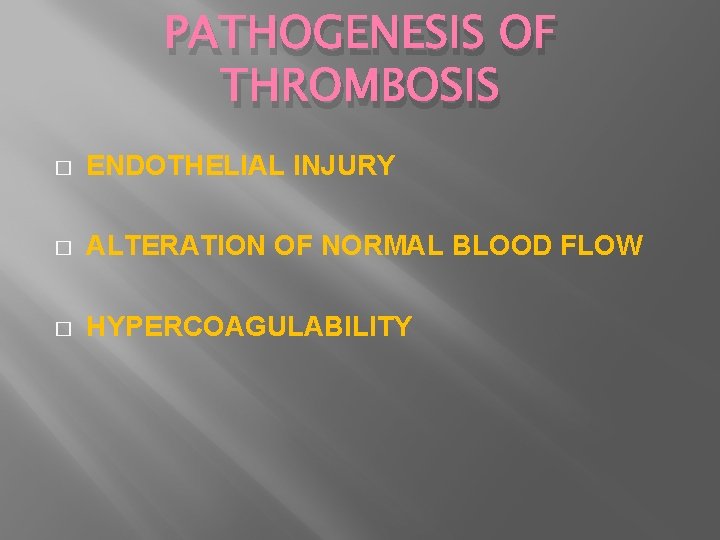
PATHOGENESIS OF THROMBOSIS � ENDOTHELIAL INJURY � ALTERATION OF NORMAL BLOOD FLOW � HYPERCOAGULABILITY
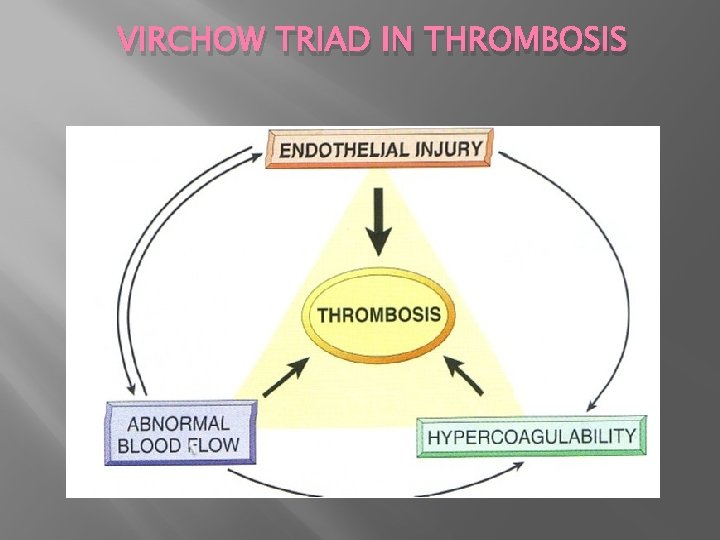
VIRCHOW TRIAD IN THROMBOSIS
ENDOTHELIAL INJURY � � � � � MI Valvulitis Traumatic-hemodynamic stress Inflammation Endotoxins Homocystinuria Hypercholesterolemia Radiation Cigarette smoke
ALTERATION OF NORMAL BLOOD FLOW � Disrupt laminar flow � Prevent dilution activated clotting factor � Reduce inflow of clotting factor inhibitors � Promote endothelial cell activation
CONDITIONS ASSOCIATED WITH AN INCREASED THROMBOSIS � PRIMARY(GENETIC): � FACTOR V MUTATIONS � PROTHROMBIN MUTATION ANTITHROMBIN III DEFICIENCY PROTEIN C OR S DEFICIENCY � � *
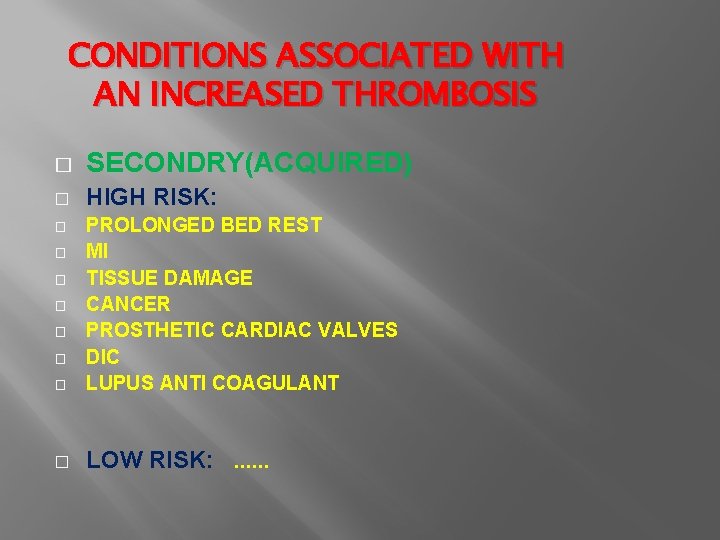
CONDITIONS ASSOCIATED WITH AN INCREASED THROMBOSIS � SECONDRY(ACQUIRED) � HIGH RISK: � PROLONGED BED REST MI TISSUE DAMAGE CANCER PROSTHETIC CARDIAC VALVES DIC LUPUS ANTI COAGULANT � LOW RISK: . . . � � �
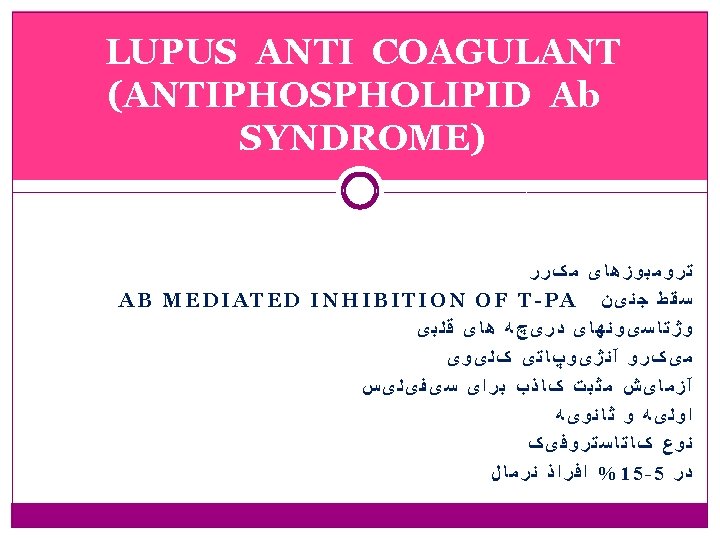

LUPUS ANTI COAGULANT ANTIPHOSPHOLIPID Ab SYNDROME) (ANTIPHOSPHOLIPID � INVITRO: INHIBIT COAGULATION � INVIVO: INDUCE COAGULATION
MORPHOLOGY OF THROMBOSIS � CARDIAC THROMBI � ATERIAL THROMBI � VENOUS THROMBOSIS
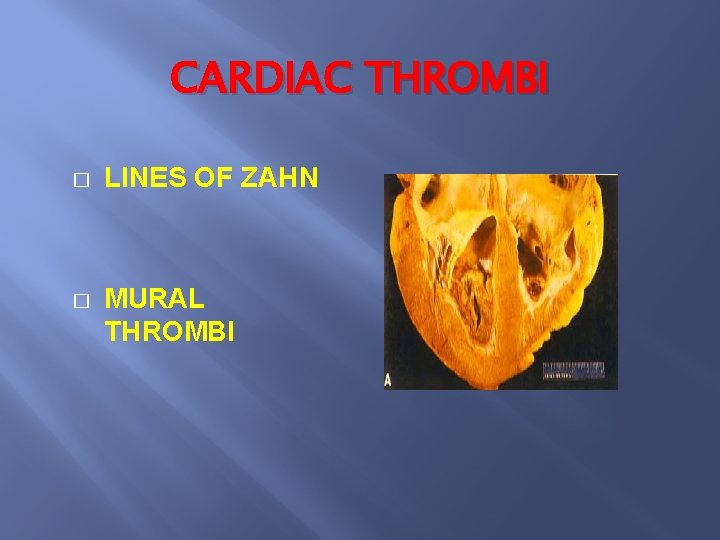
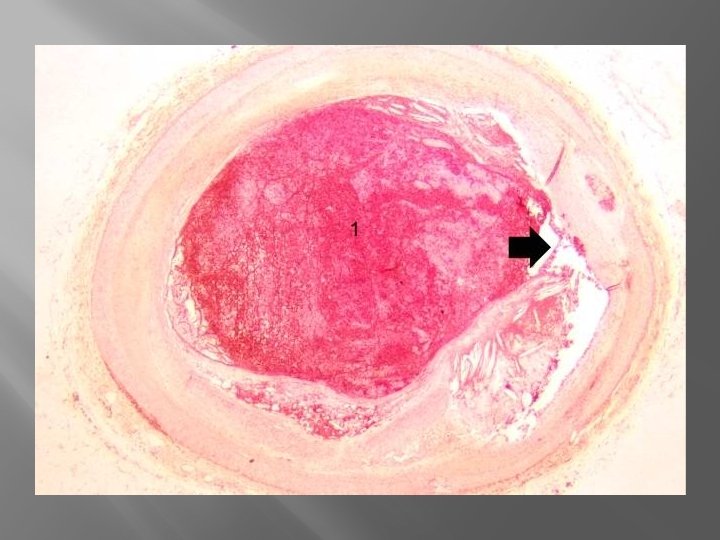
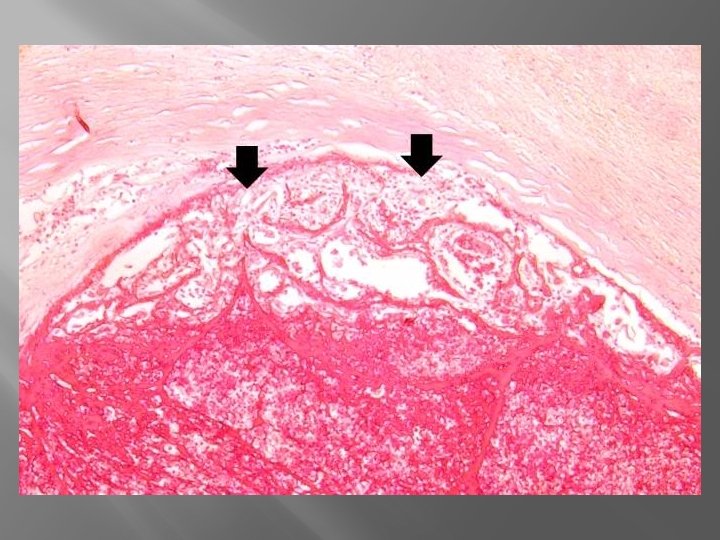
CARDIAC THROMBI � LINES OF ZAHN � MURAL THROMBI
ATERIAL THROMBI � � � � USUALLY OCCULSIVE CORONARY CEREBRAL FEMORAL … ATHEROSCLEROTIC PLAQUE FIRMLY ADHERENT TO THE WALL GRAY-WHITE
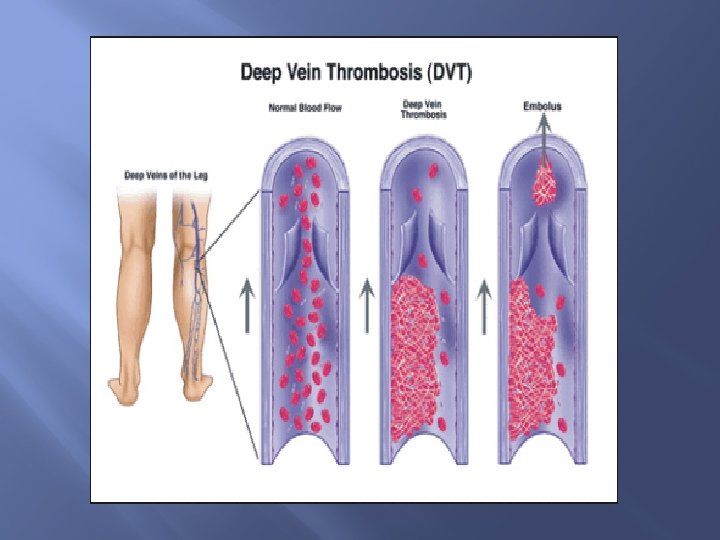
VENOUS THROMBOSIS PHELEBOTHROMBOSIS � ALMOST INVARIABLY OCCULUSIVE � RED STASIS THROBI � LOWER EXTREMITIES � POST MORTOM CLOTS MAY BE MISTAKEN
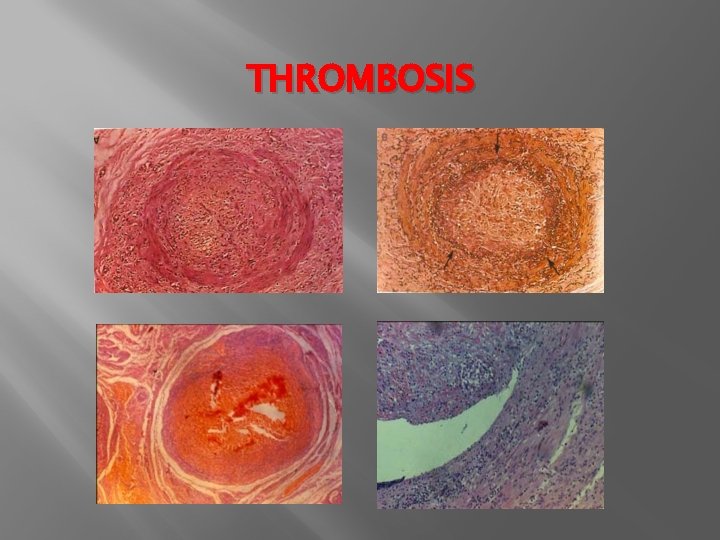
THROMBOSIS
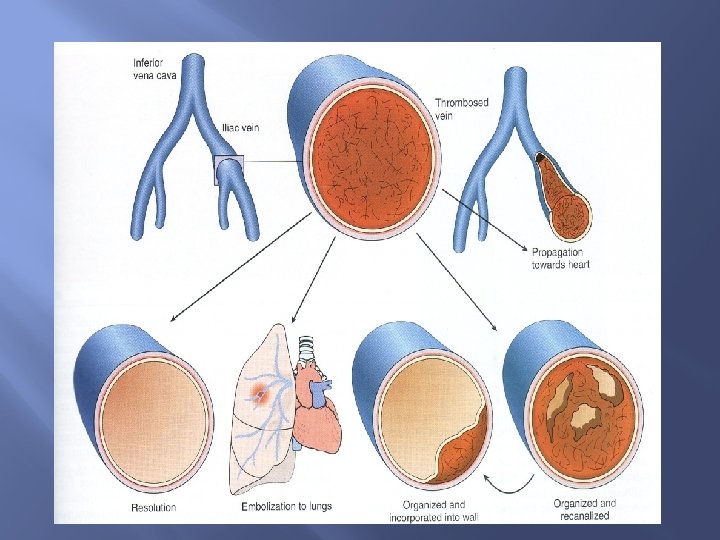
FATE OF THROMBUS � PROPAGATION � EMBOLIZATION � DISSOLUTION � ORGANIZATION
DISSEMINATED INTRA VASCULAR COAGULATION (DIC) � � Not primary Comsumption coagulopathy � Widespread fibrin thrombi in the microcirculation � Diffuse circulatory insufficiency Brain lung heart kidney… �
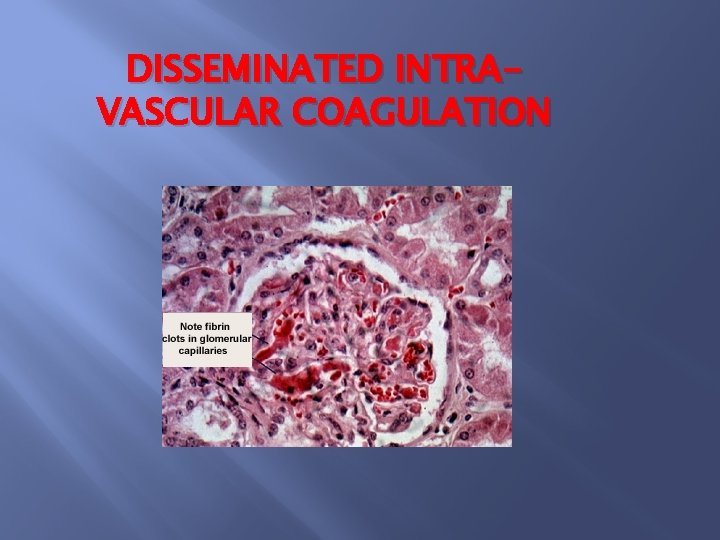
DISSEMINATED INTRAVASCULAR COAGULATION
INFARCTION � � � � ISCHEMIC INFARCTION 90% THROMBOTIC OR EMBOLIC VASOSPASM SWELLING OF ATHROMA EXTRINSIC COMPRESSION TORSION, VOLVULUS …. .
MORPHOLOGY OF INFARCTION � RED(HEMORRHAGIC � WHITE(ANEMIC) � SEPTIC
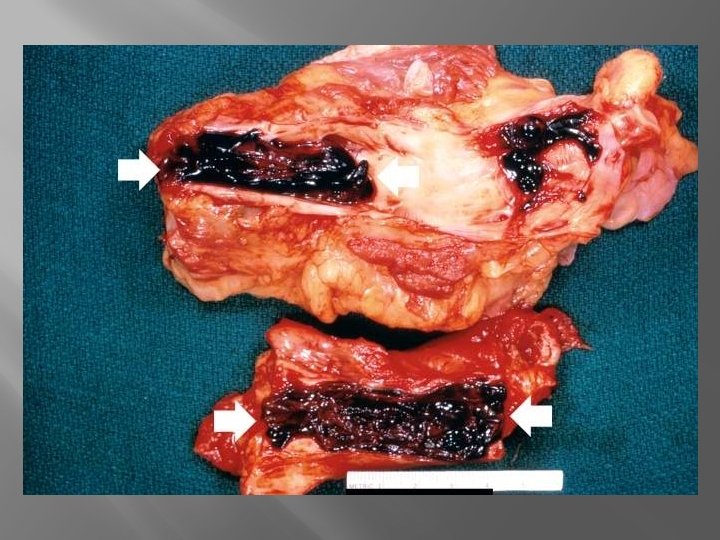
RED INFARCT � VENOUS OCCLUSION � LOOSE TISSUES � DUAL CIRCULATION � PERVIOS CONGESTION � REPERFUSION

DARK RED INFARCT IN HEART

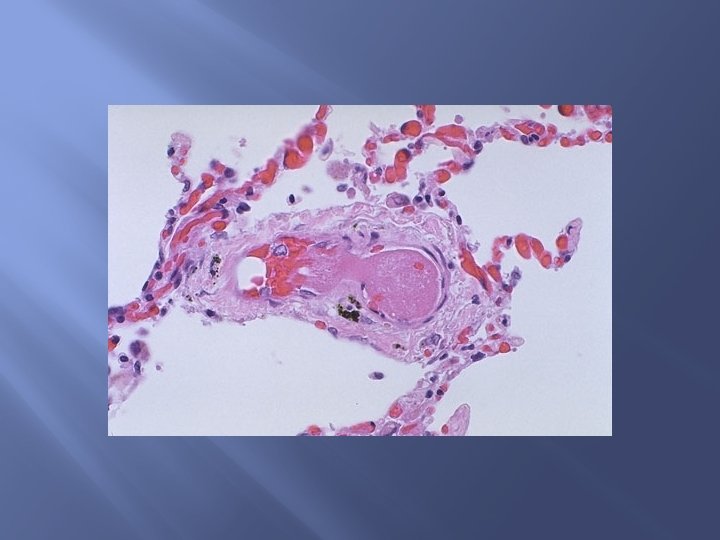
RED INFARCT LUNG
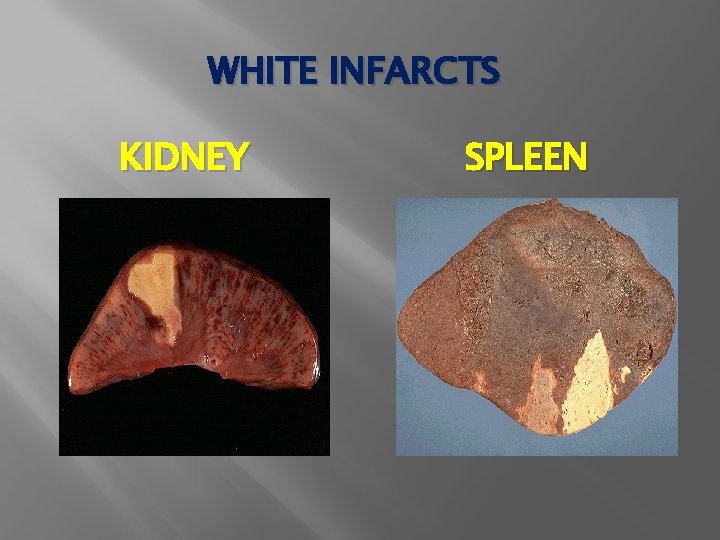
WHITE INFARCTS KIDNEY SPLEEN
HISTOLOGY OF INFARCTS � ISCHEMIC COAGULATIVE NECROSIS � LIQUEFACTIVE NECROSIS � ABCESS
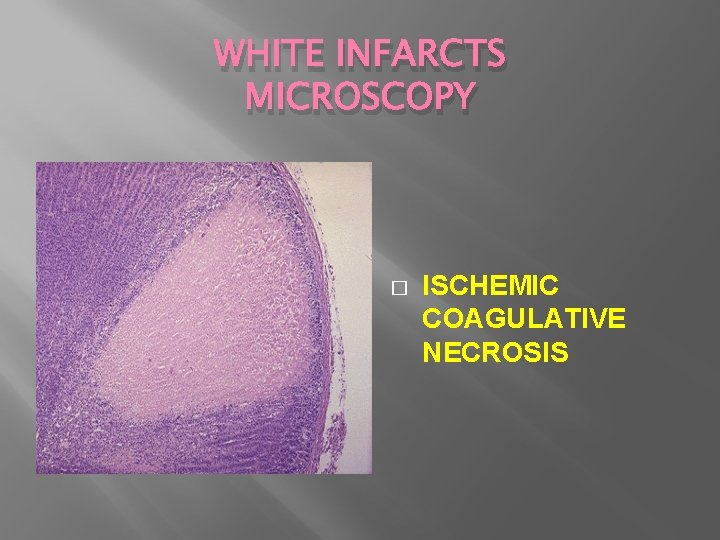
WHITE INFARCTS MICROSCOPY � ISCHEMIC COAGULATIVE NECROSIS
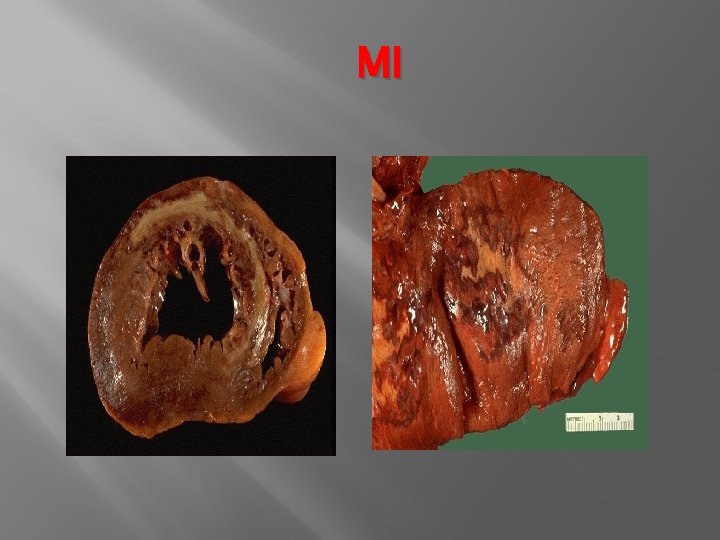
MI

BRAIN INFARCT

BRAIN INFARCT LIQUEFACTIVE NECROSIS
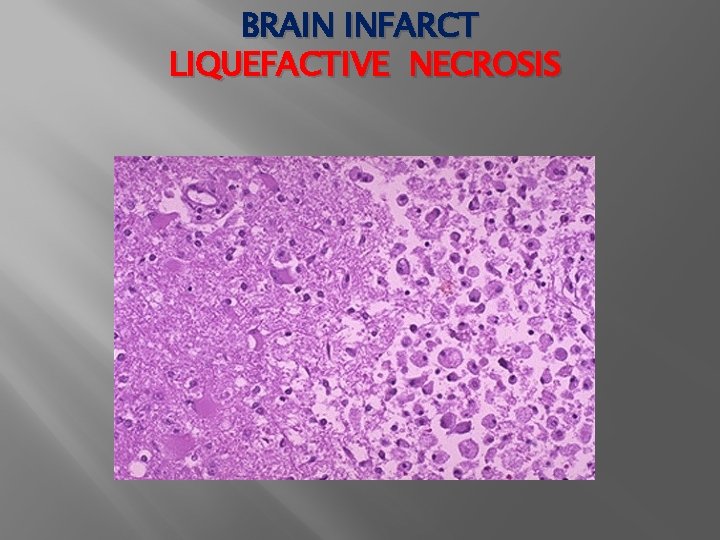
BRAIN INFARCT LIQUEFACTIVE NECROSIS

Septic infarction
FACTORS THAT INFLUENCE DEVELOPMENT OF AN INFARCT � NATURE OF THE VASCULAR SUPPLY � RATE OF DEVELOPMENT OF OCCLUSION � VULNERABILITY TO HYPOXIA � OXYGEN CONTENT OF BLOOD
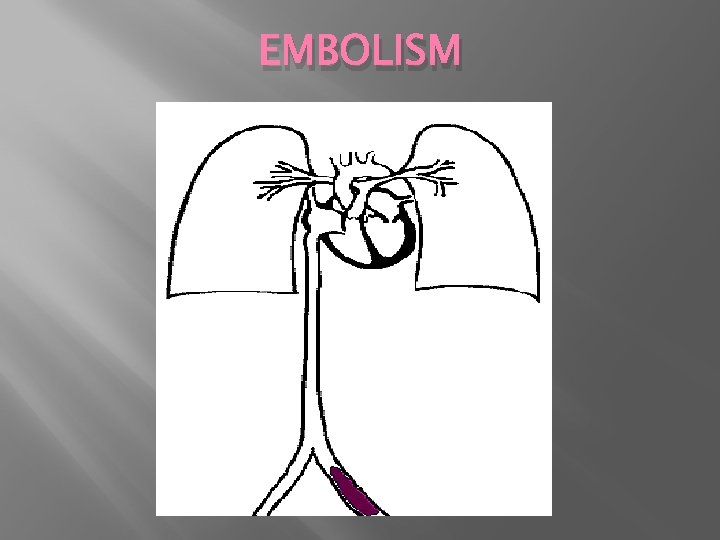
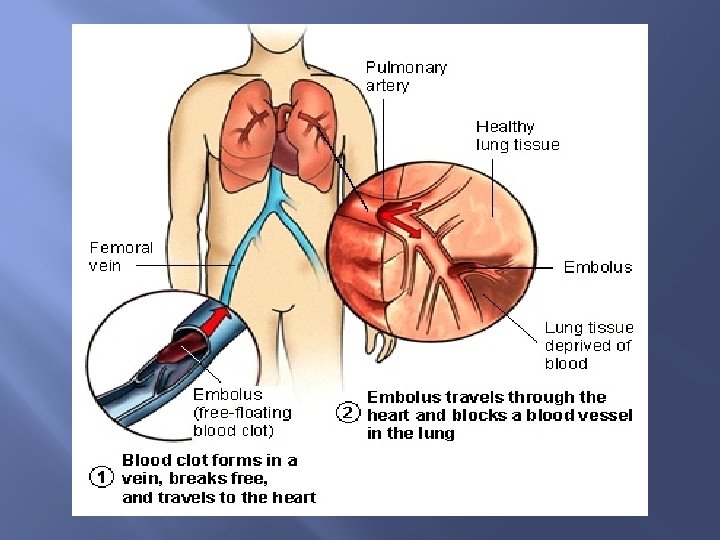
EMBOLISM
EMBOLISM � � � � Thromboembolism 99% Fat Air bubbles Cholestrol emboli Tumor fragment Bits of B. M Foreign bodies
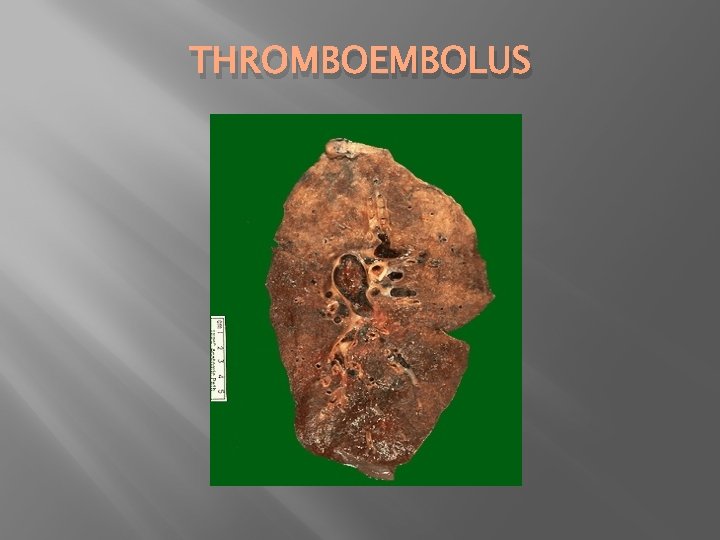
THROMBOEMBOLUS
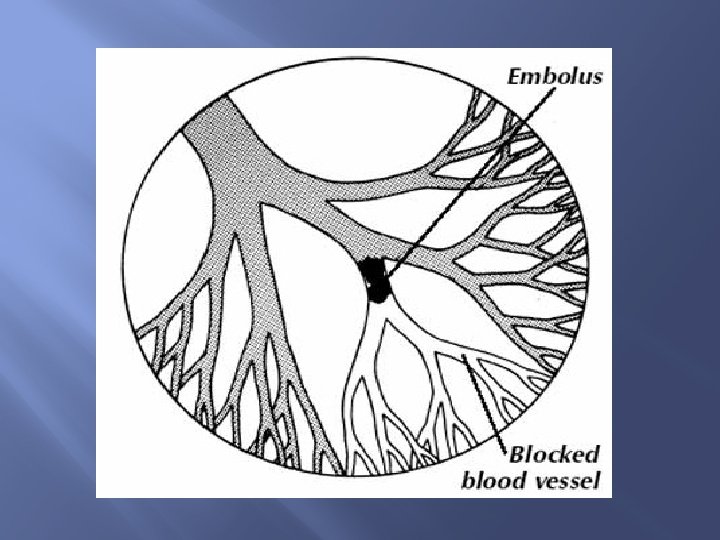
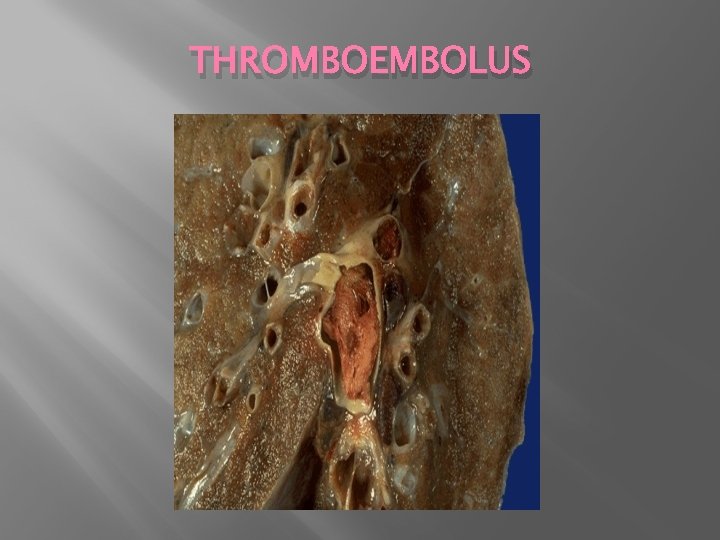
THROMBOEMBOLUS
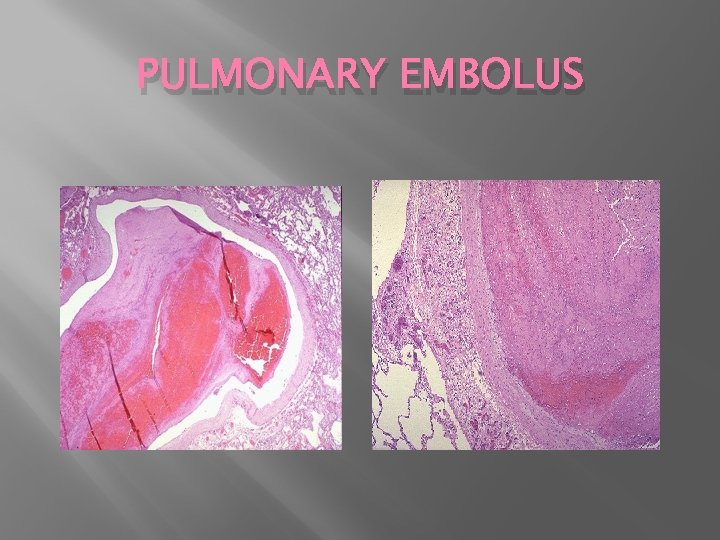
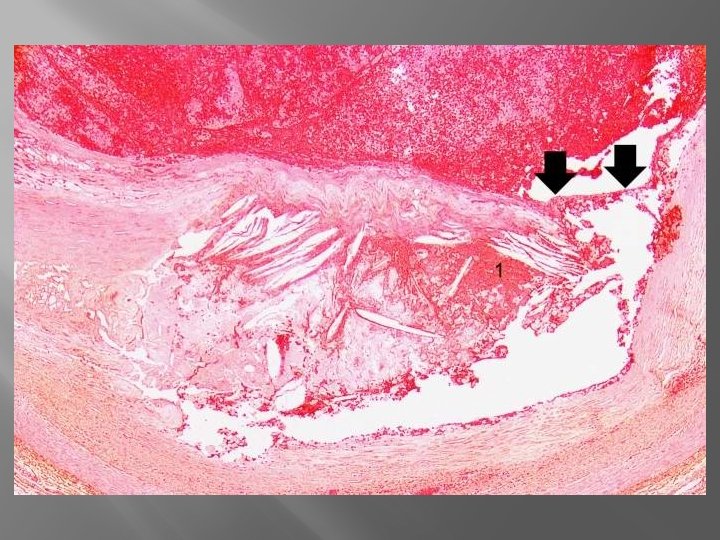
PULMONARY EMBOLUS
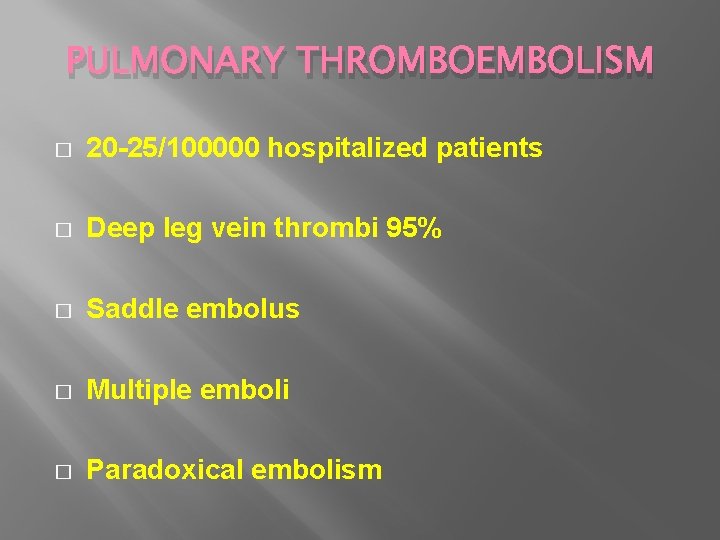
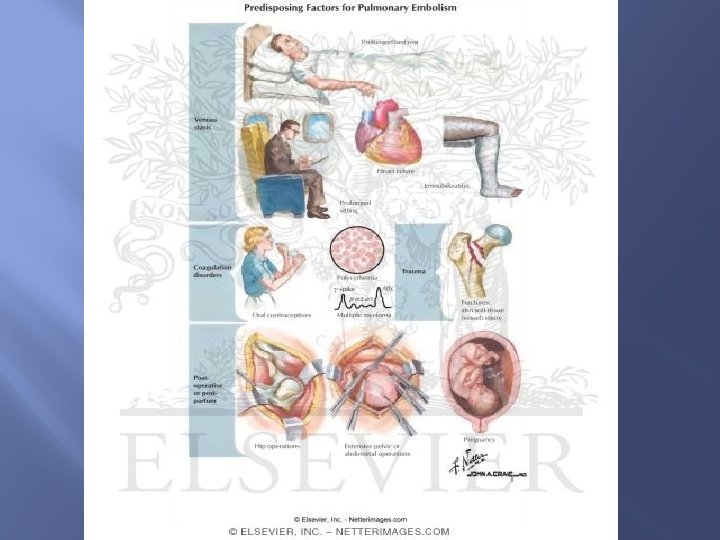
PULMONARY THROMBOEMBOLISM � 20 -25/100000 hospitalized patients � Deep leg vein thrombi 95% � Saddle embolus � Multiple emboli � Paradoxical embolism
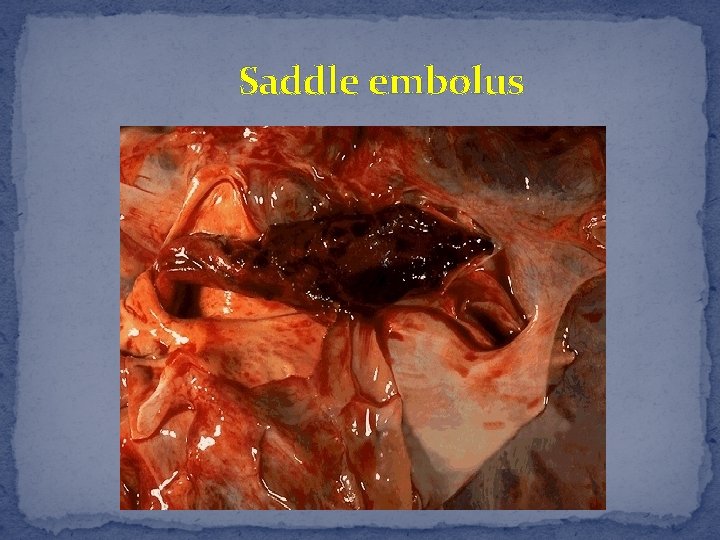
Saddle embolus
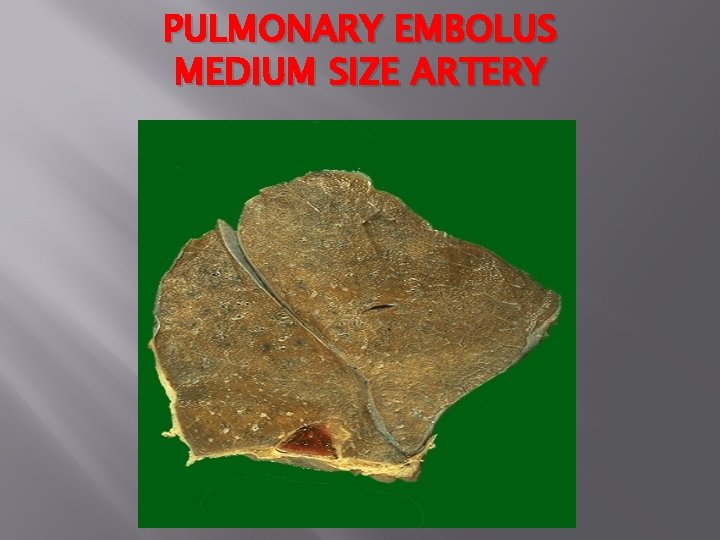
PULMONARY EMBOLUS MEDIUM SIZE ARTERY
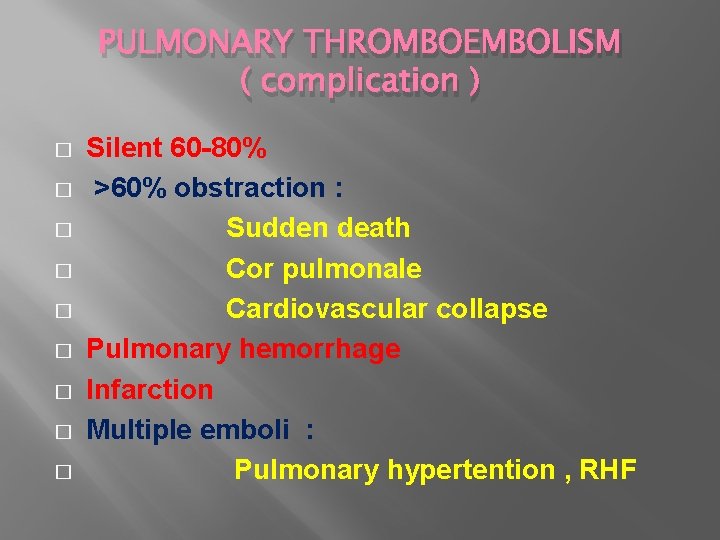
PULMONARY THROMBOEMBOLISM ( complication ) � � � � � Silent 60 -80% >60% obstraction : Sudden death Cor pulmonale Cardiovascular collapse Pulmonary hemorrhage Infarction Multiple emboli : Pulmonary hypertention , RHF
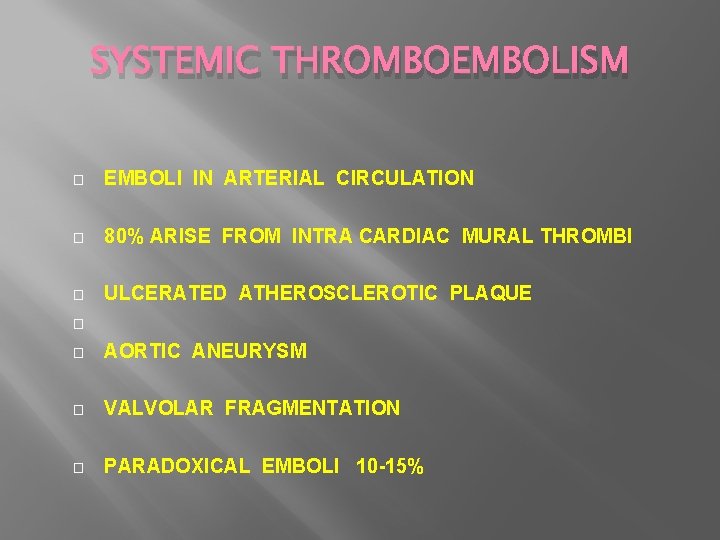
SYSTEMIC THROMBOEMBOLISM � EMBOLI IN ARTERIAL CIRCULATION � 80% ARISE FROM INTRA CARDIAC MURAL THROMBI � ULCERATED ATHEROSCLEROTIC PLAQUE � � AORTIC ANEURYSM � VALVOLAR FRAGMENTATION � PARADOXICAL EMBOLI 10 -15%
SYSTEMIC THROMBOEMBOLISM � THE SITE OF ARREST LOWER EXTREMITIES 75% � BRAIN 10% � INTESTINES � KIDNEY � SPLEEN � COMPLICATION: INFARCTION
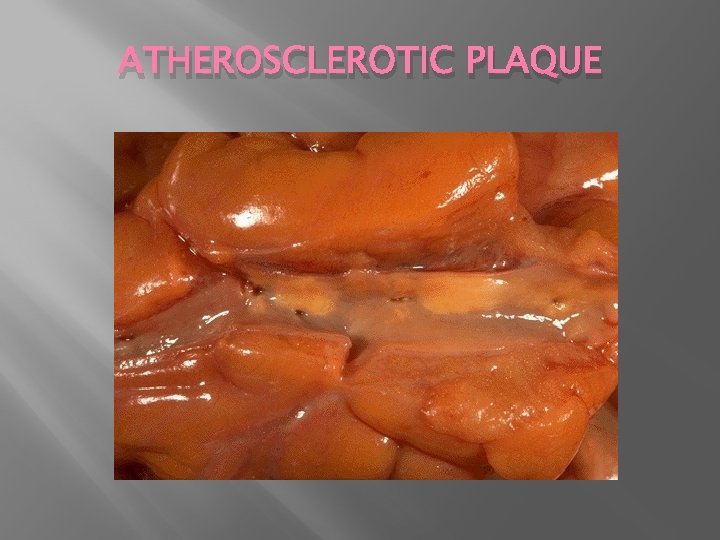
ATHEROSCLEROTIC PLAQUE
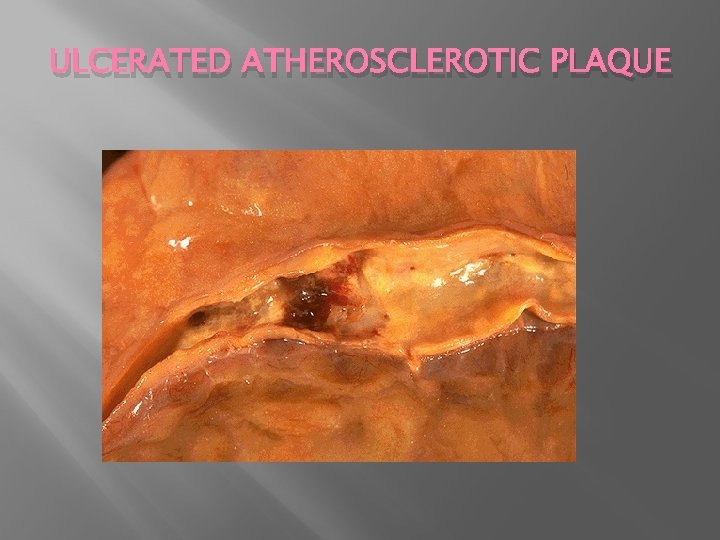
ULCERATED ATHEROSCLEROTIC PLAQUE
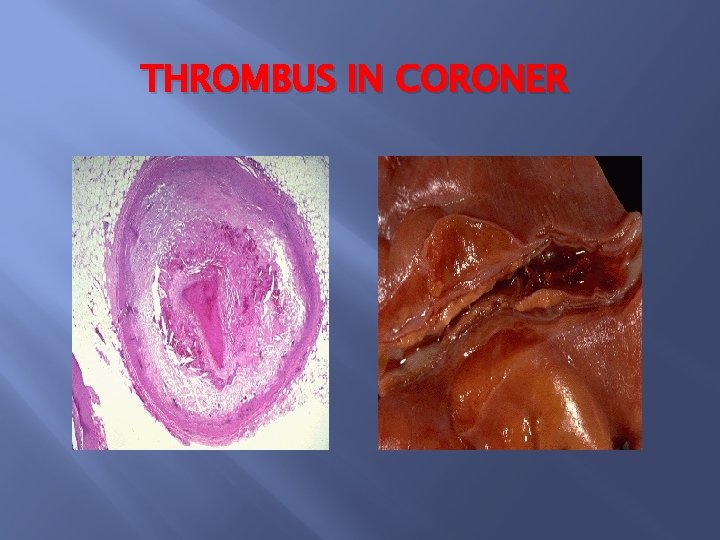
THROMBUS IN CORONER
FAT EMBOLISM � FRACTURES OF LUNG BONES � SOFT TISSUE TRAUMA � BURNS
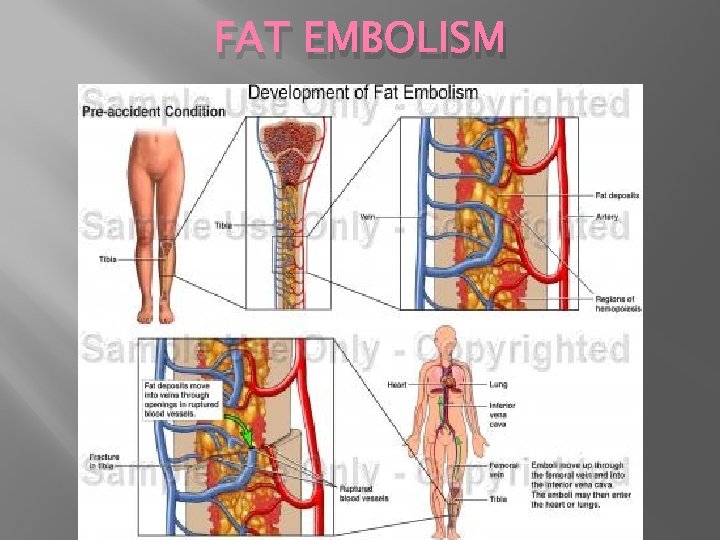
FAT EMBOLISM
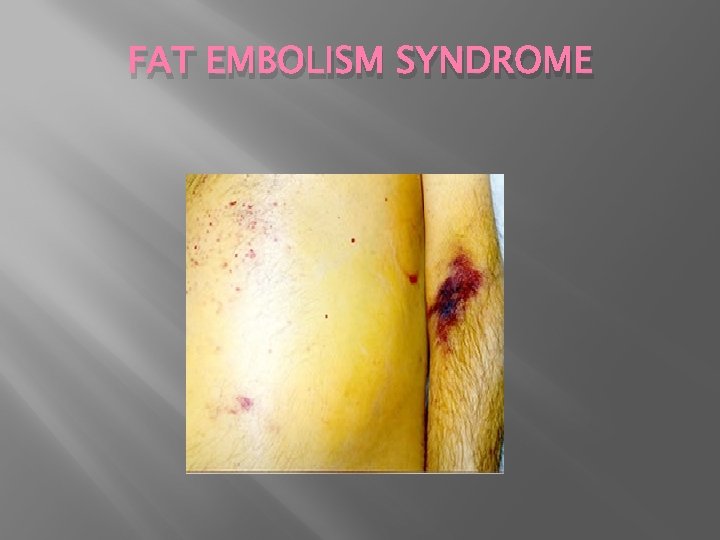
FAT EMBOLISM SYNDROME
FAT EMBOLISM SYNDROME � PULMONARY INSUFFICIENCY � NEUROLOGIC SYMPTOMS � ANEMIA � THROMBOCYTOPENIA
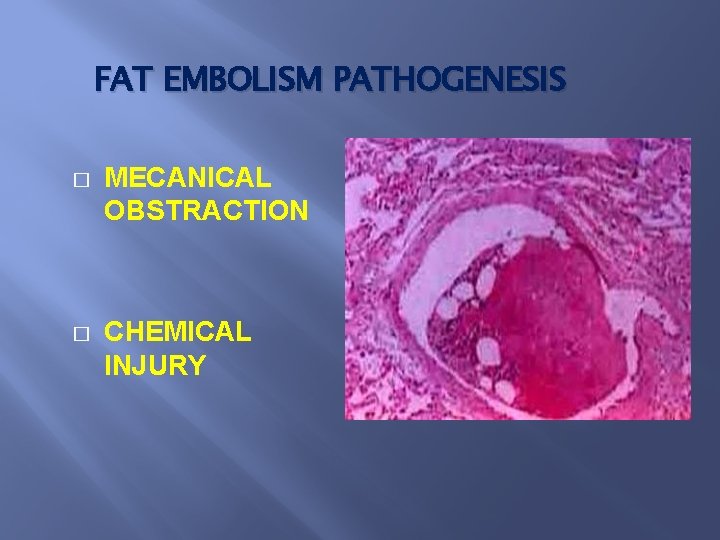
FAT EMBOLISM PATHOGENESIS � MECANICAL OBSTRACTION � CHEMICAL INJURY
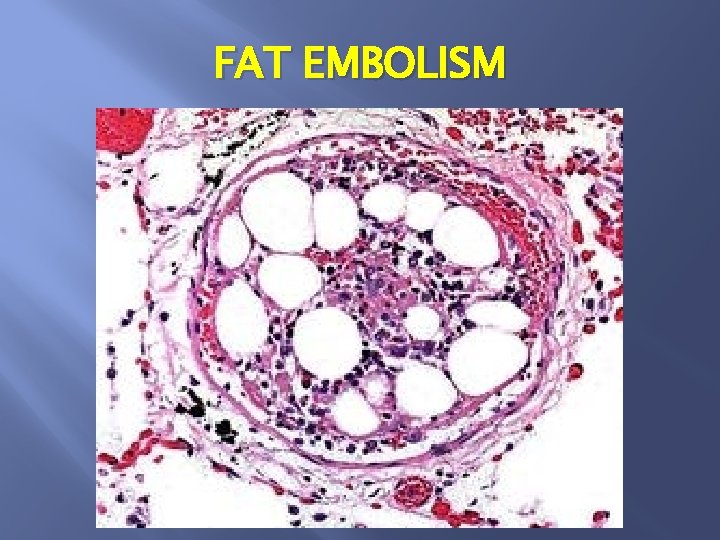
FAT EMBOLISM
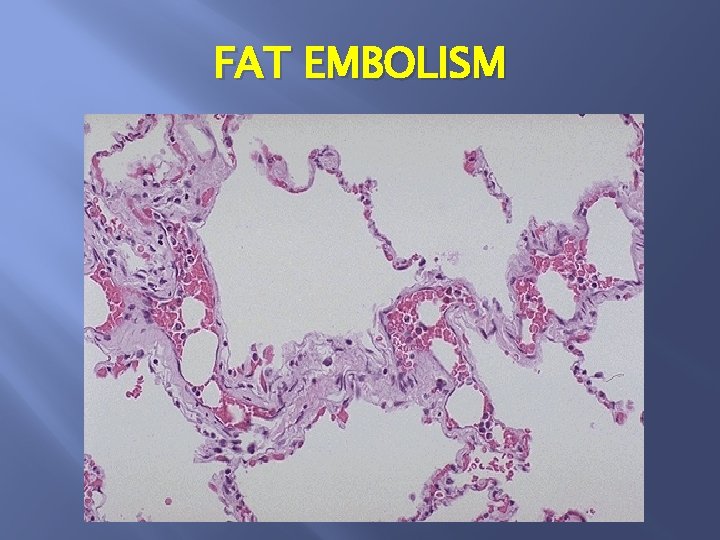
FAT EMBOLISM
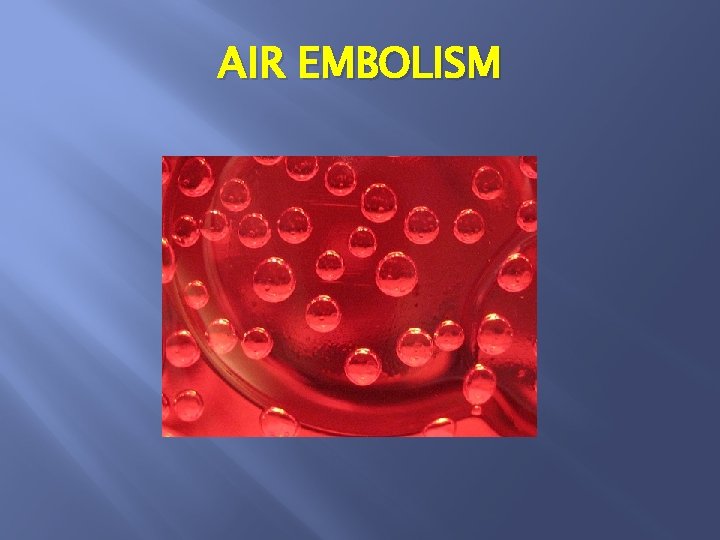
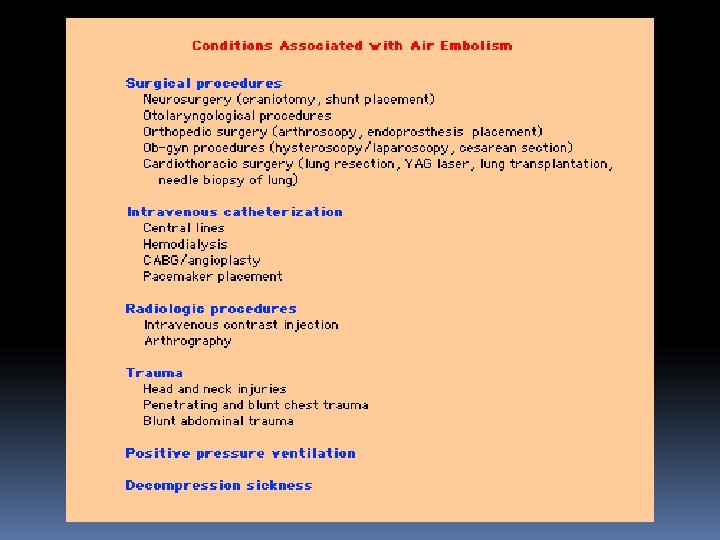
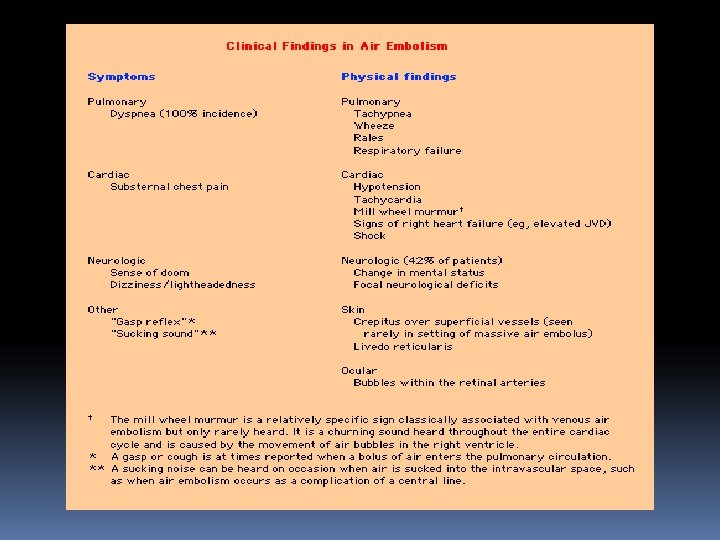
AIR EMBOLISM
DECOMPRESSION SIKNESS
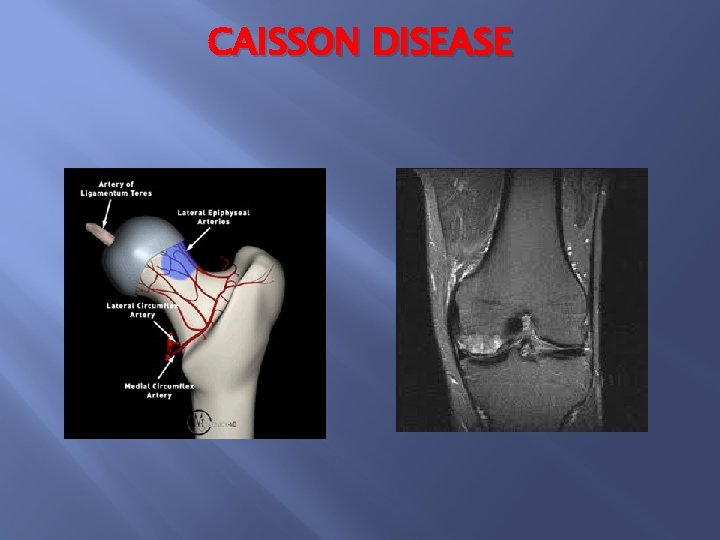
CAISSON DISEASE
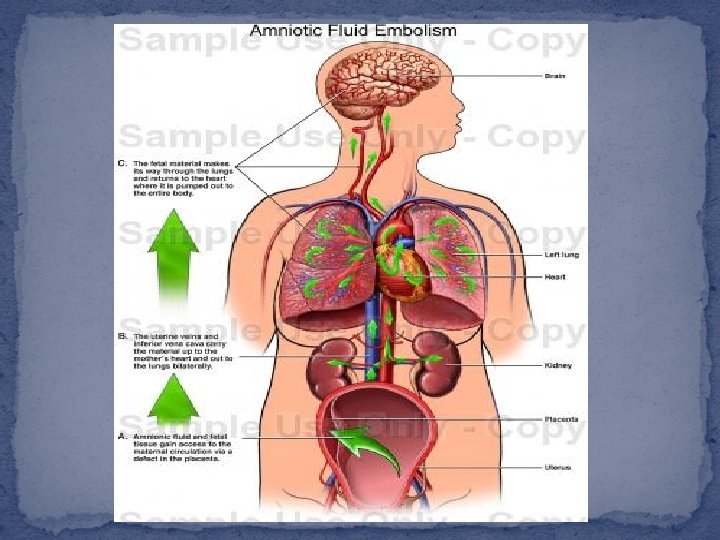
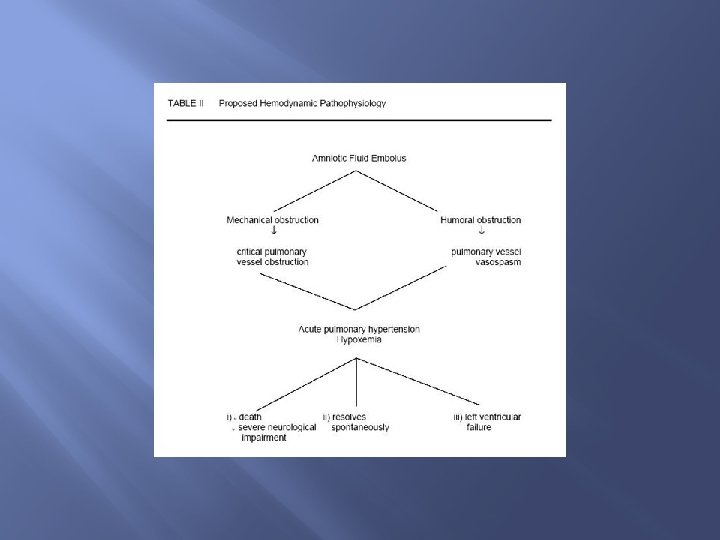
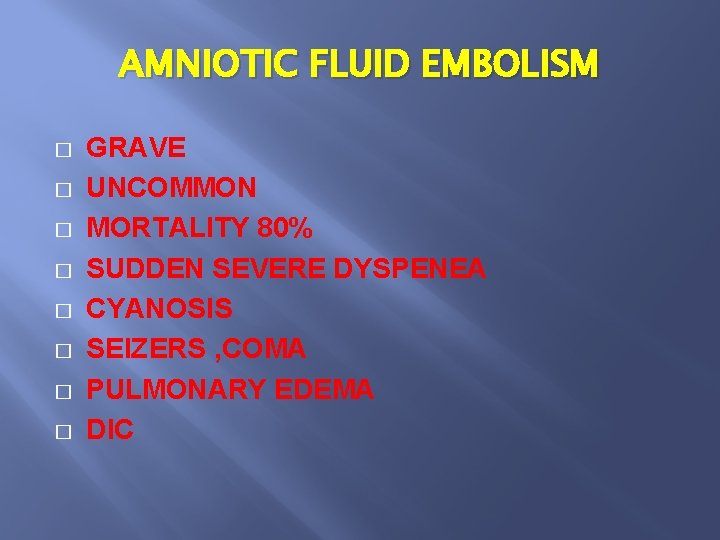
AMNIOTIC FLUID EMBOLISM � � � � GRAVE UNCOMMON MORTALITY 80% SUDDEN SEVERE DYSPENEA CYANOSIS SEIZERS , COMA PULMONARY EDEMA DIC
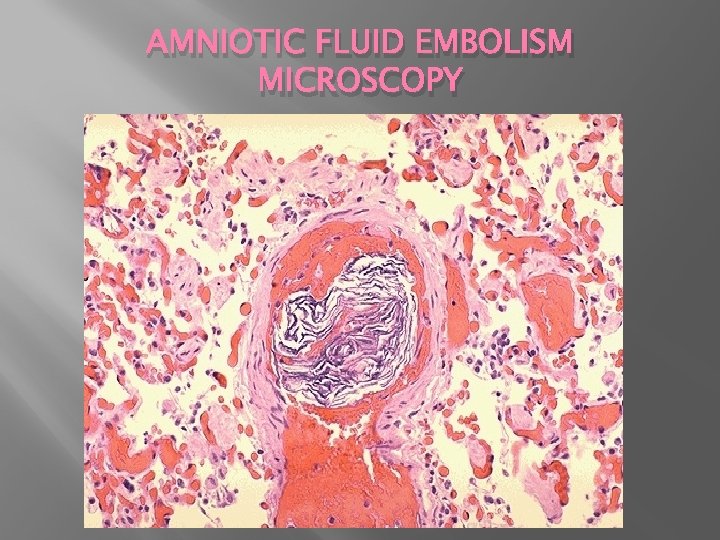
AMNIOTIC FLUID EMBOLISM MICROSCOPY
SHOCK CARDIOVASCULAR COLLAPSE
Systemic hypoperfusion duo to a reduction either in cardiac output or in the effective circulating blood volume
SHOCK CARDIOVASCULAR COLLAPSE SEVERE HEMORRHAGE EXTENSIVE TRAUMA OR BURNS LARGE MI MASSIVE PULMONARY EMBOLISM MICROBIAL SEPSIS � � �
TYPES OF SHOCK CARDIOGENIC SHOCK HYPOVOLEMIC SHOCK SEPTIC SHOCK NEUROGENIC SHOCK ANAPHYLACTIC SHOCK
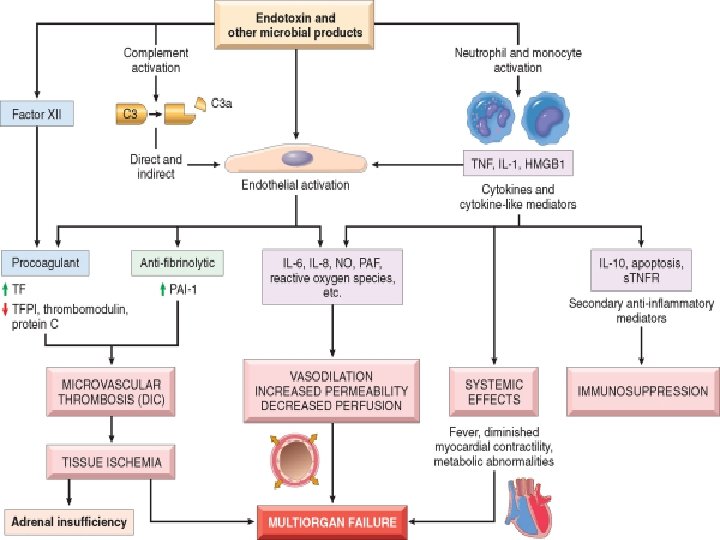
MAJOR FACTORS CONTRIBUTING TO SHOCK PATHOPHYSIOLOGY Inflammatory mediators Endothelial cell activation and injury Metabolic abnormality Immune suppression Organ dysfunction
INFLAMMATORY MEDIATORS Activation of inflammatory cells Toll-like receptors G-protein coupled receptors Production of : TNF , IL-1 , INFIL-12 , IL-18 , HMGB 1 , PAF Complement cascade Coagulation activation
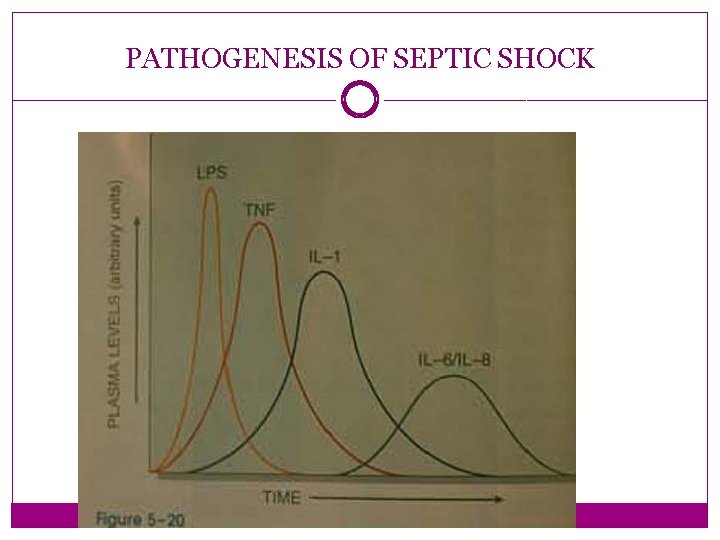
PATHOGENESIS OF SEPTIC SHOCK
PATHOGENESIS OF SEPTIC SHOCK � Endotoxin-producing gram negative bacilli � LPS � CD 14 reseptor (macrophage, monocyte, PMN, EC) � � TNF IL_1 � IL-6 , IL-8 � NO , PAF
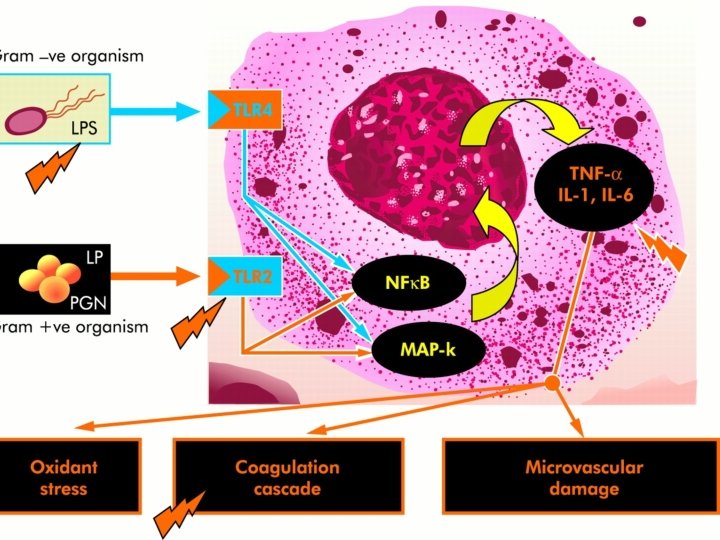
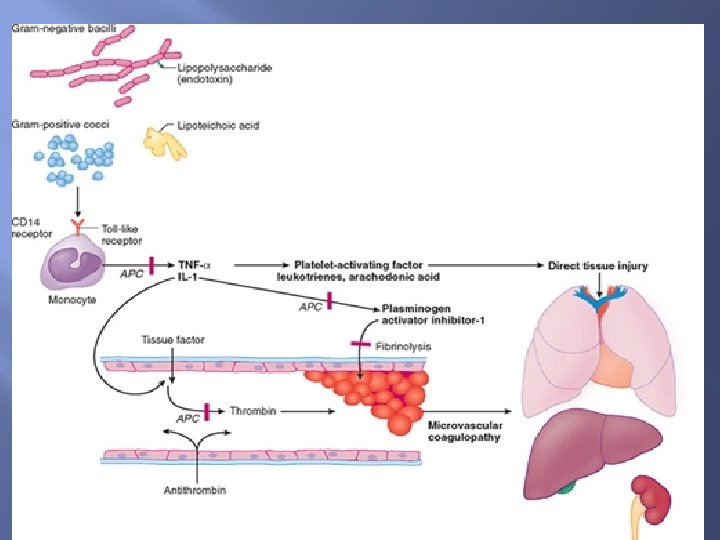
LOW QUANTITIES OF LPS LOCAL INFLAMMATION: � Monocytes, macrophage activation � Endothelial cell activation � Complement(C 3 a, C 5 a) activation
MODERATEQUANTITIES OF LPS SYSTEMIC EFFECTS: � Brain---fever � Liver---acute phase reaction � Bone---leucocytes
HIGH QUANTITIES OF LPS SEPTIC SHOCK: � Low cardiac output � Low peripheral resistance � Blood vessel injury , thrombosis, DIC
Stages of shock onprogressive stage � versible stage �
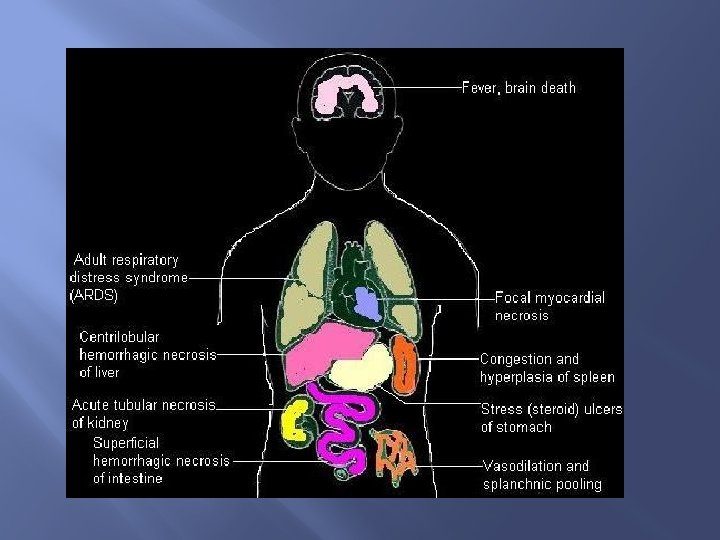
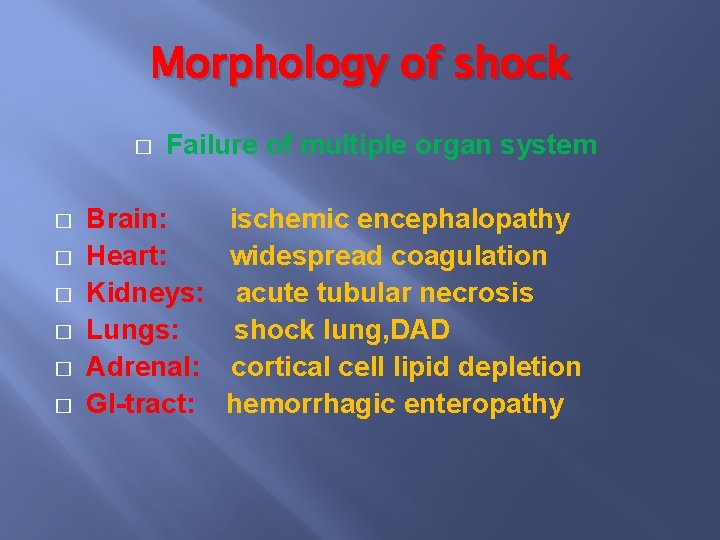
Morphology of shock � � � � Failure of multiple organ system Brain: Heart: Kidneys: Lungs: Adrenal: GI-tract: ischemic encephalopathy widespread coagulation acute tubular necrosis shock lung, DAD cortical cell lipid depletion hemorrhagic enteropathy

- Slides: 153