Hematopoiesis Lab 1 What is Hematopoiesis Hematopoiesis is
Hematopoiesis Lab 1
What is Hematopoiesis? • Hematopoiesis is the production of all of the cellular components of blood and blood plasma. It occurs within the hematopoietic system, which includes organs and tissues such as the bone marrow, liver, and spleen.
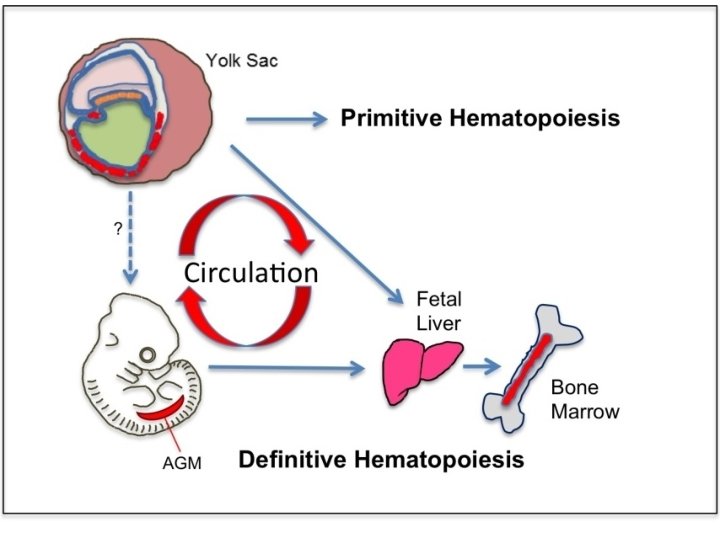
Embryonic Hematopoiesis • Hepatic haematopoiesis is a feature of the embryonic and fetal liver of mammals, including humans. The yolk sac is the initial site of haematopoiesis from primitive progenitor cells. Colonization of the liver by definitive erythroidmyeloid progenitor cells begins at about 6 weeks. • by the 12 th week the liver is the main site of haematopoiesis, having superseded the yolk sac. Hepatic haematopoietic activity begins to subside in the fifth month of gestation, when the bone marrow becomes haematopoietic, and has normally ceased within a few weeks after birth.
• After delivery approximately all bone marrow of infants are Red bone marrow. It is the place where new blood cells are produced. • There are two types of bone marrow: red marrow (also known as myeloid tissue) and yellow marrow. Red blood cells, platelets and most white blood cells arise in red marrow; some white blood cells develop in yellow marrow. The color of yellow marrow is due to the much higher number of fat cells. • Both types of bone marrow contain numerous blood vessels and capillaries.
• With age, more and more of it is converted to the yellow type. • Red marrow is found mainly in the flat bones such as hip bone, breast bone, skull, ribs, vertebrae and shoulder blades, and in the cancellous ("spongy") material at the proximal ends of the long bones femur and humerus. • In cases of severe blood loss, the body can convert yellow marrow back to red marrow in order to increase blood cell production.
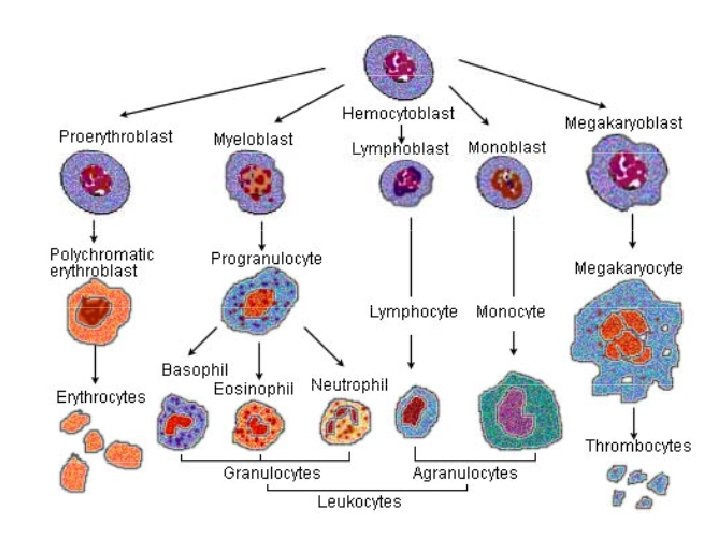
What cells are formed through Hematopoiesis? • Red blood cells (erythrocytes): These transport oxygen and hemoglobin throughout the body. • White blood cells (leukocytes): These support the immune system. There are several different types of white blood cells: 1. Lymphocytes: Including T cells and B cells, which help fight some viruses and tumors. 2. Neutrophils: These help fight bacterial and fungal infections. 3. Eosinophils: These play a role in the inflammatory response, and help fight some parasites. 4. Basophils: These release the histamines necessary for the inflammatory response. 5. Macrophages: These engulf and digest debris, including bacteria. • Platelets (thrombocytes): These help the blood to clot.
The process of Hematopoiesis • Each type of blood cell follows a slightly different path of hematopoiesis. All begin as stem cells called multipotent hematopoietic stem cells (HSC). From there, hematopoiesis follows two distinct pathways. • Trilineage hematopoiesis refers to the production of three types of blood cells: platelets, red blood cells, and white blood cells. Each of these cells begins with the transformation of HSC into cells called common myeloid progenitors (CMP). • After that, the process varies slightly. At each stage of the process, the precursor cells become more organized.

Red blood cells and platelets • Red blood cells: CMP cells activated by erythropoietin change five times before finally becoming red blood cells, also known as erythrocytes. • Platelets: CMP cells activated by thrombopoietin transform into megakaryocyte before becoming platelets.
White blood cells • There are several types of white blood cells, each following an individual path during hematopoiesis activated by colony-stimulating factors. All white blood cells initially transform from CMP cells into to myeoblasts. • T cells and B cells To produce lymphocytes, MHCs transform into cells called common lymphoid progenitors, which then become lymphoblasts. Lymphoblasts differentiate into infection-fighting T cells and B cells. Some B cells differentiate into plasma cells after exposure to infection.
- Slides: 11