Heartware HVAD Ventricular Assist System Last edited 91213





- Slides: 51
Heartware HVAD Ventricular Assist System Last edited 9/12/13 1
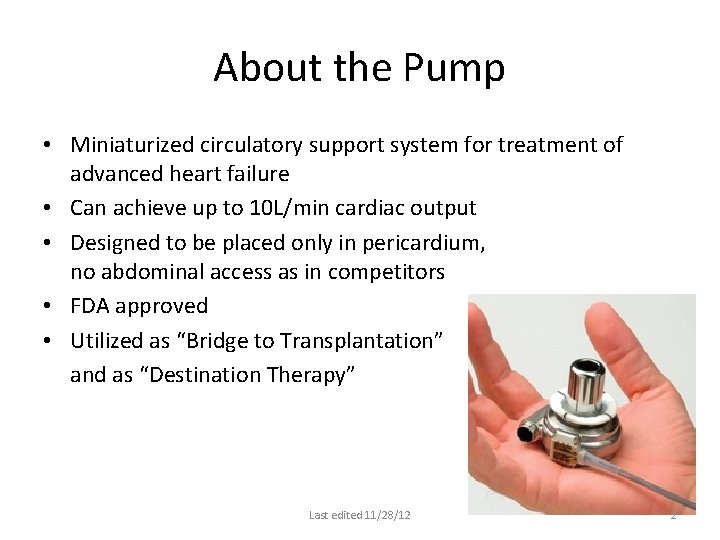
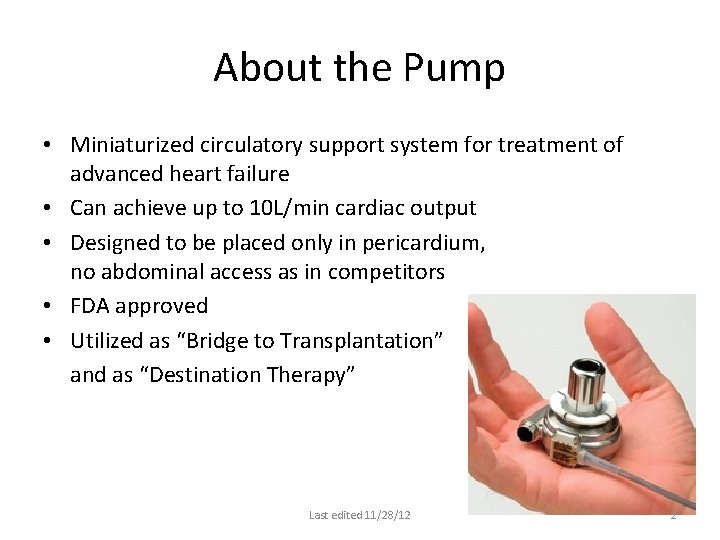
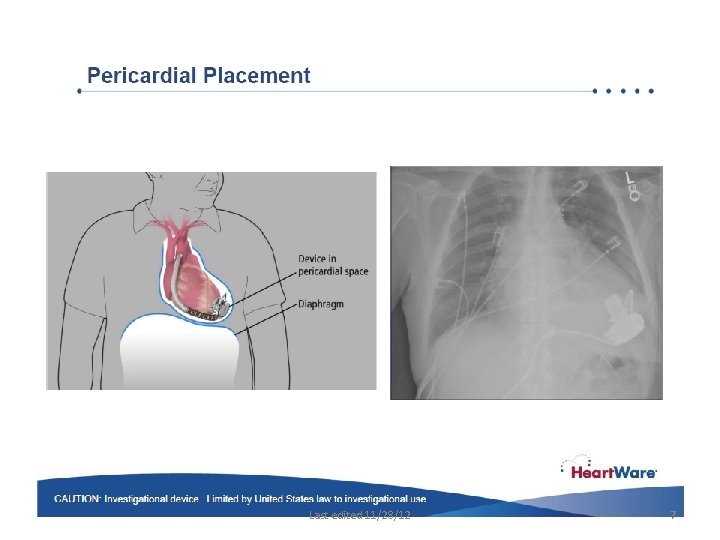
About the Pump • Miniaturized circulatory support system for treatment of advanced heart failure • Can achieve up to 10 L/min cardiac output • Designed to be placed only in pericardium, no abdominal access as in competitors • FDA approved • Utilized as “Bridge to Transplantation” and as “Destination Therapy” Last edited 11/28/12 2

Last edited 11/28/12 3
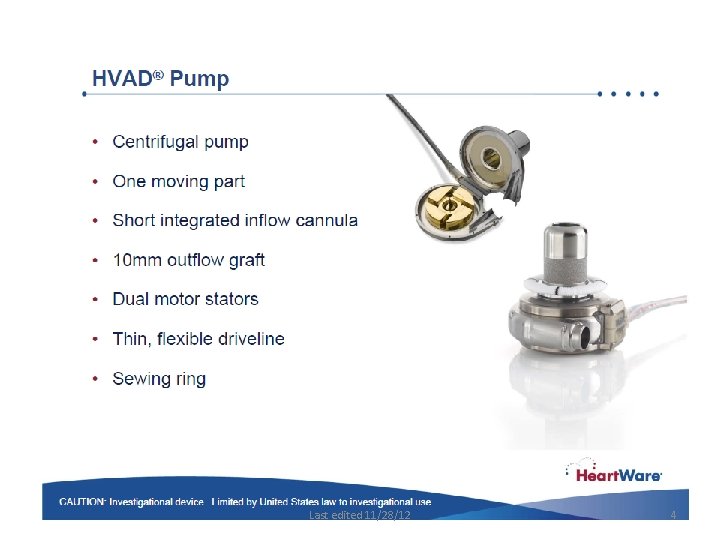
Last edited 11/28/12 4
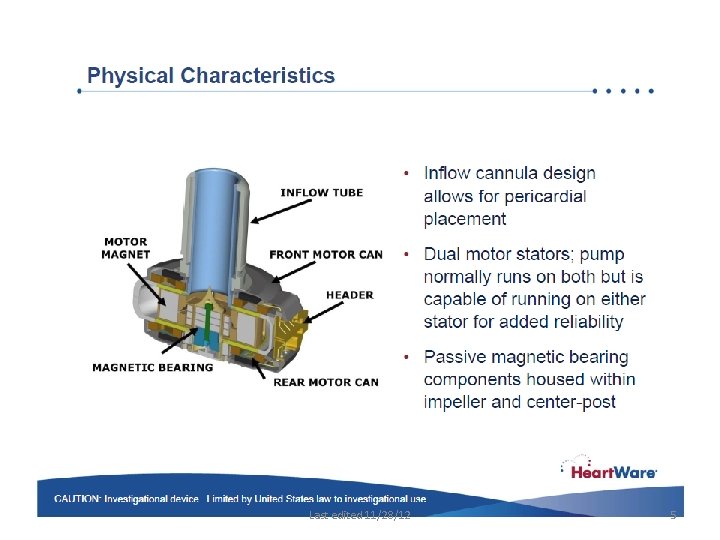
Last edited 11/28/12 5

Last edited 11/28/12 6
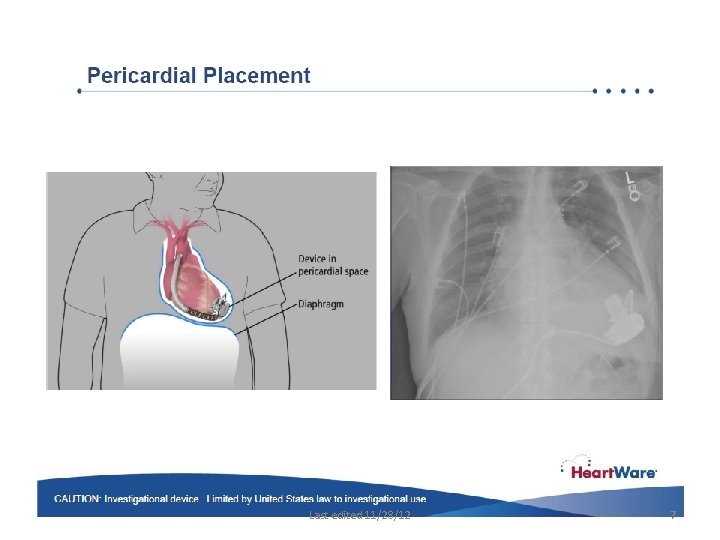
Last edited 11/28/12 7
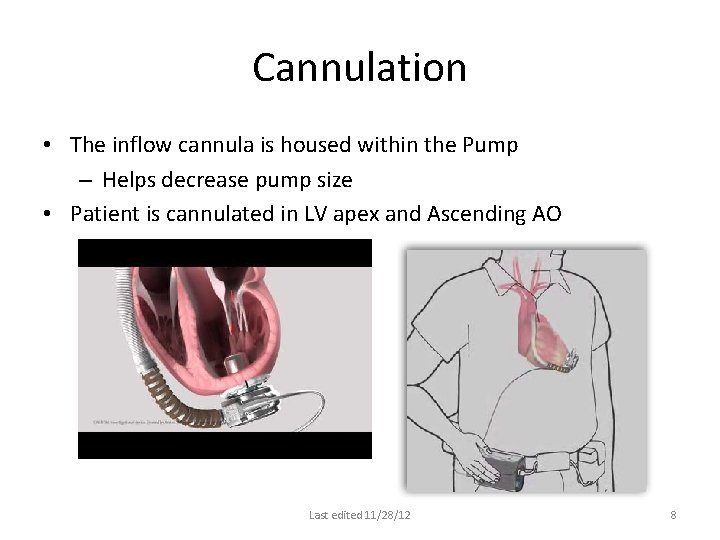
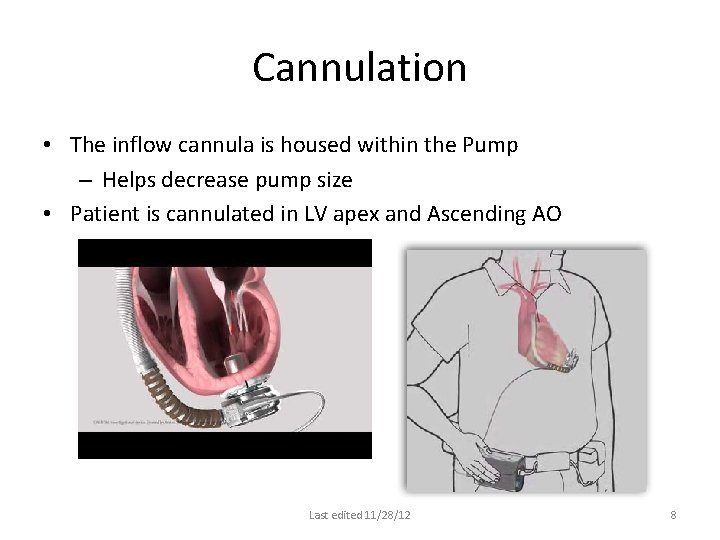
Cannulation • The inflow cannula is housed within the Pump – Helps decrease pump size • Patient is cannulated in LV apex and Ascending AO Last edited 11/28/12 8
Last edited 11/28/12 9
Last edited 11/28/12 10
Last edited 11/28/12 11
Last edited 11/28/12 12

Last edited 11/28/12 13
Last edited 11/28/12 14
Last edited 11/28/12 15
Last edited 11/28/12 16
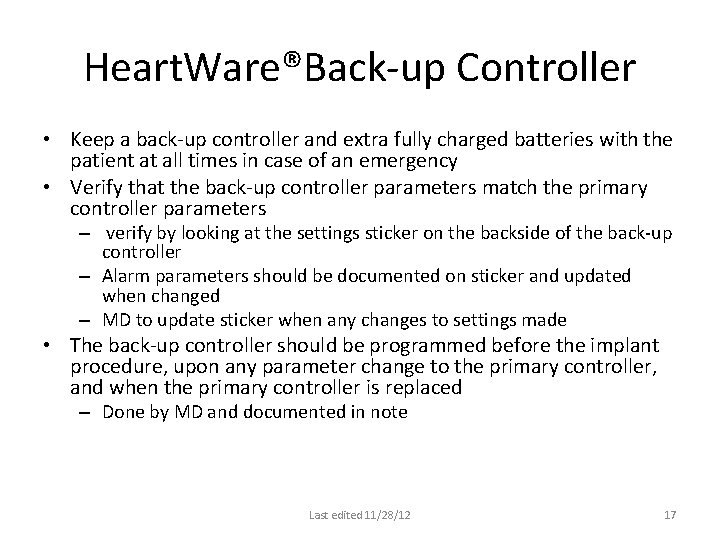
Heart. Ware®Back-up Controller • Keep a back-up controller and extra fully charged batteries with the patient at all times in case of an emergency • Verify that the back-up controller parameters match the primary controller parameters – verify by looking at the settings sticker on the backside of the back-up controller – Alarm parameters should be documented on sticker and updated when changed – MD to update sticker when any changes to settings made • The back-up controller should be programmed before the implant procedure, upon any parameter change to the primary controller, and when the primary controller is replaced – Done by MD and documented in note Last edited 11/28/12 17
Last edited 11/28/12 18
Last edited 11/28/12 19
Last edited 11/28/12 20
Last edited 11/28/12 21
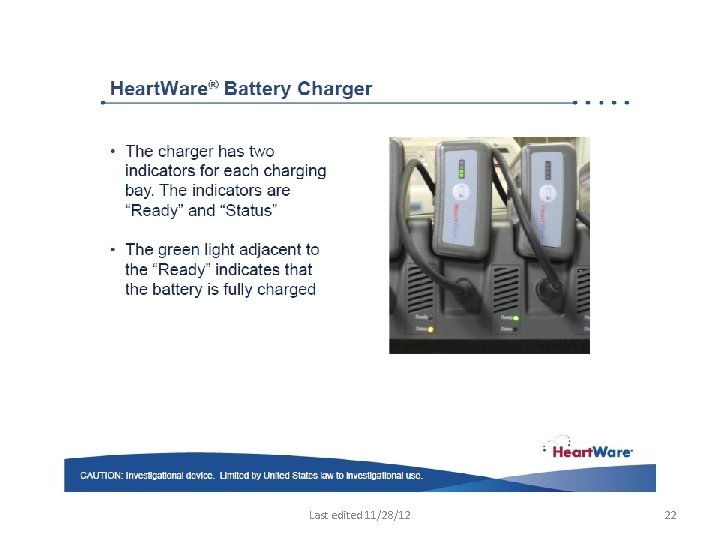
Last edited 11/28/12 22
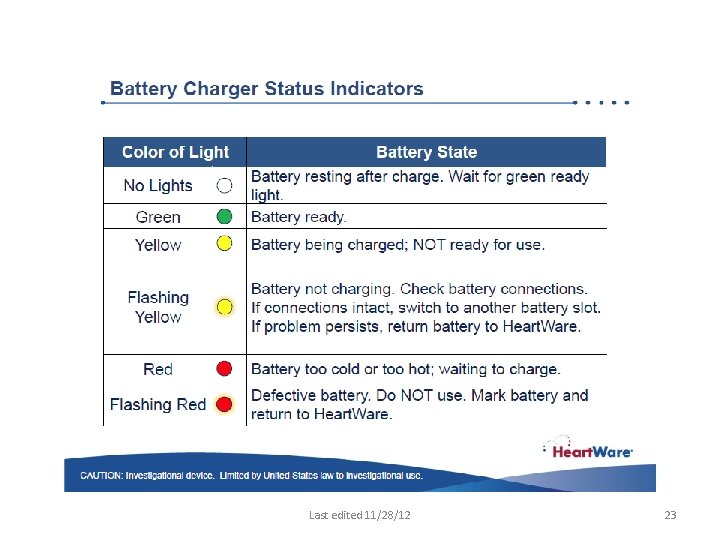
Last edited 11/28/12 23
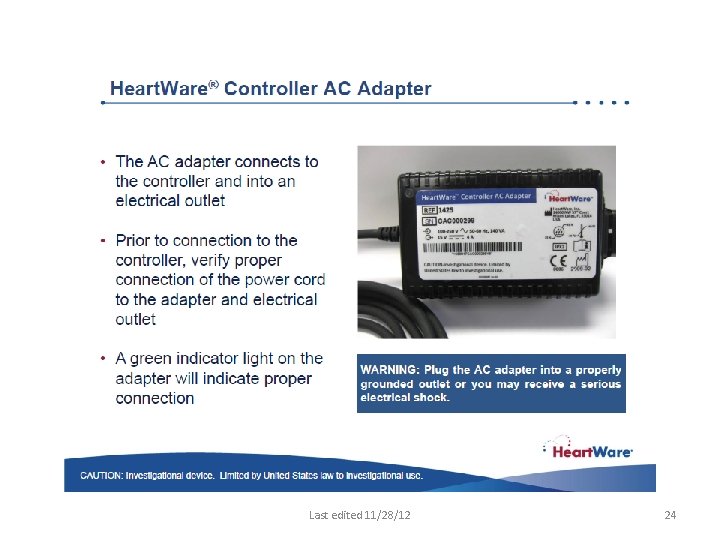
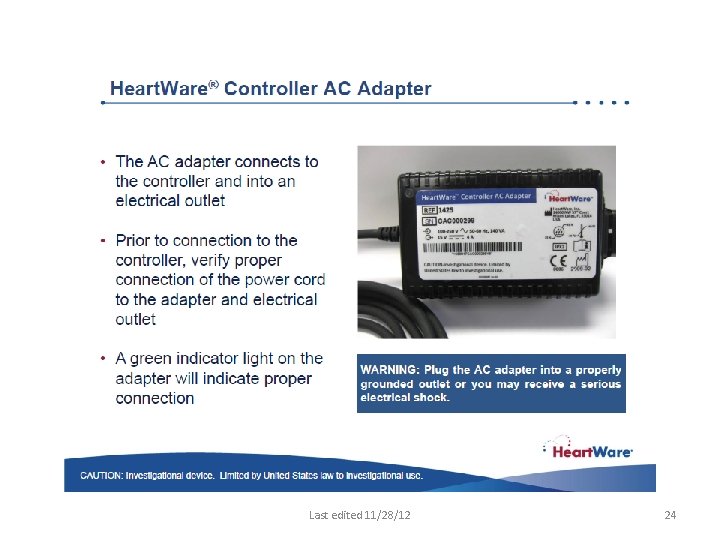
Last edited 11/28/12 24
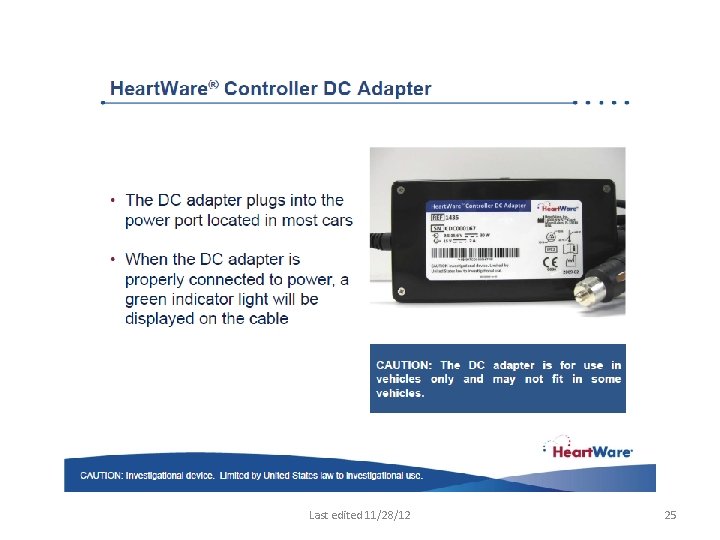
Last edited 11/28/12 25
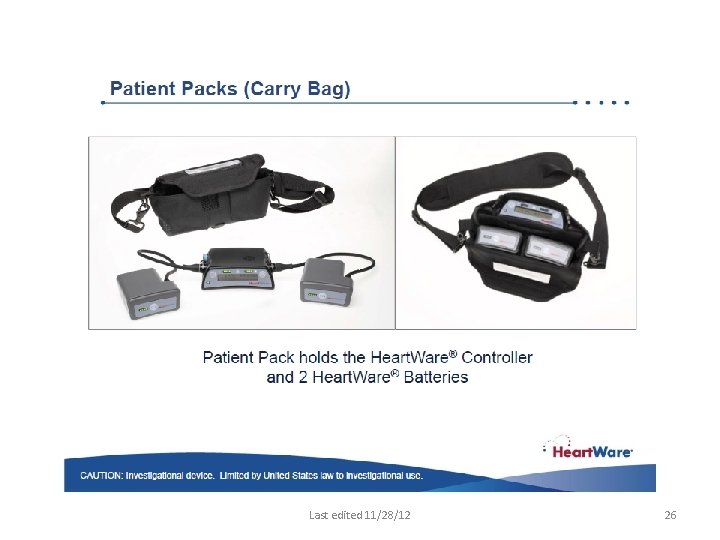
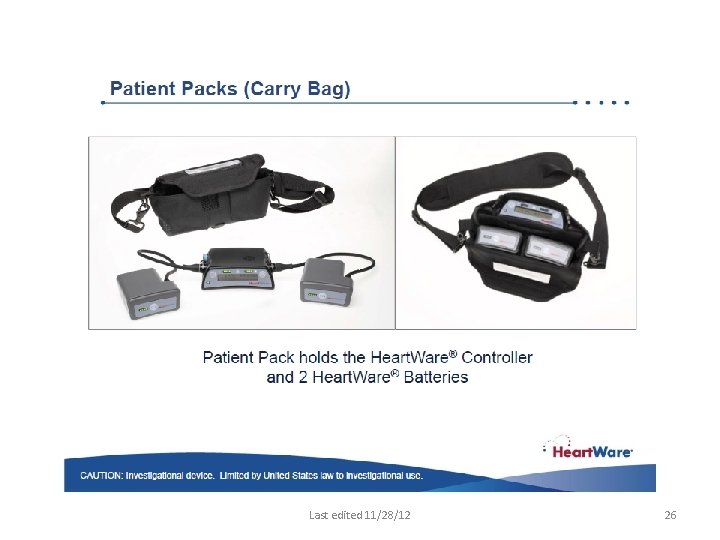
Last edited 11/28/12 26
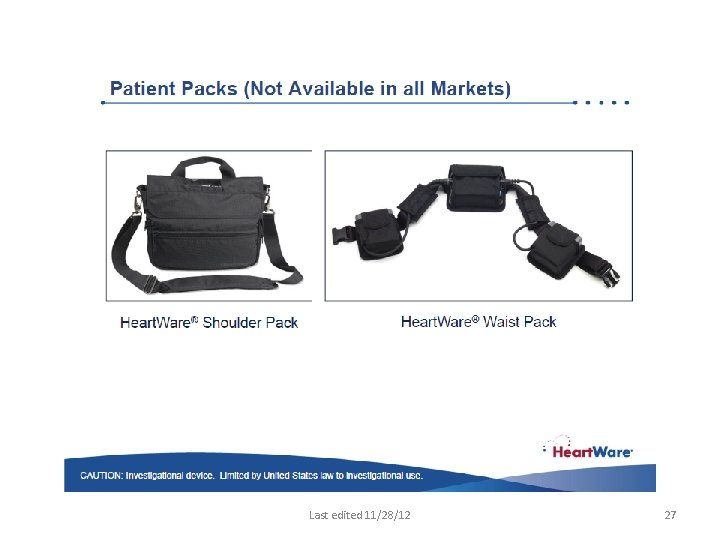
Last edited 11/28/12 27
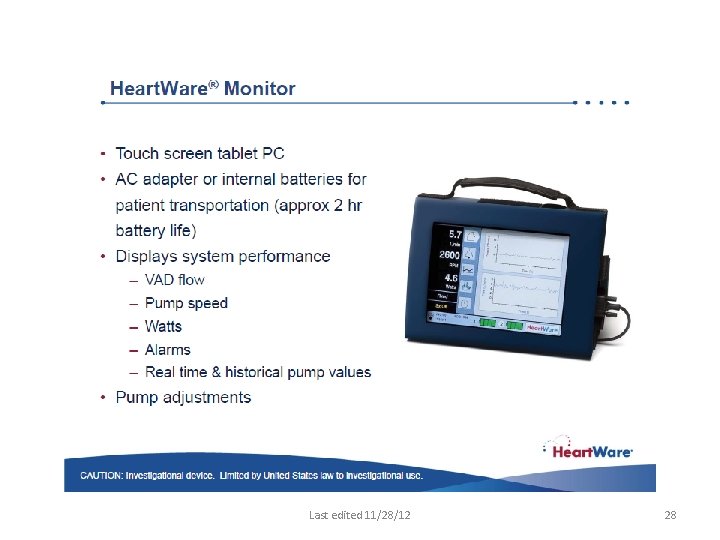
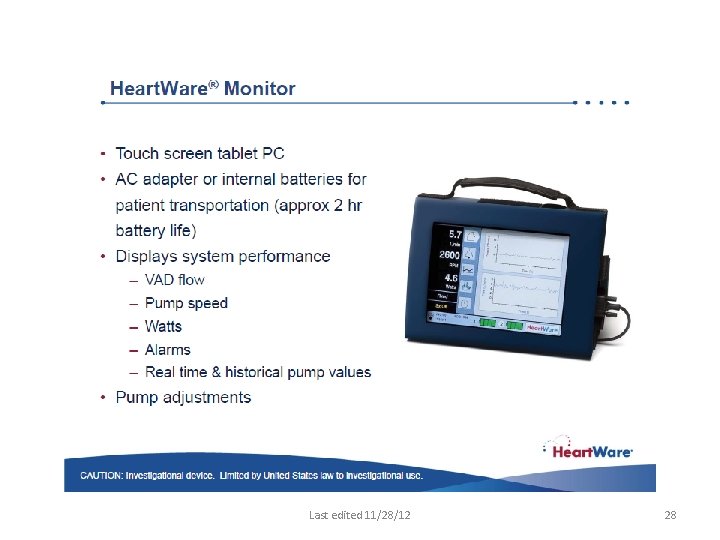
Last edited 11/28/12 28
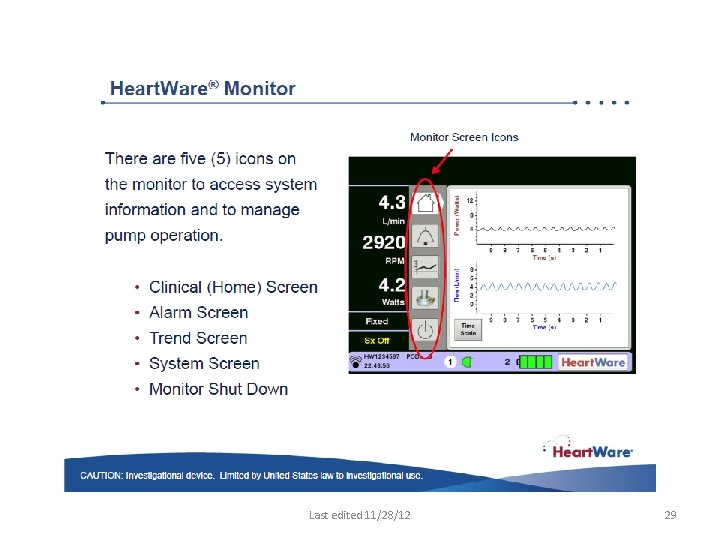
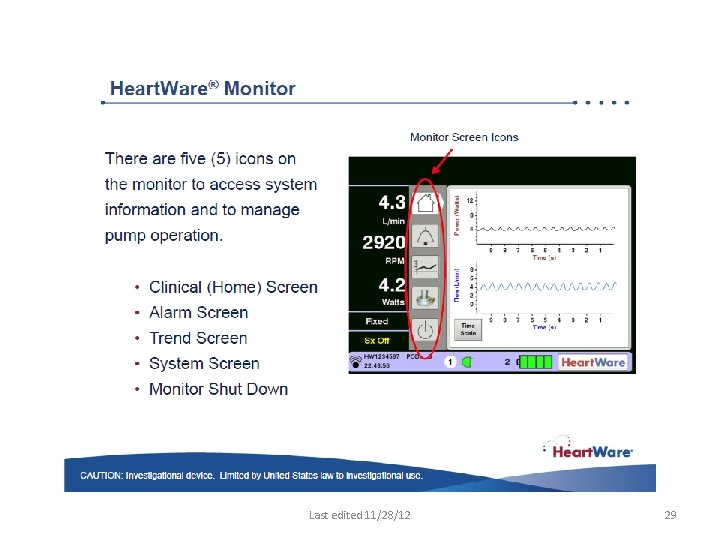
Last edited 11/28/12 29
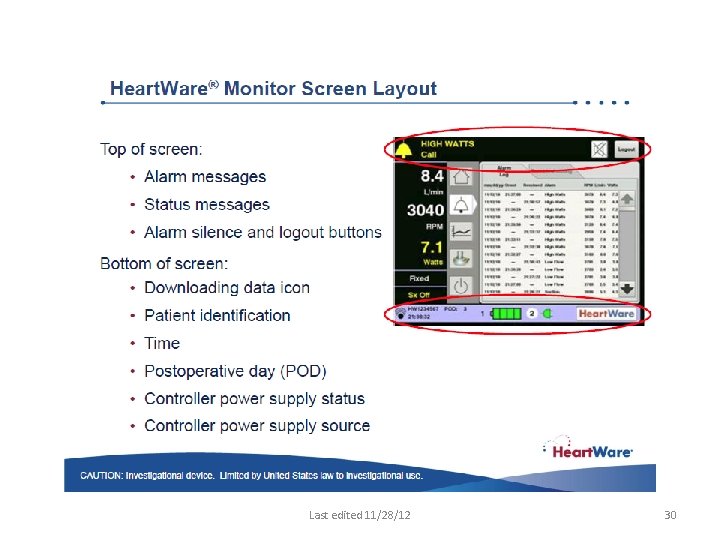
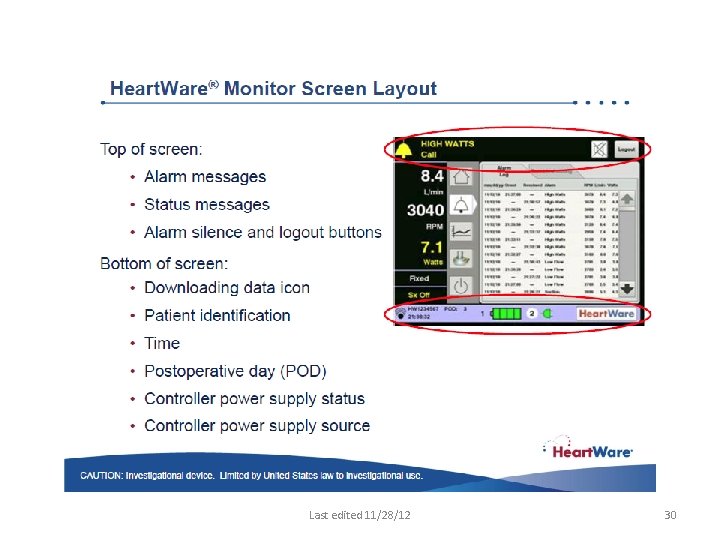
Last edited 11/28/12 30
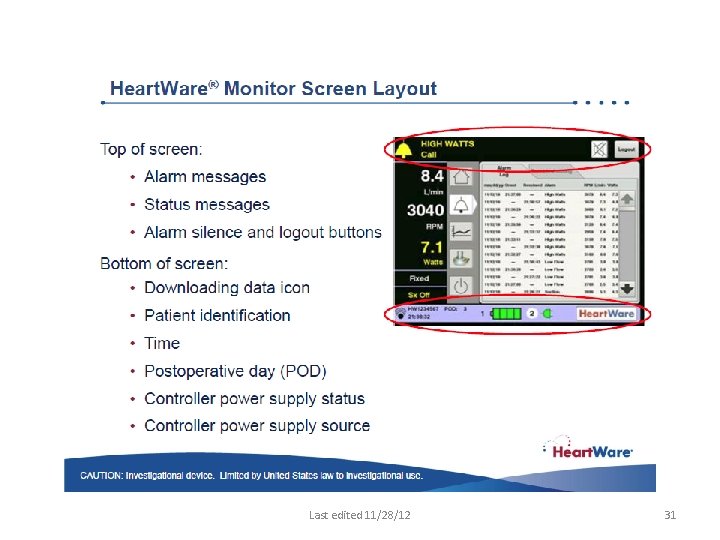
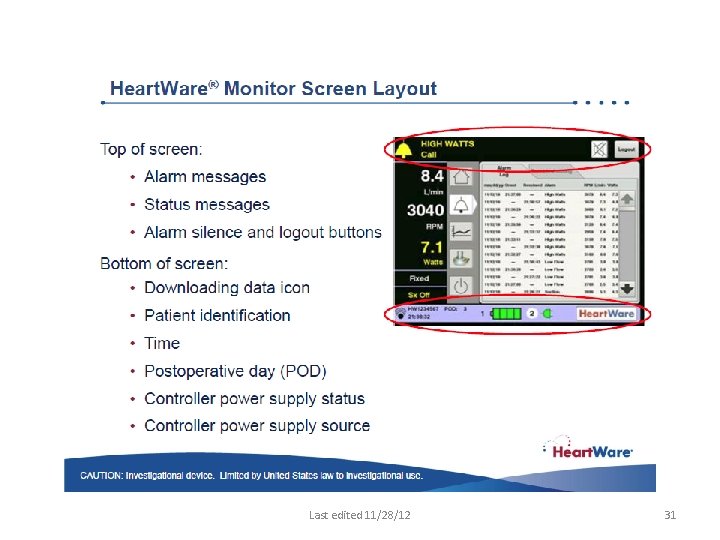
Last edited 11/28/12 31
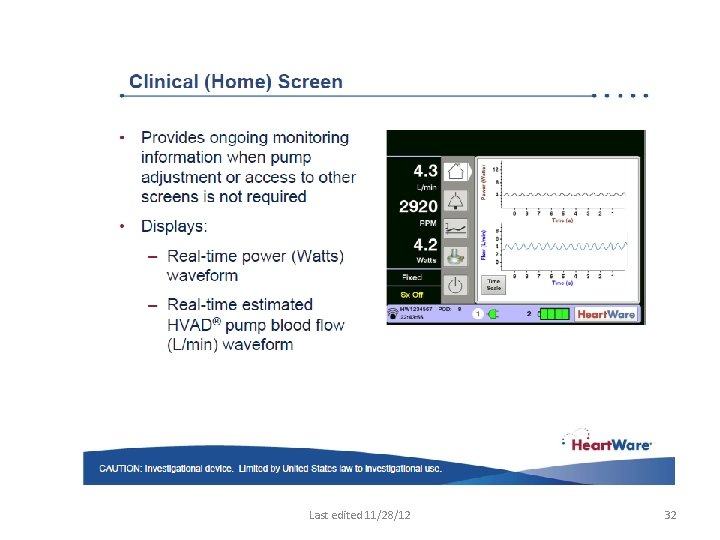
Last edited 11/28/12 32
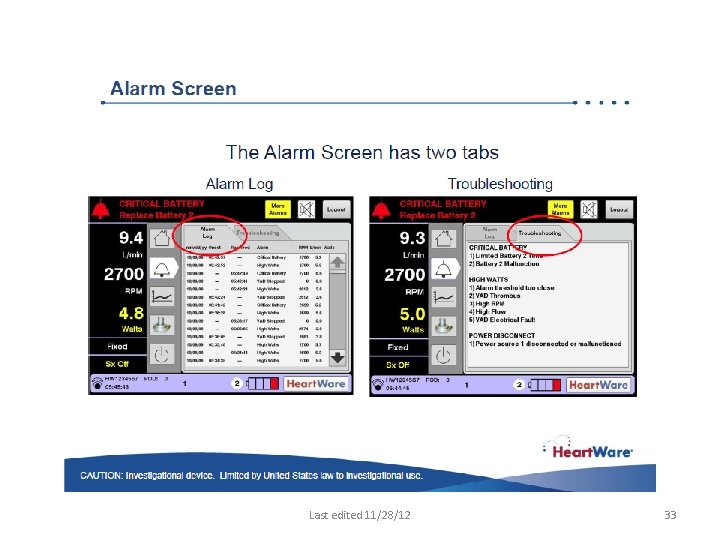
Last edited 11/28/12 33
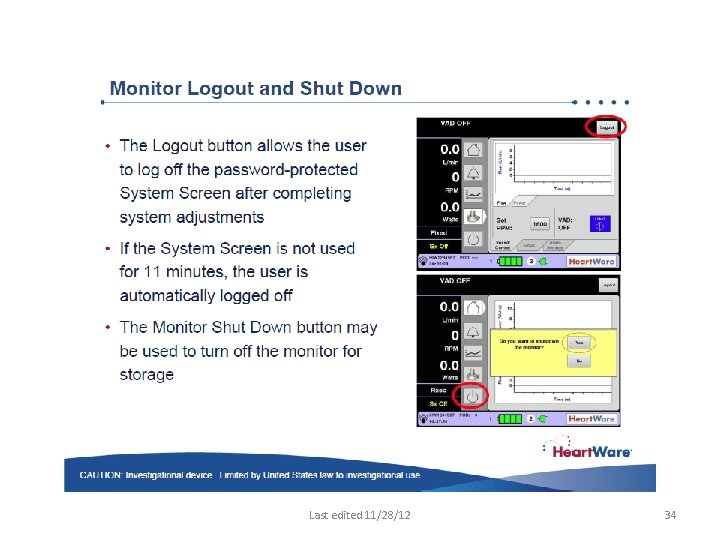
Last edited 11/28/12 34
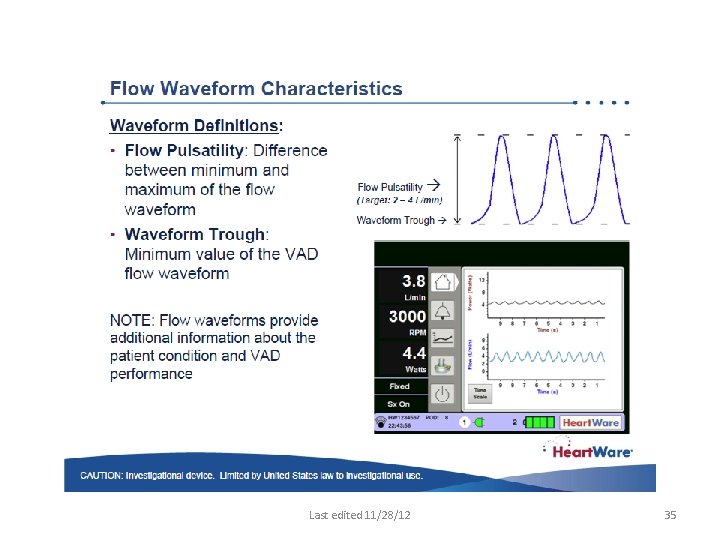
Last edited 11/28/12 35
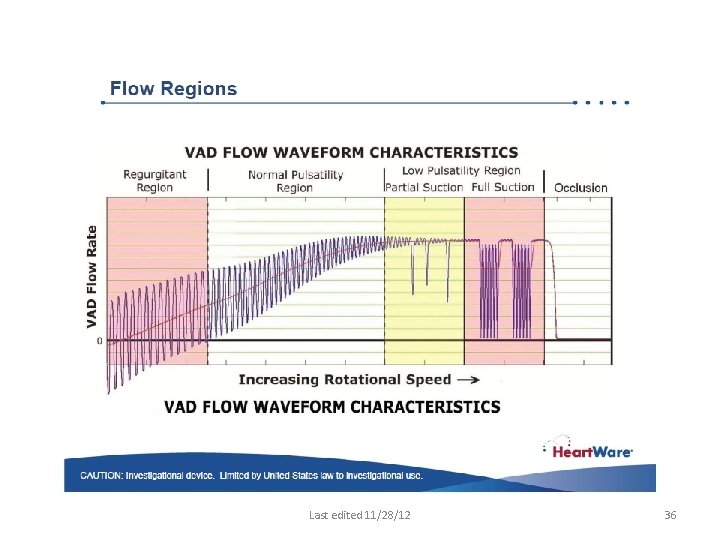
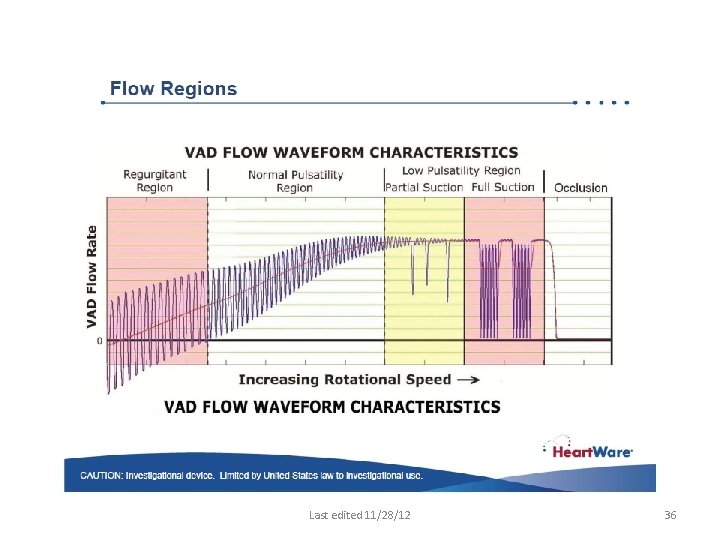
Last edited 11/28/12 36
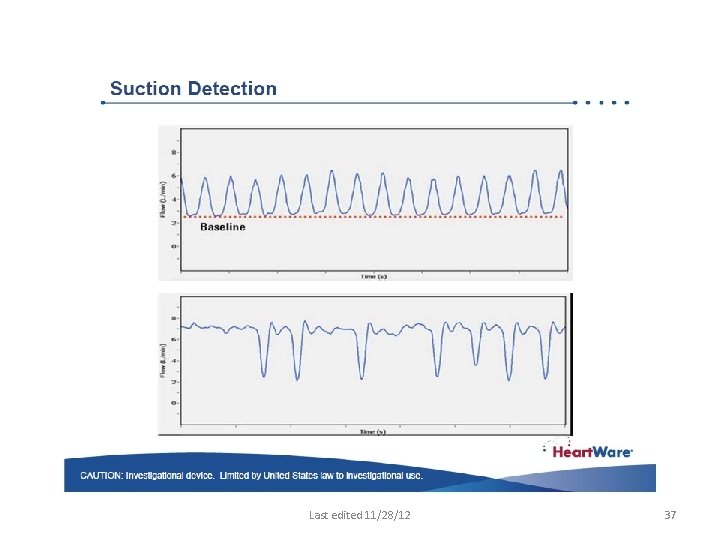
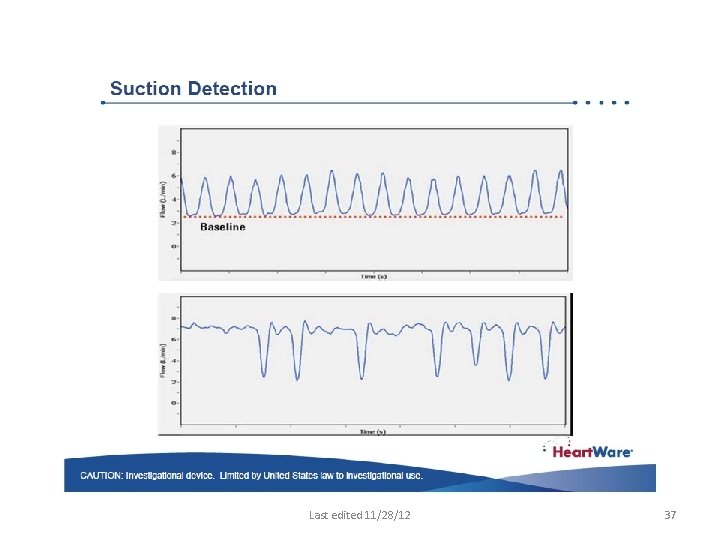
Last edited 11/28/12 37
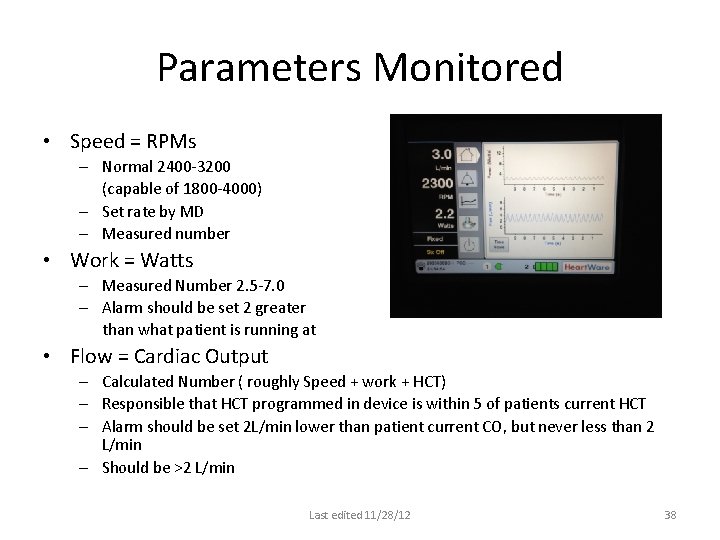
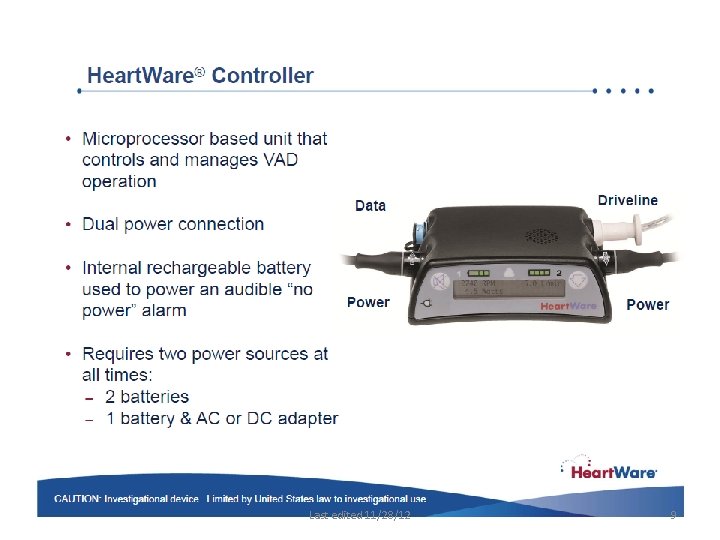
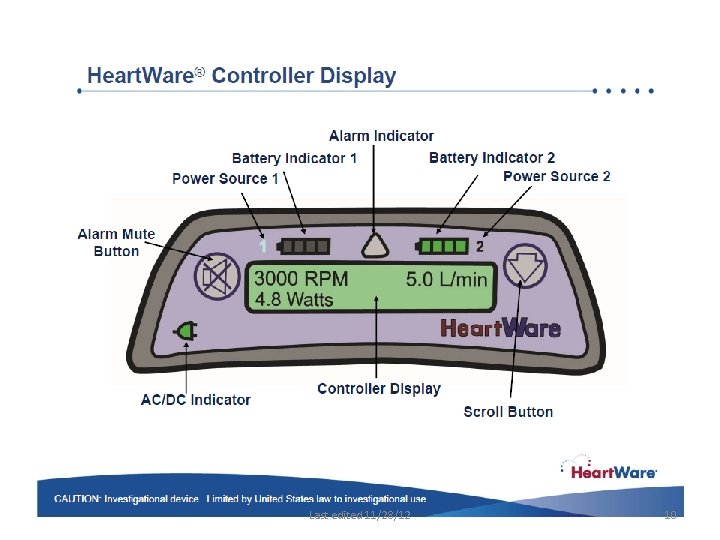
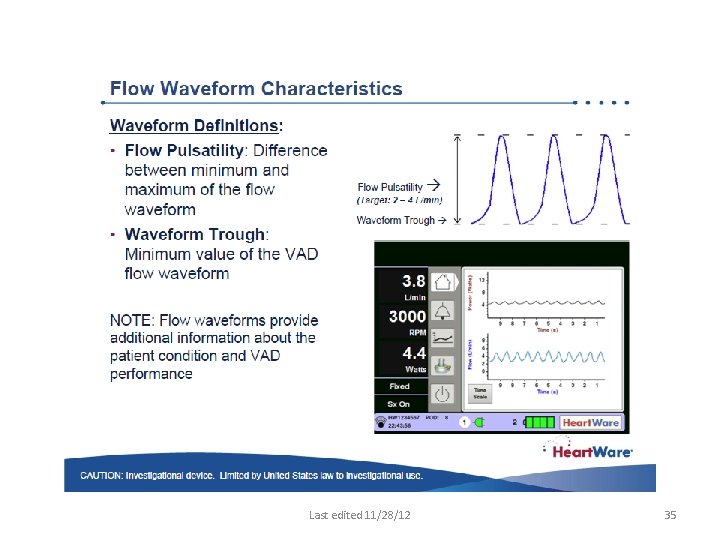
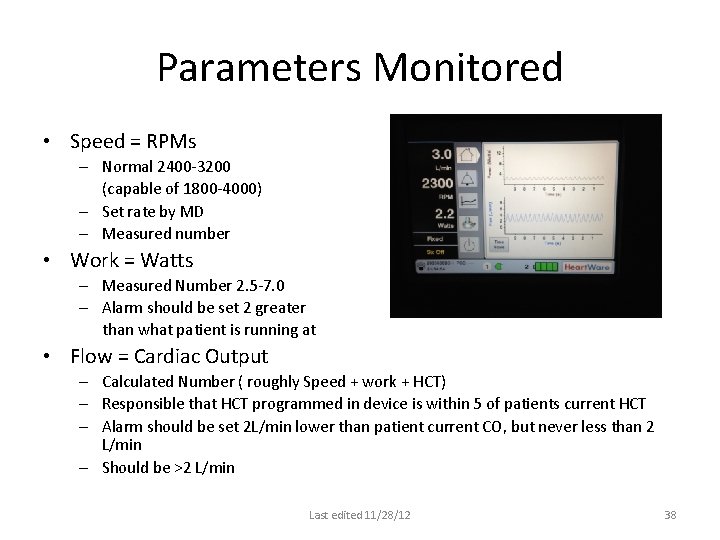
Parameters Monitored • Speed = RPMs – Normal 2400 -3200 (capable of 1800 -4000) – Set rate by MD – Measured number • Work = Watts – Measured Number 2. 5 -7. 0 – Alarm should be set 2 greater than what patient is running at • Flow = Cardiac Output – Calculated Number ( roughly Speed + work + HCT) – Responsible that HCT programmed in device is within 5 of patients current HCT – Alarm should be set 2 L/min lower than patient current CO, but never less than 2 L/min – Should be >2 L/min Last edited 11/28/12 38

Management post-operatively and beyond • Control hypertension –maintain MAP < 90 mm. Hg*** • Continuous flow pumps are preload dependent and sensitive to increased afterload. • ALWAYS : Consider clinical (patient) related changes when assessing changes in pump flow • Fluids are given to maintain pump flow index at greater than 2. 0 L/min/m 2 with central venous pressure and left atrial pressure less than 20 mm. Hg • Vasopressors and/or vasodilators can be used as required to adjust vascular tone • Patients may require inotropic assistance of right ventricular function Last edited 11/28/12 39
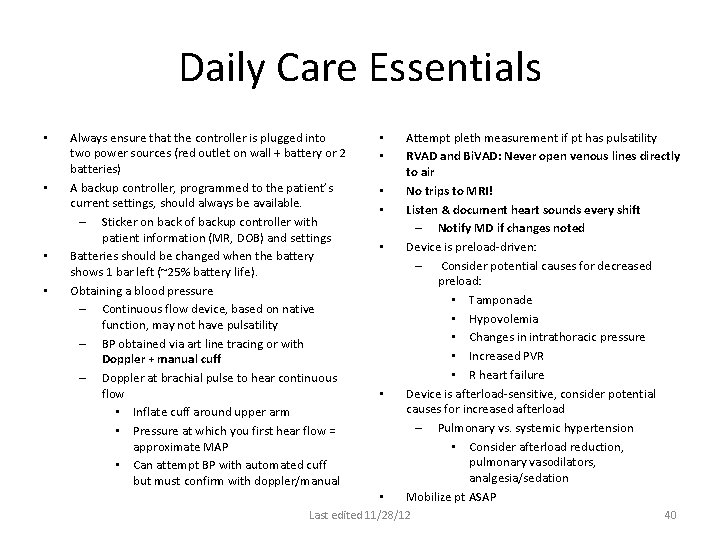
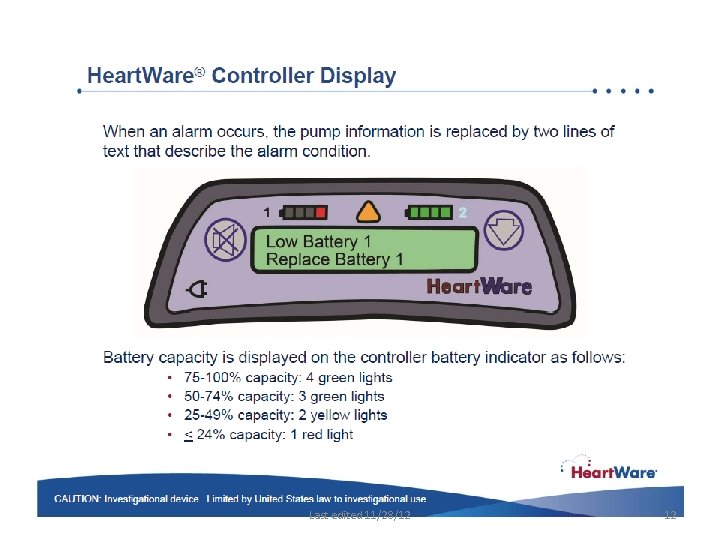
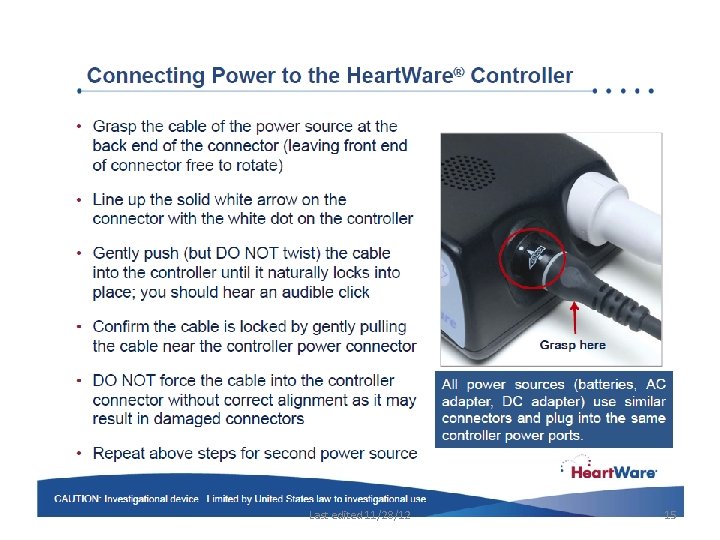
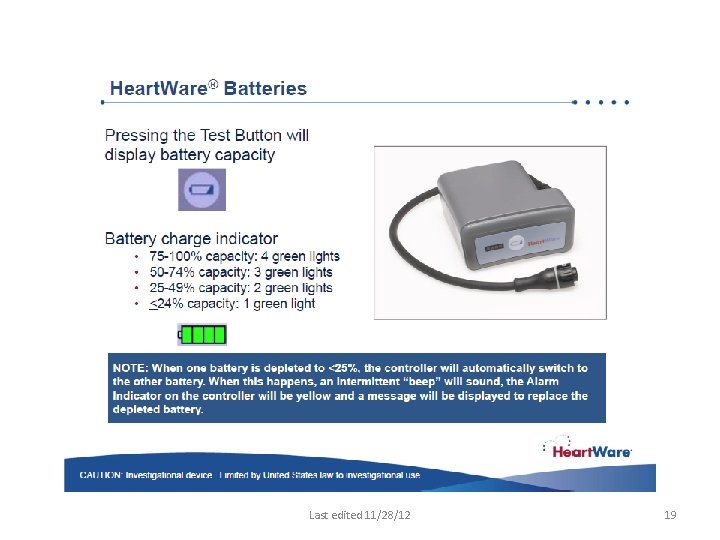
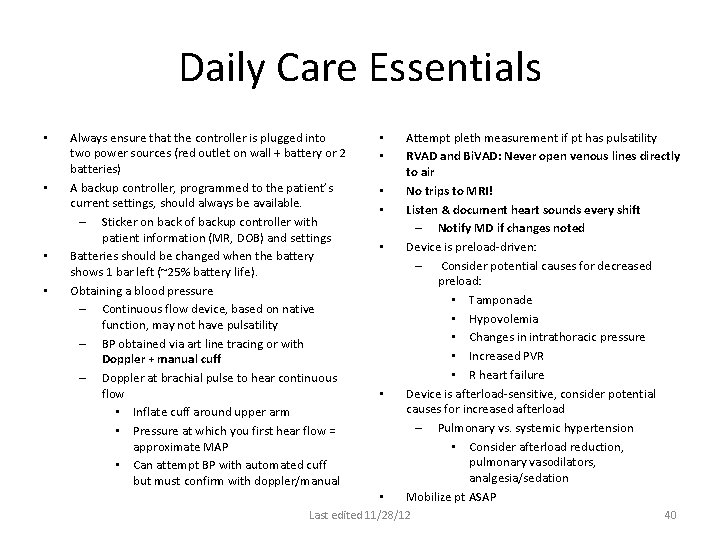
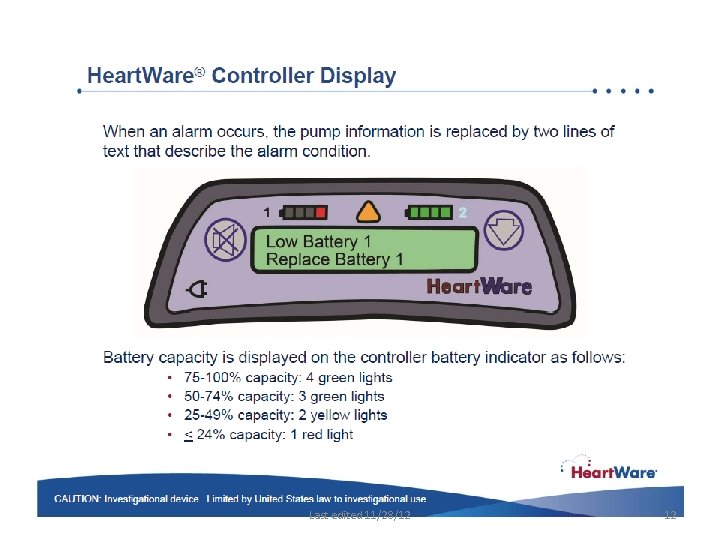
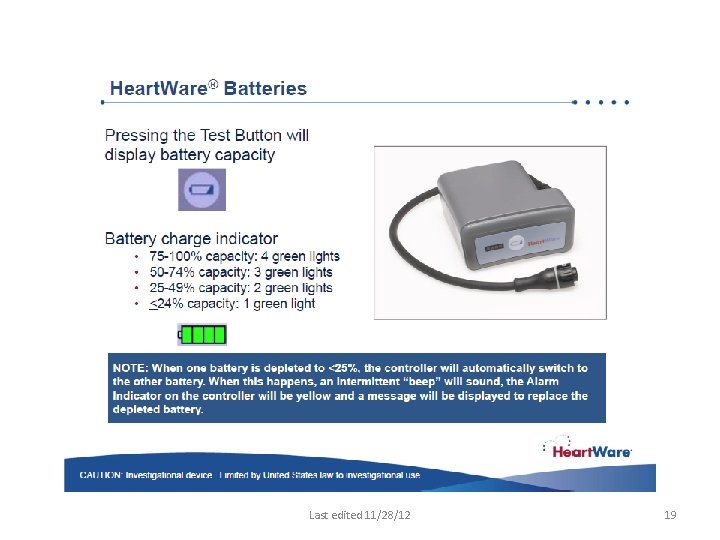
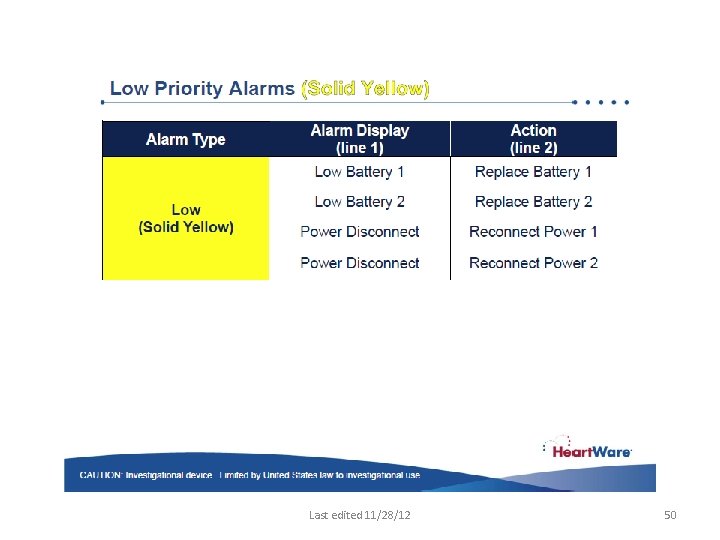
Daily Care Essentials • • Always ensure that the controller is plugged into two power sources (red outlet on wall + battery or 2 batteries) A backup controller, programmed to the patient’s current settings, should always be available. – Sticker on back of backup controller with patient information (MR, DOB) and settings Batteries should be changed when the battery shows 1 bar left (~25% battery life). Obtaining a blood pressure – Continuous flow device, based on native function, may not have pulsatility – BP obtained via art line tracing or with Doppler + manual cuff – Doppler at brachial pulse to hear continuous flow • Inflate cuff around upper arm • Pressure at which you first hear flow = approximate MAP • Can attempt BP with automated cuff but must confirm with doppler/manual • • Attempt pleth measurement if pt has pulsatility RVAD and Bi. VAD: Never open venous lines directly to air No trips to MRI! Listen & document heart sounds every shift – Notify MD if changes noted Device is preload-driven: – Consider potential causes for decreased preload: • Tamponade • Hypovolemia • Changes in intrathoracic pressure • Increased PVR • R heart failure Device is afterload-sensitive, consider potential causes for increased afterload – Pulmonary vs. systemic hypertension • Consider afterload reduction, pulmonary vasodilators, analgesia/sedation Mobilize pt ASAP Last edited 11/28/12 40
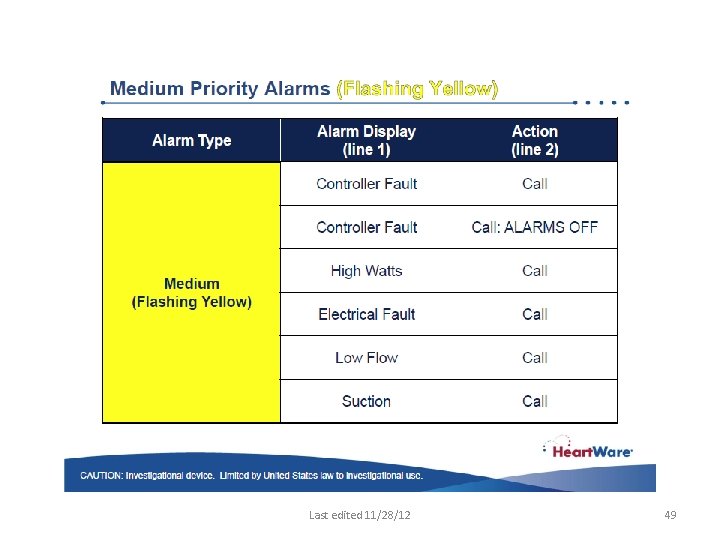
Nursing considerations • Notify MD of suction events, even if intermittent • Check Alarm Limits (on sticker; changed by MD in system) – High Power alarm 2 watts above average power – Low flow alarm 2 L/min below average flow (minimum set 2 L/min) • Assure correct HCT is programmed for CO calculation Last edited 11/28/12 41
Arrhythmias/Emergency Procedures • Arrhythmias may occur in the post-operative period • OK to defibrillate Heart. Ware® System patients • Anti-arrhythmic drugs, pacemakers, and ICDs are compatible with the Heart. Ware System • Institute appropriate PALS/ACLS protocols • If chest compressions have been administered, confirm function and positioning of HVAD® pump Last edited 11/28/12 42
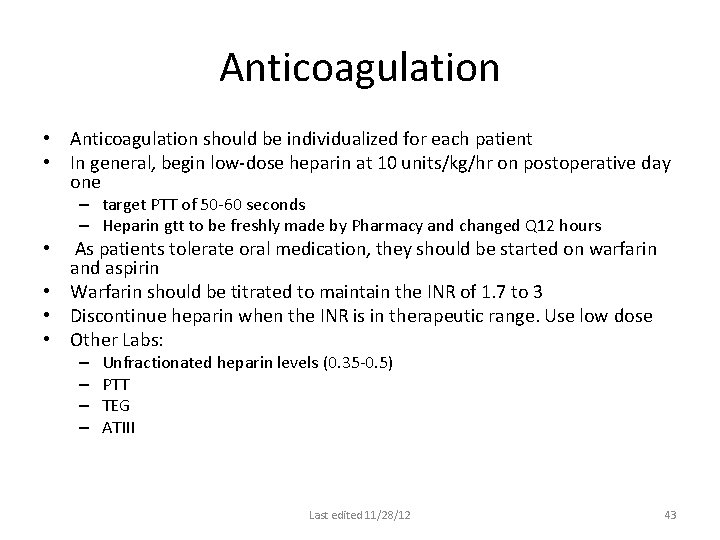
Anticoagulation • Anticoagulation should be individualized for each patient • In general, begin low-dose heparin at 10 units/kg/hr on postoperative day one – target PTT of 50 -60 seconds – Heparin gtt to be freshly made by Pharmacy and changed Q 12 hours As patients tolerate oral medication, they should be started on warfarin and aspirin • Warfarin should be titrated to maintain the INR of 1. 7 to 3 • Discontinue heparin when the INR is in therapeutic range. Use low dose • Other Labs: • – – Unfractionated heparin levels (0. 35 -0. 5) PTT TEG ATIII Last edited 11/28/12 43
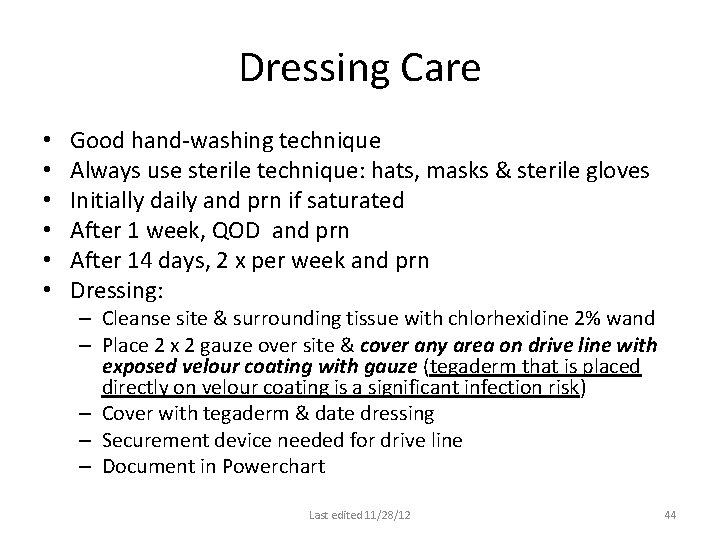
Dressing Care • • • Good hand-washing technique Always use sterile technique: hats, masks & sterile gloves Initially daily and prn if saturated After 1 week, QOD and prn After 14 days, 2 x per week and prn Dressing: – Cleanse site & surrounding tissue with chlorhexidine 2% wand – Place 2 x 2 gauze over site & cover any area on drive line with exposed velour coating with gauze (tegaderm that is placed directly on velour coating is a significant infection risk) – Cover with tegaderm & date dressing – Securement device needed for drive line – Document in Powerchart Last edited 11/28/12 44
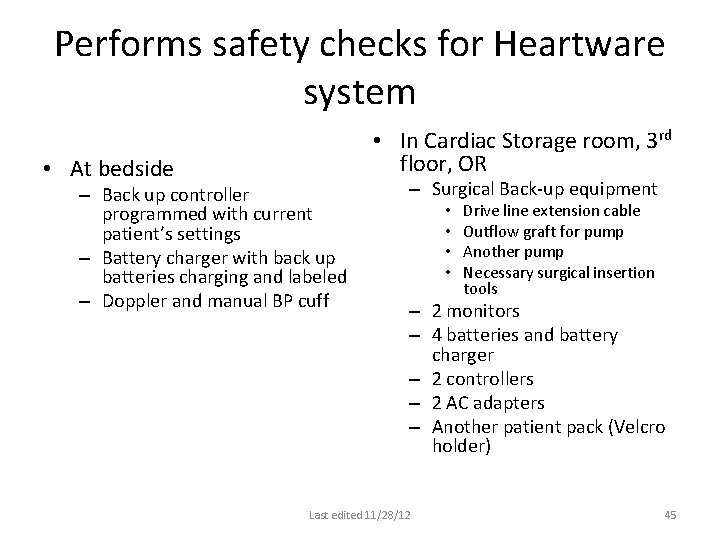
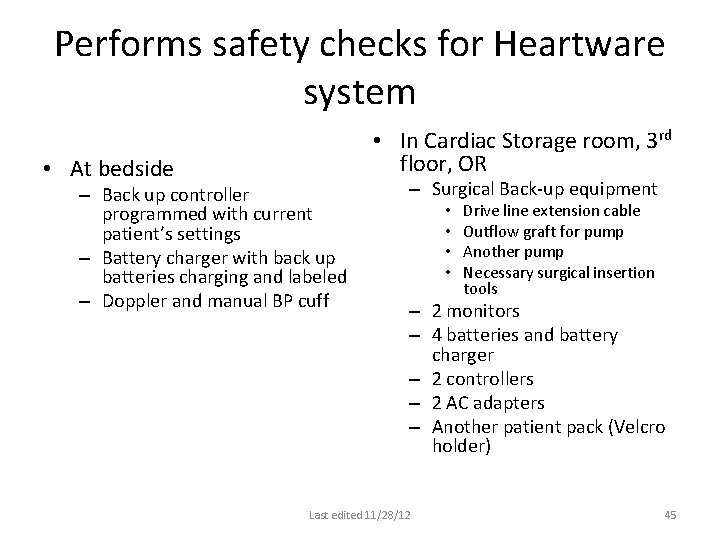
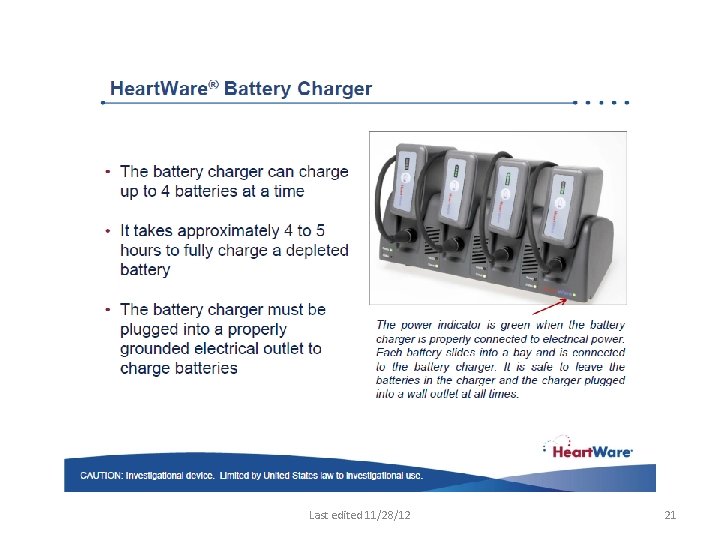
Performs safety checks for Heartware system • At bedside • In Cardiac Storage room, 3 rd floor, OR – Back up controller programmed with current patient’s settings – Battery charger with back up batteries charging and labeled – Doppler and manual BP cuff – Surgical Back-up equipment • • Drive line extension cable Outflow graft for pump Another pump Necessary surgical insertion tools – 2 monitors – 4 batteries and battery charger – 2 controllers – 2 AC adapters – Another patient pack (Velcro holder) Last edited 11/28/12 45
Last edited 11/28/12 46

Last edited 11/28/12 47
Last edited 11/28/12 48
Last edited 11/28/12 49
Last edited 11/28/12 50
Trouble shooting Page “LVAD” for heart failure team www. heartware. com cs@heartwearinc. com Heartware 205 Newbury Street, Suite 101 Framingham, MA 01701 24 - Hour Clinical Support 888. 494. 6365 Last edited 11/28/12 51