Hemiplegic Gait Contents Hemiplegic gait Spatio temporal characters


- Slides: 23
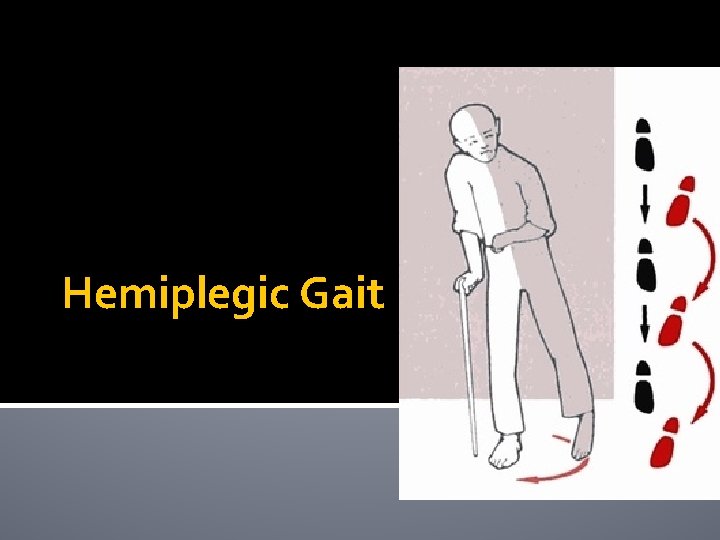
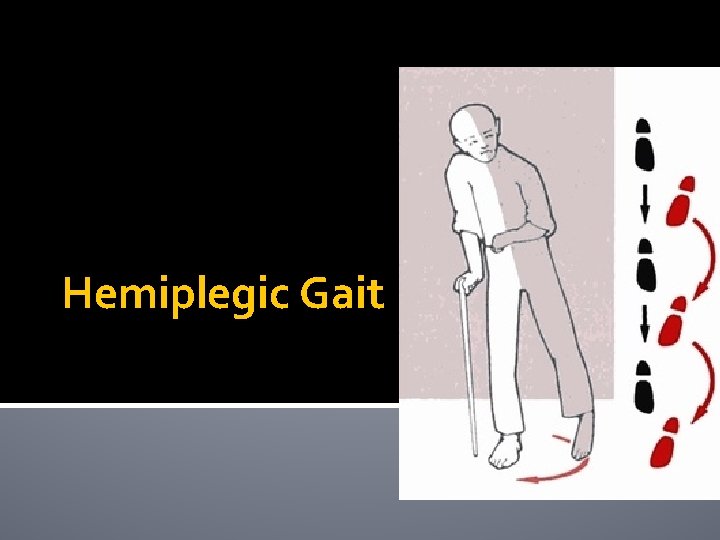
Hemiplegic Gait
Contents �Hemiplegic gait �Spatio temporal characters and considerations �Gait deviations �Gait examination �Intervention
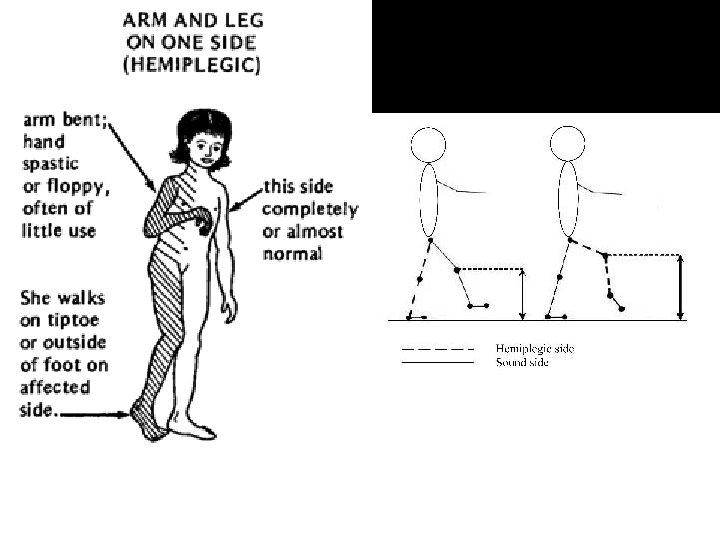
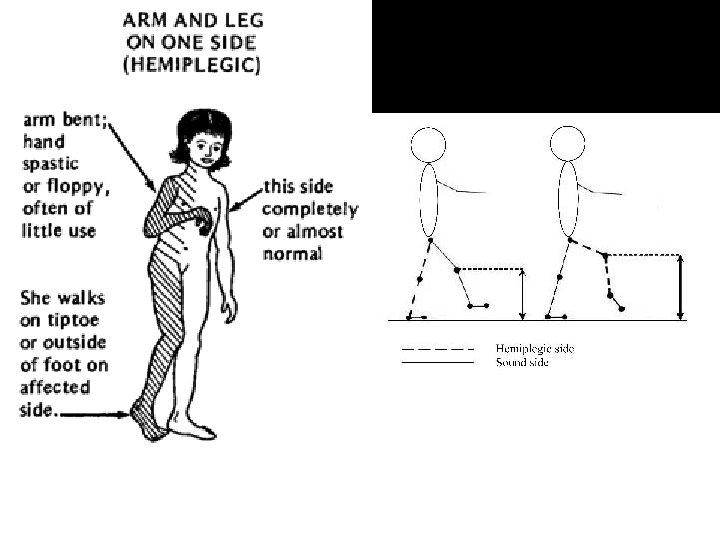
Hemiplegic gait �Slow uncoordinated gait movement. �Seen in case of CVA mainly ACA involvement. �Each patient presents with their own typical kind of gait pattern depending on the extent of injury and impairments.
Spatio-temporal characters � slow walking speed � Decrease in stride length and gait cycle duration � Inability to shift weight to paretic side in stance , � Inability to advance paretic limb ahead. � Difficulty with single limb stance. � Assymetric steps � Paretic limb has shorter step length and stance time and more swing time. � Degree of assymetry is inversely proportional to degree of motor recovery.
�Decrease in dorsiflexion & knee flexion �Increase length of limb �Increase circumduction to clear the ground with foot drag
�Decrease hip extension leads to Shorter stride length and gait velocity. �Presence of excessive downward rotation of pelvis on hemiparetic side due to gluetius medius weakness
�Trunk forward flexed to maintain COM under BOS �Leading to knee hyperextension. �Lateral weight shift of trunk for clearing the foot off the ground. �Pushers syndrome / Ipsilateral pushing.

�Video 1, 2.
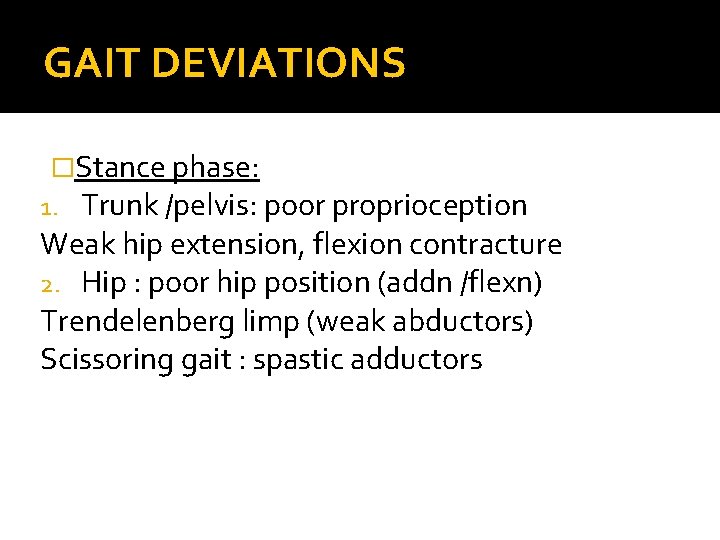
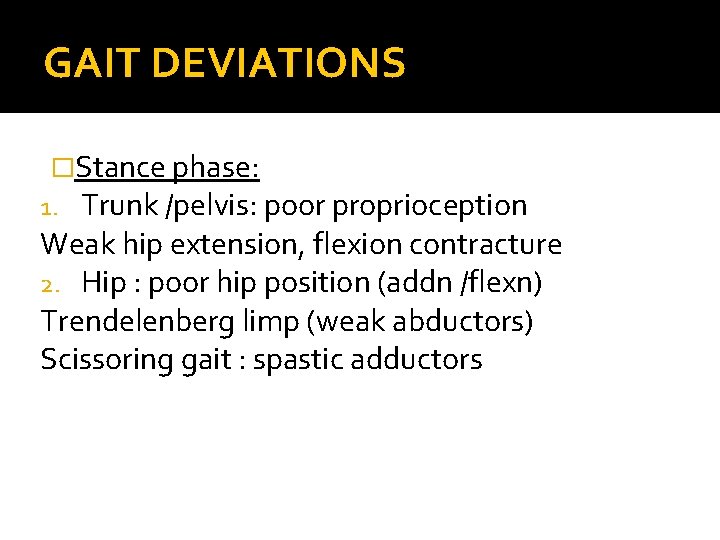
GAIT DEVIATIONS �Stance phase: 1. Trunk /pelvis: poor proprioception Weak hip extension, flexion contracture 2. Hip : poor hip position (addn /flexn) Trendelenberg limp (weak abductors) Scissoring gait : spastic adductors
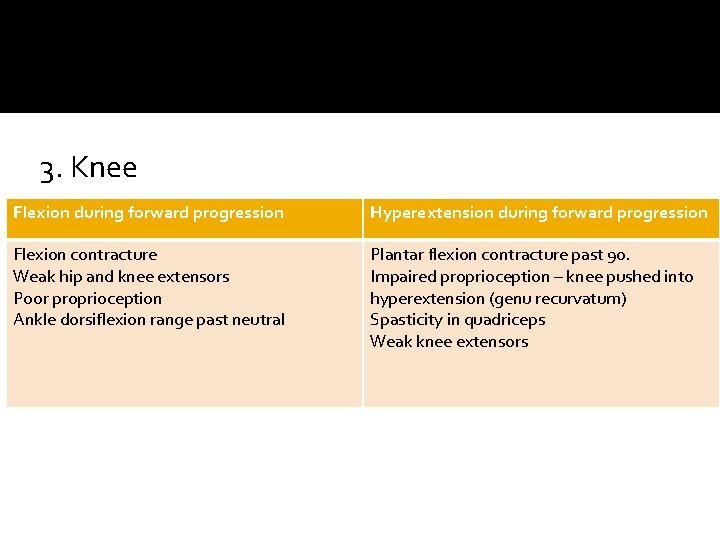
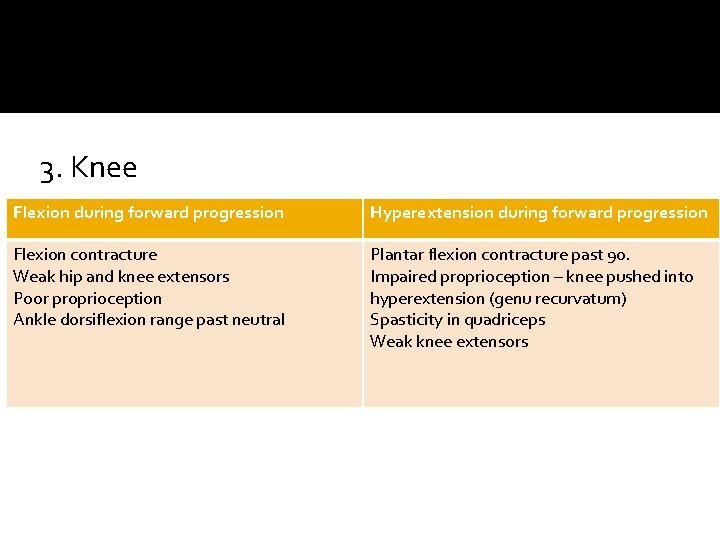
3. Knee Flexion during forward progression Hyperextension during forward progression Flexion contracture Weak hip and knee extensors Poor proprioception Ankle dorsiflexion range past neutral Plantar flexion contracture past 90. Impaired proprioception – knee pushed into hyperextension (genu recurvatum) Spasticity in quadriceps Weak knee extensors
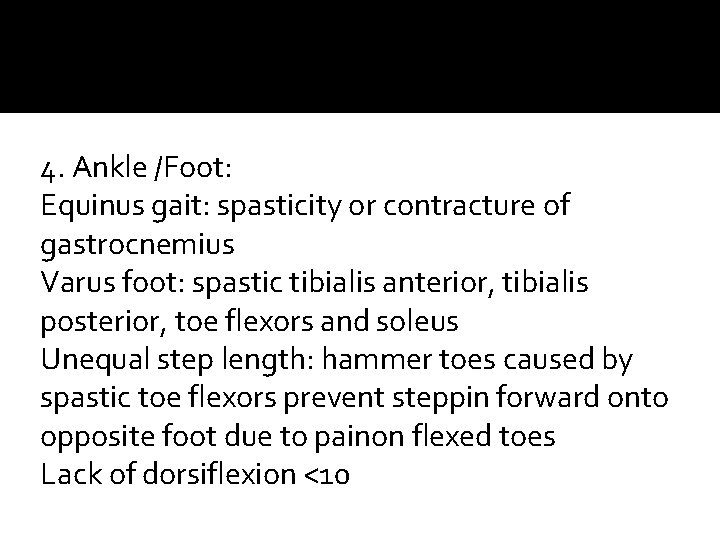
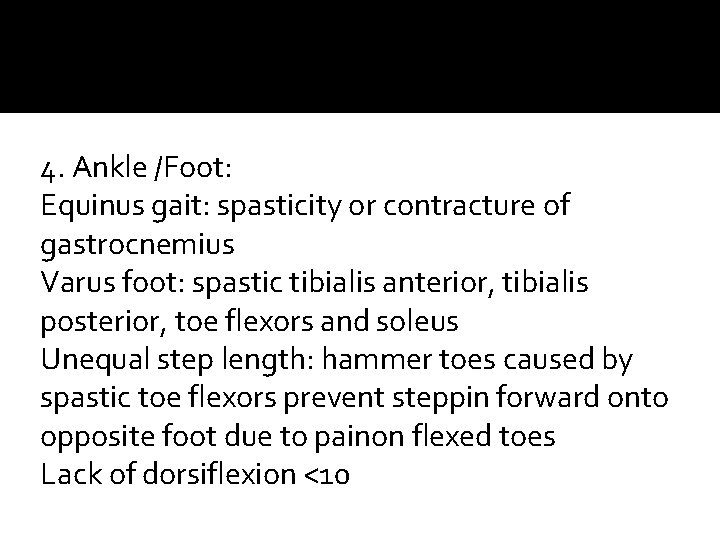
4. Ankle /Foot: Equinus gait: spasticity or contracture of gastrocnemius Varus foot: spastic tibialis anterior, tibialis posterior, toe flexors and soleus Unequal step length: hammer toes caused by spastic toe flexors prevent steppin forward onto opposite foot due to painon flexed toes Lack of dorsiflexion <10
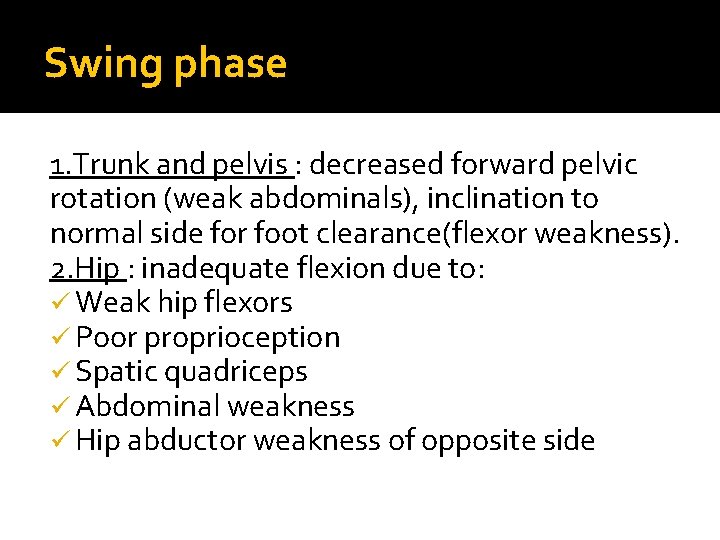
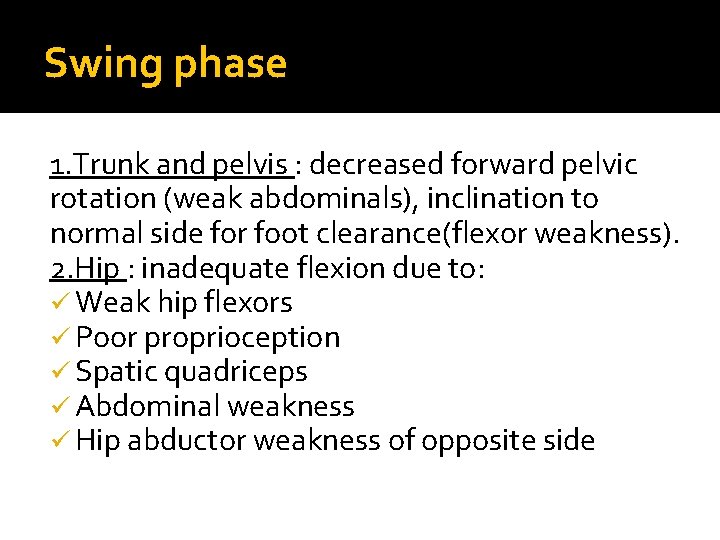
Swing phase 1. Trunk and pelvis : decreased forward pelvic rotation (weak abdominals), inclination to normal side for foot clearance(flexor weakness). 2. Hip : inadequate flexion due to: ü Weak hip flexors ü Poor proprioception ü Spatic quadriceps ü Abdominal weakness ü Hip abductor weakness of opposite side
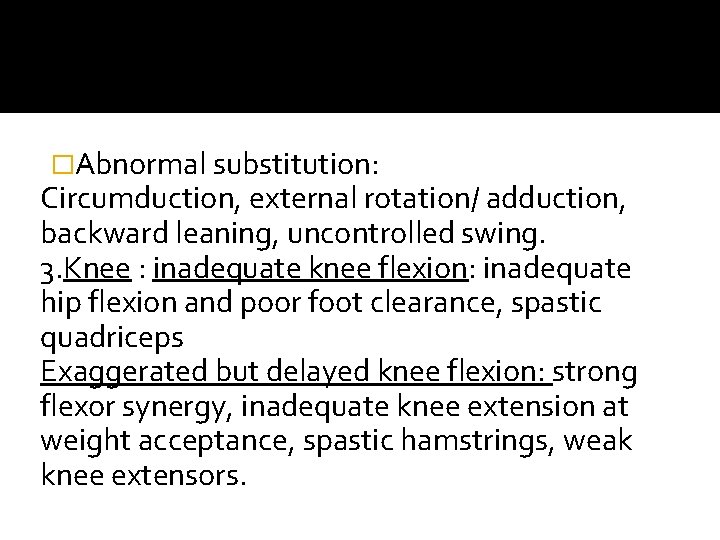
�Abnormal substitution: Circumduction, external rotation/ adduction, backward leaning, uncontrolled swing. 3. Knee : inadequate knee flexion: inadequate hip flexion and poor foot clearance, spastic quadriceps Exaggerated but delayed knee flexion: strong flexor synergy, inadequate knee extension at weight acceptance, spastic hamstrings, weak knee extensors.
4. Ankle/foot: equinus or equinovarus �Plantarflexor spasticity or contracture , weak dorsiflexors, toe drag during mid swing. �Varus: spastic tibialis anterior, weak peroneus and toe extensors �Equinovarus: spasticity of tibialis posterior and gastronemius.
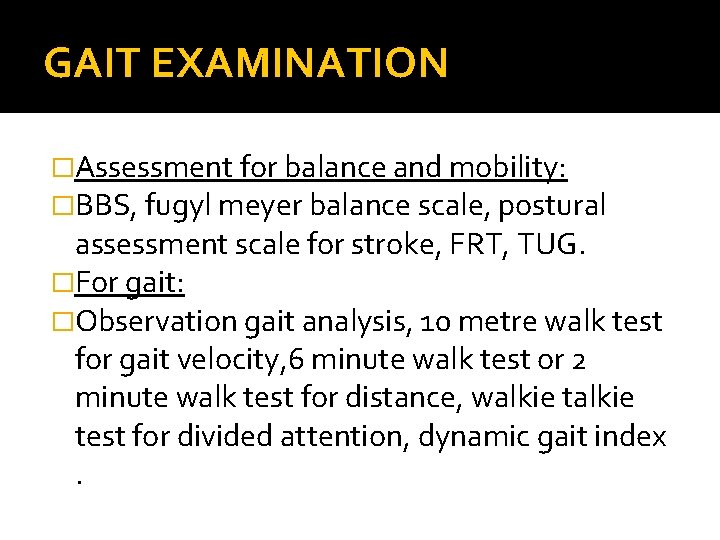
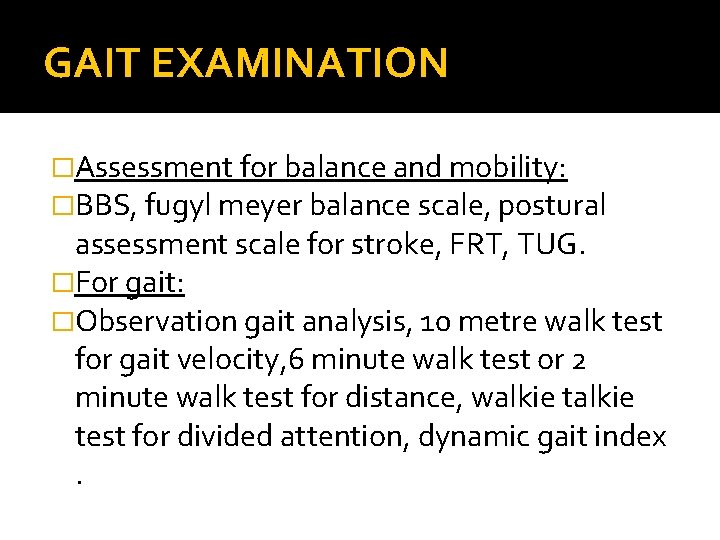
GAIT EXAMINATION �Assessment for balance and mobility: �BBS, fugyl meyer balance scale, postural assessment scale for stroke, FRT, TUG. �For gait: �Observation gait analysis, 10 metre walk test for gait velocity, 6 minute walk test or 2 minute walk test for distance, walkie test for divided attention, dynamic gait index.
GAIT TRAINING INTERVENTION �The recovery phase for the impairments following stroke is from 6 weeks to 3 months and slowly progressive till a year. �Strategies to improve impairments related to ambulation : NDT , ROODS APPROACH, PNF etc
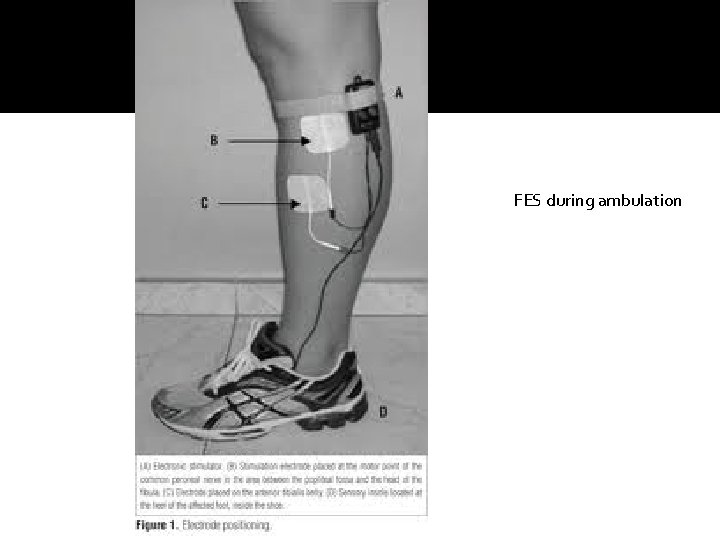
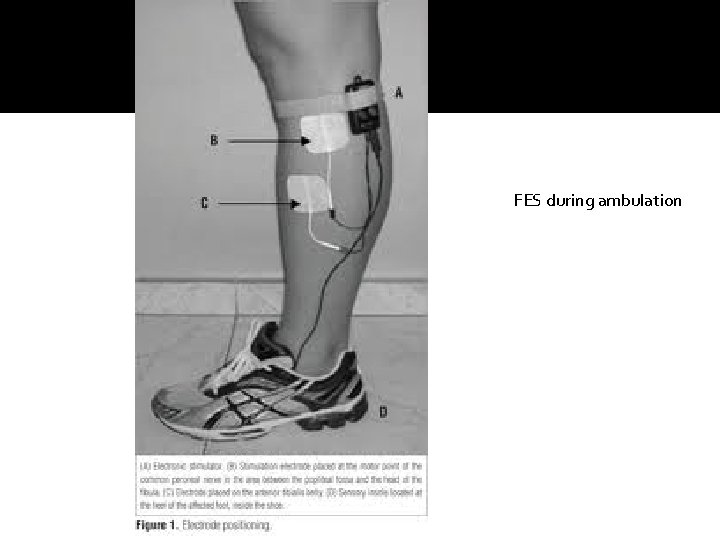
FES during ambulation
Strategies to improve locomotion �Body weight support treadmill training. �Central pattern generators �Stimulate automatic walking using intensive task oriented training. �Progression : from BWSTT reduce the support to no support to increasing speed over the treadmill to final over ground walking.

� Gait training aims at improving the quality of walking and improving the mechanics. � In certain cases assistive devices like walker canes can be given but prolonged use leads to forward lean and induces asymmetry over the unaffected side. � Encourage the patient to take even steps. � Provide visual or audio cues � Progress based on the improvement. � Gait training can be accompanied by FES /NMES to dorsiflexors to prevent foot drop. � Orthotics : AFO, KFO, HKAFO � Wheelchair prescription in severe cases.
Summarize Gait pattern presentation. Spatio temporal characters Gait deviations Gait examination intervention
References �Susan o sullivan. Physical medicine and rehabilitation. Fifth edition. 2010, jaypee publications. �Gary L Smidt. Gait in rehabilitation. �Wolley S. Characteristics of Gait in Hemiplegia. Top Stroke Rehabil 2001; 7(4): 1– 18.