HEART FAILURE HF Heart failure is the pathophysiological

- Slides: 13
HEART FAILURE (HF) • Heart failure is the pathophysiological state in which an abnormality of cardiac function is responsible for failure of the heart to pump blood at a rate commensurate with the requirements of the metabolizing tissue, or to do so only from an elevated filling pressure. • Clinical syndrome due to different structural and functional disease of the heart leading to abnormality in filling or emptying of the left ventricle.
• Myocardial insufficiency – related to impaired contractility. Not every heart failure is associated with myocardial insufficiency. • Circulatory failure – clinical syndrome which is caused by abnormality of the following components of circulation, such as the heart, blood volume, Hb level, vessels.
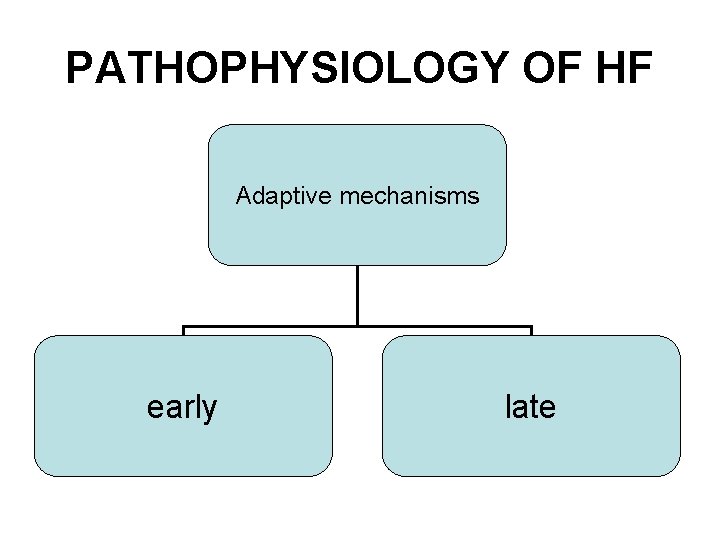
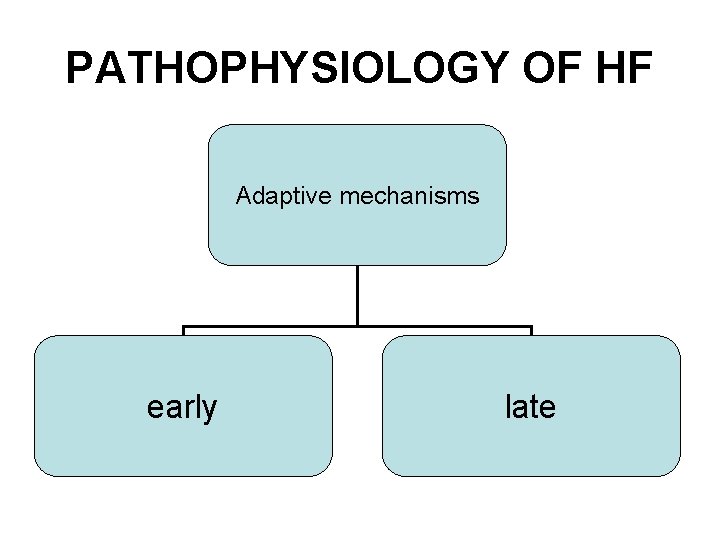
PATHOPHYSIOLOGY OF HF Adaptive mechanisms early late
Early adaptive mechanisms • Frank-Starling mechanism • Activation of neurohormonal systems
NEUROHORMONAL MECHANISMS • Elevation of norepinephrine leading to increased contractility. • Activation of renin-angiotensin-aldosterone system (RAAS). • Activation of arginine-vasopressin system. • Activation of natriuretic peptides (ANP, BNP, CNP). • Elevation of endotheline. • Elevation of cytokines (TNF-α, IL-1β). • NO (NO synthethase –NOS 1 -3). • Elevation of oxidative stress in the myocardium.
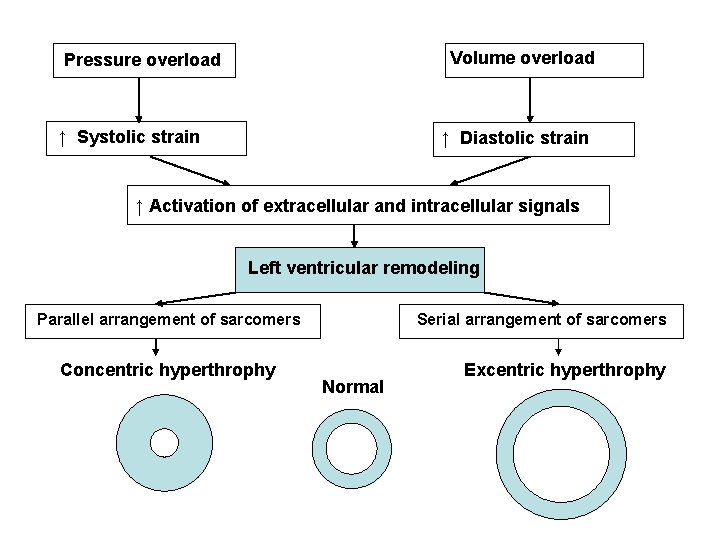
LATE ADAPTIVE MECHANISMS • Left ventricular remodeling
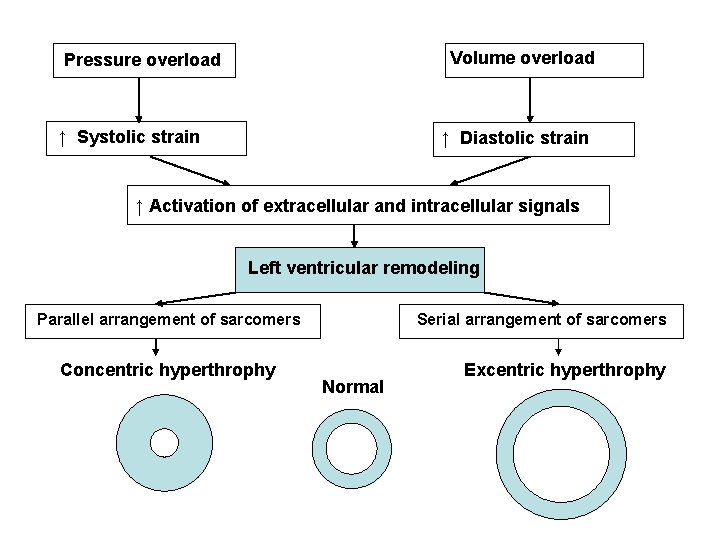
Volume overload Pressure overload ↑ Systolic strain ↑ Diastolic strain ↑ Activation of extracellular and intracellular signals Left ventricular remodeling Parallel arrangement of sarcomers Concentric hyperthrophy Serial arrangement of sarcomers Normal Excentric hyperthrophy
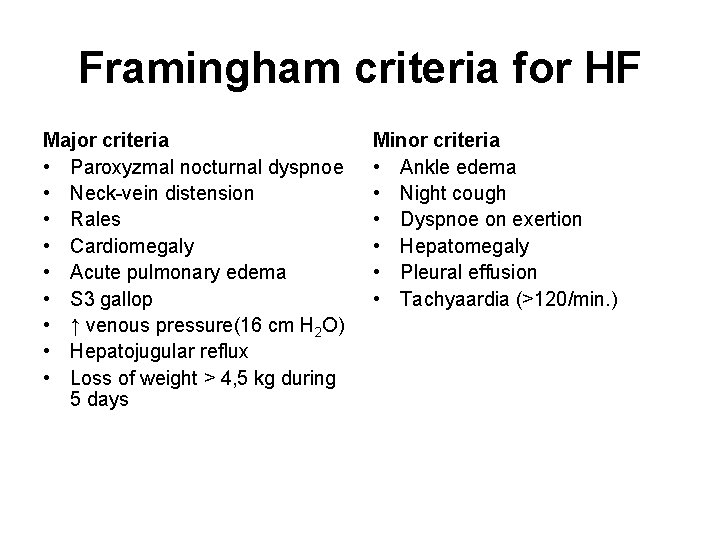
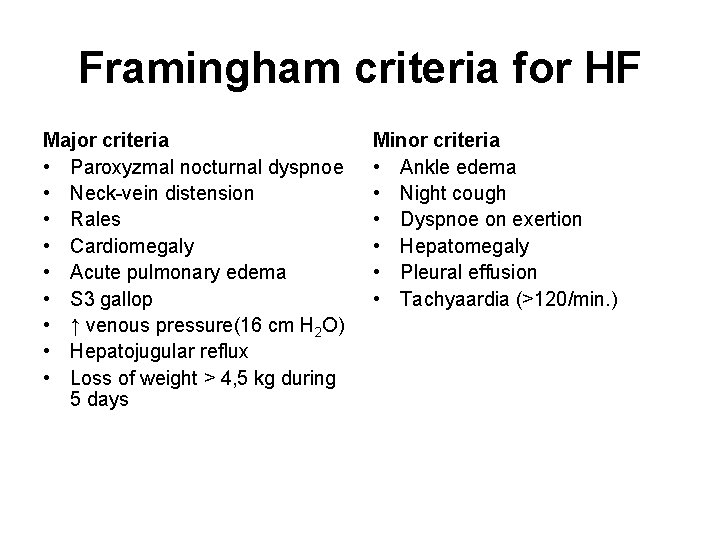
Framingham criteria for HF Major criteria • Paroxyzmal nocturnal dyspnoe • Neck-vein distension • Rales • Cardiomegaly • Acute pulmonary edema • S 3 gallop • ↑ venous pressure(16 cm H 2 O) • Hepatojugular reflux • Loss of weight > 4, 5 kg during 5 days Minor criteria • Ankle edema • Night cough • Dyspnoe on exertion • Hepatomegaly • Pleural effusion • Tachyaardia (>120/min. )
FORMS OF HF • • Right-sided vs left-sided HF Acute vs chronic HF Low-output vs high-output HF Systolic vs diastolic HF
Causes of HF • Pericardial disease (tamponade, constrictive pericarditis) • Valvular heart disease • Disease of the myocardium (dilated CMP) • Coronary heart disease • Arrhythmias (tachycardia-induced CMP)
Treatment of HF Pharmacological Nonpharmacological
Pharmacological treatment • Diuretics • Vasodilators • Positive inotropic agents (digitalis, betablockers, phosphodiesterase inhibitors, Ca -senzitisers) • Neurohormonal inhibitors (ACEI, ARB, beta-blockers)

Nonpharmacological treatment • • Intraaortic balloon contrapulsation Mechanical support CRT Transplantation