Helicopter Emergency Medical Services Not Just For Trauma









- Slides: 30
Helicopter Emergency Medical Services… Not Just For Trauma Anymore Deb Funk, M. D. , FACEP, NREMT-P Medical Director, Life Net of NY Assistant Professor, Department of Emergency Medicine, Albany Medical College
Emergency Medical Services…not just a fast ride with lights and sirens anymore
Emergency Medical Technicians…not just ambulance drivers anymore
Today’s Reality… Ø The practice of medicine in many environments has changed v. Financial issues v. Staffing shortages Ø The organization of health care has changed v. Consolidation of services v. Creation of health care systems v. Fiscal responsibility Ø Mission profiles of hospitals, ground based EMS and air medical services have changed v. Team approach to provide health care to an individual in crisis
History of Air Medical Transport in the United States Ø 1 st reported air transport of a patient in 1915 v. French pilot evacuated a Serb in an unmodified fighter plane Ø Ø Ø Through progressive conflicts, airplane evacuation of injured/ill more prominent First medical use of helicopter in 1944 in Burma First large scale medical evacuation in Korea (Sikorsky with outboard stretchers) UH-1 H “Huey” central to medical care in Vietnam This approach reduced mortality and came to the attention of the American public
Civilian Adaptation Ø Early 1970’s federally funded pilot projects to study feasibility v. Tenuous economic viability v. Need to dedicate to medical configuration v. Need for integration into ground EMS systems Ø Civilian Law Enforcement/Fire Agencies developed aviation components v. Occasionally provided medical transport v. Some pursued dedicated air medical programs èMaryland State Police èLA County Fire Dept
Development in Civilian World Ø Hospital Based v. Most common v. Aircraft is leased from vendor or owned by hospital v. First in Denver 1972 Ø Second Generation in early 1980’s v. Increasing federal interest due to cost v. Role expanded from trauma to neonatal, OB, cardiac Ø Third Generation in mid-1980’s v. Focus on safety, and cost effectiveness
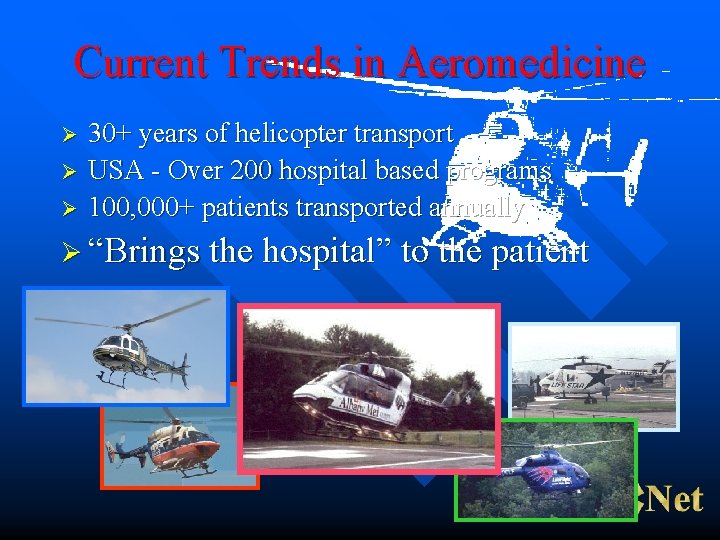
Current Trends in Aeromedicine Ø Ø Ø 30+ years of helicopter transport USA - Over 200 hospital based programs 100, 000+ patients transported annually Ø “Brings the hospital” to the patient

Review of Ground EMS Development Ø Ø Ground based EMS developed also as a result of wartime experiences Multiple models of system v. Private contractor v. FD based v. Private, for profit service v. Municipal third service Ø Multiple levels of provider-regionally dependent v. First Responders/Emergency Medical Technicians (BLS) v. Intermediate/Paramedic (ALS) v. Specialty Care Paramedic
Integration of Ground and Air EMS Ø Team approach Ø Education Ø Protocols Ø Quality Assurance
Indications for Air Transport Ø Time v. Decrease time to definitive care v. Decrease out of hospital time Ø Terrain v. Overcome environmental obstacles v. Overfly traffic gridlock Ø Talent v. Delivery of highly skilled care to patients prior to/during transport
Air Medical Triage Ø >1, 000 patients transported by helicopter since 1972 by nearly 200 programs Ø Roughly 30/70 split scene/interfacility Ø Triage of patients to receive air transport v. Intend for majority of seriously ill/injured patients get appropriate transport v. Assumes a certain over-triage rate
Practical Considerations: Method of Transport Ø Optimal time dictated by patient’s illness/injury Ø Distance, geography and traffic Ø Availability of definitive care at local hospitals Ø Carrier and personnel availability Ø Weather conditions Ø Cost

Considerations: Trauma Ø Disease of time: minutes make a difference Ø ACS/COT advocates that any seriously injured patient be primarily treated in a trauma center v. Air medical transport based upon local factors Ø Interfacility transport of seriously injured patient v. Use of helicopter based on time/terrain/talent
Considerations: Non-Trauma Ø Variety of medical/surgical conditions Ø Time/Terrain/Talent Ø May benefit from specialty team (OB/NICU/PICU) Ø Interfacility most common Ø Scene may be appropriate
Contraindications to Air Transport Ø Terminally ill with no correctable medical problems Ø Cardiac arrest without SROC Ø Patients likely to die enroute, if in a facility capable of resuscitation Ø Patients in active labor if delivery expected during transport Ø Patients prone to psychotic/violent behavior (without appropriate restraint)

Utilization Review Ø Prospective Screening v. Difficult based on limited info and time constraints Ø Retrospective Review v. Chart review of outcome, procedures performed, severity of illness, other subjective parameters Ø Follow Up v. Feedback to caller v. Revision of criteria as appropriate
Case 1 Ø Ø Ø Grandpa and Little Johnnie were involved in a high speed head on MVC 5 miles from Nowhere. Grandpa is on coumadin and has a tender, distended abdomen. His HR is 120 Johnnie is unconscious with an obvious skull fracture. His jaw is clenched. v 20 min drive to community hospital v 20 min flight to trauma center (60 min drive)

Case 1 Discussion Ø Ø Johnnie needs an airway and a pediatric neurosurgeon Determine quickest way to airway v HEMS vs community hospital v Never wait on scene if packaged Ø Definitive care at peds trauma center Ø Consideration for automatic standby PEDIATRIC MAJOR TRAUMA 1. Pulse greater than normal range for patient’s age 2. Systolic blood pressure below normal range 3. Respiratory status inadequate (central cyanosis, respiratory rate low for the child’s age, capillary refill time greater than two seconds) 4. Glasgow coma scale less than 14 5. penetrating injuries of the trunk, head, neck, chest, abdomen or groin. 6. two or more proximal long bone fractures 7. flail chest 8. combined system trauma that involves two or more body systems, injuries or major blunt trauma to the chest or abdomen 9. spinal cord injury or limb paralysis 10. amputation (except digits)
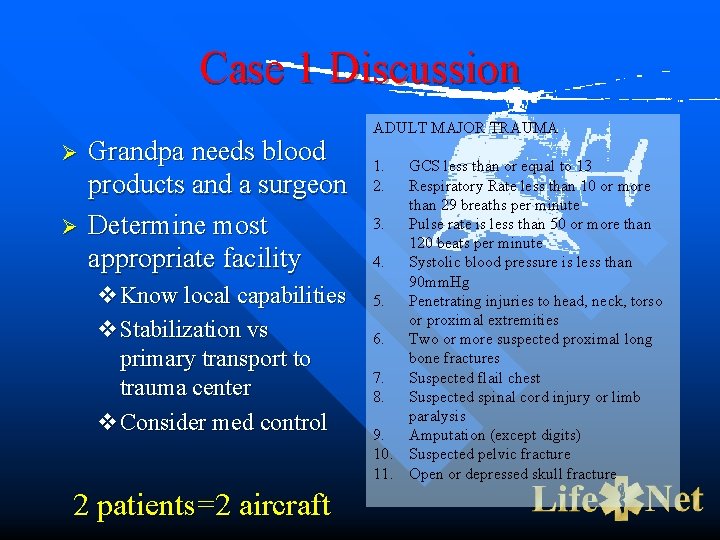
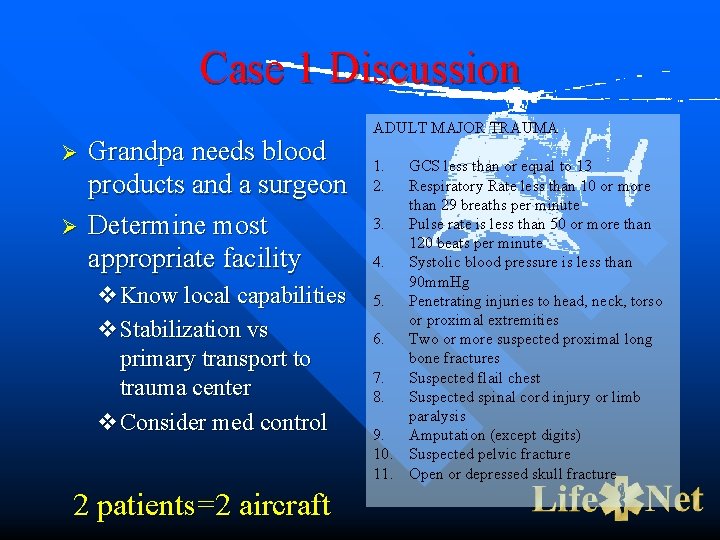
Case 1 Discussion Ø Ø Grandpa needs blood products and a surgeon Determine most appropriate facility v. Know local capabilities v. Stabilization vs primary transport to trauma center v. Consider med control 2 patients=2 aircraft ADULT MAJOR TRAUMA 1. GCS less than or equal to 13 2. Respiratory Rate less than 10 or more than 29 breaths per minute 3. Pulse rate is less than 50 or more than 120 beats per minute 4. Systolic blood pressure is less than 90 mm. Hg 5. Penetrating injuries to head, neck, torso or proximal extremities 6. Two or more suspected proximal long bone fractures 7. Suspected flail chest 8. Suspected spinal cord injury or limb paralysis 9. Amputation (except digits) 10. Suspected pelvic fracture 11. Open or depressed skull fracture

Case 2 Ø Jake narrowly escapes from his burning apartment but suffers 60% second degree burns. Ø Ø Ø 20 min drive to community hospital 20 min flight to trauma center 60 min flight to burn center
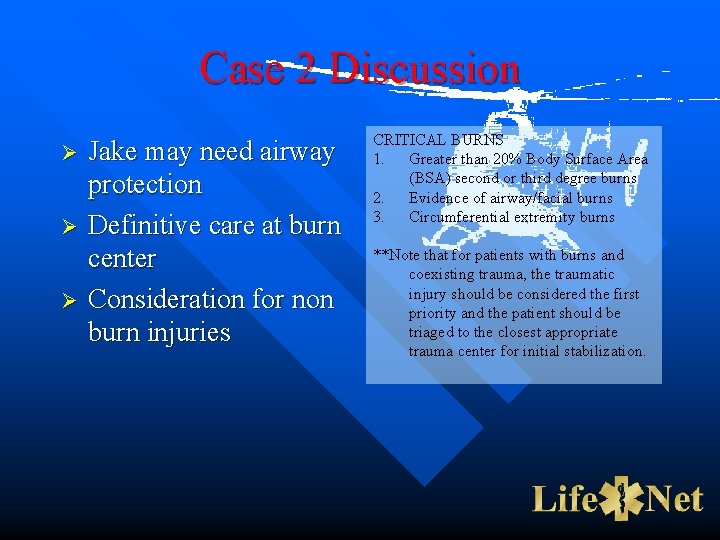
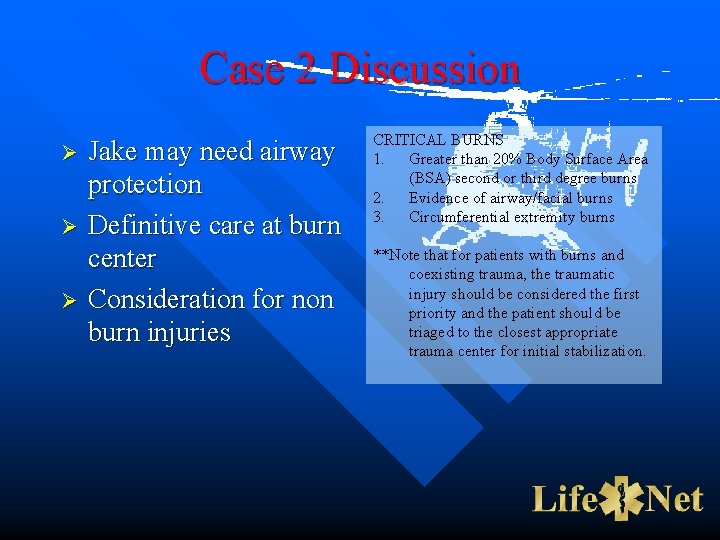
Case 2 Discussion Ø Ø Ø Jake may need airway protection Definitive care at burn center Consideration for non burn injuries CRITICAL BURNS 1. Greater than 20% Body Surface Area (BSA) second or third degree burns 2. Evidence of airway/facial burns 3. Circumferential extremity burns **Note that for patients with burns and coexisting trauma, the traumatic injury should be considered the first priority and the patient should be triaged to the closest appropriate trauma center for initial stabilization.
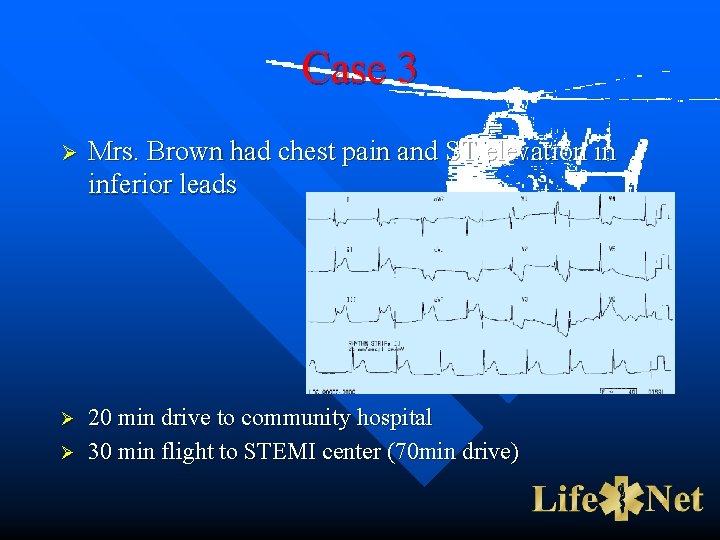
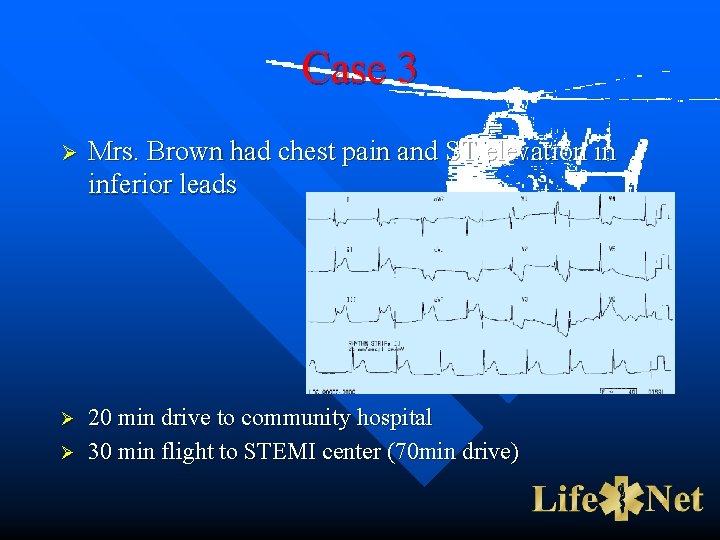
Case 3 Ø Mrs. Brown had chest pain and ST elevation in inferior leads Ø 20 min drive to community hospital 30 min flight to STEMI center (70 min drive) Ø
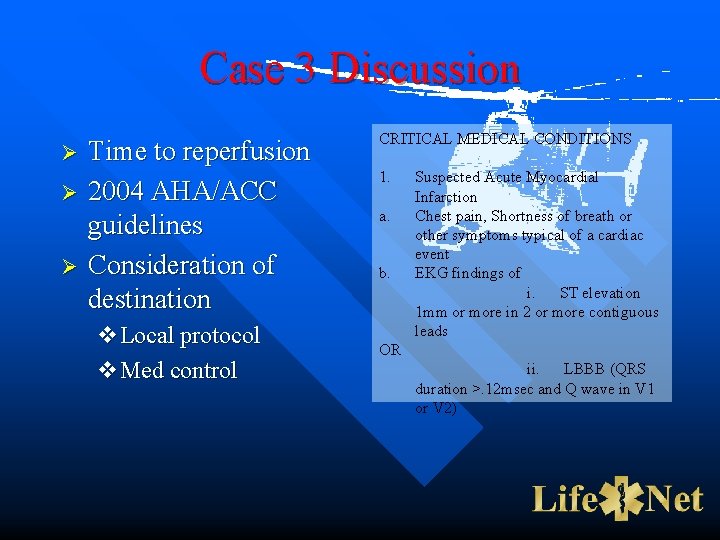
Case 3 Discussion Ø Ø Ø Time to reperfusion 2004 AHA/ACC guidelines Consideration of destination v. Local protocol v. Med control CRITICAL MEDICAL CONDITIONS 1. Suspected Acute Myocardial Infarction a. Chest pain, Shortness of breath or other symptoms typical of a cardiac event b. EKG findings of i. ST elevation 1 mm or more in 2 or more contiguous leads OR ii. LBBB (QRS duration >. 12 msec and Q wave in V 1 or V 2)
Case 4 Ø Mr. George has right arm and leg weakness with slurred speech. Last normal 30 min ago. Ø Ø 20 min drive to community hospital 30 min flight to Stroke Center (70 min drive)

Case 4 Discussion Ø Stroke is extremely time dependent v 3 hr window for IV TPA v 6 hr window for IA TPA v Endovascular intervention Ø Most appropriate destination v Patient factors v Timing v Med control CRITICAL MEDICAL CONDITIONS 1. Suspected acute stroke a. Positive Cincinnati Pre-Hospital Stroke Scale Total prehospital time (time from when the patient’s symptoms and/or signs first began to when the patient is expected to arrive at the Stroke Center) is less than two (2) hours.
NYS HEMS Utilization Criteria Ø Standard criteria described in Policy 05 -05 v. Who calls v. When to call v. When to cancel Ø Specific local differences acknowledged Ø Education tool in development

“Specific Local Differences” Ø HEMS must be integrated into current EMS and hospital system Ø Requires cooperative preplanning Ø Demands ongoing review

Summary Ø The practice of medicine evolves Ø Consolidation of specialty services continues Ø Considerations for air medical transport may be changing Ø Cooperative plans are imperative for a successful system

Questions?
 Emergency management of maxillofacial trauma
Emergency management of maxillofacial trauma Not too big not too small just right
Not too big not too small just right Who is present when juliet awakens
Who is present when juliet awakens Vocabulary workshop level d unit 1
Vocabulary workshop level d unit 1 Emergency medical responder first on scene
Emergency medical responder first on scene Red cross emergency medical responder
Red cross emergency medical responder Introduction to emergency medical care
Introduction to emergency medical care Chapter 31 assisting in a medical emergency
Chapter 31 assisting in a medical emergency Define medical emergency chapter 31
Define medical emergency chapter 31 Medical emergency student lectures
Medical emergency student lectures Emergency medical dispatch guidecards
Emergency medical dispatch guidecards Medicaid transportation texas logisticare
Medicaid transportation texas logisticare Introduction to emergency medical care
Introduction to emergency medical care Introduction to emergency medical care
Introduction to emergency medical care Emergency medical responder first on scene 10th edition
Emergency medical responder first on scene 10th edition Antecubitsl
Antecubitsl Emergency medical responder first on scene 11th edition
Emergency medical responder first on scene 11th edition Introduction to emergency medical care
Introduction to emergency medical care Helicopter weather forecast
Helicopter weather forecast Number of syllables in elephant
Number of syllables in elephant Rc helicopter governor
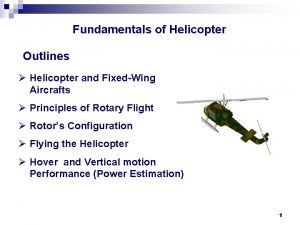
Rc helicopter governor How does a helicopter move forward
How does a helicopter move forward Helicopter short haul equipment
Helicopter short haul equipment Helicopter winching area marking
Helicopter winching area marking How does a helicopter move forward
How does a helicopter move forward Helicopter electrical system
Helicopter electrical system Tuna boat helicopter
Tuna boat helicopter Mast bumping helicopter
Mast bumping helicopter Tim madsen charlotte fox
Tim madsen charlotte fox Helicopter history timeline
Helicopter history timeline European helicopter safety team
European helicopter safety team