Healthy Lives Healthy Futures Programme Update NLAG Trust

- Slides: 10
Healthy Lives, Healthy Futures Programme Update NLAG Trust Board 27 th October 2015

A Common Purpose
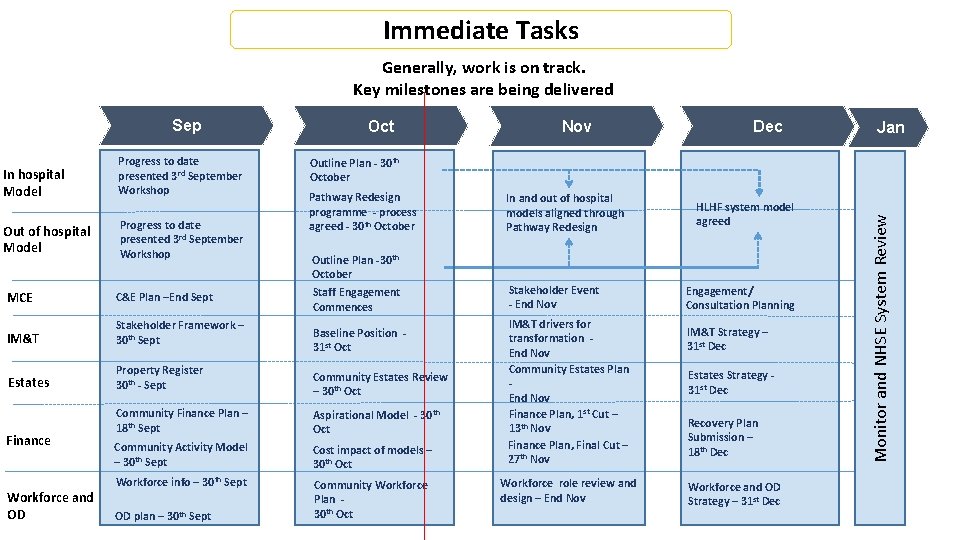
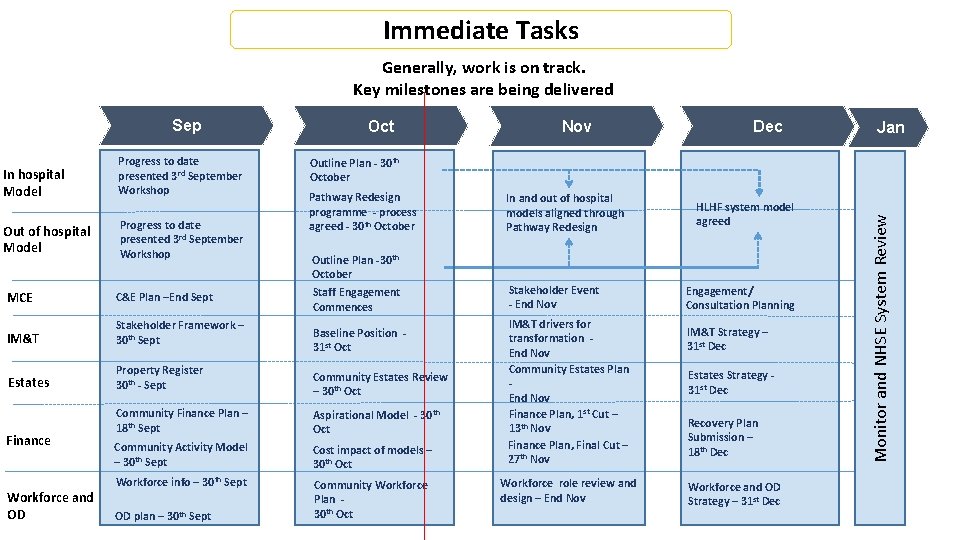
Immediate Tasks Generally, work is on track. Key milestones are being delivered In hospital Model Progress to date presented 3 rd September Workshop Out of hospital Model Progress to date presented 3 rd September Workshop MCE C&E Plan –End Sept IM&T Stakeholder Framework – 30 th Sept Estates Property Register 30 th - Sept Finance Workforce and OD Oct Dec Jan Outline Plan - 30 th October Pathway Redesign programme - process agreed - 30 th October In and out of hospital models aligned through Pathway Redesign Outline Plan -30 th October Staff Engagement Commences Stakeholder Event - End Nov Baseline Position 31 st Oct Community Estates Review – 30 th Oct Community Finance Plan – 18 th Sept Aspirational Model - 30 th Oct Community Activity Model – 30 th Sept Cost impact of models – 30 th Oct Workforce info – 30 th Sept Community Workforce Plan 30 th Oct OD plan – 30 th Sept Nov IM&T drivers for transformation End Nov Community Estates Plan End Nov Finance Plan, 1 st Cut – 13 th Nov Finance Plan, Final Cut – 27 th Nov Workforce role review and design – End Nov HLHF system model agreed Engagement/ Consultation Planning IM&T Strategy – 31 st Dec Estates Strategy 31 st Dec Recovery Plan Submission – 18 th Dec Workforce and OD Strategy – 31 st Dec Monitor and NHSE System Review Sep
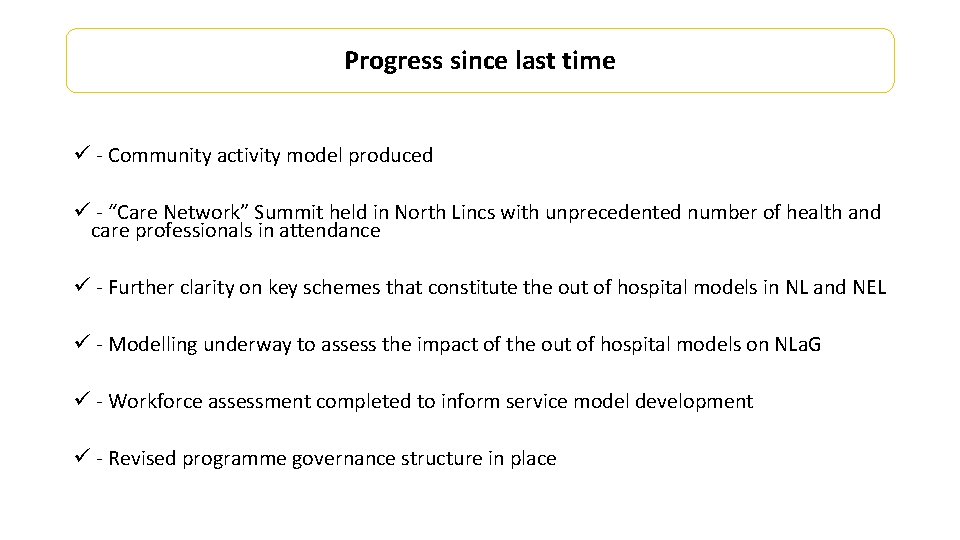
Progress since last time ü - Community activity model produced ü - “Care Network” Summit held in North Lincs with unprecedented number of health and care professionals in attendance ü - Further clarity on key schemes that constitute the out of hospital models in NL and NEL ü - Modelling underway to assess the impact of the out of hospital models on NLa. G ü - Workforce assessment completed to inform service model development ü - Revised programme governance structure in place
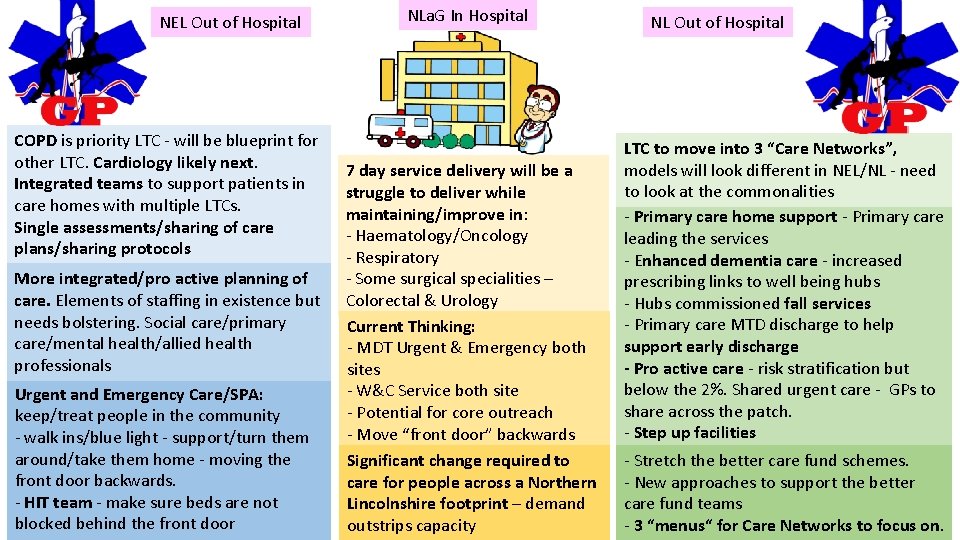
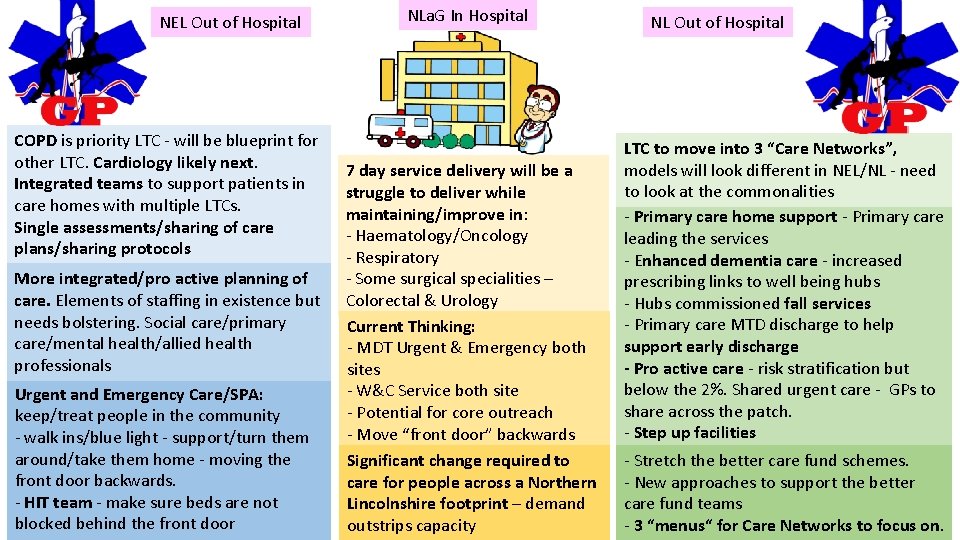
NEL Out of Hospital COPD is priority LTC - will be blueprint for other LTC. Cardiology likely next. Integrated teams to support patients in care homes with multiple LTCs. Single assessments/sharing of care plans/sharing protocols More integrated/pro active planning of care. Elements of staffing in existence but needs bolstering. Social care/primary care/mental health/allied health professionals Urgent and Emergency Care/SPA: keep/treat people in the community - walk ins/blue light - support/turn them around/take them home - moving the front door backwards. - HIT team - make sure beds are not blocked behind the front door NLa. G In Hospital 7 day service delivery will be a struggle to deliver while maintaining/improve in: - Haematology/Oncology - Respiratory - Some surgical specialities – Colorectal & Urology Current Thinking: - MDT Urgent & Emergency both sites - W&C Service both site - Potential for core outreach - Move “front door” backwards Significant change required to care for people across a Northern Lincolnshire footprint – demand outstrips capacity NL Out of Hospital LTC to move into 3 “Care Networks”, models will look different in NEL/NL - need to look at the commonalities - Primary care home support - Primary care leading the services - Enhanced dementia care - increased prescribing links to well being hubs - Hubs commissioned fall services - Primary care MTD discharge to help support early discharge - Pro active care - risk stratification but below the 2%. Shared urgent care - GPs to share across the patch. - Step up facilities - Stretch the better care fund schemes. - New approaches to support the better care fund teams - 3 “menus“ for Care Networks to focus on.
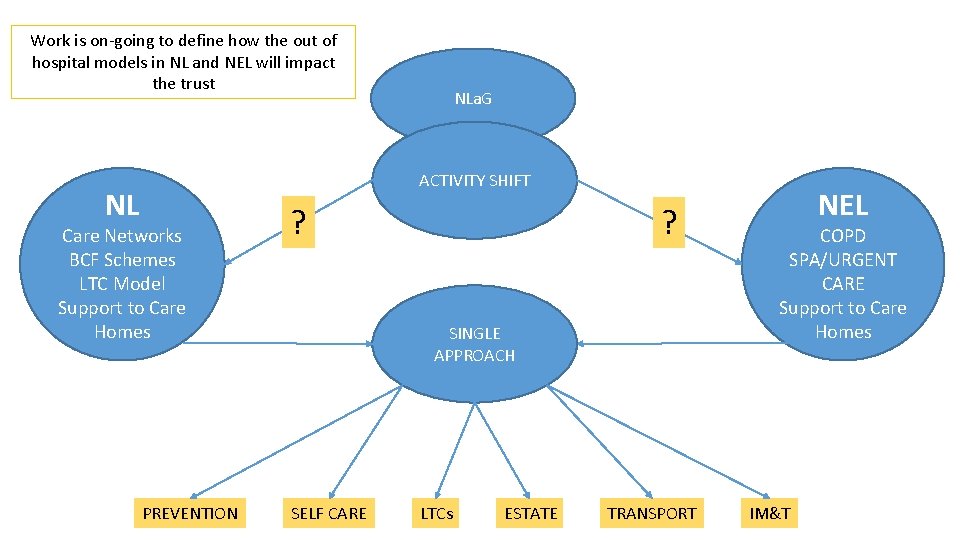
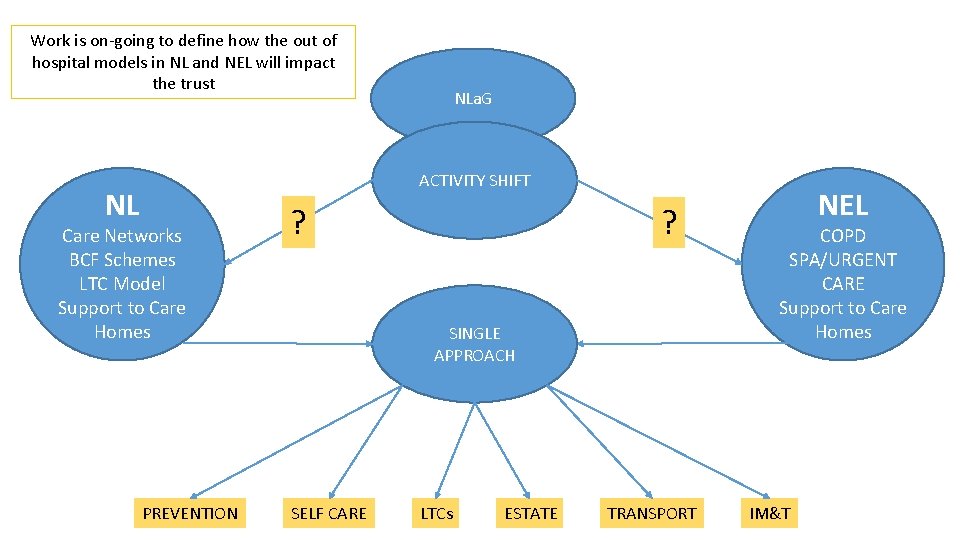
Work is on-going to define how the out of hospital models in NL and NEL will impact the trust NLa. G ACTIVITY SHIFT NL Care Networks BCF Schemes LTC Model Support to Care Homes PREVENTION ? ? SINGLE APPROACH SELF CARE LTCs ESTATE TRANSPORT NEL COPD SPA/URGENT CARE Support to Care Homes IM&T
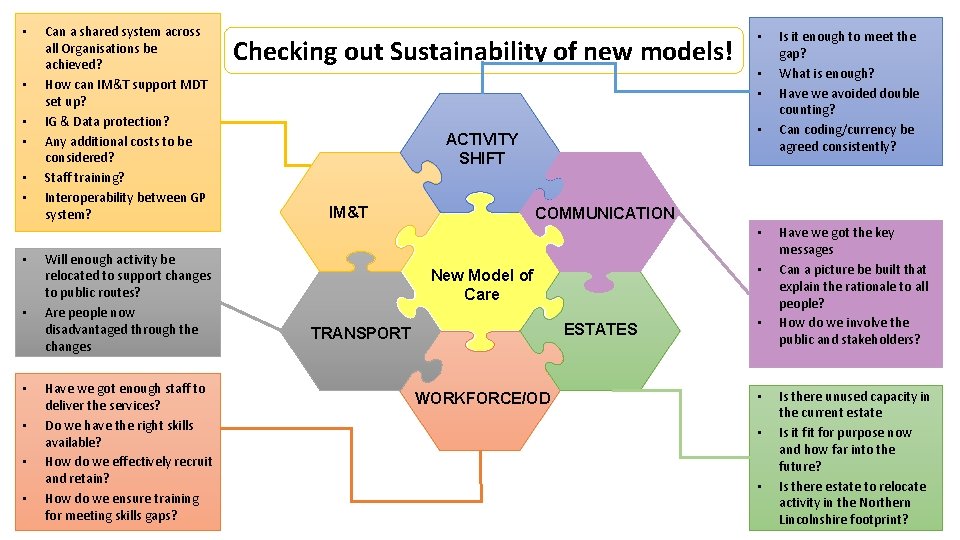
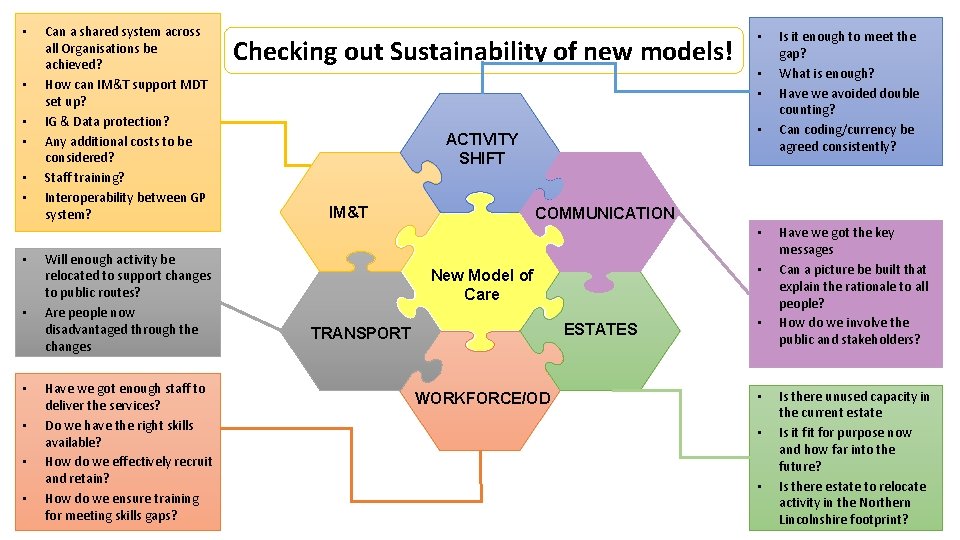
• • • Can a shared system across all Organisations be achieved? How can IM&T support MDT set up? IG & Data protection? Any additional costs to be considered? Staff training? Interoperability between GP system? Checking out Sustainability of new models! • • • ACTIVITY SHIFT IM&T • COMMUNICATION • • Will enough activity be relocated to support changes to public routes? Are people now disadvantaged through the changes Have we got enough staff to deliver the services? Do we have the right skills available? How do we effectively recruit and retain? How do we ensure training for meeting skills gaps? Is it enough to meet the gap? What is enough? Have we avoided double counting? Can coding/currency be agreed consistently? • New Model of Care ESTATES TRANSPORT WORKFORCE/OD • • Have we got the key messages Can a picture be built that explain the rationale to all people? How do we involve the public and stakeholders? Is there unused capacity in the current estate Is it for purpose now and how far into the future? Is there estate to relocate activity in the Northern Lincolnshire footprint?
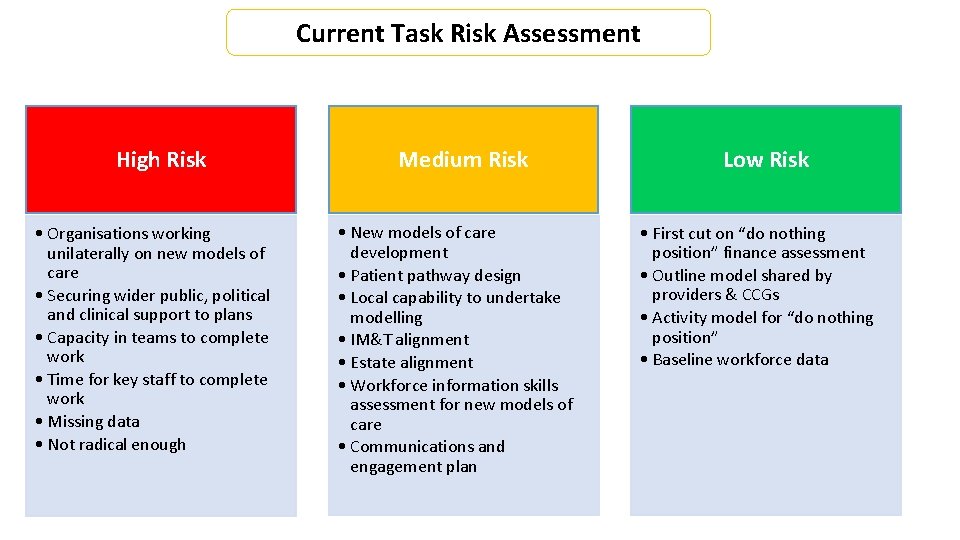
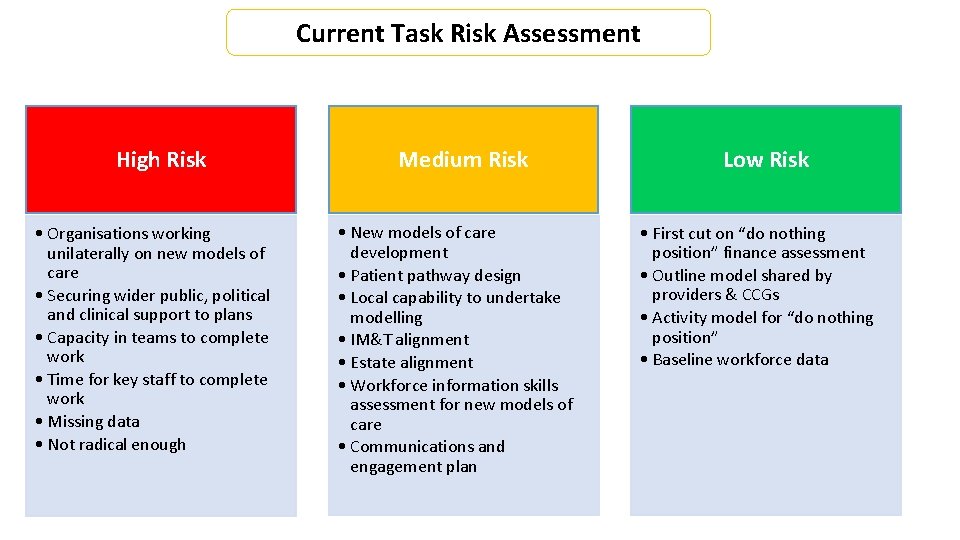
Current Task Risk Assessment High Risk • Organisations working unilaterally on new models of care • Securing wider public, political and clinical support to plans • Capacity in teams to complete work • Time for key staff to complete work • Missing data • Not radical enough Medium Risk • New models of care development • Patient pathway design • Local capability to undertake modelling • IM&T alignment • Estate alignment • Workforce information skills assessment for new models of care • Communications and engagement plan Low Risk • First cut on “do nothing position” finance assessment • Outline model shared by providers & CCGs • Activity model for “do nothing position” • Baseline workforce data
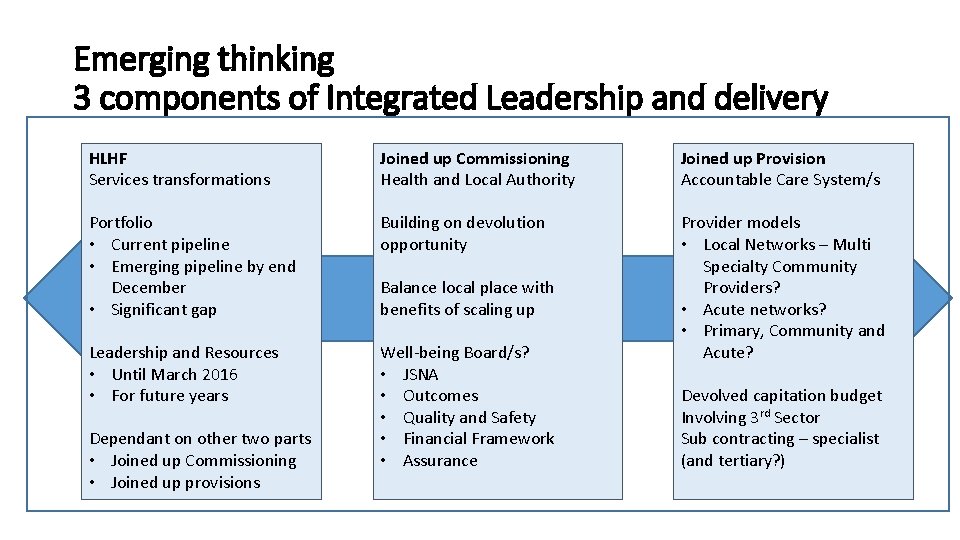
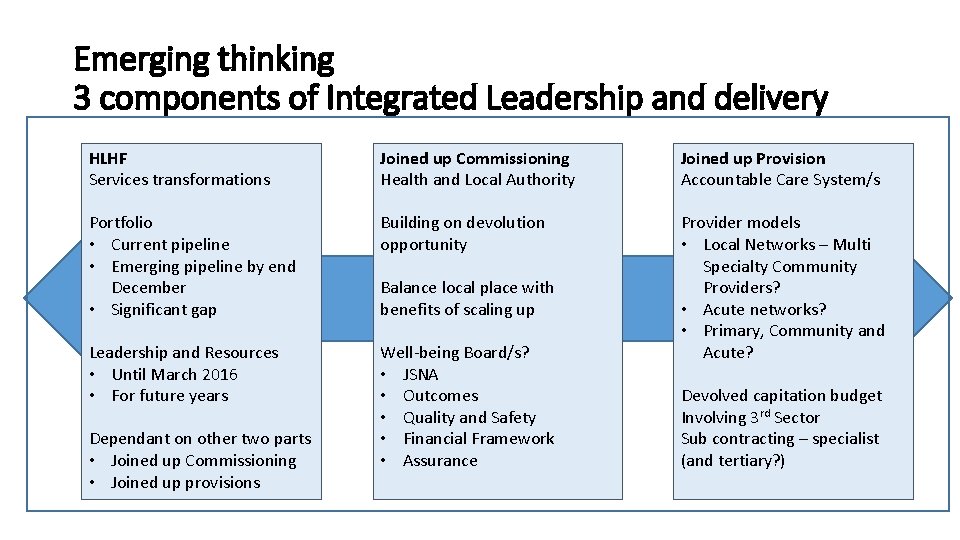
Emerging thinking 3 components of Integrated Leadership and delivery HLHF Services transformations Joined up Commissioning Health and Local Authority Joined up Provision Accountable Care System/s Portfolio • Current pipeline • Emerging pipeline by end December • Significant gap Building on devolution opportunity Leadership and Resources • Until March 2016 • For future years Well-being Board/s? • JSNA • Outcomes • Quality and Safety • Financial Framework • Assurance Provider models • Local Networks – Multi Specialty Community Providers? • Acute networks? • Primary, Community and Acute? Dependant on other two parts • Joined up Commissioning • Joined up provisions Balance local place with benefits of scaling up Devolved capitation budget Involving 3 rd Sector Sub contracting – specialist (and tertiary? )
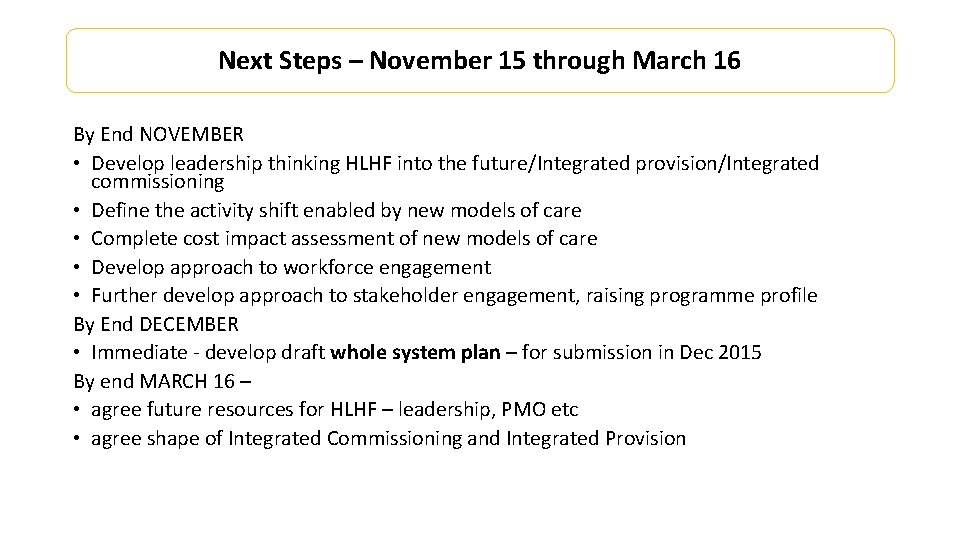
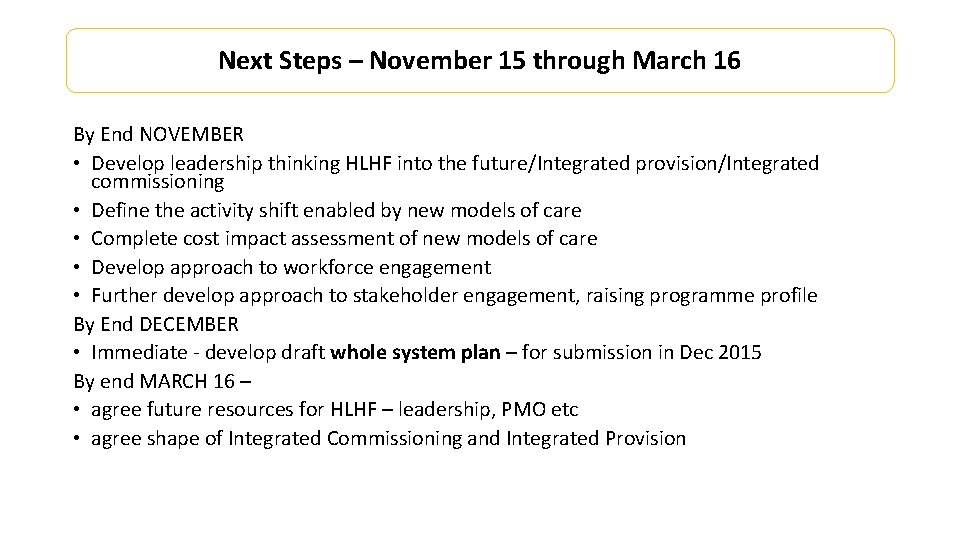
Next Steps – November 15 through March 16 By End NOVEMBER • Develop leadership thinking HLHF into the future/Integrated provision/Integrated commissioning • Define the activity shift enabled by new models of care • Complete cost impact assessment of new models of care • Develop approach to workforce engagement • Further develop approach to stakeholder engagement, raising programme profile By End DECEMBER • Immediate - develop draft whole system plan – for submission in Dec 2015 By end MARCH 16 – • agree future resources for HLHF – leadership, PMO etc • agree shape of Integrated Commissioning and Integrated Provision
 Nlag live
Nlag live Shadow paging recovery technique
Shadow paging recovery technique Northern trust charitable trust
Northern trust charitable trust The national healthy childhood programme
The national healthy childhood programme Healthy soil healthy life poster ideas
Healthy soil healthy life poster ideas Healthy forests healthy communities poster ideas
Healthy forests healthy communities poster ideas Healthy nurse healthy nation
Healthy nurse healthy nation Healthy food healthy mind journal
Healthy food healthy mind journal Nhs futures platform
Nhs futures platform Mechanics of futures market
Mechanics of futures market Managed futures glossary
Managed futures glossary