HEART FAILURE WITH PRESERVED LEFT VENTRICULAR FUNCTION HFPEF


- Slides: 26
HEART FAILURE WITH PRESERVED LEFT VENTRICULAR FUNCTION "HFPEF" David Kraus, MD, FACP, FACC, FSCAI Board Certified in Advanced Heart Failure and Transplant Medicine

DISCLOSURE David H. Kraus, MD, FACC Stern Cardiovascular Foundation I have the following personal financial relationships with commercial interests to disclose: Amgen Pharmaceutical - Speaker’s Bureau
HFPEF - Definition • HFPEF: "Defined as a clinical syndrome in which the heart is unable to deliver the requisite amount of oxygen to the tissues commensurate with their metabolic needs - but does so at the expense of increased left ventricular filling pressures - Despite a Normal Ejection Fraction" • OTHER TERMS for HFPEF: – Backwards Heart Failure – Diastolic Heart Failure
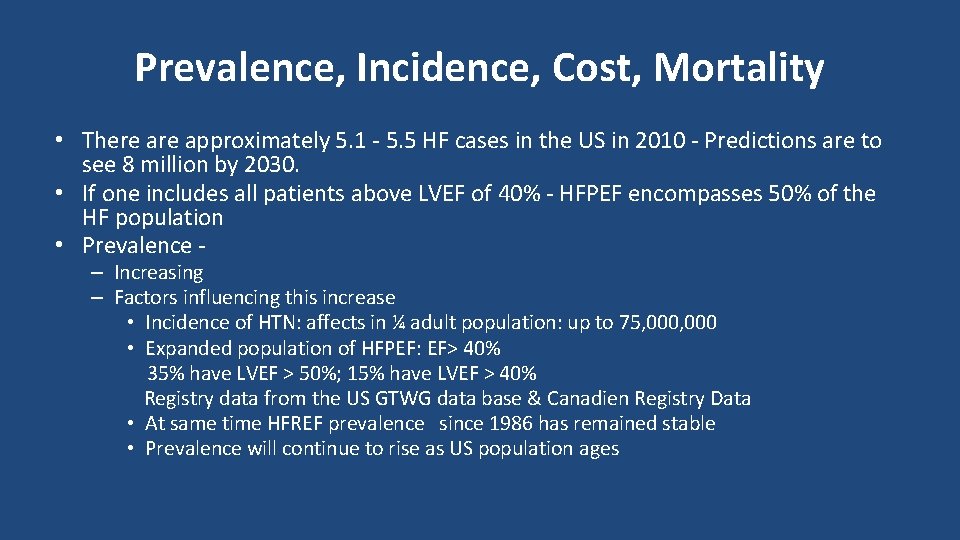
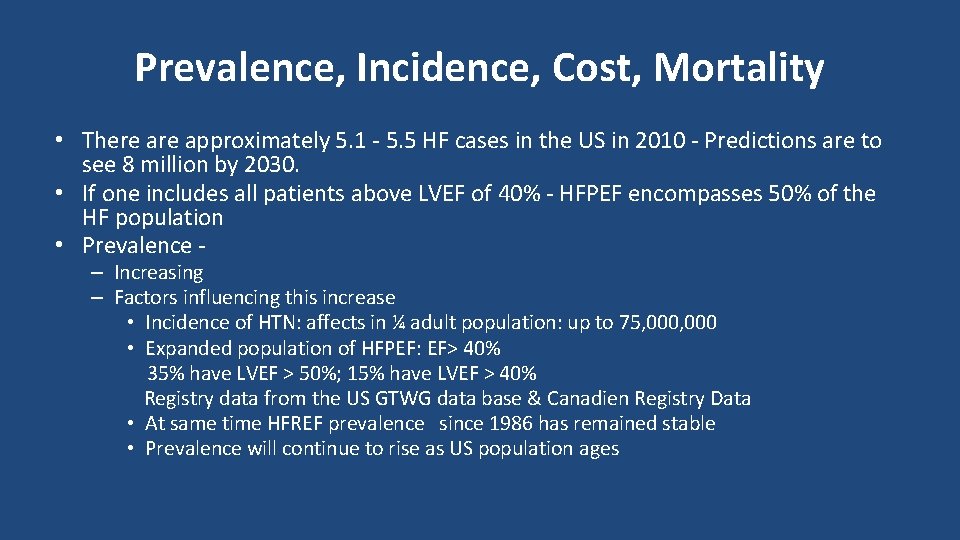
Prevalence, Incidence, Cost, Mortality • There approximately 5. 1 - 5. 5 HF cases in the US in 2010 - Predictions are to see 8 million by 2030. • If one includes all patients above LVEF of 40% - HFPEF encompasses 50% of the HF population • Prevalence – Increasing – Factors influencing this increase • Incidence of HTN: affects in ¼ adult population: up to 75, 000 • Expanded population of HFPEF: EF> 40% 35% have LVEF > 50%; 15% have LVEF > 40% Registry data from the US GTWG data base & Canadien Registry Data • At same time HFREF prevalence since 1986 has remained stable • Prevalence will continue to rise as US population ages
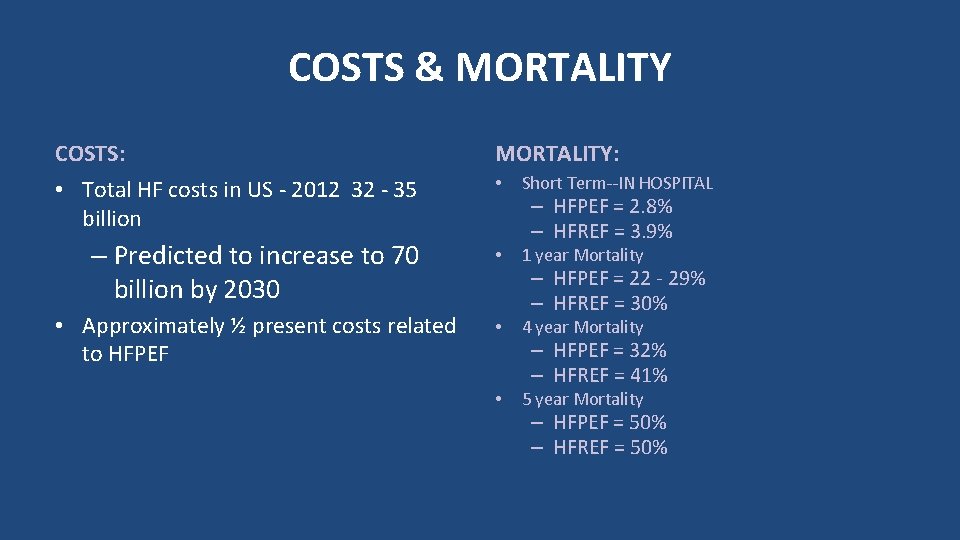
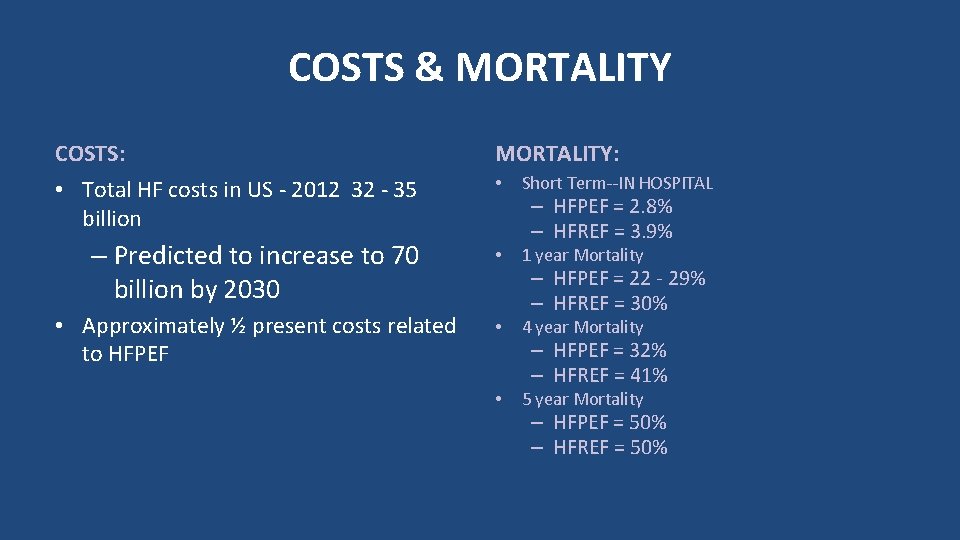
COSTS & MORTALITY COSTS: • Total HF costs in US - 2012 32 - 35 billion MORTALITY: • Short Term--IN HOSPITAL – Predicted to increase to 70 billion by 2030 • 1 year Mortality • Approximately ½ present costs related to HFPEF • 4 year Mortality • 5 year Mortality – HFPEF = 2. 8% – HFREF = 3. 9% – HFPEF = 22 - 29% – HFREF = 30% – HFPEF = 32% – HFREF = 41% – HFPEF = 50% – HFREF = 50%
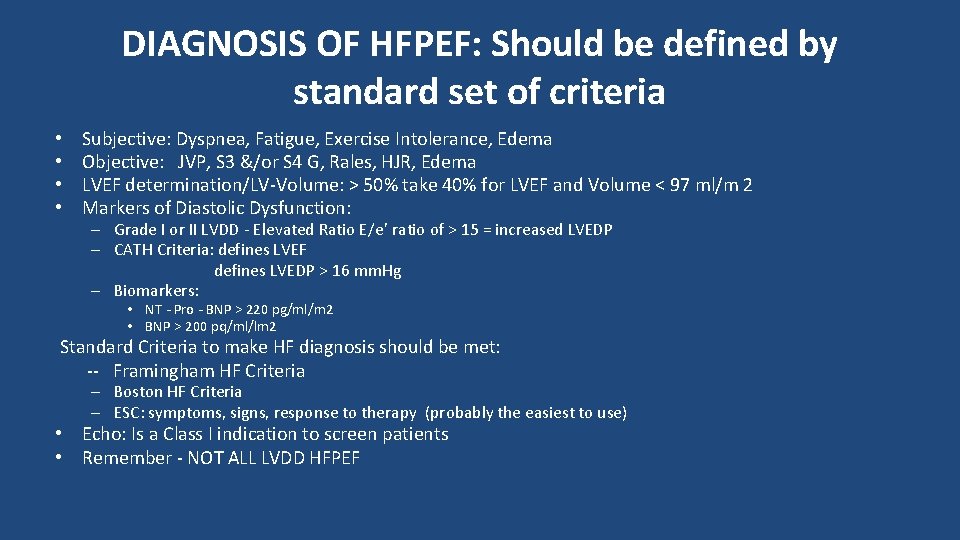
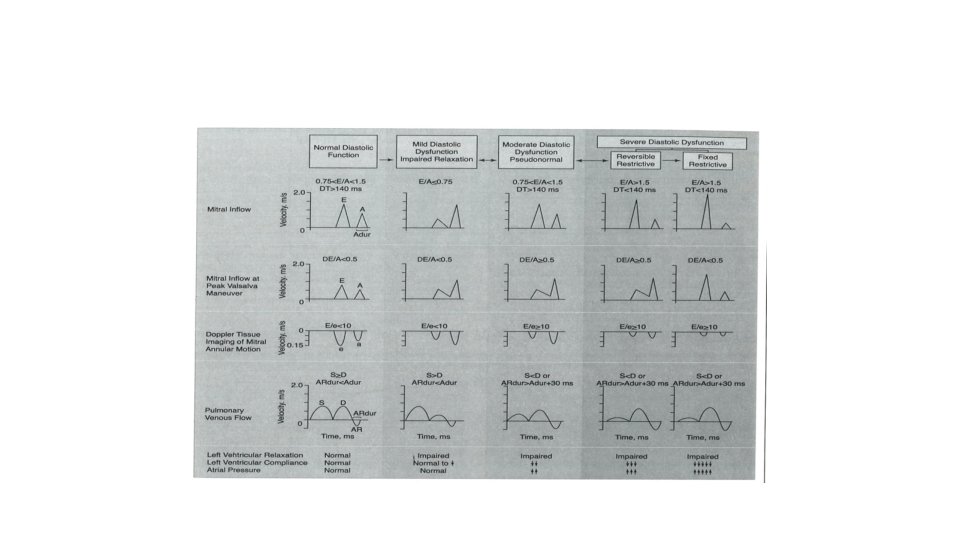
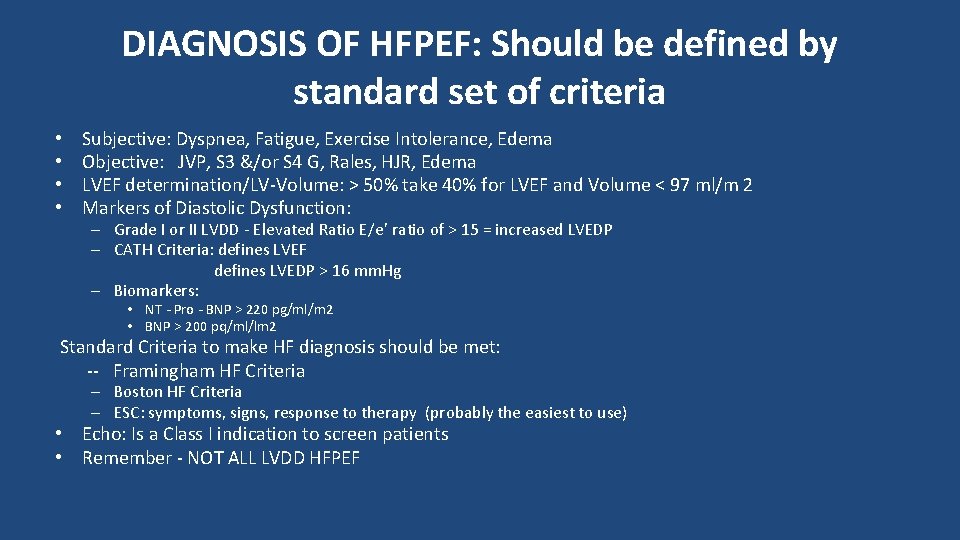
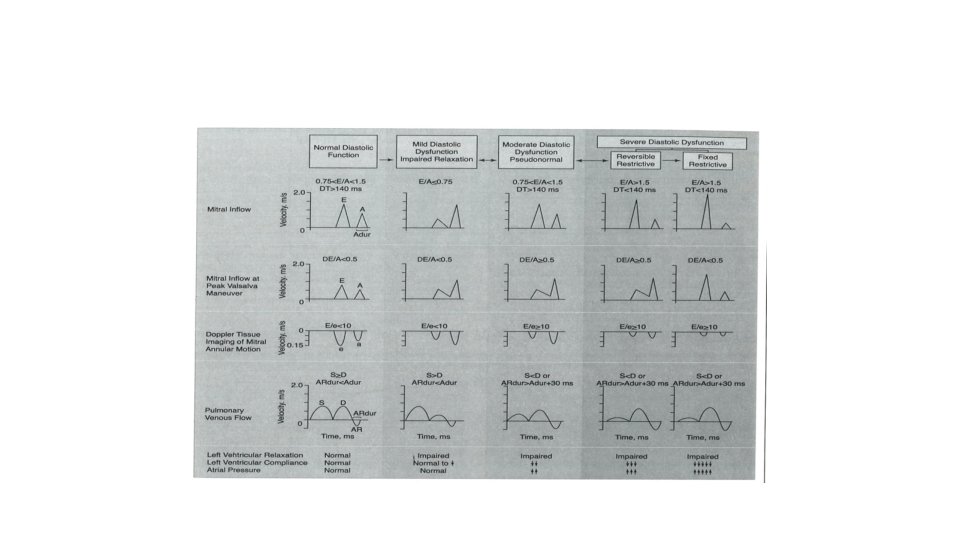
DIAGNOSIS OF HFPEF: Should be defined by standard set of criteria • • Subjective: Dyspnea, Fatigue, Exercise Intolerance, Edema Objective: JVP, S 3 &/or S 4 G, Rales, HJR, Edema LVEF determination/LV-Volume: > 50% take 40% for LVEF and Volume < 97 ml/m 2 Markers of Diastolic Dysfunction: – Grade I or II LVDD - Elevated Ratio E/e’ ratio of > 15 = increased LVEDP – CATH Criteria: defines LVEF defines LVEDP > 16 mm. Hg – Biomarkers: • NT - Pro - BNP > 220 pg/ml/m 2 • BNP > 200 pq/ml/lm 2 Standard Criteria to make HF diagnosis should be met: -- Framingham HF Criteria – Boston HF Criteria – ESC: symptoms, signs, response to therapy (probably the easiest to use) • Echo: Is a Class I indication to screen patients • Remember - NOT ALL LVDD HFPEF
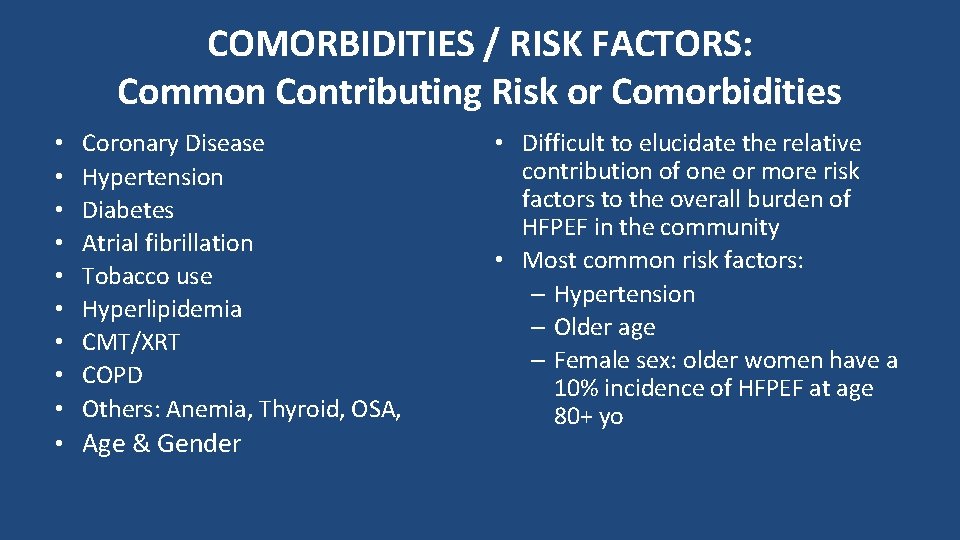
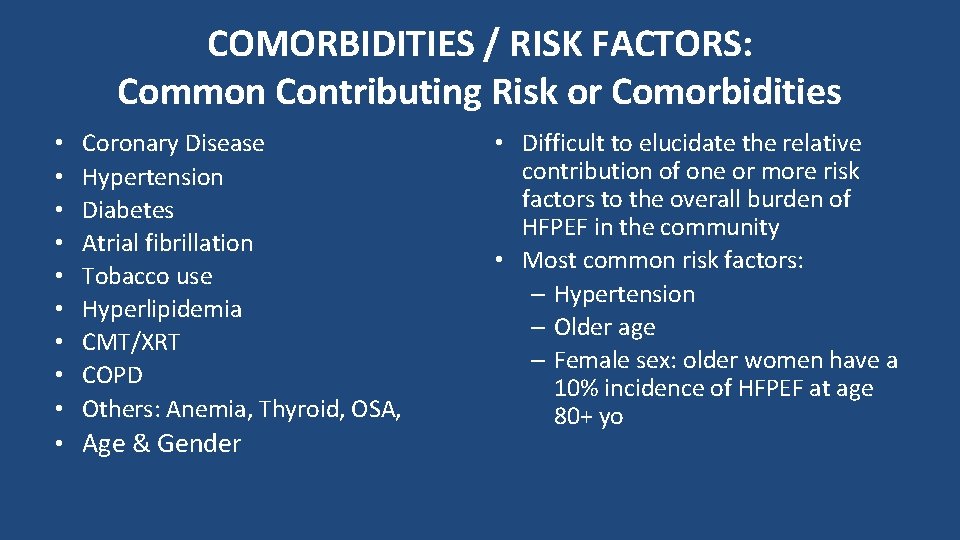
COMORBIDITIES / RISK FACTORS: Common Contributing Risk or Comorbidities • • • Coronary Disease Hypertension Diabetes Atrial fibrillation Tobacco use Hyperlipidemia CMT/XRT COPD Others: Anemia, Thyroid, OSA, Age & Gender • Difficult to elucidate the relative contribution of one or more risk factors to the overall burden of HFPEF in the community • Most common risk factors: – Hypertension – Older age – Female sex: older women have a 10% incidence of HFPEF at age 80+ yo
Risk Factors & Mortality / Readmissions Mortality: Risk Factors in Severity: Framingham Data Base • PAH, Liver Failure, Renal Failure • Coronary Disease: leads to abnormality in relaxation • Valvular: leads to higher LVEDP via volume overload as with MR or stenosis as with AS • Female Risk: goes up primarily via a microvascular process vs younger patients with obstructive CAD - developing HFr. EF from a macro-vascular etiology • READMISSIONS: Most (50%) are because of non HF reasons - are secondary to comorbid conditions - or from falls, sepsis ( the usual bad actors) Important Points To Remember • Difficult to elucidate relative contribution of each Risk Factor independently • Risk factors vary within the domain of HFPEF patients , likely act conjointly and synergistically • FINAL COMMON PATHWAY: – INFLAMMATION at the cardiac or vascular level from the underlying comorbid etiology or etiologies.
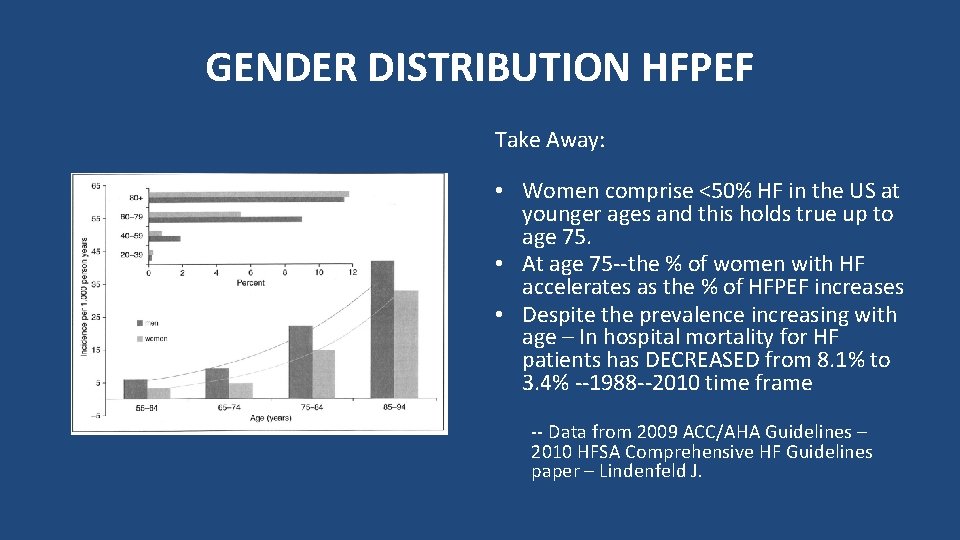
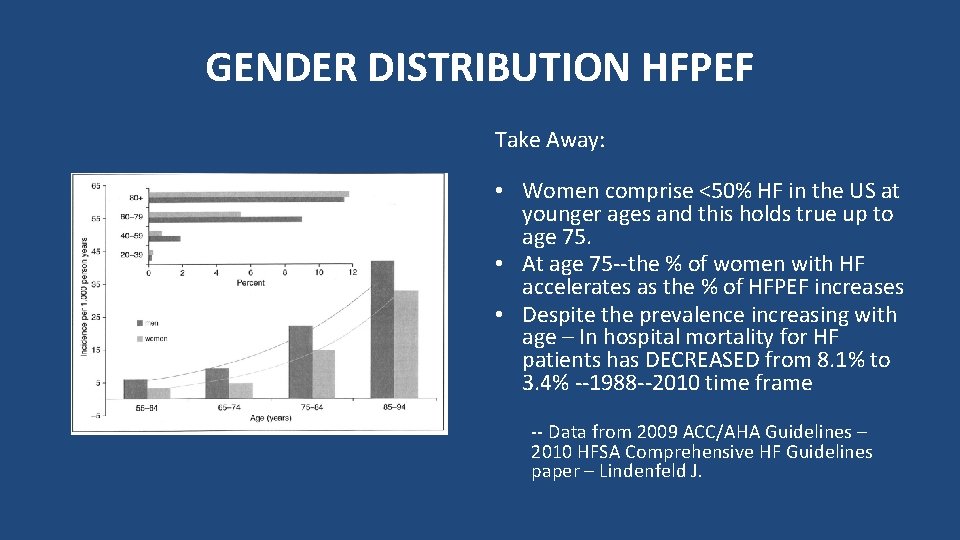
GENDER DISTRIBUTION HFPEF Take Away: • Women comprise <50% HF in the US at younger ages and this holds true up to age 75. • At age 75 --the % of women with HF accelerates as the % of HFPEF increases • Despite the prevalence increasing with age – In hospital mortality for HF patients has DECREASED from 8. 1% to 3. 4% --1988 --2010 time frame -- Data from 2009 ACC/AHA Guidelines – 2010 HFSA Comprehensive HF Guidelines paper – Lindenfeld J.
HFPEF Presentation CONGESTION Warm & dry Warm & wet Cold & dry Cold & wet No LOW PERFUSION Yes Evidence for low perfusion 92% of patients present warm & wet with HFPEF 72% of patients present warm & wet with HFREF
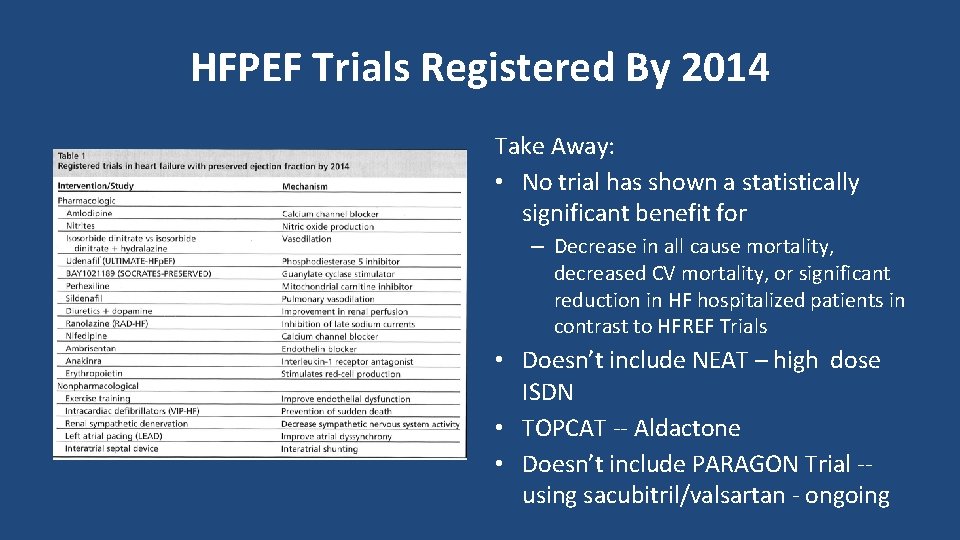
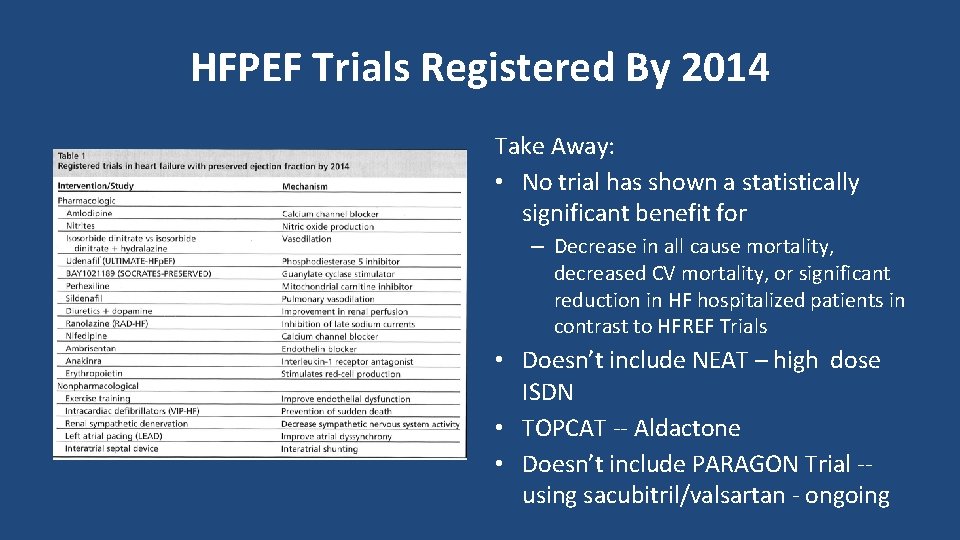
HFPEF Trials Registered By 2014 Take Away: • No trial has shown a statistically significant benefit for – Decrease in all cause mortality, decreased CV mortality, or significant reduction in HF hospitalized patients in contrast to HFREF Trials • Doesn’t include NEAT – high dose ISDN • TOPCAT -- Aldactone • Doesn’t include PARAGON Trial -using sacubitril/valsartan - ongoing
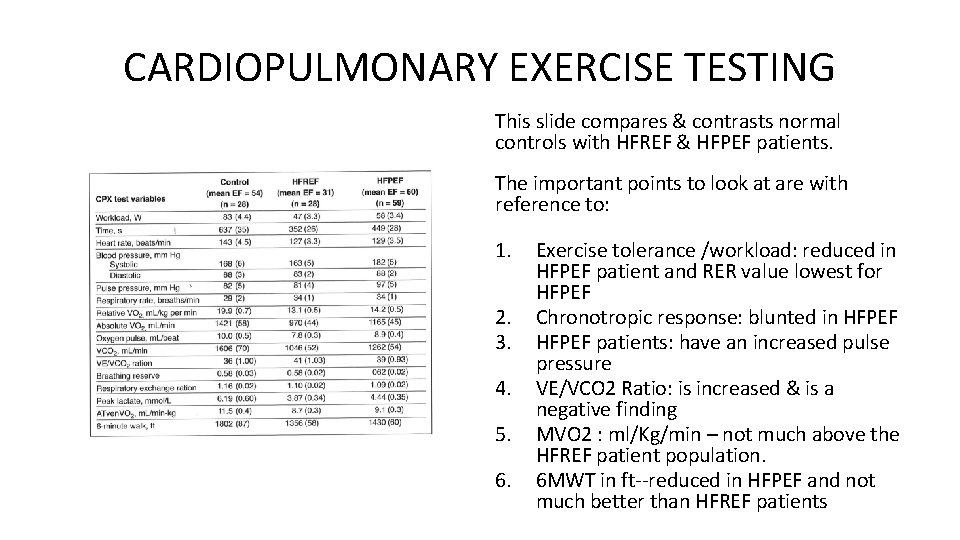
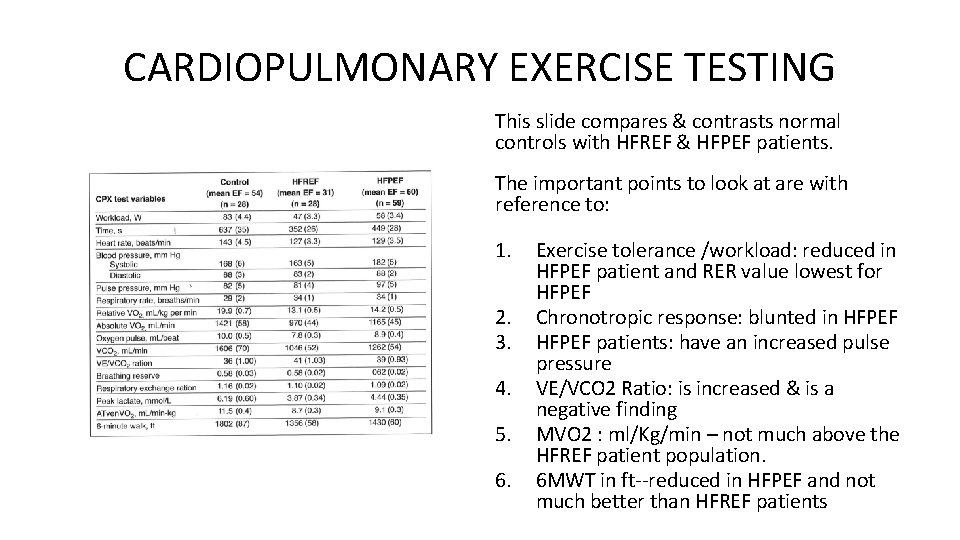
CARDIOPULMONARY EXERCISE TESTING This slide compares & contrasts normal controls with HFREF & HFPEF patients. The important points to look at are with reference to: 1. 2. 3. 4. 5. 6. Exercise tolerance /workload: reduced in HFPEF patient and RER value lowest for HFPEF Chronotropic response: blunted in HFPEF patients: have an increased pulse pressure VE/VCO 2 Ratio: is increased & is a negative finding MVO 2 : ml/Kg/min – not much above the HFREF patient population. 6 MWT in ft--reduced in HFPEF and not much better than HFREF patients
HFPEF And Ventricular Arterial Coupling • The normal physiology between the heart and vascular system relates back to the heart being able to generate a normal stroke volume from the heart to vascular tree • This coupling maintains continuous blood flow without exaggerated BP fluctuations – maintains tissue perfusion • When increase in demand is needed, in the normal functioning heart – this can be met by increasing the SV without increasing LVEDP significantly • This process is altered in HFPEF patients • HFPEF IS NOT JUST A PROBLEM OF VOLUME OVERLOAD.
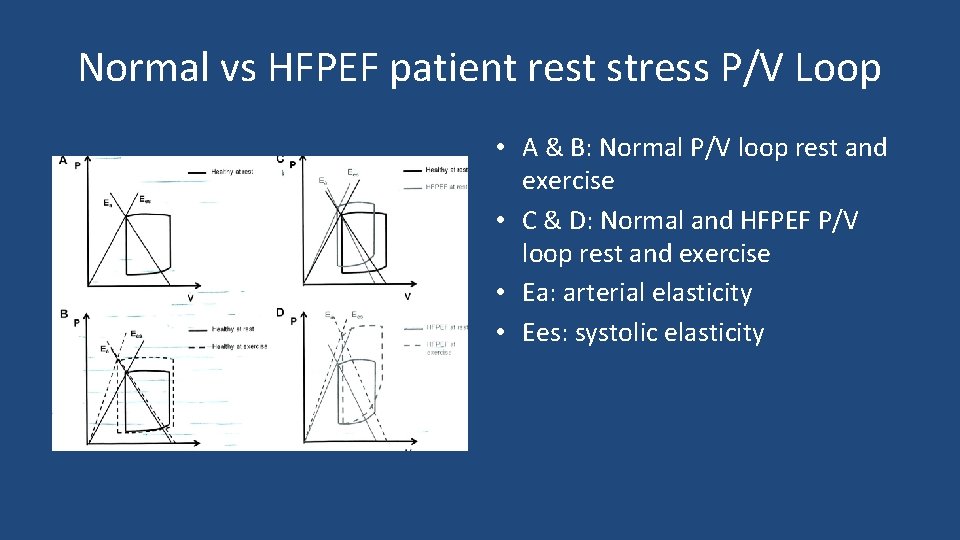
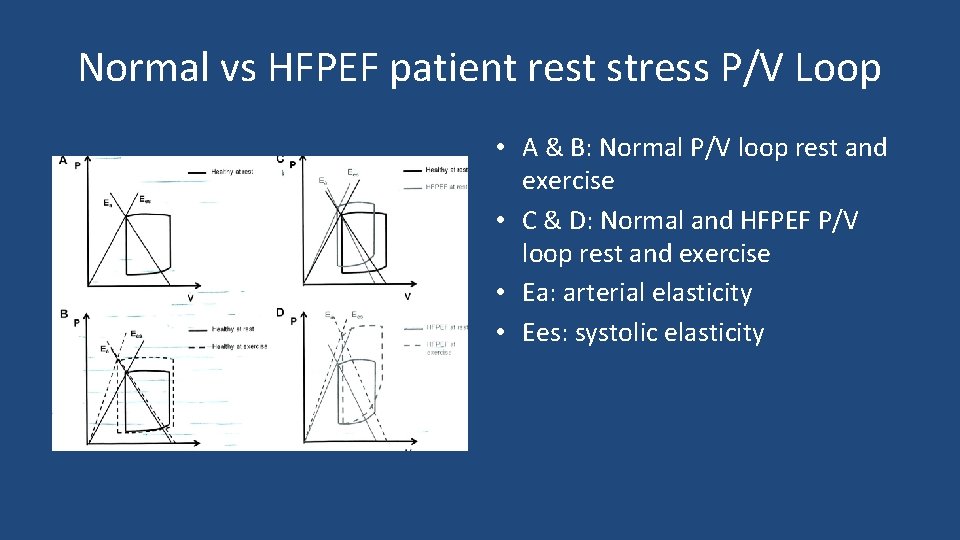
Normal vs HFPEF patient rest stress P/V Loop • A & B: Normal P/V loop rest and exercise • C & D: Normal and HFPEF P/V loop rest and exercise • Ea: arterial elasticity • Ees: systolic elasticity
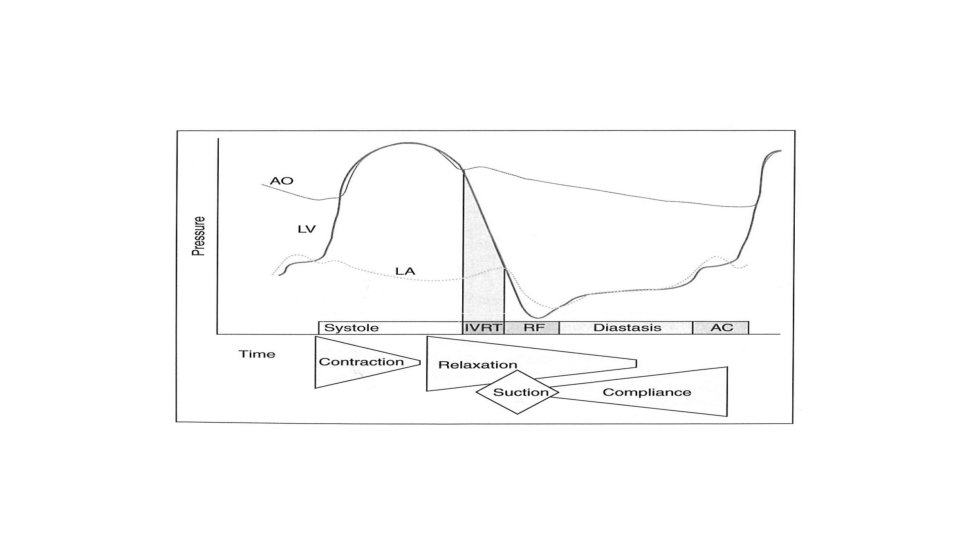
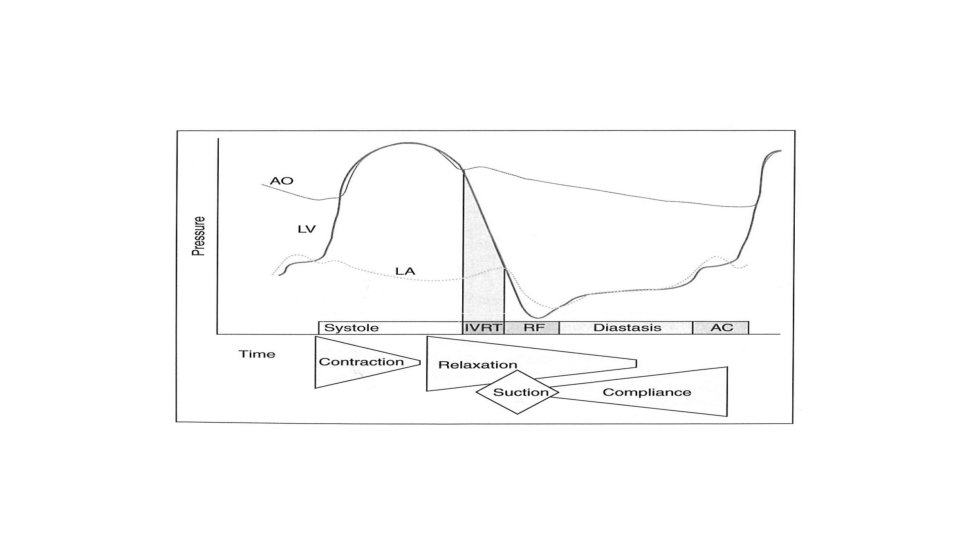
DIASTOLIC DYSFUNCTION IN HFPEF • • • Slowed LV relaxation Enhanced LV stiffness: echo criteria Reduced Ventricular Resting Forces – Calcium flux Diastolic suction – impairment Ventricular dysynchrony – Monitored by speckled tracking and echo looking at torsion, untwisting and longitudinal motion during contraction and relaxation.
VENTRICULAR SUCTION • During IVR period: LV pressure is • HFPEF: lower than LA pressure and helps 1. Reduction in adrenergic stimulation/ signaling drive blood into the LV- apex 2. One sees a mild increase in LVEDP • Adrenergic Stimulation: increased at rest altering elastic recoil at this interval and leads to a 3. Combination of a decrease in the progressive intraventricular LV pressure differential and pressure difference from base to reduced elasticity leads to a the LV apex marked rise in exercise LVEDP and symptoms ensue • Heart becomes a “Dynamic Suction Pump”
HFPEF: Chronotropic Incompetence • CPXT / ETT show blunted HR response to routine graded exercise • This reduced chronotropic response combined with abnormalities at the myocardial level leads to an increased LVEDP and this results in varying degrees of exercise intolerance • Abnormal Adrenergic Signaling – at the myocardial level may be the primary problem • HRR Time – is altered in these patients (prolonged)
HFPEF : Vascular Stiffness • Vascular compliance is decreased in HFPEF • Increase in vascular stiffness can affect both Proximal & Distal Vasculature as a consequence of Endothelial Dysfunction with decreased NO 2 delivery, abnormalities A-V O 2 extraction in the periphery and decreased soluble guanine cyclase at the cellular level - these patients do not exhibit a normal vasodilatory response to routine and or exercise related activity • Increased vascular stiffness results in augmented pulse pressure waves reflected back to heart • These augmented pulse pressure waves in combination with proximal vascular stiffness leads to impairment in systolic & diastolic LV Function
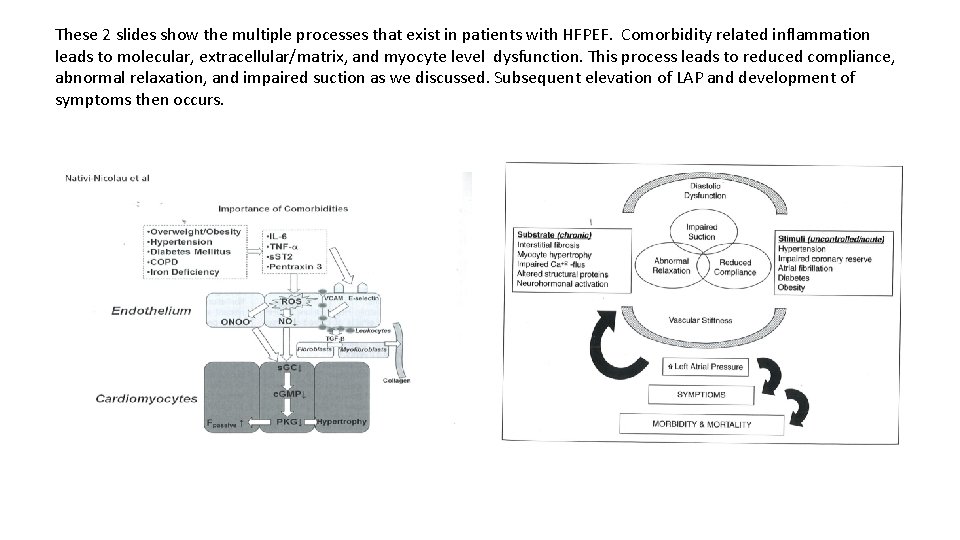
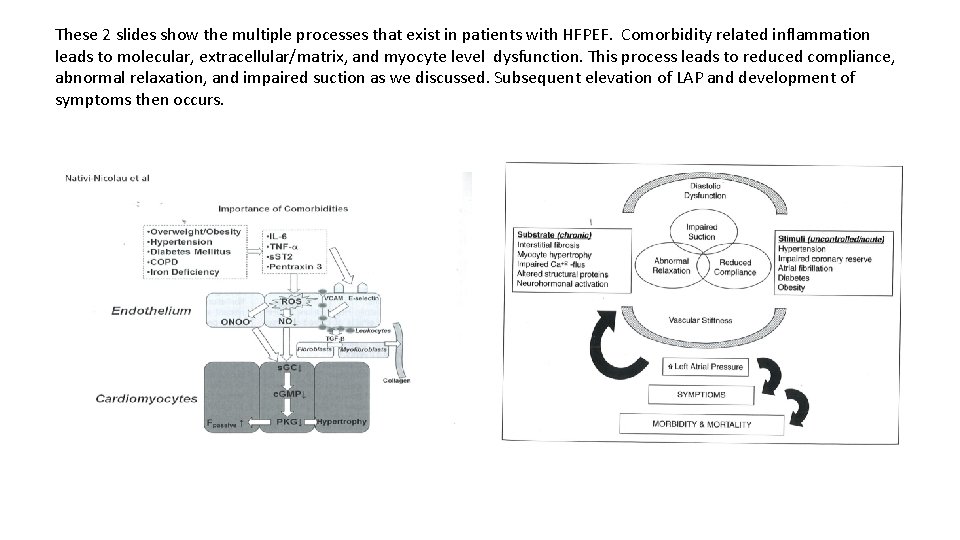
These 2 slides show the multiple processes that exist in patients with HFPEF. Comorbidity related inflammation leads to molecular, extracellular/matrix, and myocyte level dysfunction. This process leads to reduced compliance, abnormal relaxation, and impaired suction as we discussed. Subsequent elevation of LAP and development of symptoms then occurs.
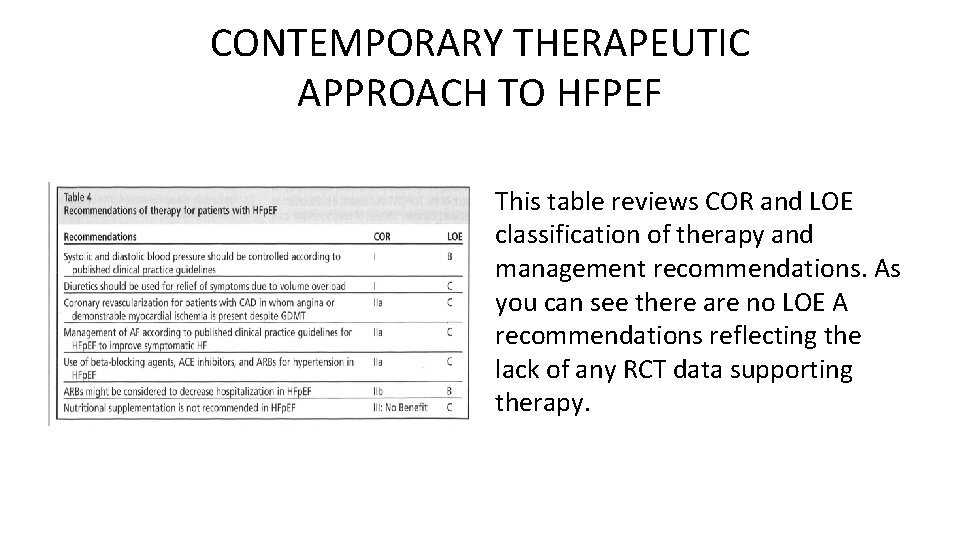
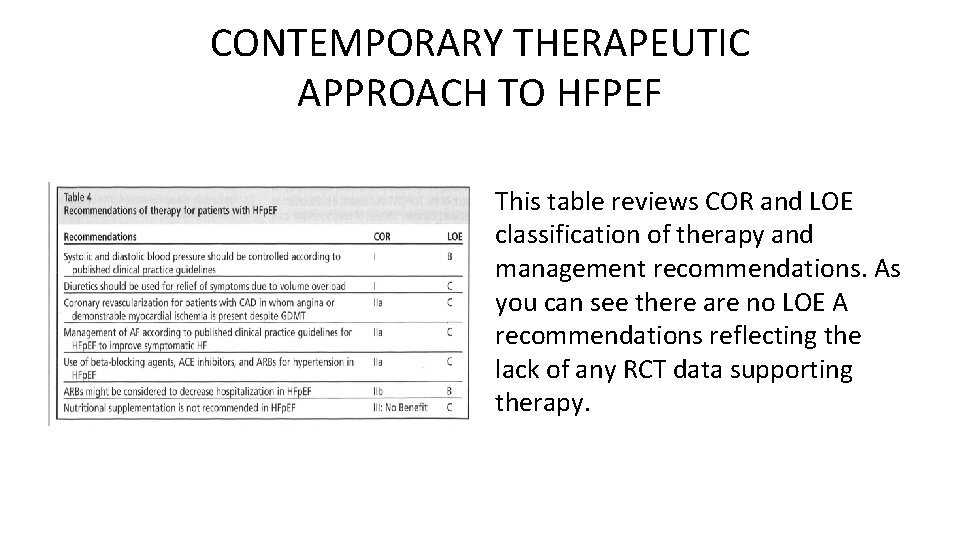
CONTEMPORARY THERAPEUTIC APPROACH TO HFPEF This table reviews COR and LOE classification of therapy and management recommendations. As you can see there are no LOE A recommendations reflecting the lack of any RCT data supporting therapy.
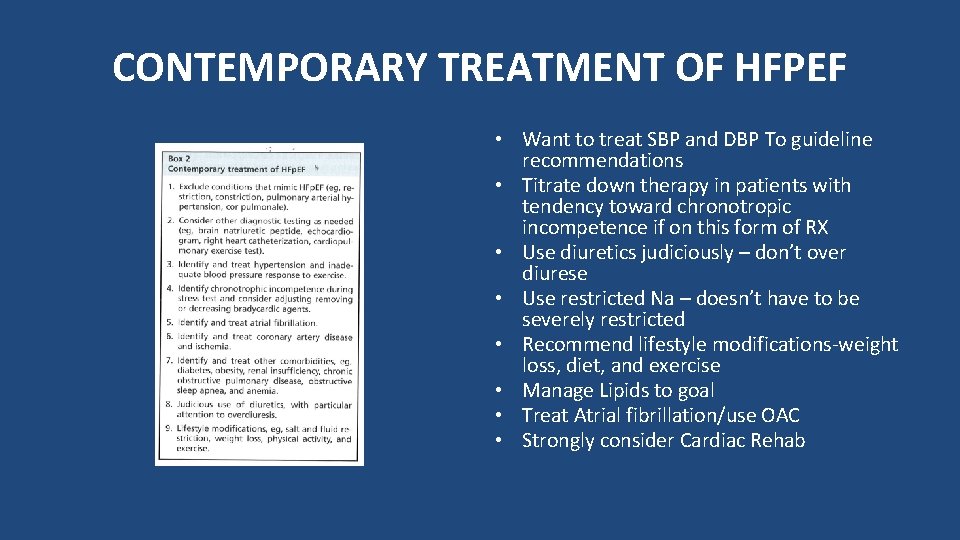
CONTEMPORARY TREATMENT OF HFPEF • Want to treat SBP and DBP To guideline recommendations • Titrate down therapy in patients with tendency toward chronotropic incompetence if on this form of RX • Use diuretics judiciously – don’t over diurese • Use restricted Na – doesn’t have to be severely restricted • Recommend lifestyle modifications-weight loss, diet, and exercise • Manage Lipids to goal • Treat Atrial fibrillation/use OAC • Strongly consider Cardiac Rehab
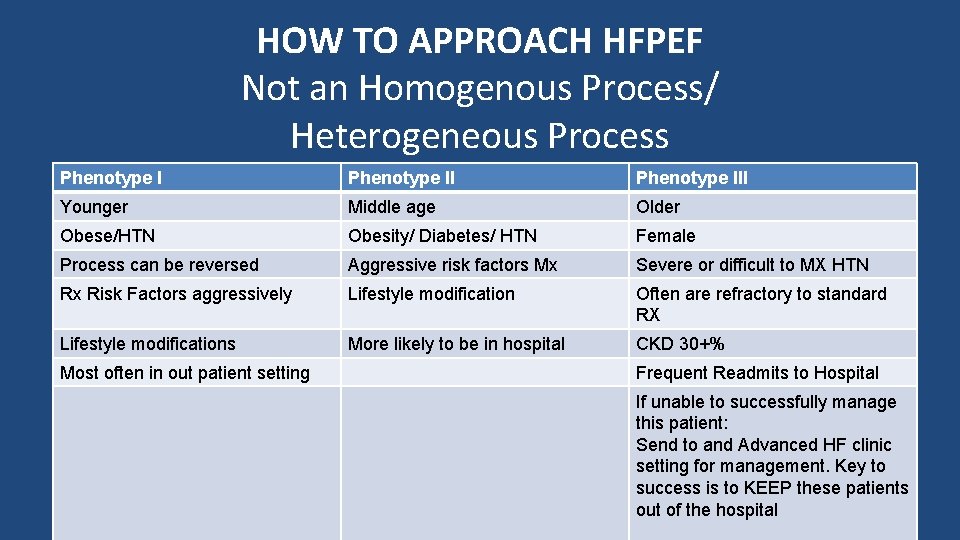
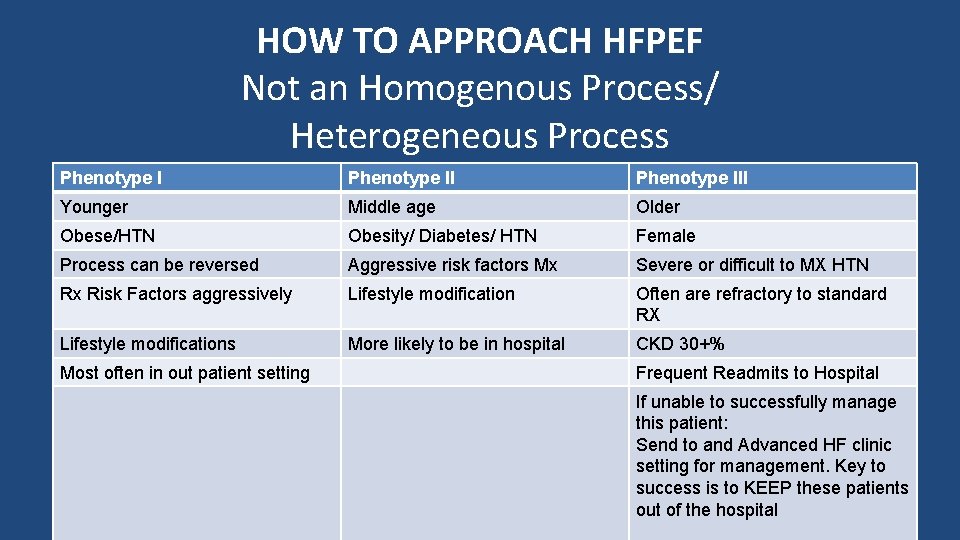
HOW TO APPROACH HFPEF Not an Homogenous Process/ Heterogeneous Process Phenotype III Younger Middle age Older Obese/HTN Obesity/ Diabetes/ HTN Female Process can be reversed Aggressive risk factors Mx Severe or difficult to MX HTN Rx Risk Factors aggressively Lifestyle modification Often are refractory to standard RX Lifestyle modifications More likely to be in hospital CKD 30+% Most often in out patient setting Frequent Readmits to Hospital If unable to successfully manage this patient: Send to and Advanced HF clinic setting for management. Key to success is to KEEP these patients out of the hospital

SUMMARY • I’d like you to think about HFPEF as more than a patient with “volume overload”. • Identify and treat all comorbidities and use standard evidence based guidelines for evaluation and management of this patient population. It is imperative to aggressively manage comorbidities. • Transitions of Care critical to the successful management of all HF patients. We need to do better with this aspect of HF care in our community. Remember with each heart failure admission the MORTALITY for a given patient increases despite all our efforts. Coordination of HF care should be a priority.
Phenotype II Obese Middle Aged Weight >400 lbs Aggressive risk factors Mx Lifestyle modification Lost more than 200 lbs and is now a Certified Trainer.