Heat Related Illness Richard Dionne MD Emergency Medicine






- Slides: 37
Heat Related Illness Richard Dionne MD Emergency Medicine – University of Ottawa March 2013
Heat Related Illness • Goals & Objectives • Discuss thermoregulation differences between hyperthermic entities and fever • Discuss the differences between Heat Exhaustion and Heat Stroke and their target organ injuries • Identify the differential diagnosis and the proper investigation in the ER • Discuss the acute management in the ER
Basics • Severe illness secondary to overwhelming heat stress • Dehydration – electrolytes – thermoregulation dysfunction – MOF • Increase temperature – increase O 2 consumption and metabolism • Failure of Oxydative Phosphorylation and certain enzymes > 42 °C
Classification 1 - Hyperthermic Diseases A - Minor Y Cramps / Edema / Syncope / Prickly Heat B - Major Y Heat Exhaustion Y Heat Stroke 2 - Hyperthermic Entities A - Malignant Hyperthermia B - Neuroleptic Malignant Syndrome 3 - Febrile Illnesses

Hyperthermia « Auto-Regulation » Peripherical & Central Thermistors Central Thermostat (Anterior Hypothalamus) Modulation Response Peripherical Adaptation Mechanism (vasodilation & sweating)
Hyperthermia vs Fever Y Hyperthermia… • Thermoregulatory mecanism are surpassed … • Peripherical mechanism dont suffice, • The Hypothalamic « set point » is normal … Y Fever… • Cytokins reaches Anterior Hypothalamus • Resets the Thermostat. . . new « set point » • Peripherical mechanism are intact. . .
Heat Exhaustion • Core T < 40° C • Fluid & electrolyte depletion • Thermoregulation is maintained • CNS function is preserved
Heat Stroke • Core T > 40. 5 C • Loss of thermoregulation, severe CNS dysfunction & MOF • Triad: Hyperthemia / CNS / Anhydrose • Classic • Exertional

Heat Stroke • Classic Heat Stroke (non-exertional) – Compromised thermoregulation – (cannot remove from source) – Days – Severe dehydration – Warm & dry skin
Heat Stroke • Exertional Heat Stroke – Younger / athletic with combined environmental & exertional heat stress – Internal heat production overwhelms dissipating mechanisms… – Sweating may be present at beginning
Heat Cramps • Secondary to excessive sweating and sodium loss – Cramps in heavily exercised muscles – Primarily in lower extremities – During or after exercise

Prickly Heat • Blockage of sweat glands leading to a maculopapular rash over clothed area …
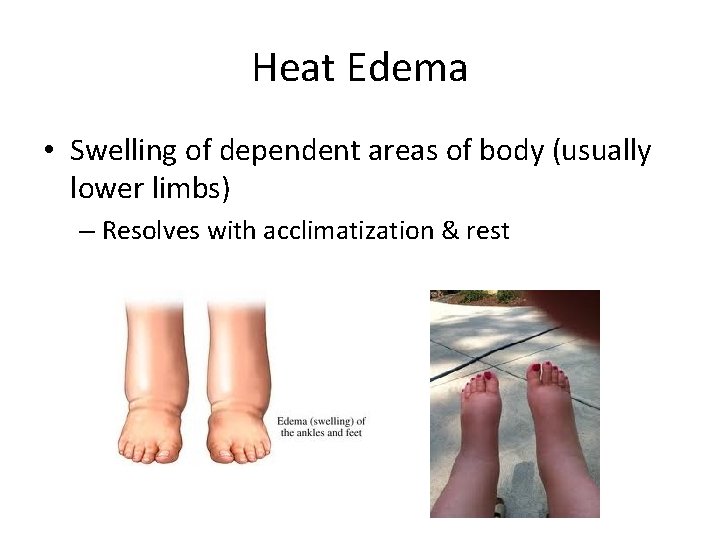
Heat Edema • Swelling of dependent areas of body (usually lower limbs) – Resolves with acclimatization & rest
Etiology • Pre-existing conditions: – Age extremes – Dehydration – Cardiovascular disease – Obesity – Hyperthyroidism – Febrile Illness – Skin disease that interferes with sweating (psoriasis / eczema)
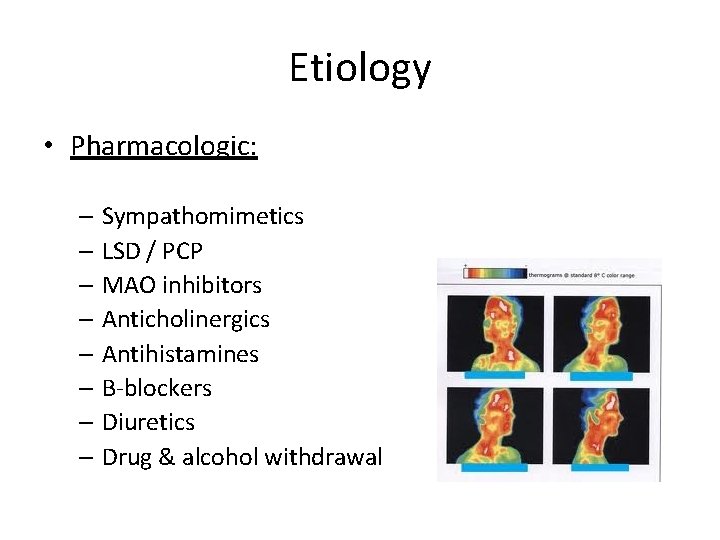
Etiology • Pharmacologic: – Sympathomimetics – LSD / PCP – MAO inhibitors – Anticholinergics – Antihistamines – B-blockers – Diuretics – Drug & alcohol withdrawal
Etiology • Physical / Environmental: – Prolonged exertion – Lack of mobility – Lack of air conditioning – Excessive humidity – Lack of acclimatization
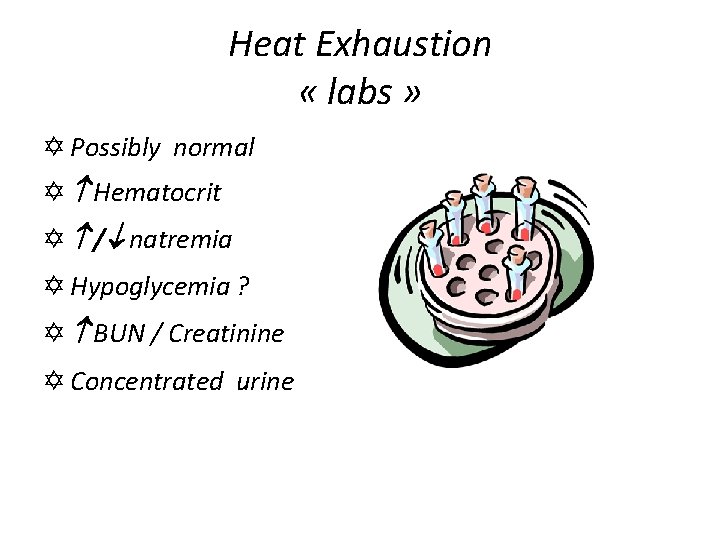
Heat Exhaustion « labs » Y Possibly normal Y Hematocrit Y / natremia Y Hypoglycemia ? Y BUN / Creatinine Y Concentrated urine
Imaging • ECG: cardiac risks • CT-scan Head: r/o CNS primary • Chest X-ray: ARDS?
Differential Diagnosis Sepsis Meningitis Malaria Thyroid storm Status Epilepticus Cerebral Hemorrhage Malignant Hyperthermia Neuroleptic malignant syndrome Tetanus Toxicology ý ASA / PCP / stimulants / Anticholinergic
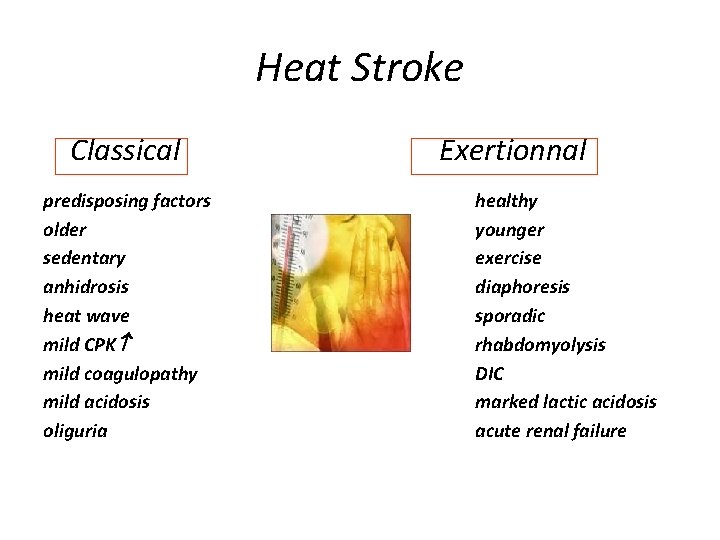
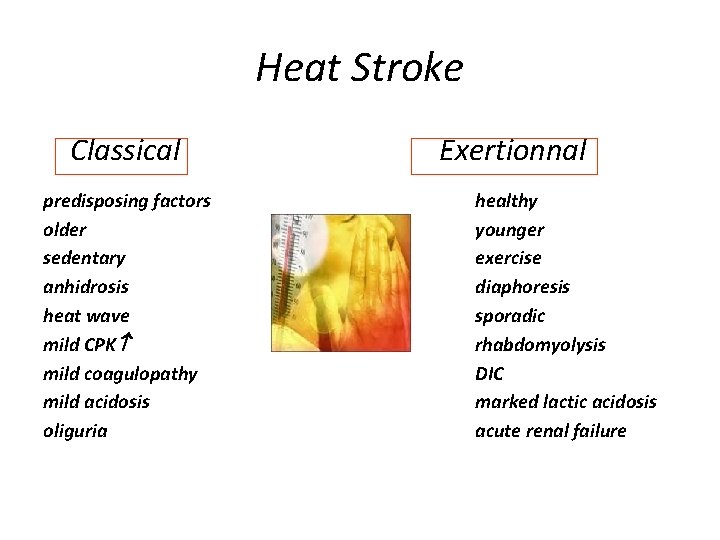
Heat Stroke Classical predisposing factors older sedentary anhidrosis heat wave mild CPK mild coagulopathy mild acidosis oliguria Exertionnal healthy younger exercise diaphoresis sporadic rhabdomyolysis DIC marked lactic acidosis acute renal failure
Treatment
Heat Exhaustion « Treatment » Y Rest / Shade / Cooling methods Y Rehydration … Y PO … 0, 1% Na. Cl solution Y IV … 0, 9% NS ( modest to avoid overhydration) YPeds 20 cc/Kg Y Shivering & seizures: Benzos Y Danger : Sodium levels

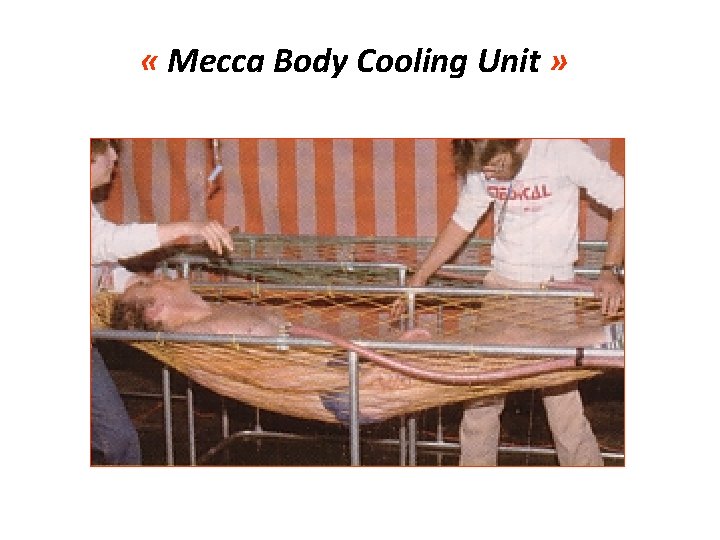
Cooling measures • Evaporative • • Very effective Spray with fine mist Airflow with fans Prevent shivering • Conductive • Ice pack groin / axilla & neck • Immersion not practical ad risk if seizures “Stop cooling at 39°C to risk hypothermia!”
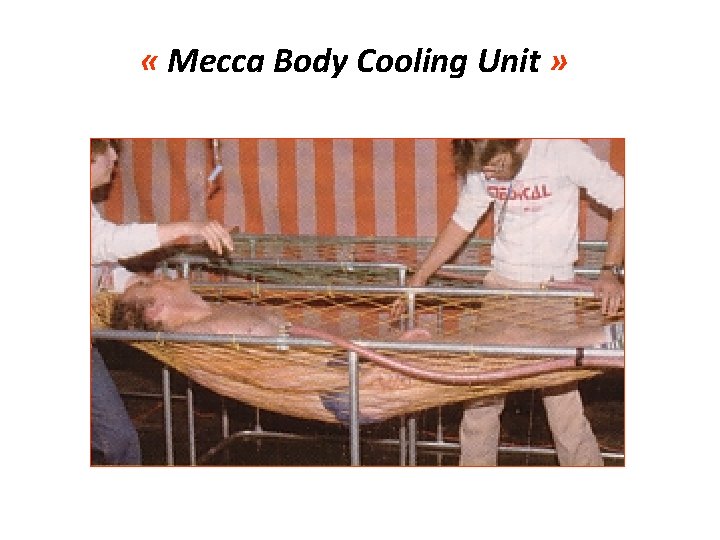
« Mecca Body Cooling Unit »
Not this way ?
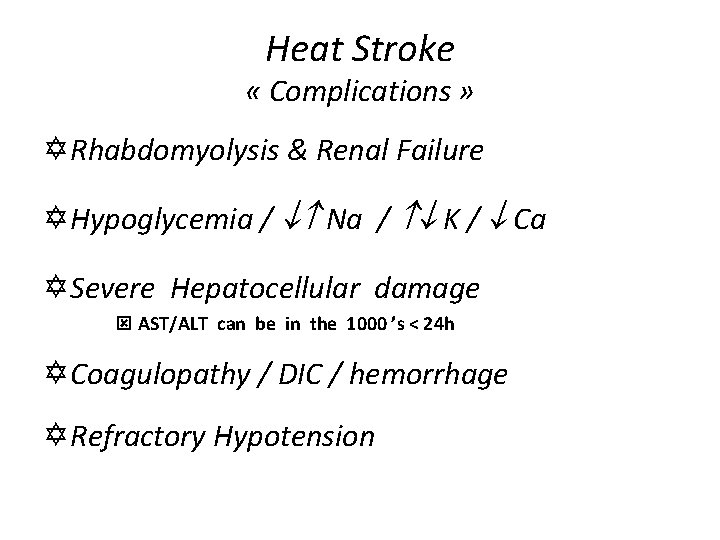
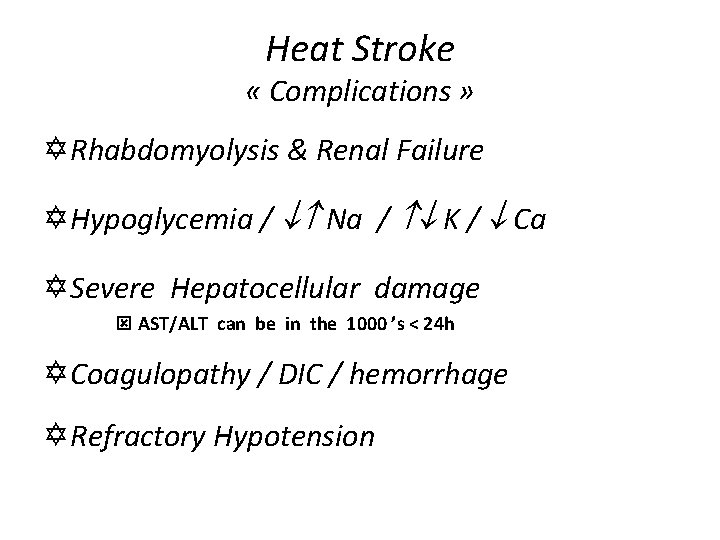
Heat Stroke « Complications » Y Rhabdomyolysis & Renal Failure Y Hypoglycemia / Na / K / Ca Y Severe Hepatocellular damage ý AST/ALT can be in the 1000 ’s < 24 h Y Coagulopathy / DIC / hemorrhage Y Refractory Hypotension
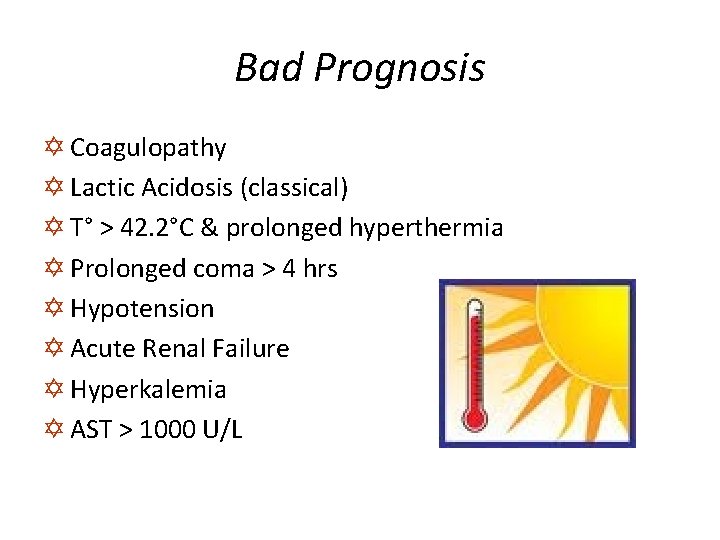
Bad Prognosis Y Coagulopathy Y Lactic Acidosis (classical) Y T° > 42. 2°C & prolonged hyperthermia Y Prolonged coma > 4 hrs Y Hypotension Y Acute Renal Failure Y Hyperkalemia Y AST > 1000 U/L
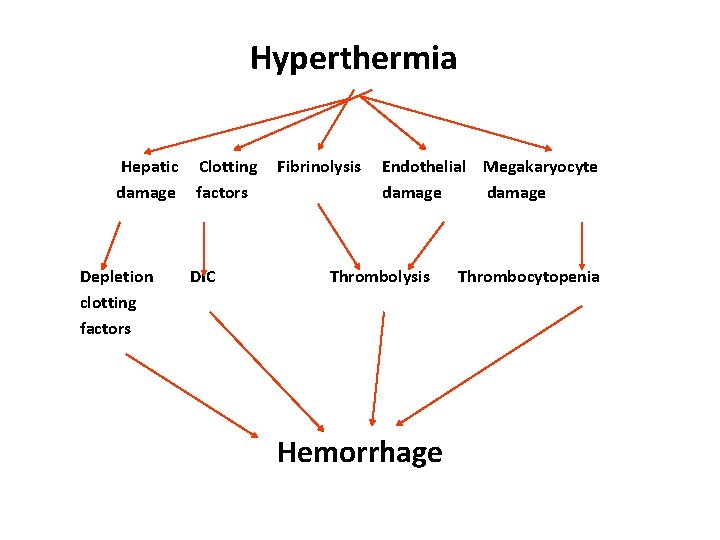
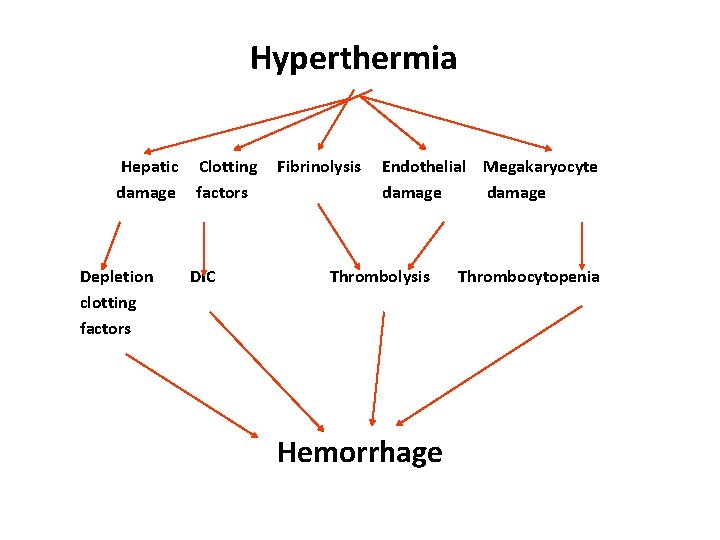
Hyperthermia Hepatic Clotting Fibrinolysis Endothelial Megakaryocyte damage factors damage Depletion DIC Thrombolysis Thrombocytopenia clotting factors Hemorrhage

Hypotension CVP & Cardiac Output Cardiac Output Hypovolemic Hypodynamic Hyperdynamic Fluids & Pressors Cooling & fluids NS 250 -500 cc then slowly (rarely) modest 300 cc/h NS correct BP > 90/60 or CVP N
Prevention 1 - Rely not on thirst 2 - Drink on schedule 3 - Favor sports drinks 4 - Monitor weight 5 - Watch urine 6 - No caffeine or alcohol 7 - Key on meals 8 - Stay cool when you can
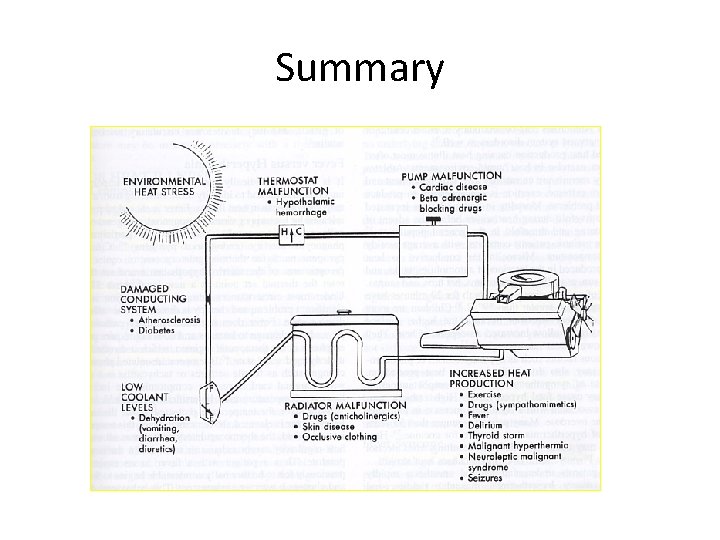
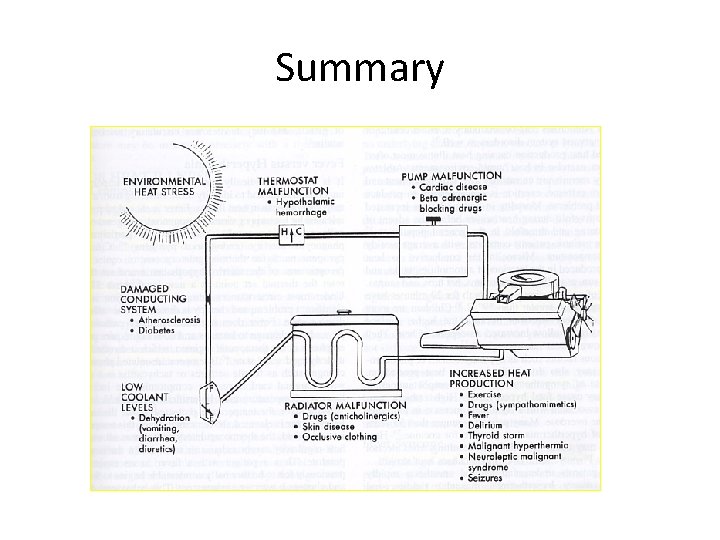
Summary
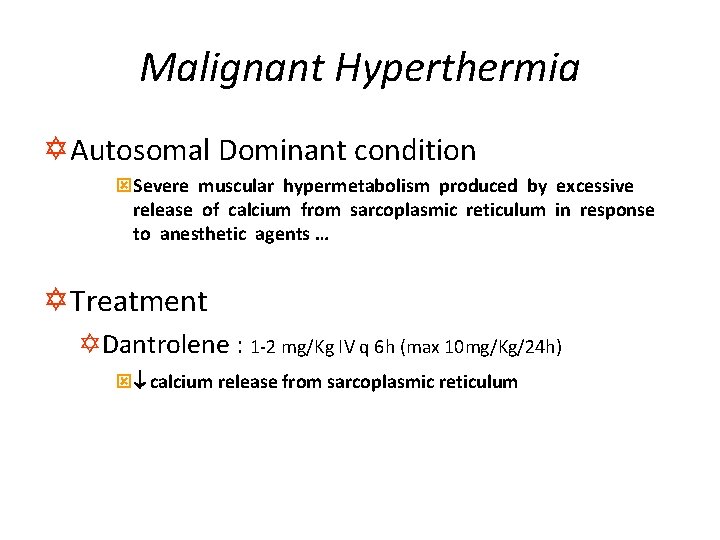
Malignant Hyperthermia Y Autosomal Dominant condition ýSevere muscular hypermetabolism produced by excessive release of calcium from sarcoplasmic reticulum in response to anesthetic agents … Y Treatment YDantrolene : 1 -2 mg/Kg IV q 6 h (max 10 mg/Kg/24 h) ý calcium release from sarcoplasmic reticulum

Neuroleptic Malignant Syndrome Dopamine receptor blocade at Corpus Striatum Muscular Spasticity & Dystonia Heat Production Target Organs (rhabdomyolysis, etc) Y Treatment : ýDantrolene ýBromocriptine (Dopamine Agonist)
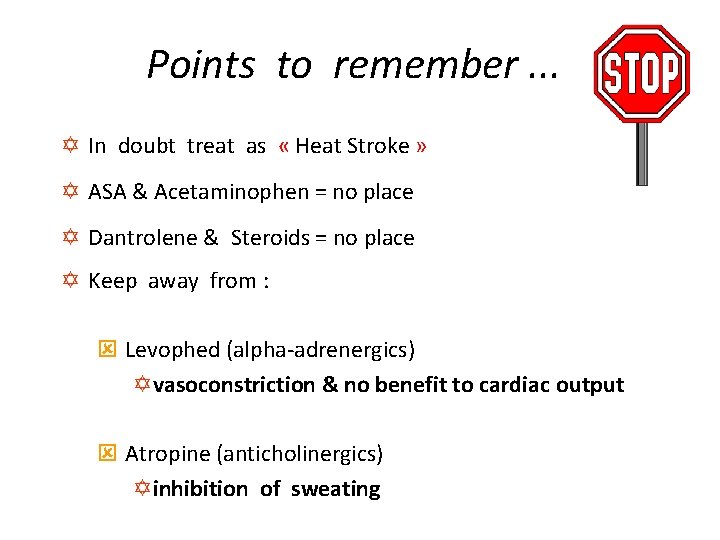
Points to remember. . . Y In doubt treat as « Heat Stroke » Y ASA & Acetaminophen = no place Y Dantrolene & Steroids = no place Y Keep away from : ý Levophed (alpha-adrenergics) Yvasoconstriction & no benefit to cardiac output ý Atropine (anticholinergics) Yinhibition of sweating
Remember Y « Heat stroke victims should be cooled as rapidly as possible. The more rapid the cooling, the lower the mortality. » Y « It does not take long to either boil an egg or to cook neurons. » D Hamilton
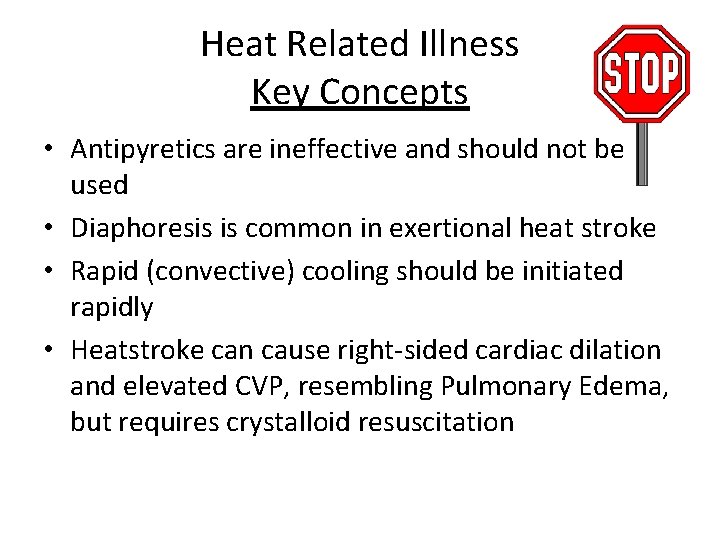
Heat Related Illness Key Concepts • Antipyretics are ineffective and should not be used • Diaphoresis is common in exertional heat stroke • Rapid (convective) cooling should be initiated rapidly • Heatstroke can cause right-sided cardiac dilation and elevated CVP, resembling Pulmonary Edema, but requires crystalloid resuscitation
Questions ?
 Dionne johnson
Dionne johnson Marvin rodriguez baruch
Marvin rodriguez baruch Edwin en dionne
Edwin en dionne Bio1015l
Bio1015l Dionne bates
Dionne bates Stages of heat illness
Stages of heat illness Two types of physical
Two types of physical Health-related skill
Health-related skill Cmc vellore handbook of emergency medicine
Cmc vellore handbook of emergency medicine Emergency medicine case presentation
Emergency medicine case presentation Dutch north sea emergency medicine conference
Dutch north sea emergency medicine conference Unm emergency medicine residents
Unm emergency medicine residents University of arizona emergency medicine
University of arizona emergency medicine Looking for richard
Looking for richard Spcific heat of water
Spcific heat of water Specific latent heat equation
Specific latent heat equation Dry heat cooking methods
Dry heat cooking methods Health illness continuum model
Health illness continuum model History of present illness example
History of present illness example Historical views of mental illness psychology ocr
Historical views of mental illness psychology ocr Food borne illness poster
Food borne illness poster Na in times of illness
Na in times of illness Foodborne illness vocabulary
Foodborne illness vocabulary Fair housing act mental illness
Fair housing act mental illness Foodborne illness
Foodborne illness Mental illness in ancient times
Mental illness in ancient times Eudemonistic model example
Eudemonistic model example Mental health and mental illness chapter 20
Mental health and mental illness chapter 20 Axis 1 and axis 2 disorders
Axis 1 and axis 2 disorders Chapter 17:4 providing first aid for shock
Chapter 17:4 providing first aid for shock What is a common signal of sudden illness
What is a common signal of sudden illness Unit 15:11 providing first aid for sudden illness
Unit 15:11 providing first aid for sudden illness Mark rothko mental illness
Mark rothko mental illness Cc hpi
Cc hpi Mike mazzalongo illness
Mike mazzalongo illness Trustmark critical illness
Trustmark critical illness Dr craig jackson
Dr craig jackson Illness script
Illness script