HEED THE HERALD BLEED An Ominous Warning for
HEED THE HERALD BLEED: An Ominous Warning for Potential Vascular Access Rupture Prepared by Pauline Byrne CNS Vascular Access Coordinator Renal Centre, Wollongong, ISHLD
HEED THE HERALD BLEED………AND ACT!! Clinical Excellence Commission (CEC), 2010 � RCA of fatal bleed from an AV fistula (IIMS) Review of similar events: �identified five other deaths and nine significant incidents. 2011: a further death as result of bleeding from an AV fistula The CEC asked ACI for advice on prevention and education resources. This Power. Point was developed to assist with staff training ¾ as part of a package of resources aimed at staff, patients and carers. Remember: Heed the Herald Bleed!. . . ACT!. . . . Save a life!
OBJECTIVES OF THIS PRESENTATION : To define a ‘Herald Bleed’ & potential outcome To assess Access Functionality & identify ‘Vascular Access at Risk’ Outline one centre’s ‘Acute Management Plan’ Describe the role of stakeholders in management of access at risk To demonstrate through a case study review: recognition and management of an access at risk of rupture.
WHAT IS A : ‘Herald Bleed’ Definition: ‘Herald’ - an indication of something that is going to happen In relation to either an Arterio-Venous Fistula (AVF) or Arterio-Venous Graft (AVG), a herald bleed refers to either a small or large spontaneous haemorrhage. A herald bleed may lead to potential vascular access rupture and loss of life.
INTRODUCING MRS. Q Mrs. Q- 68 yrs old, ESRDsecondary to Wegener’s Granulomatosis PTFE Loop inserted Right thigh-24/09/2007 Presented ED 2 years postinsertion –afebrile, chills, and graft red and painful. Blood Culture/Treated IV Antibiotics Day 7 -Abscess over graft/blister like appearance, spontaneous bleed in a Satellite unit on dialysis.
How Can We Identify Access at Risk ? Look- Visual Inspection Feel-Palpate Thrill and Pulse Listen- Character of Bruit Observe- Access re Pressure Trends during Haemodialysis Treatment.

VISUAL INSPECTION: Examine Skin Integrity Is skin thinning over access sites? Is infection present? Is Infection present with sudden appearance aneurysmal dilatation?
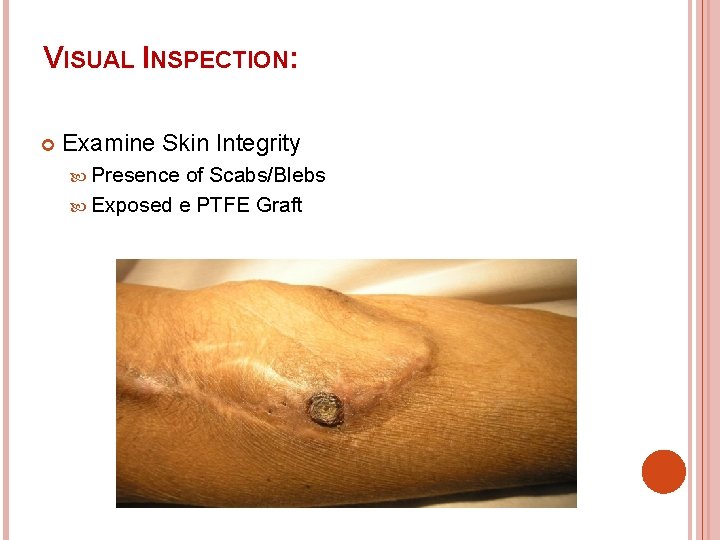
VISUAL INSPECTION: Examine Skin Integrity Presence of Scabs/Blebs Exposed e PTFE Graft
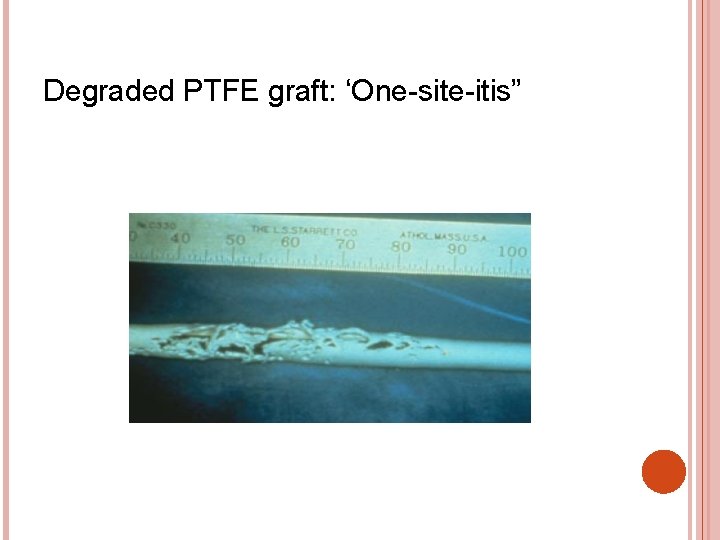
Degraded PTFE graft: ‘One-site-itis”
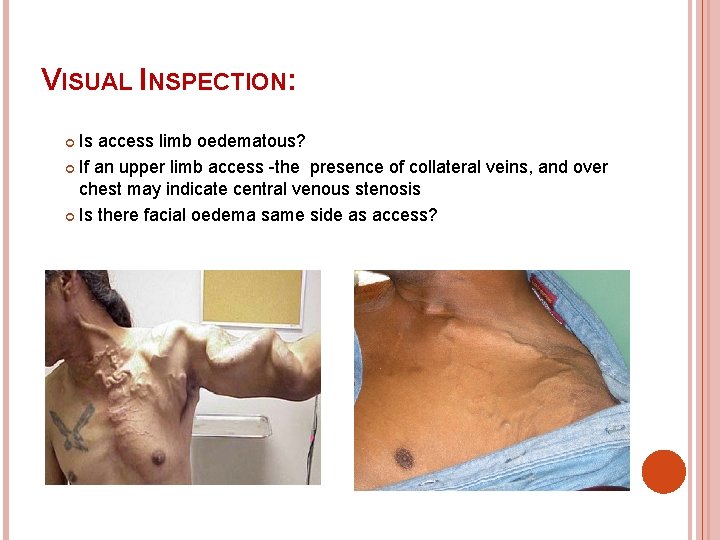
VISUAL INSPECTION: Is access limb oedematous? If an upper limb access -the presence of collateral veins, and over chest may indicate central venous stenosis Is there facial oedema same side as access?

VISUAL INSPECTION: • Development or increase in size of Aneurysmal/Pseudoaneurysmal Dilatations ?
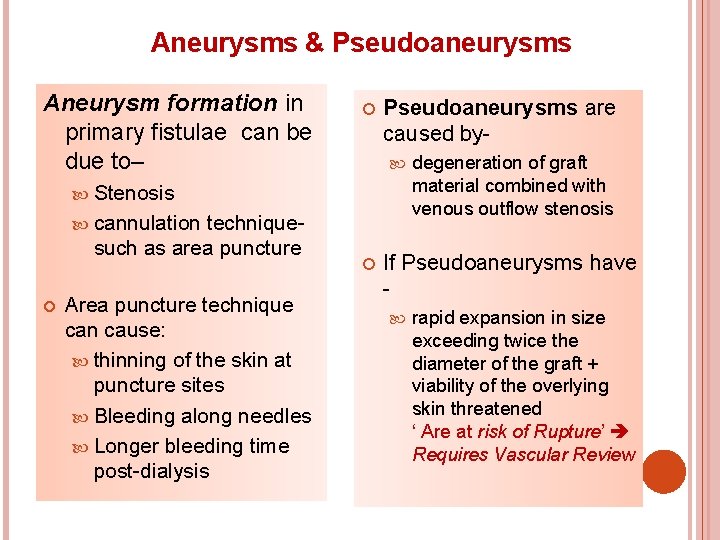
Aneurysms & Pseudoaneurysms Aneurysm formation in primary fistulae can be due to– Pseudoaneurysms are caused by Stenosis cannulation techniquesuch as area puncture Area puncture technique can cause: thinning of the skin at puncture sites Bleeding along needles Longer bleeding time post-dialysis degeneration of graft material combined with venous outflow stenosis If Pseudoaneurysms have rapid expansion in size exceeding twice the diameter of the graft + viability of the overlying skin threatened ‘ Are at risk of Rupture’ Requires Vascular Review
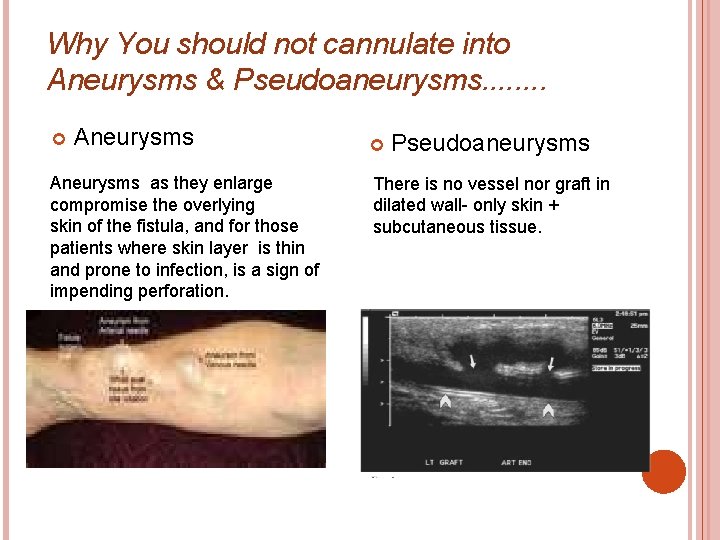
Why You should not cannulate into Aneurysms & Pseudoaneurysms. . . . Aneurysms as they enlarge compromise the overlying skin of the fistula, and for those patients where skin layer is thin and prone to infection, is a sign of impending perforation. Pseudoaneurysms There is no vessel nor graft in dilated wall- only skin + subcutaneous tissue.
ASSESSING FUNCTIONALITY: Why palpate and auscultate access? *Indicators for identifying stenosis* Palpation The ‘Thrill’-at the anastomosis- should be prominent and continuous, with the pulse soft and compressible. If stenosis –thrill may only be present in systole, the pulse may be increased and have a ‘water-hammer character’ Auscultation-The bruit should be continuous and low pitch. If stenosis- the character of the bruit changes to a high pitch & discontinuous.
ASSESSING FUNCTIONALITY: What Other Observations are Useful? Resistance on cannulation Can indicate stenosis + if clotting = possible impending thrombosis Measuring Trends in Venous & Arterial Pressures. Venous Pressure- trend upwards can indicate venous stenosis Arterial Pressure- below -150/-250 may indicate inflow stenosis Observe Bleeding time post-dialysis Post-Dialysis: stenosis Prolonged bleeding may indicate proximal
Diagnostic Confirmation of Access at Risk: Formal Duplex Assessment: a non-invasive method of evaluating: arterial & venous stenoses, graft thrombosis, infection, aneurysm, pseudoaneurysm formation and arterial steal. Access Flow Measurement: Risk of Access Failure: Fistula flow < 500 mls/min Graft < 600 mls/min. Trends and setting of individual thresholds advised.
ONE UNIT’S ACTION PLAN If Access suspected at risk of Rupture: Suspected infected fistulae/grafts, identified herald bleed, evident black scab or blebs, sudden onset aneurysmal dilatation, exposed e PTFE grafts: 1. Do not cannulate: - Renal Registrar/Vascular Registrar review 2. If infection- septic screen / IV Antibiotics 3. Exposed e PTFE-treat as infection 4. Admission 5. Formal Duplex study of access 6. Vascular Revision if clinically required
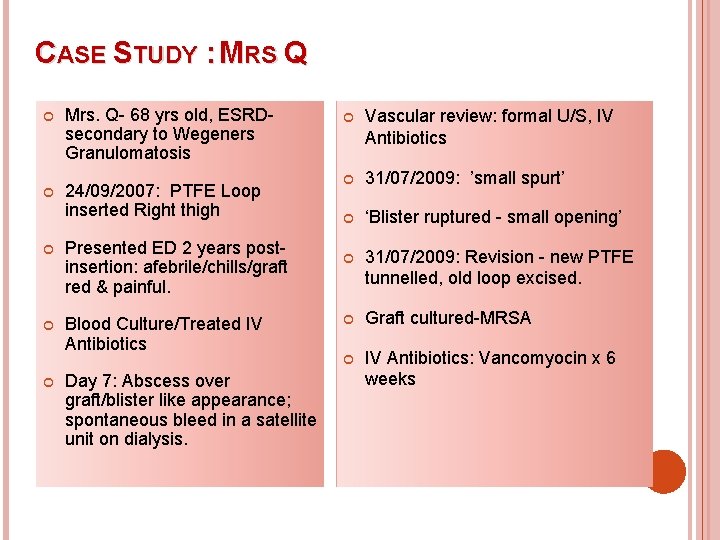
CASE STUDY : MRS Q Mrs. Q- 68 yrs old, ESRDsecondary to Wegeners Granulomatosis 24/09/2007: PTFE Loop inserted Right thigh Presented ED 2 years postinsertion: afebrile/chills/graft red & painful. Blood Culture/Treated IV Antibiotics Day 7: Abscess over graft/blister like appearance; spontaneous bleed in a satellite unit on dialysis. Vascular review: formal U/S, IV Antibiotics 31/07/2009: ’small spurt’ ‘Blister ruptured - small opening’ 31/07/2009: Revision - new PTFE tunnelled, old loop excised. Graft cultured-MRSA IV Antibiotics: Vancomyocin x 6 weeks
ONGOING MANAGEMENTTARGETING EDUCATION TO STAKEHOLDERS Patients & Carers: to recognise and inform medical & nursing staff of abnormalities noted with their vascular access, have knowledge of what to do in an emergency. Nursing Staff: to recognise a vascular access at risk & report to medical staff, provide & review education to patients on a regular basis, provide patients with a ’Bleeding Emergency Kit’ Resident Medical Officers/Medical Registrars: to recognise the normal attributes of vascular access with high blood flows, to recognise what defines a vascular access at risk, and implement treatment plan as per local policy guidelines
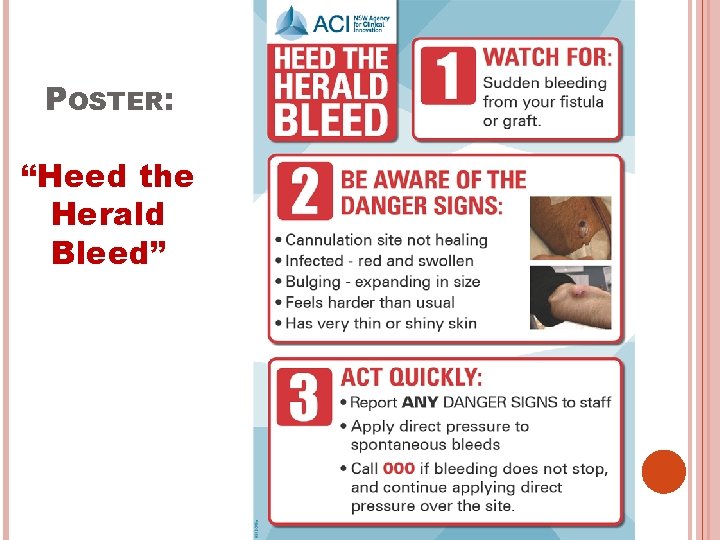
POSTER: “Heed the Herald Bleed”
What Can Your Unit Achieve?
IN SUMMARY This Presentation has: Defined a herald bleed as ‘. . . spontaneous small or large haemorrhage from an AVF/AVG’ Described: how to assess functionality of an AVF/AVG & to identify types of vascular access at-risk of rupture Outlined both an acute management plan, and a teaching strategy for relevant stakeholders Demonstrated through a patient case study: the detection of an access at risk with subsequent medical and surgical management.
REFERENCES: Bachleda et al. , 2010, ’Infectious Complications of Arteriovenous e PTFE Grafts for Haemodialysis’, Biomedical Papers of the Medical Faculty of Polacky University in Olomouc, Czech Republic, pp. 13 -19 Caksen et al. , 2003, ‘Spontaneous Rupture of Arteriovenous Fistula in a Chronic Dialysis Patient’, The Journal of Emergency Medicine, pp. 224 -225 GOOGLE IMAGES Kapoian et al. , Dialysis Access and Recirculation, Chapter 5, pp. 1 -14, www. kidneyatlas. org/book 5. Mc Cann et Al. , 2008, ’Vascular Access Management 1: An Overview’, Journal of Renal Care, pp. 77 -84 Mc Cann et Al. , 2009, ‘Vascular Access Management II: AVF/AVG Cannulation Techniques and Complications’, Journal of Renal Care, pp. 90 -98
REFERENCES (cont. ): National Kidney Foundation-KDOQI –Clinical Practice Guidelines for Vascular Access Update 2000, www. kidney. org/professionals/kdoqi/guidelines Tordoir et al. , 2007 ‘European Best Practice Guidelines on Vascular Access’, Nephrology, Dialysis and Transplant Journal. pp. 88 -117 Tricht et AL. , 2005, ’Haemodynamics and Complications Encountered with Arteriovenous Fistulas and Grafts as Vascular Access for Haemodialysis: A Review', The Annals of Biomedical Engineering pp. 1142 -1156 Yan et al. , 2009, ’Successful surgical treatment of a ruoture to an arteriovenous fistula aneurysm’, ‘Cardiovascular Journal of Africa’, pp. 186197.
ACKNOWLEDGEMENTS: Professor Maureen Lonergan Director Renal Services, Illawarra and Shoalhaven Area Dr Kohlhagen, Dr Holt, Dr Greenstein, Dr Wen and Dr Zafiriou Nephrologists, Wollongong Renal Centre Dr Huber, Dr Villalba and Dr Stanton Vascular Surgeons, Wollongong Dialysis Staff Wollongong/Shellharbour/Shoalhaven Mrs. Q Case Notes
- Slides: 25