hellomynameis Dr Paul Morgan Consultant Intensivist University Hospital







- Slides: 25

#hellomynameis Dr. Paul Morgan Consultant Intensivist University Hospital of Wales Cardiff
DNACPR, Death and Dying in Critical Care Dr. Paul Morgan Consultant Intensivist University Hospital of Wales Cardiff. Chair, Welsh Intensive Care Society

The Facts • Mortality rate in “average” critical care unit is approx 22% • Hospital mortality following critical care admission is approx. 30%
Destined to die • We all are……. • Patients who – despite all therapies – continue to deteriorate • Patients who, after a period of some improvement, reach a plateau with continuing organ failures • Patients with catastrophic brain injuries

All-Wales DNACPR Policy • Draft policy published May 2014 • No Intensivists on the Senior Steering Group…. • Introduces concept of NAAD – Natural, anticipated and accepted death.
However… • No discussion on CPR outcome statistics • Potential confusion between this policy, GMC Good Medical Practice and BMA/RCN/RCUK Joint statement 2007

And then…. The Queen on the application of David Tracey (personally and on behalf of the estate of Janet Tracey (deceased)) Appellant – and – Cambridge University Hospitals NHS Foundation Trust 1 st Respondent – and – Secretary of State for Health 2 nd Respondent – and – Equality and Human Rights Commission 1 st Intervener – and – The Resuscitation Council (UK) 2 nd Intervener
What happened? • Case revolved around medical decision to write a DNACPR order while patient was in the ICU. • Doctors claimed they had consulted the patient, who consented by a nod of her head.
European Convention on Human Rights • Case hinged around Article 8: Article 8 Right to respect for private and family life 1. Everyone has the right to respect for his private and family life, his home and his correspondence. 2. There shall be no interference by a public authority with the exercise of this right except such as is in accordance with the law and is necessary in a democratic society in the interests of national security, public safety or the economic well-being of the country, for the prevention of disorder or crime, for the protection of health or morals, or for the protection of the rights and freedoms of others.
Judgement Day • 17 th June 2014 • http: //www. judiciary. gov. uk/wpcontent/uploads/2014/06/traceyapproved. pdf
Was Article 8 engaged? • Disagreement between legal counsels for Cambridge University Hospitals NHSFT (YES) and Secretary of State for Health (NO). • Judge decided YES • “A decision as to how to pass the closing days and moments of one’s life and how one manages one’s death touches in the most immediate and obvious way a patient’s personal autonomy, integrity, dignity and quality of life. If there were any doubt as to that, it has been settled by the decision in Pretty”.
2007 Joint Statement • “Some health professionals do not find it easy to discuss CPR with their patients, but this must not prevent discussion, either to inform patients of a decision or involve patients in the decision-making process, where appropriate. ”
The case in context • Family objected to imposition of 1 st DNACPR without discussion, stated that patient would object to such an order. • GMC End of Life care guidance describes in Para 132 -142 how to make decisions about whether to resuscitate or not.
Later… • Initial DNACPR rescinded after intervention of family • Patient refused to discuss end-of-life care with hospital staff • Later, patient’s condition deteriorated • Second DNACPR written after discussion with family • Patient died a few days later
More on GMC Guidance on Treatment and care towards the end of life • Para 143 covers recording and communicating DNACPR decisions • “Any discussions with a patient, or with those close to them, about whether to attempt CPR, and any decisions made, should be documented in the patient’s record or advance care plan. If a DNACPR decision is made and there has been no discussion with the patient because they indicated a wish to avoid it, or because it was your considered view that discussion with the patient was not appropriate, you should note this in the patient’s records”

If you didn’t document it… • From the judgement: – The judge also accepted at para 112(iii) that Dr L****** believed that he had “conveyed the resuscitation issue including the use of the DNACPR notice to Alison who understood and agreed with it”. The judge then said: – “ 115 There is nothing in the medical/nursing records which suggests any agreement to DNACPR by Mrs Tracey. The tenor of entries prior to 4 March 2011 indicate that Mrs Tracey either did not agree or requested that any such discussion take place in the presence of her husband or daughters. If Dr L****** had such a conversation, it would have been of importance to note the same both on the DNACPR Notice and in the medical records. I am unable to accept that the absence of such a note is a result of no more than poor record keeping.
Errr…. . • Have doctors steered away from DNACPR discussions on the grounds that they feel it would cause the patient undue stress and harm? • Probably! • This judgement means that this defence is no longer valid • If you exclude the patient from discussion, must be clear as to why • “Distress” is not a good enough reason – must put patient at risk of harm

Resuscitation Council Statement In such circumstances the RC (UK) emphasises the importance of clinicians documenting clearly their reasons, should they decide not to discuss a DNACPR decision with a patient or explain it to them. The judgement recommends also that the court should be very slow to find that such decisions, if conscientiously taken, violate a patient’s rights under Article 8 of the European Convention.
More from the GMC When there is a possibility that CPR could restore the person’s circulation and breathing for a duration and/or to a quality of life that the patient would wish to have, decisions about CPR must be made in careful consideration of the person’s best-interests and on the basis of shared decision-making.
Vitally important • The judgement has confirmed that if a clinician considers that CPR will not work the patient cannot require him/her to provide CPR. It states that this does not, however, mean that the patient is not entitled to know that the clinical decision has been taken.
More from the Resuscitation Council (UK) • The RC (UK) emphasises the importance of clinicians considering anticipatory decisions about CPR as an integral part of delivering high-quality and compassionate end-of-life care for their patients. Whenever possible such consideration should form part of advance care planning with people who are identified as approaching the end of their life, so that carefully considered decisions can be reached with full involvement of the patient and (where appropriate) those close to them. This will reduce the need for decisions being made in haste when a clinical crisis occurs, often reducing the patient’s ability to participate fully in shared decision-making
What does this all mean in Critical Care? • Patients outside Critical Care remain at risk of inappropriate application of CPR due to failure to discuss end-of-life care prior to a crisis. • Concern this judgement may lead to even more failures to make DNACPR decisions • Instituting a DNACPR decision needs to be discussed with the patient if possible • Discuss the decision with the patient’s family in cases where patient cannot be involved (follow MCA hierarchy).
• It does not mean you have to provide any treatment considered to be ineffective or inappropriate, including CPR just because a patient or relative demands it. • GMC guidance on consent covers conflict resolution, but having a decision taken by a multi-disciplinary team or by having a second opinion will help greatly. • It may well be that Critical Care consultants are asked to give second opinions on ward patients even more frequently than we are now.
Summary • In the context of Critical Care, if you were making DNACPR decisions properly before, nothing changes – as long as you document it properly! • Conflict resolution may be needed more often – but not a lot • No change to need to treat or resuscitate inappropriately

Thank you for listening! Any questions?
 Nous hospital consultant
Nous hospital consultant Nous hospital consultant
Nous hospital consultant Tc vc
Tc vc Morgan state housing portal
Morgan state housing portal Site:slidetodoc.com
Site:slidetodoc.com University hospital of pisa
University hospital of pisa Bezmalem
Bezmalem Benha university hospital
Benha university hospital Kyorin university hospital
Kyorin university hospital University hospital tuebingen
University hospital tuebingen University hospital of pisa
University hospital of pisa Patras university hospital
Patras university hospital Pisa university hospital
Pisa university hospital Differential diagnosis for atopic dermatitis
Differential diagnosis for atopic dermatitis Portsmouth university hospital trust values
Portsmouth university hospital trust values Kyung hee university hospital at gangdong
Kyung hee university hospital at gangdong Kaohsiung medical university hospital
Kaohsiung medical university hospital University of iowa hospitals and clinics
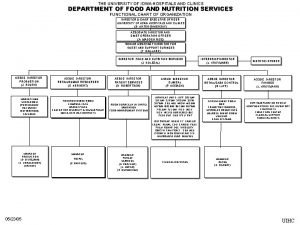
University of iowa hospitals and clinics King saud university hospital nurse salary
King saud university hospital nurse salary Modern data architecture consultants
Modern data architecture consultants Consultant mediu
Consultant mediu Claudia norman a marketing consultant
Claudia norman a marketing consultant Judith james educational consultant
Judith james educational consultant Behavioral genetics consultant
Behavioral genetics consultant Rcem consultant sign off
Rcem consultant sign off Open source consultant
Open source consultant