Helen Cockerill Drooling Diva Evelina London Childrens Hospital
- Slides: 16
Helen Cockerill Drooling Diva Evelina London Children’s Hospital Guy’s and St Thomas’ NHS Foundation Trust Saliva control: the idiot’s guide
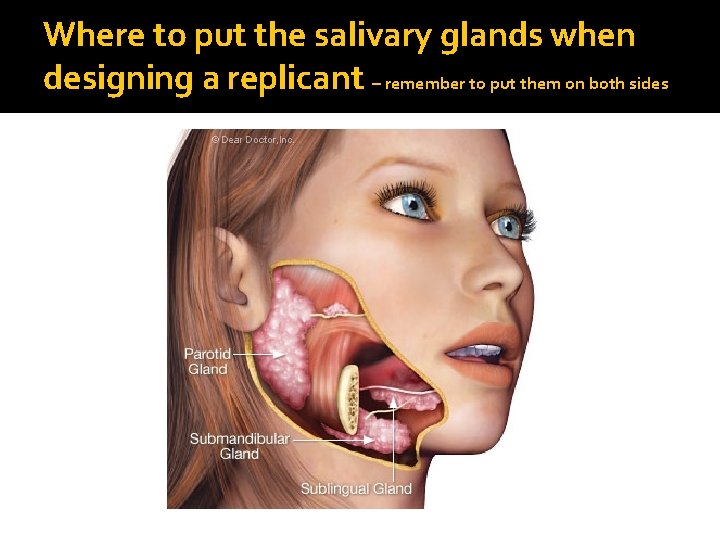
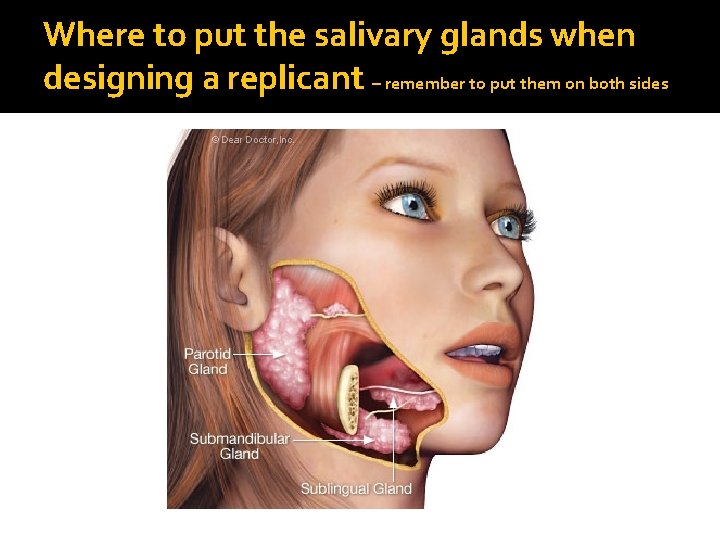
Where to put the salivary glands when designing a replicant – remember to put them on both sides
Good things about saliva – why we don’t want to dry it up completely Oral hygiene – protection against microrganisms and toxins Taste Bolus formation during chewing Enzymes start breakdown of carbohydrates Acid regulation Lubrication – speech and other things
Bad things about saliva �Needs a lot of swallowing av. 600 times per day in adults (350 when awake, 200 when eating, 50 in sleep) �Drooling in children with neurodisabilities Prevalence in CP 22% (Parkes et al. 2010) Oral motor disorders Infrequent/disordered swallowing Medication – hypersalivation: benzodiazepines e. g. Clobazam, Acetylcholine inhibitors e. g. Neostigmine, anti-psychotics e. g. Risperidone �Aspiration in children with neurodisabilities �Can be bacteria-laden associated with pooling and open mouth posture
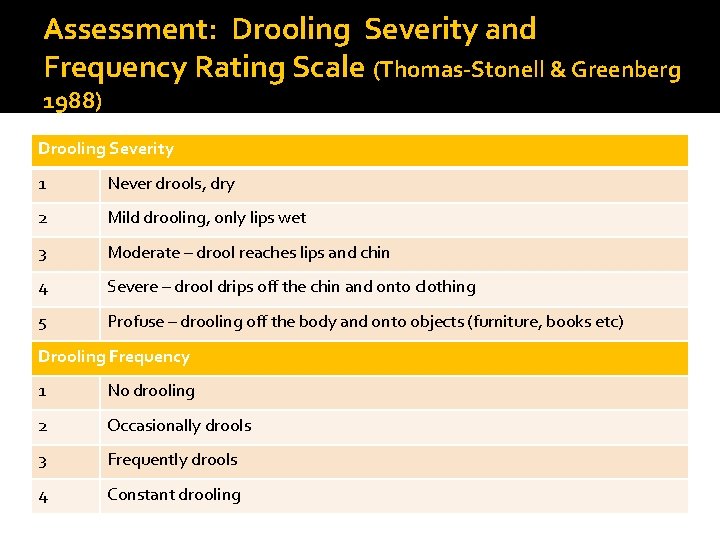
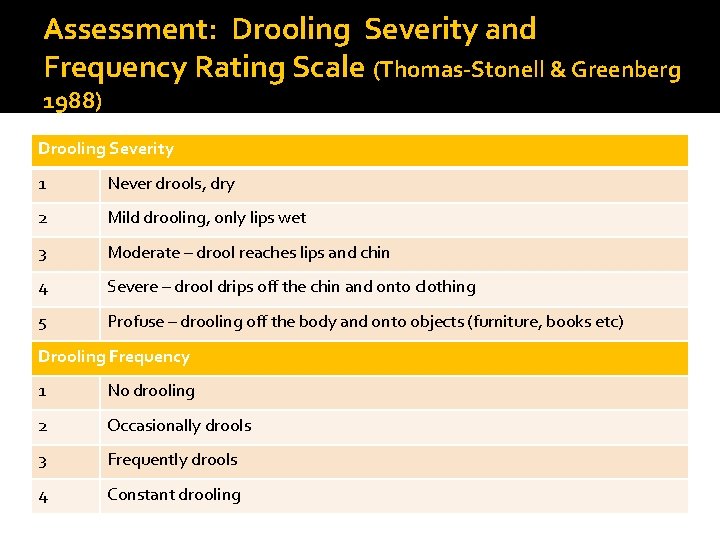
Assessment: Drooling Severity and Frequency Rating Scale (Thomas-Stonell & Greenberg 1988) Drooling Severity 1 Never drools, dry 2 Mild drooling, only lips wet 3 Moderate – drool reaches lips and chin 4 Severe – drool drips off the chin and onto clothing 5 Profuse – drooling off the body and onto objects (furniture, books etc) Drooling Frequency 1 No drooling 2 Occasionally drools 3 Frequently drools 4 Constant drooling
Assessment: Drooling Impact Scale (Reid et al. 2009)
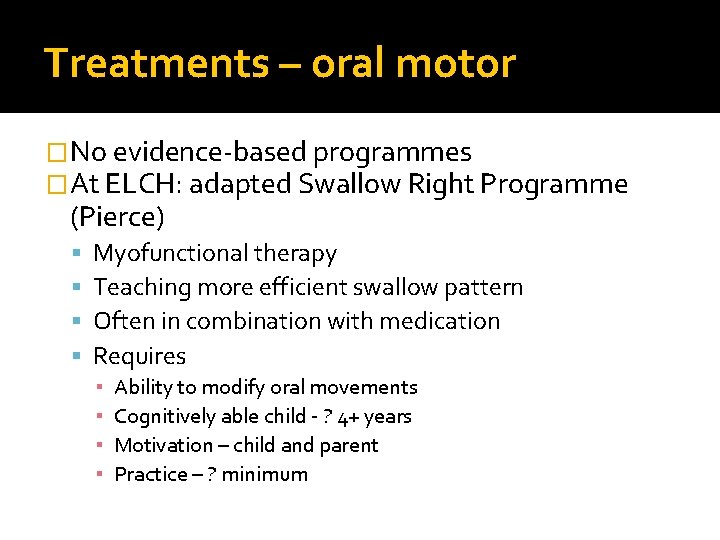
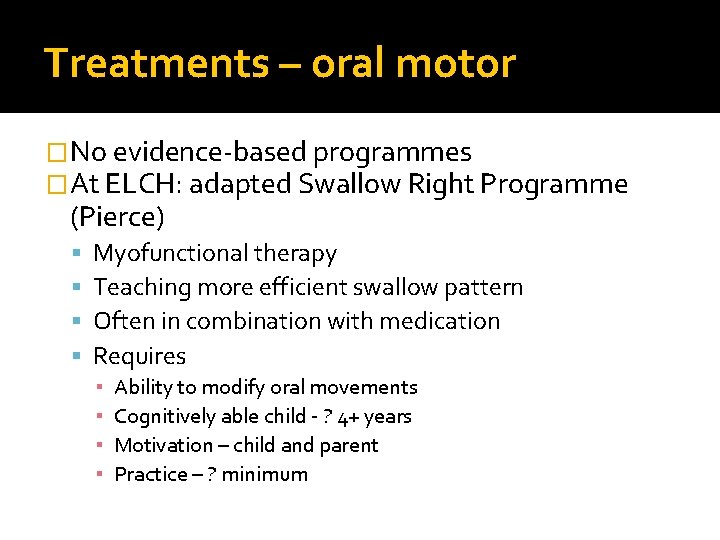
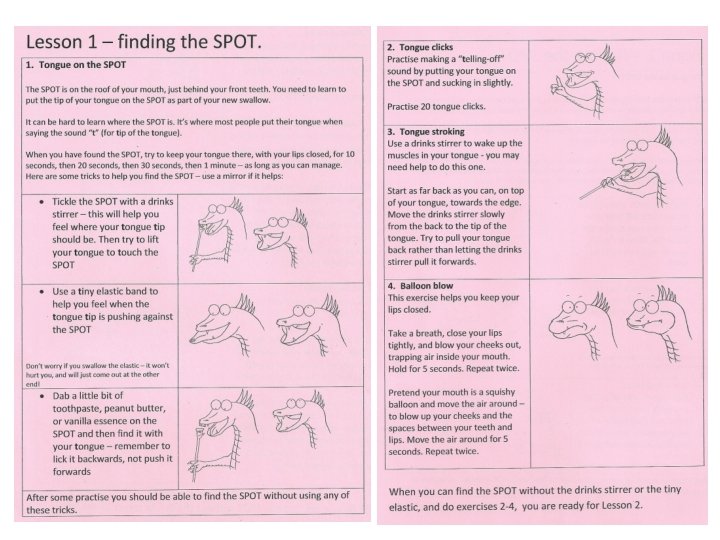
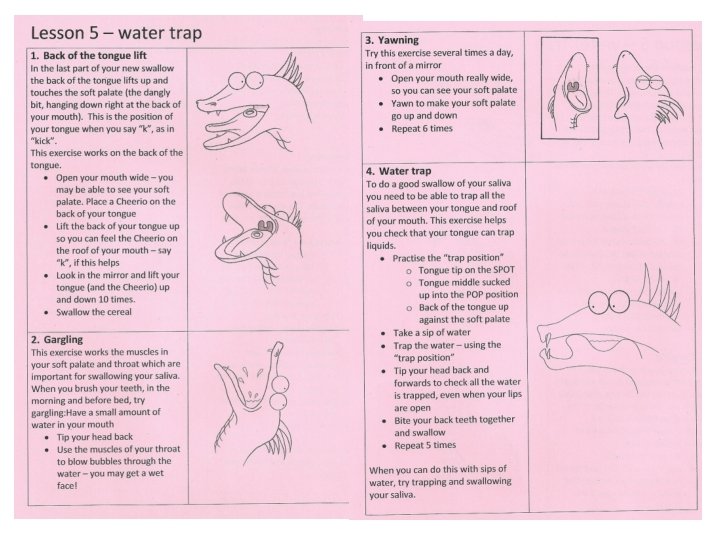
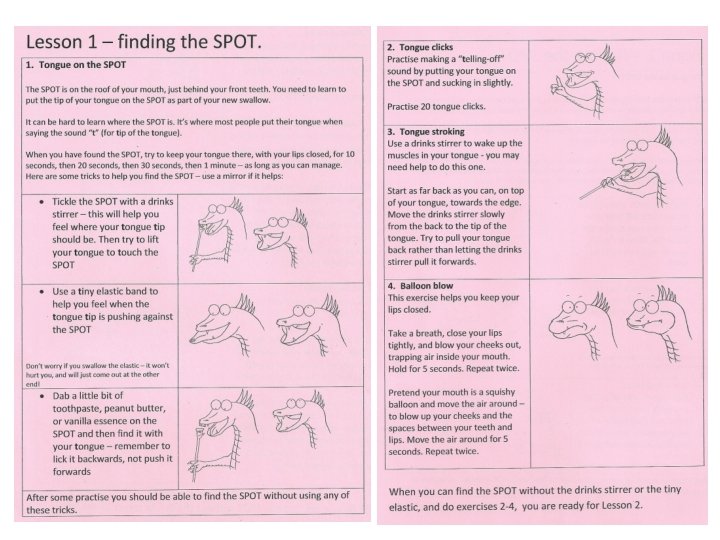
Treatments – oral motor �No evidence-based programmes �At ELCH: adapted Swallow Right Programme (Pierce) Myofunctional therapy Teaching more efficient swallow pattern Often in combination with medication Requires ▪ ▪ Ability to modify oral movements Cognitively able child - ? 4+ years Motivation – child and parent Practice – ? minimum
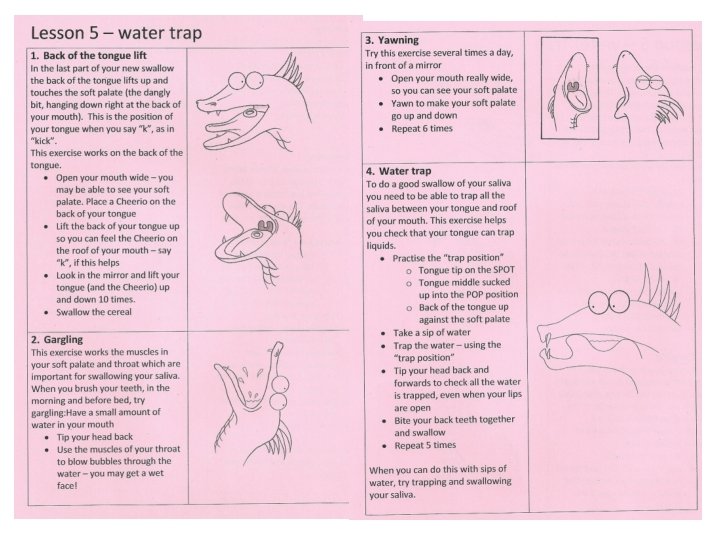
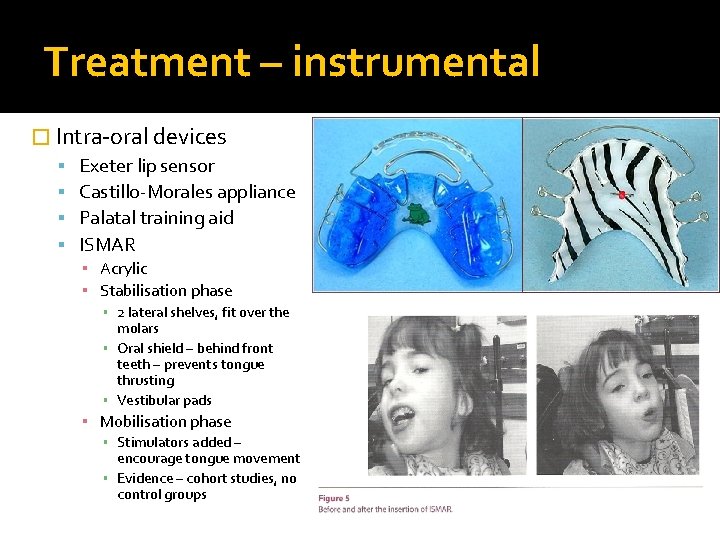
Treatment – instrumental � Intra-oral devices Exeter lip sensor Castillo-Morales appliance Palatal training aid ISMAR ▪ Acrylic ▪ Stabilisation phase ▪ 2 lateral shelves, fit over the molars ▪ Oral shield – behind front teeth – prevents tongue thrusting ▪ Vestibular pads ▪ Mobilisation phase ▪ Stimulators added – encourage tongue movement ▪ Evidence – cohort studies, no control groups
Treatment – medication � Anticholinergics Hyoscine patches (Scopolomine, Scopaderm) – not to be cut! Glycopyronnium bromide – oral medication Trihexyphenidyl (Benzhexol, Broflex) – oral medication Ipatropium bromide - inhaled � Down-regulation of achetylcholine (neurotransmitter) – parasympathetic autonomic control � High rates side effects – blurred vision, constipation, urinary retention � Glycopyrrolate - strongest evidence base, lowest side -effect profile, but very expensive
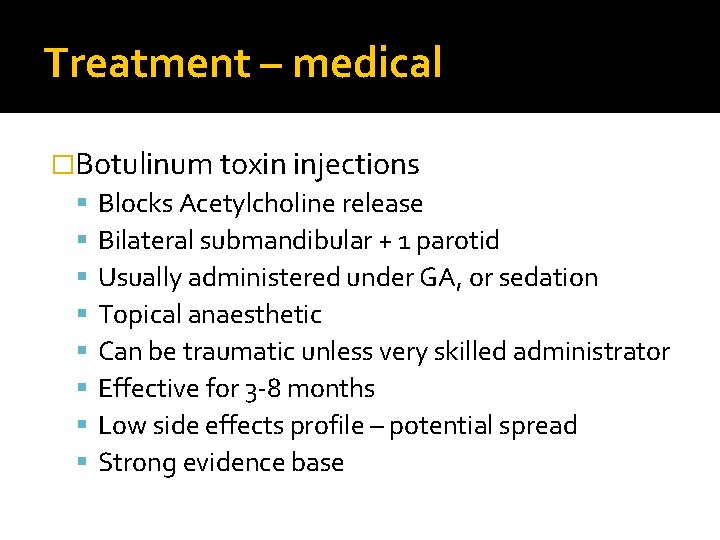
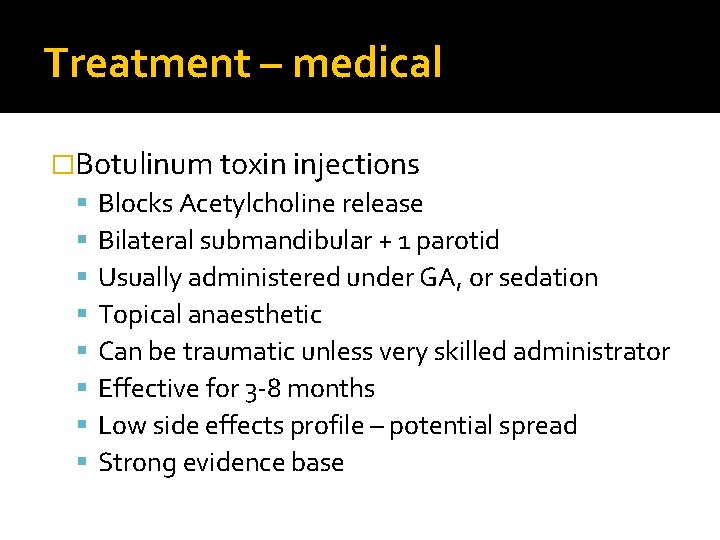
Treatment – medical �Botulinum toxin injections Blocks Acetylcholine release Bilateral submandibular + 1 parotid Usually administered under GA, or sedation Topical anaesthetic Can be traumatic unless very skilled administrator Effective for 3 -8 months Low side effects profile – potential spread Strong evidence base
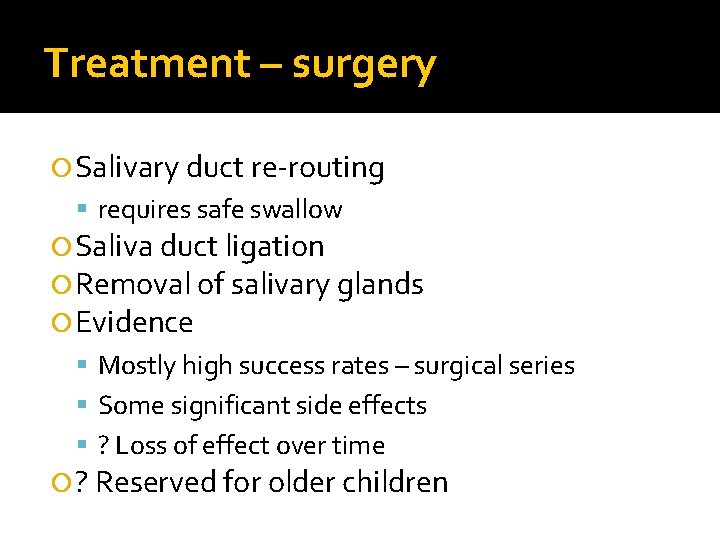
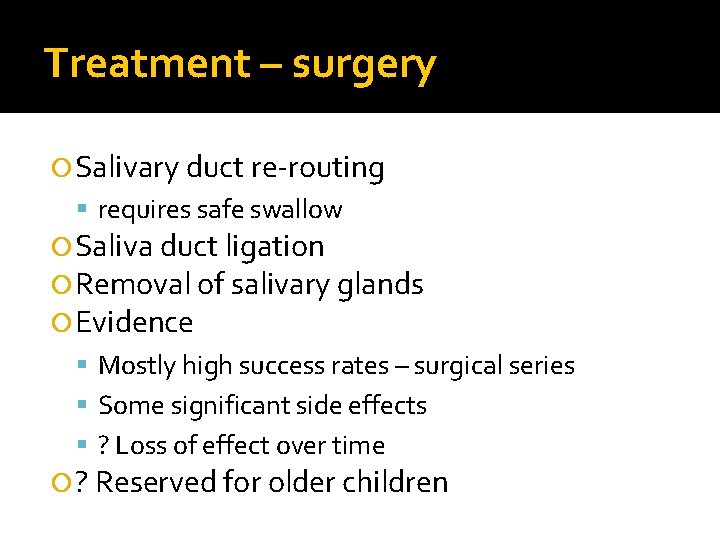
Treatment – surgery Salivary duct re-routing requires safe swallow Saliva duct ligation Removal of salivary glands Evidence Mostly high success rates – surgical series Some significant side effects ? Loss of effect over time ? Reserved for older children
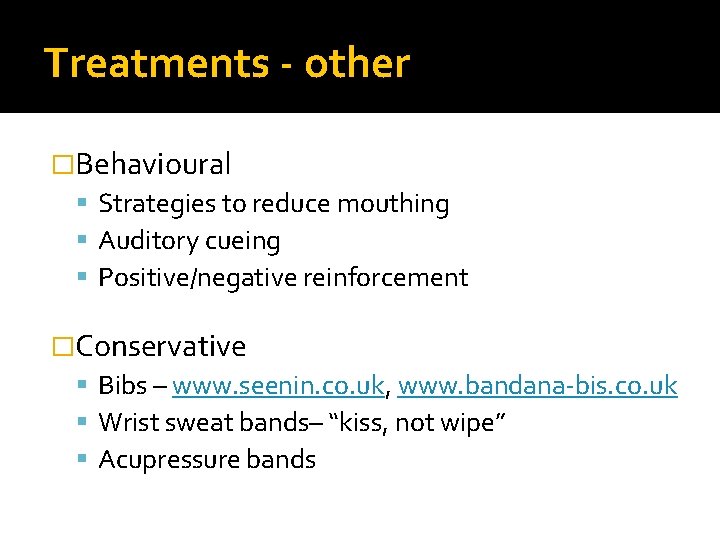
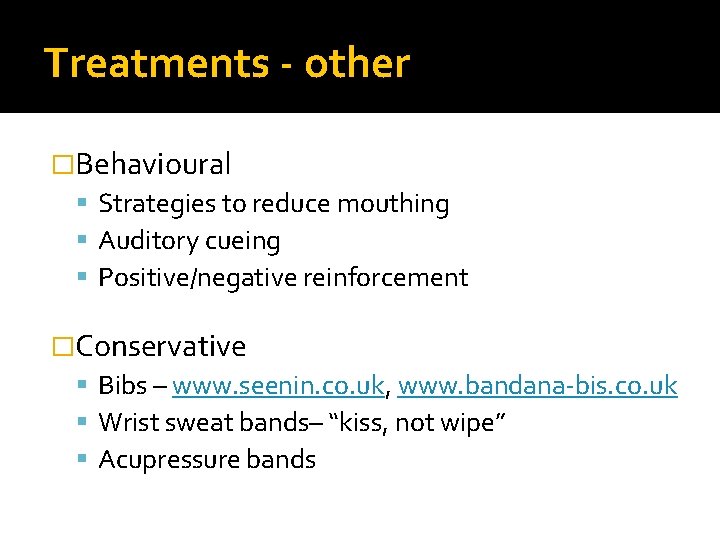
Treatments - other �Behavioural Strategies to reduce mouthing Auditory cueing Positive/negative reinforcement �Conservative Bibs – www. seenin. co. uk, www. bandana-bis. co. uk Wrist sweat bands– “kiss, not wipe” Acupressure bands
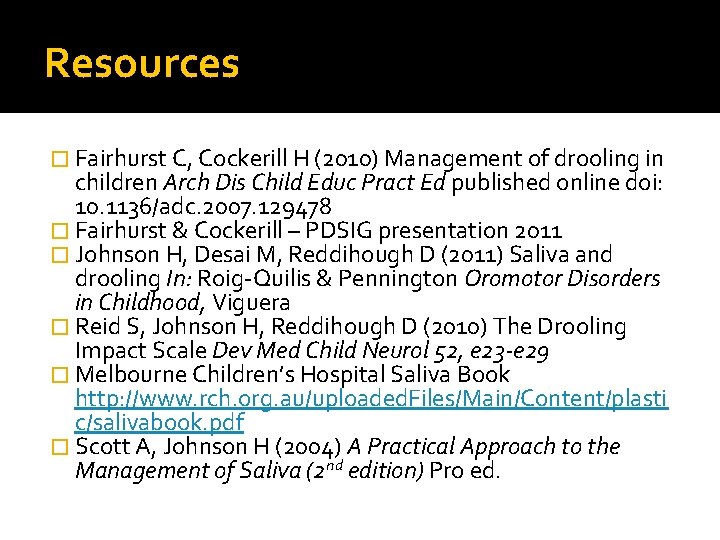
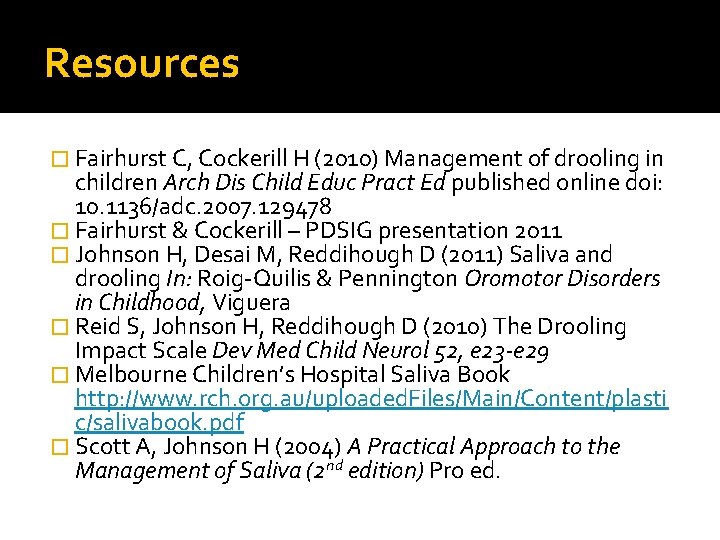
Resources � Fairhurst C, Cockerill H (2010) Management of drooling in children Arch Dis Child Educ Pract Ed published online doi: 10. 1136/adc. 2007. 129478 � Fairhurst & Cockerill – PDSIG presentation 2011 � Johnson H, Desai M, Reddihough D (2011) Saliva and drooling In: Roig-Quilis & Pennington Oromotor Disorders in Childhood, Viguera � Reid S, Johnson H, Reddihough D (2010) The Drooling Impact Scale Dev Med Child Neurol 52, e 23 -e 29 � Melbourne Children’s Hospital Saliva Book http: //www. rch. org. au/uploaded. Files/Main/Content/plasti c/salivabook. pdf � Scott A, Johnson H (2004) A Practical Approach to the Management of Saliva (2 nd edition) Pro ed.